Introduction
The number of patients with CKD has been increasing worldwide. In Thailand, 11.6 million (17.5%) people currently have CKD, 5.7 million (8.6%) have advanced CKD (stages 3–5), and over 0.1 million require dialysis (1). Every year, >20,000 people with ESKD need treatment with hemodialysis (HD) or peritoneal dialysis (PD) (2). Since the first HD performed in 1964 and the first PD performed in 1982, the number of Thai patients treated with dialysis only gradually increased in the first three decades because of limited access arising from prohibitive costs, which precipitated catastrophic health expenditure for many families. In 2008, the Thai government extended the scope of healthcare coverage to include RRT by launching the “PD First” policy. This provided Thai citizens with universal health coverage for dialysis, such that the numbers of dialyzed patients and dialysis centers increased exponentially. This short review elaborates on the principle of the “PD First” policy and three reimbursement schemes, and how they have challenged and influenced dialysis treatment in Thailand. The review also focuses on dialysis management and outcomes in Thailand.
Overview of Thailand and Its Health Care System
Located in the middle of mainland Southeast Asia, Thailand is an agricultural country divided into 77 provinces, with a current population of 66.5 million (3). One sixth of citizens live in the Bangkok metropolitan region. According to World Bank records, Thailand is classified as an upper-middle-income country, which has spent 6.5% of its gross domestic product on health (4). Currently, there are three government health insurance schemes with different features and administrative management. Firstly, the Civil Servant Medical Beneficiary System (CSMBS), under the Ministry of Finance, covers 7 million civil servants and their immediate family members. Secondly, the Social Security System (SSS), which is administered by the Social Security Office, Ministry of Labor, provides support for 14.6 million employees. The funding for this scheme originates from tripartite contributions, including employers, employees, and the government. Lastly, the Universal Coverage Scheme (UCS), which is also known as the “30 Bahts (1 U.S. Dollar) Scheme,” managed by the National Health Security Office, supports 48.8 million remaining citizens, who are mostly the lower-income population (5).
The Policy of Care for Patients with ESKD
The CSMBS has provided support for RRT since 1998 (6), whereas the SSS expanded its coverage to include dialysis in 2003 (7). Although the UCS was introduced in 2002, the compensation for RRT became established in 2008 (8). Under the UCS, patients who are suitable for PD can decline PD and choose HD as the first-line treatment, but they have to fully self-fund for dialysis-related costs. On the other hand, patients who are not suitable for PD because of a PD contraindication or a history of PD technique failure are able to access HD without additional payment. In comparison, the CSMBS and the SSS support both modalities depending on the patient’s preference (9). Thus, a proportion of the dialysis modality is varied according to the reimbursement scheme. For those patients under the CSMBS, 91% are on HD and 9% are on PD. It is similar for the SSS, with 95% and 5% on HD and PD, respectively. In contrast, PD is the predominant dialysis modality under the UCS, with 65% of patients on PD and the rest are on HD (2). It is important to note that funding of kidney care medications, including erythropoiesis-stimulating agents, iron supplements, and calcimimetic agents, is fully supported by the policy if the drugs are on the Thai National Medication List.
Current ESKD Situations in Thailand
The incidence rate of treated ESKD in Thailand has been increasing since the launch of the “PD First” policy. In 2008, the incidence rate was 100 per million population/year and expanded to 346 per million population/year in 2016 (10). According to the United States Rena Data System annual report in 2018, Thailand was in the top five countries with the highest incidence rates of treated ESKD (10). The most common cause of ESKD is diabetic nephropathy (39%), followed by hypertension (31%), obstructive nephropathy (4%), and established/presumed GN (2%) (2). The national PD penetration is now 31% and 46% of all prevalent and incident dialysis patients, respectively, compared with <10% before 2008 (2) (Figure 1). Regional differences in the relative uptake of PD modality have also been noted, ranging from 17% in the Bangkok metropolitan region to 37% in rural regions. HD patients have a relatively higher income than PD patients (165–1650 versus 35–660 USD/month, respectively) but a slightly higher unemployment rate (29% versus 26%, respectively) (2). Comparisons of prevalence, cost, and dialysis modalities among Asia countries are demonstrated in Table 1.
Figure 1.
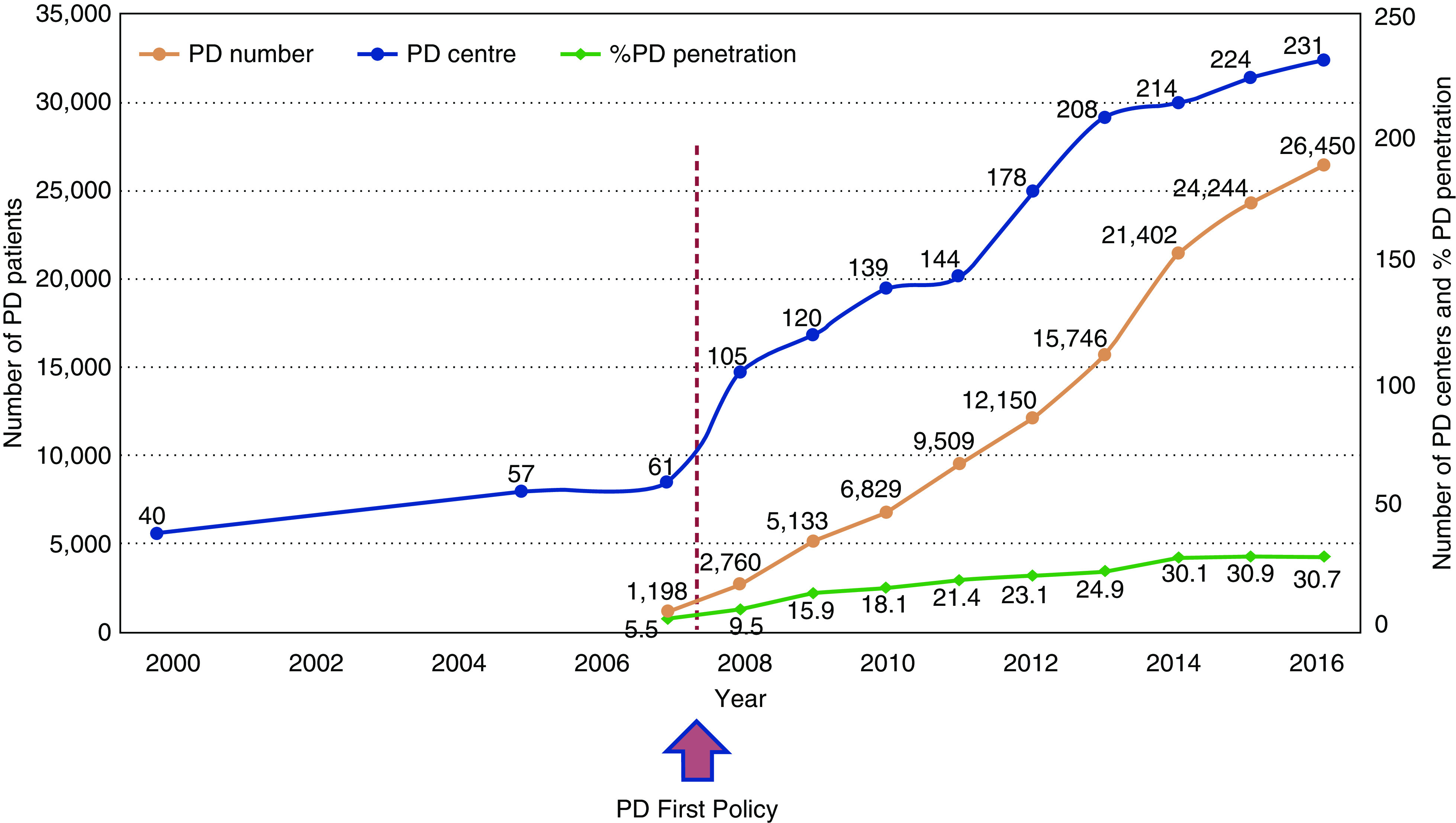
Peritoneal dialysis (PD) number and %PD penetration were derived from prevalent dialysis patient.
Table 1.
Comparison of prevalence, dialysis modality, and cost of hemodialysis in Asia ( 11 )
| Country | Prevalence of Dialysis Patients (pmp) | In-Center Hemodialysis (%) | Home Hemodialysis (%) | Peritoneal Dialysis (%) | Policy | Cost Per Session of Hemodialysis in Public Center (U.S. Dollars) |
| Hong Kong | 818 | 26 | 3 | 71 | Government funded 100%; PD First policy | 13 |
| Indonesia | 320 | 99 | 0 | 1 | Government and self-funded | 60–80 |
| Japan | 2532 | 97 | 0 | 3 | Government funded 100% | 210 |
| Jordan | 511 | 97 | 0 | 3 | Government and self-funded | 80 |
| Malaysia | 1295 | 90 | 1 | 9 | Government and self-funded | 13 |
| Singapore | 1695 | 88 | 0 | 12 | Government and self-funded | 1875/mo |
| South Korea | 1820 | 91 | 0 | 9 | Government and self-funded | 136 |
| Taiwan | 3251 | 91 | 0 | 9 | Government funded 100% | 88 |
| Thailand | 1392 | 72 | 0 | 28 | Government and self-funded; PD first policy | 60 |
pmp, per million population; PD, peritoneal dialysis.
HD Practices in Thailand
Of a total of 674 HD centers, about one quarter are located in the Bangkok metropolitan region (2). The private sector has the highest proportion of HD centers, accounting for 52%, followed by government and not-for-profit nongovernment organizations (46% and 2%, respectively) (2). A nephrologist is in charge of determining each individual patient’s treatment plan and evaluating the patient at least twice a month. However, during each HD session, either a nephrologist or internist is required to be present in the dialysis unit. Only certified HD nurses are authorized to perform patient care, whereas technicians are not (2) (Table 2).
Table 2.
| Characteristics | Hemodialysis | Peritoneal Dialysis |
| Number of dialysis patients | 67,956 (1002 pmp) | 26,450 (390 pmp) |
| Incidence rate of dialysis | 12,682 (187 pmp) | 10,783 (159 ppm) |
| Age, yr | 58±15 | 56±14 |
| Men | 53% | 49% |
| Residence in Bangkok metropolitan region | 32% | 14% |
| Health insurance scheme | CSMBS (38%), UCS (25%), SSS (19%), others (e.g. charity organization or self-payment) (18%) | UCS (89%), CSMBS (8%), SSS (2%), others (e.g. charity organization or self-payment) (3%) |
| Dialysis modalities | In-center HD (100%) | CAPD (97%), APD (3%) |
| Unit structure | Both hospital-based and free-standing units | All hospital-based, but one free-standing unit |
| Unit financial features | Both profit and nonprofit units | All nonprofit units, but one private unit |
| Staff who deliver dialysis | Certified HD nurse | Certified PD nurse (100%) with routine multidisciplinary review (46%) |
| Typical patient-to-HD nurse ratio | 4:1 | 39:1 |
| Nephrologist visit | Twice a mo (during dialysis session) | 2–4 mo |
| Access | AVF (65%), AVG (20%), and central venous catheter (15%) | Double-cuffed TK catheter (51% curled, 42% straight, 2% other, and 5% unknown) |
| Dialysis prescription and length of dialysis session | Frequency (2–3 sessions/wk), dialysis time (4 h/session), session length (240 min), blood flow rate (300–350 ml/min), and dialysis flow rate (500–550 ml/min) | CAPD: 4×2 L/d, 28% with any, 2.27% or 3.86% use |
| APD: CCPD (81%, 10 L/d), NIPD (19%, 12–14 L/d) | ||
| Cost | CSMBS: 67 USD/session, SSS: 50 USD/session (up to 150 USD/wk), UCS: 50 USD/session (cap) | CAPD: 500 USD/mo |
| APD: 1500 USD/mo |
pmp, per million population; CSMBS, Civil Servant Medical Beneficiary System; UCS, Universal Coverage Scheme; SSS, Social Security System; HD, hemodialysis; CAPD, continuous ambulatory PD; APD, automated peritoneal dialysis; PD, peritoneal dialysis; AVF, arteriovenous fistula; AVG, arteriovenous graft; CCPD, continuous cyclic peritoneal dialysis; NIPD, nightly intermittent peritoneal dialysis; TK, Tenckhoff catheter; USD, U.S. Dollars.
The prescription of HD in Thailand is typically 2–3 times per week with bicarbonate dialysate (2) (Table 2). Dialysis bloodlines are disposable, whereas dialyzer reuse is commonly practiced in Thailand (2). Online HDF is available in large hospitals, located in the Bangkok metropolitan region and other large cities. Home HD is unavailable at present. The feed water for dialysis is generally sourced from a municipal water supply, although it is occasionally derived from an alternative source (e.g., groundwater). Although all HD centers utilize standard water purification processes, including reverse osmosis systems, water quality remains a considerable challenge. Municipal water is often affected by climatic and environmental conditions, such as drought, and groundwater is frequently contaminated with trace elements and inorganic ions. Regular monitoring of organic and inorganic contaminants in reverse osmosis water and dialysate is therefore essential, and is guided by the Thailand Hemodialysis Clinical Practice Recommendation 2014 (13). To assure high-quality HD performance of the centers, the National Dialysis Accreditation Commission, Medical Council of Thailand periodically evaluates the centers by utilizing four different metrics, including treatment audits, technical inspection, HD nurse certification, and state license endorsement for newly commissioned facilities after an accreditation process.
The prevalence of chronic hepatitis B and hepatitis C virus infections is 4% and 3.7%, respectively (2), and HIV infection is rare, possibly because of a high level of HIV-related stigma among HD facilities. Currently, there are 161 HD patients with HIV-infection (2), However, the national guideline (13) does not recommend using dedicated dialysis machines for patients with bloodborne infections and suggests only isolating hepatitis B virus-infected HD patients. The guideline encourages the use of standard precautions (especially handwashing and changing gloves between patients), periodic serologic testing of patients and staff, and cleaning of dialysis machines and blood-contaminated areas with 0.5%–1.0% sodium hypochlorite solutions (13). A nationwide survey has demonstrated that Thai HD patients receive an adequate dose of HD and adequate nutritional needs, with an average single pooled Kt/V of 1.7, a normalized protein catabolic rate of 1.2 g/kg per day, and a serum albumin level of 3.7 g/dl (8). The average cost per session of HD is 60 USD, but varies according to the patient's scheme coverage and facility affiliation (2). The CSMBS and SSS subsidies are 60–67 USD for each session, whereas the UCS subsidy is 50 USD/session (2).
PD in Thailand
Under the “PD First” policy, the National Health Security Office is responsible for the delivery of overall inpatient and outpatient PD care and a home delivery PD bag (up to five PD bags daily). There are no out-of-pocket expenses for the patient unless they choose to have automated PD or nonglucose-based solutions, including icodextrin and low-glucose degradation product solutions. PD solutions are made by international brands, but are locally or regionally manufactured. The Government Pharmaceutical Organization is responsible for national procurement. The products are distributed mainly by the Thailand Post Co., Ltd, whereas local logistics companies are subcontracted for the patients residing in rural areas. Under the policy, erythropoietin is capped at 4000 units twice weekly. Over the decade that the “PD First” policy has been in place, the numbers of continuous ambulatory PD patients and centers have grown exponentially (Figure 1). Almost 90% of PD patients are under the UCS (2). Almost all facilities are affiliated with public/governmental hospitals, although one PD center is owned by an autonomous public organization and one center is a private clinic. Thai PD facilities are large, with an average of 102 (interquartile range: 48–208) PD patients per facility (14), and have low automated PD penetration (5%) (12). The physician-to-patient ratio is 1:64, whereas the PD nurse-to-patient ratio is 1:39 (12). According to results of the Thailand Peritoneal Dialysis Outcomes and Practice Patterns Study, one half of Thai PD patients have caregivers who assist with PD bag exchanges (56%), which likely reflects the high prevalence of functional impairment in PD patients (47%) (12).
PD-related infection is the leading cause of technique failure and death in Thai PD patients. In 2016, the crude peritonitis rate was 0.40 episodes/year, and the median facility peritonitis rate was 0.43 episodes/year (14). Only 18% failed to achieve the International Society for PD Guideline 2016 target of fewer than 0.5 episodes/year (14). The Gram-negative rate has overtaken the Gram-positive bacterial peritonitis rate (0.12 versus 0.10 episodes/year) (14), and there is a notably high culture-negative peritonitis rate in Thailand (0.11 episodes/year) accounting for 28% of all peritonitis episodes (14). However, the patient and technique survival rates have improved substantially. In 2016, the 1- and 5-year patient survival rates of PD patients were 83% and 54%, respectively (15). In addition, the technique survival rates (censored for death and kidney transplantation) were 95% and 81% in the first and fifth years of PD, respectively (15).
Kidney Transplantation in Thailand
The first kidney transplantation was performed in 1975. Since 2008, there has been health insurance scheme support for kidney transplant expenses. As of December 2018, there were 5360 prevalent cases (44% living donor and 56% deceased donor transplants) and 670 incident (25% living-donor and 75% deceased-donor transplants) cases (16). Both patient and graft survival rates have steadily improved, such that 5-year graft survival rates in living and deceased donor kidney transplant recipients have increased from 86% and 82% in 2000 to 93% and 88% in 2015, respectively (17). Infection is the leading cause of death, accounting for 47% of all deaths, followed by cardiovascular disease (27%) (16).
Future Challenges
The high incidence rates of CKD and ESKD in Thailand raise important national concerns regarding the sustainability of health financing and health care service delivery. Focused initiatives to mitigate CKD growth and expand kidney transplantation programs in regions outside of Bangkok should be further implemented as part of long-term cost-containment strategies. The centralization of resources and standardization of the financing mechanism of dialysis among three different health schemes could be considered, to promote more efficient use of national resources and to create reimbursement equality. In the short-term, improvements in PD supporting systems, including culture techniques and nutritional support, are urgently needed for the sustainability of the “PD First” policy. The success of the policy, in terms of both quantity and quality, highlights the crucial role of the Thai teams in advocacy and collaboration with policymakers to work toward sustainable solutions for people living with kidney disease.
Disclosures
The authors have nothing to disclose.
Funding
This review was supported by National Research Council of Thailand grant 6/2562.
Acknowledgment
We thank D. Johnson, Department of Nephrology, Princess Alexandra Hospital, Brisbane, Queensland, Australia, for full language support and contributing important intellectual content during revision.
Author Contributions
T. Kanjanabuch was responsible for reviewing and editing the manuscript; and both authors conceptualized the study, and were responsible for data curation and writing the original draft.
References
- 1.Krittayaphong R, Rangsin R, Thinkhamrop B, Hurst C, Rattanamongkolgul S, Sripaiboonkij N, Wangworatrakul W: Prevalence of chronic kidney disease associated with cardiac and vascular complications in hypertensive patients: A multicenter, nation-wide study in Thailand. BMC Nephrol 18: 115, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chuasuwan A, Praditpornsilpa K:Thailand renal replacement therapy: Year 2015. [Internet]. Available at: http://www.nephrothai.org/images/Final_TRT_report_2015_%E0%B8%89%E0%B8%9A%E0%B8%9A%E0%B9%81%E0%B8%81%E0%B9%84%E0%B8%82.pdf. Accessed January 20, 2020
- 3.Thailand Official Statistics Registration Systems: Population and house statistics-Population by age. 2019. Available at: http://stat.dopa.go.th/stat/statnew/upstat_age.php. Accessed February 14, 2020
- 4.Central Intelligence Agency: The world factbook: East Asia/Southeast Asia: Thailand. Available at: https://www.cia.gov/library/publications/the-world-factbook/geos/th.html. Accessed January 20, 2020
- 5.National Health Security Office. NHSO Annual Report 2017. Available at: http://stream.nhso.go.th/wp-content/uploads/ebooks/annual-2017. Accessed January 20, 2020
- 6.Announcement of the Ministry of finance September 21, 1998: Determining the criteria and reimbursement rate of medical expenses for patients with kidney disease. Available at: http://saraban-law.cgd.go.th/CGDWeb/simple_search.jsp. Accessed January 20, 2020
- 7.Announcement of the medical committee under the social security act: Criteria and reimbursement rate of medical expenses for renal replacement therapy 2015. Available at: https://www.sso.go.th/wpr/assets/upload/files_storage/_th/dfff6f731d973161024501fff69071d5.pdf. Accessed January 20, 2020
- 8.The Secretariat of the Cabinet : The Cabinet resolution 2007. Available at: https://cabinet.soc.go.th/soc/Program2-3.jsp?top_serl=214283. Accessed January 20, 2020
- 9.Chuengsaman P, Kasemsup V: PD First policy: Thailand’s response to the challenge of meeting the needs of patients with end-stage renal disease [published correction appears in Semin Nephrol 37: 488, 2017]. Semin Nephrol 37: 287–295, 2017 [DOI] [PubMed] [Google Scholar]
- 10.United States Renal Data System : 2018 USRDS annual data report. Chapter II: International comparisons. Available at: https://www.usrds.org/2018/download/v2_c11_IntComp_18_usrds.pdf. Accessed January 20, 2020
- 11.Tang SCW: Dialysis care and dialysis funding in Asia. AJKD 75: 2020, In press 10.1053/j.ajkd.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 12.Wang AY, Zhao J, Bieber B, Kanjanabuch T, Wilkie M, Marshall MR, Kawanishi H, Perl J, Davies S; PDOPPS Dialysis Prescription and Fluid Management Working Group : International comparison of peritoneal dialysis prescriptions from the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS) [published online ahead of print Jan 17, 2020]. Perit Dial Int [DOI] [PubMed] [Google Scholar]
- 13.Shayakul C: Hemodialysis clinical practice recommendation 2014. Available at: http://www.nephrothai.org/images/nephrothai/know/hd_guidelines_2557.pdf. Accessed January 20, 2020
- 14.Perl J, Fuller DS, Bieber BA, Boudville N, Kanjanabuch T, Ito Y, Nessim SJ, Piraino BM, Pisoni RL, Robinson BM, Schaubel DE, Schreiber MJ, Teitelbaum I, Woodrow G, Zhao J, Johnson DW: Peritoneal dialysis-related infection rates and outcomes: Results from the peritoneal dialysis outcomes and Practice Patterns study (PDOPPS) [published online ahead of print Jan 10, 2020]. Am J Kidney Dis [DOI] [PubMed] [Google Scholar]
- 15.Changsirikulchai S, Sriprach S, Thokanit NS, Janma J, Chuengsaman P, Sirivongs D: Survival analysis and associated factors in Thai patients on peritoneal dialysis under the PD-first policy. Perit Dial Int 38: 172–178, 2018 [DOI] [PubMed] [Google Scholar]
- 16.Thai Transplantation Society: Annual report 2018: Kidney transplantation in Thailand. Available at: http://transplantthai.org/upload/editor/file/2019%20Annual%20report(1).pdf. Accessed Mar 16, 2020
- 17.Noppakun K, Ingsathit A, Pongskul C, Premasthian N, Avihingsanon Y, Lumpaopong A, Vareesangthip K, Sumethkul V; Subcommittee for Kidney Transplant Registry; Thai Transplantation Society : A 25-year experience of kidney transplantation in Thailand: Report from the Thai transplant registry. Nephrology (Carlton) 20: 177–183, 2015 [DOI] [PubMed] [Google Scholar]


