Abstract
Objective
To investigate the effectiveness of robot-assisted therapy on balance function in stroke survivors.
Data sources
PubMed, the Cochrane Library, Embase and China National Knowledge Infrastructure databases were searched systematically for relevant studies.
Study selection
Randomized controlled trials reporting robot-assisted therapy on balance function in patients after stroke were included.
Data extraction
Information on study characteristics, demographics, interventions strategies and outcome measures were extracted by 2 reviewers.
Data synthesis
A total of 19 randomized trials fulfilled the inclusion criteria and 13 out of 19 were included in the meta-analysis. Analysis revealed that robot-assisted therapy significantly improved balance function assessed by berg balance scale (weighted mean difference (WMD) 3.58, 95% confidence interval (95% CI) 1.89–5.28, p < 0.001) compared with conventional therapy. Secondary analysis indicated that there was a significant difference in balance recovery between the conventional therapy and robot-assisted therapy groups in the acute/subacute stages of stroke (WMD 5.40, 95% CI 3.94–6.86, p < 0.001), while it was not significant in the chronic stages. With exoskeleton devices, the balance recovery in robot-assisted therapy groups was significantly better than in the conventional therapy groups (WMD 3.73, 95% CI 1.83–5.63, p < 0.001). Analysis further revealed that a total training time of more than 10 h can significantly improve balance function (WMD 4.53, 95% CI 2.31–6.75, p < 0.001). No publication bias or small study effects were observed according to the Cochrane Collaboration tool.
Conclusion
These results suggest that robot-assisted therapy is an effective intervention for improving balance function in stroke survivors.
LAY ABSTRACT
Balance is an important factor in ability to perform independent walking. Many patients with stroke gain little benefit from neural rehabilitation because their balance control is impaired. Robot-assisted therapy is a promising intervention approach, which has developed rapidly in recent years. Several previous reviews have focused on gait-related measurements, such as walking speed and endurance; however, the effectiveness of robot-assisted therapy on balance has not been clearly outlined. This systematic review and meta-analysis showed that robot-assisted therapy can significantly improve balance recovery compared with conventional therapy, especially for people in the acute/subacute phase after stroke treated with an exoskeleton and a total training time of more than 10 h.
Key words: robot-assisted therapy, stroke, balance function, Berg Balance Scale, meta-analysis
Globally, Stroke is the second cause of death and one of the most common causes of disability. Although the total incidence of stroke is decreasing in most regions worldwide, the number of disability adjusted life years is increasing, indicating that the overall burden of stroke is increasingly high (1).
Balance function is the ability of a person to maintain their centre of gravity within their base of support with minimal postural sway (2). Balance impairments are common in patients with stroke due to impaired integration of multiple sensorimotor information, postural control, and muscle strength (3). The current evidence indicates that balance is an important factor in ability to perform independent walking, and it is a significant predictive factor for gait function (4). Due to the nature of walking, the majority of the gait cycle is spent in single-limb support. During this phase, the person’s centre of gravity moves outside the base of support, making the balance inherently unstable (5). Stroke patients may have uneven weight distribution during standing and walking, and therefore are more likely to fall (6). Thus, to improve balance function is one of the main goals in a majority of stroke survivors (7).
Robot-assisted therapy (RT) is a promising intervention, which has recently expanded rapidly. RT has the potential to provide automatic and repetitive training that could enhance functional restitution and motor control for stroke patients; it can also reduce the manual burden during rehabilitation (8). Previous studies have assessed the effectiveness of RT on motor function in stroke patients. Nam et al. reported that RT could improve muscle strength of the lower limb (9). Another study noted that RT had a significant effect on improving motor control and muscle strength (10). Although balance function is essential to the readiness for walking training, to date, only a few reviews have focused on this item (11). During their recovery, treatment effects may vary according to time since stroke onset. It has been reported that acute stroke may benefit from RT, but those in the chronic phase may not (12). On the other hand, with regard to the effectiveness of RT, the device type is of major concern. Generally, robot-assisted devices can be divided into exoskeleton and end-effector. Exoskeleton devices consist of programmable drives or passive elements, which flex the hips and knees during the swing phase. Feet are placed on the foot plates in the end-effector design, and the device works to simulate the stance and swing phases (13). Training intensity may also affect the outcome of stroke.
The aims of this study were to assess the effects of RT for improving balance function after stroke, in comparison with conventional therapy, and to investigate the potential impacts of recovery stage, device type and training intensity on stroke prognosis.
METHODS
A systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (14). The protocol was previously registered at PROSPERO (registration number CRD42018115589).
Search strategy and selection criteria
An electronic search of the published literature was conducted in PubMed, the Cochrane Library, Embase and China National Knowledge Infrastructure databases. Studies were collected from inception up to 17 January 2020. Indexing terms and free-text words of the following key terms and synonyms were used: (Participants) “stroke”; (Intervention) “robot-assisted therapy; (Outcome) “gait” or “balance”; (Study design) “RCT”. A detailed search strategy used in PubMed is shown in Appendix SI. In addition, manual searching was performed to identify the relevant references in these articles.
Studies were selected based on the following inclusion criteria: (i) patients had been diagnosed with cerebral vascular accident; (ii) robot-assisted training was aimed to the recovery of balance function; (iii) control group received conventional therapy (e.g. regular physical therapy, manually-assisted body-weight supported treadmill training, etc.); (iv) RCTs were dosematched trials in which the experimental and control groups spent an equal amount of time on exercise therapy. Studies were excluded if: (i) they compared the effects of 2 different types of robot; (ii) they were trials in which RT was combined with other treatments (e.g. functional electrostimulation); (iii) they were case reports and pre-post design studies.
Data extraction
Two researchers (LW and XTZ) independently extracted the following information from individual studies: authors; publication year; country of origin; participant characteristics; method of randomization; blinding; intervention information; outcome measures; and adverse events. Data on intervention regimens, including device type, training time, frequency and duration, were extracted. Outcome measures were extracted, including one of the following tests: Berg Balance Scale (BBS), Timed Up-and-Go (TUG), Tinetti balance scale, Trunk Impairment Scale (TIS), postural sway tests and specific balance parameters using equipment sensors, such as force plates, accelerometers, and gyroscopes. If the trials had more than 2 groups and permitted multiple comparisons, only the data of interest were extracted.
Risk of bias assessment
Risk of bias for the included trials was assessed independently by 2 reviewers (LW and XTZ) according to the Cochrane Collaboration tools (15). These tools evaluate the selection, performance, detection, attrition, and reporting bias with 7 items. There are 3 evaluation options for each item: low, unclear, and high risk, based on the original research. Disputes and disagreements were solved by discussion or referral to a third reviewer (YZ).
Data analysis
As the selected RCTs used different robotic devices, methodology, and subscales of outcome measures, the treatment effect of the intervention was estimated by pooling the weighted mean difference (WMD) with 95% confidence interval (95% CI). In assessing heterogeneity among studies, the Cochran’s Q and I2 statistics were used. I2 values represent the amount of total variation explained by variation among studies, with a value of greater than 50% indicating severe heterogeneity (16).
The primary analysis was performed to explore the efficacy of RT on balance function reflected with BBS immediately after the intervention. Secondary analysis was conducted in a subset of patients according to: (i) recovery stage (acute/subacute < 6 months or chronic > 6 months); (ii) device type (end-effector or exoskeleton); and (iii) training intensity (total time < 10 or ≥ 10 h). The training intensity was presented using total time (number of sessions × time per session, in h) (17). This cut-off because was arbitrarily applied it was the most frequently used point in the included studies.
Publication bias was assessed by using funnel plots and the Egger linear regression test, with p-values less than 0.1 indicating potential publication bias. All statistical analyses were performed using RevMan 5.2 (The Cochrane Collaboration/The Nordic Cochrane Centre, Copenhagen, Denmark) and Stata12.0 (StataCorp, College Station, TX, USA ).
RESULTS
Literature search and study characteristics
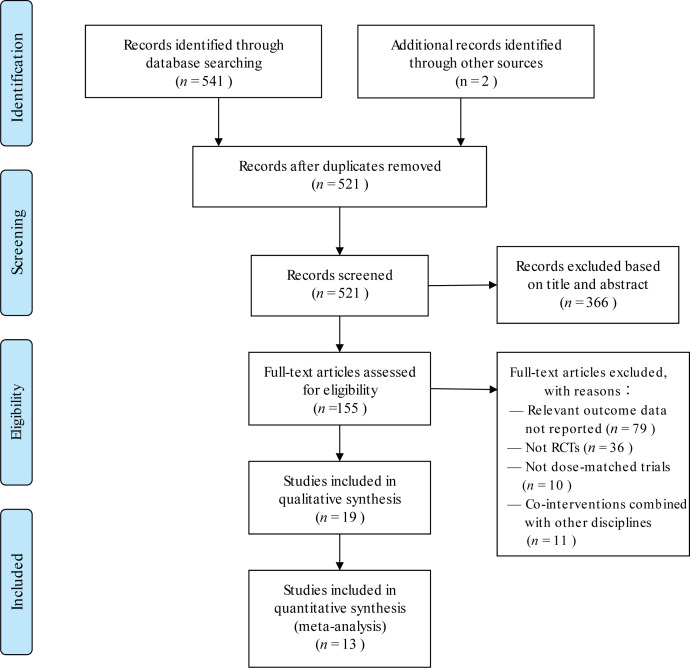
Fig. 1 summarizes the trial selection procedure. After searching the electronic databases, 521 unique records were screened, of which 155 titles and abstracts were considered to be relevant for further screening. After checking the full-text according to the inclusion and exclusion criteria, 19 RCTs were included in qualitative synthesis and 13 RCTs were included in quantitative synthesis. Out of 19 studies 17 were published in English and 2 in Chinese (17, 23). Table I shows the characteristics of included trials. The duration of the intervention ranged from 2 weeks to 5 months, with the training frequency varied from 1 to 6 days. The time spent per session of intervention ranged from 20 min to 1 h and the total time of intervention ranged from 6 to 20 h. In the included studies, Lokomat (Hocoma AG, Zurich, Switzerland), Exowalk (HMH Co. Ltd., South Korea), Walkbot ((P&S Mechanics, Seoul, South Korea)) and Flexbot-B (Jinghe robot Co. Ltd., Shanghai, China) were documented as exoskeleton and G-EO system (Reha Technology, Olten, Switzerland), Morning Walk (Hyundai Heavy Industries and Taeha Mechatronics, South Korea) and Gait Trainer (Reha-Stim, Berlin, Germany) were end-effector robots.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for trial inclusion and exclusion. RCT: randomized controlled trial.
Table I.
Characteristics of selected randomized controlled trials
| Reference | Country | Participants | Intervention methods | Outcome of interest | Conclusions |
|---|---|---|---|---|---|
| Bang et al. (18) 2016 | South Korea | 53.66±3.33 years, 9 M/9 F, 13 I/5 H, Duration after stroke >6 months | EG: 60 min RT (Lokomat), 5 times per week for 4 weeks CG: 60 min treadmill gait training, 5 times per week for 4 weeks |
BBS, ABC | RT was more effective than treadmill gait training in improving balance, and balance confidence in patients with chronic stroke. |
| Bei et al. (19) 2015 | China | 62.6±6.48 years, 63 M/17 F, 44 I/36 H, Duration after stroke <1 month | EG: 20 min RT (Lokomat) and 40 min CT, 6 times per week for 6 weeks CG: 20 min TAGT and 40 min CT, 6 times per week for 6 weeks |
BBS | RT was more effective in improving the balance function compared with TAGT. |
| Gandolfi et al. (20) 2019 | Italy | 64.12±10.83 years, 23 M/9 F, 26 I/6 H, Duration after stroke >6 months | EG: 50 min RT (G-EO system), 2 times per week for 5 weeks CG: 50 min sensory integration balance training, 2 times per week for 5 weeks |
BBS, Dynamic gait index, TUG, length of sway and sway area of the centre of pressure | RT had no significant improvement in balance function compared with sensory integration balance training. |
| Han et al. (21) 2016 | South Korea | 65.7±13.22 years, 32 M/24 F, 33 I/23 H, Duration after stroke >6 months | EG: 30 min RT (Lokomat) and 30 min CT, 5 times per week for 4 weeks CG: 60 min CT, 5 times per week for 4 weeks |
BBS | Both group were effective in improving balance function, while the balance function had no statistically significant difference between 2 groups. |
| Hornby et al. (22) 2008 | USA | 57±10.4 years, 30 M/18 F, 22 I/26 H, Duration after stroke >6 months | EG: 30 min RT (Lokomat), 12 sessions CG: 30 min TAGT, 12 sessions |
BBS | RT cannot facilitate greater improvement in balance function in ambulatory stroke survivors compared with a similar dosage of TAGT. |
| Kim-JY et al. (23) 2018 | South Korea | 58.99±12.98 years, 33 M/15 F, 32 I/16 H, Duration after stroke Mean=2.3 months | EG: 30 min RT (Morning Walk) and 60 min CT, 5 times per week for 3 weeks CG: 90 min CT, 5 times per week for 3 weeks |
BBS | Compared with CT alone, balance of stroke patients might be improved with RT combined with CT. |
| Kim-SY et al. (24) 2015 | South Korea | 52.0±14.37 years, 19 M/7 F, 13 I/13 H, Duration after stroke 99.8±74.53 days | EG: 40 min RT (Walkbot) and 40 min conventional physical therapy, 5 times per week for 4 weeks CG: 80 min conventional physical therapy, 5 times per week for 4 weeks |
BBS | RT was more effective in improving the balance function when combined with the conventional one compared with the conventional one only. |
| Lu et al. (25) 2017 | China | 58.2±13.48 years, 44 M/16 F, 30 I/30 H, Duration after stroke <6 months | EG: 20 min RT (Flexbot-B) and 60 min CT, 5 times per week for 6 weeks CG: 20 min BSWTT and 60 min CT, 5 times per week for 6 weeks |
BBS | RT had no significant improvement in balance function and paretic leg motor function compared with BSWTT. |
| Maple et al. (26) 2008 | Hong Kong | 70.3±11.77 years, 34 M/19 F, 42 I/11 H, Duration after stroke <6 weeks | EG: 20 min RT (Gait-trainer), 5 times per week for 4 weeks CG: 20 min conventional overground gait training, 5 times per week for 4 weeks |
BBS | RT had no significant improvement in balance function after the 4 weeks of gait training. |
| Nam et al. (9) 2018 | South Korea | 57.85±19.15 years, 17 M/17 F, 20 I/14 H, Duration after stroke 1.14±1.01 years | EG: 30 min RT (Exowalk), 5 times per week for 4 weeks CG: 30 min TAGT, 5 times per week for 4 weeks |
BBS | RT had no significant improvement in balance function compared with TAGT. |
| Santos et al. (27) 2018 | Brazil | 50.8±13.3 years, 11 M/4 F, 4 I/11 H, Duration after stroke7.8±4.8 years | EG: 60 min RT (Lokomat) and 120 min CT,1 time per week for 5 months CG: 60 min TAGT and 120 min CT, 1 time per week for 5 months |
BBS, TUG | Chronic stroke patients with ataxia had significant improvements in balance for both RAGT and TAGT groups. RT had no significant difference in balance function compared with TAGT. |
| Westlake et al. (28) 2009 | The United States | 56.8±14.93 years, 13 M/3 F, 8 I/8 H, Duration after stroke mean=3.3 years | EG: 30 min RT (Lokomat), 3 times per week for 4 weeks CG: 30 min BWSTT, 3 times per week for 4 weeks |
BBS | Both group significantly improved balance function in persons with chronic hemiparesis post-stroke. |
| Yun et al. (29) 2018 | South Korea | 63.9±8.2 years, 19 M/17 F, 25 I/17 H, Duration after stroke 30.1±7.2 days | EG: 30 min RT (Lokomat), 5 times per week for 3 weeks CG: 30 min CT, 5 times per week for 3 weeks |
BBS, the Postural Assessment Scale for Stroke (PASS) | RT contributed to the significant improvement of balance function compared with CT in subacute stroke patients. |
| Kim-HY et al. (30) 2019 | South Korea | 47.4±11.6 years, 16 M/3 F, 10 I/9 H, Duration after stroke >2 months | EG: 30 min RT (Lokomat) and 30 min CT, 5 times per week for 4 weeks CG: 60 min CT, 5 times per week for 4 weeks |
BBS, TIS, static standing balance | RT produces significant improvements in balance function in individuals with infratentorial stroke compared with CT. |
| Fisher et al. (31) 2011 | The United States | 60±14 years, 14 M/6 F, Duration after stroke <12 months | EG: 30 min RT (Autoambulator) and 30 min TAGT, 24 sessions in roughly 6–8 weeks CG: 60 min TAGT, 24 sessions in roughly 6–8 weeks |
Tinetti balance scale | RT may provide improvements in balance comparable with conventional physical therapy. |
| Peurala et al. (32) 2005 | Finland | 51.75±7.26 years, 24 M/6 F, 15 I/15 H, Duration after stroke >6 months | EG: 20 min RT (Gait-trainer) and 55 min physiotherapy, 5 times per week for 3 weeks CG: 20 min overground walking and 55 min physiotherapy, 5 times per week for 3 weeks |
Postural sway test | Patients with chronic stroke maintained their improved dynamic balance up to 6 months after an intensive 3-week RT. Both groups had no significant difference in balance measures. |
| Taveggia et al. (33) 2016 | Italy | 72.07±6.13 years, 17 M/11 F, Duration after stroke <6 months | EG: 30 min RT (Lokomat) and 60 min CT, 5 times per week for 5 weeks CG: 30 min activities targeted at improvement in walking and 60 min CT, 5 times per week for 4 weeks |
Tinetti balance scale | Both treatments were effective in the improvement of balance function, while the balance function had no statistically significant difference between 2 groups. |
| Hidler et al. (34) 2009 | The United States | 57.38±10.69 years, 39 M/24 F, 47 I/16 H, Duration after stroke <6 months | EG: 45 min RT (Lokomat), 3 times per week for 8–10 weeks, for a maximum total of 24 sessions CG: 45 min TAGT, 3 times per week for 8 to 10 weeks, for a maximum total of 24 sessions |
BBS | Both treatments were effective in the improvement of balance function, while RT had no significant improvement in balance function compared with TAGT. |
| Dias et al. (35) 2006 | Portugal | 69.18±9.14 years, 30 M/10 F, Duration after stroke >6 months | EG: 20 min RT (Gait-trainer) and 20 min CT, 5 times per week for 5 weeks CG: 20 min gait training using Bobath methods and 20 min CT, 5 times per week for 5 weeks |
BBS | Both treatments were effective in the improvement of balance function, while the balance function had no statistically significant difference between 2 groups. |
min: minutes; EG: experimental group; CG: control group; M: males; F: females; I: ischaemic; H: haemorrhagic; NR: not reported; CT: conventional training; RT: robot-assisted therapy; TAGT: therapist-assisted gait training; BWSTT: manually-assisted body-weight supported treadmill training; ABC: activities-specific balance confidence; TIS: Trunk Impairment Scale
Quality assessment
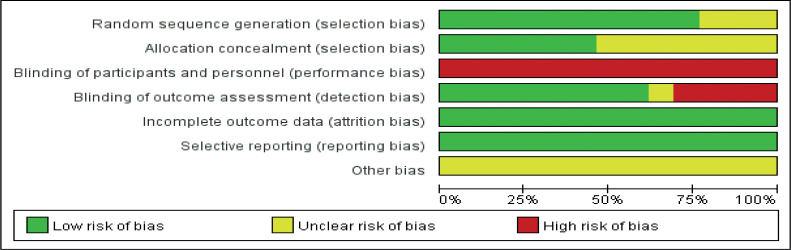
Figs 2 and 3 demonstrate the overview of risk of bias for included trials according to the Cochrane Collaboration tools. Bias regarding randomization procedure was unclear in 3 studies, and allocation concealment was unclear in 7 studies. Bias of performance was high, because therapists who supervised training and subjects can hardly be masked to the group allocation. In addition, all studies showed low risk of attribution bias and reporting bias, but were unclear for other bias. Overall quality assessment indicated that all included studies had low or moderate risk of bias.
Fig. 2.
Risk of bias graph for all included studies.
Fig. 3.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
Effects of robot-assisted training on balance
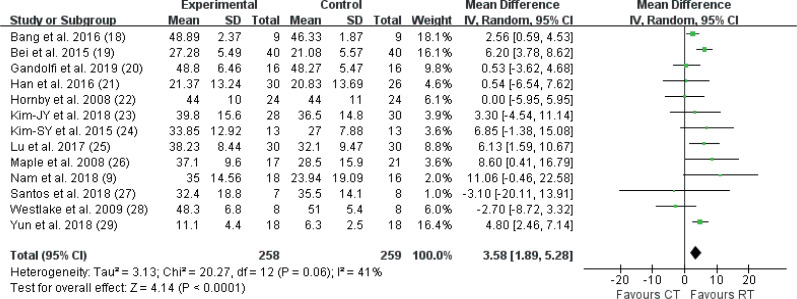
As shown in Fig. 4, 517 participants from 13 studies were included, RT significantly improved balance function compared with conventional therapy (WMD 3.58, 95% CI 1.89–5.28, p < 0.001) with no significant heterogeneity (I2 = 41%, p = 0.06). The other 6 studies were analysed qualitatively. Three reported that no significant difference in balance recovery was detected between RT and CT, although longitudinal significant improvement in balance function was observed (33–35).
Fig. 4.
Comparison of RT vs CT on BBS. 95% CI: 95% confidence interval; SD: standard deviation; IV: inverse variance; RT: robot-assisted therapy.
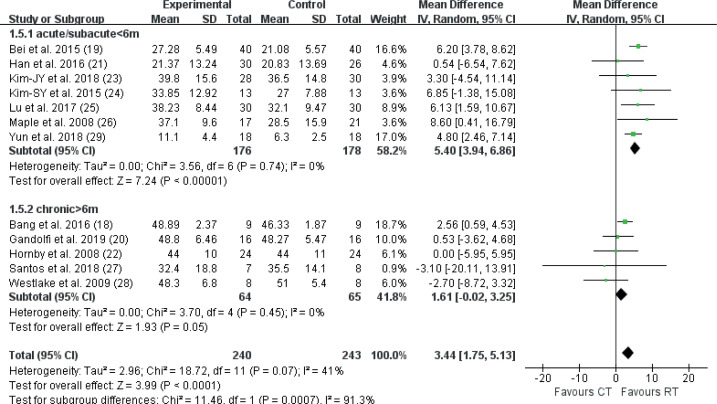
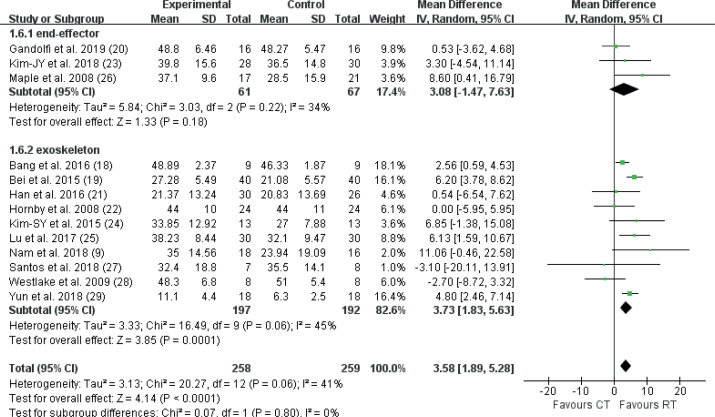
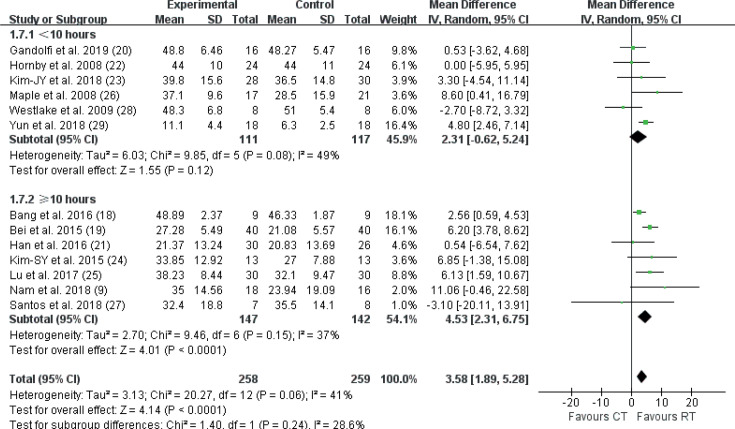
In comparing the effectiveness of RT vs CT, 3 factors may affect the outcome of interest, including recovery stage (acute, subacute or chronic), device type (end-effector or exoskeleton), and training intensity (total time ≥ 10 or < 10 h). Fig. 5 shows that RT achieved significantly greater improvement in BBS than CT during the acute/subacute stage of stroke recovery (WMD 5.40, 95% CI 3.94–6.86, p < 0.001). In contrast, no significant results supported that RT was more effective than CT in chronic patients (WMD 1.61, 95% CI –0.02–3.25, p = 0.05). In addition, there were 128 participants in 3 end-effector robot trials, and 389 participants in 10 exoskeleton robot trials (Fig. 6). With the exoskeleton the balance recovery in the RT groups was significantly better than in the CT groups (p < 0.001). However, in the end-effector subset, the improvement in the RT group was not statistically significant compared with that in the CT group (p = 0.18). In addition, Fig. 7 demonstrated that there was a statistically significant difference between RT and CT in the subset with total time ≥ 10 h (WMD 4.53, 95% CI 2.31–6.75, p = 0.12); however, when the total time was less than 10 h no significant differences were detected.
Fig. 5.
Secondary meta-analysis of RT vs CT on BBS by recovery stage. 95% CI: 95% confidence interval; SD: standard deviation; IV: inverse variance; RT: robot-assisted therapy.
Fig. 6.
Secondary meta-analysis of RT vs CT on BBS by device type. 95% CI: 95% confidence interval; SD: standard deviation; IV: inverse variance; RT: robot-assisted therapy.
Fig. 7.
Secondary meta-analysis of RT vs CT on BBS by training intensity. 95% CI: 95% confidence interval; SD: standard deviation; IV: inverse variance; RT: robot-assisted therapy.
Safety of robot-assisted training
With the exception of 2 studies, all trials reported that there were no adverse events observed during and/or after the interventions. Hornby et al. reported that 2 patients discontinued due to leg pain, 1 patient experienced pitting oedema in the RT group, 4 patients discontinued due to leg pain, 1 patient presented with significant hypertension, and 2 patients withdrew due to subjective exercise intolerance in the control group (22). Maple et al. reported that 1 patient admitted to an acute-care hospital, and another patient experienced a deteriorating medical condition in the control group, no adverse events observed in the RT group (26).
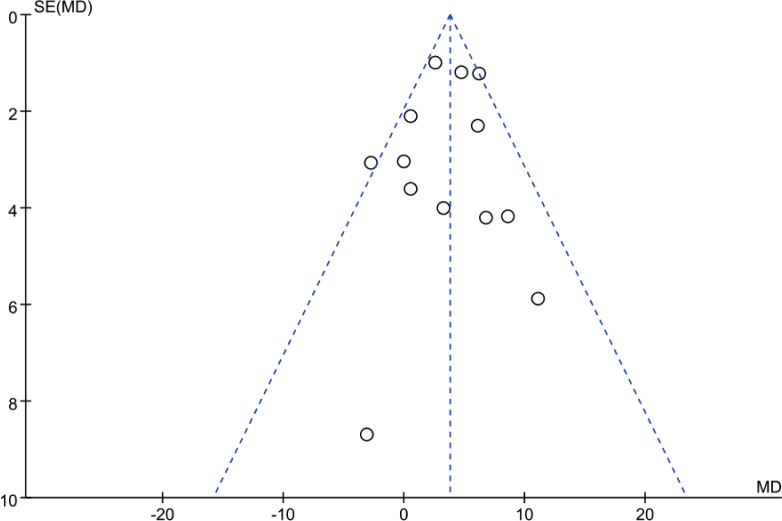
Publication bias
There was no significant funnel plot asymmetry detected, and the Egger test also indicated no evidence of publication bias (p = 0.57). Funnel plots of meta-analysis are demonstrated in Fig. 8.
Fig. 8.
Funnel plot of meta-analysis. SE: standard error; MD: mean difference.
DISCUSSION
This systematic review and meta-analysis included 19 studies comparing the efficacy of RT on balance function after stroke, in comparison with CT. Despite the heterogeneity of the included studies, RT showed superior effects to CT on balance recovery.
BBS is a static-dynamic integrated test used as a representative method for evaluating the balance ability of stroke patients. BBS evaluates a total of 14 functional tasks, yielding a maximum score of 56. A higher score represents a better balance performance (2). RT provides not only simple and repetitive movement, but also generates more complex, controlled multisensory stimulation, which is regarded as essential to balance recovery (36). In addition, RT could make stroke patients experience early verticality, and by gradually increasing weight-bearing, the patients could start standing and standing balance training as soon as possible. Another advantage of RT is that it reduces energy consumption and cardiorespiratory load, and stroke patients can tolerate longer training time and greater training intensity (37). The current results are consistent with several other reviews, showing that RT can significantly increase BBS score after a period of training. Heterogeneity of the current results cannot be ruled out, due the diversity of target population, device type or training protocol.
Brain plasticity is defined as the intrinsic ability of the brain to reorganize its function and structure in response to stimuli and injuries. It is widely recognized that neural plasticity is more likely to happen during the early stage of stroke (38). The plasticity process is initiated in an attempt to compensate for the lesion itself and its remote effects. Changed neural activity and connectivity, in terms of function and structure, could be detected in the perilesional and remote regions (39). The current study found that stroke patients treated with RT showed better outcomes of balance function in acute/subacute phase (< 6 months). The mechanisms above may benefit patients from RT at the early stage, while the correlation and interaction between the central network and the functional recovery need to be further investigated.
Subgroup analysis showed that RT presented better balance function in the exoskeleton subset. According to the device design, the structure of the exoskeleton resembles a human limb, as robot joint axis matches the joint axis of the lower limb. These devices are designed to operate side by side with the human lower limb, and are therefore attached to the lower limb at multiple locations. These systems are suitable for the early-stage patients, as they do not require significant motor ability. On the other hand, the end-effector device facilitates the gait by propulsion of footplates, which may aid movement of the feet and legs in a symmetrical manner. The joints of the end effector are not designed to match the human body. Therefore, these devices cannot perform segmental control of the lower limbs (40). For this reason, it is assumed that endeffector systems may be more suitable for patients with residual motor skills sufficient to control their movement (41). In the current study, only 3 RCTs investigated the effectiveness of an end-effector device, while 10 RCTs focused on exoskeletons. The limited sample size may conceal the real efficacy of interventions.
It was also not clear whether the observed differences between experimental and control groups may be impacted by the training intensity. The pooled results indicated that a total time of ≥ 10 h could improve balance function in the RT group. Time devoted to therapy is a rough estimation of training intensity and provided no clue for the actual amount and type of intervention (42). For instance, a 30-min training session could be either low- or high-intensity. Larger controlled trials are required to investigate the optimal frequency, intensity and duration of RT.
Study limitations
The current study has several limitations. Firstly, due to the limited sample size in individual trials, the pooled results of the current meta-analysis are different from previous ones. Therefore, multi-centre RCTs with larger sample size are warranted to clarify the effectiveness of RT. Secondly, timing of assessment may play a role in the data synthesis and it varied across individual studies. In the current study, 5 trials reported longitudinal results. Three trials performed follow-up at 1-month and other 2 at 6 months. Interestingly, 4-week follow-up demonstrated significant improvement in 2 out of 3 trials (24, 29) while another trial followed up at 4 weeks and those at 6 months did not (20, 22, 26). It is assumed that the efficacy of RT may wane with time.
It is suggested that future studies adopt longitudinal design to explore the role of timing of assessment, which may provide significant insight to training protocol modification. Last, but not least, relevant studies might be missed due to language barriers, which may have led to an incomplete synthesis of data, in particular, advanced robotics were developed in non-English countries, such as Japan and Germany.
Conclusion
This meta-analysis showed that the use of RT has positive effects on balance function compared with CT, especially for subjects in the acute/subacute phase after stroke, treated with exoskeleton and a total training time of more than 10 h. Robotics may compensate part of therapists’ workload and carry out accurate and objective monitoring of motion parameters, providing real-time feedback. RT may therefore be considered a promising intervention for improving balance function in stroke survivors. When combining these results into clinical practice, it should be cautious because of the limited sample included in the current meta-analysis. Future studies that are well-designed and large scale are required to further verify the effectiveness of RT for balance and to determine the optimal RT protocol.
Supplementary Material
ACKNOWLEDGEMENTS
Funding
This work was funded by the National Key R&D Program of China (grant number 2017YFB1303200) and the Nanjing Municipal Science and Technology Bureau (grant number 2019060002). The funding bodies had no role in the study design, data collection, analysis, or the interpretation of data.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.GBD 2016 Stroke Collaborators , Global, Regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 439–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hou YR, Chiu YL, Chiang SL, Chen HY, Sung WH. Feasibility of a smartphone-based balance assessment system for subjects with chronic stroke. Comput Methods Programs Biomed 2018; 161: 191–195. [DOI] [PubMed] [Google Scholar]
- 3.Kim HY, Shin JH, Yang SP, Shin MA, Lee SH. Robot-assisted gait training for balance and lower extremity function in patients with infratentorial stroke: a single-blinded randomized controlled trial. J Neuroeng Rehabil 2019; 16: 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louie DR, Eng JJ. Berg Balance Scale score at admission can predict walking suitable for community ambulation at discharge from inpatient stroke rehabilitation. J Rehabil Med 2018; 50: 37–44. [DOI] [PubMed] [Google Scholar]
- 5.Middleton A, Braun CH, Lewek MD, Fritz SL. Balance impairment limits ability to increase walking speed in individuals with chronic stroke. Disabil Rehabil 2017; 39: 497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris JE, Eng JJ, Marigold DS, Tokuno CD, Louis CL. Relationship of balance and mobility to fall incidence in people with chronic stroke. Phys Ther 2005; 85: 150–158. [PubMed] [Google Scholar]
- 7.Louie DR, Eng JJ. Powered robotic exoskeletons in poststroke rehabilitation of gait: a scoping review. J Neuroeng Rehabil 2016; 13: 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buesing C, Fisch G, O’Donnell M, Shahidi I, Thomas L, Mummidisetty CK, et al. Effects of a wearable exoskeleton stride management assist system (SMA®) on spatiotemporal gait characteristics in individuals after stroke: a randomized controlled trial. J Neuroeng Rehabil 2015; 12: 69–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nam YG, Lee JW, Park JW, Lee HJ, Nam KY, Park JH, et al. Effects of electromechanical exoskeleton-assisted gait training on walking ability of stroke patients: a randomized controlled trial. Arch Phys Med Rehabil 2019; 100: 26–31. [DOI] [PubMed] [Google Scholar]
- 10.Veerbeek JM, Langbroek-Amersfoort AC, van Wegen EE, Meskers CG, Kwakkel G. Effects of robot-assisted therapy for the upper limb after stroke. Neurorehabil Neural Repair 2017; 31: 107–121. [DOI] [PubMed] [Google Scholar]
- 11.Swinnen E, Beckwée D, Meeusen R, Baeyens JP, Kerckhofs E. Does robot-assisted gait rehabilitation improve balance in stroke patients? A systematic review. Top Stroke Rehabil 2014; 21: 87–100. [DOI] [PubMed] [Google Scholar]
- 12.Mehrholz J, S Thomas, C Werner J, Kugler J, Pohl M, Elsner B. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev 2017; 5: CD006185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schröder J, Truijen S, Van Criekinge T, Saeys W. Feasibility and effectiveness of repetitive gait training early after stroke: a systematic review and meta-analysis. J Rehabil Med 2019; 51: 78–88. [DOI] [PubMed] [Google Scholar]
- 14.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003, 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira FMRM, Chaves MEA, Oliveira VC, Van Petten AMVN, Vimieiro CBS. Effectiveness of robot therapy on body function and structure in people with limited upper limb function: a systematic review and meta-analysis. PLoS One 2018; 137: e0200330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bang DH. Shin WS. Effects of robot-assisted gait training on spatiotemporal gait parameters and balance in patients with chronic stroke: a randomized controlled pilot trial. NeuroRehabilitation 2016; 38: 343–349. [DOI] [PubMed] [Google Scholar]
- 19.Bei N, Bei Z, Chen Y. The effects of rehabilitation robot on lower limb function in elderly stroke patients. China Tropical Med 2015; 15: 1246–1248. [Google Scholar]
- 20.Gandolfi M, Valè N, Dimitrova E, Zanolin ME, Mattiuz N, Battistuzzi E, et al. Robot-assisted stair climbing training on postural control and sensory integration processes in chronic post-stroke patients: a randomized controlled clinical trial. Front Neurosci 2019; 13: 1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han EY, Im SH, Kim BR, Seo MJ, Kim MO. Robot-assisted gait training improves brachial-ankle pulse wave velocity and peak aerobic capacity in subacute stroke patients with totally dependent ambulation: randomized controlled trial. Medicine 2016; 95: e5078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hornby TG, Campbell DD, Kahn JH, Demott T, Moore JL, Roth HR. Enhanced gait-related improvements after therapist – versus robotic-assisted locomotor training in subjects with chronic stroke: a randomized controlled study. Stroke 2008; 39: 1786–1792. [DOI] [PubMed] [Google Scholar]
- 23.Kim J, Kim DY, Chun MH, Kim SW, Jeon HR, Hwang CH, et al. Effects of robot-(Morning Walk) assisted gait training for patients after stroke: a randomized controlled trial. Clin Rehabil 2019; 33: 516–523. [DOI] [PubMed] [Google Scholar]
- 24.Kim SY, Yang L, Park IJ, Kim EJ, JoshuaPark MS, You SH, et al. Effects of Innovative WALKBOT robotic-assisted locomotor training on balance and gait recovery in hemiparetic stroke: a prospective, randomized, experimenter blinded case control study with a four-week follow-up. IEEE Trans Neural Syst Rehabil Eng 2015; 23: 636–642. [DOI] [PubMed] [Google Scholar]
- 25.Lu JL, Chen ZM, Wu H, Yang W, Wu HH. Effect of lower limb rehabilitation robot on lower limb motor function of hemiplegic patients after stroke. Chin J Contemp Neurol Neurosurg 2017; 17: 334–339. [Google Scholar]
- 26.Ng MFW, Tong RKY, Li LSW. A pilot study of randomized clinical controlled trial of gait training in subacute stroke patients with partial body-weight support electromechanical gait trainer and functional electrical stimulation: six-month follow-up. Stroke 2008; 39: 154–160. [DOI] [PubMed] [Google Scholar]
- 27.Belas Dos Santos M, Barros de Oliveira C, Dos Santos A, Garabello Pires C, Dylewski V, Arida RM. Comparative study of conventional physiotherapy versus robot-assisted gait training associated to physiotherapy in individuals with ataxia after stroke. Behav Neurol 2018; 2018: 2892065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Westlake KP. Pilot study of Lokomat versus manualassisted treadmill training for locomotor recovery post– stroke. J Neuroeng Rehabil 2009; 6: 18-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yun N, Joo MC, Kim SC. Robot-assisted gait training effectively improved lateropulsion in subacute stroke patients: a single-blinded randomized controlled trial. Eur J Phys Rehabil Med 2018; 54: 827–836. [DOI] [PubMed] [Google Scholar]
- 30.Kim HY, Shin JH, Yang SP, Shin MA, Lee SH. Robot-assisted gait training for balance and lower extremity function in patients with infratentorial stroke: a single-blinded randomized controlled trial. J Neuroeng Rehabil 2019; 16: 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher S, Lucas L, Thrasher TA. Robot-assisted gait training for patients with hemiparesis due to stroke. Top Stroke Rehabil 2011; 18: 269–276. [DOI] [PubMed] [Google Scholar]
- 32.Peurala SH, Tarkka IM, Pitkänen K, Sivenius J. The effectiveness of body weight-supported gait training and floor walking in patients with chronic stroke. Arch Phys Med Rehabil 2005; 86: 1557–1564. [DOI] [PubMed] [Google Scholar]
- 33.Taveggia G, Borboni A, Mulé C, Villafañe JH, Negrini S. Conflicting results of robot-assisted versus usual gait training during postacute rehabilitation of stroke patients: a randomized clinical trial. Int J Rehabil Res 2016; 39: 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hidler J, Nichols D, Pelliccio M, Brady K, Campbell DD, Kahn JH, et al. Multicenter randomized clinical trial evaluating the effectiveness of the Lokomat in subacute stroke. Neurorehabil Neural Repair 2009; 23: 5–13. [DOI] [PubMed] [Google Scholar]
- 35.Dias D, Laíns J, Pereira A, Nunes R, Caldas J, Amaral C, et al. Can we improve gait skills in chronic hemiplegics? A randomised control trial with gait trainer. Eura Medicophys 2007; 43: 499–504. [PubMed] [Google Scholar]
- 36.Morone G, Paolucci S, Cherubini A, De Angelis D, Venturiero V, Coiro P, et al. Robot-assisted gait training for stroke patients: current state of the art and perspectives of robotics. Neuropsychiatr Dis Treat 2017; 13: 1303–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lefeber N, Swinnen E, Kerckhofs E. The immediate effects of robot-assistance on energy consumption and cardiorespiratory load during walking compared to walking without robot-assistance: a systematic review. Disabil Rehabil Assist Technol 2017; 12: 657–671. [DOI] [PubMed] [Google Scholar]
- 38.Rao N, Zielke D, Keller S, Burns M, Sharma A, Krieger R, et al. Pregait balance rehabilitation in acute stroke patients. Int J Rehabil Res 2013; 36: 112–117. [DOI] [PubMed] [Google Scholar]
- 39.Su F, Xu W. Enhancing brain plasticity to promote stroke recovery. Front Neurol; 2020: 11: 554089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lo HS, Xie SQ. Exoskeleton robots for upper-limb rehabilitation: state of the art and future prospects. Med Eng Phys 2012; 34: 261–268. [DOI] [PubMed] [Google Scholar]
- 41.Bertani R, Melegari C, De Cola MC, Bramanti A, Bramanti P, Calabrò RS. Effects of robot-assisted upper limb rehabilitation in stroke patients: a systematic review with meta-analysis. Neurol Sci 2017; 38: 1561–1569. [DOI] [PubMed] [Google Scholar]
- 42.Hayward KS, Brauer SG. Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clin Rehabil 2015; 29: 1234–1243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.