Abstract
Sepsis is a syndrome with high mortality, which seriously threatens human health. During the pandemic of coronavirus disease 2019 (COVID-19), some severe and critically ill COVID-19 patients with multiple organ dysfunction developed characteristics typical of sepsis and met the diagnostic criteria for sepsis. Timely detection of cytokine storm and appropriate regulation of inflammatory response may be significant in the prevention and treatment of sepsis. This study evaluated the efficacy and safety of specific interleukin (IL)-1 inhibitors, specific IL-6 inhibitors, and GM-CSF blockades in the treatment of COVID-19 (at the edge of sepsis) patients through systematic review and meta-analysis. Methodology: A literature search was conducted on PubMed, EMBASE, Clinical Key, Cochrane Library, CNKI, and Wanfang Database using proper keywords such as “SARS-CoV-2,” “Corona Virus Disease 2019,” “COVID-19,” “anakinra,” “tocilizumab,” “siltuximab,” “sarilumab,” “mavrilimumab,” “lenzilumab,” and related words for publications released until August 22, 2021. Other available resources were also used to identify relevant articles. The present systematic review was performed based on PRISMA protocol. Results: Based on the inclusion and exclusion criteria, 43 articles were included in the final review. The meta-analysis results showed that tocilizumab could reduce the mortality of patients with COVID-19 (at the edge of sepsis) [randomized controlled trials, RCTs: odds ratio (OR) 0.71, 95%CI: 0.52–0.97, low-certainty evidence; non-RCTs: risk ratio (RR) 0.68, 95%CI: 0.55–0.84, very low-certainty evidence) as was anakinra (non-RCTs: RR 0.47, 95%CI: 0.34–0.66, very low-certainty evidence). Sarilumab might reduce the mortality of patients with COVID-19 (at the edge of sepsis), but there was no statistical significance (OR 0.65, 95%CI: 0.36–1.2, low-certainty evidence). For safety outcomes, whether tocilizumab had an impact on serious adverse events (SAEs) was very uncertain (RCTs: OR 0.87, 95%CI: 0.38–2.0, low-certainty evidence; non-RCTs 1.18, 95%CI: 0.83–1.68, very low-certainty evidence) as was on secondary infections (RCTs: OR 0.71, 95%CI: 0.06–8.75, low-certainty evidence; non-RCTs: RR 1.15, 95%CI: 0.89–1.49, very low-certainty evidence). Conclusions: This systematic review showed that tocilizumab, sarilumab, and anakinra could reduce the mortality of people with COVID-19 (at the edge of sepsis), and tocilizumab did not significantly affect SAEs and secondary infections. The current evidence of the studies on patients treated with siltuximab, mavrilimumab, and lenzilumab is insufficient. In order to establish evidence with stronger quality, high-quality studies are needed.
Systematic Review Registration: PROSPERO (https://www.crd.york.ac.uk/prospero/), identifier CRD42020226545
Keywords: specific interleukin-1 inhibitors, specific interleukin-6 inhibitors, GM-CSF blockades, coronavirus disease 2019 (COVID-19), SARS-CoV-2, sepsis
1 Introduction
Sepsis is a life-threatening organ dysfunction syndrome caused by host response imbalance due to an infection or infectious factors. The mortality and treatment expenditure of sepsis are relatively high, and there is no specific drug so far. An article published in The Lancet in 2020 pointed out that the number of sepsis patients worldwide reached 48.9 million in 2017, among which 11 million patients died, accounting for one-fifth of the global death toll (Rudd et al., 2020).
During the pandemic of coronavirus disease 2019 (COVID-19), patients with severe and critically ill COVID-19 may develop circulation disorders and severe lung damage. Some patients with multiple organ dysfunction, such as that of the liver and kidney, showed typical characteristics of sepsis and meet the diagnostic criteria for sepsis (Li et al., 2020). According to Sepsis-3, sepsis is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection. The organ dysfunction can be represented by an increase in the Sequential (Sepsis-Related) Organ Failure Assessment (SOFA) score of 2 points or more, which is associated with an in-hospital mortality greater than 10% (Singer et al., 2016). Recent studies have shown that patients with severe and critical diseases may experience immune hyperactivity with increased levels of interleukin (IL)-1, IL-6, granulocyte–monocyte colony-stimulating factor (GM-CSF), interferon-γ-inducible protein 10 (IP-10), tumor necrosis factor-α (TNF-α), and other several inflammatory cytokines and were associated with adverse clinical outcomes (Huang et al., 2020; Qin et al., 2020; Coomes and Haghbayan, 2020; Lucas et al., 2020). Therefore, inhibition of proinflammatory cytokines may be a potential therapeutic strategy in COVID-19 (at the edge of sepsis) patients. This study was the first to screen COVID-19 patients with sepsis or at the edge of sepsis through the SOFA score and systematically reviewed the efficacy and safety of anti-cytokine therapy, such as specific IL-1, IL-6 inhibitors, and anti-GM-CSF in COVID-19 patients with organ dysfunction (SOFA ≥2). This paper could help sepsis treatment strategy researchers to grasp the current status of anti-cytokine therapy for COVID-19 patients (at the edge of sepsis) and provide a new perspective for clinical treatment.
2 Methodology
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline (Supplementary Material S1) (Moher et al., 2009) and registered with the National Institute for Health Research international prospective register of systematic reviews (PROSPERO registration number: CRD42020226545) (Wang et al., 2020).
2.1 Search Strategy and Selection Criteria
Electronic searches were carried out in PubMed, EMBASE, Clinical Key, Cochrane Library, China National Knowledge Infrastructure (CNKI), and Wanfang Database. The search terms that we used were “SARS-CoV-2,” “corona virus disease 2019,” “COVID-19,” “anakinra,” “tocilizumab,” “siltuximab,” “sarilumab,” “mavrilimumab,” and “lenzilumab” and relevant keywords for publications released until August 22, 2021. The search strategies are available as supplementary data (Supplementary Material S1). Other available resources were also used to identify relevant articles. The language will be limited to Chinese and English. Eligible articles were identified for inclusion by screening the titles, abstracts, and full text. Other relevant studies were manually screened by investigators from the reference list of included studies for further analysis. There was no date limit. Two independent reviewers (YW and KZ) carried out the search in a standardized process, followed with identifying eligible records through the examination of each title, abstract, and full text. Disagreements were resolved by consensus, and unresolved conflicts were decided by a third reviewer (QY).
The studies were selected based on the following inclusion criteria: (1) The patients were diagnosed with SARS-CoV-2 infection and their SOFA score (include mean value, median, and absolute value) ≥2 or, according to the SOFA scoring tool, a certain system index (including mean, median, and absolute value) should be within the range corresponding to the system score ≥2—for example, PaO2/FiO2 ratio (P/F) (including absolute value, mean value, or median value) was less than 300 mmHg (Singer et al., 2016). A SpO2/FiO2 ratio (S/F) of 315 corresponded with a P/F ratio of 300 mmHg [S/F = 64 + 0.84*(P/F)] (Rice et al., 2007). In this review, we defined such COVID-19 patients to be at the edge of sepsis. (2) The intervention of interest was a specific IL-1 inhibitor (anakinra), specific IL-6 inhibitors (tocilizumab, siltuximab, and sarilumab), GM-CSF blockades (mavrilimumab and lenzilumab) with or without standard of care (or treatment), and glucocorticoids. Comparator treatments included placebo, standard of care (or treatment), glucocorticoids, or no intervention; studies with no comparator group were also included. (3) Randomized clinical trials (RCTs), cohort studies, case–control studies, case series, case reports, clinical guidelines, protocols for clinical trials, and any other gray literatures will be included. The studies will not be limited in terms of country. The exclusion criteria were as follows: (1) The patients were not diagnosed as COVID-19; (2) The SOFA score (absolute value, mean value, or median value) of the patients was less than 2 or did not reach 2 on any of the system indicators; (3) Data on SOFA score or certain indicators in the SOFA scoring tool for the patients studied were not available in the study text, additional materials, or any other relevant resources; and (4) Studies without an available full text or whose data were incomplete or unavailable, posters, commentaries, letters, opinion articles, and in vitro studies were excluded. The defined primary outcome was all-cause mortality at 28–30 days. The safety outcomes included serious adverse events (SAEs) and (serious) secondary infection. Adverse events were graded according to the Common Terminology Criteria for Adverse Events, version 4.0 (National Institutes of Health, 2017).
2.2 Data Extraction and Quality (Risk of Bias) Assessment
Two independent reviewers (YW and KZ) extracted data from the eligible studies, and a third one (QY) validated it. The following information will be extracted: year of publication, authors, country, study type, sample size, participant demographics, time of administration, intervention characteristics (name of agent, dose, and route), concomitant medications, survival outcome, treatment-related adverse events, and conclusions of the authors.
The included studies were assessed in terms of potential bias by two reviewers (RD and RL) independently. The third researcher (XL) was consulted for resolving any difference of opinion. The Quality Assessment for Case Series of the National Institute for Health and Care Excellence will be used to evaluate the quality of the case reports (series). The total score is 8 points, in which a score of 4–8 is high quality, and a score less than 4 is low quality. The methodological quality for cohort and case–control studies was assessed based on the Newcastle–Ottawa Scale (NOS) (NOS, 2020). The total score is 9 points, in which scores of 0–3, 4–6, and 7–9 are respectively considered as low, moderate, and high quality. The methodological quality of RCTs was assessed based on the “Risk of Bias” 2.0 tool (Sterne et al., 2019). Each checklist item was judged as “low,” “moderate,” “serious,” and “critical,” The quality of evidence was assessed by using the “Grading of Recommendations Assessment Development and Evaluation (GRADE)” tool (Granholm et al., 2019). The quality of evidence of each outcome is classified as “high,” “moderate,” “low,” or “very low”.
2.3 Data Synthesis and Analysis
The Review Manager version 5.4.1 software was used for analyses. One reviewer (YW) would have to enter the data into the software, and another reviewer (M.L) would have to check the data for accuracy. For dichotomous outcomes, the number of events and total number of participants in the two groups were recorded. The different types of studies were analyzed separately, such as non-RCTs (cohorts and case–control studies) and RCTs. The risk ratio (RR) and odds ratio (OR) with 95% confidence intervals (CIs) were respectively assessed for non-RCTs and RCTs. Fixed-effects model was used if the result of the Q test was not significant (p > 0.1) and I2 <50%. Chi-square test, with a significance level at p ≤ 0.1, was used to assess the heterogeneity of treatment effects between trials. The I 2 statistic was used to quantify possible heterogeneity (75–100% considerable heterogeneity). We would explore potential causes through sensitivity and subgroup analyses if heterogeneity had been above 80%. We would not have conducted a meta-analysis if we had not found a reason for heterogeneity. If we could not perform a meta-analysis, we had planned to comment on the results from all studies.
3 Results
3.1 Search Results
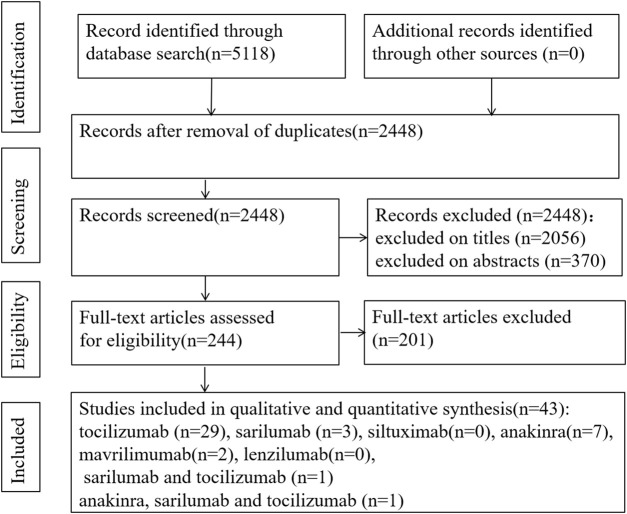
Because of insufficient evidence available from RCTs, we also included cohort studies, case–control studies, and case reports (series). The search of the electronic databases on Aug 22, 2021 yielded a total of 5,118 studies. Following the elimination of duplicates and screening of titles and abstracts, we evaluated 244 articles in full text. Among these, we found 43 eligible articles (5 RCTs, 16 cohort studies, 2 case–control studies, and 20 case reports) (Figure 1) (Salvarani et al., 2021; REMAP-CAP Investigators et al., 2021; Canziani et al., 2020; Menzella et al., 2020; Fisher et al., 2021; Campochiaro et al., 2020; Vazquez Guillamet et al., 2021; Rajendram et al., 2021;Huang et al., 2021; Galván-Román et al., 2021; Saffo et al., 2021; Somers et al., 2021; Brosnahan et al., 2021; Corominas et al., 2021; Cavalli et al., 2021; Abe et al., 2021; Patel et al., 2020; Mady et al., 2020; Bernardo et al., 2020; Morillas et al., 2020; Cascella et al., 2020; Al-Kaf et al., 2021; Eroglu et al., 2021; Kataoka et al., 2021; Kishaba et al., 2021; Leelayuwatanakul et al., 2021; McKenzie et al., 2021; Nourié et al., 2021; Ladna et al., 2021; Senegaglia et al., 2021; Thammathiwat et al., 2021; Lescure et al., 2021; Della-Torre et al., 2020; Gremese et al., 2020; Kyriazopoulou et al., 2021a; Bozzi et al., 2021; Franzetti et al., 2021; Kyriazopoulou et al., 2021b; Erden et al., 2021; Filocamo et al., 2020; Franzetti et al., 2020; Cremer et al., 2021; De Luca et al., 2020). All studies were published in peer-reviewed journals.
FIGURE 1.
PRISMA flow chart of study selection.
In the process of full-text review, there were four articles for which we failed to obtain the full texts. The four studies were related to tocilizumab. Two studies did not report the efficacy and safety of tocilizumab (Garg et al., 2020; Kashin et al., 2020). The other two studies were case reports, in which one patient developed tuberculosis reactivation during treatment and the other patient had a secondary infection. The authors of the two case reports suggested that patients might be at a high risk for secondary infection after receiving tocilizumab or tocilizumab combined with glucocorticoid. They suggested that clinicians should use tocilizumab with caution and screen for latent tuberculosis before medication (Mazankova et al., 2020; Moideen et al., 2020).
3.2 Risk of Bias Assessment
The risk of bias of the RCTs was low to moderate, respectively. The results are shown in Supplementary Figure S1 (Supplementary Material S2, Appendix p1). Some studies reported only one outcome, and we assessed the risk of bias for the results—for instance, bias in the measurement of outcomes was not available for safety for the study of Brosnahan et al. (2021) because they did not report it. For mortality outcomes, the methodological quality of 16 cohorts was moderate to high, and those of 2 case–control studies were moderate. For safety outcomes, the methodological quality of 14 cohorts was low to high, and those of 2 case–control studies were low to moderate (NOS assessment results are shown in Supplementary Material S2, Appendix p2–40). The methodological quality evaluation results of the included case reports (series) showed that the quality was low to moderate (the results of quality are shown in Supplementary Material S2, Appendix, p41–42).
3.3 Characteristics of Patients
The 43 studies included were identified and critically evaluated, which included a total of 4,951 patients with confirmed SARS-CoV-2 infection, of whom 2,243 received mechanical ventilation. Only 11 studies reported the SOFA score of enrolled patients, of which 4 studies reported SOFA scores greater than or equal to 6 (tocilizumab), 3 studies reported scores between 4 and 5 (tocilizumab), and 4 studies reported scores between 2 and 3 (3 for anakinra, 1 for mavrilimumab). The remaining 32 articles reported the respiratory status (including P/F or S/F) and platelet of patients, of which 5 studies included patients with P/F less than or equal to 100 mmHg and of which 13 studies reported patients with P/F between 100 and 200 mmHg.
Most patients received standard of care (or standard of treatment) based on local treatment guidelines. However, the medication regimens of the standard of care were different, mainly including antiviral drugs, antibiotics, glucocorticoids, and other symptomatic drugs. Anti-cytokine agents were mainly used by intravenous injection and, in a few studies, by subcutaneous administration. In addition, there is still no consensus on the dosage of anti-cytokine agents for such patients until now. In the included articles, the dosage of most patients was as follows: tocilizumab, 8 mg/kg/dose and up to a maximum of 800 mg; sarilumab, 400 mg/dose with 1 to 2 doses; anakinra 100 mg/dose 1–4 times a day; and mavrilimumab 6 mg/kg/dose. The characteristics of the included studies are presented in Table 1.
TABLE 1.
Characteristics of the included studies.
| Study | Country | Study type | P | SOFA score or indicators, median (IQR) | Laboratory values, median (IQR) | Intervention group | Control group | Time of administration, median (IQR)-days | Dosage | Usage | Comorbidities(n) | Concomitant medications(n) | Effective outcomes | Safety outcomes | Authors’ conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Salvarani et al. (2020) | Italy | RCT, MC, open-labal | 126; 77 M:49 F | P/F: 264.5 (243.0–290.0) mmHg | CRP- mg/dl: 8.2 (3.7–13.5).; IL-6-pg/ml: 42.1 (20.6–74.9); ferritin-ng/ml: 569.0 (317.0–1,156.0) | TCB + standard of care | Standard of care | Days from symptom onset to randomization, median (IQR): 8.0 (6.0–11.0) | A dose of 8 mg/kg up to a maximum of 800 mg, followed by a second dose after 12 h | Intravenous | DB (19), obesity: BMI ≥30 (38), HTN (56), COPD (4) | HCQ (115), antiretrovirals (52), azithromycin (26), steroids | Within 14 days, 17 of 60 in the experimental group and 17 of 63 in the control group showed clinical worsening; 1 in the control group and 2 patients in the experimental group died before 30 days from randomization | AE (n, %): TCB (14, 23.3%); control (7, 11.1%). SAE (n): TCB (1), control group (2) | No benefit on disease progression was observed compared with standard care |
| REMAP-CAP Investigators, et al. (2021) | United Kingdom, Australia, Canada, New Zealand, France | RCT, MC, open label | 865; 629 M:236 F | P/F: 116.5 (89–165) mmHg | CRP-µg/ml: 136 (79–208) | TCB, sarilumab | Standard of care | Median days from hospital admission to enrollment (IQR): 1.2 (0.8–2.8) | TCB: 8 mg/kg (up to a maximum of 800 mg), 1 to 2 doses; sarilumab: 400 mg, 1 dose | Intravenous | DB (304), Kidney disease (81), respirator (206) | COVID-19 antivirals, corticosteroid | The analysis of 90-day survival showed that the survival rate of the IL-6 inhibitor groups was improved. Compared with the control group, the HR was 1.61 (95%CI 1.25–2.08) and the posterior probability of superiority was more than 99.9% | SAEs: 9 in the TCB group, 11 in the control group, and 0 in the sarilumab group | In critical patients with organ support, treatment with TCB and sarilumab improved the outcomes |
| Canziani et al. (2020) | Italy | MC, retrospective cohort | 128; 94 M:34 F | P/F, mean (SD): 94 (67) mmHg | Ferritin, mean (SD)-ng/ml:1,604 (1,201); CRP, mean (SD)-g/dl: 19.1 (8.6) | TCB + standard of care | Standard of care | Time since symptom onset (SD): 11 (6) | 8 mg/kg per dose, followed by a second dose 24 h later if no clinical worsening occurred | Intravenous | CCI, mean (SD): 2.4 (1.6); HTN (66) | HCQ, azithromycin, glucocorticoids | TCB did not significantly affect the risk of death, but TCB was associated with the use at baseline of NIV or invasive MV and the presence of comorbidities | TCB was not associated with the risk of infections, bleeding, or thrombosis | TCB did not affect the 30-day mortality in severe respiratory impairment patients |
| Menzella et al. (2020) | Italy | SC, retrospective, case–control study | 79; 56 M:23 F | SOFA score: mean (SD): 4.3 (1.3) | CRP, mean (SD)-mg/dl: 11.9 (7.2); IL-6, mean (SD)-pg/m: 147.2 (180.4) | TCBb + standard therapy | Standard therapy | – | Intravenous: 8 mg/kg—max 800 mg, Q12 h; subcutaneous: 2 to 4 doses of 162 mg | Intravenous | Number of comorbidities, mean (SD): 2.9 (2.1) | HCQ (20), azithromycin (60), methylprednisolone | The probability of death and intubation in patients treated with TCB was significantly lower than that in patients not treated with TCB | 2 patients treated with TCB developed cavitating lung lesions | TCB may be helpful in COVID-19 patients with severe respiratory impairment receiving NIV |
| Fisher et al. (2021) | United States | SC, retrospective cohort study | 115; 80 M:35 F | SOFA score within 24-h intubation: 6.0 (3.0) | CRP-mg/dl: TCB 19.5 (15.7); control 17.6 (18.0); ferritin-ng/ml: TCB 1,507 (1,518), control 1,462 (1,435) | TCB + standard of care | Standard of care | Mean time from intubation to treatment was 2.5 days | 400 mg/dose | Intravenous | CCI: TCB 2.0 (3.0), control 3.0 (3.0) | HCQ (108), corticosteroids | No reduction in mortality associated with receipt of TCB | The increased risk of secondary infection in patients given TCB was not observed | TCB was not associated with a reduction in mortality in MV patients with COVID-19 after controlling for severity of illness, age, and co-morbidities |
| Campochiaroa et al. (2020) | Italy | SC, retrospective, cohort | 65; 56 M:9 F | P/F-mmHg: TCB 107 (82–181), control 124 (91–172) | CRP-mg/L: TCB 156 (100–208); control: 169 (98–226); ferritin-ng/ml: TCB 1,400 (1,027–2,777); 1,448 (793—4,131) | TCB + standard treatment | Standard treatment | Duration of symptoms (days): TCB11 (8–14); control: 9 (8–10) | 400 mg/dose; in case of respiratory worsening, a second dose was given after 24 h | Intravenous | HTN (28), CKD (8), DB (10), CAD (10) | HCQ, azithromycin | During the 28-day follow-up, mortality was 33% in the standard treatment group and 33% in the TCB group | The rate of pulmonary thrombosis and infection was similar between the two groups | At day 28, compared to standard treatment, the clinical improvement and mortality were not statistically different |
| Vazquez Guillamet et al. (2021) | United States | SC, retrospective cohort study | 43; 16 M:27 F | P/F-mmHg: 171.5 (122–221) | CRP- mg/dl:142.7 (97.7–213.7); IL-6-pg/ml: 61 (28.6–439) | TCB + standard care | Standard care | – | 8 mg/kg, a second dose at 12–24 h later | Intravenous | DB (12), CKD (17), CAD (11); Charlson score, median (IQR): TCB 0 (0–3), control 2 (0–4) | —— | Treatment with TCB was a significant predictor of survival | Treatment with TCB might increase the risk of infection | After adjusting for severity of critical illness, administration of IL-6 inhibitor was associated with improved survival |
| Rajendram et al. (2021) | United States | MC, retrospective observational cohort | 164; 103 M:61 F | SOFA score, mean (SD): TCB 6.0 (3.3), control 6.4 (3.6); P/F, mean (SD)-mmHg: TCB 134.8 (68.4), control 149.8 (82.2) | CRP, mean (SD)-mg/dl: TCB 20.4 (10.1), control 17.2 (12.3); ferritin- ng/ml: TCB 1,398.2 (1,143.3), control 4,159.9 (13,454.1) | TCB | Did not receive TCB | – | 4–8 mg/kg (maximum dose 400 mg), one dose only | Intravenous | DB (67), COPD (48) | HCQ (88), azithromycin (78), systemic corticosteroids | ICU mortality was lower in the TCB group, with more hospital-, ICU-, and vasoactive-free days at day 28 compared with those who did not receive TCB. There was no difference in MV-free days at day 28 or development of secondary infections | There was no difference in the rates of secondary infection | Administration of TCB might decrease in ICU mortality of critical COVID-19 patients with severe hypoxemic respiratory failure |
| TCB use was associated with a significant decrease in ICU death rate in critically ill COVID-19 patients with severe hypoxemic respiratory failure | |||||||||||||||
| Huang et al. (2021) | United States | SC, retrospective cohort study | 96; 64 M:32 F | SOFA score median (range): TCB 4 (0–13), non-TCB 5 (0–13) | CRP, median (range)-mg/L: TCB 122.3 (2.4–327.2); non-TCB 122.5 (11.10–343.1) | TCB | Non-TCB | Median (range): TCB:2 (0–16) | A single 400 mg dose | Intravenous | HTN (62), cardiac arrhythmias (33), DB (47), other comorbidities (84) | HCQ (63), azithromycin (69), and remdesivir (9), DXMS | Fewer deaths were observed among TCB-treated patients, both in the overall population and among the subgroup of patients requiring MV | Secondary infections were not different between the two groups and were predominantly related to invasive devices, such as urinary and central venous catheters | Administration of TCB was associated with fewer deaths compared to non-treatment despite predominantly being used in patients with more advanced respiratory disease |
| Galván-Román et al. (2021) | Spain | SC, retrospective observational study | 146; 97 M:49 F | Baseline P/F, median (p25–p75): 215 (112–310) | CRP, median (p25–p75)-mg/dl: 11.55 (5.16–22.53) | TCB | Not treated with TCB | Duration of symptoms at admission, median (p25–p75)-d: 6 (4–7) | 8 mg/kg (maximum 800 mg) followed by a second one after 12 h | Intravenous | Comorbidities, median (p25–p75): 100 (69) | HCQ (136), azithromycin (82), Lpv/Rtv(119), and glucocorticoids | Early TCB treatment might improve in oxygenation (P/F) in patients with high IL-6. Patients with high IL-6 not treated with TCB showed a high mortality as well as those with low IL-6 treated with TCB | Relevant SAEs were not observed in TCB-treated patients | Baseline IL-6 more than 30 pg/ml predicts IMV requirement in patients with COVID-19 and contributes to the establishment of an adequate indication for the treatment of TCB |
| Saffo et al. (2021) | United States | Retrospective cohort | 130; 93 M:37 F | SOFA score mean (SD): TCB 5.7 (2.2); control 6.0 (3.2) | Mean (SD) IL-6-pg/ml: TCB 108.8 (179), control 62.3 (105.3); mean (SD) CRP-mg/dl: TCB 13.2 (7.4); control: 12.6 (6.4) | TCB | Did not receive TCB | Mean (SD) symptom onset to admission: TCB 6.9 (3.4); control 7.1 (4.4) | A dose of 8 mg/kg; 400 mg single dose | Intravenous | HTN (98), DB (53), COPD (27), CA (24) | HCQ, azithromycin, methylprednisolone | A Kaplan–Meier survival curve demonstrated no difference in survival between TCB and comparator patients. In the multivariable Cox regression model for mortality at 30 days, administration of TCB was not associated with decreased mortality | Positive blood culture was not statistically significant between the groups | No difference in survival was observed in critical patients treated with TCB |
| Somers et al. (2021) | United States | SC, observational controlled cohort | 154; 102 M:52 F | P/F (n = 80): 165 (136.5–231.5) mmHg | CRP-mg/L: 220 (125–293); ferritin-ng/ml:1,418 (692–2,139) | TCB | Did not receive TCB | – | 8 mg/kg (maximum 800 mg) × 1 dose | Intravenous | HTN (102), DB (25), CKD (64), asthma (31) | HCQ, remdesivir, corticosteroid | In IPTW-adjusted models, TCB was associated with a 45% reduction in hazard of death | TCB was associated with an increased proportion of patients with superinfections, but there was no difference in the 28-day case fatality rate between the two groups | In the cohort, administration of TCB was associated with a lower mortality in spite of higher superinfection occurrence |
| Brosnahan et al. (2021) | United States | MC, retrospective cohort | 537; 366 M:171 F | SOFA score: TCB:7 (7–9); control: 8 (3–10) | —— | Steroid + TCB | Steroid | – | A total of 90% of patients received 400 mg as a single dose | Intravenous | HTN without complication (394); DB without complication (229) | Antivirals, immune globulins, HCQ, methylprednisolone, DXMS, hydrocortisone, prednisone | The combination group (TCB 400 mg and daily equivalent DXMS 10 mg) had an improved 28-day mortality compared with the steroid-only group (daily equivalent DXMS 10 mg) without increasing the risk of infection | There was no statistical significance difference in the rate of infections between the propensity-matched groups | The combination group had an improved 28-day mortality compared with the steroid-only group without increasing the risk of infection |
| Corominas et al. (2021) | Spain | Single-center, observational study | 104; 72 M:32 F | P/F, mean (SD): 201.3 (78.1) mmHg | IL-6-pg/ml, mean (SD): 171.6 (40–210.7); CRP-mg/L, mean (SD): 198.4 (161.5) | TCB | – | If ≥75 kg: a single dose of 600 mg, less than <75 kg: a single dose of 400 mg | – | HTN, dyslipidemia, obesity, CLD, DB | HCQ | The overall mortality rate was 5.8% patients. Mortality in hospitalized non-TCB treated patients was 10%. The regional death rate was 11% | – | Early treatment of IL-6 inhibition in COVID-19 patients with imminent hyper-inflammatory response may be safe and effective | |
| Cavalli et al. (2021) | Italy | Cohort study | 392; 301 M:91 F | P/F ≤ 300 mmHg | CRP-mg/L: 129 (100–171) | Anakinra, tocilizumab, sarilumab | No interleukin inhibitors | None | Anakinra: 5 mg/kg/dose twice daily (total daily dose of 10 mg/kg) until clinical benefit. TCB: 400 mg/dose, which was repeated after 24 h if the respiratory function further worsened; sarilumab: 400 mg/dose | Intravenous | CAD (119); history of neoplasia (66); DB (72) | HCQ, glucocorticoid | There was no difference in adverse clinical outcome risk in patients treated with IL-6 or IL-1 inhibition relative to patients who did not receive interleukin inhibitors | – | IL-1 inhibition was associated with a significant reduction of mortality in COVID-19 patients. IL-6 and IL-1 inhibition were effective in patients with low lactate dehydrogenase concentrations |
| Abe et al. (2020) | Japan | Case reports | 2; 1 M:1 F | PLT <20*109/L | P1: IL-6-pg/ml: 47.8; P2: IL-6-pg/ml: 93.6 | TCB | Days from symptom onset to TCB application: P1: 8 days later; P2: 4 days later | 8 mg/kg of TCB twice | Intravenous | DB; KD | P1: peramivir and favipiravir; P2: peramivir and favipiravir, immunoglobulin | P1: He was released from the isolation unit on day 29. P2: She was released from the isolation unit on day 36 based on negative results of PCR assays | – | Anti-cytokine therapy might be effective for severe COVID-19 in end-stage renal disease patients | |
| Patel et al. (2020) | United States | Case reports | 1; F (12 years old) | PLT <10*109/L | IL-6-pg/ml: 34; CRP-mg/dl: 8.3 | TCB | Days from symptoms onset to TCB application: 12 | 2 doses of TCB (8 mg/kg 12 h apart) | Intravenous | Severe thrombocytopenia | HCQ, remdesivir, immunoglobulin; methylprednisolone | Discharged | – | Treatment with cytokine-directed agents such as TCB could be considered in critical patients | |
| Mady et al. (2020) | Saudi Arabia | A case series | 61; 54 M:7 F | SpO2/FiO2, median (IQR): 162 (145–209.2) mmHg | CRP, median (IQR)-mg/L: 31.7 (30.5–49.9) | TCB | – | 8 mg/kg (two consecutive intravenous infusions 12 h apart) | Intravenous | More than one comorbidity (%): 38 (62.3%) | Lpv/Rtv or ribavirin | Administration of TCB did not affect the mortality of critical COVID-19 patients | No SAEs due to TCB were recorded; 12 patients developed nosocomial acquired infections | TCB could be an adjunct safe therapy in rapidly evolving COVID-19 and associated critical illness | |
| Bernardo et al. (2020) | Italy | Case reports | 1; M | P/F: 295 mmHg | CRP-mg/L: 89.8 (9 × the upper limit of normal) | TCB | 8th day of admission | Two doses of TCB 8 mg/kg administered 12 h apart | Intravenous | Hypertensive cardiomyopathy, paroxystic AF, CRD | HCQ, Lpv/Rtv | On day 30 after the TCB injections, the ANC of the patient began to improve in spite of far-from-normal values | Severe prolonged neutropenia | Considering the increasing use of TCB in COVID-19 patients, this case warrants further studies regarding the possible adverse hematological effects that need to be monitored in order to prevent superimposed infections | |
| Morillas et al. (2020) | United States | Case reports | 5; 2M:3F | P1: P/F: 196 mmHg; P2: P/F: 200 mmHg; P3: P/F: 113 mmHg; P4: P/F: 283 mmHg; P5: P/F: 156 mmHg | P1: CRP-mg/dl: 9.7, IL-6-pg/ml: 7; P2: CRP-mg/dl: 18.8, IL-6-pg/ml: 13; P3: CRP-mg/dl 36.5, IL-6-pg/ml: 438; P4: CRP-mg/dl: 5.2; P5: CRP-mg/dl: 32.7 | TCB | TCB administration after symptoms onset (day): P1: 7; P2: 5; P3: 10; P4: 13; P5: 12 | P1: 400 mg/dose; P2: 400 mg/dose; P3: 400 mg/dose; P4: 310 mg/dose (adjusted based on weight); P5: 400 mg/dose | Intravenous | P1: HTN, kidney transplants; P2: lung transplant, DB, HF, HTN, hemodialysis, CA; P3: a motor vehicle accident on tacrolimus; P4: liver transplant, rheumatic heart disease, CKD stage 3; P5: HTN, DB, pulmonary embolism, coronary artery by-pass graft surgery, and kidney transplantation | P1: Lpv/Rtv; P2/3: HCQ, steroids | P1/2/3/5: discharged; P4: Ddied | There were no immediate drug-related side effects, although 2 patients developed 3 proven bacterial infections within 14 days after dosing | TCB can be used without major direct toxicity in SOT/CTTRs early after initiation of MV due to COVID-19, regardless of type of organ transplanted | |
| Cascella et al. (2020) | Italy | Case reports | 1; M | P/F: 150 mmHg | CRP-mg/L: 193; IL-6-pg/ml: 93 | TCB | 2nd day of admission | 8 mg/kg, 800 mg | Intravenous | – | Lpv/Rtv, HCQ | Discharged | – | The combination of IL-6 inhibitor with calibrated ventilatory strategies may improve outcomes | |
| AL-Kaf et al. (2021) | Kingdom of Saudi Arabia | Case reports | 1; M | P/F: 133 mmHg | IL-6-pg/ml: 130 | TCB | 5th day of admission | – | – | Down syndrome | Hydrocortisone | After a total of 31 days of MV support, the patient was successfully weaned off and planned for tracheostomy closure | – | This is a rare critical presentation of COVID-19 in a Down syndrome patient with cardiac tamponade, ARDS, and severe hypothyroidism who responds well to pericardiocentesis, levothyroxine, hydrocortisone and TCB | |
| Eroglu et al. (2021) | Turkey | Case reports | 1; M | P/F: 204 mmHg | IL-6-pg/ml: 14 (0–6.4); CRP-mg/L: 78 (0–5) | TCB | 8th day of admission | TCB 400 mg was infused 2×/day for 2 days | Infused intravenously | HTN | Favipiravir, oseltamivir, HCQ | On day 14, the patient was transferred to a negative COVID-19 service with negative PCR test and better clinical condition | – | Patients with severe COVID-19 should be monitored for hemophagocytic lympho-histiocytosis syndrome, and TCB can be used early under NIV delivered by helmet mask | |
| Kataoka et al. (2021) | Japan | Case reports | 1; M (age 85) | P/F: 100 mmHg | CRP-mg/dl: 13.02; IL-6-pg/ml: 154 | TCB | – | A single dose of 480 mg/body | Intravenous | Sjögren’s syndrome | Favipiravir, ciclesonide | Discharged | – | IL-6 inhibition may be an optional treatment in patients with a severe respiratory condition | |
| Kishaba et al. (2021) | Japan | Case reports | 1; M (age 74) | P/F: 115 mmHg | CRP-mg/dl: 32 | TCB | On the day of admission | 480 mg (8 mg/kg/day) | Intravenous | HTN | Favipiravir, methylprednisolone | Discharged | – | In order to secure good outcomes in critical COVID-19 patients, early administration of intensive combination therapy requires suppression of both viral replication and inflammation | |
| Leelayuwatanakul et al. (2021) | Thailand | Case reports | 2; 1 M:1 F | P1: P/F: 260 mmHg; P2: P/F: 130 mmHg | P1: CRP-mg/L 228; IL-6-pg/ml: 1,091; P2: hs-CRP-mg/L:225; IL-6-pg/ml: 426.2 | TCB | P1: 8th day of admission; P2: 4th day of admission | 400 mg/dose | Intravenous | P1: HIV infection, DB, dyslipidaemia; P2: relapse multiple myeloma, triple vessel disease, DB, HTN | Favipiravir, HCQ, darunavir/ritonavir, immunoglobulin | Discharged | – | Combined therapeutic modalities are promising treatment for severe COVID-19 infection in the immunocompromised host. Timely adjunctive therapies that alleviate overwhelming inflammation may improve the outcome | |
| McKenzie et al. (2021) | United States | Case series | 16; 9M:7 F | P/F: 84 (IQR: 69–108.6) mmHg | CRP-mmol/L: 219.6 ± 72.1; IL-6-pg/ml: 248.7 (IQR: 69.5–719.2) | TCB | Time from admission to administration: 7.08 ± 3.5 (days) | 400 mg (400–600) | Intravenous | HTN (31%); DB (25%) | HCQ, convalescent plasma, steroids | 8 (50%) patients were discharged home, 7 (44%) patients died, and 1 (6%) patient was still hospitalized at the end of data collection | – | The study did not support the effectiveness of TCB in the treatment of critical COVID-19 patients | |
| Nourié et al. (2021) | France | Case reports | 1; M | SOFA score: 13 | CRP-mg/L: 62.2 | TCB | On day 7 of the illness | 400 mg/dose | – | Von Hippel–Lindau; HTN; DB; CAD | HCQ, hydrocortisone | Discharged | – | A single dose of 400 mg of TCB was effective and well tolerated | |
| Ladna et al. (2021) | United States | Case series | 2; 2 M | P1: P/F: 117 mmHg; P2: P/F: 116 mmHg | P1: IL-6-pg/ml 45; hs-CRP-mg/L: 74.9; P2: IL-6 pg/ml:31; hs-CRP-mg/L: 244 | TCB | First hospital day | 400 mg/dose | – | P1: CAD, DB, HTN, and prior stroke; kidney and heart transplant; P2: chronic hepatitis B complicated by hepatocellular carcinoma status post orthotopic liver transplant, HTN, DB | HCQ, P1: tacrolimus, hydrocortisone, mycophenolate; P2: hydrocortisone | Discharged | – | TCB appears to hold promise for critical COVID-19 patients who require MV when given shortly after intubation | |
| Senegaglia et al. (2021) | Brazil | Case report | 1; M | P/F: 87 mmHg | CRP-mg/ml: 25.3 (<5.0) | TCB | 2nd, 3rd hospital day | 400 mg/dose for 2 days | Infusion | HTN, urethral stenosis | DXMS | Discharged | No adverse events | Administration of TCB and mesenchymal stromal cells proved to be safe, and the results of the report prove to be a promising alternative in patients with severe acute respiratory syndrome | |
| Thammathiwat et al. (2021) | Thailand | Case report | 1; M | P/F: 226 mmHg | IL-6-pg/ml: 17.1 (reference level <7) | TCB | 6th hospital day | 8 mg/kg/dose | – | Kidney transplantation, HTN, dyslipidemia, and post-transplant DB | Darunavir, ritonavir, favipiravir, tacrolimus, prednisolone, and immunoglobulin | COVID-19 was undetected | – | For this COVID-19 patient with kidney transplant, favipiravir together with decreased immunosuppression and IL-6 inhibitor antibody provides favorable outcomes. Decision on timing for IL-6 inhibitor initiation can be guided by IL-6 level monitoring | |
| Lescure et al. (2021) | Argentina, Brazil, Canada, Chile, France, Germany, Israel, Italy, Japan, Russia, and Spain | MC, RCT | 416, 261 M:155 F | SpO2/FiO2, median (IQR)-mmHg: 237.5 (173.6–300.0) | CRP-mg/L: 94.6 (48.1–167.9); IL-6-pg/ml: 12.3 (4.8–25.5) | Sarilumab | Placebo | Time from dyspnea onset to baseline, days: 5.0 (2.0–9.0) | 200 mg, 400 mg | Intravenous | HTN (177), DB (110), CA (42), obesity (86), HL (41), CAD (22), COPD (18) | HCQ/CQ, azithromycin, remdesivir, convalescent plasma, and corticosteroids | At day 29, there were numerical, non-significant survival differences between sarilumab 400 mg and placebo for critical COVID-19 patients | No unexpected safety signals were seen | The result of this study did not show the efficacy of sarilumab in patients admitted to the hospital with COVID-19 and receiving supplemental oxygen |
| Della- Torre et al. (2020) | Italy | SC, open- label cohort study | 56; 44 M:12 F | P/F <300 mmHg | CRP-mg/L: 152 (116–210); ferritin-ng/ml: 1,376 (1,023–6,927) | Sarilumab + standard care | Standard of care | Duration of symptoms before enrollment (days): 7 (7–10) | 400 mg | Intravenous | HTN (17), DB (9), HLD (8), COPD (2), and CAD (6) | HCQ, Lpv/Rtv, azithromycin, corticosteroids | A total of 61% of patients treated with sarilumab experienced clinical improvement and 7% of patients died. These findings were not significantly different from the comparison group (clinical improvement 64%, mortality 18%) | The rate of pulmonary thrombosis and infection was similar between the 2 groups | Overall mortality and clinical improvement were not significantly different between standard of care and sarilumab. Sarilumab was associated with faster recovery in a subset of patients showing minor lung consolidation at baseline |
| Gremese et al. (2020) | Italy | SC, observational cohort | 53; 47 M:6 F | P/F-mmHg: medical wards 146 (120–212), ICU 112 (100–141.5) | – | Sarilumab + standard care | No control group | – | 400 mg, 1 to 2 doses | Intravenous | 34 (64.2%) had at least one comorbidity | Darunavir/ritonavir; Lpv/Rtv | Within the medical wards, 89.7% of inpatients significantly improved, 70.6% were discharged. Within the ICU, 64.2% were discharged from ICU to the ward and 35.8% were still alive at the last follow-up | Sarilumab appears to be safe | IL-6 receptor inhibition leads to good clinical outcome in severe COVID-19 patients, and sarilumab is a safe and effective alternative in the therapeutic armamentarium of this disease without a defined standardized treatment |
| Kyriazopoulou et al. (2021a) | Greece, Italy | MC, RCT | 594; 344 M:250 F | SOFA score, mean (SD): 2.4 (1.1); P/F-mmHg: 237 (181–301) | CRP, mean (SD)-mg/L: 50.6 (25.3–99.7); IL-6, mean (SD)-pg/ml: 16.8 (7.0–39.8); ferritin, mean (SD)-ng/ml: 585.2 (294.5–1,047.0) | Anakinra + standard of care | Placebo + standard of care | From symptom onset to start of study drug (days), median (Q1–Q3) 9 (7–11) | 100 mg/daily,7–10 days | Subcutaneous | CCI, mean (SD): 2.2 (1.6); DB (94), chronic heart failure (18), CRD (10), COPD (24), CAD (41), Atrial fibrillation (28), depression (34) | Remdesivir, DXMS | Anakinra protected from severe disease or death; the 28-day mortality decreased | The incidence of treatment-emergent SAEs through day 28 was lower in patients in the anakinra combined with standard of care group compared to the placebo combined with standard of care group | Early administration of anakinra guided by suPAR shows 2.78 times better improvement of overall clinical status in moderate and severe COVID-19 |
| Bozzi et al. (2020) | Italy | SC, prospective observational cohort | 120; 96 M:24 F | P/F-mHg: 151 (105–204.5), 32.5% patients on MV | Ferritin-mcg/L: 1,555 (1,239–2,679); CRP-mg/dl: 15.2 (10.8–23.1) | Anakinra + methylprednisolone + standard treatment | Methylprednisolone + standard treatment | Days between hospitalization and inclusion: intervention: 3 (1–6); control: 1 (0–2) | 200 mg q8 h for 3 days and then 100 mg q8h up to day 14 | Intravenous | Median CCI was 0 (IQR 0–1) | HCQ, Lpv/Rtv, remdesivir, methylprednisolone | At 28 days, mortality was 35.6% in controls and 13.9% in treated patients. Unadjusted and adjusted risk of death was significantly lower for treated patients compared to controls | No significant differences in laboratory alterations or bloodstream infections were observed | Administration of anakinra combined with methylprednisolone may be an effective therapy in COVID-19 patients with respiratory failure and hyper-inflammation, also on MV |
| Franzetti et al. (2021) | Italy | MC, retrospective cohort study | 112; 87 M:25 F | P/F: 133 (110–196) mmHg | CRP-mg/dl: 17.5 (11.0–24.9); ferritin-ng/ml: 1,620 (918–2,988) | Anakinra + standard of care | Standard of care | Symptom duration before hospitalization: 7 (5–10) | Regular ward: 7 days at a dosage of 100 mg four times a day, subcutaneous; ICU: 200 mg three times daily, intravenous | Intravenous or subcutaneous | CCI median (IQR): 3 (2–4); HTN (59), ischemic heart disease (20), COPD (8), DB (19) | HCQ, Lpv/Rtv | Survival at day 28 was significantly higher in anakinra-treated patients than in the controls. When stratified by continuous positive airway pressure support at baseline, the survival of anakinra-treated patients was also significant compared with the controls | No significant difference was observed in the rate of infectious-related adverse events between groups | Anakinra improved the invasive ventilation-free survival and overall survival and was well tolerated in patients with ARDS associated with COVID-19 |
| Kyriazopoulou et al. (2021b) | Greece | MC, cohort | 260; 165 M:95 F | SOFA score: 2 (1); P/F mmHg: anakinra 293.3 (195.7–371.2), parallel SOC after propensity matching 285.7 (208.5–371.7) | CRP-mg/L: anakinra 47.4 (14.3–105.5), parallel SOC after propensity matching 68.8 (19.7–141.8) | Anakinra + SOC | SOC | Days from onset of symptoms to start of treatment, median (range): anakinra 8 (1–23), parallel SOC after propensity matching 7 (1–12) | 100 mg once daily for 10 days | Subcutaneous | CCI, mean (SD): 3 (2); DB (73), CAD (21), CRD (5), HTN (125), COPD (18) | HCQ, remdesivir, azithromycin, DXMS | 22.3% with anakinra treatment and 59.2% comparators progressed into severe respiratory failure; the 30-day mortality was 11.5 and 22.3%, respectively | The rate of SAEs was lower among anakinra-treated patients | Early soluble urokinase plasminogen activator receptor guided anakinra decreased severe respiratory failure and restored the pro-/anti-inflammatory balance |
| Erden et al. (2021) | Turkey | SC, retrospective case review | 17; 12 M:5 F | SOFA score, median IQR: 3 (3) | CRP-mg/L: 45.6 (101.8); ferritin concentration-μg/L: 397 (307) | Anakinra | No control group | Duration of COVID-19 symptoms before anakinra, days: 7 (4.5) | 100 mg/12 h from day (D) 1 to D3, then at 100 mg/24 h from D3 to D5 | Subcutaneously | HTN (9), DB (4), asthma (1), CAD (3), CA (1) | HCQ, azithromycin, favipiravir | The mortality rate was 17.6%; 1 patient was receiving low-flow oxygen supply, 3 patients no longer needed oxygen supply, and 10 patients were discharged | Treatment was well tolerated | The other factors that enhance the administration of anakinra in the situation of viremia could also be sorted as no response to full-dose antiviral drugs, antiviral side effects, or no success to antiviral treatment |
| Filocamo et al. (2020) | Italy | Case report | 1; M | P/F:160 mmHg | – | Anakinra | Day 10 after admission | 200 mg intravenously followed by 100 mg/6 h subcutaneously | Intravenous and subcutaneous | – | Lpv/Rtv, HCQ | Discharged | – | This critical COVID-19 patient was successfully treated with IL-1 receptor antagonist | |
| Franzetti et al. (2020) | Italy | Case report | 1; M | P/F: 50 mmHg | – | Anakinra | Day 7 after admission | 100 mg/6 h | Subcutaneous | – | Lpv/Rtv, remdesivir | By day 16, a substantial improvement in the respiratory function of the patient was also noticed, with SaPO2 levels of 92% while on Venturi mask | – | This report highlights the high tolerability and the interesting immunomodulatory profile of anakinra in the setting of severe patients associated with remdesivir therapy | |
| Cremer et al. (2021) | United States | MC, RCT, double-blind | 40; 26 M:14 F | Baseline SOFA score, median (IQR): 2 (2–3); baseline P/F-mmHg: 137 (88–193) | CRP-mg/dl: 13.1 (9.8–18.8); ferritin-ng/ml: 1,040 (486–1860) | Mavrilimumab | Placebo | Time from symptom onset to hospitalization: 7 (4–8) | A single dose of 6 mg/kg | Intravenous | HTN (22), DB (17), HL (18), CAD (4) | Antiviral drugs, convalescent plasma, corticosteroids, other immunosuppressive agents | At 14 days, 12 patients in the mavrilimumab group were alive and off supplemental oxygen therapy compared with 9 patients in the placebo group | Adverse events were similar between groups. Treatment-related deaths were not observed | There was no significant difference in the proportion of patients alive and off oxygen therapy at day 14; despite the harm or benefit of mavrilimumab therapy in this patient population, it remains possible given the wide confidence intervals |
| De Luca et al. (2021) | Italy | SC, prospective cohort | 39; 29 M:10 F | P/F-mmHg (KPa): mavrilimumab 196 (167–215), control 217 (138–258) | CRP-mg/L: mavrilimumab 152 (100–177), control 123 (77–190); ferritin, µg/L: mavrilimumab 2,302 (1,040–3,217), control 1,269 (854–3,369) | Mavrilimumab + standard of care | Standard of care | Fever duration (days): mavrilimumab 11 (10–12), control 7 (4–10) | A single dose of 6 mg/kg | Intravenous | – | HCQ, Lpv/Rtv, azithromycin | During the 28-day follow-up, 7 patients in the control group died, and no patient in the mavrilimumab group died. At day 28, 17 patients in the control group showed clinical improvement and all patients in the mavrilimumab group. Fever resolution was faster in mavrilimumab recipients versus controls | Mavrilimumab group with no infusion reactions; 3 patients in the control group developed infectious complications | Treatment of mavrilimumab was associated with improved clinical outcomes compared with standard care in non-MV patients with severe COVID-19 and systemic hyper-inflammation |
MC, multi-center; SC, single-center; F, female; M, male; IL-6, interleukin-6; CRP, C-reactive protein; ALT, alanine aminotransferase; INR, international normalized ratio; PLT, platelet; AF, atrial fibrillation; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; DB, diabetes; CKD, chronic kidney disease; HL, hyperlipidemia; CVI, cardiovascular impairment; CVD, cardiovascular disease; HTN, hypertension; HI, hepatic impairment; HF, heart failure; CA, cancer; CLD, chronic lung disease; CCD, chronic cardiac disease; CPD, chronic pulmonary disease; AMN, active malignant neoplasm; NIV, noninvasive ventilation; MV, mechanical ventilation; CI, confidence interval; TCB, tocilizumab; CP, cumulative percentage; SAE, serious adverse events; AE, adverse events; HCQ, hydroxychloroquine; Lpv/Rtv, lopinavir/ritonavir; IFN, interferon; HR, hazard ratio; OR, odds ratios; P/F, PaO2:FiO2; SOC, standard of care; KD, kidney disease; IPTW, inverse probability treatment weighting; DXMS, dexamethasone; P, patient; SOT/CTTR, solid organ and composite tissue transplant recipients; CCI, Charlson Comorbidity Index; suPAR, soluble urokinase plasminogen activator receptor.
3.4 Results of the Meta-analysis
We cannot conduct a quantitative analysis of anakinra, sarilumab, and mavrilimumab for some outcomes, owing to differences in outcomes reported, study design, and limited study numbers. Especially for mavrilimumab, only one RCT and one cohort met the inclusion criteria. If we could not perform a meta-analysis, we commented on the results from all included studies.
3.4.1 Mortality Outcome (All-Cause Mortality at Days 28–30)
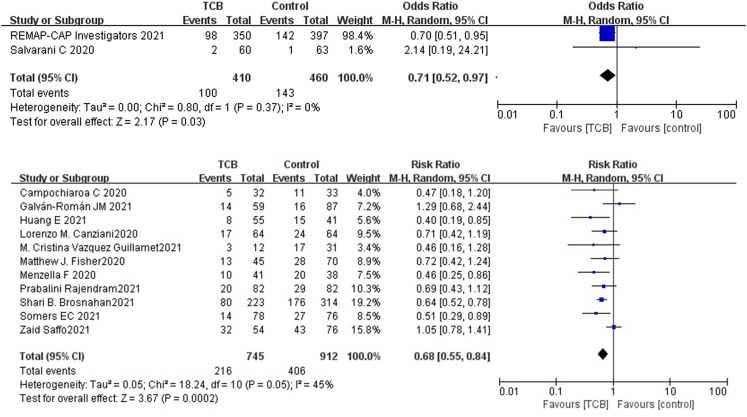
Tocilizumab
Among the 14 controlled studies, one RCT and 6 cohorts neither reported a difference for mortality at days 28–30 between the tocilizumab and control groups. Compared to the control group, the results of RCTs showed that the use of tocilizumab for patients with COVID-19 (at the edge of sepsis) might decrease the mortality rate (OR 0.71, 95%CI: 0.52–0.97, I 2 = 0%), and there was a significant difference between the two groups (Figure 2A). The non-RCTs showed a similar result (RR 0.68, 95%CI: 0.55–0.84, I 2 = 45%), and there was statistical significance (Figure 2B).
FIGURE 2.
(A) Results from randomized controlled trials (RCTs): the mortality outcome of tocilizumab for COVID-19 (at the edge of sepsis).
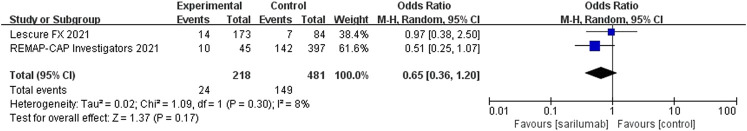
Sarilumab
For sarilumab, of the studies that met the inclusion criteria, only two RCTs (one of the RCTs studied tocilizumab and sarilumab) and two non-RCTs provided data on mortality outcome. Among the two non-RCTs, one cohort did not set up a control group. Compared to the control group, the results of RCTs showed that the use of sarilumab for patients with COVID-19 (at the edge of sepsis) might reduce the mortality rate (OR 0.65, 95%CI: 0.36–1.2, I 2 = 8%), but there was no significant difference between the two groups (Figure 3). However, due to the lack of research, data synthesis for outcomes of non-RCTs was not conducted.
FIGURE 3.
Results from randomized controlled trials: the mortality outcome of sarilumab for COVID-19 (at the edge of sepsis).
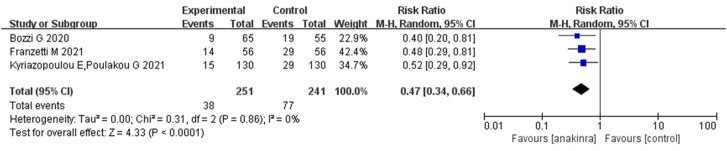
Anakinra
For anakinra, of the studies that met the inclusion criteria, 1 RCT and 4 non-RCTs provided data on mortality outcome. Due to the insufficiency of RCTs, we only quantitatively synthesized the results of non-RCTs. Compared to the control group, the results of non-RCTs showed that the use of anakinra for patients with COVID-19 (at the edge of sepsis) might reduce the mortality rate (RR 0.47, 95%CI: 0.34–0.66, I 2 = 0%), and there was statistical significance (Figure 4).
FIGURE 4.
Results from non- randomized controlled trials: the mortality outcome of anakinra for COVID-19 (at the edge of sepsis).
Mavrilimumab
The only RCT, published in 2021, explored outcomes in 21 patients who received mavrilimumab and 19 patients who received placebo. The median (IQR) baseline SOFA score of enrolled patients was 2 (2 to 3). The study reported no significant association with the proportion of patients alive and off oxygen therapy at day 14. The other cohort, published in 2020, explored outcomes in 12 patients who received mavrilimumab and 26 patients who received standard of care. The median (IQR) P/F ratio of the mavrilimumab and control group was 196 (167–215) and 217 (138–258) mmHg, respectively. The study reported that mavrilimumab was associated with a reduced mortality rate and improved clinical outcomes. The benefits of mavrilimumab therapy for those patients remained uncertain, given the insufficient controlled studies and the small sample size.
3.4.2 Safety Outcomes
Treatment-related adverse events (TRAEs) were reported in the majority of research and typically included neutropenia, secondary infections, increase in liver enzymes, and thromboembolism (Table 2). Due to the insufficient studies of safety outcome, we only conducted a quantitative synthesis for tocilizumab.
TABLE 2.
Adverse events (AEs) summarized from controlled studies.
| Author | Immunomodulator | AEs (percentages) |
|---|---|---|
| Salvarani et al. (2021) | Tocilizumab | Control group: 2 severe infections; treatment group: 1 upper gastrointestinal tract bleeding. The most common adverse events were increased alanine aminotransferase level and decreased neutrophil count |
| REMAP-CAP Investigators et al. (2021) | Tocilizumab, sarilumab | Treatment group: 1 secondary bacterial infection, 5 bleeding events, 2 cardiac events, 1 deterioration in vision. Control group: 4 bleeding events, 7 thromboses |
| Canziani et al. (2020) | Tocilizumab | Thrombosis: treatment group (19%), control group (17%). Bleeding: treatment group (17%), control group (13%). Infection: treatment group (31%), control group (39) |
| Fisher et al. (2021) | Tocilizumab | No observed increased risk of secondary infection within 14 days of treatment with tocilizumab |
| Campochiaroa et al. (2020) | Tocilizumab | Pulmonary thrombosis: treatment group (6%), control group (9%). Raised ALT, AST level: treatment group (15%), control group (18%). Neutropenia: treatment group (16%), control group (0) |
| Vazquez Guillamet et al. (2021) | Tocilizumab | Culture-negative sepsis: treatment group (41.7%), control group (19.4) |
| Rajendram et al. (2021) | Tocilizumab | Secondary infection: treatment group (25.6%), control group (25.6%) |
| Huang et al. (2021) | Tocilizumab | Secondary infection: treatment group (31%), control group (17%) |
| Saffo et al. (2021) | Tocilizumab | Bleeding: treatment group (24.1%), control group (14.5%). Blood stream infection: treatment group (7.4%), control group (9.2%). Pulmonary infection (endotracheal aspirates/sputum): treatment group (25.9%), control group (30.3%) |
| Somers et al. (2021) | Tocilizumab | Superinfection: treatment group (54%), control group (26%). Bloodstream infection: treatment group (14%), control group (9%). Pneumonia: treatment group (45%), control group (20%) |
| Brosnahan et al. (2021) | Tocilizumab | Positive blood culture: combination group (steroid + tocilizumab) (11.6%), steroid group (12.7%). Positive Fungitell test: combination group (6.9%), steroid group (10.4%). Positive T2Candida panels: combination group (6.4%), steroids group (6.9%). Cytomegalovirus viral loads elevated: combination group (3.5%), steroids group 4.6% |
| Lescure et al. (2021) | Sarilumab | Serious infection: treatment group (12%), control group (12%). ALT increase: treatment group (31.02%), control group (19%). Invasive bacterial or fungal infection: treatment group (6.9%), control group (4%). Grade ≥2 hypersensitivity reaction: treatment group (2.4%), control group (0%). Grade 4 neutropenia: treatment group (2.7%), control group (0) |
| Della-Torre et al. (2020) | Sarilumab | Infections: treatment group (21%), control group (18%). Neutropenia: treatment group (14%), control group (0). Increase in liver enzymes: treatment group (14%), control group (0). Thromboembolism: treatment group (7%), control group (7%) |
| Kyriazopoulou et al. (2021a) | Anakinra | Infections and infestations: treatment group (8.4%), control group (15.9%). Anemia: treatment group (14.3%), control group (19.6%). Increase of liver function tests: treatment group (35.8%), control group (33.3%). Hyperglycemia: treatment group (36.5%), control group (40.2%). Hyponatremia: treatment group (7.9%), control group (12.2%). Hypernatremia: treatment group (11.4%), control group (9%) |
| Bozzi et al. (2021) | Anakinra | Treatment group: grade ≥3 GGT increase (27.7%), anemia (24.6%), ALT increase (6.2%), granulocytopenia (1.5%). Control group: a comparable proportion of these AEs |
| Franzetti et al. (2021) | Anakinra | Bloodstream infections: treatment group (16%), control group (7.1%). Urinary tract infections: treatment group (3.5%), control group (1.8%). Pneumonia infections: treatment group (7.1%), control group (7.1%) |
| Kyriazopoulou et al. (2021b) | Anakinra | Electrolyte abnormalities: treatment group (26.9%), control group (31.5%). Elevated liver function tests: treatment group (30.8%), control group (39.2%). Gastrointestinal disturbances: treatment group (11.5%), control group (6.9%). Anemia: treatment group (16.9%), control group (20%) |
| Cremer et al. (2021) | Mavrilimumab | Bacterial pneumonia: treatment group (10%), control group (5%). SAEs: treatment group (24%), control group (21%). Circulatory shock: treatment group (10%); control group (5%); Acute kidney injury: treatment group (19%), control group (16%). ALT ≥3ULN: treatment group (24%), control group (16%). AST ≥3ULN: treatment group (29%), control group (21%) |
| De Luca et al. (2020) | Mavrilimumab | Infectious complications: treatment group (0), control group (12%) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transferase; ULN, upper limit of normal.
Tocilizumab
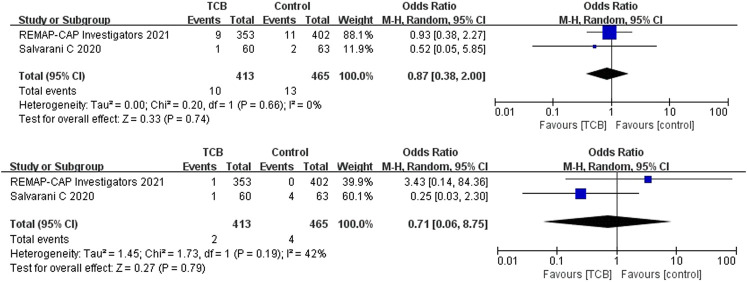
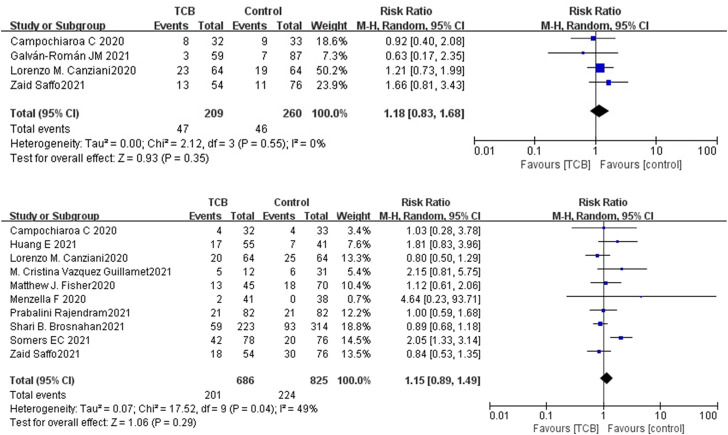
Both 2 RCTs reported SAEs and secondary infections; 4 of 11 non-RCTs reported SAEs and 10 reported secondary infections. Tocilizumab was associated with less SAEs (OR 0.87, 95%CI: 0.38–2.00, I 2 = 0%) and lower rates of secondary infections (OR 0.71, 95%CI: 0.06–8.75, I 2 = 42%) compared with the control groups, which both did not reach significance in RCTs (Figures 5A,B). For non-RCTs, tocilizumab was associated with slightly more SAEs (RR 1.18, 95%CI: 0.83–1.68, I 2 = 0) and secondary infections (RR 1.15, 95%CI: 0.89–1.49, I 2 = 49%) compared with the control arm, but there was no statistical significance (Figures 6A,B).
FIGURE 5.
(A) Results from randomized controlled trials (RCTs): the serious adverse events (SAEs) of tocilizumab for COVID-19 (at the edge of sepsis).
FIGURE 6.
(A) Results from non-randomized controlled trials (non-RCTs): the serious adverse events of tocilizumab for COVID-19 (at the edge of sepsis).
Other Anti-cytokine Agents
The included RCTs reported that the incidence of treatment-emergent SAEs through day 28 was higher in the placebo and standard-of-care group (21.2%) compared to the anakinra and standard-of-care group (16.5%). The non-serious TRAEs were similar in both treatment groups (Kyriazopoulou et al., 2021a). Only two cohorts reported secondary infection outcomes, and none reported SAEs. Both Franzetti M et al. and Bozzi G et al. reported that the rate of adverse events related to infection (or bloodstream infections) was similar between groups—for example, 26.8% occurred in the anakinra group and 16.1% in the control group (Bozzi et al., 2021; Franzetti et al., 2021). Among these infectious events, 9/56 developed bloodstream infections in the anakinra group and 4/56 in the control group (Franzetti et al., 2021). Meanwhile, they all suggested that special attention should be paid to possible infective reactivations or bacterial sepsis due to anakinra. In studies with a comparator arm exploring outcomes from patients who received mavrilimumab or sarilumab, the frequency of TRAEs was similar in both treatment and comparator groups.
3.5 Quality of Evidence
For mortality outcomes, the quality of evidence of tocilizumab for COVID-19 (at the edge of sepsis) was of low and very low quality for RCTs and non-RCTs, respectively. Meanwhile, the quality of evidence of sarilumab and anakinra for COVID-19 (at the edge of sepsis) was of low and very low quality, respectively. As for the SAEs and secondary infections of tocilizumab for COVID-19 (at the edge of sepsis), the quality of evidence was all low for RCTs and very low for non-RCTs, respectively. The results are shown in Supplementary Table S8 (Supplementary Material S2, Appendix p43–45).
4 Discussion
In terms of etiology, sepsis can be classified as bacterial sepsis, fungal sepsis, and viral sepsis based on different pathogens. Sepsis patients with a SOFA score of 2 or more in a general hospital population with presumed infection had an increased risk of death by 2–25 times compared to patients with a SOFA score of less than 2 (Singer et al., 2016; Seymour et al., 2016). The population included in this study was COVID-19 patients with SOFA score ≥2, who were already in the state of sepsis or were about to deteriorate into sepsis, and these patients urgently needed appropriate, safe, and effective treatment. In this study, we evaluated the efficacy and safety of tocilizumab, sarilumab, siltuximab, anakinra, mavrilimumab, and lenzilumab to provide relevant clinical evidence and research ideas for treatment.
4.1 Anti-cytokine Therapy
The local inflammatory response caused by an infection can promote the replacement of damaged tissues by new tissues and play a role in weakening the damage that has occurred, but when excessive inflammation occurs, it may cause systemic inflammatory response syndrome (SIRS) and lead to sepsis. Therefore, timely detection of cytokine storms and proper regulation of inflammatory response may be of great significance to the prevention of sepsis. The “Expert Consensus on Early Prevention and Blocking of Sepsis in China” recommended that when infected patients experience significant increases in cytokines or inflammatory imbalances, the inflammation should be adjusted as soon as possible using glucocorticoids, nonsteroidal anti-inflammatory drugs, traditional Chinese medicine preparations, antibodies targeting inflammatory mediators, etc. (Emergency medicine branch of CPAM et al., 2020). Many studies showed that the factors mainly involved in SIRS and compensatory anti-inflammatory response syndrome include TNF-α, IL-1, IL-6, etc. The Expert Consensus suggested that, for patients with high-risk sepsis infection, cytokine monitoring should be carried out regularly (2–4-h repetition) to find suspected sepsis patients in time. At present, the cytokine commonly detected in hospitals is IL-6. As a cytokine, IL-6 mainly stimulates the proliferation and differentiation of cells involved in immune response and plays an important role in the anti-infection immune response (Emergency Medicine Branch of CPAM et al., 2020).
IL-6 inhibitors include tocilizumab, sarilumab and siltuximab. Tocilizumab and sarilumab were approved for rheumatoid arthritis, and siltuximab was approved for Castleman’s disease. The IL-1 receptor antagonist (anakinra) is a cornerstone treatment for hyperinflammatory conditions such as Still’s disease. Some studies showed that cytokine-directed agents such as IL-6 and IL-1 inhibitors might be effective in the treatment of cytokine storm syndromes, including macrophage activation syndrome and cytokine release syndrome (La Rosée et al., 2019). The GM-CSF blockade included mavrilimumab and lenzilumab, which is designed to prevent and treat cytokine storm (De Luca et al., 2020; Aroldi et al., 2019). This systematic review identified and summarized RCTs, non-RCTs, and case reports (series) to evaluate the effect and safety of tocilizumab, sarilumab, siltuximab, anakinra, mavrilimumab, and lenzilumab. The meta-analysis results showed that tocilizumab might reduce the mortality of patients with COVID-19 (at the edge of sepsis) (RCTs: OR: 0.71, 95%CI: 0.52–0.97, low-certainty evidence; non-RCTs: RR: 0.68, 95%CI: 0.55–0.84, very low-certainty evidence) as was anakinra (non-RCTs: RR: 0.47, 95%CI: 0.34–0.66, very low-certainty evidence). Sarilumab might reduce the mortality of patients with COVID-19 (at the edge of sepsis), but there was no statistical significance (OR: 0.65, 95%CI: 0.36–1.2, low-certainty evidence). For safety outcomes, whether tocilizumab had an impact on SAEs was very uncertain (RCTs: OR: 0.87, 95%CI: 0.38–2.0, low-certainty evidence; non-RCTs: OR: 1.18, 95%CI: 0.83–1.68, very low-certainty evidence) as was on secondary infections (RCTs: OR: 0.71, 95%CI: 0.06–8.75, low-certainty evidence; non-RCTs: RR: 1.15, 95%CI: 0.89–1.49, very low-certainty evidence).
4.2 Special Population
At present, there are still few large-scale randomized controlled prospective studies on COVID-19 (at the edge of sepsis). The experiences of case or case series still have a certain reference significance for clinical treatment, especially for the individualized treatment of special populations, such as critically ill children, immunocompromised individuals, and elderly patients with a variety of chronic diseases. Patel PA et al. reported a case of severe pediatric COVID-19 presenting with respiratory failure and severe thrombocytopenia. On day 7, because of continued fever and elevated inflammatory markers, remdesivir and tocilizumab were given. On the next day, she had significant clinical improvement, so the treatment with cytokine-directed agents may be considered in critically ill patients (Patel et al., 2020).
Patients with impaired immune function are more at risk in case of adverse outcomes. Leelayuwatanaku N et al. reported two patients (P/F < 300 mmHg) with human immunodeficiency virus (HIV) infection and multiple myeloma relapse, respectively. After tocilizumab, hemoperfusion, and immunoglobulin comprehensive treatment, their P/F levels increased significantly, and they survived to discharge (Leelayuwatanaku et al., 2021). In addition, Kataoka H et al. reported an 85-year-old patient with Sjögren’s syndrome, whose P/F decreased to 100 mmHg. After receiving a single dose of tocilizumab, the symptoms improved. This patient represents a supplementary case confirming the safety and efficacy of tocilizumab for elderly COVID-19 patients with autoimmune diseases. It is also suggested that combination therapy may be a promising treatment for severe COVID-19 in immunocompromised hosts (Kataoka et al., 2021).
The experience of COVID-19 patients with solid organ and composite tissue transplantation has not been reported in detail before. Morillas JA et al. reported 5 patients with COVID-19 (P/F < 300 mmHg) who received kidney transplantation, lung transplantation, face transplantation, and liver transplantation, respectively. These patients also had chronic diseases, such as heart diseases, bladder cancer, rheumatic heart disease, etc. Their C-reactive protein (CRP) levels decreased significantly within a few days after the application of tocilizumab. The findings showed that tocilizumab could be used without major direct toxicity in solid organ and composite tissue transfer recipients early after initiation of mechanical exploitation due to COVID-19, regardless of the type of organ transferred. However, the authors suggested that the diagnosis and side effects need to be further studied (Morillas et al., 2020). Ladna M et al. and Thammathiwa T et al. shared the treatment experiences of transplant patients, respectively. One patient who received a kidney and heart transplant in February 2020 had a relatively poor clinical condition with a P/F level of 117 mmHg. On day1, he was given a dose of 400 mg of tocilizumab, broad-spectrum antibiotics, and hydroxychloroquine, and transplant immunosuppression with tacrolimus was continued. After 11 days of treatment, he was discharged without supplemental oxygen requirement (Ladna et al., 2021; Thammathiwat et al., 2021).
In addition to tocilizumab treatment cases, there are few case reports on IL-1 receptor antagonist. Filocamo G et al. and Franzetti M et al. in Italy treated two severe patients (P/F <200 mmHg) with IL-1 receptor antagonist anakinra. These studies suggested that, in the cytokine storm occurring during severe COVID-19 pneumonia, the high tolerability, short half-life, and immunomodulatory profile of anakinra may be useful. IL-1 inhibition may represent a safe and promising strategy to reduce inflammation, thus preventing multi-organ dysfunction (Filocamo et al., 2020; Franzetti et al., 2020).
4.3 Limitation
First, the lack of RCTs limited our analyses. Some included studies were case reports or series and had no proper control groups. Meanwhile, some articles of which the full texts or data were not accessible and those in languages other than Chinese and English were excluded from the analysis. This might have led to overlooking some critical findings or observations. In addition, in this study, the SOFA score or related indicators of some patients included in the study were median or mean, so not all patients were septic patients, but the results of this population also reflected a trend problem because some patients might be or would be in a state of sepsis. Thirdly, we found that most patients use antiviral drugs, glucocorticoids, immunoglobulins, plasma, broad-spectrum antibiotics, and other drugs at the same time. We cannot rule out the impact of these drugs on the disease.
5 Conclusion
The results of this systematic review showed that tocilizumab, sarilumab, and anakinra might reduce the mortality of people with COVID-19 (at the edge of sepsis), and tocilizumab did not significantly affect SAEs and secondary infections. However, given the limited clinical researches and low-quality evidence, this conclusion needs more clinical evidence to be verified. In addition, so far, there is still no unified opinion on the timing, dosage, usage, and applicable population of these drugs all over the world, which also adds to the uncertainty of the conclusion of this study.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author Contributions
YW and KZ contributed equally to this work. YW, KZ, and QY conceived and designed the study protocol. YW and KZ executed the search strategy and screening and performed data extraction. RL, RD, and XL performed risk of bias assessments, and YW and RL assessed the quality of evidence. YW, ML, and RD analyzed or interpreted the data. YW and KZ drafted the manuscript. QY contributed to writing—review and editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Supplementary Material
The supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.804250/full#supplementary-material
References
- Abe T., Izumo T., Ueda A., Hayashi M., Ishibashi Y. (2021). Successful Treatment of Two Japanese ESRD Cases With Severe COVID-19 Pneumonia. CEN Case Rep. 10 (1), 42–45. 10.1007/s13730-020-00512-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kaf F. A., Al Garni T. A., Al-Harbi N., Sandokji H., Samargandy S. (2021). Cardiac Tamponade, Sever Hypothyroidism and Acute Respiratory Distress Syndrome (ARDS) With COVID-19 Infection. J. Saudi Heart Assoc. 33 (1), 71–76. 10.37616/2212-5043.1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aroldi A., Chiarle R., Gambacorti-Passerini C. (2021). Clinical Benefit of Lenzilumab in Cases of Coronavirus Disease 2019. Mayo Clin. Proc. 96 (3), 817. 10.1016/j.mayocp.2020.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo L., Del Sesto S., Giordano L., Benincaso A. R., Biondi P., Goj V., et al. (2020). Severe Prolonged Neutropenia Following Administration of Tocilizumab in a Patient Affected by COVID-19: a Case Report and Brief Review of the Literature. Drugs Ther. Perspect. 14, 1–5. 10.1007/s40267-020-00777-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzi G., Mangioni D., Minoia F., Aliberti S., Grasselli G., Barbetta L., et al. (2021). Anakinra Combined With Methylprednisolone in Patients With Severe COVID-19 Pneumonia and Hyperinflammation: An Observational Cohort Study. J. Allergy Clin. Immunol. 147 (2), 561–e4. e4. 10.1016/j.jaci.2020.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosnahan S. B., Chen X. J. C., Chung J., Altshuler D., Islam S., Thomas S. V., et al. (2021). Low-Dose Tocilizumab With High-Dose Corticosteroids in Patients Hospitalized for COVID-19 Hypoxic Respiratory Failure Improves Mortality Without Increased Infection Risk. Ann. Pharmacother. 28, 10600280211028882. 10.1177/10600280211028882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campochiaro C., Della-Torre E., Cavalli G., De Luca G., Ripa M., Boffini N., et al. (2020). Efficacy and Safety of Tocilizumab in Severe COVID-19 Patients: a Single-centre Retrospective Cohort Study. Eur. J. Intern. Med. 76, 43–49. 10.1016/j.ejim.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canziani L. M., Trovati S., Brunetta E., Testa A., De Santis M., Bombardieri E., et al. (2020). Interleukin-6 Receptor Blocking with Intravenous Tocilizumab in COVID-19 Severe Acute Respiratory Distress Syndrome: A Retrospective Case-Control Survival Analysis of 128 Patients. J. Autoimmun. 114, 102511. 10.1016/j.jaut.2020.102511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella M., Mauro I., De Blasio E., Crispo A., Del Gaudio A., Bimonte S., et al. (2020). Rapid and Impressive Response to a Combined Treatment With Single-Dose Tocilizumab and NIV in a Patient With COVID-19 Pneumonia/ARDS. Medicina (Kaunas). 56 (8), 377. 10.3390/medicina56080377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalli G., Larcher A., Tomelleri A., Campochiaro C., Della-Torre E., De Luca G., et al. (2021). Interleukin-1 and Interleukin-6 Inhibition Compared With Standard Management in Patients With COVID-19 and Hyperinflammation: a Cohort Study. Lancet Rheumatol. 3 (4), e253–e261. 10.1016/S2665-9913(21)00012-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coomes E. A., Haghbayan H. (2020). Interleukin-6 in Covid-19: A Systematic Review and Meta-Analysis. Rev. Med. Virol. 30 (6), 1–9. 10.1002/rmv.2141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corominas H., Castellví I., Pomar V., Antonijoan R., Mur I., Matas L., et al. (2021). Effectiveness and Safety of Intravenous Tocilizumab to Treat COVID-19-Associated Hyperinflammatory Syndrome: Covizumab-6 Observational Cohort. Clin. Immunol. 223, 108631. 10.1016/j.clim.2020.108631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cremer P. C., Abbate A., Hudock K., McWilliams C., Mehta J., Chang S. Y., et al. (2021). Mavrilimumab in Patients With Severe COVID-19 Pneumonia and Systemic Hyperinflammation (MASH-COVID): an Investigator Initiated, Multicentre, Double-Blind, Randomised, Placebo-Controlled Trial. Lancet Rheumatol. 3 (6), e410–e418. 10.1016/S2665-9913(21)00070-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Luca G., Cavalli G., Campochiaro C., Della-Torre E., Angelillo P., Tomelleri A., et al. (2020). GM-CSF Blockade With Mavrilimumab in Severe COVID-19 Pneumonia and Systemic Hyperinflammation: a Single-Centre, Prospective Cohort Study. Lancet Rheumatol. 2 (8), e465–e473. 10.1016/S2665-9913(20)30170-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della-Torre E., Campochiaro C., Cavalli G., De Luca G., Napolitano A., La Marca S., et al. (2020). Interleukin-6 Blockade With Sarilumab in Severe COVID-19 Pneumonia With Systemic Hyperinflammation: an Open-Label Cohort Study. Ann. Rheum. Dis. 79 (10), 1277–1285. 10.1136/annrheumdis-2020-218122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emergency medicine branch of CPAM (2020). Emergency Medicine Branch of Chinese Medical Association, Emergency Physicians branch of Chinese Medical Doctor Association, Professional Committee of Emergency Medicine of Chinese People's Liberation Army. Expert Consensus on Early Prevention and Blocking of Sepsis in China. Cli Emer J. (China). 21 (7), 517–529. [Google Scholar]
- Erden A., Ozdemir B., Karakas O., Mutlu N. M., Izdes S., Kalem A. K., et al. (2021). Evaluation of 17 Patients With COVID-19 Pneumonia Treated With Anakinra According to HScore, SOFA, MuLBSTA, and Brescia-COVID Respiratory Severity Scale (BCRSS) Scoring Systems. J. Med. Virol. 93 (3), 1532–1537. 10.1002/jmv.26473 [DOI] [PubMed] [Google Scholar]
- Eroglu A., Kartal S., Saral O. B. (2021). Helmet Mask and Tocilizumab for a Patient With Hemophagocytic Lymphohistiocytosis Syndrome and COVID-19: a Case Report. Braz. J. Anesthesiol. 71 (1), 79–83. 10.1016/j.bjane.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filocamo G., Mangioni D., Tagliabue P., Aliberti S., Costantino G., Minoia F., et al. (2020). Use of Anakinra in Severe COVID-19: A Case Report. Int. J. Infect. Dis. 96, 607–609. 10.1016/j.ijid.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher M. J., Marcos Raymundo L. A., Monteforte M., Taub E. M., Go R. (2021). Tocilizumab in the Treatment of Critical COVID-19 Pneumonia: A Retrospective Cohort Study of Mechanically Ventilated Patients. Int. J. Infect. Dis. 103, 536–539. 10.1016/j.ijid.2020.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzetti M., Forastieri A., Borsa N., Pandolfo A., Molteni C., Borghesi L., et al. (2021). IL-1 Receptor Antagonist Anakinra in the Treatment of COVID-19 Acute Respiratory Distress Syndrome: A Retrospective, Observational Study. J. Immunol. 206 (7), 1569–1575. 10.4049/jimmunol.2001126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzetti M., Pozzetti U., Carugati M., Pandolfo A., Molteni C., Faccioli P., et al. (2020). Interleukin-1 Receptor Antagonist Anakinra in Association With Remdesivir in Severe COVID-19: A Case Report. Int. J. Infect. Dis. 97, 215–218. 10.1016/j.ijid.2020.05.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galván-Román J. M., Rodríguez-García S. C., Roy-Vallejo E., Marcos-Jiménez A., Sánchez-Alonso S., Fernández-Díaz C., et al. (2021). IL-6 Serum Levels Predict Severity and Response to Tocilizumab in COVID-19: An Observational Study. J. Allergy Clin. Immunol. 147 (1), 72–80. e8. 10.1016/j.jaci.2020.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg N., Lee Y. I. (2020). Reactivation TB With Severe COVID-19. Chest. 158, A777. 10.1016/j.chest.2020.08.724 [DOI] [Google Scholar]
- Granholm A., Alhazzani W., Møller M. H. (2019). Use of the GRADE Approach in Systematic Reviews and Guidelines. Br. J. Anaesth. 123 (5), 554–559. 10.1016/j.bja.2019.08.015 [DOI] [PubMed] [Google Scholar]
- Gremese E., Cingolani A., Bosello S. L., Alivernini S., Tolusso B., Perniola S., et al. (2020). Sarilumab Use in Severe SARS-CoV-2 Pneumonia. EClinicalMedicine. 27, 100553. 10.1016/j.eclinm.2020.100553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. (2020). Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, China. Lancet. 395 (10223), 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang E., Isonaka S., Yang H., Salce E., Rosales E., Jordan S. C. (2021). Tocilizumab Treatment in Critically Ill Patients With COVID-19: A Retrospective Observational Study. Int. J. Infect. Dis. 105, 245–251. 10.1016/j.ijid.2021.02.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashin M., Gorski J., Minkin R. (2020). Lung Abscesses in A Patient Treated With Tocilizumab for Covid-19 Pneumonia Complicated by Severe Hypoxemic Respiratory Failure. Chest. 158 (4), A2568. 10.1016/j.chest.2020.09.165 [DOI] [Google Scholar]
- Kataoka H., Kodama F., Tomita T., Kondo M., Nagasaka A., Nishikawa S., et al. (2021). Immediate Amelioration of Severe Respiratory Distress in Sjögren's Syndrome With COVID-19 Treated With a Single Dose of Off-Label Tocilizumab. Intern. Med. 60 (4), 639–643. 10.2169/internalmedicine.6010-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishaba T., Maeda A., Fukuoka S., Imai T., Takakura S., Yokoyama S., et al. (2021). A Case Report of Super Responder of Critical COVID-19 Pneumonia. J. Med. Invest. 68 (1.2), 192–195. 10.2152/jmi.68.192 [DOI] [PubMed] [Google Scholar]
- Kyriazopoulou E., Panagopoulos P., Metallidis S., Dalekos G. N., Poulakou G., Gatselis N., et al. (2021a). An Open Label Trial of Anakinra to Prevent Respiratory Failure in COVID-19. Elife. 10, e66125. 10.7554/eLife.66125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriazopoulou E., Poulakou G., Milionis H., Metallidis S., Adamis G., Tsiakos K., et al. (2021b). Early Treatment of COVID-19 with Anakinra Guided by Soluble Urokinase Plasminogen Receptor Plasma Levels: a Double-Blind, Randomized Controlled Phase 3 Trial. Nat. Med. 27 (10), 1752–1760. 10.1038/s41591-021-01499-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Rosée P., Horne A., Hines M., von Bahr Greenwood T., Machowicz R., Berliner N., et al. (2019). Recommendations for the Management of Hemophagocytic Lymphohistiocytosis in Adults. Blood. 133 (23), 2465–2477. 10.1182/blood.2018894618 [DOI] [PubMed] [Google Scholar]
- Ladna M., Villanueva F. L., Maharrey P. B., Lascano J. (2021). Post-Transplant Patients With COVID-19 Associated Acute Respiratory Distress Syndrome, a Role for Tociluzumab: A Case Series. Respir. Med. Case Rep. 32, 101319. 10.1016/j.rmcr.2020.101319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leelayuwatanakul N., Kongpolprom N., Sriprasart T., Phoophiboon V., Thanthitaweewat V., Thawanaphong S., et al. (2021). Multimodality Treatment in Immunocompromised Patients With Severe COVID-19: the Role of IL-6 Inhibitor, Intravenous Immunoglobulin, and Haemoperfusion. Respirol Case Rep. 9 (4), e0733. 10.1002/rcr2.733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lescure F. X., Honda H., Fowler R. A., Lazar J. S., Shi G., Wung P., et al. (2021). Sarilumab COVID-19 Global Study Group. Sarilumab in Patients Admitted to Hospital With Severe or Critical COVID-19: a Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Respir. Med. 9 (5), 522–532. 10.1016/S2213-2600(21)00099-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Liu L., Zhang D., Xu J., Dai H., Tang N., et al. (2020). SARS-CoV-2 and Viral Sepsis: Observations and Hypotheses. Lancet. 395 (10235), 1517–1520. 10.1016/S0140-6736(20)30920-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas C., Wong P., Klein J., Castro T. B. R., Silva J., Sundaram M., et al. (2020). Longitudinal Analyses Reveal Immunological Misfiring in Severe COVID-19. Nature. 584 (7821), 463–469. 10.1038/s41586-020-2588-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mady A., Aletreby W., Abdulrahman B., Lhmdi M., Noor A. M., Alqahtani S. A., et al. (2020). Tocilizumab in the Treatment of Rapidly Evolving COVID-19 Pneumonia and Multifaceted Critical Illness: A Retrospective Case Series. Ann. Med. Surg. (Lond). 60, 417–424. 10.1016/j.amsu.2020.10.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazankova L. N., Osmanov I. M., Samitova E. R., Malakhov A. B., Koroid V. V., Nedostoev A. A., et al. (2020). A Teenager With a Severe Form of COVID-19. Rossiyskiy Vestnik Perinatologii i Pediatrii. 65 (5), 58–65. 10.21508/1027-4065-2020-65-5-58-65 [DOI] [Google Scholar]
- McKenzie M. G., Lee Y. M., Mathew J., Anderson M., Vo A. T., Akinyele S., et al. (2021). Tocilizumab for the Critically Ill With Severe COVID-19: A Community Hospital Case Series. J. Pharm. Pract. 19, 8971900211002353. 10.1177/08971900211002353 [DOI] [PubMed] [Google Scholar]
- Menzella F., Fontana M., Salvarani C., Massari M., Ruggiero P., Scelfo C., et al. (2020). Efficacy of Tocilizumab in Patients With COVID-19 ARDS Undergoing Noninvasive Ventilation. Crit. Care. 24 (1), 589. 10.1186/s13054-020-03306-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Plos Med. 6 (7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moideen S., Maheshwari V., Syam Prakash K. R., Rajagopal S., Sherief S. H. (2020). Different Treatment Approaches, Clinical Outcome, Effectiveness of the Drug towards Covid 19 With 5 Different Cases: A Case Series. Int. J. Pharm. Sci. Rev. Res. 65 (1), 98–103. 10.47583/ijpsrr.2020.v65i01.014 [DOI] [Google Scholar]
- Morillas J. A., Marco Canosa F., Srinivas P., Asadi T., Calabrese C., Rajendram P., et al. (2020). Tocilizumab Therapy in 5 Solid and Composite Tissue Transplant Recipients With Early ARDS Due to SARS-CoV-2. Am. J. Transpl. 20 (11), 3191–3197. 10.1111/ajt.16080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health(NIH) (2017). Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. Available at: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40 (Accessed October 17, 2021).
- NOS (2020). Abbreviations.com. STANDS4 LLC. Available at: https://www.abbreviations.com/term/1418908 (Accessed October 17, 2021).
- Nourié N., Chamaa M. A., Mouawad S., Kotait M. M., Finianos S., Azar H., et al. (2021). Effective Treatment With Tocilizumab in a COVID-19 Patient on Maintenance Hemodialysis: A Case Report. CEN Case Rep. 10 (3), 364–369. 10.1007/s13730-021-00577-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P. A., Chandrakasan S., Mickells G. E., Yildirim I., Kao C. M., Bennett C. M. (2020). Severe Pediatric COVID-19 Presenting With Respiratory Failure and Severe Thrombocytopenia. Pediatrics. 146 (1), e20201437. 10.1542/peds.2020-1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., et al. (2020). Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 71 (15), 762–768. 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajendram P., Sacha G. L., Mehkri O., Wang X., Han X., Vachharajani V., et al. (2021). Tocilizumab in Coronavirus Disease 2019-Related Critical Illness: A Propensity Matched Analysis. Crit. Care Explor. 3 (1), e0327. 10.1097/CCE.0000000000000327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- REMAP-CAP Investigators Gordon A. C., Mouncey P. R., Al-Beidh F., Rowan K. M., Nichol A. D. (2021). Interleukin-6 Receptor Antagonists in Critically Ill Patients With Covid-19. N. Engl. J. Med. 384 (16), 1491–1502. 10.1056/NEJMoa2100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice T. W., Wheeler A. P., Bernard G. R., Hayden D. L., Schoenfeld D. A., Ware L. B., et al. (2007). Comparison of the SpO2/FIO2 Ratio and the PaO2/FIO2 Ratio in Patients With Acute Lung Injury or ARDS. Chest. 132 (2), 410–417. 10.1378/chest.07-0617 [DOI] [PubMed] [Google Scholar]
- Rudd K. E., Johnson S. C., Agesa K. M., Shackelford K. A., Tsoi D., Kievlan D. R., et al. (2020). Global, Regional, and National Sepsis Incidence and Mortality, 1990-2017: Analysis for the Global Burden of Disease Study. Lancet. 395 (10219), 200–211. 10.1016/S0140-6736(19)32989-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffo Z., Guo W., Springer K., Maksimowicz-McKinnon K., Kak V., McKinnon J. E., et al. (2021). The Role of Tocilizumab Therapy in Critically Ill Patients With Severe Acute Respiratory Syndrome Coronavirus 2. J. Osteopath Med. 121 (8), 705–714. 10.1515/jom-2020-0292 [DOI] [PubMed] [Google Scholar]
- Salvarani C., Dolci G., Massari M., Merlo D. F., Cavuto S., Savoldi L., et al. (2021). Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized With COVID-19 Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 181 (1), 24–31. 10.1001/jamainternmed.2020.6615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senegaglia A. C., Rebelatto C. L. K., Franck C. L., Lima J. S., Boldrini-Leite L. M., Daga D. R., et al. (2021). Combined Use of Tocilizumab and Mesenchymal Stromal Cells in the Treatment of Severe Covid-19: Case Report. Cell Transpl. 30, 9636897211021008. 10.1177/09636897211021008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seymour C. W., Liu V. X., Iwashyna T. J., Brunkhorst F. M., Rea T. D., Scherag A., et al. (2016). Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 315 (8), 762–774. 10.1001/jama.2016.0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M., Deutschman C. S., Seymour C. W., Shankar-Hari M., Annane D., Bauer M., et al. (2016). The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 315 (8), 801–810. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somers E. C., Eschenauer G. A., Troost J. P., Golob J. L., Gandhi T. N., Wang L., et al. (2021). Tocilizumab for Treatment of Mechanically Ventilated Patients With COVID-19. Clin. Infect. Dis. 73 (2), e445–e454. 10.1093/cid/ciaa954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne J. A. C., Savović J., Page M. J., Elbers R. G., Blencowe N. S., Boutron I., et al. (2019). RoB 2: a Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ. 366, l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Thammathiwat T., Tungsanga S., Tiankanon K., Torvorapanit P., Chumpangern W., Udomkarnjananun S., et al. (2021). A Case of Successful Treatment of Severe COVID-19 Pneumonia With Favipiravir and Tocilizumab in post-kidney Transplant Recipient. Transpl. Infect. Dis. 23 (1), e13388. 10.1111/tid.13388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vazquez Guillamet M. C., Kulkarni H. S., Montes K., Samant M., Shaikh P. A., Betthauser K., et al. (2021). Interleukin-6 Trajectory and Secondary Infections in Mechanically Ventilated Patients With Coronavirus Disease 2019 Acute Respiratory Distress Syndrome Treated With Interleukin-6 Receptor Blocker. Crit. Care Explor. 3 (2), e0343. 10.1097/CCE.0000000000000343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Dai R., Lv X., Qian Y., Zhu K. (2020). Specific Interleukin-1 Inhibitors, Specific Interleukin-6 Inhibitors and Anti-GM-CSF for COVID-19 (At the Edge of Sepsis): a Living System Review. PROSPERO 2020 CRD42020226545 Available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020226545 (Accessed October 17, 2021). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.