Introduction
The number of deaths attributable to CKD in India rose from 0.59 million in 1990 to 1.18 million in 2016 (1). Data on incidence and prevalence of kidney failure remain estimates because there are no kidney failure registries. The Million Death Study estimated the number of kidney failure deaths to be 136,000 in 2015 (2). A 2018 estimate put the number of patients on chronic dialysis in India at about 175,000, giving a prevalence of 129 per million population (3). A systematic review estimated that about two thirds of all patients with kidney failure died without receiving dialysis in 2010 (4).
The burden of kidney failure deaths in India is greater in comparison to other low- and middle-income economies with a similar sociodemographic index, suggesting an improvement in mortality rates in India is possible, even with the existing resources (1). Both in absolute and relative terms, the proportion of patients with kidney failure who have access to treatment and are covered by an insurance scheme is lower than China, the only country more populous than India.
According to a 2012 report from the Indian CKD Registry, the most commonly identified causes of kidney failure were diabetes, hypertension, and GN, whereas the cause was not discernible in about 16% of patients (5). Dubbed CKD of unknown etiology, such cases are reported from all over the country, with the states of Andhra Pradesh, Odisha, Maharashtra, Goa, and Tamil Nadu reporting a particularly high burden (6). The exact causes of CKD of unknown etiology is a topic of ongoing research, with recurrent dehydration as a result of outdoor work in hot and humid weather, consumption of water contaminated with heavy metals, and exposure to pesticides being implicated most frequently (6).
There are few data on the burden of comorbidities and complications of kidney failure. Hypertension was reported in 85%–97% of patients with kidney failure (7,8). CKD–mineral bone disease is widely prevalent, with most patients taking calcium-based phosphate binders (8), and there is a high prevalence of malnutrition (9). Cardiovascular disease and infections are responsible for two thirds of overall mortality (10). The most common infections include those related to dialysis catheters (11) and tuberculosis. About 7%–10% of patients on dialysis get tuberculosis, with atypical extrapulmonary presentations being common (12). The reported prevalence of hepatitis B and C in dialysis units varies between 2%–42% and 4%–45%, respectively.
Dialysis Services in India
Hemodialysis (HD) is the most common RRT modality in India (3). The first HD was performed at Christian Medical College (Vellore, Tamil Nadu) in 1961 on an erstwhile Maharaja under the supervision of Dr. Satoru Nakamoto, who had flown in from Seattle, Washington (13). Until 1970, only patients with AKI were dialyzed at the four centers across the country, and maintenance HD was available at six centers in India in 1978 (13). Growth in the following years was slow, with HD being restricted to a few public and private hospitals in large cities until the 1990s. The number and distribution of HD units has increased over the last 20 years, and dialysis is now available in all 28 states and eight union territories (3).
The number of HD stations in India was estimated at 12,881 in 2018 (3). The union government announced a National Dialysis Program in 2016, that envisages setting up an eight-station dialysis facility in all 688 districts of the country to provide HD to poor patients. If patients were dialyzed twice a week (which is commonly done in India), only about 50,000 new patients (representing about a third of the current requirement) would be accommodated under this program, even without future growth (14).
Like many of the secondary- and tertiary-level healthcare services, dialysis services in India are predominantly driven by the private sector, reflecting low public spending on healthcare. Public-sector hospitals largely manage patients who are critically sick and those with AKI, leaving limited capacity for accommodating patients on maintenance dialysis.
Large inequities exist in access to dialysis. Two thirds of the population of India live in rural areas, where the availability of HD is limited. According to one study (2), almost 60% of patients on dialysis had to travel >50 km to access HD, and nearly a quarter lived >100 km away from the facility. The burden of travel increases costs and exacerbates loss of wages. Further, women are under-represented (15), and there are few pediatric dialysis services. Shared decision making is practiced infrequently, and access to conservative care is virtually nonexistent.
There is variability in frequency, session length, and HD prescription. The globally accepted standard of thrice-a-week dialysis delivery is restricted to affluent patients getting dialysis in corporate hospitals. Twice-a-week HD is the most common practice, delivered in the majority of centers (7,8). About a quarter of patients receive dialysis once a week or “as needed” for financial feasibility. Dialysis sessions are usually 3–4 hours long. The adequacy of dialysis is not uniformly reported. A study of 463 patients reported a single-pool Kt/V of more than one in only 50% of sessions (16). In another study of 50 patients on twice-weekly treatment, only 28% had a standardized Kt/V of two per week (17). The long-term effects of having dialysis twice a week have not been examined. According to one report from a state-wide database (15), about 49% of patients stopped dialysis and 13% died within 1 year. The reasons for poor outcomes are unclear but are postulated to be a mix of financial burden, multiple comorbidities, poor access, and poor dialysis quality. An incremental dialysis approach has been suggested, but has not been rigorously studied. Close monitoring of residual kidney function might support this practice to optimize resource utilization (18).
Vascular-access care is an area of concern, resulting from a combination of factors including poor vessel protection; high and prolonged temporary catheter use; shortage of intervention nephrologists, surgeons, and radiologists skilled in creating permanent vascular access; and managing access-related complications (19).
In 2009, the Indian Society of Nephrology published recommendations for setting up and running HD units, which were endorsed by the Union Ministry of Health (20). These include all aspects of care, including technical specifications for HD equipment and water treatment, human-resource needs, and quality standards. However, there are no enforcement mechanisms, and the degree of compliance with the recommended standards is unknown. Most centers use a combined deionization and reverse-osmosis water treatment system, but water quality standards are not mandatorily monitored in many centers. Most units have separate areas for dialyzing patients who are positive for hepatitis B and/or hepatitis C. Dialyzer reuse (manual or automated) is common, especially in publicly funded facilities. The number of times a dialyzer is reused varies, but can be up to 25 times. Some private centers provide a single-use service, but at a higher cost.
Despite the potential advantages of peritoneal dialysis (PD) (no requirement to set up expensive infrastructure; avoids long travel to dialysis centers; and allows for patient-friendly, home-based therapy), PD penetration is poor—there were only about 8500 patients on PD in India in 2019 (3). The reasons for poor utilization include high cost of supplies, deprioritization by nephrologists due to lower reimbursement for PD, and fear of complications. The number of patients on home HD is <50 in the entire country.
Even as a large proportion of the population remains disenfranchised from dialysis, the use of more expensive convective therapies, such as hemodiafiltration, is increasing in corporate hospitals that cater to rich patients and to those with access to insurance.
In recent years, HD services have grown in the public-private partnership (PPP) mode. In this model, governments contract private entities to finance, build, and operate dialysis units at an agreed-upon rate. PPP offers several advantages, such as economies of scale through strategic purchasing and process efficiencies, scalable training of workforce, opportunities to implement standard operating procedures, and monitoring of quality. PPP transfers responsibilities and risks of infrastructure and service delivery to the private sector, but at the taxpayer’s expense and, therefore, requires strong oversight and governance. No formal evaluation of these programs has been undertaken so far. Currently, there are around ten large dialysis providers providing PPP services, with the largest one (NephroPlus) managing 16,000 patients in >210 centers.
Workforce
India has one of the lowest nephrology workforce densities worldwide. There are only about 2600 nephrologists (1.9 per million population), and there is a chronic shortage of dialysis nurses and technicians. There are about 72 nephrology training programs, with an intake of approximately 150 trainees every year who go through a 3-year course. Similar statistics for other personnel are not available. Nurses are required to receive 6 months of practical training in the dialysis unit, in addition to basic nursing training, and dialysis technicians undergo a certificate course in dialysis technology. Some stand-alone dialysis centers are run by dialysis technicians and are not regularly supervised by nephrologists. Other multipurpose workers provide sanitation, machine cleaning, and dialyzer reprocessing services. Very few centers have access to renal dieticians.
Funding
Health expenditure is 4% of the gross domestic product in India, as opposed to an average of 10% worldwide (21). Public-health spending is approximately a quarter of the overall health expenditure, or about 22 USD per capita, one of the lowest in the world. Universal health insurance is meager, with only 37% of the population having access to some health insurance in 2017–2018.
The Indian dialysis market is estimated to be growing at a rate of 31% per annum, compared with 8% in the rest of the world. Payment for dialysis is a mixture of state funding, employment-based insurance, charity, and self-funding (Box 1). Most patients pay for dialysis from their own resources because they are not eligible for state funding and are not covered under insurance. This includes most of the rural population engaged in farming and those working in the unorganized sectors. The high rate of catastrophic healthcare spending, supported by distress financing, that pushes families into poverty is well documented (22).
Box 1.
Box 1. An overview of dialysis services in India
Number of patients on dialysis in India (total number and per 1000 people in the general population).
Number of patients on home dialysis in India.
Are all dialysis sessions covered by insurance, or do some patients have out-of-pocket expenses?.
Are the dialysis units hospital based or freestanding?.
Are the dialysis units for profit or nonprofit?.
What is the reimbursement per dialysis session in USD?.
Are all of the staff who deliver dialysis nurses, or do you also use patient-care technicians?.
What is the typical patient to RN ratio in the dialysis units? 3–5:1 What is the average length of a dialysis session?.
How many times per month are patients seen by a nephrologist during dialysis sessions?.
What is the proportion of patients on HD in India using an AVF, AVG, and CVC?.
174,478 (as of 2018) (3).
8500.
About 35% of patients on dialysis have some insurance coverage. Most patients incur out-of-pocket expenses to varying degrees. New reimbursement schemes are expected to increase insurance coverage.
Both hospital-based and freestanding dialysis units exist, with predominant freestanding units.
Units are for profit in corporate and freestanding units; public hospital units and those run by charities are nonprofit What is the reimbursement per dialysis session in USD? Approximately 15–63 USD.
Nurses and technicians work interchangeably to deliver dialysis.
3–5:1.
3–4 h.
Variable. In smaller cities and towns, once in 2–3 mo; in larger cities, four to six times per mo.
Prevalent patients: AVF, 56%–87%; CVC, 13%–44%; AVG, 1% Incident patients: CVC .75%; AVF, 25%.
RN, registered nurse; HD, hemodialysis; AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, central venous catheter
The annual reimbursement for HD in India ranges from approximately 1400 USD to 10,800 USD, depending on the nature of the facility. However, this reimbursement is not based on any health technology assessment, and largely reflects only the cost of dialysis consumables and overhead costs in private centers (Figure 1). Many of the cost components are hidden because they are part of the overall hospital budgets and not included in calculation of reimbursement for HD. In the only comprehensive study of costing of HD, the total cost incurred in one session of HD in a public hospital was estimated at 4148 INR (64 USD) (23). The cost of creating an arteriovenous fistula varies between 6000 INR (78.7 USD) and 20,000 INR (262.2 USD).
Figure 1.
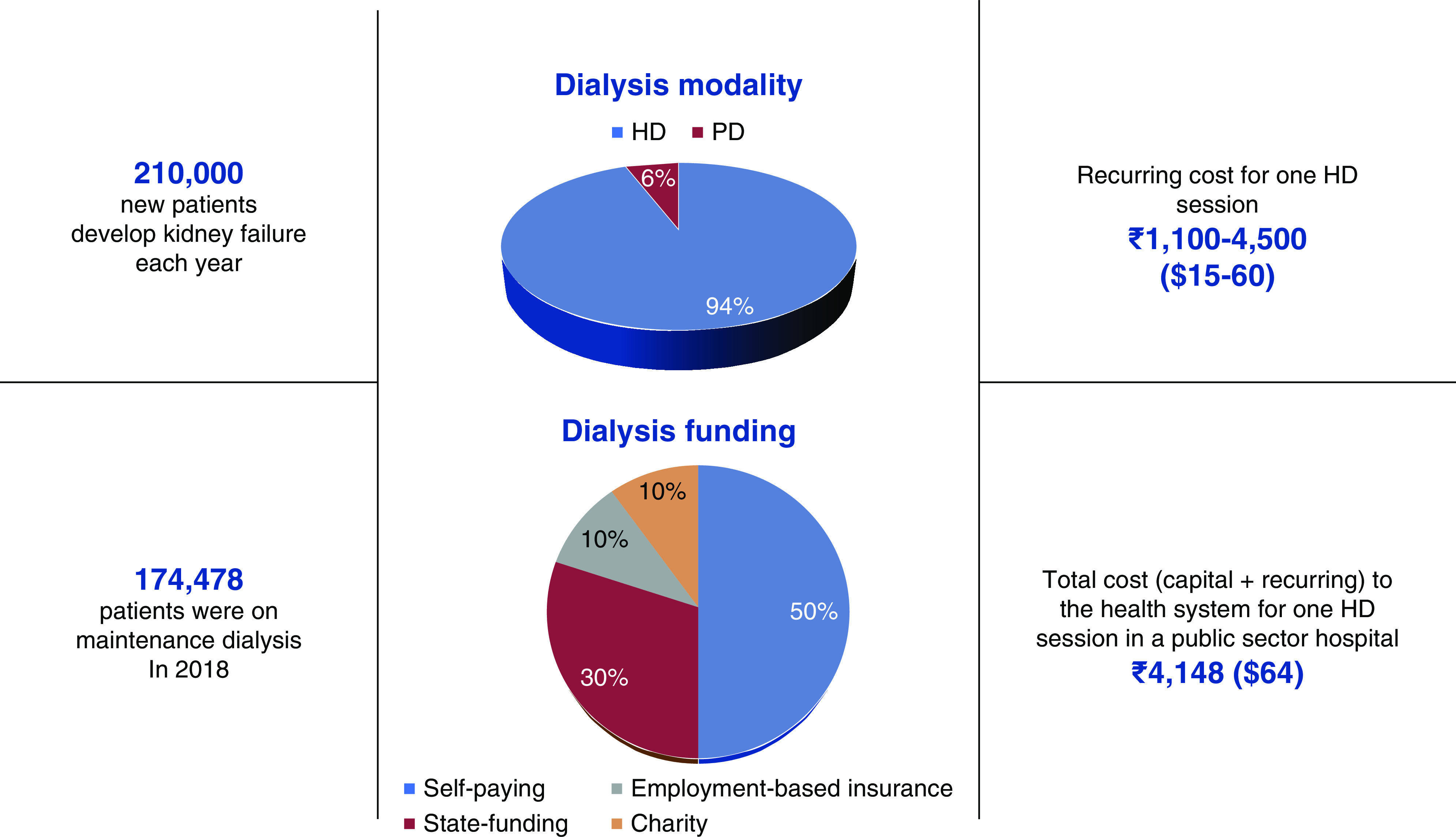
Number of patients on dialysis, modality distribution, and funding. HD, hemodialysis; PD, peritoneal dialysis.
In addition to the aforementioned National Dialysis Scheme, which operates through designated district-level centers, eligible patients can receive dialysis in other hospitals that are reimbursed under the National Health Protection Scheme (launched in 2018), later renamed the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (24). Both of these schemes do not cover direct (e.g., medication, management of complications) or indirect (e.g., travel) expenses that are not dialysis related. In a study that examined the outcomes of patients dialyzed through a publicly funded insurance scheme (Aarogyasri) in the state of Andhra Pradesh, only about 53% of patients continued HD after 6 months (15). In 2019, the government added reimbursement for PD to the National Dialysis Scheme. There are a number of other government-run employee health schemes that offer a reimbursement of 2900–3335 INR (45–51 USD) per dialysis session, and also reimburse other direct medical costs (25). Private-sector employees can get reimbursed through private insurance schemes.
Looking Ahead
Dialysis is growing rapidly in India, but there is room to improve access and quality of service. With commitment from the union and state governments and entry of new service providers, scaling up of service delivery seems a realistic goal. Although HD is the dominant modality currently, wider adoption of PD might allow for more rapid and equitable expansion, including to remote rural areas. Training of a cadre of professionals that provide all-round care and address common issues related to dialysis delivery, including expertise in vascular access care, is a priority. Development of a registry would allow ongoing monitoring of the quality of service delivery, provide iterative feedback for service improvement, and allow international comparisons. For maximum effect, dialysis services should develop as a component of an integrated kidney replacement therapy program that includes kidney transplantation for suitable subjects and conservative care for those deemed to be unsuitable for dialysis. Finally, the health systems should be reoriented to increase focus on primary care that prioritizes early detection and prevention of progression of kidney disease.
Disclosures
V. Jha has received fees from AstraZeneca, NephroPlus, and Zydus Cadilla, and grants from Baxter Healthcare, Biocon, and GlaxoSmithKline. All funds are paid to his organization. The remaining author has nothing to disclose.
Funding
None.
Acknowledgments
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Author Contributions
J. Bharati wrote the original draft and was responsible for data curation; V. Jha conceptualized the study, provided supervision, and reviewed and edited the manuscript.
References
- 1.Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, Maddukuri G, Tsai CY, Floyd T, Al-Aly Z: Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int 94: 567–581, 2018. 10.1016/j.kint.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 2.Dare AJ, Fu SH, Patra J, Rodriguez PS, Thakur JS, Jha P; Million Death Study Collaborators: Renal failure deaths and their risk factors in India 2001-13: Nationally representative estimates from the million death study. Lancet Glob Health 5: e89–e95, 2017. 10.1016/S2214-109X(16)30308-4 [DOI] [PubMed] [Google Scholar]
- 3.Jha V, Ur-Rashid H, Agarwal SK, Akhtar SF, Kafle RK, Sheriff R; ISN South Asia Regional Board: The state of nephrology in South Asia. Kidney Int 95: 31–37, 2019. 10.1016/j.kint.2018.09.001 [DOI] [PubMed] [Google Scholar]
- 4.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, Zhao MH, Lv J, Garg AX, Knight J, Rodgers A, Gallagher M, Kotwal S, Cass A, Perkovic V: Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 385: 1975–1982, 2015. 10.1016/S0140-6736(14)61601-9 [DOI] [PubMed] [Google Scholar]
- 5.Rajapurkar MM, John GT, Kirpalani AL, Abraham G, Agarwal SK, Almeida AF, Gang S, Gupta A, Modi G, Pahari D, Pisharody R, Prakash J, Raman A, Rana DS, Sharma RK, Sahoo RN, Sakhuja V, Tatapudi RR, Jha V: What do we know about chronic kidney disease in India: First report of the Indian CKD registry. BMC Nephrol 13: 10, 2012. 10.1186/1471-2369-13-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anupama YJ, Sankarasubbaiyan S, Taduri G: Chronic kidney disease of unknown etiology: Case definition for India – a perspective. Indian J Nephrol 2019. 10.4103/ijn.IJN_327_18 [DOI] [PMC free article] [PubMed]
- 7.Lakshminarayana GR, Sheetal LG, Mathew A, Rajesh R, Kurian G, Unni VN: Hemodialysis outcomes and practice patterns in end-stage renal disease: Experience from a tertiary care hospital in Kerala. Indian J Nephrol 27: 51–57, 2017. 10.4103/0971-4065.177210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kulkarni MJ, Jamale T, Hase NK, Jagdish PK, Keskar V, Patil H, Shete A, Patil C: A cross-sectional study of dialysis practice-patterns in patients with chronic kidney disease on maintenance hemodialysis. Saudi J Kidney Dis Transpl 26: 1050–1056, 2015 [DOI] [PubMed] [Google Scholar]
- 9.Vijaya KL, Aruna M, Narayana Rao SVL, Mohan PR: Dietary counseling by renal dietician improves the nutritional status of hemodialysis patients. Indian J Nephrol 29: 179–185, 2019. 10.4103/ijn.IJN_272_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandrashekar A, Ramakrishnan S, Rangarajan D: Survival analysis of patients on maintenance hemodialysis. Indian J Nephrol 24: 206–213, 2014. 10.4103/0971-4065.132985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devraj A, Siva Tez Pinnamaneni V, Biswal M, Ramachandran R, Jha V: Extranasal Staphylococcus aureus colonization predisposes to bloodstream infections in patients on hemodialysis with noncuffed internal jugular vein catheters. Hemodial Int 21: 35–40, 2017. 10.1111/hdi.12450 [DOI] [PubMed] [Google Scholar]
- 12.Jha V, Chugh S, Chugh KS: Infections in dialysis and transplant patients in tropical countries. Kidney Int 57: S-85–S-93, 2000. 10.1046/j.1523-1755.2000.07415.x [DOI] [Google Scholar]
- 13.Chugh KS: Five decades of Indian nephrology: A personal journey. Am J Kidney Dis 54: 753–763, 2009. 10.1053/j.ajkd.2009.06.027 [DOI] [PubMed] [Google Scholar]
- 14.Jha V: Providing dialysis in India: Many pieces in the puzzle [published online ahead of print October 30, 2019]. Natl Med J India, 2019. 10.4103/0970-258X.279969 [DOI] [PubMed] [Google Scholar]
- 15.Shaikh M, Woodward M, John O, Bassi A, Jan S, Sahay M, Taduri G, Gallagher M, Knight J, Jha V: Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int 94: 440–445, 2018. 10.1016/j.kint.2018.03.028 [DOI] [PubMed] [Google Scholar]
- 16.Rao M, Juneja R, Shirly RB, Jacob CK: Haemodialysis for end-stage renal disease in Southern India--a perspective from a tertiary referral care centre. Nephrol Dial Transplant 13: 2494–2500, 1998. 10.1093/ndt/13.10.2494 [DOI] [PubMed] [Google Scholar]
- 17.Chauhan R, Mendonca S: Adequacy of twice weekly hemodialysis in end stage renal disease patients at a tertiary care dialysis centre. Indian J Nephrol 25: 329–333, 2015. 10.4103/0971-4065.151762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Obi Y, Streja E, Rhee CM, Ravel V, Amin AN, Cupisti A, Chen J, Mathew AT, Kovesdy CP, Mehrotra R, Kalantar-Zadeh K: Incremental hemodialysis, residual kidney function, and mortality risk in incident dialysis patients: A cohort study. Am J Kidney Dis 68: 256–265, 2016. 10.1053/j.ajkd.2016.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bansal D, Kher V, Gupta KL, Banerjee D, Jha V: Haemodialysis vascular access: Current practices amongst Indian nephrologists. J Vasc Access 19: 172–176, 2018. 10.5301/jva.5000817 [DOI] [PubMed] [Google Scholar]
- 20.Indian Society of Nephrology : The Indian Society of Nephrology guidelines for hemodialysis units. Available at: http://isn-india.org/images/Image/Docs/HD_GL.pdf. Accessed August 28, 2020
- 21.The World Bank : Current health expenditure (% of GDP). Available at: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS. Accessed August 28, 2020
- 22.Bradshaw C, Gracious N, Narayanan R, Narayanan S, Safeer M, Nair GM, Murlidharan P, Sundaresan A, Retnaraj Santhi S, Prabhakaran D, Kurella Tamura M, Jha V, Chertow GM, Jeemon P, Anand S: Paying for hemodialysis in Kerala, India: A Description of household financial hardship in the context of medical subsidy. Kidney Int Rep 4: 390–398, 2018. 10.1016/j.ekir.2018.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaur G, Prinja S, Ramachandran R, Malhotra P, Gupta KL, Jha V: Cost of hemodialysis in a public sector tertiary hospital of India. Clin Kidney J 11: 726–733, 2018. 10.1093/ckj/sfx152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ministry of Health and Family Welfare, Government of India: Year ender 2018: Ministry of Health and Family Welfare, New Delhi, India, Press Information Bureau, 2019. Available at: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1559536. Accessed August 28, 2020 [Google Scholar]
- 25.Central Government Health Scheme, Ministry of Health and Family Welfare: List of empanelled hospitals, diagnostic centers, and CGHS rates. Available at https://cghs.nic.in/reports/view_hospital.jsp. Accessed September 1, 2020


