Introduction
The first reported case of coronavirus disease 2019 (COVID-19) infection in Australia (population 26 million) occurred on January 24th, 2020 in a returned traveler from Wuhan, China (1) followed by a rapid rise in new cases (Figure 1). The Australian government activated the Health Sector Emergency Response Plan for Novel Coronavirus (2) in late February, with subsequent implementation of strict social distancing measures and closure of international boarders in late March (Figure 1). We describe the response taken by the Australian and New Zealand Society of Nephrology (ANZSN) to prepare for the potential exponential increase in case load that was seen in other countries, such as Italy, the United Kingdom, and the United States.
Figure 1.
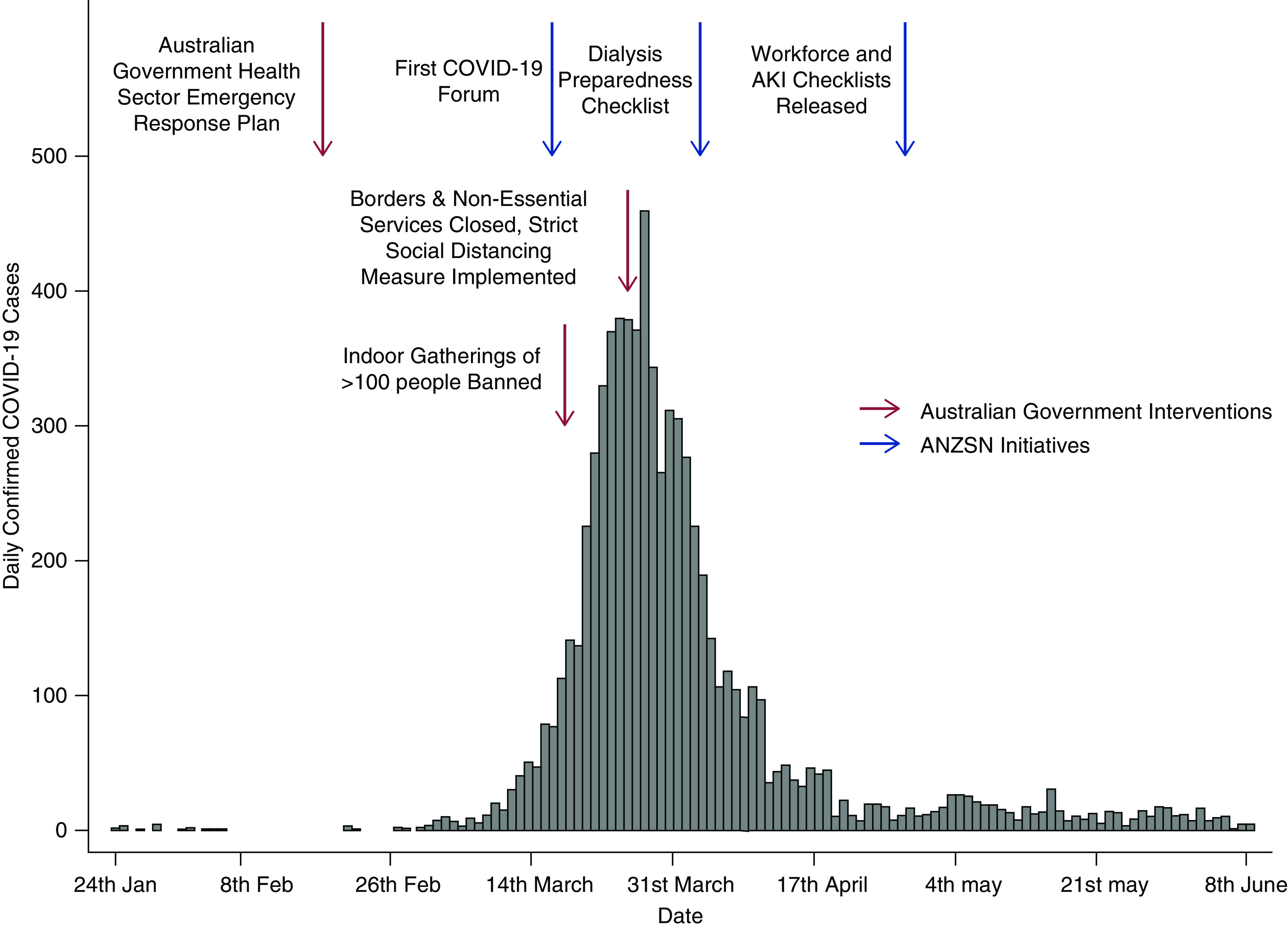
Daily coronavirus disease 2019 (COVID-19) infection numbers in Austraia January 24th to June 8th, 2020 showing peak cases mid to late March. Blue and red arrows illustrate timing of Australian Government and Australian and New Zealand Society of Nephrology (ANZSN) initiatives in relation to daily COVID-19 infection numbers.
On March 4th, 2020, the ANZSN Council canvassed members to determine if any had commenced preparations for the COVID-19 infection. It became clear that no coordinated approach to this infection had been instigated. As such, the ANZSN Council held a members-only virtual meeting (the COVID-19 Forum) to gauge the preparedness of society members and obtain guidance on further actions.
The first COVID-19 Forum was held on March 18th at a time when daily case numbers were rapidly escalating (Figure 1). It was clear at this meeting that the society and its members were not prepared for the COVID-19 infection. This directed the ANZSN Council to create a COVID-19 Working Group (WG) comprising nephrologists and renal nursing and patient advocacy experts with geographic representation across Australia and New Zealand. Specifically, the WG performed three broad functions—monitor and remain informed of the COVID-19 situation with a focus on the issues affecting the care of patients with CKD and/or AKI; facilitate the identification and discussion of common issues requiring a coordinated response at a renal unit and/or state or national level; and provide a vehicle for the discussion, development, and dissemination of information, including guidelines and protocols, to support renal units.
The COVID-19 Forum continued initially weekly, open to all members (nephrology and nursing), to assist with planning and provide assistance as well as opportunities for cooperation to all during the crisis. Real-time feedback during the forum provided the WG with focus topics on which to assist members in their response to the crisis. The WG and the forum initially identified a number of key areas of focus, of which we discuss three below. A summary of the key features for each key focus area is presented in Table 1.
Table 1.
Key features of coronavirus disease 2019 checklists
| Checklist and Major Section | Examples |
| Dialysis preparedness checklist | |
| Infection prevention and control policies and training for HCWs | Importance of HH |
| Respiratory hygiene | |
| Cough etiquette | |
| CPR in COVID-19–positive patients | |
| Education and culturally appropriate communication with patients | COVID-19 (e.g., symptoms, how it is transmitted) |
| The importance of continuing to attend dialysis as scheduled | |
| Patients receive advice to minimize risks if dialysis duration or frequency has to be reduced due to staffing shortages | |
| Process for rapidly identifying and isolating patients with confirmed or suspected COVID-19 | Unit has a system to receive and triage phone calls from patients with symptoms of fever or respiratory infection |
| Signs are posted in triage areas advising patients with fever or symptoms of respiratory infection to immediately notify triage personnel so that appropriate precautions can be put in place | |
| Unit has a process to ensure that patients with confirmed or suspected COVID-19 are placed in the designated COVID-19 triage or treatment area | |
| Patient placement and testing | Units limit as far as practicable use of waiting rooms, with patients being taken directly into dialysis units |
| The unit identifies a specific isolation room for the testing of patients for COVID-19 | |
| Unit has a plan for cohorting patients and HCWs if they are dialyzing multiple patients with confirmed COVID-19 | |
| Transmission-based precautions | Unit has a procedure for assessing supply (inventory) of PPE and other infection prevention and control supplies (e.g., HH supplies) |
| HCWs receive appropriate training, including “just in time” training on selection and proper use of (including putting on and removing) PPE, with a required demonstration of competency | |
| Movement of patients with undiagnosed respiratory infection and/or confirmed or suspected COVID-19 within the dialysis unit | Patient movement outside of the isolation room (isolation station) will be limited to essential purposes |
| The unit has a plan for wearing of PPE by patients (e.g., face mask) | |
| HH and environmental cleaning | HH supplies, including alcohol-based hand sanitizer, are readily accessible in inpatient care areas, including areas where HCW put on and remove PPE |
| Unit has a process to ensure that shared or nondedicated equipment is cleaned and disinfected after use and according to the manufacturer’s recommendations | |
| Monitoring and managing HCW | Unit has sick leave policies that are nonpunitive, are flexible, and allow ill HCWs to stay home |
| Unit has considered cohort staffing to minimize the risk of transmission between HCWs | |
| Visitor access and movement within the dialysis unit | Unit has a plan to restrict nonessential visitors |
| Visitors are screened for symptoms of acute respiratory infection before entering the unit | |
| Unit management structure and situational awareness | Smaller units should identify support networks with regional and/or state partners |
| Unit knows where COVID-19 testing is being performed locally and has a plan to refer patients who need COVID-19 testing if not available at the unit | |
| Transportation | Unit has explored options for patients to travel individually to dialysis either by private car or by single-occupancy taxi |
| If patients must come in group shuttles, the unit has liaised with transport providers to use screening questions before boarding transport and have developed an infection control plan in collaboration with the transport provider | |
| AKI preparedness checklist | |
| Meet/liaise with ICU to determine management plan for AKI | Determine ICU capacity for CRRT and/or SLED |
| Evaluate access to water in the ICU or other high-dependency care areas to enable HD | |
| Is there a plan for the transition of care of the dialysis-dependent patient with AKI discharged from the ICU? | |
| What capacity does the renal unit have for intermittent HD for AKI? | Determine whether HD can be performed in designated COVID-19 ward(s)? (water access, isolation, cohorting of staff, clinical COVID-19 expertise, etc.) |
| Assess use and capacity of spare HD machines | |
| Assess capacity of dialysis staff to provide dialysis out of the usual HD unit? | |
| Managing patients with COVID-19 in the dialysis unit | Plan for cohorting of COVID-19–positive patients with AKI |
| Isolation/infection control protocols in place? | |
| Staff adequately trained? | |
| Other issues | Vascular access placement in COVID-19–positive patients—access to nontunneled and tunneled central line |
| Acute PD—capacity for PD catheter insertion in COVID-19–confirmed/suspected patient | |
| Nephrology follow-up procedures in place for patients with AKI after discharged home? | |
| Workforce preparedness checklist | |
| Sick leave policies and health of staff | Nonpunitive, flexible sick leave policies |
| Influenza vaccination for all HCWs in renal facilities, recognizing that this may be done in accordance with local immunization policies | |
| Communication strategies | Consider communication strategies in advance, particularly if a staff member was to test positive for the virus |
| Consider how news of an infected staff member may be communicated to patients | |
| Cohorting of staff | Consider restrictions to staff socializing (e.g., joint lunch breaks) and access to shared spaces, such as tea rooms or lockers |
| Units have considered how to redeploy specialist nurses to maximize number of staff able to perform HD and have retrained staff as appropriate | Estimate/chart in advance your minimum required safe staffing levels to remain capable of providing treatment to your patient population, recognizing that modifications to usual practices may be needed in case of significant workforce shortages |
| Consider employing nonspecialist nurses (e.g., theater nurses) within renal units to help monitor patients on dialysis if this will reduce the number of experienced nurses required per shift | |
| Unit management structure and situational awareness | Consider stopping rotation of junior staff between renal units |
| Consider allied health workers and administrative and cleaning staff attached to renal units; make attempts to minimize rotation between units/other areas of the hospital | |
| Advocacy | The specialized nature of their work makes renal nursing staff members hard to replace with other nursing personnel from other streams |
HCW, health care worker; HH, hand hygiene; CPR, cardiopulmonary resuscitation; COVID-19, coronavirus disease 2019; PPE, personal protective equipment; ICU, intensive care unit, CRRT, continuous RRT; SLED, sustained low-efficiency dialysis; HD, hemodialysis; PD, peritoneal dialysis.
Facility Dialysis Preparedness
Dialysis unit preparedness is highlighted as a key issue. Nephrology services, and hence, dialysis, are primarily delivered via large metropolitan and rural publicly funded (not-for-profit) health care networks (3). Specialist tertiary centers provide access to dialysis and transplantation while supporting smaller facilities that are located at a range of distances from the main tertiary facility. Center-based hemodialysis (HD) is the predominant therapy at 75% (4).
At a national level, the ANZSN COVID-19 WG developed the “ANZSN dialysis preparedness checklist” (5) (Table 1), which was adapted for local use from the Centers for Disease Control and Prevention COVID-19 outpatient dialysis facility document (6). The checklist is intended for use by renal unit senior management to assist them in considering key components of COVID-19 contingency planning for their units while recognizing that each unit will have specific circumstances and challenges that will require local solutions. The checklist is for general information only and is not a list of mandatory requirements. Additionally, within each state and territory, renal unit heads have been meeting regularly by teleconference to assist in coordination and develop uniform approaches to dialysis preparedness adapted to local conditions.
The ability to cohort infected patients on HD is a particular challenge in Australia, where the majority of units have little room to increase capacity. The availability of isolation rooms in the facility dialysis unit is limited, and most are dialyzing to maximum capacity. Depending on the location, some jurisdictions proposed to cohort all COVID-19–positive patients on HD within a single facility, but this was not always practical under local conditions.
Workforce Capacity
Workforce capacity, particularly in the dialysis facility, was highlighted by the forum as a point of major focus. The loss of frontline dialysis nursing staff, with expertise that is not easily replaceable, due to COVID-19 infection was of great concern. This issue is particularly acute for the smaller regional and remote facilities, which do not have flexibility and capacity to replace dialysis nursing staff easily. The need for additional staff was also highlighted given the overseas experience with increased numbers of dialysis-dependent patients with AKI (7–11).
The WG has developed a workforce preparedness checklist to assist units in planning (12) (Table 1). The checklist highlights mitigation strategies aimed at reducing the risk of staffing shortages in the dialysis facility, including cohorting staff into separate groups, employing nonspecialist nurses (e.g., theater nurses) within renal units in the event of reduced availability of experienced nurses, and relaxing accreditation procedures to help facilitate movement across health services where there is acute need.
AKI
The preparation for and the management of AKI in patients with COVID-19 was the third area of focus. Dialysis-dependent AKI within the intensive care unit (ICU) is primarily managed by the ICU physicians using continuous RRT and/or sustained low-efficiency dialysis. Nephrology input is usually sought in the case of diagnostic uncertainty, and/or when recovery is delayed with the clear need for ongoing dialysis upon discharge from the ICU. Given the emerging reports of the large number of patients requiring acute dialysis (and even acute peritoneal dialysis [PD]) (7–11), nephrology unit preparedness and capacity to manage additional dialysis-dependent patients with AKI were clearly important. As such, an AKI preparedness checklist was also developed to assist units in their preparations (13) (Table 1). The checklist covers a range of aspects, including liaising with ICU on the capacity to manage such patients and assessing the capacity of the renal unit to perform intermittent HD in patients with AKI post-ICU, as well as the ability to perform acute PD if needed.
Implementation
Although the ANZSN has no authority to formally implement the described recommendations within renal units and health care services, it took a top-down and bottom-up approach. The president of the ANZSN wrote to each individual federal and state health minister to highlight important kidney-specific issues and the WG outputs. The WG members included key members of state-based renal networks that develop and help implement state-based policies. Finally, the forum and society communications ensured that all health care professionals in renal care were made aware of the WG recommendations and were motivated to ensure their uptake.
Other Considerations
As part of the national preparations to the COVID-19 pandemic, all elective surgery was temporarily ceased, with only urgent and emergency surgery to continue. Dialysis access surgery in most but not all centers has continued due to the urgent nature of the surgery. Outpatient clinic services have been largely converted to telehealth consultations, except where onsite assessment is deemed absolutely essential. The clinical management of patients on home HD and PD has largely remained unchanged, except for the clinic appointments to telehealth. Routine remote monitoring of patients on home HD is not routinely performed, and in PD, remote monitoring is currently only performed in a few units across Australia. The ANZSN Council also met with key personnel of dialysis companies to ensure that adequate supply chains for dialysis were present and that business continuity plans were created.
Finally, the Australian and New Zealand Dialysis and Transplant Registry has facilitated real-time tracking of COVID-19 infection in the dialysis and transplant populations. As of June 8th, 2020, the infection rate in the ESKD population was fortunately low with five patients on HD and eight transplant recipients infected across Australia, with three deaths.
As in all countries around the world, the COVID-19 pandemic presents huge and novel challenges on how the Australian health care system will be able to continue to treat and deliver quality care to patients on dialysis and patients with transplants. The public health response to COVID-19 has seen a marked reduction in the case load such that as of June 8th, 2020, Australia’s total case number was 7265 with 102 deaths. The national forum and the WG likely served as catalysts to motivate the various jurisdictions into action by providing a stimulus for the state-based renal networks to meet and coordinate response plans and provided opportunity for people to feel supported and unified in dealing with the pandemic. Thus, although at present, Australia has been relatively spared in terms of the case load seen in other countries, we believe that Australian (and New Zealand) nephrology units are now well placed to ensure the best possible care for their patients should the case load increase. The rapid cooperation and support seen across Australia and New Zealand in response to the crisis have been an illustration of how nephrologists and nursing staff can come together for a common goal to ensure ongoing quality care to patients on dialysis and patients with transplants.
Disclosures
N. Boudville reports personal fees from Baxter, personal fees from Roche, and personal fees from Amgen outside the submitted work. All remaining authors have nothing to disclose.
Funding
None.
Acknowledgment
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Author Contributions
K.R. Polkinghorne, N. Boudville, and P.G. Kerr conceptualized the study; K.R. Polkinghorne wrote the original draft; and K.R. Polkinghorne, N. Boudville, and P.G. Kerr reviewed and edited the manuscript.
References
- 1.Caly L, Druce J, Roberts J, Bond K, Tran T, Kostecki R, Yoga Y, Naughton W, Taiaroa G, Seemann T, Schultz MB, Howden BP, Korman TM, Lewin SR, Williamson DA, Catton MG: Isolation and rapid sharing of the 2019 novel coronavirus (SARS-CoV-2) from the first patient diagnosed with COVID-19 in Australia. Med J Aust 212: 459–462, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Australian Government Department of Health: Australian health sector emergency response plan for novel coronavirus (COVID-19), 2020. Available at: https://www.health.gov.au/resources/publications/australian-health-sector-emergency-response-plan-for-novel-coronavirus-covid-19. Accessed June 8, 2020
- 3.Damasiewicz MJ, Polkinghorne KR: Global dialysis perspective: Australia. Kidney360 1: 48–51, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ANZDATA Registry : The 42nd Annual ANZDATA Report, Adelaide, SA, Australia, ANZDATA Registry, 2019 [Google Scholar]
- 5.ANZSN: ANZSN dialysis preparedness checklist, 2020. Available at: https://www.nephrology.edu.au/covid-19-updates.asp. Accessed April 27, 2020
- 6.CDC: CDC Coronavirus Disease 2019 (COVID-19) outpatient dialysis facility preparedness assessment tool, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/downloads/COVID-19-outpatient-dialysis.pdf. Accessed April 27, 2020
- 7.Goldfarb DS, Benstein JA, Zhdanova O, Hammer E, Block CA, Caplin NJ, Thompson N, Charytan DM: Impending shortages of kidney replacement therapy for COVID-19 patients [published online ahead of print April 28, 2020]. Clin J Am Soc Nephrol doi: 10.2215/CJN.05180420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, Hazzan AD, Fishbane S, Jhaveri KD; Northwell COVID-19 Research Consortium; Northwell Nephrology COVID-19 Research Consortium : Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 98: 209–218, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durvasula R, Wellington T, McNamara E, Watnick S: COVID-19 and kidney failure in the acute care setting: Our experience from Seattle. Am J Kidney Dis 76: 4–6, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G: Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int 97: 829–838, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V: The novel coronavirus 2019 epidemic and kidneys. Kidney Int 97: 824–828, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ANZSN: COVID-19 workforce preparedness checklist, 2020. Available at: https://www.nephrology.edu.au/covid-19-updates.asp. Accessed April 27, 2020
- 13.ANZSN: COVID-19 AKI preparedness checklist, 2020. Available at: https://www.nephrology.edu.au/covid-19-updates.asp. Accessed April 27, 2020


