Abstract
Objectives
To examine patient-reported needs for care and rehabilitation in a cohort following different subacute pathways of rehabilitation, and to explore factors underpinning met and unmet needs.
Design
Observational multicentre cohort study.
Patients and methods
A total of 318 Norwegian and 155 Danish patients with first-ever stroke were included. Participants answered questions from the Norwegian Stroke Registry about perceived met, unmet or lack of need for help and training during the first 3 months post stroke. The term “training” in this context was used for all rehabilitative therapy offered by physiotherapists, occupational or speech therapists. The term “help” was used for care and support in daily activities provided by nurses or health assistants.
Results
Need for training: 15% reported unmet need, 52% reported met need, and 33% reported no need. Need for help: 10% reported unmet need, 58% reported met, and 31% reported no need. Participants from both Norway and Denmark had similar patterns of unmet/met need for help or training. Unmet need for training was associated with lower functioning, (odds ratio (OR) = 0.32, p < 0.05) and more anxiety (OR = 0.36, p < 0.05). Patients reporting unmet needs for help more often lived alone (OR = 0.40, p < 0.05) and were more often depressed (OR = 0.31, p < 0.05).
Conclusion
Similar levels of met and unmet needs for training and help at 3 months after stroke were reported despite differences in the organization of the rehabilitation services. Functioning and psychological factors were associated with unmet rehabilitation needs.
LAY ABSTRACT
The aim of this study was to examine patient-reported needs for care and rehabilitation among selected patients with stroke in Norway and Denmark. A total of 318 Norwegian and 155 Danish patients with first-ever stroke were included. Participants answered the following 2 questions from the Norwegian Stroke Registry: Have you received enough help after the stroke? Have you received as much training as you wanted after the stroke? The term “training” in this context was used for all rehabilitative therapy offered by physio-, occupational or speech therapists. The term «help» was used for care and support in daily activities provided by nurses or health assistants. Levels of anxiety and depression were investigated. With regard to training needs, 15% of all participants reported unmet needs, 52% reported that their needs had been met, and 33% reported that they had no need for training. Regarding the need for help, 10%, 58% and 31% reported unmet needs, that needs had been met, and that they had no need for care, respectively. Participants in the 2 countries had similar patterns of unmet/met needs for help or training. Unmet need for training was associated with low function and anxiety. Patients reporting an unmet need for help more often lived alone and were more often depressed. There was no difference in met or unmet needs between Norwegian and Danish participants.Different rehabilitative follow-up after stroke did not affect levels of met and unmet rehabilitation needs. Health services should pay special attention to patients at risk, including those who are anxious or depressed, live alone or have functional deficits after stroke.
Key words: stroke, rehabilitation, unmet needs, rehabilitation pathways
Stroke is a major cause of death, with an increasing number of patients affected worldwide (1). Stroke survivors often have varying degrees of physical, psychosocial and cognitive disabilities, which may substantially affect their functional ability in daily and working life (2). Treatment offered by specialized stroke units (3), inpatient multidisciplinary rehabilitation teams (4) and community-based rehabilitation services adapted to patients’ home environment (5) are key elements to successful rehabilitation. At all intervention levels, the identification of patients’ individual needs is crucial for the optimization of rehabilitation outcomes. The definition of a need is, however, not unambiguous (6). A pragmatic approach is to adopt the most commonly used definition of healthcare needs and define rehabilitation needs as the needs that can be fulfilled by rehabilitation interventions and services (7). From the patient’s perspective, a need represents the perception of a situation in which help or support is desired. If adequate help is not offered, the provision of services does not fit the needs, gaps occur and needs become unmet (8).
A perceived need for therapy, comprehensive care, pscyhological support or information are examples of commonly reported unmet needs post-stroke (9).
Unmet rehabilitation needs may persist for years after stroke (10). According to a UK study, they are more often reported by people with disabilities, those belonging to ethnic minorities, and those living in the most deprived areas (10). According to a recent systematic review of 19 studies, mostly cross-sectional in design, 74% of stroke survivors experienced at least one unmet need. The studies revealed heterogeneous levels of unmet needs, ranging between 5% and 40% for care and between 2% and 36% for therapy (9). In most studies, unmet needs were assessed by using different multi-item questionnaires, such as the Longer-term Unmet Need after Stroke (11) and the Greater Manchester Stroke Assessment Tool (12), or by the self-report of long-term needs after stroke (10).
In a Swedish registry study evaluating perceived unmet or partly met rehabilitation needs with a single question, 21.5% of patients reported unmet needs one year after stroke. Important underpinning factors were older age, dependency on others, pain and depressive/ affective symptoms (13).
Rehabilitation practices are formulated and enacted in a cultural and historical context aligned to the development of healthcare services (14). Specialized stroke rehabilitation is integrated in the public healthcare systems in Nordic countries (15), but, whereas the Norwegian study region mainly emphasizes inpatient rehabilitation, the Danish region has developed an additional and more specialized, community-based rehabilitation programme (16). Although some studies have reported different rehabilitation pathways in the early subacute phase of stroke (17), no previous studies have, to our knowledge, compared unmet needs post stroke in participants with different subacute rehabilitation pathways.
The primary aim of this study was to examine patient-reported needs for healthcare and rehabilitation services in a cohort with different rehabilitation pathways recruited from 2 Nordic country-regions. Secondary aims were to assess to what extent these needs were met or unmet 3 months post stroke and to explore factors associated with met and unmet needs.
METHODS
Participants
Danish patients were included if they were: (i) diagnosed with a first-ever stroke using the World Health Organization (WHO) International Classification of Diseases, version 10 (ICD-10) (code I.I61, I.I63); (ii) admitted to the stroke unit at Aarhus University Hospital (AUH); (iii) ≥18 years old; (iv) living in either the Favrskov municipality or the Randers municipality, with 47,655 and 90,800 citizens, respectively, located in the Central Region of Denmark (5), from 1 June 2014 to 31 December 2015.
Norwegian patients were included if they were: (i) diagnosed with a first-ever stroke; (ii) admitted to 1 of 3 stroke units of the University Hospital of North Norway (UNN); (iii) ≥18 years old; and (iv) living in 1 of 30 municipalities in the hospital catchment area in the northern region of Norway, with a total of 190,000 citizens (5), from 20 March 2014, until 31 December 2015.
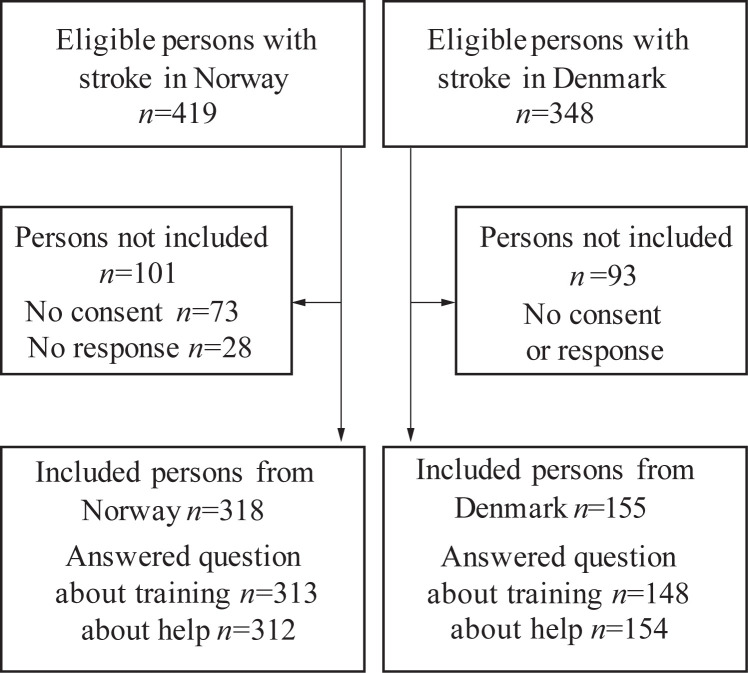
The study flowchart, following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria (18), is shown in Fig. 1. The response rates for eligible patients were 76% and 45% in Norway and Denmark, respectively.
Fig. 1.
Flowchart in Norway and Denmark.
Help and rehabilitation needs
Help and rehabilitation needs were assessed at 3 months post stroke using the following 2 questions from the Norwegian Stroke Registry follow-up questionnaire:
Have you received enough help after the stroke?
Have you received as much training as you wanted after the stroke?
Response options were yes (met need), no (unmet need), no need, and unknown.
Patients who answered one or both of these questions were included as participants.
The term “training” in this context was used for all rehabilitative therapy offered by physiotherapists, occupational or speech therapists. The term “help” was used for care provided by health professionals.
Acute treatment and rehabilitation of stroke in 2 regions of Denmark and Norway
Both countries have public-tax-financed healthcare systems, including free access to general practitioners, hospital treatment, care and rehabilitation and subsequent inpatient or outpatient treatment in the municipalities (19).
Norway and Denmark follow well-established common principles for acute treatment, including multidisciplinary rehabilitation in stroke units (20, 21).According to their national stroke registries, more than 90% of all patients with stroke in Denmark and Norway receive treatment in a stroke unit. However, the size of stroke units differs in these countries, as, in Denmark, all stroke patients in the region were treated at a single large stroke unit, whereas in Norway, the treatment structure was decentralized, with 3 stroke units. The mean number of inhabitants in the municipalities in the Arctic North is also far lower than that in the region in Denmark.
Following discharge from stroke units, a higher proportion of patients in Norway appear to receive inpatient rehabilitation (16). The Danish region had specialized multidisciplinary team-based neurorehabilitation available at the municipal level, while this service was scarce in the northern Norwegian region.
All Danish patients receive a compulsory individual rehabilitation plan at discharge, while rehabilitation at the municipal level in Norway varies according to local competence and capacity (16). Individual rehabilitation plans may be adapted for younger patients with stroke in Norway, but seldom for elderly patients.
Table I gives an overview of rehabilitation services provided after discharge from stroke units.
Table I.
Rehabilitation services after discharge from stroke units in the selected regions in Norway and Denmark during the study period
| Rehabilitation services | Denmark | Norway |
|---|---|---|
| In-patient specialized neurorehabilitation | Yes | Yes |
| In-patient hospital-linked rehabilitation units outside the hospital, less specialized in neurorehabilitation | Yes | Yes |
| In-patient rehabilitation nursing home and other in-patient rehabilitation location in the municipality | Yes | Yes |
| Ambulatory consulting team at the specialist level | Yes | Yes |
| Specialized neurorehabilitation team at the municipality level | Yes | No |
| Out-patient specialized day rehabilitation | Yes | No |
| Community-based day rehabilitation at a centre | Yes | No |
| Out-patient rehabilitation in private physiotherapy clinic | Yes | Yes |
| Home-based rehabilitation | ||
| Provided by home help | Yes | No |
| Provided by therapists | Yes | Yes |
| Brain injury coordinator in municipalities | Yes | No |
| Job consultants | Yes | No |
| Compulsory rehabilitation plan at discharge from stroke unit | Yes | No |
Assessing stroke severity
Stroke severity was recorded at baseline within 24 h after admission to the hospital. Data were collected from the national registries. In Norway, the National Institute of Health Stroke Scale (NIHSS) (22) is used to measure neurological impairment after stroke, while the Scandinavian Stroke Scale (SSS) (23) is the preferred scale to determine stroke severity in Denmark. In dealing with data from both Norway and Denmark, the authors chose to use the SSS, as data from the Danish National Stroke Registry (24) were more complete than those in the Norwegian Stroke Registry. Primary missing Norwegian NIHSS scores were retrospectively coded from medical records. All conversions from the NIHSS to the SSS were made by one experienced clinician using the unadjusted mathematical model of Gray et al. (25), which was derived for interconversion between these 2 stroke scales.
The SSS sum score is divided into 4 categories: an SSS score of 0–14 indicates very severe stroke, 15–29 indicates severe stroke, 30–44 indicates moderate stroke, and 45–58 indicates mild impairment post stroke.
Recruitment and data collection
Patients from the northern Norwegian region were asked for consent at the stroke unit or by post within 3 months after stroke. In Denmark, a health professional retrieved information on patients with stroke directly from the Danish National Stroke Registry. The patients were informed about the study by telephone or letter. Those who responded became consenting participants in the study.
Both Norway and Denmark have mandatory national stroke registries that aim to acquire person-identifiable information about patients with acute stroke admitted to hospitals. The registries contain information about risk factors prior to stroke and hospital treatment in the acute stage of stroke.
In Norway, information is also collected through a follow-up questionnaire administered by telephone interview at 3 months after hospital admittance and input into the National Stroke Registry. The telephone interview was performed by professionals at the stroke units in Norway and by the study personal in Denmark. As Denmark has no regular follow-up stroke registries, selected questions from the Norwegian follow-up registry were collected by telephone interview in Denmark at 3 months post stroke, in order to acquire similar data from both countries.
This study has 3 data sources: the National Stroke Registry, telephone interviews and study-specific postal questionnaires at 3 months post stroke.
Stroke registry data: information about age; sex; pre-stroke living conditions, such as living alone or receiving help; stroke subtypes; stroke severity; thrombolysis; and length of stay (LOS) in stroke units were collected. Met/unmet need status and no need for care or rehabilitation were assessed with the 2 questions concerning help and training presented earlier.
Telephone interview at 3 months post stroke. Pre-stroke data on working status and dependency on help in activities of daily living were obtained. In addition, patients from both countries answered study-specific questions regarding rehabilitation services after stroke unit treatment. Rehabilitation was classified into 3 categories (in-hospital, community-based or no rehabilitation) according to the first type of rehabilitative follow-up the patient received immediately after discharge from the stroke unit.
The level of functioning was assessed using the modified Rankin scale (mRS) (26), a clinician-reported measure of global disability widely used to evaluate post-stroke outcomes. The scale consists of categories assessing the level of independence, ranging from completely independent to bedridden or death. There is extensive evidence on the validity of the mRS (26).
Questionnaire at 3 months post stroke: mental health status was assessed using the Hospital Anxiety and Depression Scale (HADS) (27). The HADS is a widely used screening instrument for symptoms of anxiety (HADS-A) and depression (HADS-D). The scale is favourable, as it is relatively less affected by common somatic symptoms not related to affective symptoms, such as fatigue or sleeping problems (28). The scale range is 0–21 for both subscales, with a cut-off score of 8 being indicative of anxiety or depression possibly needing treatment.
Ethics
In Denmark, approval was obtained from the Danish Data Protections Agency (reference number 1-16-02-363-14), while in Norway, the study was approved by the Committee for Medical Research Ethics, Health Region North (reference number 2013/1472).
Statistical analysis
All statistical analyses were conducted in IBM SPSS 26. Descriptive statistics are presented as percentages, medians with interquartile ranges (IQR) or means with 95% confidence intervals (95% CI). Simple group difference testing based on continuous and categorical data was performed with independent t-tests and χ2 tests, respectively. The distributional properties of the variables were examined visually using P-P plots. In the case of heavily skewed data, the Mann–Whitney U test was applied.
Multivariable logistic regression analyses
The study had 2 outcome variables: (1) patients reporting needs for help; and (2) patients reporting needs for rehabilitation training. Both outcome variables had 3 response options: (a) needs met, (b) needs unmet, and (c) no needs stated. Logistic regression analyses were conducted for each of the outcome variables to identify predictors of needs. This analysis combined categories (a) and (b) (met + unmet needs) relative to category (c) as the reference (no needs).
Two additional logistic regression analyses were conducted comparing the subgroups reporting such needs, specifying category (a) (met needs) with category (b) as the reference (unmet needs). As the current study was exploratory rather than hypothesis-testing, non-significant variables were removed using the backward procedure (excluded if p > 0.05.). All final models were adjusted for country, age and sex.
The included potential explanatory variables were based on the reference literature and on discussions held by the research group. These were country (Norway/Denmark), age (<65 / ≥65 years), sex (male/female), living alone (yes/no), working (yes/no), dependent on help pre-stroke (yes/no), SSS score, stroke subtype (cerebral bleeding/ischaemic stroke), thrombolysis (yes/no), LOS, HADS-A scores (<7/≥ 8), HADS-D scores (< 7/≥ 8), mRS scale scores (0–2/3–5), and type of rehabilitation after discharge from the stroke unit (inpatient, community-based, or no rehabilitation (no/yes)).
In the multivariate analysis of rehabilitation services, no rehabilitation was the reference category. The reference category of the dichotomous variables is the last variable within parentheses.
All analyses were also performed without the HADS to investigate whether a lower number of respondents had an impact on the results. As no substantial difference was observed, we chose to keep the HADS within the analyses.
The effect sizes of the predictors are given as odds ratios (ORs) with 95% confidence intervals (95% CIs). An alpha level of <0.05 was required to discard the null hypothesis.
The degree of multicollinearity was checked using the variance inflation factor (VIF: range 0 to infinity) and the tolerance statistic (range: 0–1). The VIF was below 2 in all analyses, with a tolerance level from 0.06–0.09, which is quite acceptable. Model fit was investigated with the Hosmer–Lemeshow test to assess the agreement between the observed outcomes and the predicted outcomes of our models. The degree of pseudoexplained variance was reported according to Nagelkerke’s R2.
RESULTS
Representativeness of included patients
A total of 473 patients were included. In the Norwegian region, there were more men in the included cohort than among the non-included patients (58% vs 37%, respectively, p = 0.001). In the Danish cohort, no statistically significant difference in age, sex or stroke severity was demonstrated when comparing included patients and non-included patients.
Country differences
Norwegian stroke patients were older, more frequently lived alone and were dependent on personal assistance pre-stroke to a higher degree than Danish patients. Norwegian patients also had more severe strokes and longer LOS in stroke units (Table II). The proportion of patients receiving thrombolysis was higher in Denmark. However, the level of functioning measured with the mRS at 3 months post stroke was comparable between the countries.
Table II.
Participants’ characteristics
| Pre-stroke demographics | All patients (n = 473) | Norwegian patients (n = 318) | Danish patients (n = 155) | p-value |
|---|---|---|---|---|
| Age, years, mean (95% CI) | 71.1 (70.0–72.2) | 72.0 (69.4–72.3) | 69.3 (67.4–71.3) | 0.03 |
| 18–64 years, n (%) | 122 (26) | 80 (25) | 42 (27) | 00.65 |
| 65+ years, n (%) | 351 (74) | 238 (75) | 113 (73) | |
| Sex, n (%) | ||||
| Male | 272 (57) | 182 (57) | 90 (58) | 0.86 |
| Female | 201 (43) | 136 (43) | 65 (42) | |
| Living alone, n (%) | 175 (39) | 131 (42) | 44 (28) | 0.005 |
| Working, n (%) | 101 (21) | 60 (19) | 41 (26) | 0.06 |
| Need assistance, n (%) | 42 (8) | 39 (12) | 3 (2) | 0.001 |
| Stroke characteristics | ||||
| Ischaemic stroke, n (%) | 433 (92) | 286 (90) | 147 (95) | 0.072 |
| Total SSS score, median (IQR 25–75%) | 47 (42–54) | 47 (41–52) | 50 (43–56) | 0.001 |
| Very severe SSS score, n (%) | 9 (2) | 8 (2) | 1 (1) | 0.057a |
| Severe SSS score, n (%) | 22 (5) | 15 (5) | 7 (5) | |
| Moderate SSS score, n (%) | 144 (30) | 108 (34) | 36 (23) | |
| Mild SSS score, n (%) | 297 (63) | 187 (59) | 110 (71) | |
| Stroke unit treatment | ||||
| Thrombolysis, n (%) | 76 (16) | 43 (14) | 33 (21) | 0.032 |
| LOS (days), median (IQR 25%-75%) | 4 (2–7) | 5 (3–8.25) | 2 (1–4) | 0.001 |
| Early subacute rehabilitation | ||||
| Inpatient rehabilitation, n (%) | 163 (34) | 131 (41) | 32 (21) | 0.001 |
| Community-based rehabilitation, n (%) | 118 (25) | 52 (17) | 66 (42) | 0.001 |
| No rehabilitation after discharge from stroke unit, n (%) | 189 (40) | 135 (43) | 54 (37) | 0.15 |
| Level of functioning at 3 months post stroke | ||||
| mRS score 0–1 (no or mild symptoms), n (%) | 306 (65) | 203 (64) | 103 (66) | 0.28 |
| mRS score 2–3 (moderate symptoms), n (%) | 129 (27) | 85 (27) | 44 (28) | |
| mRS score 4–5 (severe symptoms), n (%) | 38(8) | 30 (9) | 8 (5) | |
p-values are for comparisons between the Norwegian and Danish patients.
Mild SSS score compared with moderate, severe and very severe SSS score.
IQR: interquartile range; SSS: Scandinavian Stroke Scale; LOS: length of stay in stroke unit; mRS: modified Rankin scale.
HADS anxiety and depression data were available for 308 patients. At 3 months, 14% and 16% of Norwegian and Danish participants reported anxiety (p = 0.59), and 13% and 14% reported depression (p = 0.81), respectively.
The rehabilitation services provided differed markedly; a much larger portion of the Norwegian cohort than the Danish cohort received inpatient rehabilitation, whereas community-based rehabilitation was far more common among the Danish participants (Table II).
As shown in Table III, at 3 months post stroke, 67% of participants reported needs (met/unmet) for training. A total of 69% reported needs (met/unmet) for help. Only 25% of the participants did not perceive any need for help or training. There was no difference between the participants from the two countries regarding perceived need or no need for help or training after stroke (Table III).
Table III.
Met, unmet and no need for training and help in participants answering these questions in Norway and Denmark
| Norway, n = 313 | Denmark, n = 148 | p-value | |
|---|---|---|---|
| As much training as wanted, n = 461 | |||
| Met need, n (%) | 157 (50) | 84 (57) | 0.144 |
| Unmet need, n (%) | 47 (15) | 20 (14) | |
| No need, n (%) | 109(35) | 44 (30) | |
| As much help as needed, n = 466 | n =312 | n = 154 | p-value |
| Met need, n (%) | 189(61) | 84 (55) | 0.336 |
| Unmet need, n (%) | 33 (10) | 15 (10) | |
| No need, n (%) | 90 (29) | 55 (35) | |
Rehabilitation needs (met and unmet) vs no need
Multivariate binary logistic regression revealed that country (Norway), a longer LOS and a lower mRS function score significantly predicted a need for training (either met or unmet) (Table IV). The need for help, whether met or unmet, was predicted by a longer LOS and a lower level of function (Table V). In addition, both inpatient rehabilitation and community-based rehabilitation (Tables IV and V) were associated with a need (met/unmet) for training and help, with the highest OR for inpatient rehabilitation.
Table IV.
Predictors of the need for training (met and unmet) vs no need for training.
| Variables | n = 461 | Met and unmet need for training (n = 307) | No need for training (n = 154) | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Country, n (%) | |||||||||
| Norway | 313 | 204 (65) | 109 (71) | 1.26 | 0.82–1.93 | 0.28 | 2.23 | 1.26–3.94 | 0.006 |
| Denmark | 148 | 104 (34) | 44 (29) | ||||||
| Age, n (%) | 0.94 | 0.61–1.47 | 0.79 | 0.57 | 0.32–1.00 | 0.052 | |||
| < 65 years | 121 | 82 (27) | 39 (25) | ||||||
| > 65 years | 340 | 226 (73) | 115 (75) | ||||||
| Sex, n (%) | 0.71 | 0.47–1.05 | 0.08 | 1.63 | 98–2.70 | 0.060 | |||
| Male | 266 | 169 (55) | 97 (63) | ||||||
| Female | 195 | 139 (45) | 56 (37) | ||||||
| Living alone pre-stroke, n (%) | 168 | 121 (39) | 47 (31) | 0.71 | 47–1.07 | 0.10 | |||
| Dependent on help pre-stroke, n (%) | 40 | 33 (11) | 7 (5) | 2.55 | 1.01–5.92 | 0.03 | |||
| Working pre-stroke, n (%) | 100 | 66 (21) | 34 (22) | 1.04 | 0.66–1.69 | 0.82 | |||
| SSS median score (25–75% IQR) | 461 | 46 (41–52) | 50 (46–56) | 1.07 | 1.07–1.10 | 0.001 | |||
| Stroke subtype, ischaemic, n (%) | 421 | 285 (93) | 136 (89) | 1.54 | 0.80–2.99 | 0.19 | |||
| Treated with thrombolysis, n (%) | 73 | 51 (17) | 22 (14) | 0.84 | 0.49–1.45 | 0.54 | |||
| LOS in stroke unit, median days (25–75% IQR) | 461 | 5 (2–8) | 2 (2–4.5) | 0.81 | 0.76–0.87 | 0.001 | 0.85 | 0.78–0.94 | 0.001 |
| mRS score at 3 months | 8.30 | 3.51–19.55 | 0.001 | 19 | 0.07–0.51 | 0.001 | |||
| 0–2, n (%) | 375 | 229 (75) | 147 (95) | ||||||
| 3–5, n (%) | 86 | 78 (25) | 7 (5) | ||||||
| HADS Anxiety score > 8 at 3 months | 45 | 33 (11) | 12 (8) | 1.50 | 0.72–3.11 | 0.28 | |||
| HADS Depression score >8 at 3 months | 40 | 31(10) | 9(6) | 1.83 | 0.84–3.92 | 0.13 | |||
| Inpatient rehabilitation | 161 | 153 (50) | 8 (3) | 18.1 | 8.54–37.98 | 0.001 | 23.5 | 10.4–53.2 | 0.001 |
| Community-based rehabilitation | 114 | 90 (28) | 24 (15) | 2.20 | 1.34–3.63 | 0.002 | 5.61 | 3.15–10.0 | 0.001 |
| No rehabilitation | 186 | 65 (21) | 121 (51) | 0.007 | 0.04–0.11 | 0.001 | Reference | ||
Nagelkerke’s R2 = 0.49. OR: odds ratio; 95% CI: 95% confidence interval; IQR: interquartile range; HADS: Hospital Anxiety and Depression Scale; SSS: Scandinavian Stroke Scale; LOS: length of stay; mRS: modified Rankin scale.
Table V.
Predictors of need for help (met and unmet) vs no need for help.
| Variables | n = 466 | Met/unmet need for help (n = 321) | No need for help (n = 145) | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Country, n (%) | 312 | 222 (69) | 90 (62) | 0.73 | 0.48–1.10 | 0.13 | 1.05 | 0.62–1.77 | 0.85 |
| Norway | 312 | 222 (69) | 90 (62) | 0.73 | 0.48–1.10 | 0.13 | 1.05 | 0.62–1.77 | 0.85 |
| Denmark | 154 | 99 (31) | 55 (38) | ||||||
| Age, n (%) | 0.90 | 0.72–1.40 | 0.64 | 0.75 | 0.45–1.24 | 0.26 | |||
| <65 years | 122 | 82 (25) | 40 (28) | ||||||
| >65 years | 344 | 239 (75) | 105 (72) | ||||||
| Sex, n (%) | 1.11 | 0.78–1.73 | 0.47 | 1.15 | 0.72–1.84 | 0.55 | |||
| Male | 268 | 181 (57) | 87 (60) | ||||||
| Female | 198 | 140 (43) | 58 (40) | ||||||
| Living alone pre-stroke, n (%) | 171/464 | 128 (40) | 43 (30) | 1.57 | 1.03–2.39 | 0.037 | |||
| Dependent on help pre-stroke, n (%) | 38/449 | 34 (11) | 4 (3) | 4.31 | 1.50–12.40 | 0.007 | |||
| Working pre-stroke, n (%) | 101/466 | 71 (22) | 30 (21) | 0.93 | 0.57–1.50 | 0.76 | |||
| Scandinavian Stroke Scale (SSS), median score (25–75% IQR) | 466 | 46 (41–53) | 50 (45–56) | 1.05 | 1.03–1.08 | 0.001 | |||
| Stroke subtype, ischaemic, n (%) | 426/466 | 293 (91) | 133 (92) | 0.95 | 0.46–1.91 | 0.87 | |||
| Treated with thrombolysis, n (%) | 76/466 | 50 (16) | 26 (18) | 1.18 | 0.70–1.99 | 0.53 | |||
| LOS in stroke unit, median days (IQR) | 466 | 5 (2–8) | 2 (1–5) | 0.82 | 0.76–0.88 | 0.001 | 0.89 | 0.82–0.97 | 0.010 |
| Modified Rankin scale (mRS) score at 3 months | 15.9 | 4.9–51.3 | 0.001 | 11.11 | 3.30–37.46 | 0.001 | |||
| 0–2, n (%) | 382 | 240 (75) | 142 (98) | ||||||
| 3–5, n (%) | 84 | 81 (25) | 3 (2) | ||||||
| HADS Anxiety score > 8 at 3 months | 45/297 | 30 (9) | 15 (10) | 1.02 | 0.52–2.00 | 0.95 | |||
| HADS Depression score > 8 at 3 months | 40/304 | 26 (8) | 14 (9) | 0.99 | 0.49–1.97 | 0.96 | |||
| Inpatient rehabilitation | 159 | 148 (46) | 11 (7) | 10.7 | 5.56–20.51 | 0.001 | 9.8 | 4.78–20.11 | 0.001 |
| Community-based rehabilitation | 117 | 84 (26) | 33 (23) | 0.82 | 0.52–1.30 | 0.41 | 2.84 | 16.65–4.81 | 0.001 |
| No rehabilitation | 187 | 86 (27) | 101 (69) | 0.16 | 0.10–0.25 | 0.001 | Reference | ||
Nagelkerke’s R2 = 0.36. OR: odds ratio; 95% CI: 95% confidence interval; IQR: interquartile range; HADS: Hospital Anxiety and Depression Scale; SSS: Scandinavian Stroke Scale; LOS: length of stay; mRS: modified Rankin scale.
Met vs unmet need for rehabilitation services
In the subgroup of patients reporting a need (met/unmet) for help (n = 322) or training (n = 308), 15% and 22% reported unmet needs for help and training, respectively. Country did not significantly predict unmet needs (Tables V and VI). The LOS in the stroke unit or the type of rehabilitation after discharge was not associated with the perceived level of met or unmet need for training or help during the first 3 months post stroke.
Table VI.
Predictors of met need for training vs unmet need for training.
| Variables | n = 308 | Met need for training (n = 241) | Unmet need for training (n = 67) | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Country, n (%) | 1.13 | 0.69–2.26 | 0.48 | 1.43 | 67–3.05 | 0.36 | |||
| Norway | 204 | 157 (77) | 47 (23) | ||||||
| Denmark | 104 | 84 (81) | 20 (19) | ||||||
| Age, n (%) | 0.95 | 0.52–1.71 | 0.86 | 1.15 | 49–2.70 | 0.75 | |||
| <65 years | 82 | 65 (27) | 17 (25) | ||||||
| >65 years | 226 | 176 (73) | 50 (75) | ||||||
| Sex, n (%) | 0.92 | 0.53–1.57 | 0.73 | 1,72 | 0.80–3.70 0.17 | ||||
| Male | 169 | 131 (54) | 38 (57) | ||||||
| Female | 139 | 110 (46) | 29 (43) | ||||||
| Living alone pre-stroke, n (%) | 121/308 | 94 (39) | 27 (40) | 0.85 | 0.55–164 | 0.95 | |||
| Dependent on help pre-stroke, n (%) | 33/295 | 22 (9) | 11 (16) | 0.51 | 0.23–1.11 | 0.09 | |||
| Working pre-stroke n (%) | 66/308 | 55 (23) | 11 (16) | 0.67 | 0.33–1.36 | 0.26 | |||
| SSS, median score (25%–75% IQR) | 308 | 46 (41–53) | 44 (37–49) | 0.97 | 0.95–1.00 | 0.016 | |||
| Stroke subtype, ischaemic, n (%) | 285/308 | 223 (93) | 62 (93) | 0.99 | 0.36–2.80 | 0.99 | |||
| Treated with thrombolysis, n (%) | 51/307 | 40 (16) | 11 (16) | 1.01 | 0.48–2.08 | 0.99 | |||
| LOS in stroke unit, median days (25%–75% IQR) | 308 | 5 (2–9) | 4 (2–8) | 0.97 | 0.93–1.03 | 0.36 | |||
| Modified Rankin scale (mRS) score at 3 months | 0.37 | 0.21–0.65 | 0.001 | 0.32 | 13–0.77 | 0.011 | |||
| 0–2, n (%) | 230 | 191 (79) | 39 (58) | ||||||
| 3–5, n (%) | 78 | 50 (21) | 28 (42) | ||||||
| Available data on HADS A+D | 208 | ||||||||
| HADS Anxiety score >8 at 3 months | 33/199 | 21(9) | 12 (18) | 0.34 | 0.15–0.77 | 0.008 | 0.36 | 0.15–0.86 0.021 | |
| HADS Depression score > 8 at 3 months | 31/202 | 20 (8) | 11 (16) | 0.37 | 0.16–0.86 | 0.020 | |||
| Inpatient rehabilitation | 153 | 118 (49) | 35 (52) | 1.14 | 0.66–1.96 | 0.63 | |||
| Community-based rehabilitation | 90 | 75 (31) | 15 (22) | 1.57 | 0.83–2.96 | 0.17 | |||
| No rehabilitation | 65 | 48 (20) | 17 (25) | 1.36 | 73–2.58 | 0.33 | Reference | ||
Nagelkerke’s R2 = 0.15. OR: odds ratio; 95% CI: 95% confidence interval; IQR: interquartile range; HADS: Hospital Anxiety and Depression Scale; SSS: Scandinavian Stroke Scale; LOS: length of stay; mRS: modified Rankin scale.
An unmet need for training was associated with a lower mRS function score at 3 months post stroke. The percentage was 2-fold higher for unmet needs for training among those with the mRS scores of 3–5 (p = 0.011) (Table V). A patient with a severe loss of functioning (mRS score 3–5) had a 68% higher probability of reporting unmet needs for training than a patient with an mRS score 0–2. In addition, anxiety (p = 0.021) was a significant factor, with more anxiety among those who had unmet needs for training (Table VI).
Patients reporting unmet needs for help more often lived alone pre-stroke (p = 0.039) and were also more depressed at 3 months post stroke (p = 0.028) (Table VII).
Table VII.
Predictors of met need for help vs unmet need for help.
| Variables | n = 322 | Met need for help (n = 274) | Unmet need for help (n = 48) | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Country, n (%) | 1.03 | 0.50–1.98 | 0.95 | 0.70 | 0.30–1.64 | 0.41 | |||
| Norway | 223 | 190 (69) | 33 (69) | ||||||
| Denmark | 99 | 84 (31) | 15 (31) | ||||||
| Age, n (%) | 1.40 | 0.72–2.73 | 0.32 | 1.46 | 0.59–3.64 | 0.42 | |||
| <65 years | 82 | 67 (25) | 15 (31) | ||||||
| >65 years | 240 | 207 (75) | 33 (69) | ||||||
| Sex, n (%) | 0.82 | 0.44–1.50 | 0.52 | 1.89 | 0.76–4.77 | 0.17 | |||
| Male | 182 | 157 (57) | 25 (48) | ||||||
| Female | 140 | 117 (43) | 23 (52) | ||||||
| Living alone, n (%) | 128/319 | 103 (38) | 25 (52) | 0.56 | 0.30–1.03 | 0.066 | 0.40 | 0.17–0.96 | 0.039 |
| Dependent on help, n (%) | 34/306 | 29 (11) | 5 (10) | 1.03 | 0.38–2.81 | 0.96 | |||
| Working, n (%) | 71/322 | 62 (23) | 9 (19) | 0.79 | 0.36–1.71 | 0.54 | |||
| SSS, median score (IQR) | 322 | 46.5 (41–53.75) | 44.5 (38.25–49.75) | 0.98 | 0.96–1.01 | 0.15 | |||
| Stroke subtype, ischaemic, n (%) | 294/322 | 249 (91) | 45 (94) | 0.66 | 0.19–2.28 | 0.51 | |||
| Treated with thrombolysis, n (%) | 50/321 | 40 (15) | 10 (21 | 0.66 | 0.30–1.42 | 0.28 | |||
| LOS in stroke unit, median days (IQR) | 322 | 5 (2–8.5) | 4 (2–7) | 0.98 | 0.92–1.03 | 0.41 | |||
| Modified Rankin scale (mRS) score at 3 months | 1.27 | 0.64–2.51 | 0.49 | ||||||
| 0–2, n (%) | 241 | 207 (75) | 34 (71) | ||||||
| 3–5, n (%) | 81 | 67 (25) | 14 (29) | ||||||
| HADS Anxiety score >8 at 3 months | 30/197 | 23 (8) | 7 (14) | 0.47 | 0.18–1.23 | 0.13 | |||
| HADS Depression score >8 at 3 months | 30/199 | 19 (7) | 7 (14) | 0.37 | 0.14–0.99 | 0.05 | 0.31 | 0.11–0.88 | 0.028 |
| Rehabilitation | |||||||||
| Inpatient rehabilitation | 149 | 125 (46) | 24 (50) | 0.86 | 0.46–1.58 | 0.62 | |||
| Community-based | 84 | 76 (28) | 8 (17) | 1.94 | 0.88–4.37 | 0.10 | |||
| No rehabilitation | 86 | 70 (26) | 16 (33) | 0.69 | 0.36–1.37 | 0.28 | Reference | ||
Nagelkerke’s R2 = 0.011. OR: odds ratio; 95% CI: 95% confidence interval; IQR: interquartile range; HADS: Hospital Anxiety and Depression Scale; SSS: Scandinavian Stroke Scale; LOS: length of stay; mRS: modified Rankin scale.
DISCUSSION
This study is, to our knowledge, the first to explore the level of met and unmet post-stroke rehabilitation needs in association with different rehabilitation pathways in participants recruited from 2 countries. Two-thirds of an unselected population of consecutive patients with stroke in Norway and Denmark reported the need for help and training during the first 3 months post stroke, demonstrating the considerable negative impact that stroke has on patients (1).
The 2 cohorts differed, as the Norwegian participants were older, more often dependent on help pre-stroke, more often lived alone, and had more severe strokes than the Danish participants.
The population density and travel distances differed, yet according to data from the national stroke registries, there was no difference in hospital arrival time or acute stroke treatment after stroke in these 2 regions.
The received rehabilitation services differed markedly between the participants in the 2 countries. Nevertheless, the participants from the 2 countries reported similar levels of met and unmet needs for both training and help at 3 months after stroke. The result may imply that a longer stay in a stroke unit and more inpatient rehabilitation during the first 3 months after stroke to a certain extent compensate for the more severe strokes and less use of community-based rehabilitation in Norway. Cultural differences in expectations of help and training may also contribute to the comparable findings of met and unmet needs in the 2 countries.
Living alone and depression were significantly associated with unmet needs for help, whereas a low level of functioning and anxiety at the 3-month follow-up were associated with unmet needs for training.
Unmet need for training and help
We regard it as especially important to investigate predictors that might explain unmet needs for help and training to identify correctable factors to reduce patient-reported unmet rehabilitation needs. At the individual level, unmet rehabilitation needs may reduce functional ability, increase psychological burden, and hence reduce autonomy, post stroke (29). Insufficient professional efforts increase caregivers’ burdens (30).
On the systemic level, unmet rehabilitation needs may lead to increased use of health services (29), institutionalization and economic costs (31).
The level of unmet rehabilitation needs must be interpreted within the post-stroke time frame and by the definition of the needs used. Most studies report unmet rehabilitation needs in a later phase post stroke and use questionnaires reflecting a much broader definition of rehabilitation needs. In the systematic review (9), only 2 validation articles included participants within the first year.
There are no comparable studies of unmet needs at 3 months post-stroke. Studies at 6 and 12 months post stroke demonstrate great variability in unmet needs, which may stem from large differences in operationalization or use of measures, as well as differing contexts (9).
Unmet needs in the Swedish registry study (13) were assessed using the following single question: Have your needs for rehabilitation after stroke been met? Rehabilitation was defined as activities or training to improve or maintain the ability to cope with daily life. This finding of unmet needs is higher than in the current study, but answering options of partly met needs were included in unmet needs in the Swedish study, whereas the patients in the current study had only yes-or-no answer alternatives. Using dichotomous response options may influence the results, as partial unmet needs may be categorized as both met needs and unmet needs. The recognition of unmet needs may also increase over time, particularly for those facing unfulfilled needs who are hampered in their capability of returning to work (32).
In line with others (33), the current found psychological distress to be correlated with the perception of unmet needs. Anxiety at 3 months was significantly elevated among persons reporting an unmet need for training, while depression was more frequent when the need for help was unfulfilled. Depression was highly significantly associated with unmet needs at 12 months in the Swedish registry study (13).
The estimates of depression and anxiety at 3 months are lower than those observed in other studies (33, 34), but the results must be interpreted with caution because of missing data. In contrast to the Swedish registry study, the higher age and dependency on help pre-stroke among Norwegian participants did not increase the level of unmet needs compared with the level of unmet needs in Danish participants.
The type of rehabilitation offered had no impact on the level of experienced unmet needs. Approximately 50% of persons reporting an unmet need for training or help had completed inpatient rehabilitation. One out of every 7 participants in the current study stated an unmet need for training. Among these patients, 38% had an mRS score of 0–1, indicating no or slight symptoms at 3 months post stroke. This somewhat surprising fact indicates that the mRS might not identify all symptoms patients expect help to solve. Though extensively used, the mRS has a non-linear correlation with cognitive screening tools, as 7.5% of patients with an mRS score of 0–1 have findings of cognitive deficits detected by the Quality of Life in Neurological Disorder (Neuro-QOL) questionnaire (35). Questionnaire screening identifies significantly more needs than clinical evaluation, especially cognitive problems (36). Another possibility is unrealistic expectations for rehabilitation due to symptoms without local available treatment options; for instance, fatigue (37) or minor cognitive deficits (38).
Despite the findings described above, a low level of functioning, as measured with the mRS, at 3 months post stroke was highly significantly associated with unmet needs for training. The Swedish registry study also found a correlation between dependency in activities of daily living and unmet needs at the evaluation time-point at 12 months post stroke (13).
Operationalizing the rehabilitation need concept using questions about help and training
In this study, the questions about training and help were together designed as an expression of the broader concept of rehabilitation. The majority of patients in the study received both training and help, but while training is offered to facilitate functional improvement (39), help may often represent a compensating strategy. Theoretically, the concept of needs is multidimensional. According to Bradshaw (40), felt needs are equated with wants and are limited by the perceptions of the individuals with regard to the health services available. Expressed needs are demands or felt needs turned into action. Expressed needs are commonly used in healthcare services where waiting lists are taken as a measure of unmet needs. Normative needs are those defined by health professionals, administrators or experts in relation to norms or a desirable standard. Finally, comparative needs refer to a measure established by studying the characteristics of those in receipt of a service; in other words, populations in which the evaluated needs are generalized.
We have no possible way of distinguishing between felt needs and expressed needs in patients, as some patients may have had felt needs that were not expressed until their rehabilitation needs were subsequently formulated when asked at 3 months post stroke. In our study, 7/88 patients (8%) with mRS scores of 3–5 expressed no need for training, indicating a mismatch between clinical functioning and patient-reported needs. A plausible interpretation is patients’ unawareness of their own needs, due to a lack of insight. Unmet rehabilitation needs may therefore represent a lack of rehabilitation services, unexpressed or unidentified needs, or unrealistic expectations for rehabilitation. Patients and healthcare workers may also have different perspectives on needs (29).
Strengths and limitations
The study included the majority of eligible Norwegian patients with stroke in a given period of time and location. The representativeness of Danish participants is, however, lower. The difference in response rate may be due to different recruitment practices, as the personal contact of the study teams with patients at the stroke units in Norway may have enhanced participation in the study. In addition, some patients in Norway were excluded due to severe medical conditions, resulting in a selection of eligible patients in Norway, which was not possible in Denmark.
When using single questions about help and training, limitations occur because of lack of ability to recognize other unmet needs, as well as partly met or unmet needs.
Data on psychological function must be interpreted with caution because of possible selection bias.
Conclusion
This study is the first to explore unmet needs for rehabilitation within the context of different subacute rehabilitation settings in the regions of Norway and Denmark. The participants from the 2 countries reported similar levels of met and unmet needs for both training (15% unmet needs) and help (10% unmet needs) at 3 months after stroke.
Low levels of functioning and anxiety at 3 months post stroke were associated with perceived unmet needs for training. Living alone pre-stroke and having depression at 3 months enhanced the risk of reporting an unmet need for help. The health services should pay special attention to at-risk patients who are anxious or depressed, live alone, or have more functional deficits after stroke. Variations in service pathways for in-hospital or community-based rehabilitation did not affect the levels of met and unmet rehabilitation needs.
ACKNOWLEDGEMENTS
Collaborators at the stroke units contributed to the recruitment of patients.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Johnson C, Naghavi M, Nguyen M, Roth G, Nichols E, Alam T, et al. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ 2019; 364: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis 2009; 27: 204–214. [DOI] [PubMed] [Google Scholar]
- 3.Ringelstein EB, Chamorro A, Kaste M, Langhorne P, Leys D, Lyrer P, et al. European Stroke Organisation recommendations to establish a stroke unit and stroke center. Stroke 2013; 44: 828–840. [DOI] [PubMed] [Google Scholar]
- 4.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011; 377: 1693–1702. [DOI] [PubMed] [Google Scholar]
- 5.Hillier S, Inglis-Jassiem G. Rehabilitation for community-dwelling people with stroke: home or centre based? A systematic review. Int J Stroke 2010; 5: 178–186. [DOI] [PubMed] [Google Scholar]
- 6.Wiggins D, Dermen S. Needs, need, needing. J Med Ethics 1987; 13: 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchan H, Gray M, Hill A, Coulter A. Needs assessment made simple. Health Serv J 1990; 100: 240–241. [PubMed] [Google Scholar]
- 8.Heinemann AW, Sokol K, Garvin L, Bode RK. Measuring unmet needs and services among persons with traumatic brain injury. Arch Phys Med Rehabil 2002; 83: 1052–1059. [DOI] [PubMed] [Google Scholar]
- 9.Chen T, Zhang B, Deng Y, Fan JC, Zhang L, Song F. Longterm unmet needs after stroke: systematic review of evidence from survey studies. BMJ Open 2019; 9: e028137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKevitt C, Fudge N, Redfern J, Sheldenkar A, Crichton S, Rudd AR, et al. Self-reported long-term needs after stroke. Stroke 2011; 42: 1398–1403. [DOI] [PubMed] [Google Scholar]
- 11.Forster A, Murray J, Young J, Shannon R, Mellish K, Horton M, et al. Validation of the Longer-term Unmet Needs after stroke (LUNS) monitoring tool: a multicentre study. Clin Rehabil 2013; 27: 1020–1028. [DOI] [PubMed] [Google Scholar]
- 12.Rothwell K, Boaden R, Bamford D, Tyrrell PJ. Feasibility of assessing the needs of stroke patients after six months using the GM-SAT. Clin Rehabil 2012; 27: 264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ullberg T, Zia E, Petersson J, Norrving B. Perceived unmet rehabilitation needs 1 year after stroke. Stroke 2016; 47: 539–541. [DOI] [PubMed] [Google Scholar]
- 14.Mpofu E, Chronister J, Johnson ET, Denham G. Aspects of culture influencing rehabilitation and persons with disabilities. In: Kennedy P, editor. The Oxford handbook of rehabilitation psychology. New York, NY: Oxford University Press; 2012, p. 500–516. [Google Scholar]
- 15.Langhammer B, Becker F, Sunnerhagen KS, Zhang T, Du X, Bushnik T, et al. Specialized stroke rehabilitation services in seven countries. Int J Stroke 2015; 10: 1236–1246. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen SG, Friborg O, Heiberg GA, Arntzen C, Holm Stabel H, Thrane T, et al. Stroke-Specific Quality of Life one-year post-stroke in two Scandinavian country-regions with different organisation of rehabilitation services: a prospective study. Disabil Rehabil 2020. May; 1–11. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 17.Bråndal A, Eriksson M, Glader EL, Wester P. Effect of early supported discharge after stroke on patient reported outcome based on the Swedish Riksstroke registry. BMC Neurol 2019; 19: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 2007; 4: e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyttkens CH, Christiansen T, Häkkinen U, Kaarboe O, Sutton M, Welander A. The core of the Nordic health care system is not empty. Nord J Health Econ 2016; 4: 7–27. [Google Scholar]
- 20.Indredavik B, Ellekjær H, Selmer R. Stroke in Norway. Int J Stroke 2008; 3: 205–206. [DOI] [PubMed] [Google Scholar]
- 21.Jørgensen HS, Kammersgaard LP, Nakayama H, Raaschou HO, Larsen K, Hübbe P, et al. Treatment and rehabilitation on a stroke unit improves 5-year survival. Stroke 1999; 30: 930–933. [DOI] [PubMed] [Google Scholar]
- 22.Kwah LK, Diong J. National Institutes of Health Stroke Scale (NIHSS). J Physiother 2014; 60: 61. [DOI] [PubMed] [Google Scholar]
- 23.Lindenstrøm E, Boysen G, Christiansen LW, Hansen BR, Würtzen Nielsen P. Reliability of Scandinavian Neurological Stroke Scale. Cerebrovasc Dis 1991; 1: 103–107. [Google Scholar]
- 24.Johnsen S, Ingeman A, Hunborg HH, Schaarup SZ, Gyllenborg J. The Danish Stroke Registry. Clin Epidemiol 2016; 8: 697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gray LJ, Ali M, Lyden PD, Bath PMW. Interconversion of the National Institutes of Health Stroke Scale and Scandinavian Stroke Scale in acute stroke. J Stroke Cerebrovasc Dis 2009; 18: 466–468. [DOI] [PubMed] [Google Scholar]
- 26.Banks JL, Marotta CA. Outcomes validity and reliability of the Modified Rankin Scale: implications for stroke clinical trials. Stroke 2007; 38: 1091–1096. [DOI] [PubMed] [Google Scholar]
- 27.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 28.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. J Psychosom Res 2002; 52: 69–77. [DOI] [PubMed] [Google Scholar]
- 29.Vincent C, Deaudelin I, Robichaud L, Rousseau J, Viscogliosi C, Talbot LR, et al. Rehabilitation needs for older adults with stroke living at home: perceptions of four populations. BMC Geriatr 2007; 7: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ekstam L, Johansson U, Guidetti S, Eriksson G, Ytterberg C. The combined perceptions of people with stroke and their carers regarding rehabilitation needs 1 year after stroke: a mixed methods study. BMJ Open 2015; 5: e006784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walsh ME, Galvin R, Loughnane C, Macey C, Horgan NF. Community re-integration and long-term need in the first five years after stroke: results from a national survey. Disabil Rehabil 2014; 37: 1834–1838. [DOI] [PubMed] [Google Scholar]
- 32.Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. J Rehabil Med 2003; 35: 127–131. [DOI] [PubMed] [Google Scholar]
- 33.Stokman-Meiland DCM, Groeneveld IF, Arwert HJ, van der Pas SL, Meesters JJL, Mishre RDR, et al. The course of depressive symptoms in the first 12 months post-stroke and its association with unmet needs. Disabil Rehabil 2020: p. 1–8. [DOI] [PubMed] [Google Scholar]
- 34.Barkercollo S. Depression and anxiety 3 months post stroke: prevalence and correlates. Arch Clin Neuropsychol 2007; 22: 519–531. [DOI] [PubMed] [Google Scholar]
- 35.Sangha RS, Caprio FZ, Askew R, Corado C, Bernstein R, Curran Y, et al. Quality of life in patients with TIA and minor ischemic stroke. Neurology 2015; 85: 1957–1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edwards DF, Hahn MG, Baum CM, Perlmutter MS, Sheedy C, Dromerick AW. Screening patients with stroke for rehabilitation needs: validation of the post-stroke rehabilitation guidelines. Neurorehabilit Neural Repair 2006; 20: 42–48. [DOI] [PubMed] [Google Scholar]
- 37.Kutlubaev M, Mead G. Fatigue after stroke. In: Godefrey O, editor. The behavioral and cognitive neurology of stroke. Cambridge: Cambridge Universigy Press; 2011, p. 375–386. [Google Scholar]
- 38.Cumming TB, Marshall RS, Lazar RM. Stroke, cognitive deficits, and rehabilitation: still an incomplete picture. Int J Stroke 2013; 8: 38–45. [DOI] [PubMed] [Google Scholar]
- 39.Saunders DH, Sanderson M, Hayes S, Kilrane M, Greig CA, Brazzelli M, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev 2016; 3: CD003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Butler JR. The taxonomy of social need. In: McLachlan G, editor. Problems and progress in medical care. Oxford, UK: Oxford University Press; 1972, p. 71–82. [Google Scholar]