Introduction
The first hemodialysis (HD) in Singapore was conducted in September 1961 for acute kidney failure with the twin-coil artificial kidney. It was not until 1968 when the chronic HD program was instituted (1). Since then, the incidence and prevalence of CKD stage 5 (CKD5) and dialysis have increased significantly. The Singapore Renal Registry is maintained by the National Registry of Diseases Office. On the basis of its Annual Report 2018, the crude incidence rate of CKD5 increased from 341.5 per million population (pmp) in 2009 to 504.1 pmp in 2017 (2). Although the age-standardized incidence rate (ASIR) of CKD5 remained stable (256.6–289.2 pmp), the ASIR of dialysis increased significantly from 159.0 pmp in 2009 to 187.0 pmp in 2018 (Table 1). Eighty percent of the new patients on dialysis were aged 50–79 years in 2018, supporting the notion that the greater incidence of dialysis was related to an aging population. However, the crude incidence rate of dialysis also increased significantly for those aged 30–39 and 40–49 years over a 10-year period, which could possibly be explained by the increase in incidence of diabetes.
Table 1.
Age-standardized incidence rate of CKD stage 5 and dialysis (2)
| Year | CKD Stage 5 (Age-Standardized Incidence Rate) | Dialysis (Age-Standardized Incidence Rate) | ||
| N | Per Million Population | N | Per Million Population | |
| 2009 | 1275 | 256.5 | 769 | 159.0 |
| 2010 | 1448 | 273.8 | 741 | 144.7 |
| 2011 | 1587 | 288.9 | 903 | 169.6 |
| 2012 | 1557 | 274.0 | 921 | 169.6 |
| 2013 | 1570 | 266.7 | 978 | 171.2 |
| 2014 | 1785 | 295.0 | 1041 | 175.8 |
| 2015 | 1712 | 270.4 | 1090 | 177.7 |
| 2016 | 1925 | 290.9 | 1170 | 186.2 |
| 2017 | 1999 | 289.2 | 1174 | 179.5 |
| 2018 | — | — | 1257 | 187.0 |
CKD stage 5 is defined when serum creatinine is ≥500 μmol/L, eGFR is <15 ml/min per 1.73 m2, or RRT has been initiated for at least 6 months. —, information unavailable.
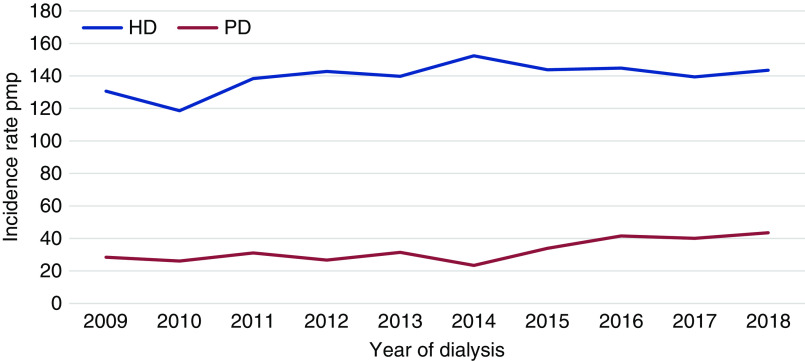
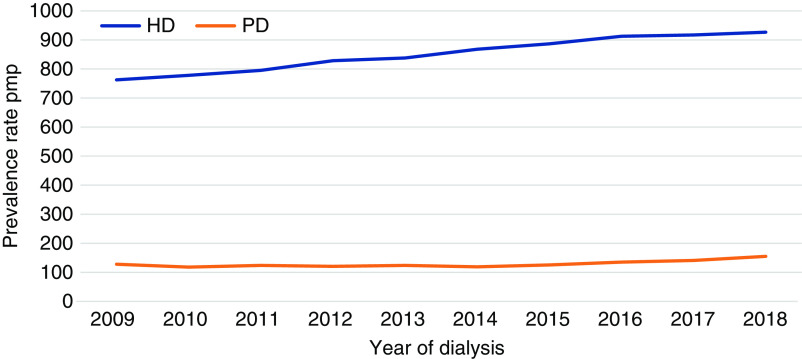
The age-standardized prevalence rate of dialysis also increased from 890.6 pmp in 2009 to 1081.7 pmp in 2018 (2). The ASIR of HD was consistently higher compared with that of peritoneal dialysis (PD). Although the ASIR for HD remained relatively stable (2), the ASIR for PD increased significantly over the years (Figure 1). Similarly, the prevalence rates of HD were consistently higher than those of PD across the years. However, the increment in age-standardized prevalence rate for HD was higher than that of PD (2) (Figure 2).
Figure 1.
Incidence rate (per million population [pmp]) of dialysis by modality from 2009 to 2018. HD, hemodialysis; PD, peritoneal dialysis. Adapted from ref. 2, with permission.
Figure 2.
Prevalence rate (pmp) of dialysis by modality. Adapted from ref. 2, with permission.
All-cause mortality for HD has been stable over the years (11.5%–13.5% from 2009 to 2018), but there was proportionally higher mortality among patients on PD, which could possibly be due to higher prevalence of diabetes mellitus in the Singapore population or patient selection bias (3).
The disparity in mortality between both modalities narrowed as the death rate fell from 22.35% in 2009 to 13.4% in 2018 for PD (2).
The incidence of CKD5 due to diabetes progressively increased over the years; 65.8% of new patients on dialysis had diabetic nephropathy, whereas 14.4% had GN in 2018 compared with 61.8% and 18.7%, respectively, in 2009 (2).
Health Care Funding and Dialysis Subsidies
Cost of Dialysis
For an average of 13 dialysis sessions a month, the cost of HD treatment in private centers starts at $2500 (United States dollar [USD] $1792)/mo, and depending on the center, it may include routine bimonthly laboratory tests. Additional charges are levied for transonic access flow measurements (where available) and administration of medications during dialysis treatments. The cost of PD treatment ranges between $1110 (USD $790)/mo and $1800 (USD $1295)/mo depending on the PD regimen, as well as the type of dialysate used.
HD and PD Subsidy
As of the first of July 2019, the Singapore government subsidizes Singapore citizens with a monthly household income of <$2800 (USD $2007) for HD on the basis of per capita household monthly income, ranging from $357 (USD $256)/mo to $1230 (USD $882)/mo (4). The PD subsidy rates per patient range from $407 (USD $292)/mo to $1280 (USD $918)/mo for per capita household monthly incomes for citizens with a monthly household income of <$2800 (USD $2007) (4).
Funding
Funding for dialysis is through a combination of cash, medical insurance, and medical savings account, and there are additional government subsidies or not-for-profit voluntary welfare organizations (VWOs) for eligible patients. These consist of the MediSave and MediShield Life schemes; private health insurance; VWOs, which include the National Kidney Foundation and the Kidney Dialysis Foundation portable funding; and Ministry of Health Subsidy. The latter three options are subject to eligibility via a household means test.
MediSave is a national health care savings scheme that can be used for patient’s own or for their dependents’ health care expenses. Each patient can withdraw up to $450 (USD $323)/mo for dialysis treatments from their MediSave accounts (4). MediShield Life is a mandatory national medical insurance scheme for all Singapore citizens and permanent residents. It is designed to help pay for part of expenses from hospitalizations and government-approved outpatient dialysis treatments. Each patient can claim up to $1000 (USD $717)/mo for dialysis treatments from MediShield Life (4).
The amount of assistance that patients can receive from VWOs is subject to financial assessments and is generally reserved for those who are financially needy. In addition, there are institution-based charity funds available for eligible patients who initiate on dialysis emergently and require financial assistance for interim HD (while awaiting approval of VWO funding). Lastly, the Civil Services Card is a government medical scheme for civil servants, pensioners, and their dependents that subsidizes some of the cost of dialysis treatments. The amount of subsidy depends on the scheme the patient is enrolled in. Under this scheme, the dialysis center will be reimbursed for the government’s share of medical bills incurred by eligible patients on dialysis at private dialysis centers.
In summary, a typical patient on dialysis will first be able to utilize his or her MediShield and MediSave for part of the dialysis cost. The remainder of payment will be either out of pocket or if the patient is eligible, subsidies from VWOs. This funding mechanism applies to both patients on HD and patients on PD.
Dialysis Practices
HD Practices
As of 2018, the majority of patients on prevalent HD were undergoing dialysis treatments at freestanding ambulatory satellite dialysis centers managed by VWOs (62.8%), followed by private dialysis centers (35.6%) and public hospitals or their affiliated dialysis centers (1.6%) (2). In 2019, the National Kidney Foundation, the largest VWO in Singapore, operated 37 dialysis centers with a total of 802 dialysis stations (5). Fresenius Medical Care in Singapore is the largest private sector provider of HD with 28 dialysis centers and 249 dialysis stations.
HD sessions are usually 4 hours of treatment time (98.6% of patients underwent thrice weekly dialysis in 2018 [2]) with a blood flow rate of 250–300 ml/min and a dialysate flow of 500–800 ml/min. Most of the freestanding ambulatory satellite dialysis centers use high-flux dialyzers, and dialyzer reuse is uncommon.
Dialysis treatments are managed by registered or enrolled nurses and nurse aides. The ratio of dialysis center staff to patient per dialysis shift is minimally 1:5, and it varies by dialysis centers (6). In-center reviews of patients on dialysis are conducted monthly by a nephrologist or a physician in charge, and laboratory tests are performed at regular 2-month intervals (Table 2). Some centers practice vascular access surveillance with a transonic access flow measurement every 3–6 months. Additionally, these patients are reviewed by their primary nephrologists bi- or triannually in their dialysis clinics to oversee their treatments received.
Table 2.
Summary of dialysis delivery in Singapore in 2018
| Characteristics | Details |
| No. of patients on dialysis | N=7405, 1081.7 pmp |
| Patients by modality, % | Hemodialysis: 86.3 |
| Peritoneal dialysis: 13.7 | |
| Dialysis centers, % | VWO: 62.8 |
| Private: 35.6 | |
| Public hospitals: 1.6 | |
| Location of dialysis center, % | Community: 98.4 |
| Institution: 1.6 | |
| Cost per hemodialysis session, USD | Approximately $150 |
| Reimbursement per dialysis session, USD | Approximately $63; not inclusive of VWO subsidy, which is dependent on means testing |
| Dialysis delivery staff | Registered/enrolled nurse |
| Nurse aides | |
| Ratio of dialysis center staff to patients | 1:5 |
| Average hemodialysis session length, h | 4 |
| Nephrologist review, times per mo | At least once a month |
pmp, per million population; VWO, voluntary welfare organization; USD, United States dollar.
Currently, there is no formal program for home HD, but there are a few patients who are doing home-based HD and are either self-assisted or nurse-assisted.
PD Practices
In 2018, 99.7% of the patients on PD were under the care of nephrologists from public hospitals and affiliated dialysis centers (2). The patients on PD are enrolled in the public hospital–respective PD programs, which are helmed by nephrologists and experienced nurses. All PD treatments are performed by the patient or their caregivers at home or by trained nursing staff in community nursing homes.
Dialysis Access
Vascular Dialysis Access
Arteriovenous fistulas (AVFs) remain the preferred vascular access of patients on HD in Singapore. These are predominantly created by vascular surgeons. Overall AVF maturation rates vary from 65.6% to 72.6%, with a median maturation time of 66–78 days (7,8).
Polytetrafluoroethylene arteriovenous grafts (AVGs) have been in use in Singapore since 1989, but graft survival was limited by infective complications during the early 1990s (9). A total of 2% to 5% of patients on HD had an AVG as an initial vascular access (7,8). The prevalence of patients dialyzing via an AVG is unknown and is institution dependent.
However, only 19.5% of patients on incident ESKD have a permanent access created prior to initiation of dialysis (7). In the authors’ institution, the majority of patients (up to 63%) are still initiated via a tunneled dialysis catheter, of which 35% are inserted by interventional nephrologists (unpublished data).
In recent years, there has been a welcomed interest in interventional nephrology, with nephrologists inserting tunneled dialysis catheters (10) and PD catheters (11) and performing endovascular interventions for AVF/AVG (12).
PD Access
PD catheter insertions were mainly performed by surgical specialties until recent years; there has been a significant rise in catheters inserted by interventional nephrologists across the country. The methods of insertion by nephrologists vary by institution, and they include percutaneous PD catheter insertion under fluoroscopy, the Y-TEC peritoneoscopic (Merit Medical) technique, and the traditional open surgical method. In the authors’ institution, >90% of the PD catheter insertions are placed percutaneously under fluoroscopy by interventional nephrologists (unpublished data).
Conclusions
Singapore has limited natural resources and land. This is further compounded by an aging population characterized by longer life expectancy and multiple comorbidities. Given the growing prevalence of dialysis, a sustainable dialysis care delivery system needs to expand in parallel to include greater infrastructure and man-power support, as well as exploring options of home-based therapies.
Disclosures
All authors have nothing to disclose.
Funding
None.
Acknowledgments
We thank Associate Prof. Boon Wee Teo (Division of Nephrology, National University Hospital, Singapore), Dr. Titus Lau (Division of Nephrology, National University Hospital, Singapore), Dr. Yue-Harn Ng (Division of Nephrology, University of Washington Medical Center), and Dr. Yong Pey See (Department of Renal Medicine, Tan Tock Seng Hospital, Singapore) for proofreading this manuscript.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Author Contributions
C. Leo conceptualized the study; C. Leo was responsible for data curation; C. Leo wrote the original draft; and G. Chan and C. Leo reviewed and edited the manuscript.
References
- 1.Pwee HS, Khoo OT: The history of dialysis in Singapore. Ann Acad Med Singapore 11: 370–373, 1982 [PubMed] [Google Scholar]
- 2.National Registry of Diseases Office: Singapore renal registry annual report 2018, 2020. Available at: https://www.nrdo.gov.sg/publications/kidney-failure. Accessed June 14, 2020
- 3.Yang F, Khin LW, Lau T, Chua HR, Vathsala A, Lee E, Luo N: Hemodialysis versus peritoneal dialysis: A comparison of survival outcomes in South-East Asian patients with end-stage renal disease. PLoS One 10: e0140195, 2015. Available at: 10.1371/journal.pone.0140195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Health Singapore: Subsidies for government funded intermediate long term care services, 2019. Available at: https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/subsidies-for-government-funded-intermediate-long-term-care-services. Accessed July 5, 2020
- 5.National Kidney Foundation: Annual report 2018, 2019. Available at: https://nkfs.org/wp-content/uploads/2019/07/NKF_Annual_Report_2018-2019.pdf. Accessed June 16, 2020
- 6.Ministry of Health Singapore: Guidelines for renal dialysis centres, 2001. Available at: https://www.moh.gov.sg/docs/librariesprovider5/licensing-terms-and-conditions/guidelines-for-private-healthcare-institutions-providing-renal-dialysis.pdf. Accessed July 5, 2020
- 7.Tan TLX, May KK, Robless PA, Ho P: Outcomes of endovascular intervention for salvage of failing hemodialysis access. Ann Vasc Dis 4: 87–92, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee KG, Chong TT, Goh N, Achudan S, Tan YL, Tan RY, Choong HL, Tan CS: Outcomes of arteriovenous fistula creation, effect of preoperative vein mapping and predictors of fistula success in incident haemodialysis patients: A single-centre experience. Nephrology (Carlton) 22: 382–387, 2017. Available at: 10.1111/nep.12788 [DOI] [PubMed] [Google Scholar]
- 9.Chia KH, Ong HS, Teoh MK, Lim TT, Tan SG: Chronic haemodialysis with PTFE arterio-venous grafts. Singapore Med J 40: 685–690, 1999 [PubMed] [Google Scholar]
- 10.Nikam M, Renaud CJ, Lee JS, Saifful SFB, Liu AYL, Lim EK, Seow YY, Yeoh LY: Outcomes of a nephrologist-driven tunnelled dialysis catheter insertion service in South East Asia. J Vasc Access 18: 279–283, 2017 [DOI] [PubMed] [Google Scholar]
- 11.Javaid MM, Lee E, Khan BA, Subramanian S: Description of an urgent-start peritoneal dialysis program in Singapore. Perit Dial Int 37: 500–502, 2017 [DOI] [PubMed] [Google Scholar]
- 12.Pang SC, Tan RY, Kwek JL, Lee KG, Foo MWY, Choong LHL, Chong TT, Tan CS: Current state of vascular access in Singapore. J Vasc Access 21: 582–588, 2020. Available at: 10.1177/1129729819878595 [DOI] [PubMed] [Google Scholar]