Introduction
In recent studies, 5%–20% of hospitalized patients with coronavirus disease 2019 (COVID-19) developed AKI requiring RRT (CoV-AKI-RRT) (1,2) (L. Chan et al., unpublished observations). Hypercoagulability has been recognized as a salient feature of COVID-19 in the critically ill (3,4) and there have been anecdotal accounts of unexpectedly frequent dialysis filter clotting. However, there are limited data describing the magnitude of the problem. A recent report described clotting events in 28 of 29 patients with CoV-AKI-RRT and shorter filter lifespan compared with a historical control, but no details were provided regarding anticoagulation (4). Our objective was to examine the delivery of RRT and circuit interruptions in patients with CoV-AKI-RRT in comparison with those in the pre-COVID-19 era.
Materials and Methods
With approval of the Institutional Review Board, waiver of informed consent, and in accordance with the Declaration of Helsinki, we conducted a retrospective single-center study, ancillary from our previously reported cohort (2). We identified hospitalized patients with COVID-19 (positive severe acute respiratory syndrome coronavirus 2 RNA PCR by nasopharyngeal swab) and AKI, who underwent RRT by sustained low-efficiency dialysis (SLED) for ≥8 hours in an intensive care unit between March and April of 2020 (study period: 4 weeks) by either prolonged intermittent or continuous RRT modality (5,6) using Fresenius 2008K/K2 (Bad Homburg, Germany) machines. At our hospital, continuous venovenous hemodiafiltration (CVVHDF) with PrismaFlex (Deerfield, IL) machines was restricted to the neurointensive care unit and was not expanded during the pandemic due to logistics. As pre-COVID-19 control, we included consecutive patients (reverse chronological order) with AKI without COVID-19 who underwent SLED in December of 2019. Electronic medical records were accessed and RRT flowsheets were manually reviewed to extract timing of initiation and interruption, blood flow rate (BFR), dialysate flow rate, and filter transmembrane pressure (TMP). Standard BFR was 200 ml/min and standard dialysate flow rate was 200 ml/min. After the first week of the study period, BFR was increased to 250 ml/min as an attempt to reduce the risk of circuit failure. We quantified the duration of RRT by computing the duration of each continuous uninterrupted SLED session after each initiation and the percentage of shortened SLED runs (<6 hours). Anticoagulation modalities included: none, regional citrate, prefilter heparin, minimally intensive heparin, systemic low-intensity heparin, systemic high-intensity heparin, and combined systemic high-intensity heparin plus regional citrate (Table 1).
Table 1.
Infusion protocols for each modality of anticoagulation
| Anticoagulation Regimen | Initial Bolus (U/kg) | Maximum Bolus (U) | Starting Infusion Rate | Goal aPTT (s) | Goal anti-Xa (IU/ml) | Maximum Infusion Rate |
| Regional citrate ACD-A | None | N/A | 22.4 mmol/hr (200 ml/h) | N/A | N/A | 33.6 mmol/h (300 ml/h) |
| Prefilter heparin | None | N/A | 200 U/h | None | None | 600 U/h |
| Minimally intensive heparin | None | N/A | 12 U/kg per h | 39–54 | 0.3–0.5 | None |
| Low-intensity heparin | 60 | 4000 | 12 U/kg per h | 39–69 | 0.3–0.5 | None |
| High-intensity heparin | 80 | None | 18 U/kg per h | 39–69 | 0.3–0.7 | None |
ACD-A contains 3% citrate (112 mmol/L, dextrose-sodium-citrate-citric acid 2.45–2.2 g –800 mg/100 ml solution). Heparin formulation was 25,000 units (U)/500 ml 5% dextrose solution. Dialysate calcium concentration was 1.0–2.25 mEq/L with regional citrate and 2.5–3.0 mEq/L with heparin-based anticoagulation. aPTT, activated partial thromboplastin time; ACD-A, anticoagulant dextrose citrate solution-A; N/A, not applicable.
To determine whether circuit interruption was linked to hypercoagulability or inflammation, we examined the correlation between the median duration of SLED sessions per patient and the peak D-dimer or peak C-reactive protein (CRP). As an indicator of filter clogging, we examined the changes in TMP between the beginnings and ends of the SLED runs.
Statistical analyses were performed utilizing GraphPad Prism 7 software (San Diego, CA). Proportions were compared by chi-squared test. Continuous variables were assessed by ANOVA for multiple comparisons or by paired t test or Mann–Whitney U test. P value <0.001 was deemed significant.
Results
Of 161 patients with COVID-19 and AKI, 70 underwent RRT. We excluded those treated with intermittent hemodialysis (3) or solely with CVVHDF (2) to limit heterogeneity. Of the remaining 65 patients, we excluded those with missing data or total therapy <8 hours (13). Thus, 52 patients with CoV-AKI-RRT treated with SLED were included. The median age was 60 (43–78) and 71% were Black. As control, 51 patients without COVID-19 who had AKI and were dialyzed by SLED were included. The mean body mass index was higher in the CoV-AKI-RRT cohort (Table 2). In patients with CoV-AKI-RRT, the median (interquartile range) durations of SLED/session under each anticoagulation protocol were: 4.1 hours (2.5–11.3 hours) without anticoagulation, 4.5 hours (2.5–9.3 hours) with regional citrate, 12.0 hours (3.9–17.0 hours) with prefilter heparin, 10.1 hours (4.0–20.1 hours) with minimally intensive heparin, 11.2 hours (4.2–17.0 hours) with systemic low-intensity heparin, 10.5 hours (5.3–22.0 hours) with systemic high-intensity heparin, and 12.3 hours (7.2–24.5 hours) with combined systemic high-intensity heparin plus regional citrate. As anticoagulation intensified, the duration of SLED increased (ANOVA for trend, P<0.001). In pre-COVID-19 AKI-RRT, the median (interquartile range) durations of SLED/session were: 10.5 hours (5.5–13.4 hours) without anticoagulation, 9.5 hours (3.5–13.4 hours) with regional citrate, and 20.2 hours (12.6–34.6 hours) with heparin-based protocol (prefilter or systemic high-intensity heparin) (Figure 1). The percentage of shortened runs was the highest for CoV-AKI-RRT under either no anticoagulation (62.0%) or with regional citrate (61.7%), compared with either pre-COVID-19 AKI-RRT control (23%, 36%, and 19% without anticoagulation, with citrate, or with heparin-based protocol, respectively), or CoV-AKI-RRT with heparin-based anticoagulation (28%, 36%, 28%, 28%, and 22% for prefilter, minimally intensive, systemic low-intensity, systemic high-intensity, and combined systemic high-intensity heparin plus regional citrate, respectively) (P<0.001). Overall, more patients with CoV-AKI-RRT required heparin (96% versus 10%, P<0.001). (Figure 1).
Table 2.
Baseline characteristics of study cohorts
| Control | CoV-AKI-RRT | |||
| Parameter | All (n=51) | All (n=52) | ≥1 Shortened | No Shortened |
| SLED Run (n=44) | SLED Run (n=8) | |||
| Age (yr) | 63 (33–88) | 60 (39–81) | 58 (39–80) | 71 (62–81)a |
| Sex (%) | ||||
| Men | 34 (67) | 42 (79) | 35 (80) | 5 (62) |
| Women | 17 (33) | 11 (21) | 9 (20) | 3 (38) |
| Race (%) | ||||
| Black | 14 (27) | 37 (71)b | 33 (75) | 4 (50) |
| White | 34 (67) | 13 (25)b | 10 (23) | 3 (38) |
| Hispanic | 2 (4) | 2 (4) | 1 (2) | 1 (13) |
| Asian | 1 (2) | 0 | 0 | 0 |
| BMI (kg/m2) | 32 (20–53) | 38 (24–67)b | 39 (24–67) | 33 (29–40)c |
| DM | 17 (33%) | 27 (52%) | 24 (55%) | 3 (38%) |
| CKD | 20 (39%) | 18 (35%) | 14 (32%) | 4 (50%) |
| HTN | 32 (63%) | 42 (81%) | 37 (84%) | 4 (50%)c |
Data are presented as n (%), except for age and BMI [median (range)]. CoV-AKI-RRT, patients with coronavirus disease 2019 who developed AKI requiring RRT; SLED, sustained low efficiency dialysis; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension.
P<0.01 versus ≥1 shortened run group.
P<0.001 versus control.
P<0.05 versus ≥1 shortened run group.
Figure 1.
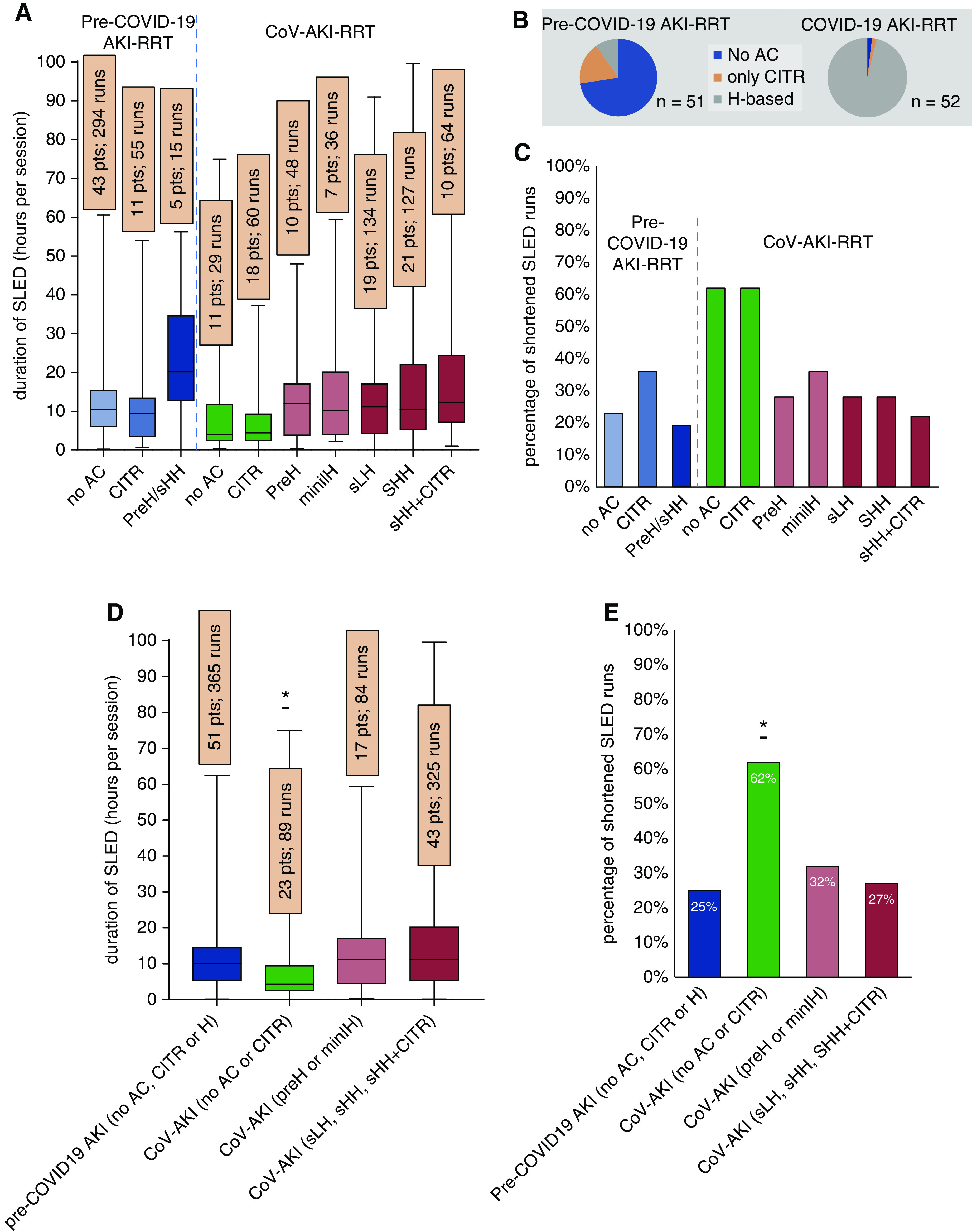
Duration of sustained low-efficiency dialysis (SLED) sessions in patients with pre-COVID-19 control AKI requiring dialysis (AKI-RRT) (n=51) and patients with coronavirus disease 2019 (COVID-19) and AKI-RRT (CoV-AKI-RRT) (n=52). (A) Distribution of duration of individual SLED sessions according to anticoagulation (AC) protocol. For pre-COVID-19 control AKI: no AC, regional citrate (CITR), and prefilter heparin (preH)/systemic high-intensity heparin (sHH). For CoV-AKI-RRT, no AC, CITR, preH, minimally intensive heparin (miniIH), systemic low-intensity heparin (sLH), sHH, and sHH + CITR. (B) Distribution of mode of AC [none, CITR, or heparin-based (H-based)] in AKI-RRT before versus during COVID-19. (C) Proportion of patients with shortened SLED runs (<6 hours). (D) Distribution of duration of individual SLED sessions grouped in four categories: data for pre-COVID-19 control AKI-RRT combine sessions with either no AC, with CITR, or with either preH or sHH. Data for CoV-AKI-RRT are presented grouped per intensity of AC: no AC or CITR; preH or minIH; and sLH, sHH, or sHH + CITR; * P<0.001 (ANOVA). (E) Proportion of patients per category with shortened SLED sessions (<6 hours); * P<0.001 (chi square).
Bleeding complications occurred in 23% patients with CoV-AKI-RRT compared with 10% in the pre-COVID-19 group (P<0.001). To determine whether subtherapeutic anticoagulation affected the results, we examined the relationship between activated partial thromboplastin time (aPTT) or anti-Xa levels within SLED runs (±3 hours) and filter life. Among 334 long SLED runs (lasting ≥6 hours), 145 (43%) were therapeutic/supratherapeutic, 82 (25%) were subtherapeutic, and 107 (32%) had no aPTT/anti-Xa available. Among 164 shortened SLED runs, 22 (13%) were therapeutic/supratherapeutic, 43 (26%) were subtherapeutic, and 99 (60%) had no aPTT/anti-Xa available. Assessing only runs with available data, the proportion of subtherapeutic runs was greater for the shortened SLED runs [43/65 (66%) versus 82/227 (35%), P<0.001].
Within the CoV-AKI-RRT group, no association was found between peak D-dimer and duration of SLED sessions (r=0.01, P=0.87). However, higher CRP significantly correlated with shorter SLED sessions (r=−0.34, P=0.013) (Figure 2). TMP data were available for 305 (61%) out of the 498 SLED runs. We observed a significantly faster rise in TMP in the shortened runs (10.1 versus 2.3 mm Hg/h between the start of a session and the time of interruption, P=0.0024) (Figure 2).
Figure 2.
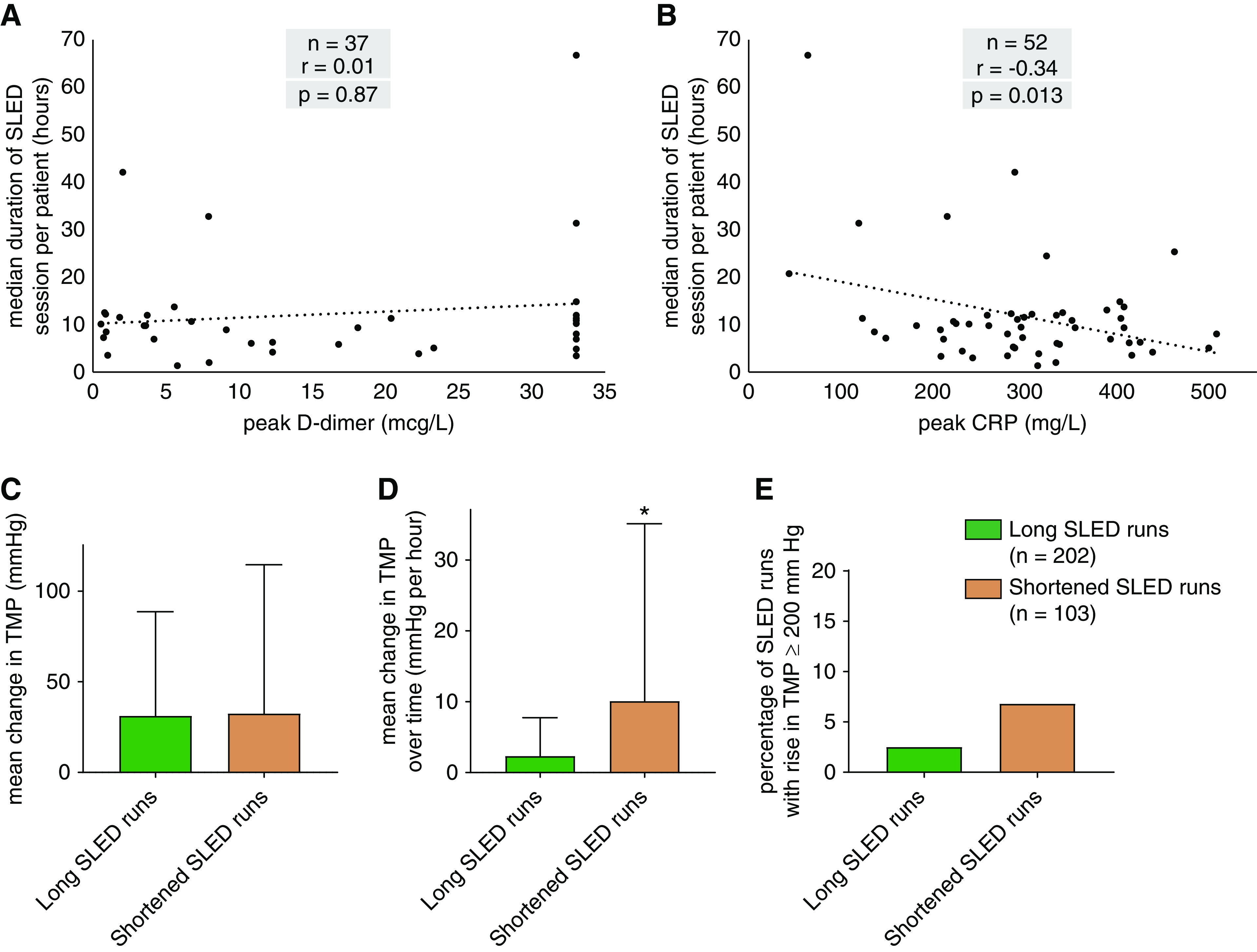
Relationship between markers of thrombogenicity and inflammation and dialysis circuit interruptions in patients with CoV-AKI-RRT. (A) Correlation between peak D-dimer value and median duration of SLED sessions (NS). (B) Correlation between peak C-reactive protein (CRP) value and median duration of SLED sessions (significant). (C–E) Comparison of changes in intradialyzer transmembrane pressure (TMP) during long (lasting ≥6 hours) and shortened SLED runs represented by mean change in TMP (C), mean change in TMP over time (D), and proportion of SLED runs with rise in TMP ≥200 mm Hg (E). * P<0.001.
Discussion
Our findings demonstrate that patients with CoV-AKI-RRT are affected by a shorter duration of runs of prolonged intermittent/continuous RRT due to loss of patency of the dialysis circuit. Execution of SLED under either no anticoagulation or with regional citrate was significantly halted in patients with CoV-AKI-RRT compared with what was observed in patients with AKI-RRT treated during the pre-COVID-19 era. With escalation to heparin-based anticoagulation, filter lives were restored. These findings suggest that systemic heparin may be more effective than regional citrate in maintaining circuit lifespan in patients with CoV-AKI-RRT treated with SLED. Because heparin and citrate interfere with different steps in the coagulation cascade (7), a difference in therapeutic effect is plausible. Anticoagulation with prefilter heparin and combined systemic high-intensity heparin and regional citrate were associated with numerically longer median duration of SLED sessions, and fewer shortened SLED runs. However, the therapeutic advantages of such protocols will require prospective examination. Although subtherapeutic runs were more common during shortened SLED runs, aPTT/anti-Xa data were missing in 60% of the shortened SLED runs, thus limiting room for interpretation.
The partial efficacy of heparin-based anticoagulation was an indirect demonstration that hypercoagulability played a role in the shortened duration of RRT. Unexpectedly, we did not find a correlation between the magnitude of D-dimer elevation and shortened RRT sessions. However, other markers of thrombosis, such as antithrombin III and factor VIII, were not measured. Thus, a link between hypercoagulability and circuit interruptions cannot be discounted. Interestingly, the correlation of higher CRP with shorter SLED runs suggests a connection between hyperinflammation in patients with COVID-19 and circuit interruptions. Elevated CRP and acute-phase inflammation have been linked to hyperviscosity (8), and the latter has been recognized in critically ill patients with COVID-19 (9). Cytokines and Igs are thought to promote rapid protein layering and clogging of dialysis filters, a phenomenon that mechanistically differs from clotting (6,10). A progressive rise in TMP during a SLED run is a parameter indicative of filter clogging (11). Indeed, we observed that the TMP increased faster during the shortened SLED sessions. Thus, we speculate that, in addition to thrombogenicity, hyperinflammation and filter clogging may explain the shortened SLED runs in patients with CoV-AKI-RRT.
This study has limitations. The use of a historical control may not account for the intensiveness of care during the COVID-19 pandemic. Conversely, COVID-19-related contact precautions may have limited nurses in promptly responding to alarms and addressing positioning and access issues. Our institutional regional citrate anticoagulation protocol differs from those conventionally used in CVVHDF by lacking monitoring of circuit ionized calcium (12). It is possible that a regional citrate protocol with monitoring of circuit ionized calcium could have been more effective. However, the same protocol was successfully utilized in our SLED platform during the pre-COVID-19 era. Although the duration of SLED sessions was used as marker of filter life, other factors such as catheter malfunction, hemodynamic instability, and performance of procedures could have accounted for circuit interruptions (13,14). However, most of the shortened SLED runs were charted as “clotting” in the flowsheets. Another caveat is that the state of inflammation and thrombogenicity may have increased over time as patients became more critically ill. Nevertheless, this factor could have biased the results in favor of the less-aggressive anticoagulation schemes that were instituted earlier (none or regional citrate), thus further validating our findings.
In conclusion, CoV-AKI-RRT was associated with shorter duration of SLED sessions compared with those of a pre-COVID-19 AKI-RRT cohort. The shorter dialysis circuit lifespan was likely driven by increased filter clotting and clogging due to hyperinflammation. Heparin-based anticoagulation with or without regional citrate in CoV-AKI-RRT were successful in restoring the duration of RRT back to that observed in patients with AKI-RRT in the pre-COVID-19 era, but was associated with greater incidence of bleeding complications. Prospective studies are required to better define the optimal anticoagulation scheme in CoV-AKI-RRT.
Disclosures
J.C.Q. Velez has participated in Advisory Board meetings for Mallinckrodt Pharmaceuticals and Retrophin, and in a Speaker Bureau for Otsuka Pharmaceuticals. None of the products related to those engagements are discussed in this manuscript. All remaining authors have nothing to disclose.
Funding
None.
Author Contributions
I. Lukitsch, J.C.Q. Velez, and Y. Wen conceptualized the study; J.R. LeDoux, M. Mohamed, D. Mundy, A. Ramanand, K. Scharwath, J.C.Q. Velez, and Y. Wen were responsible for data curation; J.R. LeDoux, M. Mohamed, A. Ramanand, J.C.Q. Velez, and Y. Wen were responsible for investigation; J.R. LeDoux and J.C.Q. Velez were responsible for methodology; M. Mohamed and J.C.Q. Velez were responsible for project administration; J.R. LeDoux was responsible for resources; J.R. LeDoux, I. Lukitsch, and J.C.Q. Velez were responsible for supervision; A. Ramanand and J.C.Q. Velez were responsible for visualization; J.C.Q. Velez was responsible for software; J.C.Q. Velez and Y. Wen were responsible for formal analysis and writing the original draft; and all authors were responsible for validation and reviewing and editing the manuscript.
Footnotes
See related editorial, “Dialysis Filter Life in COVID-19: Early Lessons from the Pandemic,“ on pages 1334–1336.
References
- 1.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, Hazzan AD, Fishbane S, Jhaveri KD; Northwell COVID-19 Research Consortium; Northwell Nephrology COVID-19 Research Consortium: Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 98: 209–218, 2020. 10.1016/j.kint.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohamed MMB, Lukitsch I, Torres-Ortiz AE, Walker JB, Varghese V, Hernandez-Arroyo CF, Alqudsi M, LeDoux JR, Velez JCQ: Acute kidney injury associated with coronavirus disease 2019 in urban New Orleans. Kidney360 1: 614–622, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H: Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 191: 145–147, 2020. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, Merdji H, Clere-Jehl R, Schenck M, Fagot Gandet F, Fafi-Kremer S, Castelain V, Schneider F, Grunebaum L, Anglés-Cano E, Sattler L, Mertes PM, Meziani F; CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis): High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med 46: 1089–1098, 2020. 10.1007/s00134-020-06062-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edrees F, Li T, Vijayan A: Prolonged intermittent renal replacement therapy. Adv Chronic Kidney Dis 23: 195–202, 2016. 10.1053/j.ackd.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 6.Connor MJ Jr, Karakala N: Continuous renal replacement therapy: Reviewing current best practice to provide high-quality extracorporeal therapy to critically ill patients. Adv Chronic Kidney Dis 24: 213–218, 2017. 10.1053/j.ackd.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 7.Weiss R, Fischer MB, Weber V: The impact of citrate concentration on adhesion of platelets and leukocytes to adsorbents in whole blood lipoprotein apheresis. J Clin Apher 32: 375–383, 2017. 10.1002/jca.21519 [DOI] [PubMed] [Google Scholar]
- 8.Nwose EU: Whole blood viscosity assessment issues IV: Prevalence in acute phase inflammation. N Am J Med Sci 2: 353–358, 2010. 10.4297/najms.2010.2353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maier CL, Truong AD, Auld SC, Polly DM, Tanksley CL, Duncan A: COVID-19-associated hyperviscosity: A link between inflammation and thrombophilia? Lancet 395: 1758–1759, 2020. 10.1016/S0140-6736(20)31209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dana AP, Ahmar CA, Clapp WL, Ross EA: A new form of myeloma “kidney”: Shortened hemofilter survival and implications for membrane filtration plasmapheresis. Clin Nephrol 75: 120–124, 2011. 10.5414/CNP75120 [DOI] [PubMed] [Google Scholar]
- 11.Honore PM, Spapen HD: What a clinician should know about a renal replacement membrane? J Transl Int Med 6: 62–65, 2018. 10.2478/jtim-2018-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tolwani AJ, Prendergast MB, Speer RR, Stofan BS, Wille KM: A practical citrate anticoagulation continuous venovenous hemodiafiltration protocol for metabolic control and high solute clearance. Clin J Am Soc Nephrol 1: 79–87, 2006. 10.2215/CJN.00040505 [DOI] [PubMed] [Google Scholar]
- 13.Baldwin I, Jones D, Carty P, Fealy N: Continuous renal replacement therapy without anticoagulation: Top ten tips to prevent clotting. Blood Purif 49: 490–495, 2020. 10.1159/000505260 [DOI] [PubMed] [Google Scholar]
- 14.Dunn WJ, Sriram S: Filter lifespan in critically ill adults receiving continuous renal replacement therapy: The effect of patient and treatment-related variables. Crit Care Resusc 16: 225–231, 2014 [PubMed] [Google Scholar]


