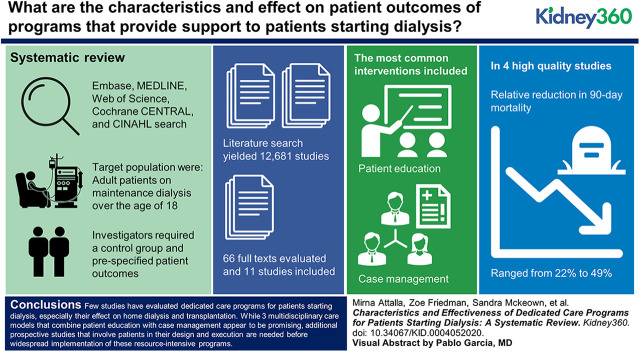
Visual Abstract
Keywords: dialysis, chronic dialysis, chronic hemodialysis, chronic kidney failure, end stage kidney disease, mortality, vascular access
Abstract
Background
Dedicated care programs that provide increased support to patients starting dialysis are increasingly being used to reduce the risk of complications. The objectives of this systematic review were to determine the characteristics of existing programs and their effect on patient outcomes.
Methods
We searched Embase, MEDLINE, Web of Science, Cochrane CENTRAL, and CINAHL from database inception to November 20, 2019 for English-language studies that evaluated dedicated care programs for adults starting maintenance dialysis in the inpatient or outpatient setting. Any study design was eligible, but we required the presence of a control group and prespecified patient outcomes. We extracted data describing the nature of the interventions, their components, and the reported benefits.
Results
The literature search yielded 12,681 studies. We evaluated 66 full texts and included 11 studies (n=6812 intervention patients); eight of the studies evaluated hemodialysis programs. All studies were observational, and there were no randomized controlled trials. The most common interventions included patient education (n=11) and case management (n=5), with nurses involved in nine programs. The most common outcomes were mortality (n=8) and vascular access (n=4), with only three studies reporting on the uptake of home dialysis and none on transplantation. We identified four high-quality studies that combined patient education and case management; in these programs, the relative reduction in 90-day mortality ranged from 22% (95% CI, −3% to 41%) to 49% (95% CI, 33% to 61%). Pooled analysis was not possible due to study heterogeneity.
Conclusions
Few studies have evaluated dedicated care programs for patients starting dialysis, especially their effect on home dialysis and transplantation. Whereas multidisciplinary care models that combine patient education with case management appear to be promising, additional prospective studies that involve patients in their design and execution are needed before widespread implementation of these resource-intensive programs.
Introduction
The transition period during dialysis initiation, particularly the first few months, is associated with increased morbidity and mortality. During this time, the hospitalization rate at 90 days approaches 1.4 admissions per patient year and the mortality rate at 180 days for patients aged >65 years is 44% (1,2). These poor outcomes after starting dialysis are multifactorial, related not only to dialysis complications but also preexisting comorbidities, cardiovascular disease, and infection (2,3). Functional status and mental health are also negatively affected (4,5), further compounding the health care needs for an increasingly elderly incident dialysis population (6). Despite dialysis initiation being a well-recognized vulnerable period for patients, nearly all dialysis programs provide similar care to both incident and prevalent patients on maintenance dialysis.
Dedicated care programs or transitional care units, which aim to provide increased support for patients starting dialysis, may improve outcomes in this high-risk group of patients. Examples of these programs have been informally described (7–9), noted to consist of structured care pathways or case management, patient education, and increased involvement from multidisciplinary health care providers (i.e., social workers, dieticians, and psychologists). The rationale for these programs and their components is that more intensive multidisciplinary care during the transition to dialysis will help optimize vascular access and laboratory parameters, as well as address lifestyle and psychosocial challenges. There may also be an opportunity to promote the benefits of home dialysis and kidney transplantation (9).
As descriptions of dedicated care programs continue to emerge, it remains unclear how these programs should be designed and organized, as well as which outcomes they might improve and the associated costs. Accordingly, the aims of this systematic review were to describe the characteristics of previously evaluated dedicated care programs for patients starting maintenance dialysis and to determine their effect on patient outcomes so as to provide guidance for other centers who wish to institute similar programs.
Materials and Methods
We reported this systematic review in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines (10). The protocol has been registered with PROSPERO (CRD42018099814).
Data Sources and Searches
We used a comprehensive search approach developed with a health sciences librarian (SM) to locate published studies. We conducted a preliminary search in Ovid Embase using a combination of text words and subject headings, followed by an analysis of relevant citations to identify other text words and subject headings. We then adapted the optimized Ovid Embase search strategy for Ovid MEDLINE, Web of Science, Ovid EBM Reviews for the Cochrane Central Register of Controlled Trials, and the Cumulative Index of Nursing and Allied Health Literature. We searched all databases from inception to March 2018, with a search update completed to November 20, 2019. We screened the reference lists of all identified articles to locate any additional studies. The complete search strategies for Ovid Embase and Ovid MEDLINE are provided in Supplemental Appendix 1.
Study Selection
The target population was adult patients on maintenance dialysis over the age of 18 with ESKD. Any study design was eligible, but we required English-language articles and the presence of a control group. We excluded unpublished conference abstracts, as well as studies that did not preferentially report data on incident patients, describe dedicated care programs (i.e., programs that provide increased support for patients on dialysis), or include patient outcomes.
We defined dedicated or transitional care programs as different models of care designed to enhance the adjustment on dialysis for new patients, which is a categorization used by others (8,9). Because of anticipated heterogeneity in the approaches to transitional care, we required the interventions to include at least one component from a taxonomy of complex and quality improvement interventions adapted from the Cochrane Effective Practice and Organizations of Care group, which have been previously described (11–13). These components included patient education, self-management, psychosocial support, health care provider education/reminders, case management, and checklists. We also prespecified a wide range of eligible patient outcomes, which included mortality, hospitalizations, quality of life, choice of kidney replacement modality (including kidney transplantation), vascular access, BP, dialysis adequacy, and laboratory parameters (e.g., hemoglobin, albumin, and phosphate).
Data Abstraction
For initial selection, two authors (MA and ZKF) scanned through the titles and abstracts. We resolved any discrepancies by discussion with the corresponding author (SAS). We reviewed selected full-text papers in detail to ensure eligibility before data abstraction. For each study, we collected data on the study details (e.g., study design, population, and inpatient/outpatient setting), patient characteristics (e.g., age, sex, and comorbidities), the nature of the interventions (e.g., target, components, and staff affected), and the measured outcomes. We assessed study quality using the Newcastle–Ottawa Quality Assessment Scale for nonrandomized studies (14). Two authors (MA and ZKF) evaluated study quality and risk of bias, with discrepancies resolved by the corresponding author (SAS).
Analysis
We qualitatively synthesized the results of all included studies, focusing on the patient population, study design, details of the intervention, and outcomes. We did not perform meta-analyses because there were too few studies to apply random effects-based methodology and the included studies were too heterogeneous to apply fixed effects-based methodology.
Results
Our search strategy yielded 12,681 unique citations. We identified six additional studies through bibliography review. We excluded 12,621 citations on the basis of title/abstract screening due to duplicate articles, reviews, nonincident population, nonrelevant interventions, lack of comparison group, or absence of patient outcomes. We then reviewed the full texts of the remaining 66 studies and excluded 55 articles due to review articles (n=9), nonincident dialysis population (n=5), nonrelevant interventions (n=30), lack of comparison group (n=6), or absence of patient outcomes (n=2); we excluded three more articles that were only available as abstracts (n=2) or did not have English-language full texts (n=1). This strategy yielded 11 studies for further analysis (15–25), which totaled 6812 intervention patients (Figure 1).
Figure 1.
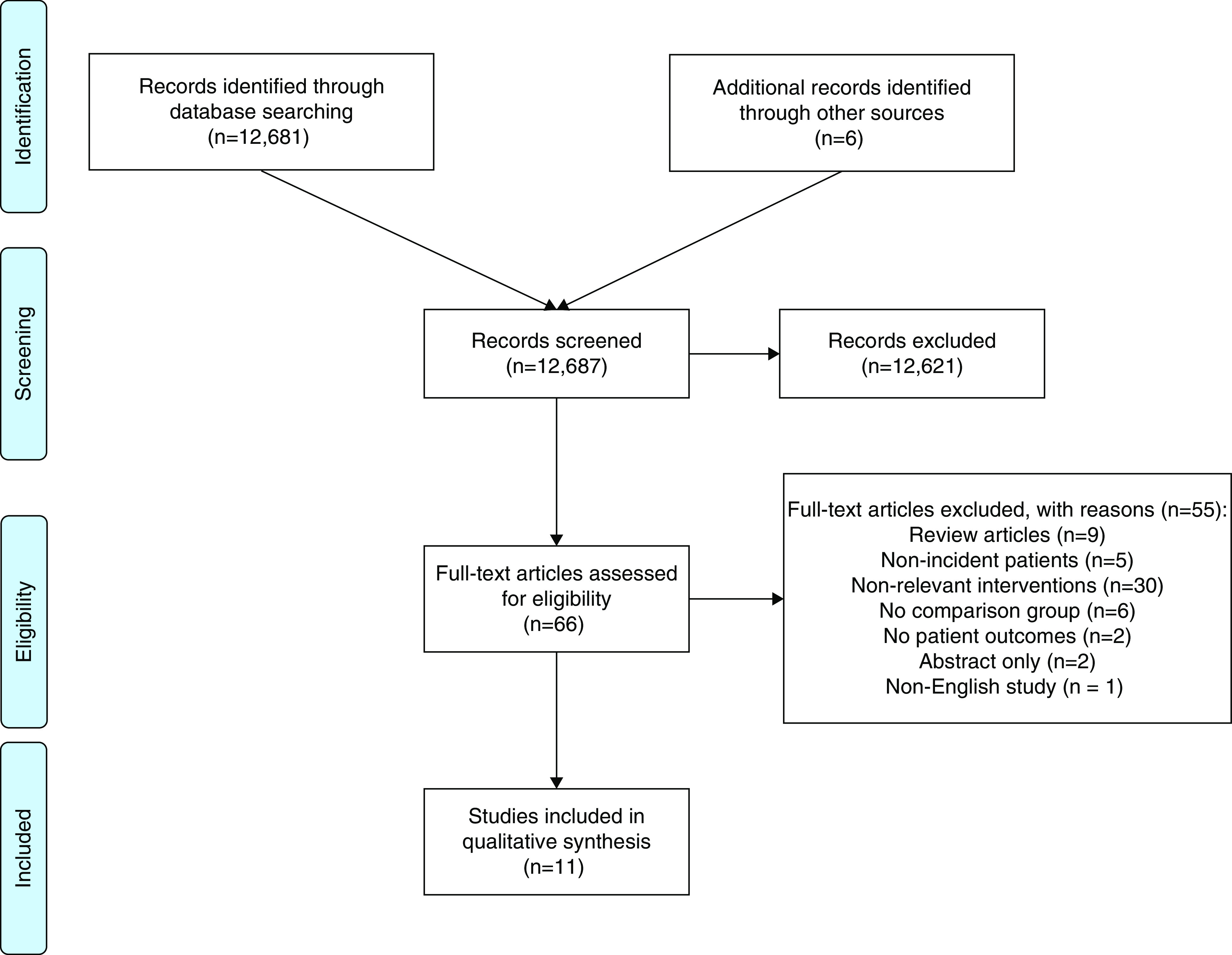
Preferred Reporting Items for Systematic Review and Meta-Analyses flow diagram of included studies.
Study Characteristics
Of the 11 programs, seven evaluated patients on hemodialysis, three evaluated patients on peritoneal dialysis, and one evaluated patients transitioning to either modality (Table 1). Only one program targeted inpatient dialysis starts (25). Most of the studies were conducted in the United States (n=6) and had retrospective designs (n=7); we did not identify any quasiexperimental or randomized trials. The median (25th/75th percentile) number of intervention patients was 341 (56–804), and only three studies included >500 patients in each group (17,20,22). The most common interventions included patient education (n=11), case management (n=5), self-management (n=4), and psychosocial support (n=4), with nurses involved in 9/11 dedicated care programs. Case management involved initial patient education followed by structured pathways and/or follow-up of modality decisions (n=4), vascular access (n=4), or laboratory parameters (n=2). The self-management and psychosocial support interventions were all combined and delivered in hemodialysis units, usually by social workers (n=3). The control groups consisted of historical (n=3) or contemporary (n=8) patients who received local standard of care, without the specialized interventions and personnel above to prioritize and specifically address the needs of incident patients.
Table 1.
Characteristics of dedicated care programs for patients new to dialysis
| Study/Country/Yr/Setting | Study Design | No. of Control Patients | No. of Intervention Patients | Mean age | Men (%) | RRT Modality | Intervention Components | Description of Control Group | Staff Required | Duration of Follow-Up | Primary Outcome | Secondary Outcomes |
| Friend et al. (15)/USA/1986/single-center hospital-based hemodialysis | Retrospective cohort | 38 | 88 | 49 | 57 | Hemodialysis | Peer support group to discuss common problems of stress, quality of life, and coping mechanisms (patient education, self-management, and psychosocial support) | Hemodialysis patients at the same facility | Multidisciplinary team members invited to attend, as needed | 5–15 yr | Mortality | None |
| Unit | ||||||||||||
| Rasgon et al. (16)/USA/1993/multiple hemodialysis units affiliated with the same health maintenance organization | Prospective cohort | 57 | 45 | 50 | 62 | Hemodialysis | Multidisciplinary patient education and social work support designed to assist patients on hemodialysis in integrating dialysis into their lives and maintaining employment (patient education, self-management, and psychosocial support) | Maintenance hemodialysis patients within the same health maintenance organization | Physician and social worker | 6 mo | Employment status | Karnofsky Scale of Physical Performance, quality of life, self-esteem, and attitude toward work |
| Wingard et al. (17)/USA/2007/multiple hemodialysis units affiliated with large dialysis organization | Prospective cohort | 1020 | 918 | 62 | 46 | Hemodialysis | Patient education program coupled with interventions focused on anemia management, adequate dialysis dose, nutrition, reduction of catheter use, review of medications, logistical support, and psychosocial assessment, as well as encouragement to participate in self-care and rehabilitation services (patient education, self-management, psychosocial support, and case management) | Hemodialysis patients in the same dialysis chain, area, and often the same physician practices | Case manager (often nurses) | 1 yr | Not specified | Mortality, hospitalization days, quality of life, dialysis knowledge, hematocrit, albumin, dialysis adequacy, and vascular access |
| Souqiyyeh et al. (18)/Saudi Arabia/2008/single-center peritoneal dialysis unit | Retrospective cohort | 64 | 312 | 46 | 50 | PD | Patient education on PD technique and telephone support after training (patient education) | Patients trained on PD at other hospitals in Saudi Arabia | Nurses | 1–3 yr | Not specified | PD technique survival, mortality |
| Hanko et al. (19)/Canada/2011/single-center hospital-based hemodialysis unit | Retrospective cohort | 42 | 36 | 59 | 63 | Hemodialysis | Standard assessment and education on home dialysis of suboptimal/late hemodialysis starts until modality plan established (patient education) | Suboptimal hemodialysis starts at the same facility | Nurse, with focus on home therapies | 6 mo | Modality selection | None |
| Lacson et al. (20)/USA/2011/large dialysis organization | Prospective cohort | 27,052 | 3165 | 63 | 57 | Hemodialysis and PD | Multiple-touch program with initial predialysis education completed in a single group class session, followed up by contact at 30, 90, and 180 d to review treatment options, inquire about kidney function/status, plan dialysis access, and provide feedback to the referring physician (patient education and case management) | Patients in the same dialysis chain | Program leaders, usually home dialysis nurse | 3 mo | Mortality, modality selection, central venous catheter use | PD uptake, vascular access |
| Ghaffari (21)/USA/2012/since-center study | Prospective cohort | 9 | 18 | 48 | 63 | PD | Standardized process by which patients without a plan for dialysis modality were started on PD, including rapid PD access placement, PD nursing education, and standardized protocols for modality selection (with recommendation), initial prescription, and prevention and management of complications (patient and provider education with case management) | Patients from the same facility started on PD nonurgently | Physician, nurse, PD access provider | 3 mo | Not specified | PD technique survival, PD complications, mortality, need for hemodialysis, dialysis adequacy, hemoglobi, iron saturation, calcium, phosphate, PTH, and albumin |
| Wilson et al. (22)/USA/2012/large hemodialysis organization | Retrospective cohort | 2424 | 1212 | 64 | 57 | Hemodialysis | Structured intake process, 90-d patient education program and management pathway, monthly monitoring of patient/facility progress (patient education, self-management, psychosocial support, and case management, checklists) | Patients in the same dialysis chain | Multidisciplinary team consisting of nephrologists, nurses, dietitians, social workers, and clinical care providers | 1 yr | Not specified | Mortality, dialysis adequacy, vascular access, hemoglobin, and albumin |
| Yu et al. (23)/China/2014/since-center study | Retrospective cohort | 249 | 370 | 44 | 60 | PD | Dedicated PD team for catheter insertion, patient education, follow-up, and continuous quality improvement (patient and provider education) | PD patients at the same facility before program implementation | Physician, nurse | 3 yr | Not specified | PD technique survival, PD complications, mortality, and cardiac morphology |
| Gill et al. (24)/Canada/2017/regional hemodialysis program | Retrospective cohort | 146 | 463 | 66 | 62 | Hemodialysis | Multidisciplinary assessment of vascular access suitability, referrals, surgery, monitoring, and surveillance, with monthly rounds to evaluate challenging patients (patient and provider education with case management) | Patients in the same region before program implementation | Physician, nurse, surgeon, interventional radiologist | 1 yr | Probability of catheter-free fistula use within 1 yr | Vascular access procedures, mortality |
| Schanz et al. (25)/Germany/2018/three hospital-based nephrology programs | Retrospective cohort | 151 | 185 | 68 | 63 | Hemodialysis | Structured, patient-centered in-hospital education program on dialysis modality; option to involve family members and peer support (patient education) | Patients at two of the three hospitals before program implementation | Nurse, with focus on home therapies | 1 yr | Modality selection | None |
PD, peritoneal dialysis; PTH, parathyroid hormone; RRT, renal replacement therapy.
There were important differences in study quality and risk of bias (Table 2). We rated six studies as high quality, five of which were published after 2005. The five low-quality studies were rated as such because they lacked comparability and failed to adjust for differences in patient case mix or potential confounders. The most common variables adjusted for in the higher-quality studies included age (n=5), sex (n=5), and diabetes (n=4), with two studies using propensity score methodology (20,22). All three studies that focused exclusively on peritoneal dialysis were rated low quality (18,21,23).
Table 2.
Newcastle–Ottawa Scale for quality assessment of nonrandomized studies
| Study | Design | Selection | Comparability | Outcome | Total Points | ||||||
| S1 | S2 | S3 | S4 | C1 | C2 | O1 | O2 | O3 | |||
| Friend et al. (15) | Retrospective cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Rasgon et al. (16) | Prospective cohort | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 |
| Wingard et al. (17) | Prospective cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Souqiyyeh et al. (18) | Retrospective cohort | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 3 |
| Hanko et al. (19) | Retrospective cohort | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 8 |
| Lacson et al. (20) | Prospective cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Ghaffari (21) | Prospective cohort | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 6 |
| Wilson et al. (22) | Retrospective cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Yu et al. (23) | Retrospective cohort | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 4 |
| Gill et al. (24) | Retrospective cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| Schanz et al. (25) | Retrospective cohort | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 6 |
For quality assessment, >7 points is considered “high quality.” S1, representativeness of exposed cohort; S2, selection of controls; S3, ascertainment of exposure; S4, outcome not present at start of study; C1/C2, design/analysis controls for important factors; O1, assessment of outcomes; O2, follow-up duration sufficient for outcomes to occur; O3, all subjects accounted for.
Study Outcomes
Only five studies specified a primary outcome (Table 1). Mortality and vascular access were the most common primary or secondary outcomes reported (mortality n=8 and vascular access n=4). Other common outcomes included dialysis adequacy (n=3), anemia parameters (n=3), nutritional parameters (n=3), and peritoneal dialysis complications/technique survival (n=3). We also identified three studies that reported on the uptake of home dialysis. Only two studies included quality of life as outcome and only one described hospitalizations, none of which were published after 2007. No study measured transplant uptake, reported costs or cost-effectiveness, or collected feedback from patients, caregivers, or staff.
We identified four high-quality studies that evaluated an effect of combined patient education and case management programs on mortality and vascular access (Table 3). In these programs, the relative reduction in 90-day mortality ranged from 22% (95% CI, −3% to 41%) to 49% (95% CI, 33% to 61%). The likelihood of achieving arteriovenous access at 90 days was more variable, with odds ratios that ranged from 0.99 (95% CI, 0.78 to 1.26) to 2.06 (95% CI, 1.88 to 2.26). The mortality results were similar in the two studies that reported 1-year outcomes. The likelihood of arteriovenous access continued to fluctuate at 1 year, with odds ratios that ranged from 1.09 (95% CI, 0.83 to 1.29) to 2.01 (95% CI, 1.72 to 2.35); however, the one study that focused exclusively on vascular access found no difference in catheter-free fistula use (odds ratio 0.87; 95% CI, 0.52 to 1.43) after introduction of a multidisciplinary assessment and monitoring process (24).
Table 3.
Mortality and vascular access outcomes for combined patient education and case management programs
| Study | Adjustment Methods | Outcomes | |
| 3 Mo | 1 Yr | ||
| Wingard et al. (17) | Cox models (mortality) | Mortality: relative riska 0.51 (95% CI, 0.39 to 0.67) | Mortality: hazard ratio 0.59 (95% CI, 0.45 to 0.79) |
| AV access: odds ratiob 0.99 (95% CI, 0.78 to 1.26) | AV access: odds ratiob 1.09 (95% CI, 0.83 to 1.29) | ||
| Lacson et al. (20) | Cox models (mortality) | Mortality: hazard ratio 0.61 (95% CI, 0.50 to 0.74) | Not reported |
| Logistic regression (AV access) | AV access: odds ratio 2.06 (95% CI, 1.88 to 2.26) | ||
| Wilson et al. (22) | Propensity-score matching | Mortality: hazard ratio 0.78 (95% CI, 0.59 to 1.03) | Mortality: hazard ratio 0.80 (95% CI, 0.67 to 0.95) |
| AV access: odds ratiob 1.10 (95% CI, 0.94 to 1.29) | AV access: odds ratiob 2.01 (95% CI, 1.72 to 2.35) | ||
| Gill et al. (24) | Cox models (mortality) | Not reported | Mortality: hazard ratio 0.94 (95% CI, 0.53 to 1.68) |
| Logistic regression (AV access) | AV access: odds ratio 0.87 (95% CI, 0.52 to 1.43) | ||
AV, arteriovenous; CI, confidence interval.
Relative risk calculated from 3-mo mortality rates.
Unadjusted odds ratios calculated from manuscript.
In the three studies that reported on the uptake of home dialysis (19,20,25), its utilization increased across three different settings. In outpatients with CKD, the odds of peritoneal dialysis increased five-fold (odds ratio 5.13; 95% CI, 3.58 to 7.35) (20). In patients who started hemodialysis in the hospital or without predialysis education, the odds of home dialysis increased four-fold (odds ratio 3.75; 95% CI, 1.08 to 13.05) (19). Last, in patients still admitted to hospital, delivery of an in-hospital education program increased the uptake of peritoneal dialysis from 0% to 15% (25). Across all settings, peritoneal dialysis was the most common home modality initiated, and the three dedicated care programs were led by home dialysis nurses/educators.
The only high-quality study that measured quality of life demonstrated improvement on the Kidney Disease Quality of Life Short Form from baseline to 6 months after starting hemodialysis (17). This test was only administered to the intervention group, but the changes in the Mental and Physical Composite Scores were statistically significant, and the 6-month scores higher than the Dialysis Outcomes and Practice Patterns Study reference scores (26).
Discussion
In this systematic review of dedicated care programs designed to support patients initiating dialysis, we found few high-quality evaluations that included patient outcomes, with most studies only reporting on mortality and vascular access. However, multidisciplinary programs that combined patient education with case management (i.e., structured care pathways usually led by dialysis nurses) during the first 3 months of dialysis did appear to achieve 20%–50% relative reductions in mortality (17,20,22). These results provide dialysis programs with multidisciplinary models of care to emulate if resources permit, but also reinforce the need for prospective interventional trials to inform care for this vulnerable population in whom over one in four patients die within 120 days of starting dialysis (27).
Our review identified an important strategy for improving early mortality that was used by large dialysis organizations with access to nurses, dieticians, social workers, and case managers: the coupling of patient education with periodic follow-up by multidisciplinary teams of dialysis staff to ensure the achievement of important care milestones (e.g., vascular access, hemodialysis adequacy, and anemia targets). A similar strategy has also been found to be effective in improving the proportion of patients with nondialysis CKD interested in home dialysis and the proportion of prevalent patients on hemodialysis who completed steps in the transplant process (28,29). These latter interventions were evaluated with randomized controlled trials, and so it would be important to further test the combination of patient education and case management in patients initiating dialysis to ensure these promising results can be reproduced in more rigorous designs outside of large dialysis organizations.
Another promising strategy that we identified involved intensive education by home dialysis nurses to promote the uptake of home dialysis (19,20,25). This strategy was effective in three different settings: (1) outpatients with CKD, (2) outpatients with ESKD categorized as suboptimal hemodialysis starts, and (3) patients still admitted to hospital. However, only 221 patients in two studies received home dialysis education after initially starting hemodialysis and multivariable adjustment in both studies was suboptimal (19,25). These results suggest that is important to include home dialysis nurses in transitional care programs, but the optimal population, setting, and timing of their engagement remains unclear.
Current efforts are underway to develop and implement care models for patients starting dialysis that specifically target home dialysis and transplantation, and combine some of the beneficial components identified in this study; that is, combined patient education and case management delivered by a multidisciplinary team of home dialysis staff (8,9,30). These preliminary reports describe 4- to 8-week programs that consist of dedicated multidisciplinary teams delivering educational curriculums and milestone-based care in a setting physically isolated from the main hemodialysis unit. Other novel, less-studied components include more frequent hemodialysis to eliminate the long-interval, hemodialysis delivery via home machines to increase patient comfort and familiarity, and early advance care planning.
To help inform these and the development of other care models for patients starting dialysis, our systematic review also identified several important knowledge gaps and potential solutions. Importantly, none of the dedicated care programs reported patient involvement or feedback in their design or execution; this may explain why we did not identify any studies focusing on patient-reported outcome/experience measures such as depression, anxiety, caregiver burden, or decisional regret. The participation of both patients and staff may help determine the necessity and feasibility of understudied dialysis unit structures (i.e., nursing ratios, social work/psychologist involvement, and caregiver and peer support) and processes (i.e., inpatient/outpatient setting, advance care planning, and more frequent dialysis). Furthermore, patients and staff can help identify the outcomes that programs should target (31,32), as care models focused on quantity of life, home dialysis, and transplantation may not require the same elements as those that focus on quality of life, mental health, or reducing hospitalizations. These decisions will also affect the patient populations most likely to benefit, and whether dedicated care programs should be available to all incident patients or reserved for high-risk patients without prior CKD education who “crash” onto dialysis.
Once these steps are undertaken, potential programs should be piloted using quality improvement principles (33), collecting data on fidelity (i.e., the program was delivered as intended), retention/comprehension of the education components, and costs. None of the studies reported the costs associated with their interventions, which may be particularly important to spreading successes to universal health care systems and smaller dialysis units. Finally, evaluation of these new interventions needs to move beyond retrospective studies toward quasiexperimental and randomized designs to build confidence that these resource-intensive efforts produce improvements in patient outcomes. Pragmatic, cluster-randomized controlled trials may be particularly well suited to achieve this objective (34,35).
The strengths of our systematic review include the use of a comprehensive search strategy that documented key components of the dedicated care programs reported in the literature, along with a broad range of prespecified patient outcomes. We also used operational definitions for the different care models to facilitate future comparisons (11–13).
Our study also has limitations. First, the high study heterogeneity and small sample size precluded quantitative analyses, and prevented any formal conclusions on the efficacy of a specific care program. Factors that contributed to heterogeneity included the nature of the interventions, descriptions of control groups, and patient outcomes. Even for similar programs (Table 3), adjustment for case-mix differences was inconsistent, which was particularly evident for the vascular access outcomes. Second, most high-quality studies that reported benefits were conducted by large dialysis organizations (17,20,22), whose results may not be generalizable to smaller programs with less resources. Third, we excluded studies without control groups so we could better compare clinical outcomes; as a result, some unique components of other dedicated care programs may have been missed. This limitation also applies to unpublished studies.
Our systematic review found that few studies have evaluated dedicated care programs for patients starting dialysis, and most only report on mortality and vascular access. Programs that combine patient education with case management that entails periodic patient follow-up toward care milestones delivered by a multidisciplinary team (including dialysis nurses) appear to be a promising strategy if resources permit, with statistically significant reductions in 90-day mortality. However, uncertainty remains on how to leverage these care models to improve other outcomes that matter to patients such as the uptake of home dialysis, transplantation, mental health, and quality of life. Given that home dialysis and transplantation are key priorities of the Advancing American Kidney Health kidney care strategy, we expect there will be several opportunities in the near future to redesign patient-centered dialysis care for incident patients (36). These efforts should involve patients, the multidisciplinary dialysis team, and pragmatic interventional trialists before widespread implementation of any resource-intensive care models.
Disclosures
All authors have nothing to disclose.
Funding
The Kidney Foundation of Canada, the Canadian Society of Nephrology, and the Canadian Institutes of Health Research cofunded a Kidney Research Scientist Core Education and National Training (KRESCENT) Program New Investigator Award (to S. Silver).
Supplemental Material
This article contains the following supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0004052020/-/DCSupplemental.
Database search strategies. Download Supplemental Appendix 1, PDF file, 89 KB (88.7KB, pdf)
Author Contributions
M. Attalla, Z. Friedman, S. McKeown, and S. Silver were responsible for data curation; M. Attalla, Z. Friedman, Z. Harel, J. Hingwala, A. Molnar, P. Norman, and S. Silver were responsible for formal analysis; M. Attalla, S. McKeown, and S. Silver were responsible for methodology; M. Attalla and Z. Friedman were responsible for project administration; S. Silver conceptualized the study and was responsible for funding acquisition, investigation, resources, software, supervision, validation, and visualization; M. Attalla, Z. Friedman, S. McKeown, P. Norman, and S. Silver wrote the original draft; and all authors reviewed, edited, and approved the final version of the submitted manuscript.
References
- 1.Wachterman MW, O’Hare AM, Rahman O-K, Lorenz KA, Marcantonio ER, Alicante GK, Kelley AS: One-year mortality after dialysis initiation among older adults. JAMA Intern Med 179: 987–990, 2019. Available at: 10.1001/jamainternmed.2019.0125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molnar AO, Moist L, Klarenbach S, Lafrance J-P, Kim SJ, Tennankore K, Perl J, Kappel J, Terner M, Gill J, Sood MM: Hospitalizations in dialysis patients in Canada: A national cohort study. Can J Kidney Health Dis 5: 2054358118780372, 2018. Available at: 10.1177/2054358118780372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biesenbach G, Hubmann R, Janko O, Schmekal B, Eichbauer-Sturm G: Predialysis management and predictors for early mortality in uremic patients who die within one year after initiation of dialysis therapy. Ren Fail 24: 197–205, 2002. Available at: 10.1081/JDI-120004096 [DOI] [PubMed] [Google Scholar]
- 4.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE: Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361: 1539–1547, 2009. Available at: 10.1056/NEJMoa0904655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knight EL, Ofsthun N, Teng M, Lazarus JM, Curhan GC: The association between mental health, physical function, and hemodialysis mortality. Kidney Int 63: 1843–1851, 2003. Available at: 10.1046/j.1523-1755.2003.00931.x [DOI] [PubMed] [Google Scholar]
- 6.Tonelli M, Riella M: Chronic kidney disease and the aging population. Nephrol Dial Transplant 29: 221–224, 2014. Available at: 10.1093/ndt/gft519 [DOI] [PubMed] [Google Scholar]
- 7.Humber River Hospital Transitional Care Unit . Available at: https://www.hrh.ca/programs/kidney-care-nephrology/. Accessed Sept 21, 2020
- 8.Bowman BT: Transitional care units: Greater than the sum of their parts. Clin J Am Soc Nephrol 14: 765–767, 2019. Available at: 10.2215/CJN.12301018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morfín JA, Yang A, Wang E, Schiller B: Transitional dialysis care units: A new approach to increase home dialysis modality uptake and patient outcomes. Semin Dial 31: 82–87, 2018. Available at: 10.1111/sdi.12651 [DOI] [PubMed] [Google Scholar]
- 10.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med 151: W65–W94, 2009. Available at: 10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- 11.Tricco AC, Ivers NM, Grimshaw JM, Moher D, Turner L, Galipeau J, Halperin I, Vachon B, Ramsay T, Manns B, Tonelli M, Shojania K: Effectiveness of quality improvement strategies on the management of diabetes: A systematic review and meta-analysis. Lancet 379: 2252–2261, 2012. Available at: 10.1016/S0140-6736(12)60480-2 [DOI] [PubMed] [Google Scholar]
- 12.Silver SA, Bell CM, Chertow GM, Shah PS, Shojania K, Wald R, Harel Z: Effectiveness of quality improvement strategies for the management of CKD: A meta-analysis. Clin J Am Soc Nephrol 12: 1601–1614, 2017. Available at: 10.2215/CJN.02490317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shojania K, Ranji S, Shaw L, Charo L, Lai J, Rushakoff R, McDonald K, Owens D: Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. AHRQ Publication No. 04-0051-2, Rockville, MD, Agency for Healthcare Research and Quality, 2004 [PubMed]
- 14.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P: Newcastle-Ottawa quality assessment scale. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed May 3, 2020
- 15.Friend R, Singletary Y, Mendell NR, Nurse H: Group participation and survival among patients with end-stage renal disease. Am J Public Health 76: 670–672, 1986. Available at: 10.2105/AJPH.76.6.670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasgon S, Schwankovsky L, James-Rogers A, Widrow L, Glick J, Butts E: An intervention for employment maintenance among blue-collar workers with end-stage renal disease. Am J Kidney Dis 22: 403–412, 1993. Available at: 10.1016/S0272-6386(12)70143-9 [DOI] [PubMed] [Google Scholar]
- 17.Wingard RL, Pupim LB, Krishnan M, Shintani A, Ikizler TA, Hakim RM: Early intervention improves mortality and hospitalization rates in incident hemodialysis patients: RightStart program. Clin J Am Soc Nephrol 2: 1170–1175, 2007. Available at: 10.2215/CJN.04261206 [DOI] [PubMed] [Google Scholar]
- 18.Souqiyyeh MZ, Al-Wakeel J, Al-Harbi A, Al-Shaebi F, Al-Kanhal F, Mousa FM, Wahdan EY, Shaheen FA: Effectiveness of a separate training center for peritoneal dialysis patients. Saudi J Kidney Dis Transpl 19: 574–582, 2008 [PubMed] [Google Scholar]
- 19.Hanko J, Jastrzebski J, Nieva C, White L, Li G, Zalunardo N: Dedication of a nurse to educating suboptimal haemodialysis starts improved transition to independent modalities of renal replacement therapy. Nephrol Dial Transplant 26: 2302–2308, 2011. Available at: 10.1093/ndt/gfq669 [DOI] [PubMed] [Google Scholar]
- 20.Lacson E Jr., Wang W, DeVries C, Leste K, Hakim RM, Lazarus M, Pulliam J: Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis 58: 235–242, 2011. Available at: 10.1053/j.ajkd.2011.04.015 [DOI] [PubMed] [Google Scholar]
- 21.Ghaffari A: Urgent-start peritoneal dialysis: A quality improvement report. Am J Kidney Dis 59: 400–408, 2012. Available at: 10.1053/j.ajkd.2011.08.034 [DOI] [PubMed] [Google Scholar]
- 22.Wilson SM, Robertson JA, Chen G, Goel P, Benner DA, Krishnan M, Mayne TJ, Nissenson AR: The IMPACT (Incident Management of Patients, Actions Centered on Treatment) program: A quality improvement approach for caring for patients initiating long-term hemodialysis. Am J Kidney Dis 60: 435–443, 2012. Available at: 10.1053/j.ajkd.2012.04.009 [DOI] [PubMed] [Google Scholar]
- 23.Yu Y, Zhou Y, Wang H, Zhou T, Li Q, Li T, Wu Y, Liu Z: Impact of continuous quality improvement initiatives on clinical outcomes in peritoneal dialysis. Perit Dial Int 34[Suppl 2]: S43–S48, 2014. Available at: 10.3747/pdi.2013.00123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gill S, Quinn R, Oliver M, Kamar F, Kabani R, Devoe D, Mysore P, Pannu N, MacRae J, Manns B, Hemmelgarn B, James M, Tonelli M, Lewin A, Liu P, Ravani P: Multi-disciplinary vascular access care and access outcomes in people starting hemodialysis therapy. Clin J Am Soc Nephrol 12: 1991–1999, 2017. Available at: 10.2215/CJN.03430317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schanz M, Ketteler M, Heck M, Dippon J, Alscher MD, Kimmel M: Impact of an in-hospital patient education program on choice of renal replacement modality in unplanned dialysis initiation. Kidney Blood Press Res 42: 865–876, 2017. Available at: 10.1159/000484531 [DOI] [PubMed] [Google Scholar]
- 26.Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F, Fukuhara S, Young EW, Kurokawa K, Saito A, Bommer J, Wolfe RA, Held PJ, Port FK: Health-related quality of life as a predictor of mortality and hospitalization: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 64: 339–349, 2003. Available at: 10.1046/j.1523-1755.2003.00072.x [DOI] [PubMed] [Google Scholar]
- 27.Robinson BM, Zhang J, Morgenstern H, Bradbury BD, Ng LJ, McCullough KP, Gillespie BW, Hakim R, Rayner H, Fort J, Akizawa T, Tentori F, Pisoni RL: Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney Int 85: 158–165, 2014. Available at: 10.1038/ki.2013.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manns BJ, Taub K, Visser M, Vanderstraeten C, Jones H, McLaughlin K: A patient-centered educational intervention to improve the utilization of self-care dialysis among predialysis patients: A randomized controlled trial. J Am Soc Nephrol 15: 135A, 2004 [Google Scholar]
- 29.Sullivan C, Leon JB, Sayre SS, Marbury M, Ivers M, Pencak JA, Bodziak KA, Hricik DE, Morrison EJ, Albert JM, Navaneethan SD, Reyes CM, Sehgal AR: Impact of navigators on completion of steps in the kidney transplant process: A randomized, controlled trial. Clin J Am Soc Nephrol 7: 1639–1645, 2012. Available at: 10.2215/CJN.11731111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bowman B, Zheng S, Yang A, Schiller B, Morfín JA, Seek M, Lockridge RS: Improving incident ESRD care via a transitional care unit. Am J Kidney Dis 72: 278–283, 2018. Available at: 10.1053/j.ajkd.2018.01.035 [DOI] [PubMed] [Google Scholar]
- 31.Urquhart-Secord R, Craig JC, Hemmelgarn B, Tam-Tham H, Manns B, Howell M, Polkinghorne KR, Kerr PG, Harris DC, Thompson S, Schick-Makaroff K, Wheeler DC, van Biesen W, Winkelmayer WC, Johnson DW, Howard K, Evangelidis N, Tong A: Patient and caregiver priorities for outcomes in hemodialysis: An international nominal group technique study. Am J Kidney Dis 68: 444–454, 2016. Available at: 10.1053/j.ajkd.2016.02.037 [DOI] [PubMed] [Google Scholar]
- 32.Manns B, Hemmelgarn B, Lillie E, Dip SC, Cyr A, Gladish M, Large C, Silverman H, Toth B, Wolfs W, Laupacis A: Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 9: 1813–1821, 2014. Available at: 10.2215/CJN.01610214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Silver SA, Harel Z, McQuillan R, Weizman AV, Thomas A, Chertow GM, Nesrallah G, Bell CM, Chan CT: How to begin a quality improvement project. Clin J Am Soc Nephrol 11: 893–900, 2016. Available at: 10.2215/CJN.11491015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee EJ, Patel A, Acedillo RR, Bachynski JC, Barrett I, Basile E, Battistella M, Benjamin D, Berry D, Blake PG, Chan P, Bohm CJ, Clemens KK, Cook C, Dember L, Dirk JS, Dixon S, Fowler E, Getchell L, Gholami N, Goldstein C, Hahn E, Hogeterp B, Huang S, Hughes M, Jardine MJ, Kalatharan S, Kilburn S, Lacson E Jr., Leonard S, Liberty C, Lindsay C, MacRae JM, Manns BJ, McCallum J, McIntyre CW, Molnar AO, Mustafa RA, Nesrallah GE, Oliver MJ, Pandes M, Pandeya S, Parmar MS, Rabin EZ, Riley J, Silver SA, Sontrop JM, Sood MM, Suri RS, Tangri N, Tascona DJ, Thomas A, Wald R, Walsh M, Weijer C, Weir MA, Vorster H, Zimmerman D, Garg AX: Cultivating innovative pragmatic cluster-randomized registry trials embedded in hemodialysis care: Workshop proceedings from 2018. Can J Kidney Health Dis 6: 2019. Available at: 10.1177/2054358119894394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dember LM: A pragmatic step forward: AKI and beyond. J Am Soc Nephrol 30: 371–372, 2019. Available at: 10.1681/ASN.2019010076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tummalapalli SL, Peralta CA: Preparing the nephrology workforce for the transformation to value-based kidney care: Needs assessment for advancing American kidney health. Clin J Am Soc Nephrol 14: 1802–1804, 2019. Available at: 10.2215/CJN.08080719 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Database search strategies. Download Supplemental Appendix 1, PDF file, 89 KB (88.7KB, pdf)