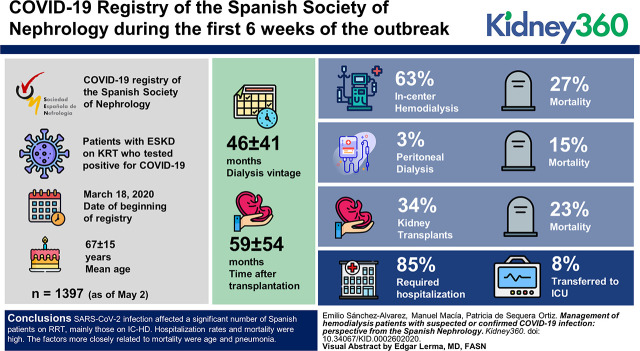
Visual Abstract
Keywords: dialysis, COVID-19, hemodialysis, pandemic, renal dialysis, Spain
Abstract
Background
The recent SARS-CoV-2 coronavirus pandemic has signified a significant effect on the health of the population worldwide. Patients on chronic RRT have been affected by the virus, and they are at higher risk due to the frequent comorbid conditions. Here, we show the results of the COVID-19 Registry of the Spanish Society of Nephrology during the first 6 weeks of the outbreak.
Methods
This study is an analysis of the data recorded on a registry of patients with ESKD on RRT who tested positive for COVID-19. The aim was to evaluate clinical conditions, therapeutic management, and consequences, including outcome. The registry began on March 18th, 2020. It includes epidemiologic data, cause of CKD, signs and symptoms of the infection, treatments, and outcomes. Patients were diagnosed with SARS-CoV-2 infection on the basis of the results of PCR of the virus obtained from nasopharyngeal/oropharyngeal swabs. The tests were performed on symptomatic patients and on those who mentioned contact with infected patients.
Results
As of May 2, the registry included data on 1397 patients (in-center hemodialysis [IC-HD], 63%; kidney transplant [Tx], 34%; peritoneal dialysis [PD], 3%; and home hemodialysis, 0.3%). The mean age was 67±15 years, and two-thirds were men. Dialysis vintage was 46±41 months, and the time after transplantation was 59±54 months. Eighty-five percent of the patients required hospital admission, and 8% had to be transferred to intensive care units. Overall mortality was 25% (IC-HD, 27%; Tx, 23%; and PD, 15%), and significant proportions of deceased patients have advanced age, are on IC-HD, and presented pneumonia. Age and pneumonia were independently associated with the risk of death.
Conclusions
SARS-CoV-2 infection affected a significant number of Spanish patients on RRT, mainly those on IC-HD. Hospitalization rates and mortality were high. The factors more closely related to mortality were age and pneumonia.
Introduction
The new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causes several clinical conditions under the term coronavirus disease 2019 (COVID-19) that vary from common cold symptoms to severe pneumonia, respiratory distress syndrome, septic shock, and multiorgan failure. Interestingly, most of the COVID-19 cases reported so far start with mild symptoms (1).
Certain groups of patients (i.e., the elderly and those with chronic obstructive pulmonary disease) are at higher risk of COVID-19 infection and its complications. Patients on RRT are of special concern (2).
During the first days of the COVID-19 outbreak, the Spanish Society of Nephrology (SEN), together with health authorities and associations of patients with CKD (Association for the Fight Against Kidney Diseases), established an action plan with specific strategies to obtain all possible information from patients on RRT with this new and serious disease (3). One of the first commitments was to create a Spanish registry of patients on chronic RRT, referred as the “SEN Registry of COVID-19.”
In this study, we describe some of the factors influencing the clinical condition, the therapeutic management, and the consequences of COVID-19 infection on patients on RRT (those on dialysis and transplant [Tx] recipients) in Spain during the first 6 weeks of the outbreak.
Material and Methods
The data collection of the COVID-19 registry began on March 18, 2020. The following variables were included: epidemiologic, modalities of RRT (in-center hemodialysis [IC-HD], peritoneal dialysis [PD], home hemodialysis [HHD], and Tx), infection data, comorbid conditions, accompanying symptoms, treatments, and outcomes. The registry was approved by the Regional Ethical Committee of Asturias.
The COVID-19 registry has an “online” structure with access through a website (www.senefro.org). Only members of the society have access to the website to enter the data from their patients. After identification, they may access to information of their own patients. The majority of dialysis and Tx centers in Spain (93%) entered patients in the registry. A coordinator of the registry was designated and granted full access to all of the database information. Patients were diagnosed with SARS-CoV-2 infection on the basis of the results of a real-time PCR test from nasopharyngeal/oropharyngeal swabs. These tests were performed in symptomatic patients and in those who had any contact with an infected patient. The registry will remain operational as long as the current coronavirus pandemic situation continues. Thus, the results presented are from the data recorded up to May 2, 2020.
Continuous variables were expressed as mean ± SD, and categorical variables were expressed as percentages. Baseline values were compared using the t test and the chi-squared test as appropriate. The Kolmogorov–Smirnov test was used to determine whether the values were normally distributed. Linear or logistic regression models were used to know the factors associated with mortality. A P value of 0.05 was considered significant. The statistical package SPSS 20 for Windows (SPSS Inc., Chicago, IL) was used to analyze the results.
Results
Data from 1397 patients with documented SARS-CoV-2 coronavirus infection were included in the registry. All regions of Spain reported cases (Supplemental Table 1). The mean age of patients was 67±15 years, and two-thirds were men. Causes of CKD were diabetic nephropathy in 22%, ischemic/hypertensive nephropathy in 19%, and glomerular disease in 17%. The type of RRT was IC-HD in 875 (63%), Tx in 470 (34%), PD in 48 (3%), and HHD in four (0.3%). Mean time on dialysis was 46±41 months. In accordance with these data and considering all patients on RRT in Spain (4), it can be stated that 4.5% of the total population on IC-HD was infected compared with 1.8% of the patients on PD and 1.6% of Tx recipients. In patients with Tx, the most common immunosuppressive treatment was a combination of steroids, tacrolimus, and mycophenolate, followed by tacrolimus and mycophenolate, and the mean time on Tx was 59 months (interquartile range, 9–132). Unfortunately, there was no information collected about the donation, but it should be pointed out that in Spain, >90% of Tx are from deceased donors.
Every patient who presented with COVID-19 infection was investigated for prior contacts. Three of ten reported contact with an infected individual. This represents 297 (34%) patients on IC-HD, 11 (24%) patients on PD, and 103 (22%) patients with Tx. Only four patients were on HHD. The mean incubation period was 7±4 days.
In relation to clinical manifestations, 1048 (75%) patients had fever, 1046 (75%) patients had pneumonia, 838 (60%) patients had upper respiratory tract infection, and 699 (50%) patients had dyspnea. Interestingly, only 182 (13%) patients were asymptomatic, and lymphopenia was present in 1118 (80%) patients.
A high percentage of registered patients (85%) required hospital admission, 112 (8%) had to be admitted to intensive care units, and mechanical ventilation was required in two-thirds of these patients. The mean length of hospital stay (taking into account only recovered patients) was 10±4 days.
The most commonly prescribed treatments (Table 1) were hydroxychloroquine and lopinavir–ritonavir. Other therapies, such as steroids, IFN, and tocilizumab, were used less frequently.
Table 1.
Pharmacologic therapies targeting coronavirus disease 2019
| Drug | Percentage |
| Hydroxychloroquine | 85 |
| Lopinavir–ritonavir | 39 |
| Steroids | 35 |
| Tocilizumab | 10 |
| IFN | 5 |
Clinical characteristics were different in patients on dialysis (IC-HD, HHD, and PD) versus patients with Tx (Table 2). Patients with Tx were younger, had more prior hospital admissions, developed pneumonia, and received specific treatments (lopinavir–ritonavir, hydroxychloroquine, steroids, and tocilizumab) more frequently than patients on dialysis. Also, we found that most of them were receiving renin-angiotensin-aldosterone system (RAAS) inhibitors.
Table 2.
Dialysis (including in-center hemodialysis, home hemodialysis, and peritoneal dialysis) versus transplant populations
| Variable | Dialysis | In-Center Hemodialysis | Peritoneal Dialysis | Transplant |
| N | 927 | 875 | 48 | 470 |
| Age,a yr ± SD | 70±16 | 71±16 | 68±14 | 60±13 |
| Men, % | 64.9 | 64.1 | 72.5 | 63.6 |
| Admitted,a % | 76.8 | 75.1 | 94.0 | 92.9 |
| Admitted to ICU,a % | 6.0 | 6.1 | 0 | 14.9 |
| Treatment, % | ||||
| Lopinavir–ritonavir | 40.1 | 39.6 | 41.6 | 37.5 |
| Hydroxychloroquinea | 81.1 | 78.1 | 92.2 | 90.8 |
| Pulses of steroidsa | 25.1 | 25.4 | 24.4 | 52.4 |
| IFN | 4.3 | 3.5 | 12.2 | 4.8 |
| Tocilizumaba | 5.6 | 5.2 | 13.9 | 17.4 |
| Previous treatment, % | ||||
| ACEI | 12.1 | 10.6 | 19.6 | 14.8 |
| ARBa | 17.9 | 15.9 | 45.1 | 26.7 |
| Botha | 29.0 | 25.6 | 62.7 | 39.5 |
| Days of admission, d ± SD | 12±9 | 13±10 | 12±9 | 13±9 |
| Recovered,a % | 38.6 | 37.2 | 54.7 | 52.6 |
| Time to recover,a d ± SD | 18±8 | 20±9 | 16±9 | 15±8 |
| Still ill,a % | 35.1 | 35.5 | 29.6 | 24.4 |
| Death,b % | 26.3 | 27.3 | 15.7 | 23.0 |
ICU, intensive care unit; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
P<0.001.
P=0.004.
To date, 352 patients (25% of the registered patients) have died; the characteristics of these patients are disclosed in Table 3. Compared with patients who recovered, the deceased were older, more were diabetic, most of them were on IC-HD, they presented pneumonia, and they more frequently received lopinavir–ritonavir and steroids. However, only a few of them were on RAAS inhibitors. The remaining 440 patients are on follow-up.
Table 3.
Characteristics of patients who have either recovered or died (N=957), according to outcome
| Outcome | Recovered, N=605 | Deceased, N=352 | P Value |
| Age, yr | 63±16 | 74±12 | <0.001 |
| Men, % | 66.4 | 63.8 | NS |
| Diabetes, % yes | 21.9 | 31.8 | 0.003 |
| RRT modality, % | 0.005 | ||
| IC-HD | 54.5 | 66.7 | |
| PD | 4.3 | 2.0 | |
| Transplant | 40.8 | 30.7 | |
| Developed pneumonia, % | 66.1 | 90.4 | <0.001 |
| Acute treatment, % | |||
| Hydroxychloroquine | 88.1 | 84.4 | NS |
| Lopinavir–ritonavir | 36.9 | 48.7 | <0.001 |
| Steroids | 32.8 | 42.2 | 0.004 |
| Previous treatment, % | |||
| ACEI | 12.6 | 13.6 | NS |
| ARB | 24.7 | 14.8 | <0.001 |
| Both | 35.8 | 26.7 | 0.002 |
NS, not significant; IC-HD, in-center hemodialysis; PD, peritoneal dialysis; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
Finally, the number of deaths was lower in patients with Tx than in patients on dialysis. This finding was related to several factors: in patients with Tx, age and the presence of pneumonia were independently associated with mortality, and it was observed that there was a beneficial effect of the prior use of angiotensin II receptor blockers (ARBs) (Table 4). Similar data were observed in patients on dialysis: age and pneumonia were factors associated with mortality, and we observed an apparent beneficial effect of hydroxychloroquine treatment and the use of PD as dialysis modality (Table 4). Clinical recovery was observed in 605 (43%) patients; the mean elapsed time to recovery was 12±5 days. The remaining 32% continued in a situation of active infection.
Table 4.
Factors associated with mortality: Patients with transplants and patients on dialysis
| Variable | Univariate Analysis | Multivariate Analysis | ||
| Odds Ratio (95% Confidence Interval) | P Value | Odds Ratio (95% Confidence Interval) | P Value | |
| Patients with transplants | ||||
| Age | 1.12 (1.09 to 1.15) | <0.001 | 1.12 (1.08 to 1.15) | <0.001 |
| Diabetes mellitus | 2.68 (1.40 to 5.16) | 0.003 | 1.58 (0.71 to 3.53) | 0.26 |
| Gastrointestinal symptoms | 0.42 (0.25 to 0.71) | <0.001 | 0.49 (0.23 to 1.04) | 0.06 |
| Pneumonia | 4.31 (1.91 to 9.74) | <0.001 | 5.03 (1.88 to 13.48) | 0.001 |
| ARB | 0.56 (0.32 to 0.97) | 0.04 | 0.46 (0.25 to 0.87) | 0.02 |
| Patients on dialysis | ||||
| Age | 1.04 (1.03 to 1.06) | <0.001 | 1.04 (1.02 to 1.06) | <0.001 |
| Pneumonia | 5.95 (3.78 to 9.35) | <0.001 | 7.93 (4.53 to 13.90) | <0.001 |
| Hydroxychloroquine | 0.52 (0.30 to 0.92) | 0.009 | 0.54 (0.31 to 0.94) | 0.03 |
| ARB | 0.57 (0.37 to 0.89) | 0.01 | 0.66 (0.38 to 1.12) | 0.12 |
| HD (versus PD) | 2.88 (1.13 to 6.92) | 0.012 | 2.82 (1.17 to 6.81) | 0.02 |
ARB, angiotensin II receptor blocker; HD, hemodialysis; PD, peritoneal dialysis.
Discussion
The analysis of data collected during the first 6 weeks of the SEN Registry of COVID-19 showed that the SARS-CoV-2 infection affects a significant number of Spanish patients on RRT, mainly those on IC-HD. The number of hospital admissions and mortality rate were very high. In general, age and the presence of pneumonia were risk factors associated with mortality. Interestingly, in patients with Tx, the use of ARBs was associated with a lower mortality; in patients on dialysis, the use of hydroxychloroquine as well as being on PD (instead of IC-HD) was also associated with lower mortality.
According to the 2018 Spanish Registry of Renal Patients on RRT (4), 55% are kidney Tx recipients, 40% are on IC-HD, and 5% are on PD. Only a small percentage is on HHD. The mean age is 67±11 years; two-thirds are men, and diabetes is the most frequent cause of kidney disease (16%). The mean age of patients on RRT infected with SARS-CoV-2 was similar to the rest of the patients infected in Spain (4). Also, in both cohorts, the infection more frequently affects men than women (4). Even though more than half of the Spanish patients on RRT are transplanted, SARS-CoV-2 infection was more frequent in patients on IC-HD. This finding could be related to the fact that patients on IC-HD have to move to the dialysis facilities (by public transportation or ambulances) coupled with the fact that some of them live in nursing homes, conditions that increase the risk of infections. Surprisingly, patients with Tx were only one-third of infected patients, despite being, potentially, at higher risk due to immunosuppression. Finally, patients on PD and those on HHD had very low rates of infection (but it should be noted that they represent a low percentage of total patients on RRT in Spain).
In relation to clinical manifestations, these are similar to those reported in the general population of patients infected (1). In a cohort of Chinese patients, the most frequent manifestations were fever and upper respiratory tract infection. One-quarter of our patients also reported gastrointestinal symptoms, a proportion that is higher than that observed in the general population (1). Other registries referred a higher rate of these digestive symptoms (5). One explanation for these differences could be related to screening methods or diagnostic procedures of the infection.
In our patients, the rate of hospital admissions was very high compared with infected patients of the general population (6), although that paper describes the United States population. It should be taken into consideration that patients on RRT are older and have more comorbidities, resulting in a more fragile condition. A recent meta-analysis disclosed that CKD was a risk factor for developing a more severe SARS-CoV-2 infection (7). One of the possible explanations is that uremic milieu affects lymphocytic function (8). Hospital admissions were more frequent in patients with Tx than patients on dialysis, and the former also had more admissions to the intensive care unit. It could be that that immunosuppression plays a role (9).
The mortality rate was high. Patients on dialysis have a higher risk of death compared with patients with Tx, probably due to older age and more comorbidities (a variable that was not recorded). Age and the presence of pneumonia were independent risk factors associated with death. In patients on dialysis, hydroxychloroquine was associated with a lower rate of death; however, the significance of this association requires further evaluation in a large number of patients. Presently, there is controversy about the potential benefits of hydroxychloroquine administration. A recent French study found some benefit from the use of hydroxychloroquine (10); by contrast, another study from China did not find a beneficial effect (11). In our study, the effect of hydroxychloroquine was observed in patients on dialysis but not in patients with Tx. Nevertheless, our registry shows that hydroxychloroquine and other drugs commonly used in SARS-CoV-2 infection are more frequently prescribed in patients with Tx than in patients on dialysis.
This study is the first showing that patients on PD are at lower risk of SARS-CoV-2 infection than patients on IC-HD; this analysis was adjusted by age and diabetes but not by comorbidity, which may have affected the result. An analysis of the situation of PD patients has been previously published (12).
The benefit of RAAS inhibitors is also controversial. Some publications warned about the possibility that the use of these drugs may increase the risk of infection by SARS-CoV-2 (13). A recent meta-analysis suggests a beneficial effect of ARBs on the severity of SARS-CoV-2 pneumonia in elderly patients (Liu Y, Huang F, Xu J, Yang P, Qin Y, Cao M, Wang Z, Li X, Zhang S, Ye L, Lv J, Wei J, Xie T, Gao H, Xu K-F, Wang F, Liu L, Jiang C: Anti-hypertensive angiotensin II receptor blockers associated to mitigation of disease severity in elderly COVID-19 patients. https://doi.org/10.1101/2020.03.20.20039586, 2020). Presently, health authorities recommend to continue the administration of the drugs that these patients were receiving as their regular treatment (14).
This study has some limitations. It is possible that the registry did not include the total number of patients infected by SARS-CoV-2 undergoing RRT in Spain. The registry is made up of the voluntary contributions of doctors, and we are certain that most patients have been registered. It is possible that some patients on home techniques (PD, HHD, or Tx) have had the disease without symptoms, and diagnostic tests were not performed. It must be said that the pandemic continues to evolve (both in Spain and globally), and it is necessary to maintain the collection of information in order to obtain more solid conclusions.
To date and after 6 weeks of data collection in this registry, 43% of patients have recovered, and 31% continue to show active infections. During the coming weeks, there will be information available about the outcome of all patients; this will provide additional knowledge on the effects of SARS-CoV-2 in patients on RRT.
Disclosures
All authors have nothing to disclose.
Funding
None.
Supplemental Material
This article contains supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0002602020/-/DCSupplemental.
Distribution of registered cases by regions. Download Supplemental Table 1, PDF file, 80 KB (79.8KB, pdf)
Acknowledgments
We thank all the members of the Spanish Society of Nephrology for their contribution to this Registry. Without their collaboration it would not have been possible.
Author Contributions
E. Sánchez-Alvarez conceptualized the study; P. de Sequera Ortiz, M. Macía, and E. Sanchez were responsible for project administration; P. de Sequera Ortiz and E. Sanchez wrote the original draft; and M. Macía reviewed and edited the manuscript.
References
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for COVID-19 : Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708–1720, 2020. Available at: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y: Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180: 934–943, 2020. Available at: 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health , Government of Spain: Recomendaciones para el manejo, prevención y control de COVID-19 en Unidades de Diálisis, 2020. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/COVID19-hemodialisis.pdf. Accessed May 17, 2020
- 4.Durán BM: Annual report of the Spanish Registry of Renal Patients, 2018. Available at: https://senefro.org/contents/webstructure/SEN_2019_REER_modificada.pdf. Accessed May 17, 2020
- 5.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z: Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323: 1061–1069, 2020. Available at: 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, Prill M, Chai SJ, Kirley PD, Alden NB, Kawasaki B, Yousey-Hindes K, Niccolai L, Anderson EJ, Openo KP, Weigel A, Monroe ML, Ryan P, Henderson J, Kim S, Como-Sabetti K, Lynfield R, Sosin D, Torres S, Muse A, Bennett NM, Billing L, Sutton M, West N, Schaffner W, Talbot HK, Aquino C, George A, Budd A, Brammer L, Langley G, Hall AJ, Fry A: Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019-COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 69: 458–464, 2020. 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henry BM, Lippi G: Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol 52: 1193–1194, 2020. Available at: 10.1007/s11255-020-02451-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaziri ND, Pahl MV, Crum A, Norris K: Effect of uremia on structure and function of immune system. J Ren Nutr 22: 149–156, 2012. Available at: 10.1053/j.jrn.2011.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu L, Xu X, Ma K, Yang J, Guan H, Chen S, Chen Z, Chen G: Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant 20: 1859–1863, 2020. Available at: 10.1111/ajt.15869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Tissot Dupont H, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D: Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 56: 105949, 2020. Available at: 10.1016/j.ijantimicag.2020.105949 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Chen J, Liu D, Liu L, Liu P, Xu Q, Xia L, Ling Y, Huang D, Song S, Zhang D, Qian Z, Li T, Shen Y, Lu H: [A pilot study of hydroxychloroquine in treatment of patients with moderate COVID-19]. J Zhejiang Da Xue Bao Yi Xue BanUniv 49: 215–219, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sánchez-Alvarez JE, Bajo Rubio MA, Paraíso Cuevas V, López de la Manzanara V, Llópez Carratala R, Rodríguez Puyol D, Trujillo Cuéllar H, Grande Villoria J, Cuiña Barja LM: Impact of SARS-CoV-2 infection in the population on peritoneal dialysis. The Spanish experience: preliminary results. Bulletin de la Dialyse à Domicile 3: 147–154, 2020 [Google Scholar]
- 13.Sommerstein R, Gräni C: Preventing a COVID-19 pandemic: ACE inhibitors as a potential risk factor for fatal COVID-19. BMJ 368: m810, 2020 [DOI] [PubMed] [Google Scholar]
- 14.Sparks MA, Hiremath S, South A, Welling P, Luther M, Cohen J, Byrd B, Burrell LM, Battle D, Tomlinson L, Bhalla V, Soler MJ, Swaminathan S, Pettit A, Moslehi J, Bress A, Turgeon R: The coronavirus conundrum: ACE2 and hypertension edition. NephJC, 2020. Available at: http://www.nephjc.com/news/covidace2. Accessed May 17, 2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distribution of registered cases by regions. Download Supplemental Table 1, PDF file, 80 KB (79.8KB, pdf)