Abstract
Background and purpose
Patient-reported outcomes (PROMs) after primary total hip arthroplasty (THA) and revision THA are important information in the preoperative shared decision-making process. We present 1-year results on pain, function, and quality of life following primary and revision THA.
Patients and methods
From 2010 to 2018, 3,559 primary THA and 406 revision THAs were included in our institutional quality registry. PROMs were registered preoperatively, 3 months, and 1 year after surgery, numeric rating scale (0–10) for pain during mobilization and at rest, health-related quality of life (EQ-5D), and a hip-specific physical function score (HOOS-PS). 2 anchor questions were asked 1 year after surgery concerning joint function and willingness to go through surgery again.
Results
There were statistically significant improvements in all PROMs at the 3-month follow-up in both groups. All PROMs improved more in the primary group relative to the revision group. 1 year after surgery, pain during mobilization was reduced with a mean change of 5.1 (SD 2.6) for primary THA and 2.9 (SD 3.0) for revision THA. 93% of primary THA patients reported both better function 1 year after surgery and that they would have gone through surgery again, compared with 78% and 79% in the revision THA group.
Interpretation
Primary THA patients reported better function and more pain relief than the revision THA group 1 year after surgery. Pain during mobilization shows the most marked improvement in both groups, which is important preoperative information for patients.
Reporting only implant survival outcome does not necessarily give the full picture of the result of arthroplasty surgery, as patients with an unrevised implant, but with persistent pain, are likely to define their surgery as a treatment failure. Thus, the awareness and use of patient-reported outcome measures (PROMs), an objective tool to identify the clinical and functional results after surgery, has increased substantially over the last decades (1,2). PROM data can potentially provide important information on quality assurance, contribute to self-improvement, and not least shared decision-making (2), and is today considered the best tool available to measure patientcentered results (3). The terms minimal clinically important improvement (MCII) and patient acceptable symptom state (PASS) have been introduced to find the levels of improvement that patients care about and the highest level of symptoms beyond which patients consider themselves well (4). Different methods for calculating MCII and PASS have been published, resulting in large variations in results, implying that reported values should be used with caution (5-8).
Clinical results of revision THA relative to results of primary THA are lacking, except from some smaller reports (9,10) and 1 larger report (11) with a moderate response rate, which are available. It is important to increase knowledge regarding clinical results for both the physician and the patients, especially the relative differences between primary and revision THA. Also, there is a subset of patients experiencing persistent pain, where satisfactory physical function or quality of life is not restored. Information on clinical results after primary and revision THA from larger cohorts is therefore needed to give healthcare providers and patients realistic knowledge on expected outcomes.
We present 1-year results after THA in a large population of 3,559 primary THAs and 406 revision THAs over an 8-year period, based on data from an institutional registry in a large-volume public hospital department.
Patients and methods
Design
Data was routinely collected in the institutional quality register for hip and knee arthroplasty patients established at St Olavs Hospital in 2010 (12). A comparison of registry data with the hospital’s patient administration system for all surgeries in 2017 and 2018 showed a coverage of 99.0%. The primary THAs in the present study were performed by 10 different consultants and orthopedic surgeons in training assisted by these consultants. The revision THAs were performed by 5 experienced orthopedic surgeons.
Data was registered preoperatively, during hospitalization, and twice after discharge (at 3-month and 1-year follow-ups) by the patient, ward nurses, and physiotherapists.
Patients
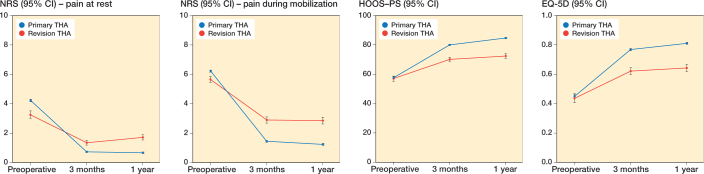
3,559 elective primary THA and 406 revision THA surgeries were included in the study (Figure 1). Demographics and length of stay are shown in Table 1. Primary THA patients were included consecutively from the start of the registry in September 2010 till December 2018, and followed till 1-year postoperatively. From 2012, all elective primary and revision THAs were included in a fast-track patient course, and hence in the quality registry. A previous study from our group has displayed the establishment of the fast-track patient course, and the results of the first 619 primary and 54 revision THAs included in the registry (9).
Figure 1.
Surgeries included in the study and the number analyzed at each follow-up.
Table 1.
Demographics and length of stay for primary and revision THA patients included in the study
| Variable | Primary THA | Revision THA |
|---|---|---|
| Age, mean (range) | 66 (18−98) | 69 (34−96) |
| Women, number (%) | 2,294 (64) | 272 (67) |
| BMI, mean (range) | 27 (14−52) | 27 (14−43) |
| Length of stay (days), mean (range) | 2.7 (1−28) | 3.8 (1−32) |
| ASA class, number (%) | ||
| I | 653 (19) | 26 (7) |
| II | 2058 (59) | 236 (61) |
| III | 730 (21) | 121 (31) |
| IV | 31 (1) | 4 (1) |
ASA = American Society of Anesthesiologists.
Patients admitted to hospital in an emergency setting such for as primary arthroplasty due to acute femoral fractures, reoperations due to infections, acute periprosthetic fractures, and acute dislocations were not included in the registry. Also, only reoperations with component revisions were included, thus excluding reconstructive muscle and fascia surgeries. Any reasons for reoperation within the 1st year were registered as a complication to the index surgery.
Each patient could be included in this study for a maximum of 4 index surgeries (1 primary and 1 revision for each side). For patients having multiple revision surgeries with exchange of components, only the 1st revision was included. 529 patients were enrolled in the database with more than 1 index surgery, of which 429 had bilateral primary THA.
Almost 80% of patients receiving primary THA had idiopathic arthritis, whereas the group with secondary arthritis was dominated by sequelae from hip dysplasia. The reasons for revision surgery were miscellaneous and often multiple reasons were given (Table 2).
Table 2.
Type of revisions performed
| Factor | Number (%) |
|---|---|
| Change of caput and polyethylene liner | 49 (12) |
| Revision of the acetabular component | 204 (50) |
| Revision of the femoral component | 48 (12) |
| Revision of both femur and acetabular component | 105 (26) |
| Total | 406 (100) |
Outcomes
Pain intensity was evaluated by the numeric rating scale (NRS), both during activity and rest. All patients were asked to rate their pain on an 11-point scale: “How would you rate your pain during mobilization/during rest, from 0–10 where 0 is no pain and 10 is worst imaginable pain.”
Health-related quality of life (HRQoL) was evaluated with the generic patient-administered European Quality of Life–5 Dimension (EQ-5D) questionnaires.
A hip-specific instrument was used to evaluate the physical function. The Hip Dysfunction and Osteoarthritis Outcome Score (HOOS) Physical Function Shortform (HOOS-PS) is derived from the 2 HOOS subscales addressing physical function. The scores range from 0 to 100, where 100 is no problem performing the specific tasks. HOOS-PS has been validated for use in patients receiving THA (13).
In addition, the patients were asked 2 anchor questions addressing their total experience with the surgery at the 1-year follow up. 1st, all patients were asked how their overall function in the joint was compared with before surgery. The answers were rated as: “better,” “same,” “unable to discriminate,” or “worse.” 2nd, they were asked whether they would go through with surgery again, knowing what they know today, where answers were given as; “yes,” “no.” or “unable to decide.”
MCII and PASS for pain
MCII estimates the smallest amount of change in a parameter that is of relevance to patients. MCII for pain has been defined as a minimum reduction in pain of 1.74 points on the 11-point NRS scale from preoperatively to 1-year follow-up (14). PASS can be a valuable supplement to MCII in estimating the PROM score patients find acceptable, defined as the overall health state at which the patients consider themselves as feeling well (4). Tubach et al. (15) have proposed a PASS value of 3.5 in pain scores as a generic threshold for NRS pain, which was defined as PASS at 1-year follow-up.
Statistics
We used a generalized linear mixed model to analyze repeated measures of PROMs collected preoperatively and at 3 months and 1 year postoperatively. Time-points and type of surgery (primary/revision) were modelled as fixed factors and a random subject intercept was included. Age, sex, BMI, and ASA classification were used as covariates in the model. The surgical approach for both primary and revision THA was changed from direct lateral approach to posterior approach in January 2015. Surgical approach was also included as a covariate in the statistical analyses. Normality of residuals was verified by histograms. Statistical analyses were performed using SPSS, version 27 software (IBM Corp, Armonk, NY, USA).
Ethics, funding, and potential conflict of interest
All patients were informed about the institutional quality register before inclusion. The patients gave signed informed consent allowing the data to be used for research purposes. The study was approved by the regional ethics committee (REC central) (approval no. 123645) and the National Archive and Center for Research Data (approval no. 480820). This study did not receive any form of grants or funding. The authors declare no conflict of interests.
Results
Changes in PROMs
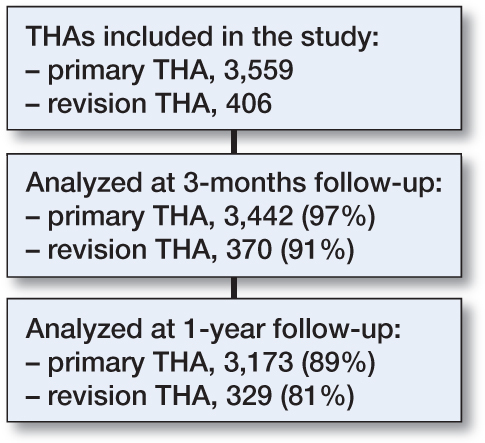
There were statistically significant improvements for pain at rest and during mobilization, HOOS-PS, and EQ-5D in both the primary and revision group from preoperatively to the first follow up 3 months postoperatively (Figure 2). Pain was reduced most during mobilization with a mean change of 5.1 (SD 2.6) on the NRS for primary THA and 2.9 (SD 3.0) for revision THA 1 year after surgery (Table 3). Patients receiving primary THA had more pain at rest and during mobilization than the revision group before surgery (Figure 2). The preoperative scores for HOOS-PS and EQ-5D were similar in the primary and revision groups.
Figure 2.
PROMs scores preoperatively, at 3-month follow up, and 1-year follow up. EQ-5D, European Quality of Life–5 Dimension score; HOOS-PS, Hip disability and Osteoarthritis Outcome Score Physical Function–Short Form. Blue line represents Primary THA and red line revision THA. The figure display model estimates with 95% confidence intervals, adjusted for age, sex, ASA, surgical approach, and BMI.
Table 3.
Mean (SD) of PROM scores preoperatively, at 3-month, and 1-year follow-up, and improvement from preoperative state to 1 year after surgery
| Type Prom | Preop. | 3 months | 1 year | Improvement preop.–1 year |
|---|---|---|---|---|
| Primary THA | ||||
| Pain at rest | 4.3 (2.4) | 0.8 (1.5) | 0.7 (1.5) | 3.6 (2.7) |
| Pain on mobilization | 6.3 (1.8) | 1.5 (1.9) | 1.2 (2.0) | 5.1 (2.6) |
| EQ-5D | 0.45 (0.29) | 0.77 (0.21) | 0.81 (0.22) | 0.36 (0.31) |
| HOOS-PS | 58 (17) | 80 (14) | 85 (14) | 27 (18) |
| Revision THA | ||||
| Pain at rest | 3.3 (2.8) | 1.4 (2.0) | 1.7 (2.4) | 1.6 (2.8) |
| Pain on mobilization | 5.7 (2.5) | 2.9 (2.6) | 2.8 (2.8) | 2.9 (3.0) |
| EQ-5D | 0.43 (0.32) | 0.62 (0.27) | 0.65 (0.28) | 0.22 (0.29) |
| HOOS-PS | 56 (18) | 69 (17) | 72 (18) | 16 (19) |
Responders
77% and 90% of patients receiving primary THA reached MCII for pain at rest and during mobilization, respectively. In contrast only 46% and 64% of the revision group reached the same criteria. The number of patients reaching the PASS criteria for pain at rest was quite high for both groups, and higher than the number of patients reaching MCII for pain at rest (Figure 3).
Figure 3.
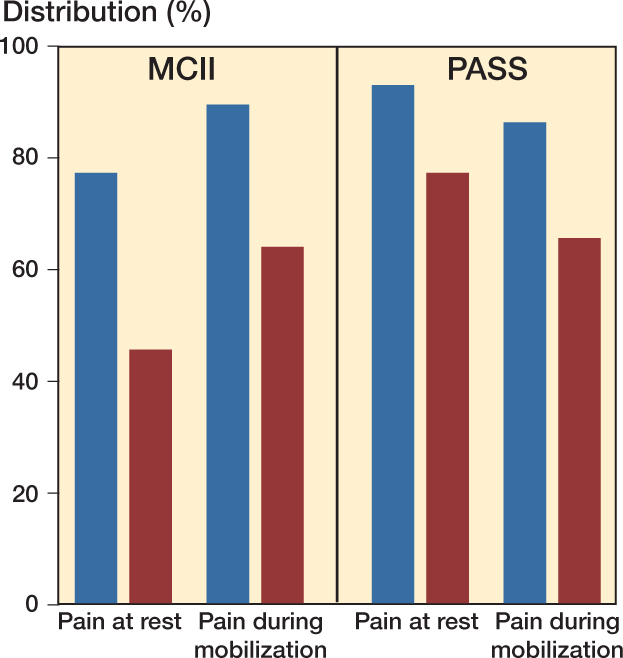
Percentage of patients reaching MCII (left) and PASS (right) for pain at rest and during mobilization. Blue displays primary THAs and red revision THA.
Anchor questions
In the primary THA group 93% of patients rated their function as better 1 year after surgery compared with before surgery, and the same percentage of patients would have been willing to go through surgery again. In the revision THA group the share of patients with better function was 78%, whereas 79% would have gone through surgery again (Figure 4).
Figure 4.
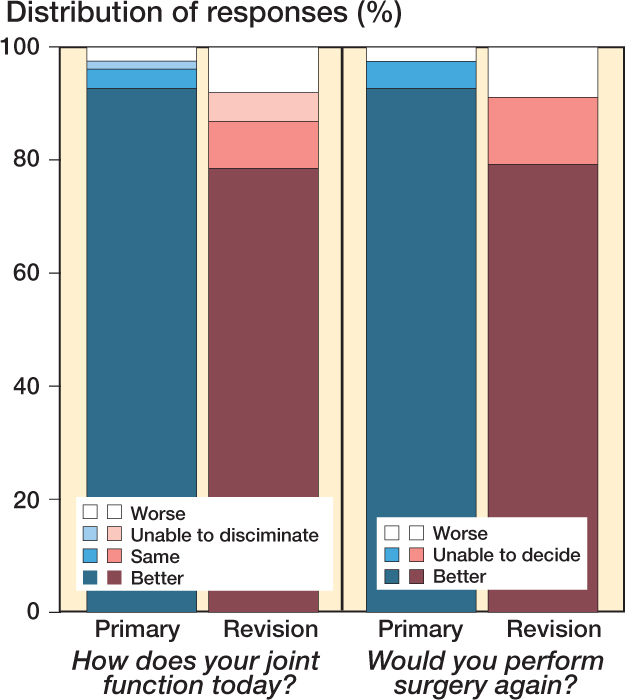
Patients’ response to anchor questions. Blue displays primary THA group and red displays revision THA group.
Discussion
We found very good results after primary THA in patients treated at a large-volume single institution by many surgeons.
78% of patients receiving revision THA rated their function as better 1 year postoperatively. This is in accordance with another study reporting that 79% of patients undergoing revision surgery in the hip joint were satisfied or very satisfied with their surgical results almost 8 years after surgery (16).
The largest improvement in pain scores was found for pain during mobilization for the primary group. This is reflected by the 90% reaching MCII for pain during mobilization. For pain at rest the proportion reaching PASS was considerably higher than the percentage reaching MCII: 77% versus 46%. This illustrates the difference between the 2 terms MCII and PASS, as some patients find that they have acceptable symptoms, even though the improvement was not as much as they probably expected. The results in our study regarding pain correspond well to those of others published for primary THA (17-19) and revision THA (11).
The primary THA group reported more pain preoperatively both at rest and during mobilization, compared with the revision THA group, whereas scores for Eq5D and HOOS-PS were similar. The difference in preoperative pain score probably contributes to the fact that fewer patients in the revision THA group reached MCII for pain.
The reported MCII for HOOS are inconsistent (20). A recent study validated PASS for EQ-5D in hip arthroplasty patients (21); however, we were not able to find reports on MCII for EQ-5D after THA surgery. These parameters are therefore not included in our analyses.
We found a substantial improvement for HOOS-PS and EQ-5D for both the primary and revision group, although to a lesser extent for the revision group. The mean change in EQ-5D for both the primary and the revision group at 1 year corresponds to findings in another study with follow-up at 6 months (10). For primary THA the improvement in EQ-5D in our study corresponds to that in other publications (19,22).
For the primary THA group the mean change in HOOS-PS preoperatively to 1 year postoperatively corresponds to the level of improvement shown in other studies evaluating PROM in THA (17,19,23). These results are, however, not as good as those published by Rosenlund et al. (22), who reported an improvement between 35 and 40 points in an RCT evaluating surgical approaches. Another large multicenter study found an overall improvement of 35 points for HOOS-PS 1 year postoperatively (24).
There are several factors known to influence the level of improvement, including the preoperative HOOS score (25). Our mean preoperative score was 58 for the primary group and 56 for the revision group, which is higher than reported in other studies, and might explain a slightly smaller change in HOOS-PS score compared with those studies. Obesity, lesser degree of joint space narrowing, and female sex are all factors found to negatively influence the chance of achieving MCII for pain or function (18,23). Further, surgical approach will affect the PROMs after THA (17).
To our knowledge, there are no reports on HOOS-PS in aseptic revision THA patients in the literature. A study on revisions due to infection found substantial lower mean HOOS-PS scores both pre- and postoperatively (26) than we found. This indicates that aseptic revisions are less dramatic for the patients as a good level of function might be restored.
It seems that results for pain and EQ-5D are more consistent than results published for HOOS-PS after primary THA surgery. Braaksma et al. (27) questions the validity of HOOS-PS used in patients receiving THA, and states that it might inadequately reflect patients’ functional level. Our results suggest that pain is the most consistent parameter when considering patients’ subjective response to hip arthroplasty surgery.
A strength of this study is the large patient population with high response rate at both follow-ups. To our knowledge this study presents the largest sample of revision THAs with a response rate of more than 80% at 1-year follow-up. This is well above the accepted levels for register studies (28), and together with a coverage of 99% this should ensure high external validity of the results. Further, the number of surgeons, including trainees, contributing to the study, the public hospital setting, and obligation to educate residents throughout the study period strengthens the generalizability of the results.
The statistical analysis considered the surgeries as independent cases. Some patients had more than 1 index surgery, and dependency would be expected. However, excluding patients would have left out important information, and we consider the data to be representative for the population. The revision THAs included in this study were all aseptic and operated on in an elective fast-track setting. This made this group more homogeneous than if infections and acute fractures had been included. This also represents a limitation of the study, as the results can only be applied for the elective setting. However, when it comes to shared decision-making the patients are submitted to a choice of surgery only in the elective setting. One might expect that PROMs could vary among patients receiving different types of revision surgery. This was not explored in the current study and should be the subject of further investigation.
In conclusion, more than 90% of patients receiving primary THA reported better function and would have the surgery again. In the revision THA group almost 80% reported better function 1 year after surgery. The most profound improvement was found for pain during mobilization, most prominent for the primary THA group. Patients should be informed preoperatively that the most marked improvement after THA surgery should be expected for pain during activity.
Acknowledgments
TSW, JK, and SBW planned the study. TSW, OSH, and AR participated in data collection. JK performed statistical analysis. All authors contributed to data analysis and writing the manuscript.
Acta thanks Gerjon Hannink for help with peer review of this study.
References
- 1.Siljander M P, McQuivey K S, Fahs A M, Galasso L A, Serdahely K J, Karadsheh M S. Current trends in patient-reported outcome measures in total joint arthroplasty: a study of 4 major orthopaedic journals. J Arthroplasty 2018; 33(11): 3416-21. [DOI] [PubMed] [Google Scholar]
- 2.Wilson I, Bohm E, Lübbeke A, Lyman S, Overgaard S, Rolfson O, et al. Orthopaedic registries with patient-reported outcome measures. EFORT Open Rev 2019; 4(6): 357-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rolfson O, Eresian Chenok K, Bohm E, Lubbeke A, Denissen G, Dunn J, et al. Patient-reported outcome measures in arthroplasty registries. Acta Orthop 2016; 87(Suppl. 1): 3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kvien T K, Heiberg T, Hagen K B. Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): what do these concepts mean? Ann Rheum Dis 2007; 66(Suppl. 3): iii 40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Terwee C B, Roorda L D, Dekker J, Bierma-Zeinstra S M, Peat G, Jordan K P, et al. Mind the MIC: large variation among populations and methods. J Clin Epidemiol 2010; 63(5): 524-34. [DOI] [PubMed] [Google Scholar]
- 6.Dekker J. The minimal clinically important difference re-considered. Osteoarthritis Cartilage 2019; 27(10): 1403-4. [DOI] [PubMed] [Google Scholar]
- 7.MacKay C, Clements N, Wong R, Davis A M. A systematic review of estimates of the minimal clinically important difference and patient acceptable symptom state of the Western Ontario and McMaster Universities Osteoarthritis Index in patients who underwent total hip and total knee replacement. Osteoarthritis Cartilage 2019; 27(10): 1408-19. [DOI] [PubMed] [Google Scholar]
- 8.Mouelhi Y, Jouve E, Castelli C, Gentile S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual Life Outcomes 2020; 18(1): 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winther S B, Foss O A, Wik T S, Davis S P, Engdal M, Jessen V, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop 2015; 86(1): 78-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Postler A E, Beyer F, Wegner T, Lutzner J, Hartmann A, Ojodu I, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int 2017; 27(2): 180-6. [DOI] [PubMed] [Google Scholar]
- 11.van der Wees P J, Wammes J J, Akkermans R P, Koetsenruijter J, Westert G P, van Kampen A, et al. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: results of twenty years clinical registry. BMC Musculoskelet Disord 2017; 18(1): 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjorgen S, Jessen V, Husby O S, Roset O, Foss O A. Internal quality register for joint prostheses. Tidsskr Nor Laegeforen 2012; 132(6): 626-7. [DOI] [PubMed] [Google Scholar]
- 13.Davis A M, Perruccio A V, Canizares M, Tennant A, Hawker G A, Conaghan P G, et al. The development of a short measure of physical function for hip OA HOOS–Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthritis Cartilage 2008; 16(5): 551-9. [DOI] [PubMed] [Google Scholar]
- 14.Farrar J T, Young J P Jr, LaMoreaux L, Werth J L, Poole M R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94(2): 149-58. [DOI] [PubMed] [Google Scholar]
- 15.Tubach F, Ravaud P, Martin-Mola E, Awada H, Bellamy N, Bombardier C, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res (Hoboken) 2012; 64(11): 1699-707. [DOI] [PubMed] [Google Scholar]
- 16.Turnbull G S, Scott C E H, MacDonald D J, Breusch S J. Return to activity following revision total hip arthroplasty. Arch Orthop Trauma Surg 2019; 139(3): 411-21. [DOI] [PubMed] [Google Scholar]
- 17.Peters R M, van Beers L, van Steenbergen L N, Wolkenfelt J, Ettema H B, Ten Have B, et al. Similar superior patient-reported outcome measures for anterior and posterolateral approaches after total hip arthroplasty: postoperative patient-reported outcome measure improvement after 3 months in 12,774 primary total hip arthroplasties using the anterior, anterolateral, straight lateral, or posterolateral approach. J Arthroplasty 2018; 33(6): 1786-93. [DOI] [PubMed] [Google Scholar]
- 18.Rojanasopondist P, Galea V P, Connelly J W, Matuszak S J, Rolfson O, Bragdon C R, et al. What preoperative factors are associated with not achieving a minimum clinically important difference after THA? Findings from an international multicenter study. Clin Orthop Relat Res 2019; 477(6): 1301-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braaksma C, Oehlers V, Veen M R, Wolterbeek N. Patient characteristics do not predict the change in physical functioning following arthroplasty measured by the HOOS-PS and KOOS-PS. J Orthop 2020; 20: 122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuo A C, Giori N J, Bowe T R, Manfredi L, Lalani N F, Nordin D A, et al. Comparing methods to determine the minimal clinically important differences in patient-reported outcome measures for veterans undergoing elective total hip or knee arthroplasty in Veterans Health Administration hospitals. JAMA Surg 2020; 155(5): 404-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Florissi I, Galea V, Shin D, Sauder N, Colon Iban Y E, Ingelsrud L H, et al. External validation of achieving the patient acceptable symptom state for the EuroQol-5 Dimension 1 year after total hip arthroplasty. J Bone Joint Surg Am 2021; 103(2): e5. [DOI] [PubMed] [Google Scholar]
- 22.Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop 2017; 88(3): 239-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katakam A, Florissi I S, Colon Iban Y E, Bragdon C R, Chen A F, Melnic C M, et al. Class III obesity increases risk of failure to achieve the 1-year Hip Disability and Osteoarthritis Outcome Score–Physical Function Short Form minimal clinically important difference following total hip arthroplasty. J Arthroplasty 2021; 36(1): 187-92. [DOI] [PubMed] [Google Scholar]
- 24.Paulsen A, Roos E M, Pedersen A B, Overgaard S. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 2014; 85(1): 39-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berliner J L, Brodke D J, Chan V, SooHoo N F, Bozic K J. John Charnley Award: Preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res 2016; 474(2): 321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tirumala V, Klemt C, van den Kieboom J, Xiong L, Kwon Y M. Comparison of patient reported outcome measures after single versus two-stage revision for chronic infection of total hip arthroplasty: a retrospective propensity score matched cohort study. Arch Orthop Trauma Surg 2021; 141(10): 1789-96. [DOI] [PubMed] [Google Scholar]
- 27.Braaksma C, Wolterbeek N, Veen M R, Prinsen C A C, Ostelo R. Systematic review and meta-analysis of measurement properties of the Hip disability and Osteoarthritis Outcome Score–Physical Function Shortform (HOOS-PS) and the Knee Injury and Osteoarthritis Outcome Score–Physical Function Shortform (KOOS-PS). Osteoarthritis Cartilage 2020; 28(12): 1525-38. [DOI] [PubMed] [Google Scholar]
- 28.Pronk Y, van der Weegen W, Vos R, Brinkman J M, van Heerwaarden R J, Pilot P. What is the minimum response rate on patient-reported outcome measures needed to adequately evaluate total hip arthroplasties? Health Qual Life Outcomes 2020; 18(1): 379. [DOI] [PMC free article] [PubMed] [Google Scholar]