Abstract
Background
Mobile phone use has brought convenience, but the long or improper use of mobile phones can cause harm to the human body.
Objective
We aimed to assess the impact of improper mobile phone use on the risks of accidents and chronic disorders.
Methods
We systematically searched in PubMed, EMBASE, Cochrane, and Web of Science databases for studies published prior to April 5, 2019; relevant reviews were also searched to identify additional studies. A random-effects model was used to calculate the overall pooled estimates.
Results
Mobile phone users had a higher risk of accidents (relative risk [RR] 1.37, 95% CI 1.22 to 1.55). Long-term use of mobile phones increased accident risk relative to nonuse or short-term use (RR 2.10, 95% CI 1.63 to 2.70). Compared with nonuse, mobile phone use resulted in a higher risk for neoplasms (RR 1.07, 95% CI 1.01 to 1.14), eye diseases (RR 2.03, 95% CI 1.27 to 3.23), mental health disorders (RR 1.16, 95% CI 1.02 to 1.32), and headaches (RR 1.25, 95% CI 1.18 to 1.32); the pooled risk of other chronic disorders was 1.20 (95% CI 0.90 to 1.59). Subgroup analyses also confirmed the increased risk of accidents and chronic disorders.
Conclusions
Improper use of mobile phones can harm the human body. While enjoying the convenience brought by mobile phones, people have to use mobile phones properly and reasonably.
Keywords: cell phone, mobile phone, accident, neoplasm, radiation
Introduction
In the first quarter of 2019, the number of mobile phone users reached 7.9 billion, with an increase of approximately 2% year-on-year [1]. China had the most net additions during this quarter (30 million), followed by Nigeria (5 million), and the Philippines (4 million). In addition, it was predicted that the worldwide mobile phone market would reach 1.5 billion shipment units by the end of 2019 and that the pending arrival of 5G would attract more phone users by 2020 or 2021 [2]. Although mobile phones facilitate people's daily lives and provide effective auxiliary means for the treatment and management of diseases [3-5], the health hazards potentially caused by using mobile phones are also a growing concern.
Although many countries and regions have passed laws prohibiting the use of mobile phones while driving, the number of reported traffic accidents caused by using mobile phones while driving has been increasing in recent years [6,7]. Nearly one-quarter of all traffic accidents in the United Kingdom in 2013 were caused by drivers using phones while driving. In addition, harm may be caused to the ears, parotid glands, and indirect brain areas during mobile phone usage [8-10]. Some in vivo or in vitro [11], simulator [12], or real-world studies [13] have been carried out to test the effects between human body and mobile phone use. There is currently no consensus on the use of mobile phones and chronic disorders, especially with respect to neoplasms, because results conflict. Mobile phone radiation has been classified as a possible carcinogen to humans [14]; radiation might cause tumors or accelerate the growth of subclinical tumors [15,16]. In recent years, head and neck injuries related to mobile phones have increased sharply [17]. A cross-sectional study [17] in the United States using a national database showed that mobile phone use can be distracting and cause injuries. In addition, increasing attention had been paid to the impact of mobile phone use on mental health (for example, addiction [18,19]), and a new term—nomophobia—which is short for no mobile phone phobia and has been considered as a symptom or syndrome of problematic digital media use in mental health [20]. However, some studies believe that the available evidence has not yet suggested that mobile phone use can cause damage to the human body (especially with respect to cancer).
Given that the use of mobile phones is growing rapidly, it is still doubted whether the improper use of mobile phones causes injuries to the human body. Our paper will provide a thorough review of literature to explore the impact of improper mobile phone use, which includes accidents and chronic disorders, on human body health.
Methods
Search Strategy
Two of the authors systematically searched PubMed, EMBASE, Cochrane, and Web of Science databases from inception to April 4, 2019. The search was limited to studies on the human body published in the English language. Additional literature was screened by manually searching the reference lists of recent reviews and studies for papers meeting the inclusion criteria.
Inclusion and Exclusion Criteria
According to the International Statistical Classification of Diseases, tenth revision [21], accidents are defined as unplanned events that sometimes have inconvenient or undesirable consequences, at times being inconsequential, and which include transport accidents and other injuries. In our study, we used the term chronic disorders for all nonaccident outcomes, including neoplasms (brain tumor, thyroid cancer, glioma and astrocytoma); mental health disorders such as attention-deficit/hyperactivity disorder (ADHD), nomophobia-anxiety, insecurity, anger, or discomfort; headaches; sleep disorders; injuries to the head (eye, ear, oral); injuries to the wrist; diseases of male genital organs; and other unspecific disorders including DNA damage, genotoxic effects, blood–cerebrospinal fluid barrier damage, serum S100B levels damage, total prostate specific antigen (tPSA) disorder, free prostate specific antigen (fPSA) disorder, fPSA/tPSA disorder, poor DNA integrity, chromosomal damage. The term nomophobia, constructed on the definitions described in the Diagnostic and Statistical Manual of Mental Disorders (Fourth edition) [22] and labeled as a “phobia for a particular/specific thing,” was used to describe the psychological condition when people had a fear of being detached from mobile phone connectivity.
Our inclusion criteria were studies that focused on (1) damage, including accidents and chronic disorders, instead of promoting healthy outcomes; (2) the use of mobile phones, including digital phone and mobile phone radio frequency radiation; (3) improper use of mobile phone, including inappropriate use occasions (eg, using mobile phone while driving or cycling), long-time or long-term use of mobile phone, and using the phone in an incorrect posture; (4) accidents occurring during mobile phone use or chronic disorders resulting from mobile phone use rather than those from any other cause (eg, occupational injuries); and studies that were (5) published in English and with (6) outcome indicators, including odd ratios (OR) or relative risk (RR) and 95% confidence intervals or mean and standard deviation.
Abstracts, comments, conferences, replies, responses, reviews (including systematic reviews), case reports, and animal studies were excluded. Additionally, studies with incomplete data and duplicate studies were also excluded.
Data Extraction and Quality Assessment
The 2 authors worked simultaneously, but independently, to screen studies, extract data from studies meeting the inclusion criteria, and assess the quality of these studies. Each author’s results were cross-checked by the other, and any disagreements on study selection, data extraction, and study quality assessment were resolved by another author.
The following information was collected using standardized data extraction forms: author information, publication year, study design, participant age, sample size, study area, measures of mobile phone use, measures of outcome-related behavior, and key outcomes.
The Newcastle-Ottawa Scale [23] was designed for the evaluation of case-control studies and cohort studies. The evaluation criteria for cross-sectional studies included 11 items recommended by the Agency for Healthcare Research and Quality [24]. The quality of each study was graded as good, fair, or poor. To be rated as good, studies needed to meet all criteria. A study was rated as poor when 1 (or more) domain was assessed as having a serious flaw. Studies that met some but not all criteria were rated as fair.
Data Analysis
A random-effects model was used to calculate overall pooled estimates. Tests for heterogeneity between studies’ results were performed with the Cochran Q statistic and were quantified with the I2 statistic.
To examine the robustness of the findings, we performed subgroup analyses by country, participant age, sample size, and study-specific outcomes (accidents and chronic disorders). To validate the robustness of the findings, we performed a sensitivity analysis. The potential for publication bias was graphically explored with funnel plots, and publication bias was tested for significance with the Egger test and Begg test. All statistical procedures were 2-tailed with a significance level of 0.05 and were conducted using Stata software (version 13.0; StataCorp LLC).
Results
Study Inclusion
A total of 4228 studies were identified by the initial database search, and 3 studies were obtained by searching references; 2329 studies remained after the removal of duplicates (Figure 1). After screening titles and abstracts, 1922 records were excluded because they did not meet the selection criteria: case reports (n=9), summary reviews (n=117), nonpopulation studies (n=255), not about mobile phone use (n=1257), non-English (n=2), replies/abstracts (n=23), and no outcome indicators (n=259). Full texts of remaining papers were assessed for eligibility; 142 records were excluded because they were duplicates (n=2), case reports (n=11), summary reviews (n=39), nonpopulation research (n=49), not about mobile phone use (n=88), not English (n=8), replies/abstracts (n=6), or lacked outcome indicators (n=163). Finally, 41 studies [25-65] were included, which included cohort studies (n=10), case-control studies (n=20), and cross-sectional studies (n=11). Details are presented in Table S1 in Multimedia Appendix 1.
Figure 1.
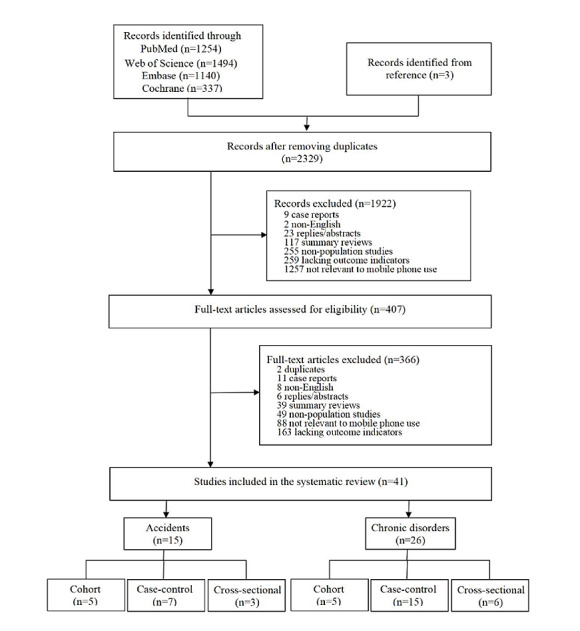
Flowchart of the selection of studies.
Study Characteristics and Quality Assessment
Of the 41 papers, 29 papers were published between 2011 and 2019 [25-28,30,31,35-37,41-43,45-48,50,54-65], 11 papers were published between 2002 and 2009 [32-34,38-40,44,49,51-53], and 1 paper was published in 1997 [29]. The sample sizes of the studies ranged from 6 to 15,406,515. All participants were over 7 years old. Studies were carried out in the United States (n=8) [26,30,32,37,45,50,59,64], Sweden (n=5) [38,51-53,61], Canada (n=3) [34,49,56], Korea (n=3) [27,62,63], China (n=2) [25,42], Vietnam (n=2) [31,58], Iran (n=2) [47,54], Denmark (n=1) [28], Italy (n=1) [33], Malaysia (n=1) [46], and Brazil (n=1) [57]; the remaining studies lacked relevant regional information. The outcomes were divided into accidents and chronic disorders—15 studies focused on accidents [30-34,45-47,49,50,54,56-58,64], which were mainly related to transport accidents (car accident, motorcycle accident, and unspecified transport accidents) and other accidental injuries, such as electrical injuries and explosions, and 26 studies [25-29,35-44,48,51-53,55,59-63,65] focused on chronic disorders, including neoplasms, ADHD, nomophobia, headaches, sleep disorders, dry eye diseases, ear injuries, oral problems, wrist injuries, reproductive health issues, and other unspecific chronic disorders (including DNA damage, genotoxic effects, blood-cerebrospinal fluid barrier, serum S100B levels, tPSA, fPSA, fPSA/tPSA, DNA integrity, chromosomal damage). Additional details can be found in Table S2 in Multimedia Appendix 1.
The results of the quality assessment indicated that 16 studies were good quality, and 25 were fair (Table S3 in Multimedia Appendix 1).
Mobile Phone Use and Accidents
Compared with nonmobile phone users, people who use mobile phones had a significantly higher risk for all accidents, with a pooled OR/RR of 1.55 (n=15,517,418, 95% CI 1.40 to 1.71; I2=93.7%). The risk for mobile phone users was 1.37 times (n=15,451,501, 95% CI 1.22 to 1.55; I2=96.6%) that for nonmobile phone users. The top 3 relative risks were 4.78 (95% CI 3.46 to 6.60) and 3.90 (95% CI 2.70 to 6.10), both for unspecified transport accidents, and 2.38 (95% CI 1.30 to 4.30) for car accidents. Those who used mobile phones long-term had a 2.10-fold (95% CI 1.63 to 2.70) higher risk of accidents than those who did not use mobile phones or who used them for short-term; the top 3 relative risks were 8.32 (95% CI 2.83 to 24.42), 7.05 (95% CI 2.64 to 18.83), and 6.76 (95% CI 2.60 to 17.55) for car accidents, car accidents, and unspecified transport accidents, respectively (Figure 2).
Figure 2.
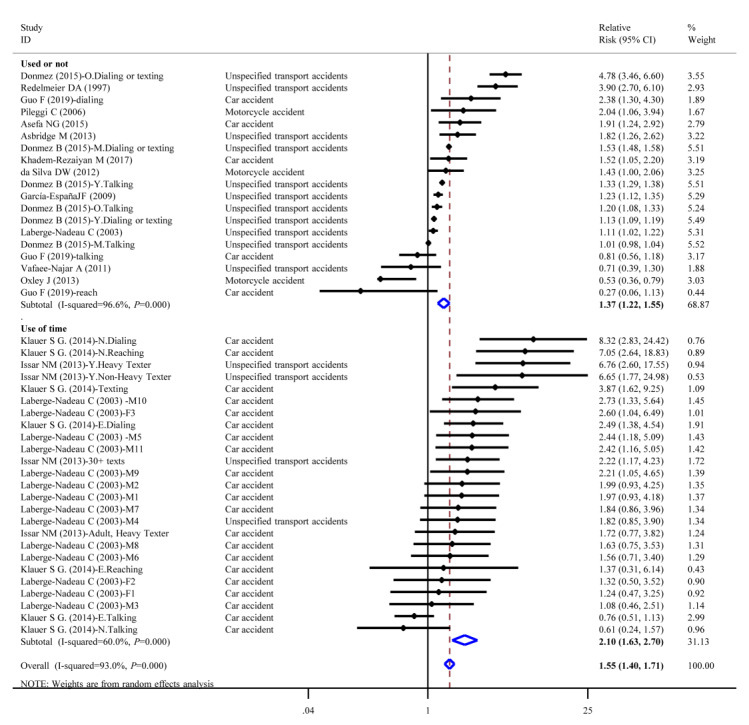
Forest plot of accident risk and mobile phone use.
Mobile Phone Use and Chronic Disorders
The pooled risk of chronic disorders caused by mobile phone use was 1.07 times that of nonmobile phone use (95% CI 1.01 to 1.14; I2=32.9%). Compared with nonmobile phone users, mobile phone users had a 1.07-fold risk of neoplasms (95% CI 0.93 to 1.23, I2=42.4%). The top relative risks of neoplasms were for brain tumor (RR 1.30, 95% CI 1.02 to 1.60), followed by thyroid cancer (RR 1.15, 95% CI 0.93 to 1.23). For long-term mobile phone users there was a higher risk of neoplasms, with a pooled relative risk of 1.07 (95% CI 0.97 to 1.17). The top 3 relative risks for outcomes were brain tumor (RR 1.80, 95% CI 1.10 to 2.90), glioma (RR 1.60, 95% CI 1.10 to 2.20), and thyroid cancer (RR 1.58, 95% CI 0.98 to 2.54). Furthermore, the position when using mobile phone also increased the risk of specific cancers; mobile phone users had a relative risk of 1.40 (95% CI 0.98 to 1.18; I2=0.0%) for brain tumor compared with nonmobile phone users (Figure 3).
Figure 3.
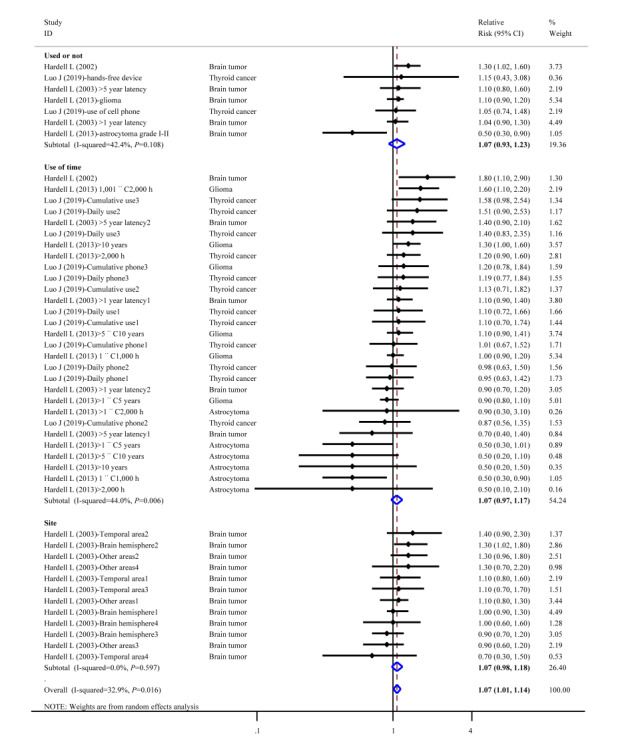
Forest plot of chronic disorder risk (neoplasms) and cell phone use.
Chronic nonneoplasm disorders caused by mobile phone use included mental disorders (ADHD, nomophobia), headaches, sleep disorders, injuries to the head (eye, ear, and oral), injuries to the wrist, male reproductive health issues, and other unspecific chronic disorders. Compared with nonmobile phone use, mobile phone use increased the risk of headaches (pooled risk 1.25, 95% CI 1.18 to 1.32, I2=41.0%; Figure 4A) and the risk of dry eye disease (RR 2.03, 95% CI 1.27 to 3.23, I2=0.0%; Figure 4B). Mobile phone users had a higher risk of ADHD than nonmobile phone users (RR 1.16, 95% CI 1.02 to 1.32, I2=51.6%; Figure 4C), and mobile phone use increased the risk of other unspecific chronic disorders, with a pooled risk of 1.20 (95% CI 0.90 to 1.59, I2=0.0%), including damage to the blood–cerebrospinal fluid barrier and elevated levels of serum S100B levels (Figure 4D).
Figure 4.
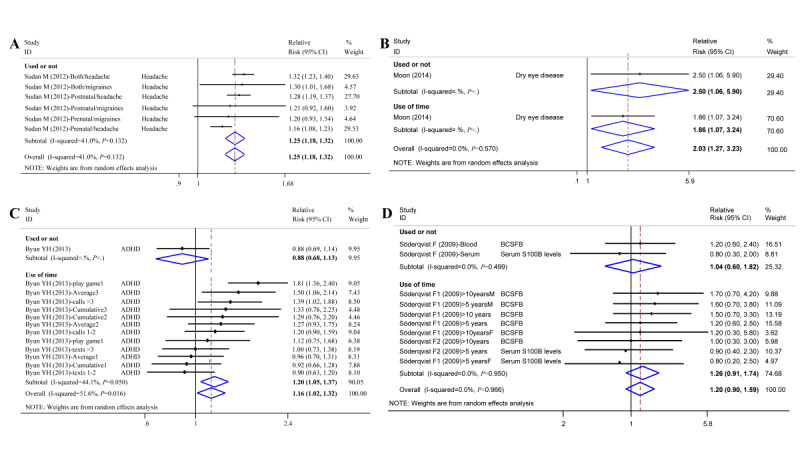
Forest plot of chronic disorder risk (nonneoplasm) and cell phone use. ADHD: attention deficit/hyperactivity disorder; BCSFB: blood-cerebrospinal fluid barrier.
Compared to nonmobile phone users and short-term users, the risk for nomophobia among long-term users was –0.06 (95% CI –0.74 to 0.63; I2=0.0%; Figure 5A); the risk was not statistically significant. Mobile phone use increased the risk of thumb injury (weighted mean difference [WMD] 218.48, 95% CI 2.93 to 434.02; I2=0.0%; Figure 5B) and wrist extension (WMD 0.82, 95% CI –0.53 to 2.16; I2=91.4%; Figure 5C). The risk of damage to hearing was 4.54 times higher for mobile phone users than that of the nonmobile phone users (WMD 4.54, 95% CI 3.29 to 5.80, I2=20.6%; Figure 5D).
Figure 5.
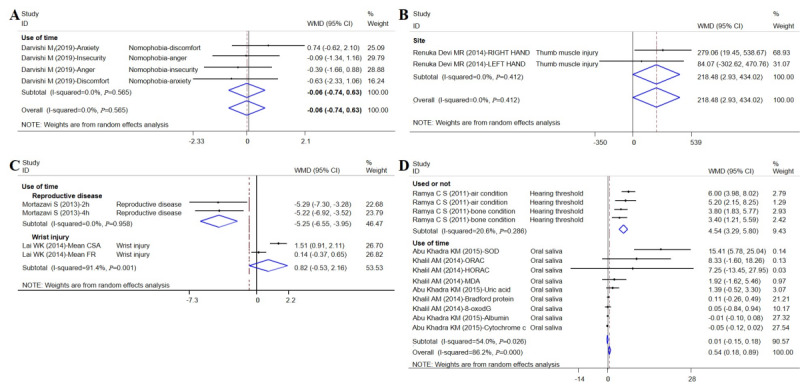
Forest plot of chronic disorder risk and cell phone use (continuous data). WMD: weight mean difference.
Subgroup Analysis
Subgroup analysis showed a consistent increase in the overall risk of cancer in the population (Table 1). Participants from the United States (OR 1.35, 95% CI 1.18 to 1.55), Denmark (OR 1.25, 95% CI 1.18 to 1.32), and aged 18 to 35 years (OR 1.62, 95% CI 1.31 to 2.00) had higher risks of injury with mobile phone use. Similarly, the larger the sample size, the higher the risk of injury caused by the use of mobile phones. The risk of unspecified transport accidents significantly increased with mobile phone use as a result of accidents (OR 1.43, 95% CI 1.25 to 1.64). The higher risks of chronic disorders on the human body were injuries to the ear (OR 4.54, 95% CI 3.29 to 5.80), headaches (OR 1.25, 95% CI 1.18 to 1.32), and other unspecific chronic disorders (OR 0.51, 95% CI 0.04 to 0.99).
Table 1.
Subgroup analyses of the risk of injuries by mobile phone use or nonuse.
| Component | Studies, n (%) | Odds ratio (95% CI) (or random-effects weighted mean differencea) | |||
| Country |
|
|
|||
|
|
Iran | 2 (2) | 1.08 (0.51, 2.27) | ||
|
|
Canada | 3 (3) | 1.95 (0.94, 4.07) | ||
|
|
United States | 5 (13) | 1.35 (1.18, 1.55) | ||
|
|
Denmark | 1 (6) | 1.25 (1.18, 1.32) | ||
|
|
Sweden | 4 (7) | 1.06 (0.91, 1.24) | ||
| Sample size |
|
|
|||
|
|
100-500 | 5 (8) | 1.17 (0.79, 1.72) | ||
|
|
500-1000 | 5 (6) | 1.76 (1.14, 2.71) | ||
|
|
>1000 | 10 (22) | 1.21 (1.11, 1.32) | ||
| Age |
|
|
|||
|
|
1-18 years | 4 (9) | 1.23 (1.15, 1.32) | ||
|
|
18-35 years | 4 (4) | 1.62 (1.31, 2.00) | ||
|
|
35-65 years | 5 (7) | 1.02 (0.87, 1.21) | ||
| Accidents |
|
|
|||
|
|
Car accident | 3 (5) | 1.31 (0.81, 2.13) | ||
|
|
Unspecified transport accidents | 6 (11) | 1.43 (1.25, 1.64) | ||
|
|
Motorcycle accident | 3 (3) | 1.13 (0.51, 2.48) | ||
| Chronic disorders |
|
|
|||
|
|
Mental disorders | 2 (2) | 1.37 (0.54, 3.51) | ||
|
|
Headache | 1 (6) | 1.25 (1.18, 1.32) | ||
|
|
Neoplasms | 4 (7) | 1.07 (0.93, 1.23) | ||
|
|
Other unspecific chronic disorders | 2 (2) | 1.04 (0.60, 1.82) | ||
| Chronic disorders |
|
|
|||
|
|
Other unspecific chronic disorders | 2 (4) | 0.51 (0.04, 0.99)a | ||
|
|
Injuries to ear | 1 (4) | 4.54 (3.29, 5.80)a | ||
|
|
DNA damage | 1 (1) | 0.13 (-0.15, 0.40)a | ||
aOutcome measures are continuous variables; therefore, random-effects weighted mean difference was used.
Among the participants with various mobile phone use duration, Canadians and Koreans had a higher risk of injury to the human body compared with that of other populations. In studies with a participant sample size that ranged from 100 to 500 and with participants aged 18 to 35 years, there was a higher risk of accidents and chronic disorders (Table 2). In general, mobile phone use increased the risk for injury to the human body. Similarly, unspecified transport accidents were the highest cause of human body injuries as a result of accidents (OR 3.23, 95% CI 1.65 to 6.30). Increasing mobile phone use was associated with the higher risks of DNA damage (OR 7.52, 95% CI 2.23 to 12.81), male reproductive health issues (OR –4.69, 95% CI –5.64 to –3.75), and mental disorders (OR 1.20, 95% CI 1.05 to 1.37).
Table 2.
Subgroup analyses of the risk of injuries by the duration of mobile phone use.
| Component | Studies (included entries), n (%) | Odds ratio (95% CI) (or random-effects weighted mean differencea) | |||
| Country |
|
|
|||
|
|
United States | 3 (23) | 1.20 (0.78, 1.84) | ||
|
|
Canada | 1 (14) | 1.91 (1.54, 2.35) | ||
|
|
Korea | 1 (12) | 1.20 (1.05, 1.37) | ||
|
|
Sweden | 4 (37) | 1.06 (0.98, 1.15) | ||
| Sample size |
|
|
|||
|
|
100-500 | 4 (19) | 1.89 (1.32, 2.71) | ||
|
|
500-1000 | 1 (12) | 1.13 (0.99, 1.28) | ||
|
|
>1000 | 5 (55) | 1.16 (1.07, 1.25) | ||
| Age |
|
|
|||
|
|
1-18 years | 1 (12) | 1.20 (1.05, 1.37) | ||
|
|
35-65 years | 6 (41) | 1.16 (1.03, 1.30) | ||
| Accidents |
|
|
|||
|
|
Car accident | 2 (21) | 1.95 (1.49, 2.55) | ||
|
|
Unspecified transport accidents | 1 (4) | 3.23 (1.65, 6.30) | ||
| Chronic disorders |
|
|
|||
|
|
Mental disorders | 1 (12) | 1.20 (1.05, 1.37) | ||
|
|
Tumors | 4 (41) | 1.07 (1.00, 1.15) | ||
|
|
Other unspecific chronic disorders | 2 (8) | 1.26 (0.91, 1.74) | ||
| Chronic disorders |
|
|
|||
|
|
Nomophobia | 1 (4) | –0.06 (–0.74, 0.63)a | ||
|
|
Oral problem | 2 (9) | 0.01 (–0.15, 0.18)a | ||
|
|
DNA damage | 2 (4) | 7.52 (2.23, 12.81)a | ||
|
|
Male reproductive health issues | 1 (4) | –4.69 (–5.64, –3.75)a | ||
|
|
Injuries to wrist | 1 (2) | 0.82 (–0.53, 2.16)a | ||
aOutcome measures are continuous variables; therefore, random-effects weighted mean difference was used.
Publication Bias
Research results that are statistically significant may be more likely to be reported and published than results that are insignificant and invalid. In our study, the funnel plot was generally symmetric, indicating the absence of publication bias (Figure S1 in Multimedia Appendix 1).
Discussion
Principal Findings
Our review included large participant-level cohort, cross-sectional, and case-control studies on the impact of mobile phone use on outcomes related to harm to the human body. The findings suggested that mobile phone use increased the risk of accidents and chronic disorders involving the human body. Mobile phone use increased the risk of accidents by 55%. Car accidents had the highest relative risk of traffic injuries for mobile phone users. Mobile phone use also increased the risk of chronic disorders, increasing the risk of neoplasms, ADHD, headaches, and eye injuries by 7%, 16%, 25%, and 103%, respectively.
Consistent with the findings of previous studies [66-69], mobile phone use while driving increased the risk of accidents, given that it may lead to decreased situational awareness and deteriorated driving performance. Phone use while driving has become a priority road safety issues, and although it is difficult to assess the absolute increased risk for collision due to distraction of drivers caused by using mobile phones, driving simulator [6] and real-world [67] naturalistic driving studies have shown that the risk for talking on the phone while driving is significantly higher than that for undistracted driving and is comparable to the risk of driving while drunk. Ludovic et al [70] found that mobile phone use while driving was a significant distraction—even when a user is not using a mobile phone, the vibration or beeping of the phone will attract the user's attention, thus becoming a cause of motor vehicle crashes. Drivers were more likely to miss traffic signals and were involved twice as often in car crashes when having a phone conversation while driving. In addition, visual manual tasks such as texting or typing were more likely to increase the risk of traffic accidents than other types of observable distractions [70,71]. Some interventional driving strategies and preventive measures have reduced the risk of traffic accidents among people, such as graduated driver licensing programs or advertising campaigns [72]. For example, United States, Great Britain, Canada, South Africa, and Australia have developed and use a graduated driver licensing program, which allows drivers to gain experience in low-risk driving conditions by adding an intermediate phase between the learning stage and the acquisition of the driving license [73]. Some studies [74,75] showed that the effectiveness of educational and preventive road safety programs is yet to be confirmed.
Although the risk of neoplasm from mobile phone use is still unclear, our meta-analysis suggests that improper use of mobile phones increases the risk of brain tumor, glioma, and thyroid cancer. Mobile phone radiation has been classified as possibly carcinogenic to humans [76]. There appears to be sufficient evidence that radiofrequency electromagnetic fields can cause nonthermal biological effects even when they do not cause tissue heating [77,78]. Previous evidence of damage from radiofrequency electromagnetic fields is the strongest for cancers caused by long-term exposure to mobile phones, especially brain tumor gliomas, glioblastomas, and acoustic neuromas [79,80]. In fact, the rates of brain tumors are increasing in Sweden, and the use of phones has been suggested to be the cause [81]. Little et al [82] found that ever having used mobile phones is not significantly associated with risk of glioma, but there could be increased risk for long-term users. Incorrect phone posture can increase the risk of wrist damage, chronic neck pain, and chronic shoulder pain, and the pain and fatigue worsen with longer mobile phone use [83-85]. When people use mobile phones, their body is relaxed, and their neck is prone to be bent. Hansraj et al [86] showed that there was a positive correlation between neck flexion and neck force, as well as head and neck posture in cervical spine stress and related neck pain. In addition, the long-term use of mobile phones may lead to ADHD in children and nomophobia. Studies have shown that adolescents with ADHD use electronic products significantly more often, and they usually have more sleep-wake problems [87]. Mobile phones are playing an increasingly important role in our lives. People have become dependent on mobile phones and suffer from no mobile phone phobia (ie, when not having a mobile phone, individuals feel discomfort, insecurity, anxiety, or anger), although the definition of nomophobia is not standardized, scholars have shown increasing interest and relevant scales have been designed and adjusted for different regions [88]. Finally, our meta-analysis demonstrated that mobile phone use can cause other chronic disorders, such as DNA damage (WMD 0.13, 95% CI –0.15 to 0.40). Several studies [89,90] have shown that radiofrequency radiation exposure can lead to oxidative stress in various tissues. Oxidative stress is known to play a central role in the development of cancer and aging, and it serves as a signaling agent in the inflammatory response. Recent studies [15,91] reported that the radiofrequency radiation emitted from mobile phones causes oxidative stress. Oxidative stress related to radiofrequency radiation leads to lipid, protein, and DNA damage in various tissues [15]. Our findings suggest that although the current allowable mobile phone radiation level is very low, it may be sufficient to induce biological effects. Some studies [82,92,93] have reported that existing data are not sufficient to support the assumption that tumors are caused by mobile phone usage. Thus, determination of whether these effects might cause any significant health effects requires further investigation, especially with respect to neoplasms.
Limitations
The inclusion criteria for our study were rigorous, and thus, some reports were excluded. For example, the incidences of taking selfies and sharing them on social media as well as selfie-related behaviors are increasing, particularly among young people, which possibly leads to selfie-related trauma [94,95]. Other studies [96,97,98] have reported physical harm caused by mobile phones, such as ear trauma, thigh injuries, electrical burns, and injuries caused by phone explosions. Furthermore, it has been suggested that electromagnetic fields generated by mobile phone may have long-term harmful effects, including an increase in infertility, Alzheimer disease, and other neurodegenerative diseases [99].
Our study also has some limitations. First, “damage” and “injury” were used as search queries in our study to retrieve papers on the health effects of mobile phones, other adverse outcomes caused by phone use may have been missed. Second, only 10 of the 41 studies were longitudinal studies. Additional longitudinal studies could confirm the causal relationship between mobile phone use and human health. Third, the different environments and behaviors of using mobile phones might lead to different risks of injury. We did not consider different patterns or reasons for using mobile phones in different regions and by different people, and we did not further analyze specific types and purposes of using mobile phones, such as texting or making phone calls. Finally, there was heterogeneity in our study (I2>75%); therefore, we performed subgroup analyses to explore the source of heterogeneity.
Conclusions
There is growing evidence that mobile phone use affects the human body. Our study suggests that the use of mobile phones causes not only accidents but also chronic disorders to the human body. Although some findings are still controversial, the harm that mobile phones cause to the human body cannot be underestimated, and more research is needed to explore the direct evidence of damage to the human body.
Acknowledgments
This study was partly funded by the National Natural Science Foundation of China (grants 91746205, 71910107004, 71673199), and the China Medical Board (grant 16-262). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The two corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit the study for publication.
Abbreviations
- ADHD
attention-deficit/hyperactivity disorder
- fPSA
free prostate specific antigen
- OR
odds ratio
- RR
relative risk
- tPSA
total prostate specific antigen
- WMD
weighted mean difference
Literature search strategy, basic characteristics of studies, quality assessment, and publication bias test.
Footnotes
Authors' Contributions: XC and YC are co-first authors. PJ (jiapengff@hotmail.com) and YW (wyg@tmu.edu.cn) are co-corresponding authors.
Conflicts of Interest: None declared.
References
- 1.Mobility Reports. Ericsson. [2019-09-01]. https://www.ericsson.com/en/mobility-report/reports .
- 2.Gartner Gartner: Global smartphone sales are expected to reach 1.5 billion units in 2019, down 2.5% year-on-year. 199IT 中国互联网数据咨询网. 2019. Aug 7, [2019-09-01]. http://www.199it.com/archives/917684.html .
- 3.Indraratna Praveen, Tardo Daniel, Yu Jennifer, Delbaere Kim, Brodie Matthew, Lovell Nigel, Ooi Sze-Yuan. Mobile phone technologies in the management of ischemic heart disease, heart failure, and hypertension: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020 Jul 06;8(7):e16695. doi: 10.2196/16695. https://mhealth.jmir.org/2020/7/e16695/ v8i7e16695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitehead Lisa, Seaton Philippa. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res. 2016 May 16;18(5):e97. doi: 10.2196/jmir.4883. https://www.jmir.org/2016/5/e97/ v18i5e97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Youfa, Xue Hong, Huang Yaqi, Huang Lili, Zhang Dongsong. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr. 2017 May;8(3):449–462. doi: 10.3945/an.116.014100. http://europepmc.org/abstract/MED/28507010 .8/3/449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wijayaratna KP, Cunningham ML, Regan MA, Jian S, Chand S, Dixit VV. Mobile phone conversation distraction: understanding differences in impact between simulator and naturalistic driving studies. Accid Anal Prev. 2019 Aug;129:108–118. doi: 10.1016/j.aap.2019.04.017.S0001-4575(18)31017-0 [DOI] [PubMed] [Google Scholar]
- 7.Sun Ming, Sun Xiaoduan, Shan Donghui. Pedestrian crash analysis with latent class clustering method. Accid Anal Prev. 2019 Mar;124:50–57. doi: 10.1016/j.aap.2018.12.016.S0001-4575(18)31192-8 [DOI] [PubMed] [Google Scholar]
- 8.de Siqueira EC, de Souza FTA, Gomez RS, Gomes CC, de Souza RP. Does cell phone use increase the chances of parotid gland tumor development? a systematic review and meta-analysis. J Oral Pathol Med. 2017 Aug 24;46(7):480–483. doi: 10.1111/jop.12531. [DOI] [PubMed] [Google Scholar]
- 9.Wall Stephen, Wang Zhong-Min, Kendig Thomas, Dobraca Dina, Lipsett Michael. Real-world cell phone radiofrequency electromagnetic field exposures. Environ Res. 2019 Apr;171:581–592. doi: 10.1016/j.envres.2018.09.015.S0013-9351(18)30502-4 [DOI] [PubMed] [Google Scholar]
- 10.Ahlbom Anders, Feychting Maria. Mobile telephones and brain tumours. BMJ. 2011 Oct 19;343:d6605. doi: 10.1136/bmj.d6605. [DOI] [PubMed] [Google Scholar]
- 11.De Iuliis Geoffry N, Newey Rhiannon J, King Bruce V, Aitken R John. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro. PLoS One. 2009 Jul 31;4(7):e6446. doi: 10.1371/journal.pone.0006446. https://dx.plos.org/10.1371/journal.pone.0006446 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stavrinos Despina, Byington Katherine W, Schwebel David C. Effect of cell phone distraction on pediatric pedestrian injury risk. Pediatrics. 2009 Feb;123(2):e179–85. doi: 10.1542/peds.2008-1382.123/2/e179 [DOI] [PubMed] [Google Scholar]
- 13.Cooper Joel M, Strayer David L. Effects of simulator practice and real-world experience on cell-phone-related driver distraction. Hum Factors. 2008 Dec;50(6):893–902. doi: 10.1518/001872008X374983. [DOI] [PubMed] [Google Scholar]
- 14.Kim K, Kabir E, Jahan SA. The use of cell phone and insight into its potential human health impacts. Environ Monit Assess. 2016 Apr 10;188(4):1–11. doi: 10.1007/s10661-016-5227-1.10.1007/s10661-016-5227-1 [DOI] [PubMed] [Google Scholar]
- 15.Dasdag S, Akdag MZ, Kizil G, Kizil M, Cakir DU, Yokus B. Effect of 900 MHz radio frequency radiation on beta amyloid protein, protein carbonyl, and malondialdehyde in the brain. Electromagn Biol Med. 2012 Mar 23;31(1):67–74. doi: 10.3109/15368378.2011.624654. [DOI] [PubMed] [Google Scholar]
- 16.de Vocht F. Inferring the 1985-2014 impact of mobile phone use on selected brain cancer subtypes using Bayesian structural time series and synthetic controls. Environ Int. 2016 Dec;97:100–107. doi: 10.1016/j.envint.2016.10.019. https://linkinghub.elsevier.com/retrieve/pii/S0160-4120(16)30386-5 .S0160-4120(16)30386-5 [DOI] [PubMed] [Google Scholar]
- 17.Povolotskiy R, Gupta N, Leverant AB, Kandinov A, Paskhover B. Head and neck injuries associated with cell phone use. JAMA Otolaryngol Head Neck Surg. 2020 Feb 01;146(2):122–127. doi: 10.1001/jamaoto.2019.3678. http://europepmc.org/abstract/MED/31804678 .2756314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khasawneh OY. Technophobia without boarders: the influence of technophobia and emotional intelligence on technology acceptance and the moderating influence of organizational climate. Comput Human Behav. 2018 Nov;88:210–218. doi: 10.1016/j.chb.2018.07.007. [DOI] [Google Scholar]
- 19.Xu Z, Turel O, Yuan Y. Online game addiction among adolescents: motivation and prevention factors. Eur J Inf Syst. 2017 Dec 19;21(3):321–340. doi: 10.1057/ejis.2011.56. [DOI] [Google Scholar]
- 20.Farooqui IA, Pore P, Gothankar J. Nomophobia: an emerging issue in medical institutions? J Ment Health. 2018 Oct 22;27(5):438–441. doi: 10.1080/09638237.2017.1417564. [DOI] [PubMed] [Google Scholar]
- 21.ICD-10 International Classification of Diseases. [2019-06-05]. http://icd-codes.info .
- 22.Battle Dolores Elaine. Diagnostic and statistical manual of mental disorders (DSM) Codas. 2013;25(2):191–2. doi: 10.1590/s2317-17822013000200017. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S2317-17822013000200017&lng=en&nrm=iso&tlng=en .S2317-17822013000200017 [DOI] [PubMed] [Google Scholar]
- 23.Wells GA. Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. The Ottawa Hospital. 2004. [2019-09-01]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 24.Methods guide for effectiveness and comparative effectiveness reviews. Agency for Healthcare Research and Quality. 2008. [2021-09-13]. https://effectivehealthcare.ahrq.gov/products/cer-methods-guide/overview . [PubMed]
- 25.Zhang G, Yan H, Chen Q, Liu K, Ling X, Sun L, Zhou N, Wang Z, Zou P, Wang X, Tan L, Cui Z, Zhou Z, Liu J, Ao L, Cao J. Effects of cell phone use on semen parameters: Results from the MARHCS cohort study in Chongqing, China. Environ Int. 2016 May;91:116–21. doi: 10.1016/j.envint.2016.02.028.S0160-4120(16)30065-4 [DOI] [PubMed] [Google Scholar]
- 26.Lewis RC, Mínguez-Alarcón Lidia, Meeker JD, Williams PL, Mezei G, Ford JB, Hauser R, EARTH Study Team Self-reported mobile phone use and semen parameters among men from a fertility clinic. Reprod Toxicol. 2017 Jan;67:42–47. doi: 10.1016/j.reprotox.2016.11.008. http://europepmc.org/abstract/MED/27838386 .S0890-6238(16)30408-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Byun Y, Ha M, Kwon H, Hong Y, Leem J, Sakong J, Kim SY, Lee CG, Kang D, Choi H, Kim N. Mobile phone use, blood lead levels, and attention deficit hyperactivity symptoms in children: a longitudinal study. PLoS One. 2013 Mar 21;8(3):e59742. doi: 10.1371/journal.pone.0059742. https://dx.plos.org/10.1371/journal.pone.0059742 .PONE-D-12-23210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sudan M, Kheifets Leeka, Arah Onyebuchi, Olsen Jorn, Zeltzer Lonnie. Prenatal and postnatal cell phone exposures and headaches in children. Open Pediatr Med Journal. 2012 Dec 05;6(2012):46–52. doi: 10.2174/1874309901206010046. http://europepmc.org/abstract/MED/23750182 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simşek Veli, Sahin Hayrettin, Akay AF, Kaya H, Bircan MK. The effects of cellular telephone use on serum PSA levels in men. Int Urol Nephrol. 2003;35(2):193–6. doi: 10.1023/b:urol.0000020295.92477.c4. [DOI] [PubMed] [Google Scholar]
- 30.Issar Neil M, Kadakia RJ, Tsahakis JM, Yoneda ZT, Sethi MK, Mir HR, Archer K, Obremskey WT, Jahangir AA. The link between texting and motor vehicle collision frequency in the orthopaedic trauma population. J Inj Violence Res. 2013 Jul 01;5(2):95–100. doi: 10.5249/jivr.v5i2.330. doi: 10.5249/jivr.v5i2.330.330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Truong LT, Nguyen HTT, De Gruyter C. Mobile phone use while riding a motorcycle and crashes among university students. Traffic Inj Prev. 2019 Mar 19;20(2):204–210. doi: 10.1080/15389588.2018.1546048. [DOI] [PubMed] [Google Scholar]
- 32.García-España J Felipe, Ginsburg KR, Durbin DR, Elliott MR, Winston FK. Primary access to vehicles increases risky teen driving behaviors and crashes: national perspective. Pediatrics. 2009 Oct 28;124(4):1069–75. doi: 10.1542/peds.2008-3443. [DOI] [PubMed] [Google Scholar]
- 33.Pileggi C, Bianco A, Nobile CG, Angelillo IF. Risky behaviors among motorcycling adolescents in Italy. J Pediatr. 2006 Apr;148(4):527–32. doi: 10.1016/j.jpeds.2005.11.017.S0022-3476(05)01087-5 [DOI] [PubMed] [Google Scholar]
- 34.Laberge-Nadeau C, Maag U, Bellavance F, Lapierre SD, Desjardins D, Messier S, Saïdi A. Wireless telephones and the risk of road crashes. Accid Anal Prev. 2003 Sep;35(5):649–660. doi: 10.1016/s0001-4575(02)00043-x. [DOI] [PubMed] [Google Scholar]
- 35.Souza LDCM, Cerqueira EDMM, Meireles JRC. Assessment of nuclear abnormalities in exfoliated cells from the oral epithelium of mobile phone users. Electromagn Biol Med. 2014 Jun 28;33(2):98–102. doi: 10.3109/15368378.2013.783856. [DOI] [PubMed] [Google Scholar]
- 36.Khalil AM, Abu Khadra KM, Aljaberi AM, Gagaa MH, Issa HS. Assessment of oxidant/antioxidant status in saliva of cell phone users. Electromagn Biol Med. 2014 Jun 19;33(2):92–7. doi: 10.3109/15368378.2013.783855. [DOI] [PubMed] [Google Scholar]
- 37.Luo J, Deziel NC, Huang H, Chen Y, Ni X, Ma S, Udelsman R, Zhang Y. Cell phone use and risk of thyroid cancer: a population-based case-control study in Connecticut. Ann Epidemiol. 2019 Jan;29:39–45. doi: 10.1016/j.annepidem.2018.10.004. http://europepmc.org/abstract/MED/30446214 .S1047-2797(18)30284-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hardell L, Hallquist A, Mild KH, Carlberg M, Påhlson A, Lilja A. Cellular and cordless telephones and the risk for brain tumours. Eur J Cancer Prev. 2002 Aug;11(4):377–86. doi: 10.1097/00008469-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Tiwari R, Lakshmi NK, Surender V, Rajesh ADV, Bhargava SC, Ahuja YR. Combinative exposure effect of radio frequency signals from CDMA mobile phones and aphidicolin on DNA integrity. Electromagn Biol Med. 2008 Jul 07;27(4):418–25. doi: 10.1080/15368370802473554.906035361 [DOI] [PubMed] [Google Scholar]
- 40.Gadhia PK, Shah T, Mistry A, Pithawala M, Tamakuwala D. A preliminary study to assess possible chromosomal damage among users of digital mobile phones. Electromagn Biol Med. 2009 Jul 07;22(2-3):149–159. doi: 10.1081/jbc-120024624. [DOI] [Google Scholar]
- 41.Çam Semra Tepe, Seyhan N. Single-strand DNA breaks in human hair root cells exposed to mobile phone radiation. Int J Radiat Biol. 2012 May 13;88(5):420–4. doi: 10.3109/09553002.2012.666005. [DOI] [PubMed] [Google Scholar]
- 42.Lai WKC, Chiu YT, Law WS. The deformation and longitudinal excursion of median nerve during digits movement and wrist extension. Man Ther. 2014 Dec;19(6):608–13. doi: 10.1016/j.math.2014.06.005.S1356-689X(14)00123-4 [DOI] [PubMed] [Google Scholar]
- 43.Renuka DMRR, Saikumar P, Pradhosh Effect of excessive mobile phone text messaging on thumb muscle. Res J Pharm Biol Chem Sci. 2014;5(4):1363–1366. https://www.rjpbcs.com/pdf/2014_5(4)/[151].pdf . [Google Scholar]
- 44.Zeni O, Romanò M, Perrotta A, Lioi M, Barbieri R, d'Ambrosio G, Massa R, Scarfì M R. Evaluation of genotoxic effects in human peripheral blood leukocytes following an acute in vitro exposure to 900 MHz radiofrequency fields. Bioelectromagnetics. 2005 May 14;26(4):258–65. doi: 10.1002/bem.20078. [DOI] [PubMed] [Google Scholar]
- 45.Donmez B, Liu Z. Associations of distraction involvement and age with driver injury severities. J Safety Res. 2015 Feb;52:23–8. doi: 10.1016/j.jsr.2014.12.001.S0022-4375(14)00111-X [DOI] [PubMed] [Google Scholar]
- 46.Oxley J, Yuen J, Ravi MD, Hoareau Effie, Mohammed Mohammed Azman Aziz, Bakar Harun, Venkataraman Saraswathy, Nair Prame Kumar. Commuter motorcycle crashes in Malaysia: an understanding of contributing factors. Ann Adv Automot Med. 2013;57:45–54. http://europepmc.org/abstract/MED/24406945 . [PMC free article] [PubMed] [Google Scholar]
- 47.Vafaeenajar A, Khabbazkhoob M, Alidadisoltangholi H. Investigating the relative risk factors of injuries caused by accidents on roads in the Mashhad area in 2007. Iran Red Crescent Med J. 2011 Aug 1;13(8):530–536. https://archive.ircmj.com/article/13/8/74723-pdf.pdf . [PMC free article] [PubMed] [Google Scholar]
- 48.Mortazavi S, Parsanezhad Me, Kazempour M, Ghahramani P, Mortazavi Ar, Davari M. Male reproductive health under threat: Short term exposure to radiofrequency radiations emitted by common mobile jammers. J Hum Reprod Sci. 2013 Apr;6(2):124–8. doi: 10.4103/0974-1208.117178. http://www.jhrsonline.org/article.asp?issn=0974-1208;year=2013;volume=6;issue=2;spage=124;epage=128;aulast=Mortazavi .JHRS-6-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Redelmeier DA, Tibshirani RJ. Association between cellular-telephone calls and motor vehicle collisions. N Engl J Med. 1997 Feb 13;336(7):453–8. doi: 10.1056/NEJM199702133360701. [DOI] [PubMed] [Google Scholar]
- 50.Guo F, Kim I, Klauer SG. Semiparametric Bayesian models for evaluating time-variant driving risk factors using naturalistic driving data and case-crossover approach. Stat Med. 2019 Jan 30;38(2):160–174. doi: 10.1002/sim.7574. [DOI] [PubMed] [Google Scholar]
- 51.Hardell L, Mild K, Carlberg M. Further aspects on cellular and cordless telephones and brain tumours. Int J Oncol. 2003 Feb 01;:399–407. doi: 10.3892/ijo.22.2.399. [DOI] [PubMed] [Google Scholar]
- 52.Söderqvist Fredrik, Carlberg M, Hardell L. Mobile and cordless telephones, serum transthyretin and the blood-cerebrospinal fluid barrier: a cross-sectional study. Environ Health. 2009 Apr 21;8:19. doi: 10.1186/1476-069X-8-19. https://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-8-19 .1476-069X-8-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Söderqvist Fredrik, Carlberg M, Hardell L. Use of wireless telephones and serum S100B levels: a descriptive cross-sectional study among healthy Swedish adults aged 18-65 years. Sci Total Environ. 2009 Jan 01;407(2):798–805. doi: 10.1016/j.scitotenv.2008.09.051.S0048-9697(08)01014-0 [DOI] [PubMed] [Google Scholar]
- 54.Khadem-Rezaiyan M, Moallem SR, Vakili V. High-risk behaviors while driving: a population-based study from Iran. Traffic Inj Prev. 2017 Apr 03;18(3):257–261. doi: 10.1080/15389588.2016.1192612. [DOI] [PubMed] [Google Scholar]
- 55.Darvishi M, Noori M, Nazer MR, Sheikholeslami S, Karimi E. Investigating different dimensions of nomophobia among medical students: a cross-sectional study. Open Access Maced J Med Sci. 2019 Feb 28;7(4):573–578. doi: 10.3889/oamjms.2019.138. http://europepmc.org/abstract/MED/30894914 .OAMJMS-7-573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Asbridge M, Brubacher JR, Chan H. Cell phone use and traffic crash risk: a culpability analysis. Int J Epidemiol. 2013 Feb 18;42(1):259–67. doi: 10.1093/ije/dys180.dys180 [DOI] [PubMed] [Google Scholar]
- 57.da Silva DW, de Andrade Selma Maffei, Soares DFPDP, Mathias TADF, Matsuo T, de Souza RKT. Factors associated with road accidents among Brazilian motorcycle couriers. ScientificWorldJournal. 2012;2012:605480. doi: 10.1100/2012/605480. doi: 10.1100/2012/605480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Asefa NG, Ingale L, Shumey A, Yang H. Prevalence and factors associated with road traffic crash among taxi drivers in Mekelle town, northern Ethiopia, 2014: a cross sectional study. PLoS One. 2015 Mar 17;10(3):e0118675. doi: 10.1371/journal.pone.0118675. https://dx.plos.org/10.1371/journal.pone.0118675 .PONE-D-14-47340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fuller C, Lehman E, Hicks S, Novick MB. Bedtime use of technology and associated sleep problems in children. Glob Pediatr Health. 2017;4:2333794X17736972. doi: 10.1177/2333794X17736972. https://journals.sagepub.com/doi/10.1177/2333794X17736972?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2333794X17736972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abu Khadra KM, Khalil AM, Abu Samak M, Aljaberi A. Evaluation of selected biochemical parameters in the saliva of young males using mobile phones. Electromagn Biol Med. 2015 Mar 05;34(1):72–6. doi: 10.3109/15368378.2014.881370. [DOI] [PubMed] [Google Scholar]
- 61.Hardell L, Carlberg M. Use of mobile and cordless phones and survival of patients with glioma. Neuroepidemiology. 2013;40(2):101–8. doi: 10.1159/000341905.000341905 [DOI] [PubMed] [Google Scholar]
- 62.Mortazavi SMJ, Mortazavi SAR, Paknahad M. Association between exposure to smartphones and ocular health in adolescents. Ophthalmic Epidemiol. 2016 Dec 23;23(6):418–418. doi: 10.1080/09286586.2016.1212992. [DOI] [PubMed] [Google Scholar]
- 63.Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus. 2014 Feb 04;51(2):87–92. doi: 10.3928/01913913-20140128-01. [DOI] [PubMed] [Google Scholar]
- 64.Klauer SG, Guo F, Simons-Morton BG, Ouimet MC, Lee SE, Dingus TA. Distracted driving and risk of road crashes among novice and experienced drivers. N Engl J Med. 2014 Jan 02;370(1):54–59. doi: 10.1056/nejmsa1204142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ramya C, Vinutha S, Karthiyanee K. Effect of mobile phone usage on hearing threshold: a pilot study. Indian J Otol. 2011;17(4):159. doi: 10.4103/0971-7749.94494. [DOI] [Google Scholar]
- 66.Al-Jasser F, Mohamed A, Choudry A, Youssef R. Mobile phone use while driving and the risk of collision: a study among preparatory year students at King Saud University, Riyadh, Saudi Arabia. J Family Community Med. 2018;25(2):102–107. doi: 10.4103/jfcm.JFCM_139_17. http://www.jfcmonline.com/article.asp?issn=2230-8229;year=2018;volume=25;issue=2;spage=102;epage=107;aulast=Al%2DJasser .JFCM-25-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alghnam S, Towhari J, Alkelya M, Alsaif A, Alrowaily M, Alrabeeah F, Albabtain I. The association between mobile phone use and severe traffic injuries: a case-control study from Saudi Arabia. Int J Environ Res Public Health. 2019 Jul 29;16(15):2706. doi: 10.3390/ijerph16152706. https://www.mdpi.com/resolver?pii=ijerph16152706 .ijerph16152706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gariazzo C, Stafoggia M, Bruzzone S, Pelliccioni A, Forastiere F. Association between mobile phone traffic volume and road crash fatalities: a population-based case-crossover study. Accid Anal Prev. 2018 Jun;115:25–33. doi: 10.1016/j.aap.2018.03.008.S0001-4575(18)30112-X [DOI] [PubMed] [Google Scholar]
- 69.Dingus TA, Guo F, Lee S, Antin JF, Perez M, Buchanan-King M, Hankey J. Driver crash risk factors and prevalence evaluation using naturalistic driving data. Proc Natl Acad Sci U S A. 2016 Mar 08;113(10):2636–2641. doi: 10.1073/pnas.1513271113. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=26903657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gicquel L, Ordonneau P, Blot E, Toillon C, Ingrand P, Romo L. Description of various factors contributing to traffic accidents in youth and measures proposed to alleviate recurrence. Front Psychiatry. 2017 Jun 01;8:94. doi: 10.3389/fpsyt.2017.00094. doi: 10.3389/fpsyt.2017.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Young R. Removing biases from crash odds ratio estimates of secondary tasks: a new analysis of the SHRP 2 naturalistic driving study data. SAE Technical Paper Series; WCX™ 17: SAE World Congress Experience; April 4-6; Detroit, Michigan. 2017. [DOI] [Google Scholar]
- 72.Scott-Parker Bridie, Oviedo-Trespalacios Oscar. Young driver risky behaviour and predictors of crash risk in Australia, New Zealand and Colombia: same but different? Accid Anal Prev. 2017 Feb;99(Pt A):30–38. doi: 10.1016/j.aap.2016.11.001.S0001-4575(16)30393-1 [DOI] [PubMed] [Google Scholar]
- 73.Huemer AK, Schumacher M, Mennecke M, Vollrath M. Systematic review of observational studies on secondary task engagement while driving. Accid Anal Prev. 2018 Oct;119:225–236. doi: 10.1016/j.aap.2018.07.017.S0001-4575(18)30317-8 [DOI] [PubMed] [Google Scholar]
- 74.Carcaillon LI, Salmi LR, Atout-Route Evaluation Group Evaluation of a program to reduce motor-vehicle collisions among young adults in the county of Landes, France. Accid Anal Prev. 2005 Nov;37(6):1049–55. doi: 10.1016/j.aap.2005.06.003.S0001-4575(05)00099-0 [DOI] [PubMed] [Google Scholar]
- 75.Olsson Bjørn, Pütz Hannah, Reitzug Fabian, Humphreys David K. Evaluating the impact of penalising the use of mobile phones while driving on road traffic fatalities, serious injuries and mobile phone use: a systematic review. Inj Prev. 2020 Aug;26(4):378–385. doi: 10.1136/injuryprev-2019-043619.injuryprev-2019-043619 [DOI] [PubMed] [Google Scholar]
- 76.IARC classifies radiofrequency electromagnetic fields as possibly carcinogenic to humans. International Agency for Research on Cancer. [2021-09-13]. http://www.iarc.fr/en/media-centre/pr/2011/pdfs/pr208_E.pdf .
- 77.Narayanan Sareesh Naduvil, Jetti Raghu, Kesari Kavindra Kumar, Kumar Raju Suresh, Nayak Satheesha B, Bhat P Gopalakrishna. Radiofrequency electromagnetic radiation-induced behavioral changes and their possible basis. Environ Sci Pollut Res Int. 2019 Oct;26(30):30693–30710. doi: 10.1007/s11356-019-06278-5.10.1007/s11356-019-06278-5 [DOI] [PubMed] [Google Scholar]
- 78.Kesari Kavindra Kumar, Siddiqui Mohd Haris, Meena Ramovatar, Verma H N, Kumar Shivendra. Cell phone radiation exposure on brain and associated biological systems. Indian J Exp Biol. 2013 Mar;51(3):187–200. [PubMed] [Google Scholar]
- 79.Prasad M, Kathuria P, Nair P, Kumar Amit, Prasad Kameshwar. Mobile phone use and risk of brain tumours: a systematic review of association between study quality, source of funding, and research outcomes. Neurol Sci. 2017 May;38(5):797–810. doi: 10.1007/s10072-017-2850-8.10.1007/s10072-017-2850-8 [DOI] [PubMed] [Google Scholar]
- 80.Yang M, Guo W, Yang C, Tang J, Huang Q, Feng S, Jiang A, Xu X, Jiang G. Mobile phone use and glioma risk: a systematic review and meta-analysis. PLoS One. 2017 May 4;12(5):e0175136. doi: 10.1371/journal.pone.0175136. https://dx.plos.org/10.1371/journal.pone.0175136 .PONE-D-16-41709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hardell L, Carlberg M. Mobile phones, cordless phones and rates of brain tumors in different age groups in the Swedish National Inpatient Register and the Swedish Cancer Register during 1998-2015. PLoS One. 2017 Oct 4;12(10):e0185461. doi: 10.1371/journal.pone.0185461. https://dx.plos.org/10.1371/journal.pone.0185461 .PONE-D-17-18222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Little MP, Rajaraman P, Curtis RE, Devesa SS, Inskip PD, Check DP, Linet MS. Mobile phone use and glioma risk: comparison of epidemiological study results with incidence trends in the United States. BMJ. 2012 Mar 08;344:e1147. doi: 10.1136/bmj.e1147. http://europepmc.org/abstract/MED/22403263 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee S, Kang H, Shin G. Head flexion angle while using a smartphone. Ergonomics. 2015 Oct 17;58(2):220–6. doi: 10.1080/00140139.2014.967311. [DOI] [PubMed] [Google Scholar]
- 84.Xie YF, Szeto G, Madeleine P, Tsang S. Spinal kinematics during smartphone texting - a comparison between young adults with and without chronic neck-shoulder pain. Appl Ergon. 2018 Apr;68:160–168. doi: 10.1016/j.apergo.2017.10.018.S0003-6870(17)30245-4 [DOI] [PubMed] [Google Scholar]
- 85.Kim S, Koo S. Effect of duration of smartphone use on muscle fatigue and pain caused by forward head posture in adults. J Phys Ther Sci. 2016 Jun;28(6):1669–72. doi: 10.1589/jpts.28.1669. http://europepmc.org/abstract/MED/27390391 .jpts-2015-926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014 Nov;25:277–279. [PubMed] [Google Scholar]
- 87.Sangwaiya A, Sharma J, Kaira V, Ratan K, Sen R, Gupta V. Burkitt′s lymphoma masquerading as intestinal obstruction: An uncommon entity with variable clinical presentation. Clin Cancer Investig J. 2014;3(5):441. doi: 10.4103/2278-0513.138090. [DOI] [Google Scholar]
- 88.Mireku MO, Barker MM, Mutz J, Dumontheil I, Thomas MS, Röösli Martin, Elliott P, Toledano MB. Night-time screen-based media device use and adolescents' sleep and health-related quality of life. Environ Int. 2019 Mar;124:66–78. doi: 10.1016/j.envint.2018.11.069. https://linkinghub.elsevier.com/retrieve/pii/S0160-4120(18)31241-8 .S0160-4120(18)31241-8 [DOI] [PubMed] [Google Scholar]
- 89.Gulati Sachin, Kosik Pavol, Durdik Matus, Skorvaga Milan, Jakl Lukas, Markova Eva, Belyaev Igor. Effects of different mobile phone UMTS signals on DNA, apoptosis and oxidative stress in human lymphocytes. Environ Pollut. 2020 Dec;267:115632. doi: 10.1016/j.envpol.2020.115632.S0269-7491(20)36320-X [DOI] [PubMed] [Google Scholar]
- 90.Panagopoulos DJ, Karabarbounis A, Yakymenko I, Chrousos GP. Human‑made electromagnetic fields: Ion forced‑oscillation and voltage‑gated ion channel dysfunction, oxidative stress and DNA damage (Review) Int J Oncol. 2021 Nov;59(5):92. doi: 10.3892/ijo.2021.5272. http://europepmc.org/abstract/MED/34617575 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dasdag S, Akdag MZ. The link between radiofrequencies emitted from wireless technologies and oxidative stress. J Chem Neuroanat. 2016 Sep;75(Pt B):85–93. doi: 10.1016/j.jchemneu.2015.09.001.S0891-0618(15)00069-1 [DOI] [PubMed] [Google Scholar]
- 92.Röösli Martin, Lagorio S, Schoemaker MJ, Schüz Joachim, Feychting M. Brain and salivary gland tumors and mobile phone use: evaluating the evidence from various epidemiological study designs. Annu Rev Public Health. 2019 Apr 01;40(1):221–238. doi: 10.1146/annurev-publhealth-040218-044037. [DOI] [PubMed] [Google Scholar]
- 93.Smeds H, Wales J, Mathiesen T, Talbäck Mats, Feychting M. Occurrence of primary brain tumors in cochlear implant patients in Sweden between 1989 and 2014. Clin Epidemiol. 2018;10:1401–1405. doi: 10.2147/CLEP.S164556. doi: 10.2147/CLEP.S164556.clep-10-1401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jain MJ, Mavani KJ. A comprehensive study of worldwide selfie-related accidental mortality: a growing problem of the modern society. Int J Inj Contr Saf Promot. 2017 Dec 14;24(4):544–549. doi: 10.1080/17457300.2016.1278240. [DOI] [PubMed] [Google Scholar]
- 95.Dokur M, Petekkaya E, Karadağ M. Media-based clinical research on selfie-related injuries and deaths. Ulus Travma Acil Cerrahi Derg. 2018 Mar;24(2):129–135. doi: 10.5505/tjtes.2017.83103. http://www.journalagent.com/pubmed/linkout.asp?ISSN=1306-696X&PMID=29569684 . [DOI] [PubMed] [Google Scholar]
- 96.Amernik K, Kabacińska A, Tarnowska C, Paradowska-Opałka B. Ostry uraz akustyczny i termiczny ucha spowodowany awarią telefonu komórkowego. Otolaryngologia Polska. 2007 Jan;61(4):484–486. doi: 10.1016/S0030-6657(07)70466-3. [DOI] [PubMed] [Google Scholar]
- 97.Görgülü Tahsin, Torun M, Olgun A. A cause of severe thigh injury: battery explosion. Ann Med Surg (Lond) 2016 Feb;5:49–51. doi: 10.1016/j.amsu.2015.12.048. https://linkinghub.elsevier.com/retrieve/pii/S2049-0801(15)00180-6 .S2049-0801(15)00180-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cherubino M, Pellegatta I, Sallam D, Pulerà E, Valdatta L. Enzymatic debridement after mobile phone explosion: a case report. Ann Burns Fire Disasters. 2016 Dec 31;29(4):273–275. http://europepmc.org/abstract/MED/28289361 . [PMC free article] [PubMed] [Google Scholar]
- 99.Bouji M, Lecomte A, Gamez C, Blazy K, Villégier A. Impact of cerebral radiofrequency exposures on oxidative stress and corticosterone in a rat model of Alzheimer’s Disease. J Alzheimers Dis. 2020 Jan 21;73(2):467–476. doi: 10.3233/jad-190593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Literature search strategy, basic characteristics of studies, quality assessment, and publication bias test.


