Purpose of review
Treatment outcome of relapsed or refractory AML patients remains dismal and new treatment options are needed. Adoptive cell therapy using CAR-T cells is a potentially interesting approach in this.
Recent findings
Several potentially interesting AML targets are being investigated with CAR-T therapy with over 60 clinical trials listed on clinicaltrials.gov. The first clinical data are only just emerging with mixed results, once more proving that further research is needed.
Summary
Adoptive cell therapy using chimeric antigen receptor T cells is being investigated in AML through many clinical trials. So far, no AML-specific antigen has been identified, requiring additional strategies to mitigate on-target off-tumor toxicity and to increase efficacy. Focus point is to acquire control over the CAR T cells once administered. Strategies to do so include biodegradable CARs, inducible CARs, suicide-switch containing CARs and two-component modular CARs. Limited and mixed results are available, confirming the risk of lasting toxicity for nonswitchable CARs. Initial results of modular CARs suggest toxicity can be mitigated whilst maintaining CAR activity by the use of modular CAR concepts that allows for ‘ON’ and ‘OFF’ switching.
Keywords: adaptor chimeric antigen receptor, adoptive immunotherapy, acute myeloid leukemia, chimeric antigen receptor T cell
INTRODUCTION
Acute myeloid leukemia (AML) is an aggressive hematologic malignancy mainly affecting elderly patients, with a poor prognosis despite the introduction of new treatment options [1,2]. A promising immunotherapeutic approach is the genetic modification of the patient's own (autologous) or a donor's (allogeneic) T cells with chimeric antigen receptors (CAR-T). In this way, leukemia-associated antigens can be specifically targeted. In B-cell-derived malignancies, CAR-T has been clinically very successful, whereas in AML, a convincing proof of the applicability of CAR-T is still missing. In this review, we highlight the pros and cons of targeting different antigens, including clinical results published to date, as well as strategies to increase safety and efficacy of CAR-T therapies in AML. Optimization of chimeric constructs as well as improvements in production processes are not within the focus of this review. The authors refer to the numerous review articles on these topics published in recent years [3–7].
Box 1.
no caption available
CHALLENGES IN IDENTIFYING POTENTIAL TARGETS FOR CHIMERIC ANTIGEN RECEPTOR T-CELL THERAPY IN ACUTE MYELOID LEUKEMIA
The ideal target antigen for CAR-T-cell therapy is characterized by four key characteristics:
-
(1)
Expression in a substantial part of AML patients ensuring broad applicability.
-
(2)
Expression on immature leukemia-initiating cells to allow for complete eradication of the leukemic clone.
-
(3)
Stable expression without downregulation or shedding to avoid antigen-loss escape variants.
-
(4)
Negligible expression on normal hematopoietic stem cells and other normal tissue reducing the risk for prolonged pancytopenia or other on-target/off-tumor effects.
So far, no antigen on AML cells fulfils all mentioned criteria. Although the biology and expression patterns of potential CAR-T-cell therapy targets in AML have been discussed elsewhere [6,8], this review will focus on published clinical data and novel strategies to handle the issue of imperfect target antigens. Table 1 shows clinical studies with results reported. An extended tabulated summary of all identified clinical trials in AML with CAR-T is provided as supplementary information.
Table 1.
Chimeric antigen receptor T-cell clinical trials recruiting acute myeloid leukemia patients that have reported (initial) results
| Study short title | Study identifier | Status | Phase | Condition | Interventional targets | Responsible party | Reference |
| Treatment of Relapsed and/or Chemotherapy Refractory CD33 Positive Acute Myeloid Leukemia by CART-33 | NCT01864902 | Unknowna | I/II | rrAML | CD33 | Chinese PLA General Hospital, Beijing, China | Wang et al., 2015 |
| CLL1-CD33 cCAR in Patients With Relapsed and/or Refractory, High Risk Hematologic Malignancies | NCT03795779 | Recruiting | Early phase 1 | rrAML | CD33, CLL-1 | iCell Gene Therapeutics, Stony Brook, New York, United States | Liu et al., 2018, 2020 |
| Multiple CAR-T Cell Therapy Targeting AML | NCT04010877 | Recruiting | I/II | rrAML | CD33, CLL-1, CD123 | Shenzhen Geno-Immune Medical Institute, Shenzhen, Guangdong, China | Zhang et al., 2020, 2021? |
| CD123 Redirected Autologous T Cells for AML | NCT02623582 | Terminated | Early phase 1 | rrAML | CD123 | Abramson Cancer Center of the University of Pennsylvania, Philadelphia, Pennsylvania, United States | Cummins et al., 2017 |
| Genetically Modified T-cell Immunotherapy in Treating Patients With Relapsed/Refractory Acute Myeloid Leukemia and Persistent/Recurrent Blastic Plasmacytoid Dendritic Cell Neoplasm | NCT02159495 | Recruiting | I | prBPDCN, rrAML | CD123 | City of Hope Medical Center, Duarte, California, United States | Budde et al., 2018 |
| Phase I Study of UCART123 in Patient With Adverse Genetic Risk Acute Myeloid Leukemia | NCT04106076 | Withdrawn | I | AML | CD123 | Cellectis S.A., Paris, France | Cummins and Gill, 2019 |
| Study Evaluating Safety and Efficacy of UCART123 in Patients With Relapsed/Refractory Acute Myeloid Leukemia | NCT03190278 | Recruiting | I | rrAML | CD123 | Cellectis S.A., Paris, France | Roboz et al., 2020 |
| Safety Study of Anti Lewis Y Chimeric Antigen Receptor in Myeloma, Acute Myeloid Leukemia or Myelodysplastic Syndrome | NCT01716364 | Unknowna | I | (rr)AML, MDS, MM | Lewis Y | Peter MacCallum Cancer Centre, Melbourne, Australia | Ritchie et al., 2013 |
| Safety Study of Chimeric Antigen Receptor Modified T-cells Targeting NKG2D-Ligands | NCT02203825 | Completed | I | AML, MDS-RAEB, MM | NKG2D Ligands | Celyad Oncology SA, New York, New York, United States | Baumeister et al., 2019 |
| A Dose Escalation Phase I Study to Assess the Safety and Clinical Activity of Multiple Cancer Indications (THINK) | NCT03018405 | Unknowna | I/II | AML, CRC, EOC, FTC, MDS, MM, PC, TCC, TNBC | NKG2D Ligands | Celyad Oncology SA, New York, New York, United States | Sallman et al., 2018, 2019 |
| DEPLETHINK - LymphoDEPLEtion and THerapeutic Immunotherapy With NKR-2 (DEPLETHINK) | NCT03466320 | Completed | I/II | AML, MDS | NKG2D Ligands | Celyad Oncology SA, New York, New York, United States | Sallman et al., 2020 |
| EPITHINK: Epigenetic Drug Treatment and Therapeutic Immunotherapy With NKR-2 | NCT03612739 | Withdrawn | I | AML | NKG2D ligands | Celyad Oncology SA, New York, New York, United States | Sallman et al., 2020 |
| Study in Relapsed/Refractory Acute Myeloid Leukemia or Myelodysplastic Syndrome Patients to Determine the Recommended Dose of CYAD-02 | NCT04167696 | Recruiting | I | MDS, rrAML | NKG2D ligands | Celyad Oncology SA, New York, New York, United States | Deeren et al. 2020 |
| Dose-escalating Trial With UniCAR02-T Cells and CD123 Target Module (TM123) in Patients With Hematologic and Lymphatic Malignancies | NCT04230265 | Recruiting | I | AML, B-ALL, BPDCN | CD123 | CPT Cellex Patient Treatment GmbH, Dresden, Germany | Wermke et al., 2021 |
As referenced on clinicaltrials.gov.
AML, acute myeloid leukemia; B-ALL, B-Cell Acute Lymphoblastic Leukemia; BPDCN, Blastic Plasmacytoid Dendritic-Cell Neoplasia; CRC, Colorectal Cancer; EOC, Epithelial Ovarian Cancer; FTC, Fallopial Tube Carcinoma; MDS, Myelodysplastic Syndrome; MM, Multiple Myeloma; PC, Prostate Cancer; RAEB, Refractory Anaemia with Excessive Blasts; rrAML, relapsed refractory AML; TCC, Transitional Cell Carcinoma; TNBC, Triple-Negative Breast Cancer.
POTENTIAL TARGET ANTIGENS FOR CHIMERIC ANTIGEN RECEPTOR T CELLS IN ACUTE MYELOID LEUKEMIA
Below, several potentially interesting targets will be discussed shortly.
NKG2D ligands
NKG2D ligands are widely expressed on many malignancies and preclinical experiments with respective CAR constructs showed promising results [9]. In a single-center phase I study with a first-generation CAR targeting NKG2D ligands, the treatment was found to be well tolerated and 3 of 12 patients, 7 with AML and 5 with multiple myeloma, achieved a Complete Response (CR) [10–12]. In contrast, another study did not report objective responses in 17 AML patients [12]. Intermittent surface expression of NKG2D ligands by activated T cells possibly inducing fratricide might explain limited clinical efficacy [13,14] and CAR-T production failures. The addition of blocking antibodies to the production process or deletion of the antigen of interest by gene editing are possible solutions to these problems [15]. A study has been initiated using NKG2D CAR-T-cells with intentional down-regulation of MICA/B by co-expression of short hairpin RNA. Promising early results show bone marrow blast reduction from baseline in seven patients treated [16]. Further studies will have to prove whether NKG2D is a valid target for AML CAR-T therapy.
C-type lectin-like molecule-1
C-type lectin-like molecule-1 (CLL-1) is expressed in about 92% of AML patients including the leukemia-initiating cell compartment whereas normal hematopoiesis lacks significant CLL-1 expression [17–19]. Early clinical results in pediatric AML patients showed promising results with three out of four patients achieving a complete remission and measurable residual disease (MRD) negativity [20]. The same group reported results from 11 patients treated either with CLL-1 or CLL-1-CD33 dual targeting CAR-T and reported five CRs being MRD-negative, and additionally three CRs with MRD detectable, one Progressive Disease (PD) and one Stable Disease (SD) [21]. Toxicity was manageable with grade 1–3 cytokine release syndrome (CRS) and myelosuppression. Another group reported seven MRD-negative CRs out of nine patients with dual targeting CD33 and CLL-1-specific CAR-T [22,23]. Several clinical trials are ongoing using CLL-1 as a target, alone or in combination with other targets (Supplementary Information), but to our knowledge, no further clinical data are available to determine whether CLL-1 is a safe antigen to be targeted with conventional CAR-T without damaging hematopoiesis.
FMS-like Tyrosine Kinase 3
The FMS-like Tyrosine Kinase 3 (FLT3) is an established AML target and expressed in 80% of patients, making it an interesting target for CAR-T treatment. CAR constructs currently under development are not specifically targeting the mutated FLT3 but FLT3, in general [24–27]. FLT3 expression on normal tissue seems to be restricted to a subpopulation of hematopoietic stem and precursor cells [25,28]. Nevertheless, significant hematopoietic toxicities have been observed in mouse models using murine or human FLT3-specific CAR-T [26,27]. Therefore, CAR constructs with a safety switch allowing for complete elimination of CAR-T cells have been developed to mitigate this risk for prolonged suppression of normal hematopoiesis [26]. At least three CAR-T trials targeting FLT3 are listed in the registries but no clinical data have been reported yet.
CD33
CD33 is a transmembrane receptor of the SIGLEC family and a proven target for AML treatment [29]. CD33 targeting CAR-T were evaluated preclinically demonstrating the potential of this approach [30,31]. As CD33 is also expressed on myeloid progenitor cells, there is a substantial risk for lasting aplasia, implying the need for a subsequent hematopoietic cell transplantation (HCT). This was indeed reported in a trial combining CLL-1 and CD33 as a target on a CAR-T cell [22]. In a single case report, a patient infused with CD33-specific CAR-T experienced CRS and pancytopenia whilst achieving a reduction in bone marrow blasts [32]. To mitigate CD33-associated toxicities, deleting CD33 expression from hematopoietic stem cells is investigated to enable CD33 CAR-T therapy along with transplantation of the gene-edited stem cells [33]. Alternatively, a safety suicide gene is implemented [34].
CD123
IL-3Rα/CD123 is overexpressed in AML and other hematological malignancies including the leukemia-initiating cell compartment [29,35–38]. Various agents have shown the potential of CD123 as a target for AML including Tagraxofusp (Elzonris) and Flotetuzumab inducing CRs in relapsed/refractory patients [39,40]. However, data from mouse models suggests that continuous anti-CD123 activity of CAR-T may be harmful for the hematopoietic progenitor cell compartment [41,42]. Outcomes of the first cohorts of a FIH clinical trial with a conventional CD123 targeting CAR-T showed responses not only including CRi but also lasting aplasias and as such an HCT was planned after CAR-T therapy [43▪]. The potential of allogeneic CD123 CAR-T is also under exploration. After an initial trial has been put on hold because of a patient's death, the study was re-initiated with a modified product and a strong dose reduction [44▪]. The initial dose level was cleared without any DLT but no efficacy data have been reported, thus far [45].
The apparent lack of clinical data amidst a multitude of clinical trials investigating CAR-T treatments in AML clearly indicates the complexity to safely target antigens that are not solely expressed on tumor cells.
STRATEGIES TO ALLOW SAFE TARGETING OF IMPERFECT ACUTE MYELOID LEUKEMIA ANTIGENS
Being able to switch CAR-T cells off is key to allow for targeting of antigens, which are shared between AML and normal hematopoiesis or other nontarget tissue. Moreover, switchable constructs may increase safety in situations of serious CAR-T-cell-associated toxicity, for example, CRS or immune effector cell-associated neurotoxicity syndrome (ICANS).
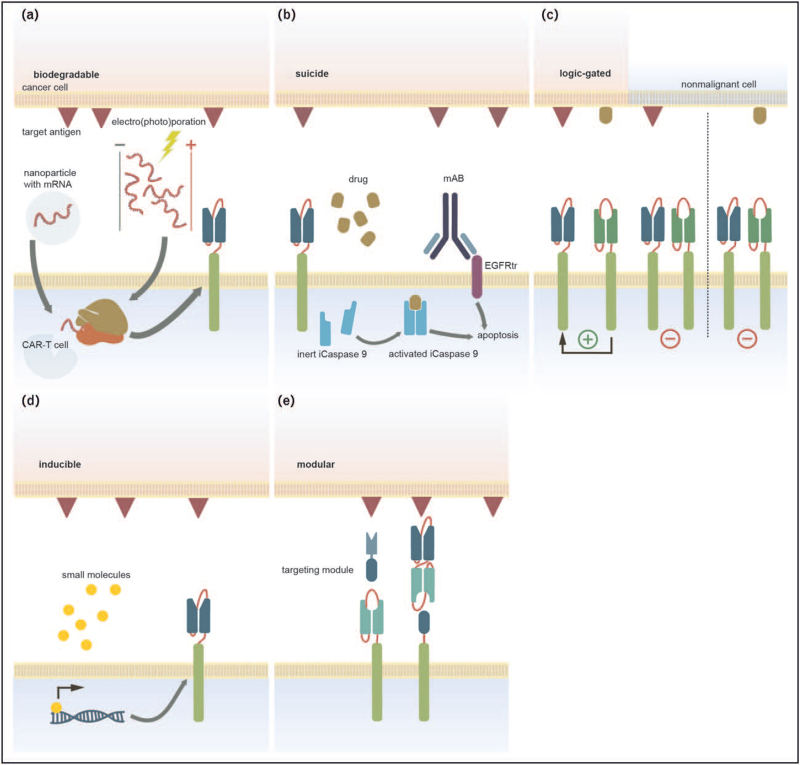
Potential strategies to turn CAR-T-cells into a tightly controllable therapeutic tool will be discussed below and are illustrated in Fig. 1.
FIGURE 1.
Schematic representation of various approaches to improve safety of Chimeric antigen receptor T-cell constructs. Panel a: Biodegradable CAR-T cell. mRNA encoding disease-specific receptor genes is inserted into the T-cell by means of nanoparticles, electroporation, or photoporation. Panel b: suicide switch CAR-T cell. Activity is abrogated by the introduction of a small molecule or antibody that triggers the degradation of the T cell. Panel c: logic gated CAR-T. The construct has two binding domains for two separate targets, CAR-T activation is only initiated upon simultaneous binding of the CAR with both domains. Panel d: inducible CAR-T. Administration of specific molecules trigger the expression or functional assembly of the CAR. Panel e: MODULAR, switchable CAR-T on the left side the UniCAR having the epitope on the target module and on the right side Rev(ersible) CAR with the epitope expressed on the CAR-T cell. In both cases, the CAR can only be activated upon connection via the targeting component connecting the tumor cell with the Universal CAR. CAR-T, Chimeric antigen receptor T-cell.
Biodegradable chimeric antigen receptor T cells
‘Biodegradable’ CAR-T cells refers to T cells that express the CAR only transiently, mostly achieved by transient transfection of mRNA encoding the CAR via, for instance, nanoparticles, electroporation, or photoporation [46–49].
Transient expression of a CD123-specific CAR-T for AML treatment was explored in a clinical trial initiated at UPenn [50]. Seven patients were enrolled, with two patients receiving all planned doses. Successful manufacturing was only achieved for approximately 60% of doses and median time from enrolment to infusion was 50 days, highlighting the technical hurdles still to be overcome. All but one patient experienced CRS upon cell product administration but the effects were only transient and CD123 CAR-T cells were neither detectable nor was a reduction of CD123-positive cells observed in the bone marrow. Thus, the trial was terminated early due to lack of efficacy.
Chimeric antigen receptor T cells containing a suicide off-switch
The severe and sometimes fatal side effects observed in the CD19 CAR-T studies prompted researchers to incorporate safety mechanisms allowing for elimination of the genetically modified cells in an emergency. In addition to the well known Herpes simplex virus thymidine kinase, which has been studied as an eliminator for CAR-T [51,52], an inducible caspase system has also been developed and preclinically tested in the context of CD33-specific CAR-T [53]. However, the authors observed that only about three quarters of CAR-T were eliminated by caspase induction and concluded that a combination with other T-cell inhibitory agents, such as BCL-2 inhibitors is required. Another way to eliminate CAR-T is antibody-dependent cellular toxicity (ADCC). In addition to the CAR, the T cells are modified with epitopes that are recognized by clinically approved monoclonal antibodies (mabs). Examples are the co-expression of a truncated epidermal growth factor receptor (tEGFR) or a portion of CD20, which are recognized by cetuximab and rituximab, respectively. Another approach would be pan T-cell ablation by T-cell targeting mabs like alemtuzumab. When the two strategies were compared in a murine xenograft model, CAR-T-cells could be ablated by using either alemtuzumab or rituximab, facilitating hematopoietic engraftment after elimination of leukemic cells [54]. The disadvantage of these strategies is that the CAR-T cells are finally eliminated and cannot combat any relapse. The elimination of an expensive autologous product does not seem very reasonable from an economic point of view either.
Logic-gated chimeric antigen receptor T cells
Another approach is to logically link signals via two synthetic receptors that recognize different antigens. The signals can act either cooperatively (‘AND’ gating) or inhibitory (’NOT’ gating). Preclinical proof-of-concept for these approaches has been provided with non-AML-specific antigens [55,56]. At the Memorial Sloan Kettering center, combinatorial CAR-T targeting ADGRE2 and CLL-1 is currently under development [57].
Inducible chimeric antigen receptor T cells
Conditional rather than constitutive CAR expression is another way to avoid or mitigate toxicities. Inducible promoter systems like the tetracycline-inducible promoter can be used for this purpose [58]. Another elegant approach is using synthetic Notch receptors, via which the expression of a CAR can be induced [59]. Small molecules like methotrexate (MTX) can be used to modify the affinity of CAR binders. CD33-specific single-chain antibodies were generated as CAR binders, which led to a reversible attenuation in the presence of MTX [60].
Modular chimeric antigen receptor T cells allowing for off-switching and on-switching
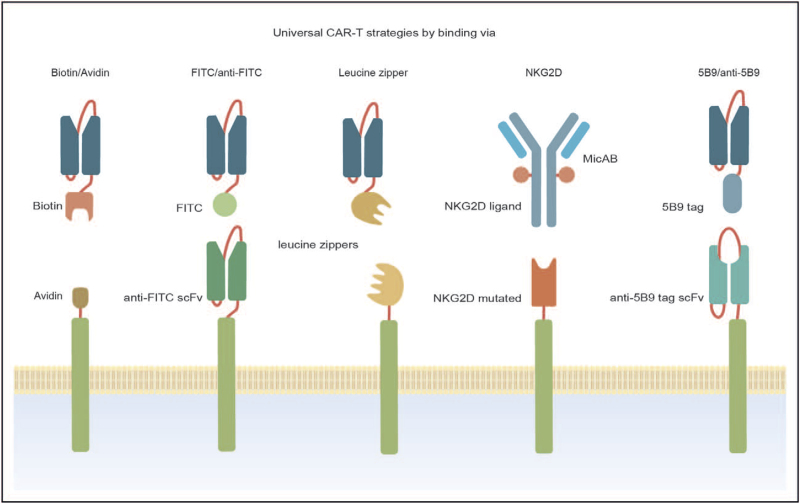
An alternative to address the limitations of aforementioned systems is to use soluble adaptors conferring tumor antigen-binding capacities to otherwise inert CARs also referred to as adaptor CARs. Various platforms exist, all based on the principle of the CAR-T cell recognizing and binding to a tag that is connected to a molecule that recognizes the tumor-associated antigen. CAR-T-cell activation only occurs upon binding of the second component. A well designed system allows for rapid up-titration and down-titration of the nonimmunogenic module as well as the ability to rapidly eliminate the binding component in case of acute life-threatening toxicity. Several reviews detail on the design of various adaptor CARs and the most prominent ones are depicted in Fig. 2 and discussed below [61▪▪,62–66].
FIGURE 2.
Graphic representation of various modular Chimeric antigen receptor T-cell platforms depicting from left to right: Biotin/Activin-mediated, FITC7anti-FITC-mediated, Leucin zipper-mediated, NKG2D-mediated and 5B9/anti 5B9-mediated systems.
Early adapter CAR systems used a biotin-binding structure or a FITC-based connection system, mostly combined with labeled full-length antibodies [67–69] or CD16 extracellular domain combined with naked antibodies [70]. The use of molecules that have a long half-life does, however, not seem to be a very suitable approach, given their slow elimination resulting in long latency switches. Fluorescein isothiocyanate (FITC) is a synthetic molecule absent in the human body and broadly used as a flow cytometry dye. The feasibility of the FITC-based system was demonstrated but no clinical data are available yet [71,72]. Both biotin-based as well as FITC-based systems face the risk of immunogenicity, both being haptens [73–76].
Another modular CAR-T switch system uses a leucine-zipper-based CAR and a fusion molecule of a leucine zipper and a tumor-targeting scFv. CAR activity can only commence once the two leucine zippers have connected. Competitive zipFv's with leucine zippers binding to the original zipFvs but not to the zipCAR can prevent activation of the CAR. Clinical trials are needed to confirm the concept's activity and controllability [77]. Whether the used leucine zippers will interact with naturally occurring leucine zippers and hence create off-target toxicity is still unclear.
Yet another strategy is the use of a modified NKG2D extracellular domain, also referred to as convertible CAR [78]. The system uses a mutated form of the NKG2D extracellular domain on the CAR (iNKG2D CAR) and ligands that engage with this CAR but not wild-type NKG2D. The ligands are fused with monoclonal antibodies against a potential tumor target, creating the connection between tumor cell and CAR-T cell. Clinical trials will start in 2021 with rituximab and trastuzumab as initial antibodies to be used, raising concern for the rapid switchability because of the long half-lives of Abs [79].
An alternative approach is the use of a unique peptide-based connection between the CAR-T cell and the target-binding component like in the UniCAR system [80,81], which has been developed by our group and will be reviewed in the following paragraph.
THE UniCAR SYSTEM, A MODULAR CHIMERIC ANTIGEN RECEPTOR-T PLATFORM WITH CLINICAL RESULTS IN ACUTE MYELOID LEUKEMIA
UniCAR is a rapidly switchable, two component CAR-T platform using a CD28 co-stimulatory domain. The first component is a universal CAR-T cell that is inert by itself. The second component is a targeting module, which confers specificity towards the cancer antigen as it contains a tumor-binding moiety linked to the epitope recognized by the UniCAR-T cell. The UniCAR-T cell can be rapidly switched on and off to abrogate and prevent toxicities simply by administering or withholding the continuous infusion of TM, which has a very short half-life. The system allows for sequential or simultaneous targeting of multiple antigens using different TMs.
UniCAR-T in combination with a CD123-specific TM (TM123) is currently explored in a phase 1 trial in relapsed/refractory AML. Clinical results of this ongoing study were presented at the 2021 AACR Annual Meeting, and preliminary initial results were published [82,83▪▪]. All reported patients showed a robust expansion of UniCAR-T cells in peripheral blood and bone marrow, leading to an overall response rate of 80% including two patients with Cri. Both granulocytes and thrombocytes recovered quickly after stop of TM administration in all patients, eliminating the need for HCT. Two patients received a second cycle of TM123 leading to the re-activation of UniCAR-T cells and renewed clinical responses, indicating the opportunity to further deepen responses and optimize response duration. Low grade (1–2) CRS was experienced in 80% of patients, rapidly abating after cessation of TM123 infusion. No ICU admissions were needed. To avoid the potential exhaustion of T cells, alternative schedules are considered, limiting the duration of TM administration and allowing T cells to recuperate.
OFF-THE-SHELF CHIMERIC ANTIGEN RECEPTOR T-CELL PRODUCTS
The rapid progressive nature of AML complicates CAR-T implementation because of lengthy manufacturing time for autologous CAR-T products. In addition, T cell quality from patients is often hampered because of the underlying disease and long history of previous treatments. Off-the-shelf allogeneic CAR-T products generated from healthy donors may provide a solution. There are, however, still many hurdles to take., Genetic edits are necessary to avoid instant rejection by the host on the one hand and to prevent development of Graft versus Host Disease (GvHD) on the other hand, making the production technically more challenging and complex. The novel gene editing techniques allow targeted knockout of, for example, the T-cell receptor and further modifications to enhance efficacy and reduce risk for GvHD, and numerous approaches are under development (e.g. [84–86]). Allogeneic CARs are also expected to significantly reduce costs, which is a major concern in CAR-T treatment [87–89]. However, it is currently unclear how many viable products can be generated from one healthy donor, impacting cost reduction and practical implementation significantly. Numerous allogenic CAR-T-cells against various targets are currently in development [90,91]. Early clinical results from allogeneic CAR-T in B-cell malignancies not only show signs of efficacy (e.g. [92]) but also suggest that limited persistence has a negative effect on effectiveness. Apart from the study with UCART123 mentioned above, the authors are currently not aware of any other published results on allogeneic CAR-T in AML but the use of ‘off-the-shelf’ CAR-T for the treatment of AML promises great potential.
CONCLUSION
CAR-T-cell therapy in AML is not as straight forward as in B-NHL because of the lack of truly AML-specific antigens, and the rapidly progressive nature of the disease further complicates treatment. Early results indicate, however, CAR-T may have a place in AML. The optimal construct is preferably modular and allowing for rapid on-switching and off-switching and targeting multiple targets. Additionally, allogeneic CARs may increase applicability to a broader population and decrease costs.
Acknowledgements
We would like to thank P. Di Benedetto for her support on the manuscript and the creation of figures and tables for this review.
Financial support and sponsorship
None.
Conflicts of interest
J.K.and M.C. are employees of AvenCell Europe GmbH, M.W. has received honoraria from AvenCell Europe GmbH for consultancy services for the development and conduct of the UniCAR study, A.E. is employee and co-owner of AvenCell Europe GmbH, G.E. is founder and co-owner of AvenCell Europe GmbH.
Supplementary Material
Footnotes
Supplemental digital content is available for this article.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Kantarjian HM, Kadia TM, DiNardo CD, et al. Acute myeloid leukemia: treatment and research outlook for 2021 and the MD Anderson approach. Cancer 2021; 127:1186–1207. [DOI] [PubMed] [Google Scholar]
- 2.Paczulla AM, Rothfelder K, Raffel S, et al. Absence of NKG2D ligands defines leukaemia stem cells and mediates their immune evasion. Nature 2019; 572:254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abou-el-Enein M, Elsallab M, Feldman SA, et al. Scalable manufacturing of CAR T cells for cancer immunotherapy. Blood Cancer Discov 2021; 2:408–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vormittag P, Gunn R, Ghorashian S, et al. A guide to manufacturing CAR T cell therapies. Curr Opin Biotechnol 2018; 53:164–181. [DOI] [PubMed] [Google Scholar]
- 5.Larson RC, Maus MV. Recent advances and discoveries in the mechanisms and functions of CAR T cells. Nat Rev Cancer 2021; 21:145–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mardiana S, Gill S. CAR T cells for acute myeloid leukemia: state of the art and future directions. Front Oncol 2020; 10:697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hofmann S, Schubert ML, Wang L, et al. Chimeric antigen receptor (CAR) T cell therapy in acute myeloid leukemia (AML). J Clin Med 2019; 8:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acharya UH, Walter RB. Chimeric antigen receptor (CAR)-modified immune effector cell therapy for acute myeloid leukemia (AML). Cancers 2020; 12:3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murad JM, Baumeister SH, Werner L, et al. Manufacturing development and clinical production of NKG2D chimeric antigen receptor-expressing T cells for autologous adoptive cell therapy. Cytotherapy 2018; 20:952–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baumeister SH, Murad J, Werner L, et al. Phase I trial of autologous CAR T cells targeting NKG2D ligands in patients with AML/MDS and multiple myeloma. Cancer Immunol Res 2019; 7:100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallman DA, Brayer JB, Poire X, et al. Results from the completed dose-escalation of the hematological arm of the Phase I Think Study evaluating multiple infusions of NKG2D-based CAR T-cells as standalone therapy in relapse/refractory acute myeloid leukemia and myelodysplastic syndrome patients. Blood 2019; 134:3826. [Google Scholar]
- 12.Sallman DA, Al-Homsi AS, Davila ML, et al. Results from the phase I clinical studies evaluating Cyad-01, a first-Generation NKG2D CAR T-cell product in relapsed or refractory acute myeloid leukemia and myelodysplastic syndrome patients. Blood 2020; 136: (Suppl 1): 40–41. [Google Scholar]
- 13.Breman E, Demoulin B, Agaugué S, et al. Overcoming target-driven fratricide for T cell therapy. Front Immunol 2018; 9:2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernández L, Fernández A, Mirones I, et al. GMP-compliant manufacturing of NKG2D CAR memory T cells using CliniMACS prodigy. Front Immunol 2019; 10:2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Celyad. White Paper: development of the Next Generation NKG2DCAR T-cell manufacturing process. Available at: https://celyad.com/wp-content/uploads/2020/06/191209-OptimAb-process-%C2%B0WHITE-PAPER.pdf. [Accessed 20 October 2021] [Google Scholar]
- 16.Deeren D, Maertens JA, Lin T, et al. First results from the dose escalation segment of the phase i clinical study evaluating Cyad-02, an optimized non gene-edited engineered NKG2D CAR T-cell product, in relapsed or refractory acute myeloid leukemia and myelodysplastic syndrome patients. Blood 2020; 136: (Suppl 1): 36.32430502 [Google Scholar]
- 17.Bakker AB, van den Oudenrijn S, Bakker AQ, et al. C-type lectin-like molecule-1: a novel myeloid cell surface marker associated with acute myeloid leukemia. Cancer Res 2004; 64:8443–8450. [DOI] [PubMed] [Google Scholar]
- 18.Tashiro H, Sauer T, Shum T, et al. Treatment of acute myeloid leukemia with T cells expressing chimeric antigen receptors directed to C-type lectin-like molecule 1. Mol Ther 2017; 25:2202–2213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willier S, Rothämel P, Hastreiter M, et al. CLEC12A and CD33 coexpression as a preferential target for pediatric AML combinatorial immunotherapy. Blood 2021; 137:1037–1049. [DOI] [PubMed] [Google Scholar]
- 20.Zhang H, Gan W-T, Hao W-G, et al. Successful anti-CLL1 CAR T-cell therapy in secondary acute myeloid leukemia. Front Oncol 2020; 10:685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang H, Wang P, Li Z, et al. Anti-CLL1 chimeric antigen receptor T-cell therapy in children with relapsed/refractory acute myeloid leukemia. Clin Cancer Res 2021; 27:3549–3555. [DOI] [PubMed] [Google Scholar]
- 22.Liu F, Cao Y, Pinz K, et al. First-in-human CLL1-CD33 compound CAR T cell therapy induces complete remission in patients with refractory acute myeloid leukemia: update on phase 1 clinical trial. Blood 2018; 132: (Suppl 1): 901. [Google Scholar]
- 23.Liu F, Zhang H, Sun L, et al. First-in-human CLL1-CD33 compound CAR (CCAR) T cell therapy in relapsed and refractory acute myeloid leukemia. Presented at 25th European Hematology Association Congress Virtual; 11–21 June 2020. p. 149. [Google Scholar]
- 24.Jetani H, Garcia-Cadenas I, Nerreter T, et al. CAR T-cells targeting FLT3 have potent activity against FLT3(-)ITD(+) AML and act synergistically with the FLT3-inhibitor crenolanib. Leukemia 2018; 32:1168–1179. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Xu Y, Li S, et al. Targeting FLT3 in acute myeloid leukemia using ligand-based chimeric antigen receptor-engineered T cells. J Hematol Oncol 2018; 11:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sommer C, Cheng H-Y, Nguyen D, et al. Allogeneic FLT3 CAR T cells with an off-switch exhibit potent activity against AML and can be depleted to expedite bone marrow recovery. Mol Ther 2020; 28:2237–2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shrestha E, Liang R, Sirochinsky C, et al. Preclinical development of anti-FLT3 CAR-T therapy for the treatment of acute myeloid leukemia. Blood 2020; 136: (Suppl 1): 4–5.32614961 [Google Scholar]
- 28.Karbowski CM, Goldstein R, Frank B, et al. Nonclinical safety assessment of AMG 553, an investigational anti-FLT3 CAR-T therapy. J Clin Oncol 2019; 37: (15 Suppl): 7032. [Google Scholar]
- 29.Ehninger A, Kramer M, Röllig C, et al. Distribution and levels of cell surface expression of CD33 and CD123 in acute myeloid leukemia. Blood Cancer J 2014; 4:e218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marin V, Pizzitola I, Agostoni V, et al. Cytokine-induced killer cells for cell therapy of acute myeloid leukemia: improvement of their immune activity by expression of CD33-specific chimeric receptors. Haematologica 2010; 95:2144–2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dutour A, Marin V, Pizzitola I, et al. In vitro and in vivo antitumor effect of anti-CD33 chimeric receptor-expressing EBV-CTL against CD33 acute myeloid leukemia. Adv Hematol 2012; 2012:683065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang QS, Wang Y, Lv HY, et al. Treatment of CD33-directed chimeric antigen receptor-modified T cells in one patient with relapsed and refractory acute myeloid leukemia. Mol Ther 2015; 23:184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borot F, Wang H, Ma Y, et al. Gene-edited stem cells enable CD33-directed immune therapy for myeloid malignancies. Proc Natl Acad Sci U S A 2019; 116:11978–11987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Minagawa K, Jamil MO, Al-Obaidi M, et al. Correction: in vitro pre-clinical validation of suicide gene modified anti-CD33 redirected chimeric antigen receptor T-cells for acute myeloid leukemia. PLoS One 2017; 12:e0172640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bras AE, de Haas V, van Stigt A, et al. CD123 expression levels in 846 acute leukemia patients based on standardized immunophenotyping. Cytometry Part B, Clinical cytometry 2019; 96:134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arai N, Homma M, Abe M, et al. Impact of CD123 expression, analyzed by immunohistochemistry, on clinical outcomes in patients with acute myeloid leukemia. Int J Hematol 2019; 109:539–544. [DOI] [PubMed] [Google Scholar]
- 37.Haubner S, Perna F, Köhnke T, et al. Coexpression profile of leukemic stem cell markers for combinatorial targeted therapy in AML. Leukemia 2019; 33:64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perriello VM, Gionfriddo I, Rossi R, et al. CD123 is consistently expressed on NPM1-mutated AML cells. Cancers 2021; 13: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Economides MP, McCue D, Lane AA, Pemmaraju N. Tagraxofusp, the first CD123-targeted therapy and first targeted treatment for blastic plasmacytoid dendritic cell neoplasm. Expert Rev Clin Pharmacol 2019; 12:941–946. [DOI] [PubMed] [Google Scholar]
- 40.Uy GL, Aldoss I, Foster MC, et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood 2021; 137:751–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gill S, Tasian SK, Ruella M, et al. Preclinical targeting of human acute myeloid leukemia and myeloablation using chimeric antigen receptor-modified T cells. Blood 2014; 123:2343–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baroni ML, Sanchez Martinez D, Gutierrez Aguera F, et al. 41BB-based and CD28-based CD123-redirected T-cells ablate human normal hematopoiesis in vivo. J Immunother Cancer 2020; 8:e000845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43▪.Budde E. Chimeric antigen receptor T-cell therapy acute myeloid leukemia: targeting CD123. EHA Library 2019; 14:261697. [Google Scholar]; First clinical data on CD123 CAR-T.
- 44▪.Cummins KD, Gill S. Chimeric antigen receptor T-cell therapy for acute myeloid leukemia: how close to reality? Haematologica 2019; 104:1302–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]; Early review on CAR-T in AML showing the complexity of targeting AML with classical CAR-Ts.
- 45.Roboz GJ, DeAngelo DJ, Sallman DA, et al. Ameli-01: phase I, open label dose-escalation and dose-expansion study to evaluate the safety, expansion, persistence and clinical activity of UCART123 (allogeneic engineered T-cells expressing anti-CD123 chimeric antigen receptor), administered in patients with relapsed/refractory acute myeloid leukemia. Blood 2020; 136: (Suppl 1): 41–42. [Google Scholar]
- 46.Lynn RC, Feng Y, Schutsky K, et al. High-affinity FRβ-specific CAR T cells eradicate AML and normal myeloid lineage without HSC toxicity. Leukemia 2016; 30:1355–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Billingsley MM, Singh N, Ravikumar P, et al. Ionizable lipid nanoparticle-mediated mRNA delivery for human CAR T cell engineering. Nano Lett 2020; 20:1578–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Foster JB, Barrett DM, Karikó K. The emerging role of in vitro-transcribed mRNA in adoptive T cell immunotherapy. Mol Ther 2019; 27:747–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raes L, Stremersch S, Fraire JC, et al. Intracellular delivery of mRNA in adherent and suspension cells by vapor nanobubble photoporation. Nano-micro Lett 2020; 12:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cummins KD, Frey N, Nelson AM, et al. Treating relapsed/refractory (RR) AML with biodegradable anti-CD123 CAR modified T cells. Blood 2017; 130: (Suppl 1): 1359. [Google Scholar]
- 51.Bonini C, Ferrari G, Verzeletti S, et al. HSV-TK gene transfer into donor lymphocytes for control of allogeneic graft-versus-leukemia. Science (New York, New York) 1997; 276:1719–1724. [DOI] [PubMed] [Google Scholar]
- 52.Ciceri F, Bonini C, Stanghellini MT, et al. Infusion of suicide-gene-engineered donor lymphocytes after family haploidentical haemopoietic stem-cell transplantation for leukaemia (the TK007 trial): a nonrandomised phase I-II study. Lancet Oncol 2009; 10:489–500. [DOI] [PubMed] [Google Scholar]
- 53.Minagawa K, Jamil MO, Al-Obaidi M, et al. In vitro pre-clinical validation of suicide gene modified anti-CD33 redirected chimeric antigen receptor T-cells for acute myeloid leukemia. PLoS One 2016; 11:e0166891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tasian SK, Kenderian SS, Shen F, et al. Optimized depletion of chimeric antigen receptor T cells in murine xenograft models of human acute myeloid leukemia. Blood 2017; 129:2395–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kloss CC, Condomines M, Cartellieri M, et al. Combinatorial antigen recognition with balanced signaling promotes selective tumor eradication by engineered T cells. Nat Biotechnol 2013; 31:71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feldmann A, Hoffmann A, Bergmann R, et al. Versatile chimeric antigen receptor platform for controllable and combinatorial T cell therapy. Oncoimmunology 2020; 9: 1785608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Haubner S, Mansilla-Soto J, Nataraj S, et al., editors. ADCLEC.SYN1, a combinatorial car platform for AML (oral presentation). Available at: https://library.ehaweb.org/eha/2021/eha2021-virtual-congress/324658/sascha.haubner.adclec.syn1.a.combinatorial.car.platform.for.aml.html?f=listing%3D3%2Abrowseby%3D8%2Asortby%3D1%2Amedia%3D1. EHA2021; 2021. [Accessed 20 October 2021] [Google Scholar]
- 58.Sakemura R, Terakura S, Watanabe K, et al. A tet-on inducible system for controlling CD19-chimeric antigen receptor expression upon drug administration. Cancer Immunol Res 2016; 4:658–668. [DOI] [PubMed] [Google Scholar]
- 59.Morsut L, Roybal KT, Xiong X, et al. Engineering customized cell sensing and response behaviors using synthetic notch receptors. Cell 2016; 164:780–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park S, Pascua E, Lindquist KC, et al. Direct control of CAR T cells through small molecule-regulated antibodies. Nat Commun 2021; 12:710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61▪▪.Arndt C, Fasslrinner F, Loureiro LR, et al. Adaptor CAR platforms-next generation of T cell-based cancer immunotherapy. Cancers 2020; 12:1302. [DOI] [PMC free article] [PubMed] [Google Scholar]; Comprehensive description of adaptor CAR technology and specific description of the UniCAR system.
- 62.Darowski D, Kobold S, Jost C, Klein C. Combining the best of two worlds: highly flexible chimeric antigen receptor adaptor molecules (CAR-adaptors) for the recruitment of chimeric antigen receptor T cells. MAbs 2019; 11:621–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang Q, Lu W, Liang CL, et al. Chimeric antigen receptor (CAR) Treg: a promising approach to inducing immunological tolerance. Front Immunol 2018; 9:2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yu S, Yi M, Qin S, et al. Next generation chimeric antigen receptor T cells: safety strategies to overcome toxicity. Mol Cancer 2019; 18:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Minutolo NG, Hollander EE, Powell DJ, Jr. The emergence of universal immune receptor T cell therapy for cancer. Front Oncol 2019; 9:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sutherland AR, Owens MN, Geyer CR. Modular chimeric antigen receptor systems for universal CAR T cell retargeting. Int J Mol Sci 2020; 21:7222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Urbanska K, Lanitis E, Poussin M, et al. A universal strategy for adoptive immunotherapy of cancer through use of a novel T-cell antigen receptor. Cancer Res 2012; 72:1844–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tamada K, Geng D, Sakoda Y, et al. Redirecting gene-modified T cells toward various cancer types using tagged antibodies. Clin Cancer Res 2012; 18:6436–6445. [DOI] [PubMed] [Google Scholar]
- 69.Lohmueller JJ, Ham JD, Kvorjak M, Finn OJ. mSA2 affinity-enhanced biotin-binding CAR T cells for universal tumor targeting. Oncoimmunology 2017; 7:e1368604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kudo K, Imai C, Lorenzini P, et al. T lymphocytes expressing a CD16 signaling receptor exert antibody-dependent cancer cell killing. Cancer Res 2014; 74:93–103. [DOI] [PubMed] [Google Scholar]
- 71.Kim MS, Ma JS, Yun H, et al. Redirection of genetically engineered CAR-T cells using bifunctional small molecules. J Am Chem Soc 2015; 137:2832–2835. [DOI] [PubMed] [Google Scholar]
- 72.Ma JS, Kim JY, Kazane SA, et al. Versatile strategy for controlling the specificity and activity of engineered T cells. Proc Natl Acad Sci U S A 2016; 113:E450–E458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Scott D, Nitecki DE, Kindler H, Goodman JW. Immunogenicity of biotinylated hapten-avidin complexes. Mol Immunol 1984; 21:1055–1060. [DOI] [PubMed] [Google Scholar]
- 74.Dale GL, Gaddy P, Pikul FJ. Antibodies against biotinylated proteins are present in normal human serum. J Lab Clin Med 1994; 123:365–371. [PubMed] [Google Scholar]
- 75.Nakamura K, Mimura Y, Takeo K. Immune response to a hapten of fluorescein isothiocyanate in a single mouse analyzed by two-dimensional affinity electrophoresis. Electrophoresis 1993; 14:81–87. [DOI] [PubMed] [Google Scholar]
- 76.Cho Y, Kwon D, Kang SJ. The cooperative role of CD326(+) and CD11b(+) dendritic cell subsets for a hapten-induced Th2 differentiation. J Immunol 2017; 199:3137–3146. [DOI] [PubMed] [Google Scholar]
- 77.Cho JH, Collins JJ, Wong WW. Universal chimeric antigen receptors for multiplexed and logical control of T cell responses. Cell 2018; 173:1426.e11–1438.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Landgraf KE, Williams SR, Steiger D, et al. convertibleCARs: a chimeric antigen receptor system for flexible control of activity and antigen targeting. Commun Biol 2020; 3:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ternant D, Monjanel H, Venel Y, et al. Nonlinear pharmacokinetics of rituximab in non-Hodgkin lymphomas: a pilot study. Br JClin Pharmacol 2019; 85:2002–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cartellieri M, Feldmann A, Koristka S, et al. Switching CAR T cells on and off: a novel modular platform for retargeting of T cells to AML blasts. Blood Cancer J 2016; 6:e458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Loff S, Dietrich J, Meyer JE, et al. Rapidly switchable universal CAR-T cells for treatment of CD123-positive leukemia. Mol Ther Oncolytics 2020; 17:408–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ehninger A, Riewaldt J, Gründer C, et al. Abstract 1506: Expansion kinetics and cytokine profiles of UniCAR-T-CD123, a rapidly switchable two-component CAR-T therapy, in patients with relapsed/refractory AML. Cancer Res 2021; 81: (13 Suppl): 1506. [Google Scholar]
- 83▪▪.Wermke M, Kraus S, Ehninger A, et al. Proof-of-concept for rapidly switchable universal CAR-T platform with UniCAR-T-CD123 in relapsed/refractory AML. Blood 2021; 137:3145–3148. [DOI] [PMC free article] [PubMed] [Google Scholar]; First clinical data with adaptor CAR-T (UniCAR) showing proof of concept of switchability.
- 84.Sommer C, Cheng H-Y, Yeung YA, et al. Preclinical evaluation of ALLO-819, an allogeneic CAR T cell therapy targeting FLT3 for the treatment of acute myeloid leukemia. Blood 2019; 134: (Suppl 1): 3921. [Google Scholar]
- 85.Guzman ML, Sugita M, Zong H, et al. Allogeneic Tcrα/β-deficient CAR T cells targeting CD123 prolong overall survival of AML patient-derived xenografts. Blood 2016; 128:765. [Google Scholar]
- 86.Torikai H, Reik A, Liu PQ, et al. A foundation for universal T-cell based immunotherapy: T cells engineered to express a CD19-specific chimeric-antigen-receptor and eliminate expression of endogenous TCR. Blood 2012; 119:5697–5705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huguet M, Raimond V, Kaltenbach E, et al. How much does the hospital stay for infusion of anti-CD19 CAR-T cells cost to the French National Health Insurance? Bull Cancer 2021; 108:1170–1180. [DOI] [PubMed] [Google Scholar]
- 88.Borgert R. Improving outcomes and mitigating costs associated with CAR T-cell therapy. Am J Manag Care 2021; 27: (13 Suppl): S253–S261. [DOI] [PubMed] [Google Scholar]
- 89.Heine R, Thielen FW, Koopmanschap M, et al. Health economic aspects of chimeric antigen receptor T-cell therapies for hematological cancers: present and future. Hemasphere 2021; 5:e524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Liu J, Zhong JF, Zhang X, et al. Allogeneic CD19-CAR-T cell infusion after allogeneic hematopoietic stem cell transplantation in B cell malignancies. J Hematol Oncol 2017; 10:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim DW, Cho JY. Recent advances in allogeneic CAR-T cells. Biomolecules 2020; 10:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mailankody S, Matous JV, Liedtke M, et al. Universal: an allogeneic first-in-human study of the anti-Bcma ALLO-715 and the anti-CD52 ALLO-647 in relapsed/refractory multiple myeloma. Blood 2020; 136: (Suppl 1): 24–25.32430494 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.