Abstract
Objectives
The aim of this study was to compare oral health–related quality of life (OHRQoL) in children with and without molar incisor hypomineralization (MIH) and to assess the impact of severity of MIH on OHRQoL in children between 8–10 years using the German version of the Child Perceptions Questionnaire (CPQ-G8-10).
Materials and methods
Children aged 8–10 years were recruited at a pediatric dental clinic in Hannover, Germany. Half of them were affected by MIH. Participants were evaluated for presence and severity of MIH (MIH-TNI), plaque and dental caries status. Children were asked to answer the CPQ-G8-10. Statistical analysis was performed using GraphPad Prism-software version 8.
Results
One hundred eighty-eight children (mean age 8.80 [± 0.84]; 43.10% female) were included in the study with 94 children having MIH. CPQ-G8-10 mean scores in MIH-affected children were significantly higher than in children showing no MIH (13.87 [± 8.91] vs. 4.20 [± 3.74]; p < 0.0001) showing that MIH has negative impact OHRQoL. Similar trends were seen in all four subdomains. Regarding severity, CPQ-G8-10 mean scores increased from mild to severe forms of MIH.
Conclusion
Children affected by MIH show an impaired OHRQoL compared to children without MIH; with increasing severity, OHRQoL gets more impaired.
Clinical relevance
To understand the patient’s perception and the individual oral health needs will help to prioritize MIH and recognize its impact.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00784-021-04150-w.
Keywords: Molar incisor hypomineralization, MIH, Child Perceptions Questionnaire, CPQ8-10, Oral health–related quality of life, OHRQoL
Introduction
Molar incisor hypomineralization (MIH) is a phenomenon defined as a quality defect of enamel of systemic origin of one to four permanent first molars frequently associated with affected incisors [1]. It affects around 13.1% of the global population that is around 878 million people. Out of these, 27.4% of the cases are affected with symptoms and post-eruptive enamel breakdown (PEB) and are in need of treatment [2]. In Germany, the average prevalence of MIH is 10.1%, with a variation from 4.3 to 14.6% in different regions [3]. Clinically, the lesions are porous and appear as well-demarcated opacity, mostly on the occlusal and buccal areas of the tooth surface which are usually more than 1 mm, and the color ranges from white, creamy or yellow, to brownish [4].
MIH-affected children face a number of difficulties in their daily life. Due to the porosity in severely affected enamel, masticatory forces break down the tooth surfaces, resulting in unprotective dentine in large atypical cavities. Exposed dentine causes hypersensitivity or rapid formation of caries [5]. These teeth are not only temperature-sensitive but can also cause pain on mechanical stimulus. This may adversely affect even the simplest of the daily vital activities like brushing or eating [6, 7]. In addition, aesthetics also plays an important role when the incisors are affected. Incisal defects are pretty extensive occurring mainly on the buccal surface leading to the aesthetic concern. The children’s appearance not only upsets the mothers but also has a negative influence on the children, preventing them from smiling [8]. Such aesthetics may lead to a negative social impact [7].
These problems described above may affect oral health–related quality of life (OHRQoL) in MIH patients. It is known that OHRQoL is an integral part of one’s well-being and general health [9]. The subjective evaluation of OHRQoL “reflects people’s comfort when eating, sleeping, and engaging in social interaction; their self-esteem; and their satisfaction with respect to their oral health” [10]. For children aged 8 to 10 years, the Child Perceptions Questionnaire (CPQ8-10) is the most frequently used instrument to measure OHRQoL in this age group [11]. It is a generic questionnaire which was designed to cover a variety of oral conditions.
Although MIH is known for 20 years now, there is still scarce data about the relationship between MIH and OHRQoL. Very few international studies have focused on this topic and have also shown varying results [12–14]. To date, only one study compared OHRQoL in children with and without MIH in Mexico [12]. However, these study patients were not matched but taken from a cross-sectional study. Furthermore, no study has focused on this topic in Germany yet.
Therefore, the aim of this study was to compare OHRQoL in children with and without MIH and to assess the impact of severity of MIH on OHRQoL in children between 8 and 10 years using the German version of the CPQ-G8-10.
Materials and methods
Design
For this prospective matched pairs study, German children aged 8 to 10 years were recruited at the “Magic Dental Clinic”, Hannover, Germany. The enrolment into this study was voluntary. Extended information leaflets on the aim of the study were handed out and explained to the parents who gave their written and oral informed consent. The approval for the study procedures was granted by the ethics committee of the local University Review Board (Hannover Medical School, 9158_BO_K_2020).
Subjects and setting
All dentists of the dental clinic were briefed about the details of the study and asked to recruit patients. A calibrated examiner (TJ) performed all clinical examinations. The criteria proposed by the European Academy of Paediatric Dentistry (EAPD) [4] were used for the diagnosis of MIH. These include the presence of demarcated opacities, post-eruptive enamel breakdown, atypical restorations, and extraction due to MIH in at least one first permanent molar. Demarcated opacities with a diameter of < 1 mm were not considered in the analysis.
German-speaking children between 8 and 10 years of age and with fully erupted all first permanent molars were included in the study. Exclusion criteria were systemic comorbidities, physical or mental disability, severe malocclusion, or undergoing orthodontic treatment, enamel developmental defects other than MIH.
According to the sample size calculation, a total of 188 subjects were required for the present study. The formula that was used for sample size calculation was n = (Z α/2 + Z β) 2 * 2 * σ2/d 2, where Z α/2 was the critical value of the normal distribution at α/2 (confidence level is of 95%, and therefore, α was 0.05 and the critical value was 1.96), Z β was the critical value of the normal distribution at β (power of 80% is considered and therefore β was 0.2 and the critical value is 0.84), σ2 is the population variance, and d is the difference which is considered to be 10. Based on this calculation, a total of 157 subjects were needed. After adding a 20% drop out rate, 188 children were recruited. The subjects were evenly divided into two groups. Group I consisted of 94 subjects with MIH and group II consisted of 94 subjects without MIH.
Data collection
During a single visit to the dental clinic, subjects were instructed to first brush their teeth followed by a clinical examination to grade the presence or absence of MIH, dental caries status using the dmft/DMFT index, and the plaque status using the Approximal Plaque Index (API). In case of presence of MIH, children were further examined for the severity of MIH using the MIH treatment need index (MIH-TNI) [15]. The MIH-TNI takes into account two most important clinical symptoms: post-eruptive breakdown and hypersensitivity: MIH-TNI 1 no breakdown, no hypersensitivity; MIH-TNI 2 breakdown, no hypersensitivity; MIH-TNI 3 no breakdown, hypersensitivity; MIH-TNI 4 breakdown, hypersensitivity.
To assess the child’s OHRQoL, the validated German version of the CPQ8-10 was used [16]. The CPQ8-10 contains a total of 25 items which can be subdivided into four domains: oral symptoms (five items), functional limitations (five items), emotional well-being (five items), and social well-being (ten items). Questions ask about the frequency of events in the child’s last 4 weeks. Responses are made on an ordinal scale (0 = ever, 1 = once/twice, 2 = sometimes, 3 = often, 4 = every day/almost every day). Higher scores refer to a worse OHRQoL status. Summing the response codes for the questionnaire items generates domain scores/sub-scales and an overall CPQ-G8-10 score. The instrument’s summary score ranges from 0 to 100. A summary score of zero indicates the absence of any problems, and higher CPQ scores represent more impaired OHRQoL. In addition to the 25 items, the CPQ-8–10 includes two questions asking the child for a global rating of the oral health and the overall well-being. These global ratings had a five-point response format (excellent, very good, good, moderate, poor).
Data analysis
After data collection, statistical analysis was done using GraphPad Prism software version 8. The D’Agostino-Pearson normality test was used to determine whether the sets of scores/indices to be compared followed a Gaussian distribution or not. Based on this, either the unpaired Student t-test or the Mann–Whitney test was performed for comparison between two groups. Wherever a comparison between multiple groups was involved, either the one-way ANOVA (analysis of variance) or the Kruskal–Wallis test was used to determine the statistical significance. A p-value of less than 0.05 was considered significant.
Results
Study population
A total of 188 subjects aged 8–10 years (43.1% female) were involved in this study. They were equally divided into two groups with 94 subjects affected with MIH (50% female). The mean age was 8.80 years (± 0.84 years) (Table 1). The mean dmft/DMFT score for the MIH group was 5.04 (± 3.73) and 5.49 (± 3.84) for the control demonstrating a comparable experience. A significant higher API was observed in children suffering from MIH (50.53% (± 33.72) vs. 40.34% (± 33.07)) (p < 0.05, Mann–Whitney test).
Table 1.
General characteristics of participants
| Characteristics | All | Control | MIH |
|---|---|---|---|
| Gender (N, %) | 188 (100%) | 94 (100%) | 94 (100%) |
| Male | 107 (56.9%) | 60 (63.8%) | 47 (50%) |
| Female | 81 (43.1%) | 34 (36.2%) | 47 (50%) |
| Mean age (years, SD) | 8.80 (0.84) | 8.74 (0.79) | 8.87 (0.88) |
| Mean dmft/DMFT score (SD) | 5.27 (3.79) | 5.49 (3.84) | 5.04 (3.73) |
| Mean API (%) | 45.29 (± 33.72) | 40.34 (± 33.07) | 50.53 (± 33.72) |
Oral health–related quality of life in patients with and without MIH
The mean CPQ-G8-10 score for MIH-affected children was 13.87 (± 8.91; median 12; range 0–48) while the control group showed a reduced score of 4.20 (± 3.73; median 3; range 0–18), indicating a better self-perceived oral-health (Table 2, Supplement). The scores of the subdomains of the CPQ-G8-10 followed the same patterns. Oral symptoms (6.88 [± 3.76] vs. 2.29 [± 2.60]), functional limitations (2.35 [± 2.36] vs. 0.88 [± 1.35]), emotional well-being (2.91 [± 3.23] vs. 0.66 [± 1.24]), and social well-being (1.72 [± 2.62] vs 0.38 [± 0.96]) were significantly increased in MIH patients (p < 0.001, t-test). Furthermore, female MIH patients showed a higher total score compared to males (15.96 [± 9.99] vs. 11.79 [± 7.20]) which was statistically significant. As expected, MIH patients’ high scores were observed in the subdomain “oral symptoms” which includes questions on the frequency of pain.
Table 2.
CPQ-G8-10 mean scores in patients with and without MIH
| Total score | Oral symptoms | Functional limitations | Emotional well-being | Social well-being | |
|---|---|---|---|---|---|
| Control (MIH-TNI 0) | |||||
| All | 4.20 (± 3.74) | 2.29 (± 2.60) | 0.88 (± 1.35) | 0.66 (± 1.24) | 0.38 (± 0.96) |
| Female | 4.50 (± 3.69) | 2.03 (± 2.12) | 0.97 (± 1.45) | 0.88 (± 1.61) | 0.62 (± 1.81) |
| Male | 4.03 (± 3.79) | 2.43 (± 2.83) | 0.82 (± 1.30) | 0.53 (± 0.96) | 0.25 (± 0.80) |
| MIH | |||||
| All | 13.88 (± 8.91) | 6.88 (± 3.76) | 2.35 (± 2.36) | 2.91 (± 3.23) | 1.72 (± 2.62) |
| Female | 15.96 (± 9.99) | 7.51 (± 3.82) | 2.55 (± 2.57) | 3.68 (± 3.72) | 2.21 (± 3.28) |
| Male | 11.79 (± 7.20) | 6.26 (± 3.62) | 2.15 (± 2.14) | 2.15 (± 2.45) | 1.23 (± 1.63) |
| MIH-TNI 1 (N = 19) | 7.26 (± 3. 94) | 9.00 (± 2.31) | 6.84 (± 1.83) | 5.68 (± 1.00) | 10.73 (± 0.93) |
| MIH-TNI 2 (N = 27) | 9.63 (± 4.77) | 10.44 (± 2.85) | 6.74 (± 2.19) | 6.74 (± 1.98) | 10.70 (± 0.95) |
| MIH-TNI 3 (N = 18) | 13.78 (± 6.73) | 11.61 (± 3.35) | 6.94 (± 1.96) | 8.00 (± 2.05) | 12.22 (± 2.41) |
| MIH-TNI 4 (N = 30) | 21.93 (± 9.24) | 15.17 (± 3.09) | 8.47 (± 2.67) | 10.33 (± 4.01) | 12.97 (± 3.67) |
Oral health–related quality of life in MIH patients with regard to severity of the condition
Within the MIH patient group, the mean CPQ-G8-10 score increased with the severity (Table 2, Fig. 1). In children with mild affected MIH teeth (MIH-TNI 1), a mean score of 7.26 (± 3.76) was observed increasing to 21.93 (± 21.93) in patients with severe MIH (MIH-TNI 4). Pairwise comparison showed statistically significant differences between the control group and MIH-TNI 2, MIH-TNI 3, and MIH-TNI 4 (p < 0.001, Kruskal–Wallis test). Although higher scores were already recorded in mild MIH cases (MIH-TNI1), this difference was not significant compared to the control group (p > 0.05, Kruskal–Wallis test).
Fig. 1.
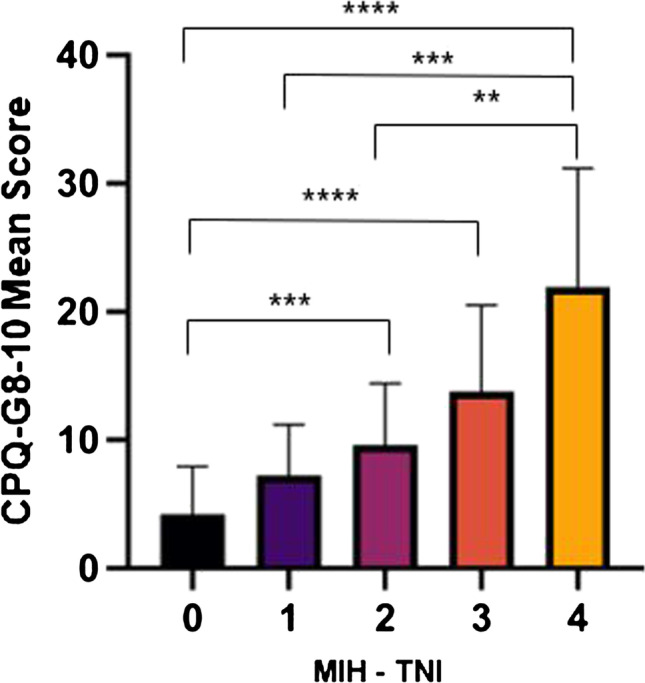
CPQ-G8-10 means in controls (MIH-TNI 0) and in MIH patients with different severities (MIH-TNI 1–4); **p < 0.01, ***p < 0.001, ****p < 0.0001
Most often reported problems
The five most often ticked items of MIH patients were “pain or sensitivity towards cold drinks and foods” (N = 72, 76.60%), “bad breath” (N = 81, 86.17%), “pain in the teeth or mouth” (N = 59, 62.77%), “needed longer time than others to eat meal because of teeth or mouth” (N = 40, 42.55%) and “been upset because of teeth or mouth” (N = 35, 37.23%). The item “pain in teeth or mouth” showed a sevenfold increase patients with MIH compared to the patients without MIH. There were also some problems which were seen only in the MIH group, but not in the control group. They were frustrated because of the teeth or mouth (25.53%) and also had a hard time attending school (11.70%)/doing homework (4.26%) or paying attention in school (5.32%). They also did not want to talk (3.19%) or be with other children (2.13%) because of the teeth or mouth and were teased (3.19%) by other children because of the teeth or mouth.
Discussion
This study compared OHRQoL in German children with and without MIH presenting in a private pediatric dental practice and also assessed the impact of severity of MIH. Although some authors have already studied the effect of MIH on OHRQoL [7, 12–14, 17–19], this is the first study focusing on this topic in Europe, using a comparable sample size of healthy and affected children and taking into account the severity of the condition by using the MIH-TNI. The study shows that children suffering from MIH have impaired OHRQoL which is decreasing with higher severity of MIH.
In the present study, the CPQ 8–10 was used to measure OHRQoL. The instrument is frequently used worldwide and has already been translated and validated in several countries. In this study, the German version was applied [16]. The CPQ 8–10 was developed for children aged 8–10 years. Therefore, the focus was placed on this age range in the study. No younger patients were included as Weerheijm et al. recommended that 8 years of age should be considered the best time for any examination for the condition as at this age, in most children, all 4 permanent molars will be erupted, as will be the majority of the incisors, while signs of MIH will still be present [4].
In this study, the presence of MIH significantly impacted OHRQoL compared to the control group (13.88 [± 8.91] vs. 4.20 [± 3.74]). Children affected with MIH showed a 3 times more impaired OHRQoL.
Furthermore, regarding severity of MIH, mean CPQ-G8-10 scores increased with increasing severity showing a more impaired OHRQoL in severe cases. In children with mild affected MIH teeth (MIH-TNI 1), a mean score of 7.26 (± 3.76) was observed increasing to 21.93 (± 21.93) in patients with severe MIH (MIH-TNI 4) which was statistically significant. However, it should be noted that although higher scores were already recorded in mild MIH cases (MIH-TNI1), this difference was not significant compared to the control group.
Similar results were observed in some other studies. Velandia et al. [18] investigated OHRQoL applying the same questionnaire in 88 children aged 7–10 years with half of them showing MIH. The mean CPQ-8–10 score in MIH patients was 17.4 compared to 4.3 in healthy patients. They also assessed the impact of severity using the severity index by Mathu Muju and Wright [20], but failed to show any statistical significance. However, it should be mentioned that this index does not take into account the possible presence of hypersensitivity of an MIH tooth which might have an influence on OHRQoL. It only focuses in the presence of post-eruptive breakdowns. Furthermore, they only included a very small number of participants (less than 10%) with severe MIH. A further study done in Mexico using a sample of 411 schoolchildren (8–10 years old) confirmed the negative impact on MIH-affected children’s OHRQoL [12]. Children with moderate/severe MIH experienced a greater impact across the four domains compared to children without MIH. Similarly, Shojaeepour et al. [21] measured OHRQoL of 129 Iranian children between 8 and 12 years of age suffering from MIH. A mean score 19.9 was observed. Unfortunately, no control group was included in this study and that no comparison to our control group can be done.
Further studies focusing on OHRQoL in MIH using other approaches for measurement point in the same direction. In another study performed to evaluate the OHRQoL in MIH children, both, the parents and children, were separately asked to fill in the questionnaire. A negative impact on OHRQoL was also found; however, it should be noted that there was poor agreement between the children and their parents [8].
It is important to understand that the QoL is not only limited to the effects caused by MIH on the oral health. It is multidimensional and affects not only psychological aspects such as emotional and social well-being, but also physical symptoms and functioning [22]. Although a negative impact of MIH was seen in all four domains, namely oral symptoms, functional limitations, emotional well-being, and social well-being, we were able to show that the highest scores were observed in the oral symptoms domain. This is also in accordance with other studies also showing the highest impacts in this domain and observing similar scores [13, 18, 21]. Children with MIH were most frequently affected with pain.
Regarding gender, it was observed that MIH-affected female patients showed more impaired OHRQoL than male patients. Other studies have shown similar results [14, 18, 21]. It can be speculated that this may be due to the fact that female patients are more worried about their self-perception and their appearance [23].
There are some strengths and limitations of this study. One of the limitations is the study design. As this was a cross-sectional study, the present design does not measure the effect prospectively but at a certain point of time in the life of the participant. Furthermore, it is noteworthy that a special setting was used in our investigation which makes a direct comparison with other studies challenging due to differences in study designs. Almost all published studies are prevalence studies being conducted at school. The current investigation was performed in a private pediatric dental clinic. Even though some patients come for routine checkups, most show up due to the presence of some uncomfortable symptoms. Therefore, the patient population is highly selective which can be seen regarding the high dmft/DMFT of the control group. However, the results of this study show that children without MIH but with a comparable and dmft/DMFT already show a better OHRQoL than MIH-affected children. Since it is already known that caries-free children have an even better OHRQoL (lower CPQ scores) compared to children with caries [16], the differences between these children and MIH children would certainly be even more notable.
Despite all the limitation, this study offers relevant perspective on OHRQoL in MIH-affected children. One of the strengths of the study is that this was the first study evaluating the impact of severity on OHRQoL in MIH patients using the MIH-TNI. The MIH-TNI is a promising index as it takes into account the two most important clinical symptoms of MIH: post-eruptive breakdown and hypersensitivity. Other indices only focus on the breakdown. However, hypersensitivity plays an important role in clinical context. As a small limitation regarding the application the index, it has to be noted for this study that no subdivision into the categories of the MIH-TNI 2 and MIH-TNI 4 (size of the post-eruptive breakdown) was undertaken.
Conclusion
Children with MIH have a poorer OHRQoL as compared to children without MIH when applying the CPQ-G8-10 questionnaire. The negative impact was seen in all the four domains, with maximum difference being observed in the oral symptoms domain. Children having severe (MIH-TNI 4) and moderate MIH (MIH-TNI 2 and MIH-TNI 3) had a poorer OHRQoL than those with mild (MIH-TNI 1) or no MIH.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
Conceived and designed the study: TJ, AR, TS, KB.
Conducted the study: TJ, SR, JR.
Analyzed the data: TJ, TS, KB.
Interpreted the data: all authors.
Wrote the manuscript: TJ, KB.
Read, revised, and agreed to be accountable for the manuscript: all authors.
Declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weerheijm KL, Jalevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35:390–1. doi: 10.1159/000047479. [DOI] [PubMed] [Google Scholar]
- 2.Schwendicke F, Elhennawy K, Reda S, Bekes K, Manton DJ, Krois J. Global burden of molar incisor hypomineralization. J Dent. 2018;68:10–18. doi: 10.1016/j.jdent.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Petrou MA, Giraki M, Bissar AR, Basner R, Wempe C, Altarabulsi MB, Schafer M, Schiffner U, Beikler T, Schulte AG, Splieth CH. Prevalence of molar-incisor-hypomineralisation among school children in four German cities. Int J Paediatr Dent. 2014;24:434–440. doi: 10.1111/ipd.12089. [DOI] [PubMed] [Google Scholar]
- 4.Weerheijm KL, Duggal M, Mejare I, Papagiannoulis L, Koch G, Martens LC, Hallonsten AL. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–113. [PubMed] [Google Scholar]
- 5.Lygidakis NA, Wong F, Jalevik B, Vierrou AM, Alaluusua S, Espelid I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an EAPD Policy Document. Eur Arch Paediatr Dent. 2010;11:75–81. doi: 10.1007/BF03262716. [DOI] [PubMed] [Google Scholar]
- 6.Jalevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002;12:24–32. [PubMed] [Google Scholar]
- 7.Dantas-Neta NB, Moura LF, Cruz PF, Moura MS, Paiva SM, Martins CC, Lima MD. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz Oral Res. 2016;30:e117. doi: 10.1590/1807-3107BOR-2016.vol30.0117. [DOI] [PubMed] [Google Scholar]
- 8.Leal SC, Oliveira TRM, Ribeiro APD. Do parents and children perceive molar-incisor hypomineralization as an oral health problem? Int J Paediatr Dent. 2017;27:372–379. doi: 10.1111/ipd.12271. [DOI] [PubMed] [Google Scholar]
- 9.Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j.2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 10.DHHS (2000) Oral Health in America: a report of the Surgeon General. Rockville, National Institute of Health
- 11.Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26:512–518. [PubMed] [Google Scholar]
- 12.Gutierrez TV, Ortega CCB, Perez NP, Perez AG. Impact of molar incisor hypomineralization on oral health-related quality of life in Mexican schoolchildren. J Clin Pediatr Dent. 2019;43:324–330. doi: 10.17796/1053-4625-43.5.4. [DOI] [PubMed] [Google Scholar]
- 13.Dias F, Gradella CMF, Ferreira MC, Oliveira LB. Molar-incisor hypomineralization: parent’s and children’s impact perceptions on the oral health-related quality of life. Eur Arch Paediatr Dent. 2020 doi: 10.1007/s40368-020-00556-4. [DOI] [PubMed] [Google Scholar]
- 14.Portella PD, Menoncin BLV, de Souza JF, de Menezes J, Fraiz FC, Assuncao L. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: a hierarchical approach. Int J Paediatr Dent. 2019;29:496–506. doi: 10.1111/ipd.12482. [DOI] [PubMed] [Google Scholar]
- 15.Bekes K, Steffen R. The Wuerzburg MIH concept: Part 1. The MIH Treatment Need Index (MIH TNI). A new index to assess and plan the treatment in patients with Molar Incisior Hypomineralization (MIH) Oralprophylaxe & Kinderzahnheilkunde. 2016;38:165–170. doi: 10.1007/s40368-017-0301-0. [DOI] [PubMed] [Google Scholar]
- 16.Bekes K, Ebel M, Omara M, Boukhobza S, Dumitrescu N, Priller J, Redzic NK, Nidetzky A, Stamm T. The German version of Child Perceptions Questionnaire for children aged 8 to 10 years (CPQ-G8-10): translation, reliability, and validity. Clin Oral Investig. 2021;25:1433–1439. doi: 10.1007/s00784-020-03451-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hasmun N, Lawson J, Vettore MV, Elcock C, Zaitoun H, Rodd H (2018) Change in oral health-related quality of life following minimally invasive aesthetic treatment for children with molar incisor hypomineralisation: a prospective study. Dent J (Basel) 6. 10.3390/dj6040061 [DOI] [PMC free article] [PubMed]
- 18.Velandia LM, Alvarez LV, Mejia LP, Rodriguez MJ. Oral health-related quality of life in Colombian children with Molar-Incisor Hypomineralization. Acta Odontol Latinoam. 2018;31:38–44. [PubMed] [Google Scholar]
- 19.Hasmun N, Vettore MV, Lawson JA, Elcock C, Zaitoun H, Rodd HD. Determinants of children’s oral health-related quality of life following aesthetic treatment of enamel opacities. J Dent. 2020;98:103372. doi: 10.1016/j.jdent.2020.103372. [DOI] [PubMed] [Google Scholar]
- 20.Mathu-Muju K, Wright JT (2006) Diagnosis and treatment of molar incisor hypomineralization. Compend Contin Educ Dent 27:604–10; quiz 611. [PubMed]
- 21.Shojaeepour S, Jalali F, Shokrizadeh M, Madvar RR, Torabi-Parizi M, Shojaeipour R. Assessing the prevalence of molar-incisor hypomineralization and its effects on oral health-related quality of life in children aged 8–12 years in the city of Kerman. Iran J Oral Health Oral Epidemiol. 2020;9:143–148. [Google Scholar]
- 22.Bowling A (2003) Current state of the art in quality of life assessment. In: Carr AJ, Higginson IJ, and Robinson PG (ed) Quality of life, BMJ Books, London,
- 23.Michel G, Bisegger C, Fuhr DC, Abel T, group K, Age and gender differences in health-related quality of life of children and adolescents in Europe: a multilevel analysis. Qual Life Res. 2009;18:1147–1157. doi: 10.1007/s11136-009-9538-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


