Abstract
Background
COVID-19 has greatly impacted older adults with pre-existing noncommunicable conditions (hereafter called pre-existing conditions) in terms of their access to essential healthcare services. Based on the theory of vertical health equity, this study investigated access to healthcare by Nepali older adults with pre-existing conditions during the COVID-19 pandemic.
Methods
A cross-sectional study surveyed 847 randomly selected older adults (≥60 years) in three districts of eastern Nepal. Survey questionnaires, administered by trained community health workers, collected information on participants reported difficulty obtaining routine care and medications during the pandemic, in addition to questions on demographics, socioeconomic factors and pre-existing conditions. Cumulative scores for pre-existing conditions were recoded as no pre-existing condition, single condition and multimorbidity for the analyses. χ2 tests and binary logistic regressions determined inferences.
Results
Nearly two-thirds of the participants had a pre-existing condition (43.8% single condition and 22.8% multimorbid) and reported experiencing difficulty obtaining routine care (52.8%) and medications (13.5%). Participants with single (OR 3.06, 95% CI 2.17 to 4.32) and multimorbid (OR 5.62, 95% CI 3.63 to 8.71) conditions had threefold and fivefold increased odds of experiencing difficulty accessing routine care. Findings were similar for difficulty obtaining medication (OR single: 3.12, 95% CI 1.71 to 5.69; OR multimorbid: 3.98, 95% CI 2.01 to 7.87) where odds were greater than threefolds.
Conclusions
Older adults with pre-existing conditions in Nepal, who require routine medical care and medication, faced significant difficulties obtaining them during the pandemic, which may lead to deterioration in their pre-existing conditions. Public health emergency preparedness should incorporate plans for both managing the emergency and providing continuing care.
Keywords: COVID-19, epidemiology, health policy, public health
Strengths and limitations of this study.
The study is one of its first kind from Nepal to assess challenges in healthcare access amidst the pandemic among older adults with non-communicable diseases.
Large sample size and data collection by trained community health workers add to the reliability of the data.
Cross-sectional study design limits causality inferences.
The information on pre-existing conditions was self-reported and may be underestimated.
Generalisability is limited due to the inclusion of three districts from Eastern Nepal.
Background
In Nepal, a South Asian country nestled in the Himalayas between India and China, population ageing is a relatively new yet rapidly expanding issue. Consistent with the United Nation’s definition, Nepal’s Senior Citizens Act1 identified individuals aged 60 and older as senior citizens. In accordance with the global trend, Nepal has been observing a continuous decline in mortality rates and an increase in life expectancy from 54.3 to 66.6 years between 1991 and 2011.2 Although the overall national population growth rate is declining, that of the older population is increasing and exceeds the national average growth rate (1.4% vs 3.1%).2 Furthermore, from 1991 to 2011, Nepal, in late demographic transition, has experienced a significant increase in the ageing index (from 13.6 to 23.3) and median age (from 18.9 to 22.3 years), reminding the society to be prepared to address the social, economic and health needs of burgeoning Nepali older adults.2 While population ageing is an emerging and neglected topic in Nepal,3 the increased vulnerability of the older population due to the ongoing pandemic has provoked us to revisit their health needs.
Nepal experienced an epidemiological shift in terms of declining burden of communicable diseases and a growing burden of non-communicable diseases (NCDs) in the last decade.4 This means that a significant share of the population has been living for many years with chronic conditions, increasing the burden on Nepal’s limited health resources.5 Among older age groups (50 and older), in 2017, NCDs contributed to 55.3% of the disease burden in Nepal.6 In addition to single NCDs, the prevalence of multimorbidity or the presence of two or more chronic conditions is increasing, both globally and in Nepal.7 8 Multimorbidity is often more challenging than a single condition because of the synergistic impact of multiple conditions, each of which may require a multitude of specialists’ referrals, biomedical investigations and treatments.9 Although nationwide estimates for multimorbidity are unavailable, estimates from rural parts of Eastern Nepal suggest that one in seven older adults had multimorbid chronic conditions.7
Nepal has experienced a series of COVID-19 outbreaks; more recently, the Delta strain, which has worsened the COVID-19 situation in Nepal. As of 6 July 2021, the pandemic has claimed 9263 lives out of 648 085 positive cases in Nepal10; the highest proportion of deaths (67.8%) reported among older adults (>54 years), and all the deceased older adults had at least one pre-existing condition.11 In Nepal, cardiovascular diseases, diabetes and respiratory illness were the most common conditions linked to COVID-19 deaths.12
Through its commitment to Sustainable Development Goals (SDGs), Nepal aims to reduce premature deaths due to NCDs by one-third by 2030.13 People with one or more NCDs have extensive and diverse health-related needs and require continuity of care, self-management, medication adherence, and often seek repeated and regular interactions with the health system.14 Horizontal health equity advocates for equal access to healthcare. In contrast, vertical health equity is defined as the principle that advocates for access to healthcare based on an individual’s needs, that is, those with greater needs should have greater access to healthcare.15 Since those with one or more health problems have greater health needs than those without a health condition, they should have greater access to healthcare. Moreover, the needs are even greater for those with multimorbidity. In the context of our study, the principle of vertical health equity is violated if those with one or more pre-existing NCDs experience greater challenges to access healthcare.
Despite the high needs, Nepal ranks far below the average in the Universal Health Coverage index16, meaning that individuals and communities in Nepal do not have access to quality essential health services due to financial hardship. The COVID-19 pandemic may have further jeopardised healthcare access. On one hand, the nationwide lockdown, imposed by the Nepal government as a measure of mass quarantine to contain the COVID-19, may have aggravated the risk factors for NCDs, such as sedentary lifestyles, unhealthy diets, smoking, alcohol, tobacco use, lack of sleep, non-compliance to medications, etc.17–19 On the other hand, it has resulted in the closure of services connected to day-to-day life like transportation, markets, city centres and general health checkups in hospitals.20 Due to the lockdowns, people have had difficulties not just fulfilling their everyday needs but also accessing healthcare in the absence of transport services.21 Consequently, a rapid decrease in the number of per-day patient visits was noted during the lockdown.22 Healthcare was inaccessible even pre-COVID, but at that time, it was tightly linked to income. During the COVID-19 lockdowns, even those who could afford healthcare were deprived of access.20 Although the impact of COVID-19 is yet to be fully understood, inaccessible healthcare due to the COVID-19 pandemic may lead to a deterioration in pre-existing conditions, increase the severity of disease and disability, escalate premature deaths and contribute to major economic loss for the country.23
Previous studies from India, Bangladesh and Hong Kong have reported difficulty accessing healthcare and/or obtaining medication during the pandemic.24–26 Although the previous literature from Nepal has suggested disruptions in health services amidst the pandemic,20 it is unknown from patients’ perspectives how much difficulty they experienced accessing healthcare amidst the pandemic. Framing the current study within the principle of vertical health equity, we aim to assess the relationships between pre-existing conditions and challenges in obtaining routine healthcare and medications during the COVID-19 pandemic among older adults in eastern Nepal.
Methodology
This study is reported following the STrengthening the Reporting of OBservational studies in Epidemiology
(STROBE) guidelines27 (online supplemental table 1).
bmjopen-2021-056342supp001.pdf (96KB, pdf)
Study design and study participants
This study followed a cross-sectional design and surveyed 847 randomly selected older adults between July and September 2020; further detailed elsewhere.28 Using an unknown prevalence of 50%, 5% precision, a design effect of 2 and a non-response rate of 5.0%, the minimum required sample size was calculated to be 847. Multistage cluster sampling was used for selecting participants. In the first stage, the three districts of province 1 in eastern Nepal, namely Morang, Pachthar and Terathum (figure 1), were randomly selected. While Morang lies in the southern plains, Pachthar and Terathum are hilly districts. The population and key infrastructure indicators for these districts are provided in online supplemental table 2. Briefly, the three study districts have a higher literacy rate and access to sanitary toilets than the national average. While Morang district is above the national average in terms of urbanisation and access to electricity and improved drinking water sources, the other two districts, Pachthar and Terathum, are below the national average (online supplemental table 2). In the second stage, one urban and one rural municipality were randomly selected in each district. Next, from each municipality, three wards (lowest administrative units in Nepal) were randomly selected, and in the final stage, participants were randomly selected from each ward. Nepali nationals who were residents in the study area for a minimum of a year and aged ≥60 years were included. Those in institutional settings and with significant hearing and communication problems that interfered with the survey were excluded.
Figure 1.
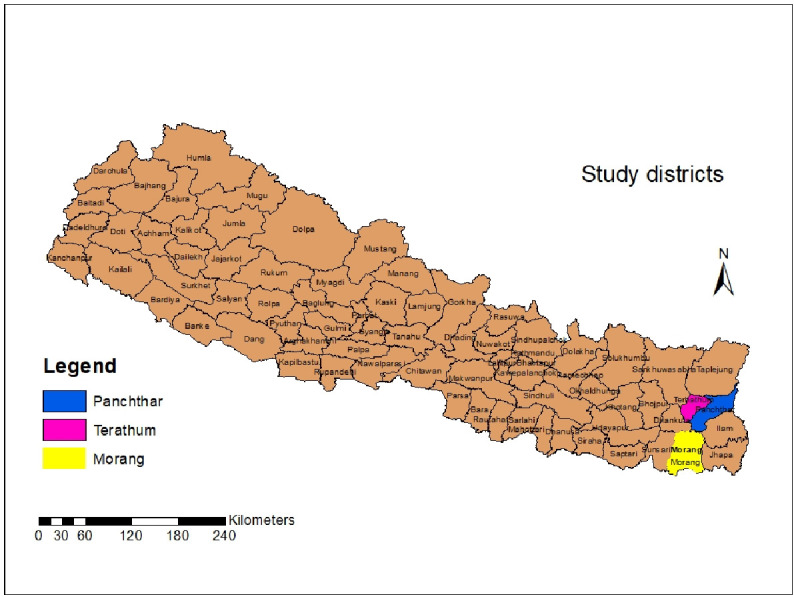
Map of Nepal highlighting the three study districts in the eastern region.
Data collection and study tools
Surveyors were community health workers, certified in General Medicine and employed by the Nepal government in the selected study areas. Surveyors received two sessions of orientations via zoom, each 4 hours long, on study methodology, tools, ethics and field logistics. Following standard COVID-19 protocols implemented by national and local governments, surveyors visited households and conducted face-to-face interviews using a questionnaire implemented in the KoBoToolbox mobile app. A common group in WhatsApp was used to share and troubleshoot any field problems and to provide consistent information to all field enumerators. Initially developed in English, the study tool was translated into Nepali and pretested among ten older adults.
Study variables
Dependent variable
There were two outcome variables: whether participants faced difficulty obtaining (1) routine medical care and (2) prescribed medicines because of the COVID-19 pandemic. For each item, participants expressed their level of difficulty in the four-response Likert scale (‘none,’ ‘some,’ ‘very much,’ ‘unable’), which were then dichotomised as no difficulties or difficulties faced (responses ‘some,’ ‘very much,’ ‘unable’).
Independent variables
The main independent variable of interest was the presence of pre-existing conditions. Participants were asked if they had any pre-existing conditions diagnosed by a health professional and/or taking any prescription medications for that condition. In multiple response type questions, participants selected all the applicable conditions. Finally, via an open-ended follow-up question, they were asked to specify any other conditions that were not already captured. A cumulative score for all the conditions was calculated for each participant and was categorised into no pre-existing conditions, single condition and multimorbidity. Definition of chronic conditions is tabulated in online supplemental table 3.
Covariates
Other variables included age, sex, marital status, ethnicity, education, urban/rural residence, current occupation, living arrangement, proximity to the health centre, financial hardships to access healthcare, and recipient of social security allowance. All these covariates were categorical with response levels as specified in table 1.
Table 1.
Characteristics of the study participants—overall and by their experiences in obtaining healthcare during the COVID-19 pandemic
| Overall n (%) (N=843) | Difficulty obtaining healthcare N (%) | Difficulty obtaining medications n (%) | |||||
| Yes (n=445, 52.8%) |
No (n=398, 47.2%) |
*P value | Yes (n=114, 13.5%) |
No (n=729, 86.5%) |
*P value | ||
| Age in years | |||||||
| 60–69 | 383 (45.4) | 164 (36.9) | 219 (55.0) | <0.001 | 35 (30.7) | 348 (47.7) | 0.001 |
| 70–79 | 315 (37.4) | 189 (42.5) | 126 (31.7) | 59 (51.8) | 256 (35.1) | ||
| 80+ | 145 (17.2) | 92 (20.7) | 53 (13.3) | 20 (17.5) | 125 (17.1) | ||
| Sex | |||||||
| Female | 412 (48.9) | 229 (51.5) | 183 (46.0) | 0.112 | 44 (38.6) | 368 (50.5) | 0.018 |
| Male | 431 (51.1) | 216 (48.5) | 215 (54.0) | 70 (61.4) | 361 (49.5) | ||
| †Marital status | |||||||
| Married | 639 (75.8) | 321 (72.1) | 318 (79.9) | 0.009 | 93 (81.6) | 546 (74.9) | 0.121 |
| Without partner | 204 (24.2) | 124 (27.9) | 80 (20.1) | 21 (18.4) | 183 (25.1) | ||
| Ethnicity | |||||||
| Brahmins/Chhetri | 266 (31.6) | 159 (35.7) | 107 (26.9) | 0.006 | 18 (15.8) | 248 (34.0) | <0.001 |
| Minorities and others | 577 (68.4) | 286 (64.3) | 291 (73.1) | 96 (84.2) | 481 (66.0) | ||
| Education | |||||||
| No formal schooling | 577 (68.4) | 298 (67.0) | 279 (70.1) | 0.328 | 70 (61.4) | 507 (69.5) | 0.082 |
| Formal schooling | 266 (31.6) | 147 (33.0) | 119 (29.9) | 44 (38.6) | 222 (30.5) | ||
| Residence | |||||||
| Rural | 370 (43.9) | 204 (45.8) | 166 (41.7) | 0.227 | 114 (100.0) | 256 (35.1) | NA |
| Urban | 473 (56.1) | 241 (54.2) | 232 (58.3) | 0 | 473 (64.9) | ||
| Current occupation | |||||||
| Agriculture | 400 (47.4) | 231 (51.9) | 169 (42.5) | 0.001 | 88 (77.2) | 312 (42.8) | <0.001 |
| Non-agriculture | 169 (20.0) | 68 (15.3) | 101 (25.4) | 12 (10.5) | 157 (21.5) | ||
| Housewife/retired | 274 (32.5) | 146 (32.8) | 128 (32.2) | 14 (12.3) | 260 (35.7) | ||
| Living arrangement | |||||||
| Live alone | 92 (10.9) | 51 (11.5) | 41 (10.3) | 0.590 | 11 (9.6) | 81 (11.1) | 0.642 |
| Live with family | 751 (89.1) | 394 (88.5) | 357 (89.7) | 103 (90.4) | 648 (88.9) | ||
| Walking proximity to the nearest health centre | |||||||
| <30 min | 272 (32.3) | 124 (27.9) | 148 (37.2) | 0.006 | 41 (36.0) | 231 (31.7) | 0.000 |
| 30–60 min | 372 (44.1) | 201 (45.2) | 171 (43.0) | 32 (28.1) | 340 (46.6) | ||
| >60 min | 199 (23.6) | 120 (27.0) | 79 (19.8) | 41 (36.0) | 158 (21.7) | ||
| Financial hardships with healthcare | |||||||
| No | 379 (45.0) | 184 (41.3) | 195 (49.0) | 0.026 | 65 (57.0) | 314 (43.1) | 0.005 |
| Yes | 464 (55.0) | 261 (58.7) | 203 (51.0) | 49 (43.0) | 415 (56.9) | ||
| Receiving social security allowance | |||||||
| No | 409 (48.5) | 185 (41.6) | 224 (56.3) | <0.001 | 51 (44.7) | 358 (49.1) | 0.385 |
| Yes | 434 (51.5) | 260 (58.4) | 174 (43.7) | 63 (55.3) | 371 (50.9) | ||
| Pre-existing (NCDs) conditions | |||||||
| None | 282 (33.5) | 84 (18.9) | 198 (49.7) | <0.001 | 17 (14.9) | 265 (36.4) | <0.001 |
| Single condition | 369 (43.8) | 220 (49.4) | 149 (37.4) | 60 (52.6) | 309 (42.4) | ||
| Multimorbidity | 192 (22.8) | 141 (31.7) | 51 (12.8) | 37 (32.5) | 155 (21.3) | ||
*P values from a χ2 test comparing participants experiencing and not experiencing difficulty.
†Includes widowed, separated and never married.
NCDs, non-communicable diseases.
Patient and public involvement
Patients and the public were not involved in the design of the study and interpretation of the results.
Statistical analyses
All analyses are performed separately for each of the two dependent variables: access to (1) routine care and (2) medications. Since all our variables were categorical, they are summarised in table 1 in terms of frequencies and percentages, and the group differences were evaluated using χ2 tests. Binary logistic regression analysis assessed if participants’ pre-existing conditions were associated with difficulty obtaining healthcare. A stepwise selection method, using Akaike information criterion (AIC) criteria, was used for model selection and started with all the covariates reported in table 1 while only retaining, in the final model, age, ethnicity, residence, occupation, walking proximity to the nearest health centre, and financial hardships with healthcare. The Variance Inflation Factor (VIF) for each variable included in the final model was below 2 suggesting no multicollinearity issues. Adjusted and unadjusted ORs and 95% CIs are reported in table 2. All statistical analyses were conducted using SAS V.9.4.
Table 2.
Association between pre-existing (NCDs) conditions and difficulty obtaining healthcare and medications
| Difficulty obtaining healthcare | Difficulty obtaining medications | |||
| Unadjusted OR (95% CI) |
*Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
†Adjusted OR (95% CI) |
|
| ‡Pre-existing (NCDs) conditions | ||||
| None | Reference | Reference | ||
| Single condition | 3.48 (2.50 to 4.84) | 3.06 (2.17 to 4.32) | 3.03 (1.72 to 5.31) | 3.12 (1.71 to 5.69) |
| Multimorbidity | 6.52 (4.33 to 9.81) | 5.62 (3.63 to 8.71) | 3.72 (2.03 to 6.83) | 3.98 (2.01 to 7.87) |
*Adjusted for age, ethnicity, residence, occupation, walking proximity to the nearest health centre, and financial hardships with healthcare.
†Adjusted for age, ethnicity, occupation, walking proximity to the nearest health centre and financial hardships with healthcare.
‡Statistically significant ORs are bolded.
NCDs, non-communicable diseases.
Results
Participants’ characteristics
Data were collected from 843 of the approached 847 participants (a response rate of 99.5%). The largest proportion of the participants were in their sixties (45.4%), male (51.1%), married (75.8%), minorities (68.4%), without formal schooling (68.4%), urban residents (56.1%), involved in agriculture (47.4%) and living with family (89.1%) (table 1). More than half of the participants faced financial hardship (55.0%) and received social security allowances (51.5%). Only one-third of the participants were free of pre-existing NCDs conditions; 43.8% had single and 22.8% had multiple conditions (table 1).
More than half of the participants reported facing difficulty obtaining healthcare (p=52.8%, 95% CI 49.4% to 56.2%) and 13.5% (95% CI 11.2% to 15.8%) reported facing difficulty obtaining medications. In bivariate analyses, among the covariates, age, ethnicity, occupation, walking proximity to the nearest health centre, and financial hardships with healthcare were significantly associated with both of the outcome variables (table 1); interestingly, only rural residents reported experiencing difficulties obtaining medications.
Association between pre-existing conditions and difficulty obtaining healthcare and medications during COVID-19
In bivariate analysis, participants’ pre-existing conditions were significantly associated with their reported difficulty getting routine healthcare and medications (p<0.001) (table 1). In the regression analyses (table 2), participants’ pre-existing condition was significantly associated with difficulty obtaining healthcare and medications in both adjusted and unadjusted models. Notably, the strength of the association was greater for those with multimorbidity than those with single conditions. After adjusting for the covariates, compared with participants without any pre-existing conditions, those with single (OR 3.06, 95% CI 2.17 to 4.32) and multiple (OR 5.62, 95% CI 3.63 to 8.71) conditions, respectively, had about three times and six times higher odds of experiencing difficulties in obtaining routine healthcare. Likewise, for medications, those with single (OR 3.12, 95% CI 1.71 to 5.69) and multiple (OR 3.98, 95% CI 2.01 to 7.87) conditions had more than three times increased odds of experiencing difficulties in obtaining medications (table 2).
Discussion
This study found a significant positive association between participants’ pre-existing conditions and difficulty obtaining both routine healthcare and medications during the COVID-19 pandemic in three studied districts of eastern Nepal. Those with multiple conditions were even more likely to experience difficulty accessing healthcare than those with single conditions despite their likely increased need.
Although people with pre-existing conditions require routine medical checkups and medication, both during and after the pandemic, our participants faced significant difficulty obtaining them. This study is the first of its kind in Nepal, and a similar study is unavailable for direct comparison. However, our findings align with studies conducted in India25 and Hong Kong24 among the general population and Bangladesh among the older population,26 which also reported significant challenges faced by those with pre-existing conditions to access healthcare during the pandemic. In India, participants missed follow-up visits, and experienced difficulty in medication procurement, resulting in a worsening of pre-existing symptoms.29
Acknowledging that inaccessible healthcare is a long-term problem in Nepal, existent even prior to the COVID-19 pandemic, several factors, at both the microlevels and macrolevels, help explain why healthcare was not easily accessible to our participants. We believe the restricted movement and cessation of public transportation, imposed as part of the nationwide lockdown, to be the most important barrier to access. As a preventive measure to curb the spread of the virus, Nepal’s government imposed several intermittent nationwide lockdowns of varying lengths. In a country where the majority rely on public transportation and a private vehicle is a privilege enjoyed only by the rich, cessation of public transportation meant that people with existing conditions had no means to reach health facilities, especially in rural areas where facilities are distant. In the current pandemic, it is obvious that an ill-equipped health system may not have been able to maintain essential services because of limited human resources for health (HRH) or shifting of HRH from primary healthcare (PHC) to COVID-19 management centres/hospitals. Furthermore, there were reported interruptions in health service delivery amidst the pandemic23 due to the closure of peripheral healthcare facilities (such as PHCs, health posts) and fears of COVID-19 transmission among healthcare workers.20 23 A rapid assessment of 163 countries by the WHO on the impact of the COVID-19 pandemic on NCDs resources and services revealed a considerable disruption to NCDs services in many countries, and in some South Asian countries, the government funds for NCDs were reallocated to COVID-19 treatment and management.23
The pandemic has been overwhelming, but we know that its impact is likely to wane over the next few years. So, what are the implications of our findings beyond the COVID-19 pandemic? The broader implications of our findings should be contextualised within the context of historical, contemporary and inevitable future outbreaks and public health emergencies. Although ‘We are all in this together’ was a highly popularised phrase during the pandemic, evidence suggests significant inequalities in severe morbidity and mortality during a pandemic, whereby certain age groups, minorities and those with low socioeconomic status bear the greater impact, as noted during the 1918 Spanish influenza pandemic, the 2009 H1N1 outbreak and the current COVID-19 pandemic.30 31 The noted disparities, on the grounds of social determinants of health, point to the gaps in our emergency preparedness and the failure of society to protect the most vulnerable in a time of catastrophe.
Although focusing on curative and preventive strategies to curb the pandemic is important, it should be noted that health systems have dual responsibilities in both responding to the outbreak as well as providing essential health services, especially to those with greater needs, such as older adults with NCDs. As demonstrated by previous32 33 and current studies, the latter was neglected in many countries, thus depriving people with NCDs of access to continuing care and essential medications. Acknowledging that Nepal government has provisions to provide universal healthcare and essential medicines, at the policy level, Nepal’s COVID-19 response plan has no specific prioritisation and provisions for either older adults and/or people with NCDs.34 Policy-makers in Nepal should recognise that the impact of the COVID-19 pandemic can only be mitigated if strategies to provide essential routine services to their vulnerable population are in place. These strategies should be informed by epidemiological data, health system capacity, and available resources during health crises. Given the disruption of healthcare access during the COVID-19 pandemic, there is a need to codesign and evaluate new models of care with the engagement of key stakeholders, citizens, local developmental partners and decision-makers. These models of care should be designed in a way that it can meet the health needs of the population during and beyond the pandemic. One important strategy is putting PHC at the centre of an emergency response plan to address the healthcare needs at the community level. There is an opportunity to focus on developing alternative pathways to deliver health services and essential drugs such as door-to-door services, mobilising community health workers, expanding telehealth or mobile health and remote health consultations.23
Strength, limitations and generalisability of the findings
This study is one of its first kind from Nepal to assess challenges to healthcare access amidst the pandemic among older adults with NCDs. Large sample size, the inclusion of both urban and rural areas, and data collection by trained community health workers add to the reliability of the data. However, this study also has some limitations. The first is that due to the cross-sectional study design, it is not possible to infer causality. However, the questionnaire did ask respondents to respond to questions with reference to ‘compared with before COVID-19’ and ‘due to COVID-19’; thus, the responses reflected their view of changes that had occurred. The information on pre-existing conditions was self-reported, and we believe it to be underestimated because, in the Nepali context, it is common to access healthcare only when the symptoms are obvious and severe. Hence, many of our participants may not be aware of their subclinical conditions, which may have introduced misclassification bias in the measurements, thereby underestimating the true burden of pre-existing conditions. The study includes a large proportion of participants from a minority background and does not represent the general Nepali population, thus limiting the generalisability of study findings. Additionally, the study districts are in hills and plain areas of eastern Nepal, and thus, the findings may not be generalisable to other settings of Nepal. Our study did not assess reasons for access problems, and future studies, employing a mixed-method approach, should explore the underlying reasons for inaccessibility.
Conclusions
Nepali older adults with one or more pre-existing conditions, despite their higher health needs, faced more difficulties obtaining routine healthcare and medications during the COVID-19 pandemic, which is against the principle of vertical health inequity. Policy-makers, healthcare practitioners and local stakeholders should be cognizant of the existing inequality in healthcare and urgently address the gaps in healthcare accessibility for older adults with NCDs. The broader consequences of inaccessible healthcare during the pandemic and its subsequent impact on Nepal’s commitment to the attainment of SDG-3 of reducing NCDs burden by one-third by 203013 is yet to be fully understood. Yet, the pandemic reminds us to revisit our national emergency preparedness and revise future planning using a more holistic approach, addressing both emerging and existing healthcare needs.
Supplementary Material
Footnotes
Twitter: @UNYadav_
Contributors: UNY, SG and SKM conceived the idea. UNY, OPY and SKM collected the data. SG, AS and UNY analysed the data. SG, AS, BC, SKM, OPY, AMA, LBR, PY and UNY drafted the first draft. MFH reviewed the first draft and provided significant contribution to in improving the piece. All authors contributed significantly and approved the final version.
UNY accepts full responsibility for the finished work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
Nepal Health Research Council approved the original study, and the Institutional Review Board at Miami University exempted this secondary data analysis. Participants provided written consent prior to data collection. For participants unable to read and write, a guardian provided proxy written consent. Participants gave informed consent to participate in the study before taking part.
References
- 1.Nepal Law Commission . Senior citizens act, 2063 (2006). Kathmandu, 2006. [Google Scholar]
- 2.Nepal ed . Population monograph of Nepal. Kathmandu: Government of Nepal, National Planning Commission Secretariat, Central Bureau of Statistics, 2014. [Google Scholar]
- 3.Shrestha L. Geriatric health in Nepal: concerns and experience. Nepal Med Coll J 2013;15:148–52. [PubMed] [Google Scholar]
- 4.Sharma SR, Page R, Matheson A, et al. Non-Communicable disease prevention in Nepal: systemic challenges and future directions. Glob Health Promot 2019;26:94–7. 10.1177/1757975917720800 [DOI] [PubMed] [Google Scholar]
- 5.Mishra SR, Shrestha N, Gyawali B. The changing patterns of non-communicable diseases and injuries in Nepal from 1990-2017: a review of evidence from global burden of disease study 2017. In Review 2020. [Google Scholar]
- 6.Roser M, Ritchie H. Burden of Disease. In: Our world in data, 2016. [Google Scholar]
- 7.Yadav UN, Ghimire S, Mistry SK, et al. Prevalence of non-communicable chronic conditions, multimorbidity and its correlates among older adults in rural Nepal: a cross-sectional study. BMJ Open 2021;11:e041728. 10.1136/bmjopen-2020-041728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Souza DLB, Oliveras-Fabregas A, Minobes-Molina E, et al. Trends of multimorbidity in 15 European countries: a population-based study in community-dwelling adults aged 50 and over. BMC Public Health 2021;21:76. 10.1186/s12889-020-10084-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 2011;10:430–9. 10.1016/j.arr.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health and Population, Nepal . COVID19-Dashboard. Available: https://covid19.mohp.gov.np/
- 11.Rayamajhee B, Pokhrel A, Syangtan G, et al. How well the government of Nepal is responding to covid-19? an experience from a resource-limited country to confront unprecedented pandemic. Front Public Health 2021;9:597808. 10.3389/fpubh.2021.597808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panthee B, Dhungana S, Panthee N, et al. Clinical and epidemiological features of COVID-19 deaths in Nepal. New Microbes New Infect 2020;38:100797. 10.1016/j.nmni.2020.100797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Nations . Transforming our world: the 2030 agenda for sustainable development. [Google Scholar]
- 14.Hopman P, Schellevis FG, Rijken M. Health-Related needs of people with multiple chronic diseases: differences and underlying factors. Qual Life Res 2016;25:651–60. 10.1007/s11136-015-1102-8 [DOI] [PubMed] [Google Scholar]
- 15.O’Donnell O, van Doorslaer E, Wagstaff A. Analyzing health equity using household survey data: a guide to techniques and their implementation. The World Bank, 2007. [Google Scholar]
- 16.World Health Organization . World Health Statistics 2019: Monitoring Health for the SDGs : Sustainable Development Goals, 2019. [Google Scholar]
- 17.Yadav UN, Rayamajhee B, Mistry SK, et al. A syndemic perspective on the management of non-communicable diseases amid the covid-19 pandemic in low- and middle-income countries. Front Public Health 2020;8:508. 10.3389/fpubh.2020.00508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta SK, Lakshmi PVM, Kaur M, et al. Role of self-care in COVID-19 pandemic for people living with comorbidities of diabetes and hypertension. J Family Med Prim Care 2020;9:5495–501. 10.4103/jfmpc.jfmpc_1684_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. The Lancet 2020;395:1678–80. 10.1016/S0140-6736(20)31067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh DR, Sunuwar DR, Shah SK, et al. Impact of COVID-19 on health services utilization in Province-2 of Nepal: a qualitative study among community members and stakeholders. BMC Health Serv Res 2021;21:174. 10.1186/s12913-021-06176-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amatya Y, Douglas AH, Gurung ND. Barriers to accessing healthcare during COVID-19 lockdown: a point prevalence study amongst patients attending emergency and general out-patient clinics of patan Hospital, Nepal. Open Access J Public Health. [Google Scholar]
- 22.Kc A, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health 2020;8:e1273–81. 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization . The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. Geneva: World Health Organization, 2020. [Google Scholar]
- 24.Chan EYY, Kim JH, Lo ESK, et al. What happened to people with non-communicable diseases during COVID-19: implications of H-EDRM policies. Int J Environ Res Public Health 2020;17:E5588. 10.3390/ijerph17155588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pati S, Mahapatra P, Kanungo S, et al. Managing multimorbidity (multiple chronic diseases) amid covid-19 pandemic: a community based study from Odisha, India. Front Public Health 2020;8:584408. 10.3389/fpubh.2020.584408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mistry SK, Ali ARMM, Yadav UN, et al. Older adults with non-communicable chronic conditions and their health care access amid COVID-19 pandemic in Bangladesh: findings from a cross-sectional study. PLoS One 2021;16:e0255534. 10.1371/journal.pone.0255534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 2007;18:800–4. 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- 28.Yadav U, Yadav OP, Singh DR. Perceived fear of covid-19 and its associated factors among Nepalese older adults in eastern Nepal: findings from a cross-sectional study, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gummidi B, John O, Jha V. Continuum of care for non-communicable diseases during COVID-19 pandemic in rural India: a mixed methods study. J Family Med Prim Care 2020;9:6012–7. 10.4103/jfmpc.jfmpc_1805_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marmot M, Allen J. COVID-19: exposing and amplifying inequalities. J Epidemiol Community Health 2020;74:jech-2020-214720–2. 10.1136/jech-2020-214720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964–8. 10.1136/jech-2020-214401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr 2020;14:965–7. 10.1016/j.dsx.2020.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saqib MAN, Siddiqui S, Qasim M, et al. Effect of COVID-19 lockdown on patients with chronic diseases. Diabetes Metab Syndr 2020;14:1621–3. 10.1016/j.dsx.2020.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ministry of Health and Population, Government of Nepal . Health sector emergency response plan: COVID-19 pandemic, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056342supp001.pdf (96KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.


