Abstract
Background.
A major challenge in clinical research today is the difficulty studies have meeting recruitment goals. Up to 48% of studies do not meet accrual goals within the specified timeframe, significantly delaying the progress of projects and the dissemination of findings. This pervasive problem is a recruitment crisis. We developed a representative, ethnically and racially diverse research participant registry in a predominantly rural state with high levels of health care disparities and minority populations. We sought input at each step of development from members of community advisory boards (CABs) across Arkansas. We report how community involvement in the development of the registry was implemented.
Methods.
Members of CABs were partners in developing all aspects of the registry website, including the name, content, appearance, educational messages and testimonials used. Constructs from the Health Belief Model informed the educational messages and supported the intense multimedia campaign used to launch and promote ongoing registrations. Using CAB guidance, community events were held throughout the state of Arkansas at venues with diverse racial and ethnic attendance.
Results.
From April 1, 2016 to September 1, 2017, 4,002 people registered statewide who match the demographic profile of Arkansas.
Conclusion.
CAB involvement in the registry, multiple cues to action, and face-to-face contact with diverse lay audiences throughout the state were key components of the successful registry launch.
Introduction
Recruitment Trends and Challenges
A universal challenge in clinical and biobehavioral research today is the inability to identify a sufficient number of diverse research volunteers who meet study inclusion criteria. Up to 48% of protocols fail to meet enrollment targets and 11% fail to enroll a single patient. In addition, most protocols require twice the amount of time to meet recruitment goals than originally planned for the study (Tufts University, 2013). This problem increases the cost of research and delays the uptake of new research findings that can improve human health.
Focus group supported research (Hennink-Kaminski, Willoughby, & McMahan, 2014) has identified primary barriers to research participation: (1) lack of understanding and knowledge about research and (2) mistrust and suspicion of research. Among 12,000 Americans surveyed, 82% acknowledged the importance of clinical and biobehavioral research, but only 30% described themselves as very informed about research, and 25% reported being very confident in knowing how to find or identify appropriate studies (Center for Information and Study on Clinical Research Participation [CISCRP], 2015). In the same study, 44% of responders reported they would be ‘very willing’ to participate in a clinical and biobehavioral research study, while 60% reported that research was ‘never’ or ‘not very often’ considered when discussing treatment options with their physician.
Exposure to information about clinical and biobehavioral research and other medical topics is often limited to media outlets reporting on sensationalized cases (Feeley, O’Mally, & Covert, 2016), which may lead to fear and mistrust about participating in research studies. This lack of trust can be especially prevalent in minority populations due to well-publicized, unethical studies, such as the United States Public Health Service Syphilis Study at Tuskegee (Centers for Disease Control and Prevention [CDC], 2015) and the case of Henrietta Lacks (Skloot, 2010). In a report on public perceptions of clinical research studies, in which 12,009 participants completed a survey and reported concern about potential health risks associated with being in a study, 38% percent expressed concern that research volunteers were test cases and 35% felt they gambled with their health if they participated in studies (CISCRP, 2015). Over 60% of 2,400 African Americans and Latinos survey reported that they felt pressured into participation (Garza et al., 2017). New strategies are needed to overcome this negative bias so that research findings will be applicable to all races and ethnic groups.
The development of research registries that effectively link potential participants with research studies addresses two significant recruitment issues: (1) assistance in meeting accrual goals, and (2) finding people who are willing to participate in research. Vanderbilt University developed a user-friendly electronic registry that allows the public to enter personal information and research areas of interest (Harris, Lane, & Biaggioni, 2005). Information about this registry was mailed to over 14,000 individuals associated with either the University or Medical Center. In response, over 800 people self-entered information within a two-week period and over 2,900 enrolled over the first 32 months. Institutional researchers found the registry to be time-saving.
Our state is largely rural, making education and recruitment challenging. Approximately 44% of the state’s population live in non-metropolitan areas, and 38 of the state’s 75 counties are considered rural (having populations of less than 20,000 people) and underserved (University of Arkansas Division of Agriculture Research and Extension, 2012). The state also has a higher African American population than the national average (15.7% versus 12.3%) and a fast-growing Hispanic population (United States Census Bureau, 2016; Infoplease, 2017). Reaching both rural and minority populations was therefore critical to developing a representative, ethnically and racially diverse research participant registry. We determined involvement of community members was essential to educate the public on the importance of medical research. Accordingly, we formulated two goals: (1) state-wide education of the public on the importance of clinical and biobehavioral research, and (2) state-wide recruitment representative of the demographics of our state. We report how community involvement in the development of the registry and multiple cues to action were implemented.
Methods
Planning and Community Involvement
Consultation with other CTSA sites informed the design of our registry. To prioritize community involvement, we met with existing university-affiliated community-based advisory boards (CABs) and patient groups to advise us on what they did and did not understand about research and sought input on how we could better educate the citizens of our primarily rural state. Based on the feedback we received, we prioritized education on the importance of participation in clinical and biobehavioral research, education on types of research, and development of trust between individuals and UAMS researchers. This collaborative process encompassed many cycles as we gathered and clarified information, developed materials based on this information, presented it to the CABs for feedback, and started the cycle once again. In addition, the CABs advised us on all aspects of content and design of the registry (color, text, images, and testimonials) and selected the name of the registry, ARresearch.org.
Developing Educational Content
The Health Belief Model (Green & Murphy, 2014; Hayden, 2014) is a well-accepted model used to support health education. The major constructs of perceived susceptibility, perceived benefits, barriers, and cues to action provided the foundation for our approach to development of the registry. The registry website features answers to four primary questions with subpages designed to educate the public about research: (1) What is the registry? (2) Why should I join the registry? (3) What happens when I join the registry? and (4) What kind of research needs volunteers like me? (Figure 1). The CABs assisted with selecting testimonial videos featuring former research participants talking about their experiences at UAMS (University of Arkansas for Medical Sciences) and the importance of research to the community. The testimonials addressed the perceived benefits of participating in research and included personal and/or family member considerations of adverse susceptibility. These videos, designed to help overcome mistrust, present ordinary, relatable people speaking about their positive experiences with research at UAMS. The CABs also helped select choices of health/disease categories for inclusion in the registry, as well as the multiple cues to action to launch and sustain enrollment in the registry.
Figure 1.
Registry landing page. Four educational questions serve as the main menu. Early versions using stock photo images were replaced with photos of state residents at the recommendation of the CABs. Arkansas, 2017.
Collaboration with experts at the UAMS Center for Health Literacy ensured that registry website content and promotional materials were understandable to a wide variety of people. A Spanish language version was also developed, as Arkansas has a growing Hispanic population.
Designing the Registry for Use
The website was designed to be user-friendly and accessible on smart phones, tablets, and computers to decrease barriers to research participation. Potential registrants are directed to a simple online registration form that collects demographics, preferred mode of contact, and disease-focused, broadly-worded areas of interest (e.g., aging, cancer, mental health, etc.), including a healthy volunteer option. The list of conditions was expanded to address diseases identified by registrants and researchers; for example, ‘allergies’ and ‘injury prevention/safety’. Registrants may select more than one areas of interest and may specify additional health interests by selecting ‘other’ and typing in their own answers, which assisted us in expanding the original list. Registrant information is maintained in a secure data set within the Arkansas Comprehensive Research Informatics Suite (AR-CRIS).
Launch and Media Promotion
After the planning and development phase, we launched our website and initiated an aggressive multimedia marketing campaign (i.e., cues to action) that included TV, radio and social media targeted to the public, UAMS patients, and to health system employees. Our public campaign included television and radio segments such as news stories and interviews. Institutional resources supported the airing of registry advertisements through public service announcements that were broadcasted on a variety of stations throughout Arkansas. Our interviews featured researchers from UAMS, past research participants, and CAB members. We sought to promote stories that highlighted the positive benefits and experiences of clinical and biobehavioral research at UAMS. Broadcast interviews were also promoted through social media. Additional marketing included printed flyers and brochures, tabletop tents placed across the UAMS campus and clinics, and patient mailings, all designed with and approved by our CABs and health literacy group.
Promotion to UAMS Patients and Employees
We worked with clinical partners to provide a link to registry information from UAMS MyChart, an online patient records management feature of our electronic health record system. This link invites users to learn more about the registry and sign up. Additionally, along with our public marketing, we launched an aggressive marketing campaign to UAMS employees via emails, in person at meetings, and through video endorsement and demonstration by the Chancellor. Since UAMS employs over 10,000 Arkansans, we reasoned that employee knowledge and interest in the registry could ultimately help us attract future registrants among their families, friends, and acquaintances. Most recently, we developed an advertisement insert which we include in the approximately 13,000 appointment reminders mailed by UAMS monthly.
Launching Community Registration
To reach a broad segment of the population, we attended numerous community events such as the Arkansas State Fair, semi-professional baseball games, college basketball games, local health fairs, Arkansas State Minority Health Commission community events, and local gatherings recommend by our CAB members. These face-to-face events decreased barriers to registration and provided education on how research participation could benefit others and potentially decrease susceptibility of specific individuals. For example, many African Americans gave family histories of hypertension and stroke. We used the construct of perceived susceptibility to educate potential registrants about the benefits of participation (e.g., to elucidate race or gene-related variability in drug response).
We continue to add community venues across the state recommended by CAB members and those identified by TRI (Translational Research Institute) staff. When we appear at community events, we display a banner and large sign promoting the registry at our booth and staff wear T-shirts that display our logo. We have also held special promotions to boost enrollment, such as entering each new registrant into a drawing for a $50 gift card, to assist us in achieving an enrollment goal; for example, reaching the 3,000 registrants mark.
At community events, we provide easy-to-use access to the registry through iPads connected to Wi-Fi. Registrants are provided with an iPad open to the registration page so they may personally enter their information, or TRI staff provide assistance entering the information. The registry link may also be accessed and information entered on personal smart phones in less than five minutes. Paper forms are available for those who do not feel comfortable using an iPad and for use during Internet or power outages. Any completed paper forms are entered into the electronic registry by TRI staff after the event. Each of these measures has decreased barriers to registration. The feasibility of registration during community events (e.g., sporting events) is particularly important.
Evaluation of Community Events
We gauge the success of each recruiting event (sporting event, state fair, community event, etc.) by information provided by the registrants on how they learned about the registry. Reports of zip code, age, gender, race/ethnicity, and health areas of interest guide our efforts to plan future targeted enrollment strategies.
Ongoing Communication
We are currently developing an easy method for registrants to access and make changes to their own record, such as updating contact information and preferred method of communication, and adding or removing diagnoses/health interests. Currently, registrants must reregister, necessitating eliminating duplicate entries and combining this data into a single updated entry. Future efforts will involve automatic email birthday greetings and twice-yearly informational messages.
Results
Over the course of 18 months since the launch of the ARresearch.org, 4,002 people registered as potential clinical and biobehavioral research participants. In the first 12 months, the site logged over 22,000 visits. The most frequently visited area on the site was the question, ‘What kind of research needs volunteers like me?’ This question is answered by testimonials of previous research participants and supports the use of the Health Belief Model as a construct to communicate the perceived benefit of participation in research.
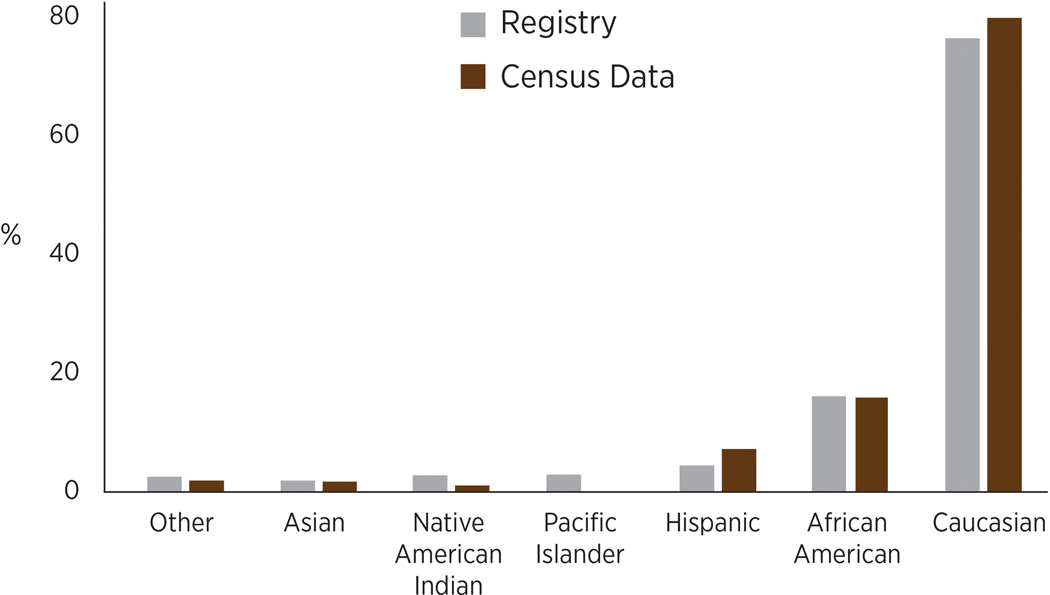
The races and ethnicities identified by registrants are representative of the 2016 demographics of Arkansas (Figure 2). We recruited people from every county in the state and enrolled adults in all age groups. Based on 3,960 registrants (42 have some error in the birthday entry), 44% (n=1750) are 18–44, 43% (n=1717) are 45–65, and 12% (n=493) are 66 years of age or older. To increase the pool of registrants above age 65, we will seek future venues that have a high attendance of older adults.
Figure 2.
Ethnicity and race distribution of registry and state census data. The registry has slightly more African Americans (16.1 versus 15.4%, respectively); Native Americans (2.8 versus 1.0%), and Pacific Islanders (2.9 versus 0.3%) than the state population. However, Hispanics/Latinos are underrepresented in the registry compared to state data (7.2 versus 4.6%). Arkansas, 2017.
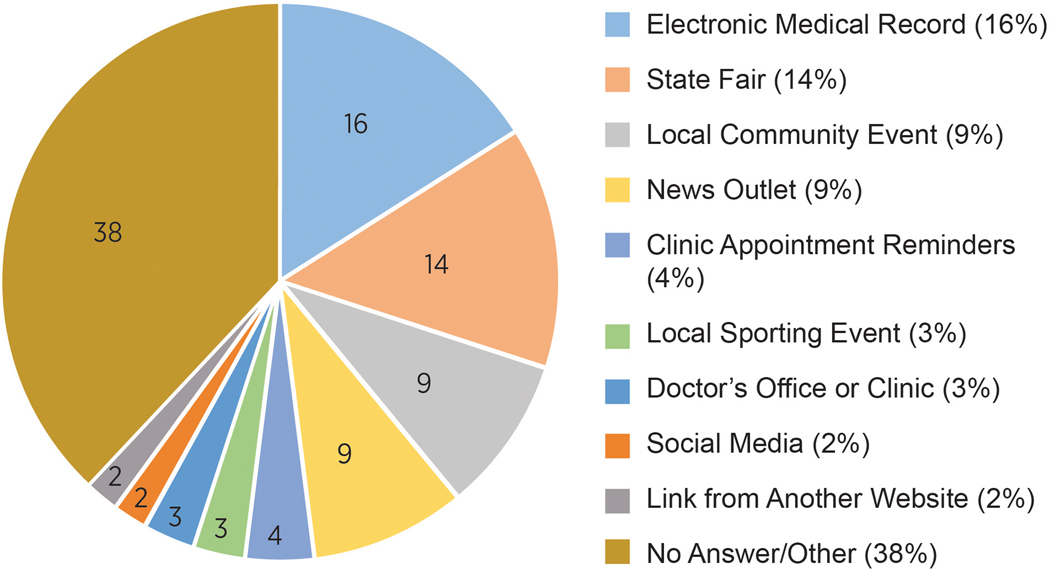
Recruitment Method Analysis
During the registration process registrants were asked to indicate how they heard of the registry (Figure 3). As we added community events, we updated this list in the registry. UAMS MyChart (the electronic link from the electronic health record) and the state fair were the two most successful recruitment approaches (Figure 3). Combined, these venues recruited 1,215 (30.4%) registrants. Other community events accounted for 9% of total registrants. Social media, which we emphasized early in the launch, had minimal success with only 89 (2.2%) registrants reporting this recruitment venue. ‘Other venue’ was selected by 1,033 (25.8%) and 502 (12.5%) did not answer this question, representing a combined 1,535 (38.3%). As a result of these findings, we have also added electronic links to the registry to university hospital clinic appointment reminder emails and to the ‘My Chart’ component of our institution’s Epic electronic health record system. The links serve as cues to action.
Figure 3.
How registrants heard of the registry. Arkansas, 2017.
Health Interests
The vast majority of registrants select more than one condition as a health interest (Table 1), with the exception of those selecting ‘healthy volunteer,’ who most often select just one topic. The most frequently selected areas of interest were weight management (2,000, 50%), mental health (1,648, 41%), healthy volunteer (1,521, 38%), heart disease (1,494, 37%), and sleep disorders (1453, 36%).
Table 1.
Distribution of health interests by registrants. Arkansas, April 1 – September 1, 2017.
| Health Category | Percentage | No. of Participants |
|---|---|---|
| Weight Management | 49.9 | 2000 |
| Mental Health | 41.1 | 1648 |
| Healthy Volunteer | 38.0 | 1521 |
| Heart Disease | 37.3 | 1494 |
| Sleep Disorders | 36.3 | 1453 |
| Women’s Health | 35.5 | 1421 |
| Neurology | 31.7 | 1270 |
| Endocrinology | 29.1 | 1168 |
| Dental Health | 28.2 | 1129 |
| Digestion | 26.3 | 1055 |
| Allergy | 25.6 | 1026 |
| Cancer | 23.4 | 937 |
| Breathing | 22.3 | 896 |
| Physical Medicine | 21.5 | 863 |
| Rheumatology/Autoimmune | 20.5 | 823 |
| Aging | 20.4 | 817 |
| Orthopedics | 18.7 | 751 |
| Substance Abuse | 14.8 | 596 |
| Men’s Health | 12.5 | 501 |
| Other | 12.1 | 488 |
| Infectious Disease | 12.1 | 487 |
| Blood Disorders | 11.4 | 457 |
| Infant/Children’s | 10.8 | 433 |
| Kidney | 10.6 | 427 |
| Liver | 9.4 | 379 |
| Chronic Pain | 9.0 | 361 |
| Vision | 6.4 | 258 |
| Injury Prevention | 6.1 | 245 |
| Skin Disorders | 5.8 | 235 |
Discussion
The development and launch of the registry website illustrate the successful integration of numerous functions across the TRI, our successful partnership with the community, and the strong support of our institution. We viewed a lay-friendly website as an important research recruitment approach as healthcare information is actively sought by 80% of Internet users (Fox & Fallows, 2003), including 84% of adults aged 50–64 and 64% of those over 65 (Pew Research Center, 2017). Further, national data demonstrate the widespread usage of the Internet by all races and ethnic groups (Pew Research Center, 2017), making it an essential tool for engaging research participants.
Involving Community Members in Planning and Recruitment
We believe the success of the ARresearch.org registry website is due in large part to the initial and ongoing involvement of the CABs. Their feedback was instrumental in building an informative and inviting website. Specifically, the CABs’ feedback on the messages and images we incorporated into the registry was invaluable. The CABs often provided constructive feedback which led to significant changes to the site that we believe helped communicate our message more effectively. The CABs, along with the literature, recommended including the educational component and the testimonials by former and current research participants, which has been an important feature of our site, as demonstrated by the number of ‘hits’ in this section. This approach aligns with the constructs of the Health Belief Model.
CAB members have also been instrumental in our success with ongoing promotion, especially with events in rural areas and those focused on minority populations. They helped us identify key community events for our recruitment efforts, and often participated in recruiting events themselves. Over the past year, we have realized that one of our biggest challenges is simply being aware of the myriad community events across the state.
Distrust of medical research is common in the African American community (Skloot, 2010; CISCRP, 2015). Our success recruiting in African American and Hispanic communities may be due to staffing our website recruitment events with African American and Hispanic TRI staff and the visible endorsement of community leaders. These approaches are not only applicable to targeting different racial demographics, but can also be applied to recruiting in rural and suburban areas. As we continue to reach out to rural communities, we will continue to involve more community representatives who help deliver the message of perceived benefit to research participation.
Recruitment Method Successes
As previously mentioned, the link from patients’ online health record has been our strongest recruiting method. One possible reason is that the online health record, by its nature, is a tool used by patients who are engaged with their health and healthcare services. As individuals access their record, they receive a cue to action, and the direct link eliminates the barrier of searching for the website. Thus, advertising a registry here and providing a link to a website for further information is more likely to be successful.
We have learned that our institute’s display at community events generally attracts those interested in health or who recognize the UAMS name. Additionally, assurance that, first, registration does not mean one is volunteering for a particular study, but instead simply agreeing to be contacted, and second, that the registrant maintains total freedom to consent for research participation, and can be removed from the registry at any time via email or telephone, has been extremely important. Another effective message to communicate is that the registration process is quick and easy, taking less than five minutes. We learned that recruitment staff need to be efficient when operating the iPads to save time, especially in recruiting potential participants eager to attend the fair or sporting event. We have not evaluated whether certain of these messages or techniques are more important than others to induce people to register; however, experience indicates they are all important and may vary by individual. We recommend incorporating each of these messages.
Media Saturation
There is evidence to suggest our initial media saturation campaign cue to action did drive significant attention to both the registry website and the registry. During the first month of the website launch, site hits totaled over 5,700, comprising 25% of all of that year’s page views. Additionally, while overall recruitment through public service announcements, news stories and social media did not gather large numbers of registrants, they increased general awareness of the registry. We continue to use these approaches to continuously raise and maintain the registry’s public profile.
Health Interests
The most frequently selected areas of interest reflect the health issues common in Arkansas. In 2017, Arkansans were identified as the third most obese in the United States (Trust for America’s Health, 2017). Moreover, Arkansas ranks fourth in heart disease mortality and third in stroke mortality in the United States (CDC, 2017). These selections provide UAMS researchers with information about community interests, and may have implications for feasibility assessments for future research studies. Researchers in these more prevalent fields can also cite the registry numbers in funding applications as evidence that recruitment is likely to be more successful at UAMS because of the pool of potential volunteers in the registry. In the long-term, decision-makers at UAMS can use trends in these data to guide research priorities, making them more responsive to community needs and interests.
Conclusions
Our experiences promoting the registry provide four main insights into promotion. First, involving CABs and representatives of communities across the state as early in the process as possible and keeping them engaged in the process is essential to success, achieved by promoting the benefits of participation and overcoming barriers. Second, educating potential registrants with clear, concise messages is important. In our primarily rural state, the use of health literacy appropriate materials is extremely important. Third, utilizing an aggressive initial approach with multiple cues to acquaint the public with the registry, followed by a sustained campaign which prioritizes going out into communities to educate and recruit has been successful. Further, attendance at multiple community events ensured that the demographics of registry participants matched those of state residents. Finally, designing a registry form that is easy to complete within five minutes on a smart phone or tablet is essential to decreasing a major barrier—time to complete enrollment.
Our goal is to allow registrants to self-identify what areas of clinical and biobehavioral research is important to them, thereby making the research-volunteer matching process more efficient. The registry will provide a service to researchers to reduce research accrual times, and make registrants less likely to be contacted to participate in studies that do not interest them. Knowledge of registrants’ health interests is also of value because it reflects the perspectives of diverse individuals across the state, information which can be used to prioritize future research endeavors at UAMS.
Acknowledgements
Funding/Support: The project described was supported by the Translational Research Institute (TRI), grant 1U54TR001629–01A1 through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Jean C. McSweeney, College of Nursing; Translational Research Institute, University of Arkansas for Medical Sciences.
Beatrice Boateng, Translational Research Institute; Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences.
Laura James, Translational Research Institute; Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences.
Pearl Anna McElfish, Office of Community Health and Research, University of Arkansas for Medical Sciences, Fayetteville, Arkansas; College of Medicine, University of Arkansas for Medical Sciences, Fayetteville, Arkansas.
David Robinson, Translational Research Institute, University of Arkansas for Medical Sciences.
Sandra E. Hatley, Translational Research Institute, University of Arkansas for Medical Sciences.
Pamela Christie, Translational Research Institute, University of Arkansas for Medical Sciences.
Nia Indelicato, Translational Research Institute, University of Arkansas for Medical Sciences.
References
- Centers for Disease Control and Prevention. (2015). U.S. Public Health Service syphilis study at Tuskegee: The Tuskegee timeline. Retrieved from https://www.cdc.gov/tuskegee/timeline.htm
- Centers for Disease Control and Prevention, National Center for Health Statistics. (2017). Stats of the State of Arkansas. Retrieved from https://www.cdc.gov/nchs/pressroom/states/arkansas/arkansas.htm
- Center for Information and Study on Clinical Research Participation. (2015). 2015 Perceptions and insights study: Public perceptions. Retrieved from https://www.ciscrp.org/services/research-services/public-and-patient-perceptions-insights-study/
- Feeley TH, O’Mally AK, & Covert JM (2016). A content analysis of organ donation stories printed in U.S. newspapers: Application of newsworthiness. Health Communication. 31(4), 495–503. doi: 10.1080/10410236.2014.973549 [DOI] [PubMed] [Google Scholar]
- Fox S, and Fallows D. (2003). Pew Internet and American life project, Internet health resources: health searches and email have become more commonplace, but there is room for improvement in searches and overall Internet access. Retrieved from http://www.pewinternet.org/files/old-media/Files/Reports/2003/PIP_Health_Report_July_2003.pdf.pdf [Google Scholar]
- Garza MA, Quinn SC, Li Y, Assini-Meytin L, Casper ET, Fryer CS,…Thomas SB (2017). The influence of race and ethnicity on becoming a human subject: Factors associated with participation in research. Contemporary Clinical Trials Communications, 7, 57–63. doi: 10.1016/j.conctc.2017.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green EC and Murphy E. (2014). Health belief model. The Wiley Blackwell encyclopedia of health, illness, behavior, and society. 766–769. doi: 10.1002/9781118410868.wbehibs410 [DOI] [Google Scholar]
- Harris PA, Lane L, & Biaggioni I. (2005). Clinical research subject recruitment: the Volunteer for Vanderbilt Research Program www.volunteer.mc.vanderbilt.edu. Journal of the American Medical Informatics Association, 12(6), 608–613. doi: 10.1197/jamia.M1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden J. (2014). Health belief model. Introduction to health behavior theory, second edition. Jones and Bartlett Learning. [Google Scholar]
- Hennink-Kaminski HJ, Willoughby JF, & McMahan D. (2014). Join the conquest: Developing a campaign to increase participation in clinical research in North Carolina. Science Communication, 36(1), 30–55. doi: 10.1177/1075547013492434 [DOI] [Google Scholar]
- Infoplease.com. (2017). Population of the United States by Race and Hispanic/Latino origin, Census 2000 and 2010. Retrieved from https://www.infoplease.com/us/race-population/population-united-states-race-and-hispaniclatino-origin-census-2000-and-2010
- Pew Research Center. (2017). Internet/Broadband fact sheet. Retrieved from http://www.pewinternet.org/fact-sheet/internet-broadband/
- Skloot R. (2010). Henrietta Lacks: A donor’s immortal legacy. [National Public Radio; ]. Retrieved from http://www.npr.org/2010/02/02/123232331/henrietta-lacks-a-donors-immortal-legacy. [Google Scholar]
- Trust for America’s Health, & Robert Wood Johnson Foundation. (2017). The state of obesity: Better policies for a healthier America. Adult obesity in the United States. Retrieved from http://www.stateofobesity.org/adult-obesity/ [Google Scholar]
- Tufts University. (2013, Jan/Feb). Impact report - Analysis and insight into critical drug development issues. Available from http://csdd.tufts.edu/news/complete_story/pr_ir_jan-feb_2013
- University of Arkansas Division of Agriculture Research and Extension. (2015). Rural profile of Arkansas. Retrieved from https://www.uaex.edu/publications/pdf/MP-531.pdf