Abstract
J Clin Hypertens(Greenwich). 2010;12:603–612. © 2010 Wiley Periodicals, Inc.
Chart reviews were conducted at 28 US physician practices to evaluate blood pressure (BP) management. The cross‐sectional study included 8250 adult patients diagnosed with hypertension. The primary outcome variable was BP control (BP <140/90 mm Hg for nondiabetic and <130/80 mm Hg for diabetic patients). Mean body mass index was 30.9 kg/m2, 49% were obese, 54% were women, mean age was 64.9 years, and 25% had diabetes. Mean BP was 132.2/77.8 mm Hg, and 55.8% of study participants had controlled BP. Patients with uncontrolled BP were more likely to be obese or African American, and more than twice as likely to have diabetes. Almost 1 in 5 nondiabetic patients (18%), and 38% of diabetic patients, were above goal BP by >10 mm Hg systolic or >5 mm Hg diastolic; among these patients, 36% used 0 or 1 antihypertensive medication, and 32% used 2 medications. Opportunity exists to improve BP control in this population.
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommends that all hypertensive nondiabetic patients should be treated to blood pressure (BP) <140/90 mm Hg, and that all diabetic patients should be treated to BP <130/80 mm Hg. 1 Recent data from the National Health and Nutrition Examination Survey (NHANES) suggests that among all hypertensive patients, about half (53.7%) are treated with antihypertensive medication, and only 57% of all treated patients have controlled BP 2 according to JNC 7 criteria. Among treated diabetic hypertensive patients, only 38% are controlled to BP <130/80 mm Hg. These estimates are somewhat lower than Healthy People 2010 goals for BP control targets among treated hypertensive persons (68% controlled to BP <140/90 mm Hg). 3 Several patient and provider factors may contribute to lack of BP control in medication‐treated patients, including patient adherence to prescribed antihypertensive medication regimen and diet and exercise recommendations and failure of providers to intensify prescribed medication regimens when warranted based on elevated BP (“clinical inertia”). Evidence of clinical inertia in usual‐care settings has been documented in hypertension, 4 , 5 , 6 , 7 as well as other chronic diseases, such as diabetes. 8 , 9
The objective of our study was to determine the proportion of patients with controlled BP among a sample of diabetic and nondiabetic hypertensive patients from physician practices across the United States. We also sought to evaluate the relationship between clinical, demographic, and treatment characteristics and the probability of BP control, and to examine current hypertension management practices across the United States.
Methods
This study was a cross‐sectional, retrospective chart review conducted among 28 practices across the United States. Participating sites varied in size, ranging from 1 to >100 physicians employed by the practice. Study sites were located across the continental United States, with a concentration in the Southern United States (50%) as compared to the Western (18%), Midwestern (18%), or Northeastern (14%) census regions of the United States. Study data were collected between November 2007 and September 2008 at the point‐of‐care via data entry by study investigators at each participating site using a Web‐based application. Requirements for site enrollment included an interest in study participation, capability to abstract required data elements, and an adult hypertensive patient population of sufficient size to allow a random sample of at least 150 patients.
Each study site identified their patient population aged 18 years or older with a documented diagnosis of hypertension (International Classification of Diseases, Ninth Revision [ICD‐9] code of 401.x or clinical diagnosis from chart) in the patient medical record at any time during the previous year. The final study sample thus included both newly‐ and previously‐diagnosed hypertensive patients. Eligible patients were required to have at least 1 year of visit history with the practice site. Patients without a diagnosis of hypertension and pregnant women were also excluded from study eligibility. Participating practices selected a random sample of 150–300 patients from the population meeting study eligibility requirements, using randomized number lists applied to the entire sample of eligible potential study subjects.
A secure Web‐based data collection form was designed for use in this study. Information obtained included patient demographic information, such as age, sex, and racial/ethnic background; information about specific risk factors, such as body mass index (BMI; calculated using inputted height and weight), smoking status, and documentation of lifestyle modification counseling (such as weight reduction, dietary changes, increased physical activity); current antihypertensive medication regimen; total number of different medications used daily for all nonacute conditions; and the specialty of the treating physician. Specific cardiovascular‐related, comorbid conditions documented in the patient record were identified, including coronary artery disease (CAD) without myocardial infarction (MI), MI, diabetes, hyperlipidemia, renal disease, heart failure, and cerebrovascular accident/transient ischemic attack based on the presence of either corresponding ICD‐9 codes or documentation of clinical diagnosis in the patient’s medical record. A composite endpoint of “cardiovascular disease” was defined as the presence of heart failure, CAD without MI, and/or MI. The primary outcome variable in this study was BP control, which was defined as BP <140/90 mm Hg for nondiabetic patients, and <130/80 mm Hg for diabetic patients, based on each patient’s most recent BP measurement. JNC 7 classifications were also used to categorize patients based on BP as normal BP (systolic BP [SBP] <120 mm Hg and diastolic BP [DBP] <80 mm Hg), prehypertensive (SBP 120–139 mm Hg or DBP 80–89 mm Hg), stage I hypertension (SBP 140–159 mm Hg or DBP 90–99 mm Hg), or stage II hypertension (SBP >159 mm Hg or DBP >99 mm Hg). 1 Obesity was defined as a body mass index (BMI) ≥30 kg/m2. In addition, the BP measurement for the visit immediately preceding this most recent BP assessment was obtained. If multiple BP measurements were performed on the same date, study investigators were instructed to record the average of these measurements; however, if different measurement techniques were recorded, such as standing, sitting, and/or supine, investigators were asked to record the sitting BP measurement for study purposes.
Prior to beginning data collection, a training session was conducted with investigators at each site. During the training session, abstraction instructions were provided for each specific data element, and questions related to specific items were answered at that time as per the study protocol. Investigators received a study guide that included a copy of the study protocol describing the study objectives and the data elements to be collected. Furthermore, the study guide contained detailed descriptions of each data element, instructions for abstracting the element from the patient medical record, and comments for each element to assist sites in answering any questions they may have regarding that data element. The study was approved and monitored by the New England Institutional Review Board (Wellesley, MA).
Statistical Methods
Univariate descriptive statistics were calculated for all study variables, including means and standard deviations for continuous variables, and frequency distributions for categorical variables. Bivariate analyses were performed for key study variables using t‐tests and analysis of variance for continuous variables, and the chi‐square test for categorical variables. Multivariate logistic regression analysis was used to assess the impact of independent variables, such as age, sex, diabetes status, and BMI, on the probability of BP control. Variables included in the final model were selected based on both clinical relevance and the results of bivariate analyses. Spline regression techniques, and associated 95% confidence intervals, were used to examine the relationship between the number of antihypertensive medications and BP control, adjusting for covariates. Several study variables were unavailable for a proportion of the study cohort (including BMI, 22%; race/ethnicity, 34%; and smoking status, 20%). A comparison of the study population missing specific data elements vs those not missing each element was conducted, and regressions using cohorts with and without missing data showed no clinically relevant differences in outcome. Missing values were thus assessed as a distinct category in the statistical analyses. Intraclass correlation coefficients were calculated to evaluate clustering of both SBP and DBP within physicians and within practices. Logistic regression was performed with physician clustering and without. Since the models which included clustering revealed little or no impact of clustering on odds ratio estimates, final regression models did not include adjustment for clustering. SAS version 8.2 and SPSS version 16.0 (SPSS Inc, Chicago, IL) were used for all study analyses.
Results
Overall, among the 28 practice sites represented in our study, 8250 patients were included in the final study population. Patient clinical and demographic characteristics are shown in Table I. More than half (53.6%) of the study population was female, and mean patient age was 64.9 (standard deviation [SD] ± 14.0 years). Women in the sample tended to be older (mean age = 66.4 vs 63.0 years for men, P<.001); 54.8% of women were aged 65 years or older, compared to 46.4% of men. About half (47.4%) were Caucasian, 13.2% were African American, and 5.0% were Hispanic; information about racial/ethnic background was not available for 33.8% of the sample. Overall, 11.3% of study patients were current smokers, while 19.6% were past smokers. Men were more likely than women to report being a current (13.5% vs 9.4%, P<.001) or past smoker (25.3% vs 14.8%, P<.001). Mean BMI overall was 30.9 kg/m2, and 48.7% were classified as “obese” (BMI ≥30 kg/m2). Obesity rates were similar by sex, but men were more likely to have diabetes or dyslipidemia. About 6 in 10 patients (59%) had documentation of lifestyle modification counseling in their medical record; obese patients were more likely to receive lifestyle modification counseling as compared to nonobese patients (66% vs 55%, P<.001).
Table I.
Study Population Demographic and Clinical Characteristics
| Men (n=3744, 45.4%) | Women (n=4418, 53.6%) | Total (N=8250) | |
|---|---|---|---|
| Age in years (mean, SD) | 63.0 (13.5) | 66.4 (14.2) | 64.9 (14.0)a |
| Age groups, %a | |||
| 18–34 y | 2.0 | 1.4 | 1.7 |
| 35–44 y | 6.9 | 5.2 | 6.0 |
| 45–54 y | 17.8 | 14.4 | 16.0 |
| 55–64 y | 26.9 | 24.2 | 25.4 |
| 65–74 y | 25.3 | 23.1 | 24.1 |
| >74 y | 21.1 | 31.7 | 26.9 |
| Racial/ethnic background, %b | |||
| Caucasian | 49.0 | 46.0 | 47.4 |
| African American | 11.5 | 14.7 | 13.2 |
| Hispanic | 5.2 | 4.9 | 5.0 |
| Unknown/not documented | 33.7 | 33.9 | 33.8 |
| BMI (kg/m2 mean, SD) | 31.4 (6.3) | 30.7 (7.5) | 30.9 (7.0) |
| Obesity, % | 49.8 | 47.7 | 48.7 |
| Current smokers, % | 13.5 | 9.4 | 11.3a |
| Comorbid cardiovascular‐related conditions, % | |||
| CHF | 3.9 | 4.7 | 4.3 |
| CAD without MI | 16.9 | 11.2 | 13.8a |
| CVA/TIA/carotid stenosis | 5.2 | 5.1 | 5.2 |
| Diabetes | 27.2 | 22.3 | 24.6a |
| Dyslipidemia | 63.6 | 54.6 | 58.7a |
| Renal disease/insufficiency | 7.5 | 6.8 | 7.1 |
| Myocardial infarction | 2.7 | 1.9 | 2.3b |
| Total number of medications for all chronic conditions (mean, SD) | 5.2 (3.4) | 5.8 (3.7) | 5.5a (3.6) |
| BP: most recent measurement in mm Hg (mean, SD) | 131.9/78.6 (16.7/11.0) | 132.5/77.2 (16.8/10.6) | 132.2/77.8a (16.7/10.8) |
| BP: prior measurement in mm Hg (mean, SD) | 131.9/79.1 (16.7/11.3) | 133.6/77.8 (17.4/10.9) | 132.8a/78.4a (17.1/11.1) |
Abbreviations: BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; CHF, congestive heart failure; CVA, cerebrovascular accident; MI, myocardial infarction; SD, standard deviation; TIA, transient ischemic attack. aDenotes that the difference between men and women is statistically significant to P<.001. bDenotes that the difference between men and women is statistically significant to P<.05.
Study participants averaged 1.2 comorbid cardiovascular‐related conditions. Almost 3 in every 5 hypertensive patients (58.7%) also had dyslipidemia, 24.6% had diabetes, 13.8% CAD without MI, 7.1% had renal disease, 5.2% a cerebrovascular accident or transient ischemic attack, 4.3% heart failure, and 2.3% had a prior MI. Overall, 15.2% of study participants had heart disease. Compared to women, men were more likely to have diabetes (27.2% vs 22.3%, P<.001), CAD without MI (16.9% vs 11.2%, P<.001), and dyslipidemia (63.6% vs 54.6%, P<.001). Patients averaged 5.5 (SD + 3.6) prescription medications for chronic conditions; diabetic patients were prescribed a higher number of chronic medications than nondiabetic patients (7.4 vs 4.9, P<.001). About one‐third (35.3%) of patients were treated by a family physician, 49.6% by an internist, and 14.1% by a cardiologist.
Mean BP at the most recent measurement was 132.2/77.8 mm Hg, and 132.8/78.4 mm Hg at the prior measurement (Table I). Overall, 55.8% of study participants had BP controlled to goal at the most recent measurement, and 54.3% had BP controlled at the prior measurement (Table II). The average duration between most recent and prior BP measurements for study participants was 3.5 months (SD ± 4.3). However, among patients who did not have controlled BP at the prior measurement, the mean time to the next BP measurement was 3.3 months (SD + 4.1), as compared to 3.7 months (SD + 4.4) for patients with controlled BP at the prior measurement (P<.001), indicating that overall, patients who were not at BP goal had their next visit, on average, almost 2 weeks earlier than patients who were at BP goal at the previous visit. Among nondiabetic hypertensive patients, two‐thirds (63.3%) had controlled BP, while only one‐third (33.1%) of diabetic hypertensive patients had controlled BP. Stratification of study participants into JNC 7 classifications, based on the most recent BP measurement, indicated that 15.4% of participants had normal BP, 48.3% were prehypertensive, 27.2% had stage I hypertension, and 9.1% had stage II hypertension.
Table II.
Clinical and Demographic Characteristics by BP Control Status Based on Most Recent BP Measurement
| BP Controlleda (n=4606, 55.8%) | BP Uncontrolleda (n=3644, 44.2%) | Total (N=8250) | |
|---|---|---|---|
| Age in years (mean, SD) | 65.2 (14.0) | 64.4 (14.0) | 64.9 (14.0)c |
| Female, % | 55.4 | 52.6 | 53.6c |
| Obese, % | 43.9 | 54.6 | 48.7d |
| With diabetes, % | 14.6 | 37.3 | 24.6d |
| Total number of medications for all chronic conditions (mean, SD) | 5.5 (3.5) | 5.6 (3.6) | 5.5 (3.6) |
| Race/ethnicityb,d | |||
| Caucasian, % | 77.7 | 63.7 | 71.6 |
| African American, % | 14.4 | 27.0 | 19.9 |
| Hispanic, % | 7.0 | 8.3 | 7.6 |
| Physician specialty, % | |||
| Family practice | 34.5 | 33.9 | 34.2 |
| Internal medicine | 51.1 | 52.8 | 51.9 |
| Cardiology | 14.1 | 13.0 | 13.6 |
| Other/not available | 0.3 | 0.2 | 0.3 |
| Antihypertensive medication use, %d | |||
| No antihypertensive medication | 6.7 | 7.3 | 6.9 |
| Monotherapy | 32.2 | 30.3 | 31.3 |
| Combination therapy, 2 antihypertensive classes | 36.3 | 32.7 | 34.7 |
| Combination therapy, >2 antihypertensive classes | 24.8 | 29.7 | 27.0 |
| Number of antihypertensive medication classes (mean, SD) | 1.9 (0.1) | 2.0 (1.2) | 1.9 (1.1)c |
Abbreviations: BP, blood pressure; SD, standard deviation. aBP control based on most recent BP measurement, and defined as <140/90 mm Hg for non‐diabetic patients, and <130/80 mm Hg for diabetic patients. bRace/ethnicity percentages calculated based on denominator of patients with non‐missing data for racial/ethnic background (n=5422). cDenotes statistical significance at P<.02. dDenotes statistical significance at P<.001.
Table II includes a comparison of characteristics for patients with controlled vs uncontrolled BP. As compared to patients with controlled BP, patients with uncontrolled BP were more likely to be obese, more than twice as likely to have diabetes, and more likely to be African American.
Control rates for individual practice sites ranged from 32% to 78% (Figure 1). The intraclass correlation coefficient for provider for SBP was 0.08, and for DBP the intraclass correlation coefficient was 0.14. The intraclass correlation coefficient for practice site for SBP was 0.05, and for DBP the intraclass correlation coefficient was 0.11. Participating practice sites were ranked in order of total proportion of patients with controlled BP, and the relationship of practice‐level BP control and patient and provider characteristics is included in Table III. Practices with the lowest proportion of patients with controlled BP had the highest proportion of African‐American patients. At a practice level, the proportion with controlled BP tended to decrease with increasing diabetes prevalence. At a geographical region level, relative to other practices, participating practices located in the Western United States tended to have lower proportions of patients controlled, while participating practices from the Midwest tended to have higher proportions with controlled BP. Practices in the highest BP control category had a higher mean number of antihypertensive medication classes per patient as compared to other BP control categories (P<.001, all comparisons). Overall, 93.1% of the hypertensive patient population was treated with an antihypertensive medication. Approximately 31% of patients received antihypertensive monotherapy, while 35% received combination therapy with 2 different classes of antihypertensive medication (Table II). About 27% of combination therapy patients used a combination regimen comprised of 3 or more antihypertensive medication classes. Mean number of antihypertensive medications used by study participants was 1.9 (SD ± 1.1). Patients classified as having either a normal BP or stage II hypertension, according to JNC 7 classification, were prescribed a mean of 2.0 (±1.2) and 2.1 (±1.2) antihypertensive medication classes, respectively; both categories of patients were prescribed significantly more antihypertensive medications than either prehypertensive patients (mean = 1.9, SD = 1.1) or stage I hypertensive patients (mean = 1.9, SD = 1.1) (P<.01, all comparisons). Most frequently used medications were angiotensin‐converting enzyme inhibitors (39%), thiazide diuretics (37%), β‐blockers (36%), and angiotensin‐II receptor blockers (28%).
Figure 1.
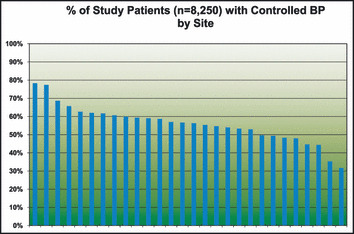
Comparison of overall blood pressure (BP) control by site for all participating study sites.
Table III.
Association of Patient and Provider Characteristics and BP Control by Participating Site BP Control Rank
| Control Rank Category (1 = Highest, 7 = Lowest) | BP Controlled, (%) | Age (Mean, SD) | Female, % | Obese, % | African American, % | Hispanic, % | Diabetes, % | Total Number of Antihypertensive Medications (Mean, SD) | Provider Specialty | Geographical Region, % | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Family Practice, % | Internal Medicine, % | Cardiology, % | Northeast | South | Midwest | West | |||||||||
| Category 1 (n=1200) | 72.5 | 63.1 (13.2) | 46.6 | 49.4 | 17.6 | 0.8 | 23.4 | 2.2 (1.2) | 24.9 | 50.1 | 25.0 | 25.0 | 50.0 | 25.0 | 0.0 |
| Category 2 (n=1050) | 61.9 | 67.9 (13.7) | 58.0 | 48.1 | 1.9 | 0.7 | 26.5 | 1.9 (1.1) | 43.0 | 53.2 | 1.9 | 25.0 | 25.0 | 50.0 | 0.0 |
| Category 3 (n=1200) | 59.3 | 67.7 (13.5) | 53.8 | 47.9 | 2.3 | 0.6 | 25.3 | 2.0 (1.1) | 8.0 | 66.4 | 25.5 | 0.0 | 75.0 | 25.0 | 0.0 |
| Category 4 (n=1200) | 56.3 | 61.0 (14.7) | 54.6 | 47.8 | 3.8 | 1.4 | 17.2 | 1.6 (1.0) | 63.2 | 36.8 | 0.0 | 25.0 | 25.0 | 0.0 | 50.0 |
| Category 5 (n=1200) | 53.8 | 67.8 (13.3) | 53.6 | 48.0 | 1.9 | 24.1 | 27.5 | 1.9 (1.1) | 27.5 | 56.0 | 16.5 | 25.0 | 50.0 | 0.0 | 25.0 |
| Category 6 (n=1200) | 48.8 | 63.8 (13.7) | 55.3 | 48.8 | 16.3 | 4.8 | 26.3 | 2.0 (1.2) | 49.2 | 25.7 | 25.0 | 0.0 | 75.0 | 0.0 | 25.0 |
| Category 7 (n=1200) | 39.0 | 63.0 (14.2) | 57.5 | 50.4 | 47.2 | 2.3 | 26.4 | 1.9 (1.1) | 25.0 | 75.0 | 0.0 | 0.0 | 50.0 | 25.0 | 25.0 |
| Total (n=8250) | 55.8 | 64.9 (14.0) | 54.1 | 48.7 | 13.2 | 5.0 | 24.6 | 1.9 (1.1) | 34.2 | 51.9 | 13.6 | 14.3 | 50.0 | 17.9 | 17.9 |
Abbreviations: BP, blood pressure; SD, standard deviation. Participating sites were ranked by proportion of total patients with controlled BP and assigned to a category based on this rank. Each ranked category comprised 4 participating sites.
Almost 1 in 5 nondiabetic patients (17.8%), and more than one‐third of diabetic patients (37.6%), had either an SBP that was above goal by 10 or more mm Hg or a DBP that was more than 5 mm Hg over goal. Additionally, 19.0% of nondiabetic patients, and 29.3% of diabetic patients, had either an SBP within 10 mm Hg or a DBP within 5 mm Hg of target BP. Analysis of antihypertensive medication prescribed for these patients indicated that 36% of patients whose BP measurement was above goal BP by >10/5 mm Hg were only prescribed 0 or 1 antihypertensive medication class, and an additional 32% were prescribed a regimen consisting of 2 antihypertensive classes of medication. Two in every 5 (40%) patients whose BP was higher than goal by no more than 10/5 mm Hg were prescribed either 0 or 1 antihypertensive medication, and an additional 34% were prescribed a regimen consisting of 2 antihypertensive medication classes.
Table IV includes multivariate odds ratios for BP control. Diabetes status was strongly associated with probability of BP control, adjusted for other covariates. Obese patients were less likely to have BP controlled, as were African Americans and persons aged 65 years and older. The number of prescribed medications for conditions other than hypertension was associated with an increased probability of BP control, controlling for other covariates. Table V provides odds ratios of BP control for the subset of patients prescribed 2 antihypertensive medications in combination (n=2866), and for patients prescribed more than 2 antihypertensive medications (n=2227). Presence of diabetes was strongly associated with uncontrolled BP. The odds associated with use of fixed dose combination regimens (compared to free combination only) and BP control was higher for patients prescribed 3 or more antihypertensive medications, but did not reach statistical significance. For both combination therapy groups, increasing chronic prescription count was associated with greater odds of BP control. Figure 2 depicts the relationship between the number of antihypertensive medication classes and BP control, adjusting for age, sex, diabetes status, presence of cardiovascular disease, and number of chronic medications.
Table IV.
Multiple Logistic Regression for Blood Pressure Control in the HATT Study Population (n=8010)a
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| Diabetes | ||
| No | 1 | |
| Yes | 0.261 | 0.232–0.294 |
| Antihypertensive regimen | ||
| No therapy | 0.887 | 0.728–1.080 |
| Monotherapy | 1.0 | |
| Combination, 2 antihypertensive meds | 1.116 | 0.993–1.254 |
| Combination, >2 antihypertensive meds | 0.880 | 0.771–1.004 |
| Age | ||
| <65 | 1 | |
| ≥65 | 0.867 | 0.784–0.959 |
| Body mass index | ||
| <30 | 1 | |
| ≥30 | 0.724 | 0.650–0.808 |
| Missing | 1.020 | 0.898–1.159 |
| Sex | ||
| Female | 1 | |
| Male | 0.951 | 0.865–1.045 |
| Race/ethnicity | ||
| Caucasian | 1 | |
| African American | 0.440 | 0.380–0.510 |
| Hispanic | 0.928 | 0.744–1.159 |
| Other, missing | 0.728 | 0.655–0.808 |
| Physician specialty | ||
| Family practice | 1 | |
| Internal medicine | 0.886 | 0.799–0.983 |
| Cardiology | 0.960 | 0.821–1.123 |
| Prescribed lifestyle modifications | ||
| No | 1 | |
| Yes | 1.122 | 1.016–1.239 |
| Number of chronic medications | ||
| 0–2 | 1 | |
| 3–4 | 1.041 | 0.906–1.198 |
| 5–6 | 1.296 | 1.109–1.516 |
| 7–9 | 1.512 | 1.278–1.789 |
| >9 | 1.630 | 1.345–1.975 |
a8010 of the 8250 subjects were included in the final logistic regression model. Abbreviation: HATT, Hypertension: Assessment of Treatment to Target.
Table V.
Multiple Logistic Regression for BP Control in the HATT Study Participants Prescribed Combination Therapy Regimens (n=5093)
| Combination, 2 Antihypertensive Medications | Combination, >2 Antihypertensive Medications | |
|---|---|---|
| N | 2866 | 2227 |
| BP controlled, % | 58.4 | 51.4 |
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Fixed dose combination (FDC) vs free combination | ||
| No FDC | 1 | 1 |
| FDC | 1.047 (0.876–1.252) | 1.116 (0.921–1.352) |
| Diabetes | ||
| No | 1 | 1 |
| Yes | 0.276 (0.227–0.336) | 0.265 (0.214–0.326) |
| Age | ||
| <65 | 1 | 1 |
| ≥65 | 0.908 (0.764–1.078) | 0.852 (0.697–1.043) |
| Body mass index | ||
| <30 | 1 | 1 |
| ≥30 | 0.705 (0.587–0.846) | 0.860 (0.696–1.063) |
| Missing | 0.906 (0.725–1.133) | 1.054 (0.816–1.363) |
| Sex | ||
| Female | 1 | 1 |
| Male | 1.005 (0.856–1.180) | 1.074 (0.894–1.289) |
| Race/ethnicity | ||
| Caucasian | 1 | 1 |
| African American | 0.507 (0.398–0.647) | 0.402 (0.309–0.522) |
| Hispanic | 0.790 (0.542–1.153) | 0.544 (0.363–0.816) |
| Other, missing | 0.705 (0.589–0.844) | 0.630 (0.510–0.778) |
| Physician specialty | ||
| Family practice | 1 | 1 |
| Internal medicine | 0.877 (0.735–1.048) | 0.738 (0.596–0.913) |
| Cardiology | 0.916 (0.697–1.205) | 0.707 (0.536–0.934) |
| Prescribed lifestyle modifications | ||
| No | 1 | 1 |
| Yes | 1.113 (0.939–1.320) | 0.914 (0.754–1.108) |
| Number of chronic medications | ||
| 0–4 | 1 | 1 |
| 5–6 | 1.490 (1.204–1.843) | 1.228 (0.938–1.609) |
| 7–9 | 1.558 (1.233–1.970) | 1.535 (1.170–2.013) |
| >9 | 1.595 (1.118–2.142) | 1.715 (1.273–2.311) |
Abbreviations: BP, blood pressure; CI, confidence interval; HATT, Hypertension: Assessment of Treatment to Target
Figure 2.
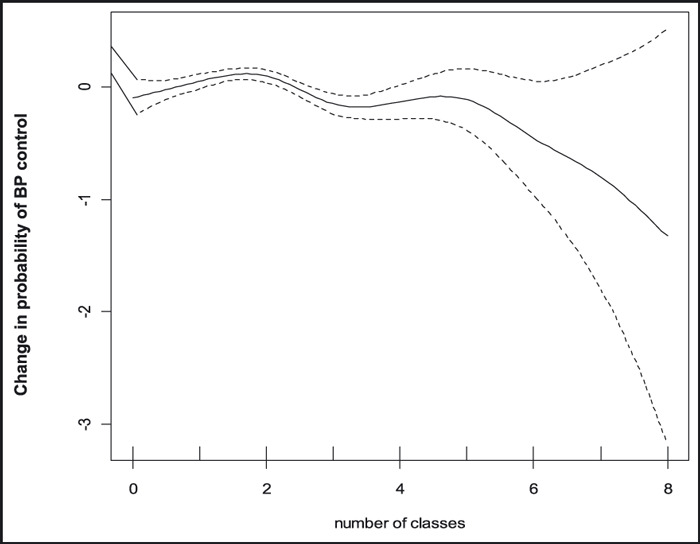
Change in probability of BP control by number of antihypertensive medication classes in regimen, adjusted for diabetes status, age, sex, presence of coronary artery disease (CAD), and number of chronic prescriptions.
Discussion
In the current study of hypertension control across 28 US practices, overall, 55.8% of patients had controlled BP. Consistent with other published studies, nondiabetic hypertensive patients were much more likely to have controlled BP (63.3%) than diabetic patients (33.1%). As compared to patients with controlled BP, patients with uncontrolled BP were more likely to be obese or African American. The proportion of patients with controlled BP at participating sites varied from 32% to 78%. Study results related to BP management for each site’s hypertensive patient sample were made available to study investigators at that site. Many of these sites shared the data at various levels within their organizations to identify areas where opportunity existed for improvement of BP control across their patient populations.
The proportion of patients from the current study with controlled BP (55.8%) is similar to the proportion of hypertensive adults with controlled BP from NHANES 2003–2004 who are treated for hypertension (56.6%); 2 this comparison is probably the most appropriate given our cohort inclusion criteria, although 7% of our study population did not receive antihypertensive medication. In addition, 33.1% of our study’s diabetic hypertensive population had controlled BP, compared to 37.5% of hypertensive diabetic subjects from NHANES. 2 In the current study, hypertensive patients were more likely to have diabetes (24.6%) as compared to hypertensive adults included in NHANES (15.3%). 10 However, the prevalence of other comorbid conditions was similar between the current study and NHANES 1999–2002: stroke (5.2% vs 5.9%), renal disease (7.1% vs 11.6%), and heart disease (18.1% vs 15.2%), 10 although the 2 studies utilized slightly different definitions for the assessment of comorbid conditions. A potential explanation for the higher prevalence of diabetes in our study is related to obesity, as almost half of our study population was obese (48.7%), compared to 40.5% from NHANES. 10
In hypertension, clinical inertia has been defined as the failure of healthcare providers to initiate or intensify antihypertensive therapy in a patient with uncontrolled BP, either by maximizing dosages of existing medications or adding another class of antihypertensive medication. 4 , 5 , 6 , 7 Heisler and colleagues studied 68,610 elevated BP events (SBP >140 mm Hg and <200 mm Hg or DBP >90 mm Hg) and found that providers intensified the prescribed antihypertensive medication regimen in only one‐third of such events. 4 Similarly, another large study demonstrated antihypertensive therapy intensification at only 38% of study visits, despite elevated BP for at least 6 months preceding the study visit. 5 Andrade and colleagues found that providers intensified antihypertensive regimens at 10% of visits with patient SBP 140–149 mm Hg, and at 45% of visits with SBP ≥180 mm Hg; 21% of visits with DBP between 90 to 99 mm Hg, and 43% of visits with DBP ≥100 mm Hg, had a subsequent therapy intensification. 7 The reasons for clinical inertia remain unclear, but may include an overestimation of the amount of care actually provided, a lack of training regarding attainment of goal BP, and the adoption of a “wait and see” approach. 11 In the current study almost 1 in 5 nondiabetic patients, and about 2 in 5 diabetic patients, had BP measurements that were at least10 mm Hg systolic or 5 mm Hg diastolic higher than target BP. However, while combination antihypertensive medication regimens were common in our population, among patients not at goal BP, 36% were prescribed 0 or 1 antihypertensive medication, and 32% were prescribed 2 medications. While practice‐level analysis of BP control suggested that participating sites with the highest proportion of controlled patients also prescribed more antihypertensive medications, this finding did not persist after statistical adjustment for other covariates. Figure 2 illustrates that, adjusted for other variables, across our study population the probability of BP control did not appear to increase with an increased number of antihypertensive medications, which suggests the role of other factors in BP goal attainment. These may include physician‐related factors such as inadequate patient education regarding the importance of lifestyle changes for long‐term hypertension control, prescription of lifestyle changes, and prescription of less than effective or inadequate pharmacologic therapy. Patient‐related factors, such as compliance with prescribed medication or lifestyle recommendations, motivation, and health literacy may also play a role. The current study was unable to evaluate medication compliance, which may contribute to lack of BP control in a substantial number of treatment failures. 12 , 13 Although we cannot attribute specific unknown factors to BP control, our population includes a sizable number of patients at higher risk (>5/10 mm Hg above goal) who are not treated more intensively (with a higher number of antihypertensive medications) despite this risk.
While this study provides useful information regarding hypertension management across a sample of physician practices, it is important to consider our results in the context of several important limitations. Some patient information was not available for analysis, including duration of hypertension, patient compliance with prescribed antihypertensive medication regimen, duration of medication use, and patient insurance status. In addition, some data elements had a sizable number of patients with missing information, particularly height for calculation of BMI, smoking status, and racial/ethnic background. Most missing BMI information was due to nondocumentation of patient height in the medical record, and many participating sites cited this as potential quality improvement initiative. While the total number of prescribed medications for all chronic conditions was obtained, information regarding specific medications used for conditions other than hypertension (such as nonsteroidal anti‐inflammatory drugs, antidepressants) which may have affected BP was not collected. The presence of other patient comorbid conditions, including sleep apnea and other sleep disorders, may affect patient BP and these were not available for our study. Because this study was retrospective in nature, standardization or validation of BP measurements was not possible, so measurement error may have played a role in our study’s findings. Furthermore, the cross‐sectional, non‐longitudinal nature of this study does not permit the assessment of a “cause and effect” relationship between BP control and medication use. Site selection was nonrandom and was based on several factors, including site interest in participation, and the study was not designed to be representative of the demographic composition of the US hypertensive population as a whole. Thus, it is difficult to ascertain whether selection bias may play a role in some of our study’s findings. Our study revealed variation among practices in the proportion of hypertensive patients with controlled BP and some interesting differences regarding practice‐level results as related to practice and patient characteristics; however, as the current study was not specifically designed to determine practice‐level predictors of BP control, some practice‐level data, including payer mix, was not available for analysis. Nevertheless, despite these limitations, this study provides important information regarding current hypertension management practices across the United States.
In conclusion, across 28 US practices, 56% of hypertensive patients had controlled BP, almost half of the hypertensive study population was obese, and 25% had diabetes. Since patients with uncontrolled BP were more likely to be obese, and more than 2 times as likely to have diabetes, as those with controlled BP, interventions targeting weight reduction in this population may have important consequences in controlling BP. It is an important challenge to physicians to understand the reasons for specific patients’ barriers to BP control. For some patients, this may be related to patient noncompliance with prescribed antihypertensive medication or lifestyle modification recommendations; however, it may be difficult for physicians to always be aware of the impact of each of these factors on BP goal attainment in specific patients despite efforts by the physician and support staff at compliance and lifestyle counseling. Other patients may benefit from an increased dosage of their current antihypertensive medication regimen. Alternatively, some physicians may not recognize the benefit of BP goal attainment, particularly for elderly and/or diabetic patients. 14 While JNC 7 emphasizes that most hypertensive patients will require 2 or more antihypertensive classes of medication to achieve and/or maintain BP control, 1 many patients from our study who were not at goal BP were prescribed 2 or fewer antihypertensive medications, and 36% of patients whose BP measurement was above goal BP by >10/5 mm Hg were only prescribed 0 or 1 antihypertensive medication class. The addition of one or more medications from other antihypertensive classes to an existing medication regimen may improve BP control in this population.
Disclosures: This study was funded by Novartis Pharmaceuticals Corporation. Daniel Belletti and Christopher Zacker are employees of Novartis Pharmaceuticals Corporation, the maker of several drugs indicated for the treatment of hypertension, and own stock and stock options in Novartis. Jenifer Wogen is with MedMentis Consulting, which received compensation from Novartis for assistance with the study and manuscript preparation.
Acknowledgments
Acknowledgment: The authors would like to thank Douglas Gause MS, DrPH, and Joanne M. Foody, MD, for their review of an earlier version of the manuscript.
References
- 1. Chobanian A, Bakris G, Black H. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 2. Ong KL, Cheung BMY, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services . Healthy People 2010 . With Understanding and Improving Health and Objectives for Improving Health, 2nd ed. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 4. Heisler M, Hogan MM, Hofer TP, et al. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008;117:2884–2892. [DOI] [PubMed] [Google Scholar]
- 5. Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician‐related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. [DOI] [PubMed] [Google Scholar]
- 6. Hyman D, Pavlik V, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens (Greenwich). 2000;2:324–330. [PubMed] [Google Scholar]
- 7. Andrade S, Gurwitz J, Field T, et al. Hypertension management: the care gap between clinical guidelines and clinical practice. Am J Manag Care. 2004;10:481–486. [PubMed] [Google Scholar]
- 8. Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Diabetes Care. 2005;28:600–606. [DOI] [PubMed] [Google Scholar]
- 9. Brown JB, Nichols GA. Slow response to loss of glycemic control in type 2 diabetes mellitus. Am J Managed Care. 2003;9:213–217. [PubMed] [Google Scholar]
- 10. Giles T, Aranda JM, Suh DC, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich). 2007;9:345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ogedegbe G. Barriers to optimal hypertension control. J Clin Hypertens. 2008;10:644–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stephenson J. Noncompliance may cause half of antihypertensive drug “failures”. JAMA. 1999;282:313–314. [DOI] [PubMed] [Google Scholar]
- 13. Bramley TJ, Gerbino PR, Nightengale BS, et al. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. 2006;12:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moser M. Physician or clinical inertia: what is it? Is it really a problem? And what can be done about it J Clin Hypertens (Greenwich). 2009;11:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


