Abstract
Context
Parents of patients with a serious illness experience psychological distress, which impacts parents’ wellbeing and, potentially, their ability to care for their children. Parent psychological distress may be influenced by children’s symptom burden and by families’ financial difficulty.
Objectives
This study examined the associations among parent psychological distress, parent-reported patient symptoms, and financial difficulty, seeking to determine the relative association of financial difficulty and of patient symptoms to parent psychological distress.
Methods
Cross-sectional study of baseline data for 601 parents of 532 pediatric palliative care patients enrolled in a prospective cohort study conducted at seven US children’s hospitals. Data included self-reported parent psychological distress and parent report of child’s symptoms and family financial difficulty. We used ordinary least squares multiple regressions to examine the association between psychological distress and symptom score, between psychological distress and financial difficulty, and whether the degree of financial difficulty modified the relationship between psychological distress and symptom score.
Results
The majority of parents were moderately to severely distressed (52%) or severely distressed (17%) and experienced some degree of financial difficulty (65%). While children’s symptom scores and family financial difficulty together explained more of the variance in parental psychological distress than either variable alone, parental distress was associated more strongly, and to a larger degree, with financial difficulty than with symptom scores alone.
Conclusions
Parent psychological distress was associated with parent-reported patient symptoms and financial difficulty. Future work should examine these relationships longitudinally, and whether interventions to improve symptom management and ameliorate financial difficulties improve parental outcomes.
Keywords: Pediatric Palliative Care, Parents, Psychological Distress, Financial Difficulty, Patient Symptoms
Parenting a child with a serious, life-threatening illness who is receiving pediatric palliative care (PPC) takes an incredible toll on parents’ health and wellbeing, and parents often experience high levels of psychological distress, anxiety, and depression.(1–3) Poorer psychological health over time may lead to lower parental quality of life and increased health care use(4–6), morbidity, and mortality.(7, 8) Poorer parent psychological health can impact other family members(5), and impaired family functioning can in turn negatively impact parents’ psychological outcomes.(9, 10)
Prior research highlights two factors, among others, that influence parental psychological health: children’s symptom burden and families’ financial challenges. Children’s symptom burden has been found to have short- and long-term effects on parents’ psychological outcomes.(4, 11–13) Financial difficulty is also often reported by families of children with serious illness, including work disruptions, income loss, and household material hardships (HMH)(14, 15), adding further challenges to caring for a seriously ill child.(9, 10, 16)
Little empirical evidence exists to quantify the relationship between parent psychological health, child symptomatology, and family financial difficulties. Symptom burden in children with cancer, as perceived by parents, was correlated with parents’ depressive symptoms, but potential associations between financial difficulty and parents’ mental health outcomes were not assessed.(13) Another study found that, among children with cancer, child health-related quality of life was significantly lower in low-income families compared to higher-income families, but did not examine parental outcomes.(17)
We, therefore, examined the relationships among parent psychological distress (along with anxiety and depression), parent-reported child symptoms, and family financial difficulty among parents of children receiving PPC. We hypothesized that higher distress would be associated with higher levels of parent-reported patient symptoms and family financial difficulty. We also sought to determine the relative association of financial difficulty and of parent-reported patient symptoms to parent distress.
METHODS
Human Subjects Protections
All study participants provided written informed consent. Institutional Review Boards approved the conduct of this study in all hospitals involved.
Study Design and Participants
We performed a cross-sectional analysis of baseline data from an on-going prospective cohort study (Pediatric Palliative Care Research Network SHARE Study) conducted at seven children’s hospitals (Children’s Hospital of Philadelphia, Boston Children’s/Dana-Farber Cancer Institute, Seattle Children’s, Children’s Hospital and Clinics of Minnesota, Akron Children’s Hospital, Children’s of Alabama, and Texas Children’s). Patients under 30 years of age receiving PPC services were eligible. Eligible participants were primary caregivers responsible for the patient (referred to as ‘parent’ in this paper, although may include biologic or adoptive/foster parents, as well as grandparents), at least 18 years old or a minor permitted by state law to consent for participation, and able to speak and understand English or Spanish.
Enrollment occurred April 2017 through December 2020. Monthly calls with SHARE site coordinators ensured consistency in participant recruitment, data collection, and study procedures. When applicable, both mothers and fathers were approached for participation to increase the traditionally low representation of fathers in PPC studies.(18)
Data Collection
Parents completed instruments in a clinical care setting or at home, with data recorded via paper- or internet-based forms (Research Electronic Data Capture, REDCap).(19, 20)
Background information:
Parents reported demographic information for themselves and their child, including age, child’s health insurance status, parents’ educational attainment (dichotomized into some college or more than some college), parents’ employment status, and household income (reported in 25 discrete categories, ranging from ≤ $10,000 to >$150,000). Household income was adjusted for household size by dividing by the square root of the number of persons in the household and standardizing at a 3-person size household.(21) Complex Chronic Conditions (CCC’s) were determined by matching patients to their data in the Pediatric Hospital Information System (PHIS; Children’s Hospital Association, Lenexa, KS) administrative database. Diagnoses recorded as ICD-10-CM codes were used to identify whether participating patients had any of 12 different and not mutually exclusive CCC categories.(22, 23)
Outcome Variables
Parent psychological distress (primary):
Parents completed the Kessler-6 (K6), a 6-item psychological distress scale screening tool that has been validated among parents of ill children.(24, 25) Total psychological distress score (range, 0–24) of 5–12 indicates moderate distress, and scores of 13 or greater indicate serious distress.(26, 27)
Parent anxiety and depression (secondary):
Parents completed the PROMIS® Adult Profile version 2.0, a validated 29-item self-reported measure including 4 items for depression and 4 items for anxiety.(28–30) Items were summed and standardized to yield t-scores for anxiety and depression using the “PROMIS Pediatric and Parent Proxy Profile Instruments” manual and scoring tables (“PROMIS Parent Proxy – 25 v2.0”).(31)
Independent Variables
Parent-reported assessment of child symptoms:
Parents completed previously adapted versions of the Memorial Symptom Assessment Scale (MSAS)(32–35), including the PQ-MSAS Proxy for parents of children 0–2 years old (20 symptoms) and the PQ-MSAS Proxy for parents of children 2 years and older (28 symptoms).(36) These versions of PQ-MSAS assessed the frequency (0, never; 1, almost never; 2, sometimes; 3, a lot; 4, almost always) and severity (0, none; 1, slight; 2, moderate; 3, severe; 4, very severe) of physical and psychological symptoms across the study age range. Wording changes were made to shift the respondent to be the parent as opposed to the patient (e.g. changing “During the past week did you. …” to “During the past week did your child/teen…”). Additional response options (“Not Applicable” and “I Prefer Not to Answer”) were added to account for cases where the item could be difficult for parents to answer due to a child’s age or cognitive ability and to make the items consistent with other study instruments. A child’s total symptom score was the average of all symptom scores for that child, transformed into a 0 to 100 range.(23, 36)
Family financial difficulty:
Based on prior research, parents reported the extent to which they experienced difficulty with paying bills over the prior 6 months: no difficulty at all (score 0), a little (1), some (2), quite a bit (3), and a great deal (4).(37) Adapting a measure from a previous study(15), parents were also asked whether they had experienced specific types or degrees of household material hardship (HMH), defined as unmet basic needs, including having to live with others (scored 0, no; 1, yes), inability to pay rent or mortgage on time (0, 1), receiving shut-off notices from utility companies (0, 1), having utilities turned off (0, 1), worrying that food would run out (scored 0, never true; 1, sometimes true; 2, often true), and running out of food (0, 1, 2).(15) A composite HMH score was created by summing the values for these 6 questions (range 0 to 8).
Analyses
Counts, proportions, means, and standard deviations were used to report parent and child demographic information and clinical outcomes. For household income only, we reported median income categories to ease comparison to national figures (typically reported as medians). T-tests (two-tailed), chi-squares, and ordinary least squares regressions were used to detect differences between demographic characteristics and psychological outcomes. Correlations were run between parent distress, anxiety, and depression.
For the main analysis, ordinary least squares multiple regression models tested the association of parental psychological distress to parent-reported child’s total symptom score and family financial difficulty, first in univariable and then multivariable models (adjusting for children’s age, and parents’ age, sex, race, educational attainment). All models accounted for family-level clustering in cases where two parents of the same child participated. For improved interpretability, parental psychological distress and child symptom scores were standardized. Due to the low proportion of missing data, analysis handled missing data with listwise deletion. Likelihood ratio testing was used to compare models. All data management, analysis, and figure creation were performed using Stata 16.1 (Stata Corp; College Station, TX).
RESULTS
Parent and patient characteristics
Of 756 eligible participants, 601 (79.5%) parents of 532 patients agreed to participate and completed baseline instruments by July 2020.
The 601 parents had a mean age of 37.9 (SD 9.5) years, and 79.2% were female (n = 476), 76.5% White (n=459), and 86.5% non-Hispanic (n=520) (Table 1). Most (76.2%) were partnered or married (n=458), and 84.9% (n=510) completed at least some college, technical, or trade school. Over 35% (n=213) were employed full-time, and 15.1% (n=91) were on leave for the child’s illness.
Table 1.
Parent psychological distress scores (Kessler-6) and family financial difficulty scores by parent characteristics
| Kessler-6 Score | Financial Difficulty | |||||
|---|---|---|---|---|---|---|
| Parents’ Characteristics (n = 601) | No. (%) | Mean (SD) | P-value | M (SD) | P-value | |
| Parent type | Mother | 476 (79.2) | 7.7 (5.1) | 0.756 | 1.6 (1.4) | 0.229 |
| Father | 125 (20.8) | 7.5 (5.0) | 1.4 (1.4) | |||
| Age | Years, Mean (standard deviation; SD) | 37.9 (9.5) | 0.169b | 0.119b | ||
| Missing | 1 | |||||
| Race | White | 459 (76.5) | 7.7 (5.0) | 1.5 (1.3) | ||
| Black | 52 (8.7) | 8.0 (5.6) | 2.0 (1.6) | |||
| Asian | 29 (4.8) | 7.3 (5.7) | 0.934 | 1.3 (1.4) | 0.024 | |
| American Indian | 21 (3.5) | 8.3 (5.7) | 2.2 (1.1) | |||
| Other | 26 (4.3) | 8.1 (5.9) | 1.7 (1.6) | |||
| Prefer not to answer/missinga | 14 (2.3) | 5.0 (0.0) | 1.4 (1.6) | |||
| Ethnicity | Non-Hispanic | 520 (86.5) | 7.6 (5.1) | 1.5 (1.3) | ||
| Hispanic | 71 (11.8) | 8.1 (5.5) | 0.718 | 1.9 (1.5) | 0.052 | |
| Missinga | 10 (1.7) | 8.3 (4.7) | 1.3 (1.3) | |||
| Highest Education Level | ||||||
| Completed | High school/General Educational Diploma | 88 (14.6) | 7.5 (5.4) | 2.3 (1.4) | ||
| Trade/technical/vocational/some college | 234 (38.9) | 7.6 (5.3) | 0.842 | 1.6 (1.3) | <0.001 | |
| College/graduate school | 276 (45.9) | 7.8 (4.8) | 1.2 (1.2) | |||
| Preferred not to answera | 3 (0.5) | 10.0 (6.6) | 2.5 (2.1) | |||
| Relationship Status | Married/partnered | 458 (76.2) | 7.6 (5.1) | 1.3 (1.3) | ||
| Separated/divorced/widowed | 53 (8.8) | 6.9 (4.5) | 0.122 | 2.3 (1.2) | <0.001 | |
| Single | 76 (12.7) | 8.8 (5.6) | 2.4 (1.3) | |||
| Prefer not to answer/other/missinga | 14 (2.3) | 6.7 (5.5) | 1.7 (1.4) | |||
| Number of Other Children | 0 | 119 (22.4) | 7.6 (5.3) | 1.2 (1.3) | ||
| 1 to 4 | 379 (71.2) | 7.5 (5.0) | 0.582 | 1.6 (1.4) | <0.001 | |
| 5 or more | 32 (6.0) | 8.3 (5.8) | 2.5 (1.5) | |||
| Missinga | 2 (0.4) | 11.5 (3.5) | 1.0 (1.4) | |||
| Employment Status | Full time | 213 (35.4) | 7.5 (5.2) | 1.3 (1.2) | ||
| Part time | 60 (10.0) | 7.2 (4.4) | 1.5 (1.4) | |||
| Not employed/Looking for employment | 7 (1.2) | 7.9 (4.9) | 1.6 (1.5) | |||
| Not employed/Not looking for employment | 111 (18.5) | 7.4 (5.1) | 0.405 | 1.9 (1.4) | <0.001 | |
| Homemaker | 113 (18.8) | 7.6 (5.0) | 1.4 (1.3) | |||
| On leave for child’s illness | 91 (15.1) | 8.8 (5.7) | 1.8 (1.5) | |||
| Preferred not to answera | 6 (1.0) | 6.7 (2.3) | 2.0 (1.2) | |||
For statistical testing purposes, the “prefer not to answer (etc.)” cells were omitted.
These statistical test regarding the association of increasing age with the scores.
The 532 children were an average of 7.1 (SD 7.0) years old, were 53.2% male (n=283), had an average of 5.5 (SD 2.1) CCCs, and over 98% had at least one CCC designation (Table 2). No more than 5% of any variable was missing.
Table 2.
Parent psychological distress scores (Kessler-6) and family financial difficulty scores by patient characteristics
| Kessler-6 Score | Financial Difficulty | |||||
|---|---|---|---|---|---|---|
| Patients’ Characteristics (n = 532) | No. (%) | Mean (SD) | P-value | M (SD) | P-value | |
| Age | <1 month | 21 (4.0) | 6.4 (3.4) | 1.0 (1.1) | ||
| 1–11 months | 127 (23.9) | 8.3 (5.2) | 1.7 (1.4) | |||
| 1–9 years | 194 (36.5) | 8.0 (5.3) | 0.109 | 1.6 (1.4) | 0.099 | |
| 10–17 years | 156 (29.3) | 7.0 (4.7) | 1.5 (1.3) | |||
| 18–28 years | 34 (6.4) | 7.7 (5.5) | 1.7 (1.4) | |||
| Sex | Female | 247 (46.6) | 7.2 (4.7) | 1.3 (1.3) | ||
| Male | 283 (53.2) | 7.9 (5.5) | 0.129 | 1.8 (1.4) | <0.001 | |
| Prefer not to answera | 1 (0.2) | 2.0 (0.0) | 2.0 (0.0) | |||
| Race | White | 380 (71.6) | 7.5 (4.9) | 1.5 (1.3) | ||
| Black | 67 (12.6) | 7.7 (5.4) | 1.5 (1.4) | |||
| Asian | 25 (4.7) | 7.8 (5.5) | 0.995 | 2.0 (1.6) | 0.016 | |
| American Indian | 17 (3.2) | 7.9 (6.1) | 2.3 (1.0) | |||
| Other | 35 (6.6) | 7.5 (5.6) | 1.7 (1.5) | |||
| Prefer not to answer/missinga | 8 (1.3) | 8.0 (8.4) | 1.7 (1.9) | |||
| Ethnicity | Non-Hispanic | 445 (83.7) | 8.3 (5.4) | 1.5 (1.4) | ||
| Hispanic | 77 (14.5) | 7.6 (5.0) | 0.447 | 1.9 (1.4) | 0.036 | |
| Prefer not to answer/missinga | 10 (1.9) | 5.0 (5.0) | 1.4 (1.0) | |||
| Complex Chronic Condition | Cardiovascular | 322 (60.5) | 7.6 (5.1) | 0.470 | 1.6 (1.4) | 0.358 |
| Respiratory | 215 (40.4) | 7.7 (5.2) | 0.978 | 1.7 (1.3) | 0.035 | |
| Congenital | 227 (42.7) | 7.8 (5.2) | 0.603 | 1.5 (1.4) | 0.834 | |
| Neuromuscular | 306 (57.5) | 7.7 (5.2) | 0.807 | 1.6 (1.4) | 0.250 | |
| Metabolic | 267 (50.2) | 8.1 (5.2) | 0.038 | 1.6 (1.3) | 0.236 | |
| Malignancy | 152 (28.6) | 7.8 (4.9) | 0.708 | 1.5 (1.3) | 0.827 | |
| Renal | 220 (41.4) | 7.8 (5.1) | 0.623 | 1.6 (1.4) | 0.089 | |
| Gastrointestinal | 376 (70.7) | 7.8 (5.1) | 0.292 | 1.6 (1.4) | 0.032 | |
| Hematologic | 180 (33.8) | 7.9 (5.0) | 0.597 | 1.6 (1.3) | 0.171 | |
| Neonatal | 124 (23.3) | 7.9 (5.0) | 0.584 | 1.9 (1.3) | <0.001 | |
| Technology Dependent | 459 (86.3) | 7.7 (5.1) | 0.404 | 1.6 (1.4) | <0.001 | |
| Transplant | 72 (13.5) | 8.1 (5.2) | 0.443 | 1.4 (1.3) | 0.567 | |
For statistical testing purposes, the “prefer not to answer (etc.)” cells were omitted.
Parent psychological distress
Kessler-6 scores (Figure 1) had a mean of 7.7 (SD 5.1). Approximately 17% of participants had scores at or above 13, indicating severe psychological distress, and 69% had a score of 5 or above, indicating moderate to severe distress. Kessler scores did not vary significantly by parent age, sex, educational attainment, race, or ethnicity (all p values >0.15), but were higher when income was low and financial difficulty was more severe (both p values <0.05). Psychological distress was highest among those experiencing “a great deal” of financial difficulty, decreased as financial difficulty became less severe, and was lowest among those experiencing “no difficulty at all.”
Figure 1.
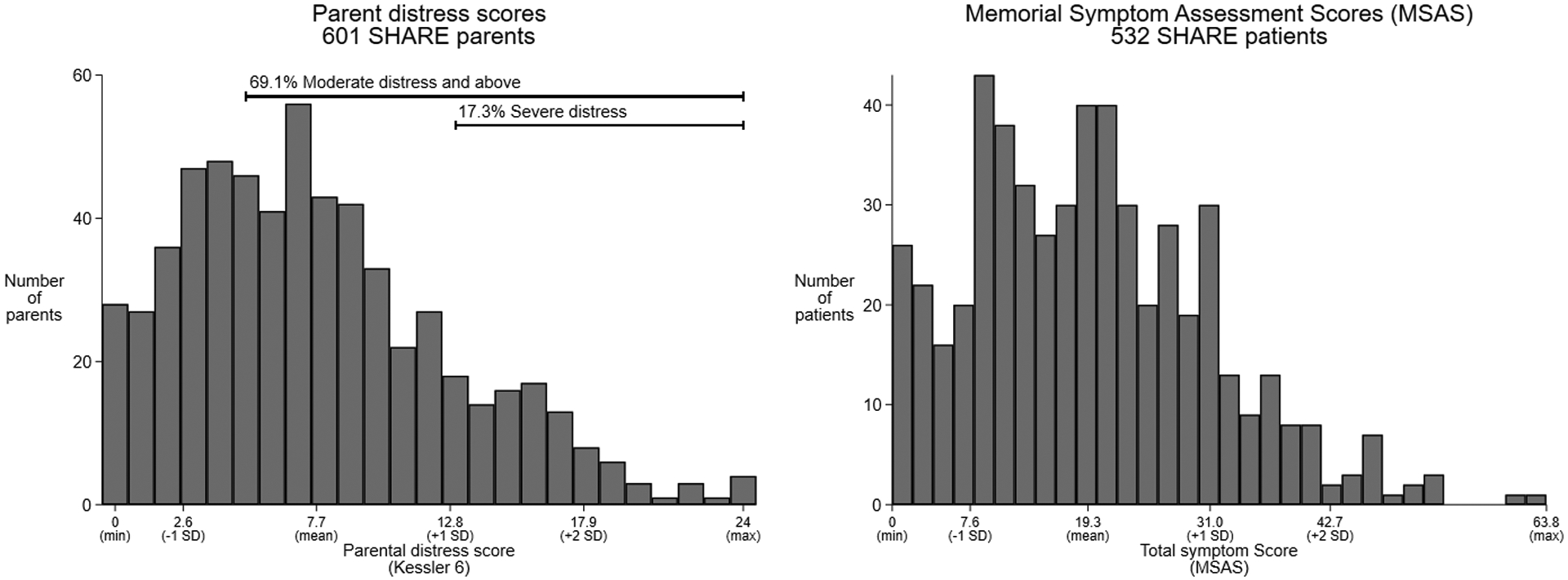
Distribution of parent psychological distress scores and parent-reported child total symptom scores
Relationship of parent anxiety and depression to psychological distress
Parents had a mean standardized PROMIS anxiety score of 59.9 (SD 10.1; minimum 40.3; maximum 81.6) and a mean standardized PROMIS depression score of 54.3 (SD 9.7; minimum 41; maximum 79.4). Anxiety and depression scores were highly correlated (r= 0.71; p<0.001; supplemental file). Psychological distress scores were significantly correlated with anxiety (r= 0.57; p<0.001) and depression scores (r=0.64; p<0.001).
Parent-reported child total symptom scores
Of 20 possible symptoms, parents reported their children having a mean of 6.6 (SD 3.4) symptoms, with 96.8% having at least one symptom, including pain, lack of energy, irritability, drowsiness, and shortness of breath. Total symptom scores ranged from 0 to 63.8 (mean 19.3; SD 11.7). Mean symptom scores and symptom counts did not differ by children’s sex, race, or ethnicity (all p values>0.05); however, both score and count increased as children’s age at baseline increased (all p values<0.001).
Household income, financial difficulty, and material hardship
The median reported unadjusted household income category was $65,001 to $70,000 per year (similar to the US national median(38)) and ranged from ≤$10,000 to ≥$150,000. Nearly 13.2% of the sample (n=79) reported household incomes below $20,000, which is below the $21,960 national poverty line for a family of three. The median household income adjusted for household size was $57,500 (IQR: $29,047 to $90,933), which is slightly lower than national data.(39)
At baseline, 31.0% (n=186) of parents reported no financial difficulty, while 17.3% (n=104) reported a little, 23.8% (n=143) some, 12.3% (n=74) quite a bit, and 10.8% (n=65) a great deal of difficulty; 4.8% (n=29) did not report. Financial difficulty varied significantly by parent race (Black and American Indian parents reported greater difficulty, p=0.02), ethnicity (Hispanic parents reported greater difficulty, p=0.01), educational attainment (participants with higher levels of education reported less difficulty, p<0.001), employment status (participants who were unemployed or on leave for their child’s medical condition reported greater difficulty, p=0.01), and household income (participants with larger household incomes reported less difficulty, p<0.001).
Parents also reported experiencing HMH. Overall, composite HMH scores ranged from 0 to 8 (mean 1.03; SD 1.70), and the percent of parents who reported specific HMH categories ranged from 4.7% (“Home was not heated/cooled”) to 22.4% (“Worried that food would run out”) (Table 3). Most (n=176) parents who reported not experiencing any financial difficulty did not report any form of HMH. Of the parents reporting some degree of financial difficulty and some form of HMH (n=368), 33% reported difficulty paying rent or mortgage on time over the past 6 months, and 5.6% and 18% reported that food often ran out or sometimes ran out, respectively, over the past 6 months (Figure 2, bottom panel). In addition, 155 parents who answered “no” to all of the HMH questions experienced at least some financial difficulty.
Table 3.
Parent psychological distress scores (Kessler-6) across levels of household income, financial difficulty, and household material hardship (HMH) categories
| Kessler-6 Score | ||||
|---|---|---|---|---|
| N (%) | Mean (SD) | P-value | ||
| Household income (unadjusted) | ≤ $10,000 | 34 (5.7 %) | 7.9 (6.3) | |
| $10,001 to $20,000 | 45 (7.5%) | 7.6 (6.2) | ||
| $20,001 to $40,000 | 82 (13.6%) | 8.4 (4.8) | ||
| $40,001 to $70,000 | 137 (22.8%) | 8.5 (4.9) | 0.042 | |
| $70,001 to $100,000 | 93 (15.5%) | 7.3 (5.5) | ||
| $100,001 to $150,000 | 91 (15.1%) | 7.4 (4.4) | ||
| >$150,000 | 60 (10%) | 6.9 (4.7) | ||
| Preferred not to answer/missingb | 59 (9.8 %) | 6.4 (4.5) | ||
| Household income (adjusted for household size of 3 personsa) | ≤ $10,000 | 24 (4.0%) | 8.5 (6.0) | |
| $10,001 to $17,500 | 49 (8.2%) | 6.9 (6.0) | ||
| $17,501 to $36,793 | 87 (14.5%) | 8.4 (5.3) | ||
| $36,794 to $67,500 | 156 (26.0%) | 8.1 (4.9) | 0.202 | |
| $67,501 to $90,033 | 89 (14.8%) | 7.6 (5.3) | ||
| $90,034 to $150,000 | 105 (17.5%) | 7.6 (4.7) | ||
| >$150,000 | 27 (4.9%) | 6.6 (5.0) | ||
| Preferred not to answer/missingb | 64 (10.7%) | 6.6 (4.6) | ||
| Financial Difficulty | A great deal of difficulty | 65 (10.8%) | 9.9 (6.1) | |
| Quite a bit of difficulty | 74 (12.3%) | 8.7 (5.4) | ||
| Some difficulty | 143 (23.8%) | 8.6 (4.5) | <0.001 | |
| A little difficulty | 104 (17.3%) | 7.8 (5.1) | ||
| No difficulty at all | 186 (31.0%) | 5.8 (4.2) | ||
| Preferred not to answer/missingb | 29 (4.8%) | 7.4 (5.7) | ||
| HMH in the last 6 months | Lived with other people | 61 (10.2 %) | 9.4 (5.9) | 0.006 |
| Rent wasn’t paid on time | 133 (22.2%) | 9.2 (5.6) | <0.001 | |
| Threatened to shut off utilities | 118 (19.7%) | 8.9 (5.4) | 0.004 | |
| Home was not heated/cooled | 28 (4.7%) | 12.6 (6.3) | <0.001 | |
| Possibility of food running out | 134 (22.4%) | 9.1 (5.3) | 0.002 | |
| Weren’t able to purchase food | 103 (17.2%) | 9.3 (5.6) | 0.001 | |
| HMH Composite Scorec | 0 | 351 (60.9%) | 6.9 (4.9) | |
| 1 | 76 (13.2%) | 8.6 (4.6) | ||
| 2 | 48 (8.3%) | 7.5 (4.4) | ||
| 3 | 44 (7.6%) | 8.0 (4.9) | ||
| 4 | 22 (3.8%) | 7.3 (4.5) | <0.001 | |
| 5 | 18 (3.1%) | 10.1 (6.3) | ||
| 6 | 7 (1.2%) | 15.4 (5.1) | ||
| 7 | 7 (1.2%) | 13.4 (3.7) | ||
| 8 | 3 (0.5%) | 9.7 (8.5) | ||
Adjustment for household size was calculated for each participating family by taking the midpoint value of their income category range and dividing by the square root of the number of persons in the household.
For statistical testing purposes, the “prefer not to answer/missing” cells were omitted.
HMH Composite Scores were comprised of the sum of HMH questions regarding financial difficulty covering housing, utility, and food costs, where higher numbers indicate greater number and severity of difficulties.
Figure 2.
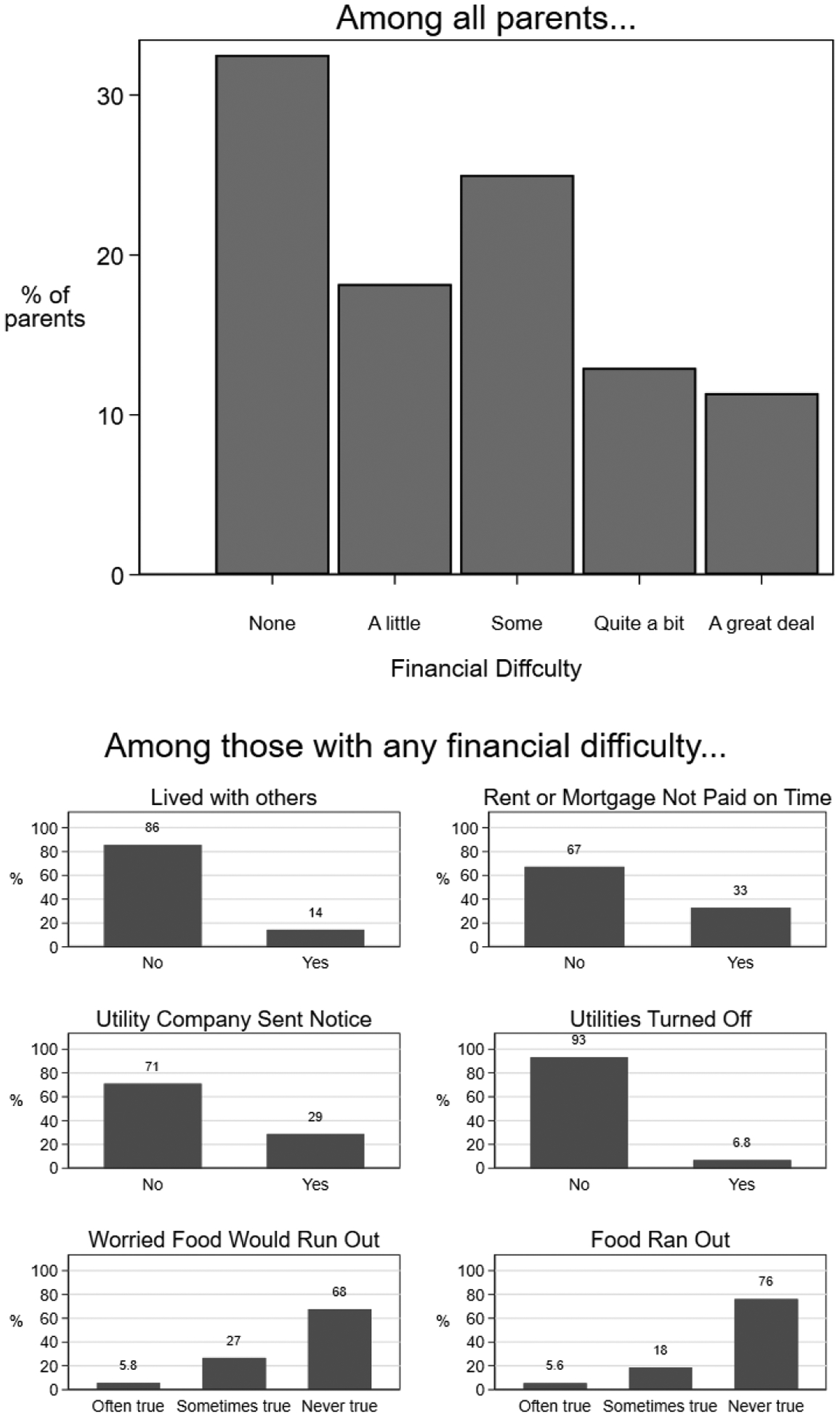
Presence of financial difficulty and characterization of household material hardship
Parental psychological distress levels were significantly associated with unadjusted household income, financial difficulty, and HMH (Table 3) (all p values<0.05). Of note, financial difficulty and composite HMH scores were significantly correlated (r=0.67, p<0.01; supplemental file).
Parent psychological distress, parent-reported patient symptoms, and family financial difficulty
Because psychological distress, anxiety, and depression were highly correlated, the main analysis used distress as the main outcome of interest. Further, given the high correlation between the financial difficulty single item and the composite HMH score, the main analysis used financial difficulty as one of the two main predictors of interest, with the child’s symptom score being the other. Lastly, these two predictors were slightly but not statistically significantly associated (a one-point rise in the financial difficulty score was associated with a 0.06 increase (95% CI: −0.01, 0.13) in the standardized child symptom score, which is to say an increase equal to 6% of 1 standard deviation of this score among these children, p=0.12).
In separate univariable models, parent psychological distress was strongly associated with child symptom score (a 1-SD increase in symptom score was associated with 0.26-SD (95% CI: 0.18, 0.34) increase in the Kessler score, p<0.001) and with financial difficulty (a 1-SD increase in financial difficulty score was associated with a 0.27-SD (95% CI: 0.19, 0.35) increase in the Kessler score, p<0.001). Of these two models, the one with financial difficulty explained more of the variance in parent psychological distress (R2 = 0.074) than did the model with child symptom score (R2 = 0.068).
In a single multivariable model, with no adjustment for other parent or child characteristics, parent psychological distress was strongly associated with both child symptom score (0.24-SD change, 95% CI: 0.16–0.32, p<0.001) and with financial difficulty (0.25-SD change, 95% CI: 0.17–0.33, p<0.001), and this model explained more variance in parent distress (R2 = 0.131) than did either of the univariable models to a statistically significant degree (likelihood ratio test comparing full model to both univariable models, p<0.001).
In multivariable models with adjustment for parent race, age, sex, educational level, and the child’s age, variation in parent psychological distress was again explained to a higher degree by the combination of child symptom score and financial difficulty (R2 = 0.164) than by models with either of these factors separately (R2 = 0.094 for symptom score model, R2 = 0.096 for financial difficulty model).
These results can be visualized graphically, modeling the financial difficulty score as distinct levels rather than as a continuous variable (Figure 3). This figure depicts that parents of children with the lowest symptom scores and in families with no financial difficulty are predicted to have a level of psychological distress that is 1.6 SD less than parents of children with the highest symptom scores and in families with a great deal of financial difficulty.
Figure 3.
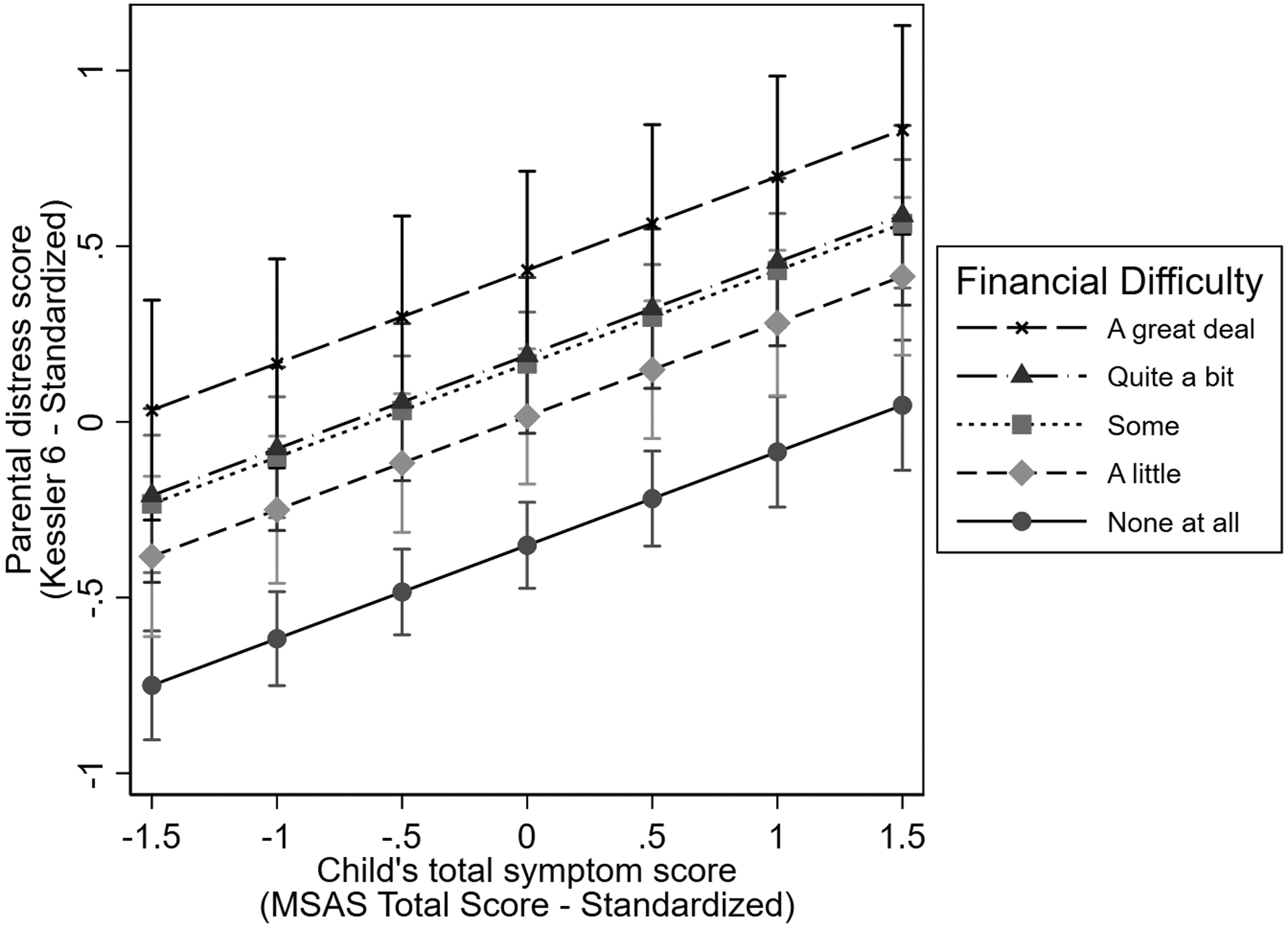
Relationship between the parent’s level of distress and the child total symptom score varies by the family’s level of financial difficulty
Note: In this figure, the vertical axis plots the score on the Kessler-6, with 0 representing the mean score and +1 and −1 representing a standard deviation (SD) in the score above and below the mean; the horizontal axis plots the child’s total symptom score in a similar manner; and each of the parallel lines indicate the scores for parents experiencing different degrees of financial difficulty. The fact that these lines slope upward indicates that higher total symptom scores are associated with higher levels of parental psychological distress; and the fact that these lines are separated vertically indicates that increasing levels of financial distress are associated with increasing levels of psychological distress. Combined, the parent of a child with the lowest level of symptom score and in a family with no financial difficulty is predicted to have a level of psychological distress that is 1.6 SD less than a parent of a child with the highest level of symptom score and in a family with a great deal of financial difficulty.
Additional analyses
The supplemental file contains analyses using the PROMIS anxiety or depression score as the outcomes of interest yielded the same pattern of findings, whereby child symptom score and financial difficulty were both independently associated with parent psychological distress to statistically significant degrees, and financial difficulty was associated to a larger degree.
We also detail an analysis where the single-item financial difficulty score was replaced by the HMH composite score and found the same pattern of findings.
DISCUSSION
In this cohort of 601 parents of children with serious illnesses receiving PPC, 69% of parents were moderately to severely distressed and 17% were severely distressed. Parents reported that their children experienced an average of 6.6 out of 20 symptoms, with total symptom scores ranging from 0 to 63.8 out of 100. Additionally, over 65% of parents reported experiencing “a little” to “a great deal” of financial difficulty. While parent-reported children’s symptom scores and family financial difficulty were associated with, and together accounted for greater variance in, parental psychological distress, parental distress was associated more strongly, and to a larger degree, with financial difficulty than with symptom scores alone.
Our findings are consistent with previous findings and provide further evidence for the impact of parent-reported children’s symptoms and families’ financial difficulty on parental mental health. Other studies observed the effects of children’s perceived disease burden(4, 11–13) and financial difficulty(9, 10, 40, 41) on parental mental health. Few studies, however, have explored the impact of clinical and socioeconomic factors together on parents.(40, 42) Our study is the first, to our knowledge, to compare the relative contributions of parent-reported children’s symptom burden and family financial difficulty levels to parental psychological distress in a sample of parents of children receiving PPC services across the full range of patient ages and underlying conditions.
Three main findings warrant further exploration. First, clinically-important (moderate to severe) levels of psychological distress were reported in nearly 70% of our parent sample, exceeding estimates from previous studies reporting psychological distress in 40% to 66% of parent participants.(6, 9, 10, 40, 42) For parents, addressing these high levels of psychological distress could reduce physical and mental health care use(10), improve quality of life and wellbeing(6), and potentially reduce morbidity and mortality from stress-associated health conditions.(7, 8) For children, improving parents’ distress may improve child psychosocial functioning and reduce non-routine health care use.(10) Improved psychological distress may also improve caregivers’ cognitive functioning(43, 44), which could benefit parents’ ability to care for their child. Parents’ mental health symptoms have also been found to affect siblings’ mental health outcomes.(45) Finally, improving parent psychological health may benefit the entire family by mitigating the impact of children’s illnesses on families(10, 46) and improving family functioning.(10)
Second, for parents in our study, psychological distress was associated more strongly, and to a larger degree, with financial difficulty than with parent-reported child symptom scores. The few studies examining contributions of children’s clinical outcomes and families’ financial factors on parents’ mental health did not compare the relative associations of these factors(42), relied on recall of these factors among bereaved parents(40), used broad measures of children’s quality of life(40), or focused on only one disease group.(40, 42) Our findings are generalizable to the broader, heterogeneous population of children receiving PPC services since our participants represent various ages, underlying conditions, and disease onset and pace of progression, all of which may result in different care experiences and illness trajectories, in turn affecting parents’ employment and family financial and material resources differently.(47–50)
Third, our findings have important implications for clinical practice. Future intervention-based research is needed to better understand how to screen for and mitigate financial difficulty and material hardships for families of children with medically-complex serious illnesses, as well as for families from marginalized and underserved communities who may be at greater risk for socioeconomic disadvantage and, thus, psychological distress.(51) Interventions may provide support focused on material conditions (e.g., financial counseling, direct income supplementation, charitable funds, food and housing assistance programs, child care supplements)(15, 47, 48), psychological response to financial hardship (e.g., counseling to cope with stress)(47, 48, 52), and coping behaviors related to financial hardship (e.g., reduced spending, finding lower cost medications and medical supplies).(52, 53) Greater involvement of PPC providers, particularly psychosocial providers, in the systematic screening for and facilitation of support for these families is therefore imperative.(15)
Our study is among the few investigating the impact of financial difficulty and HMH on child and family outcomes in PPC(15, 17, 54), particularly among a large and diverse clinical, geographic, and socioeconomic cohort. Additionally, our study used a single-item subjective measure of financial difficulty that may provide a comprehensive view of financial challenges across income levels. Several families in our study reported some financial distress without reporting any HMH, suggesting that the perception of financial distress may extend beyond these specific hardships. We propose that the measure of perceived financial difficulty be used to screen for potential financial challenges, and further assessment could be conducted into specific areas of need (e.g., HMH or other areas like difficulty paying medical bills).
Our study has several limitations. First, we cannot evaluate causality because of the cross-sectional study design. Consequently, we do not know if a child’s illness caused financial difficulty (e.g., time taken off work to care for the child; employment loss or high medical bills due to the child’s illness), or if the financial difficulty was present, independent of the child’s illness. Along the same line of thought, we don’t know if a child’s symptoms caused the parent’s psychological distress, the parent was distressed before the child had burdensome symptoms, or if a parent who is more distressed is more likely to perceive their child’s symptoms to be more severe/burdensome than a parent who is less distressed at baseline. Second, our study sample, while diverse, does not fully match national race and ethnicity characteristics, which could limit the generalizability of our findings. Third, our study measures may have excluded other factors potentially associated with psychological distress (e.g., pre-existing mental health conditions, perceived social support, access to mental health services).
Conclusion
We found that parent psychological distress was associated with parent-reported children’s symptoms and families’ financial difficulty in a large cohort of parents of children receiving PPC. Future longitudinal investigations should evaluate the temporal relationships between parental distress, financial difficulty, and children’s illness. Lastly, future intervention-based research should explore whether, and which, financial interventions can decrease psychological distress in parents of seriously ill children.
Supplementary Material
Key Message:
In the setting of pediatric palliative care, higher parent psychological distress was associated with family financial difficulty and patient symptom burden. Future work should explore the longitudinal relationship between these variables and whether greater financial support and better symptom management reduces parent psychological distress and improves patient and family outcomes.
Acknowledgements:
We thank all the parents who participated in this study. We also thank all members of the Pediatric Palliative Care Research Network (PPCRN) SHARE Project team, including Kris Catrine (site investigator), Karen Crew (project coordinator), Hannah Katkoff and Heather Griffis (database design and management), and Rui Xiao (statistical analysis), and Tatiana Arevalo-Soriano, Leah Beight, Madeline Bilodeau, Jennifer Chapman, Porag Jeet Das, Gabby Helton, Rachel Jenkins, Ali Kolste, Deborah Maglionico, Isaac Martinez, Amanda Mercer, Ashley Morris, Shimei Nelapati, Rachel Porth, Nicole Etsekson Sherr, Kelly Shipman, and Namrata Walia (study site research coordinators).
Funding/Support:
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR016223; and under Award Number F32NR019517. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the Sponsor:
The funding organization had no role in the design of the study beyond the critique offered by the peer-review process; and had no role in the conduct of the study, including the collection, analysis, and preparation of the data or the drafting, editing, review, or approval of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of NINR.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: The authors declare that they have no relevant financial relationships to disclose.
Data Usage: De-identified data from this study can be obtained directly from the study team by qualified investigators with specific research questions who complete the necessary application and data usage agreement.
REFERENCES
- 1.Boyden JY, Hill DL, Carroll KW, et al. The association of perceived social support with anxiety over time in parents of children with serious illnesses. J Palliat Med 2020;23:529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muscara F, McCarthy MC, Woolf C, et al. Early psychological reactions in parents of children with a life threatening illness within a pediatric hospital setting. Eur Psychiatry 2015;30:555–561. [DOI] [PubMed] [Google Scholar]
- 3.Siden H, Steele R. Charting the Territory: Children and families living with progressive life-threatening conditions. Paediatr Child Health 2015;20:139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boman K, Lindahl A, Bjork O. Disease-related distress in parents of children with cancer at various stages after the time of diagnosis. Acta Oncol 2003;42:137–146. [DOI] [PubMed] [Google Scholar]
- 5.Carnevale FA, Alexander E, Davis M, Rennick J, Troini R. Daily living with distress and enrichment: The moral experience of families with ventilator-assisted children at home. Pediatr 2006;117:e48. [DOI] [PubMed] [Google Scholar]
- 6.Collins A, Burchell J, Remedios C, Thomas K. Describing the psychosocial profile and unmet support needs of parents caring for a child with a life-limiting condition: A cross-sectional study of caregiver-reported outcomes. Palliat Med 2020;34:358–366. [DOI] [PubMed] [Google Scholar]
- 7.Cohen E, Horvath-Puho E, Ray JG, et al. Association between the birth of an infant with major congenital anomalies and subsequent risk of mortality in their mothers. JAMA 2016;316:2515–2524. [DOI] [PubMed] [Google Scholar]
- 8.Cohen E, Horvath-Puho E, Ray JG, et al. Cardiovascular disease among women who gave birth to an infant with a major congenital anomaly. JAMA Netw Open 2018;1:e182320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sloper P Predictors of distress in parents of children with cancer: A prospective study. J Pediatr Psychol 2000;25:79–91. [DOI] [PubMed] [Google Scholar]
- 10.Thurston S, Paul L, Loney P, et al. Associations and costs of parental symptoms of psychiatric distress in a multi-diagnosis group of children with special needs. J Intellect Disabil Res 2011;55:263–280. [DOI] [PubMed] [Google Scholar]
- 11.Clark OE, Fortney CA, Dunnells ZDO, Gerhardt CA, Baughcum AE. Parent perceptions of infant symptoms and suffering and associations with distress among bereaved parents in the NICU. J Pain Symptom Manage 2021. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.Kreicbergs U, Valdimarsdottir U, Onelov E, et al. Care-related distress: A nationwide study of parents who lost their child to cancer. J Clin Oncol 2005;23:9162–9171. [DOI] [PubMed] [Google Scholar]
- 13.Olagunju AT, Sarimiye FO, Olagunju TO, Habeebu MY, Aina OF. Child’s symptom burden and depressive symptoms among caregivers of children with cancers: An argument for early integration of pediatric palliative care. Ann Palliat Med 2016;5:157–165. [DOI] [PubMed] [Google Scholar]
- 14.Beaune L, Morinis J, Rapoport A, et al. Paediatric palliative care and the social determimants of health: Mitigating the impact of urban poverty on children with life-limiting illnesses. Pediatr Child Health 2013;18:181–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bona K, London WB, Guo D, Frank DA, Wolfe J. Trajectory of material hardship and income poverty in families of children undergoing chemotherapy: A prospective cohort study. Pediatr Blood Cancer 2016;63:105–11. [DOI] [PubMed] [Google Scholar]
- 16.Bona K, Dussel V, Orellana L, et al. Economic impact of advanced pediatric cancer on families. J Pain Symptom Manage 2014;47:594–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilowite MF, Al-Sayegh H, Ma C, et al. The relationship between household income and patient-reported symptom distress and quality of life in children with advanced cancer: A report from the PediQUEST study. Cancer 2018;124:3934–3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macdonald ME, Chilibeck G, Affleck W, Cadell S. Gender imbalance in pediatric palliative care research samples. Palliat Med 2010;24:435–444. [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pew Research Center. The middle class is losing ground: No longer the majority and falling behind financially (Methodology). 2015. Available from: https://www.pewresearch.org/social-trends/2015/12/09/methodology/ Accessed June 29, 2021.
- 22.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feudtner C, Nye R, Hill DL, et al. Poly-symptomatology in pediatric palliative care patients based on parent-reported data. JAMA Pediatr. In Press. [Google Scholar]
- 24.Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med 2003;33:357–362. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002;32:959–976. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry 2003;60:184–189. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res 2012;21:88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Institutes of Health. PROMIS: Dynamic tools to measure health outcomes from a patient perspective. 2016. Available from: www.nihpromis.org. Accessed June 15, 2021.
- 29.Reeve BB, Hays RD, Bjorner JB, et al. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care 2007;45:S22–31. [DOI] [PubMed] [Google Scholar]
- 30.Teresi JA, Ocepek-Welikson K, Kleinman M, et al. Analysis of differential item functioning in the depression item bank from the Patient Reported Outcome Measurement Information System (PROMIS): An item response theory approach. Psychol Sci Q 2009;51:148–180. [PMC free article] [PubMed] [Google Scholar]
- 31.HealthMeasures. PROMIS Pediatric and Parent Proxy Profile Instruments (page 11). 2020. Available from: https://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Pediatric_and_Proxy_Profile_Scoring_Manual.pdf. Accessed June 16, 2021. [Google Scholar]
- 32.Chang VT, Thaler HT, Polyak TA, et al. Quality of life and survival: the role of multidimensional symptom assessment. Cancer 1998;83:173–179. [DOI] [PubMed] [Google Scholar]
- 33.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: An instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer 1994;30A:1326–1336. [DOI] [PubMed] [Google Scholar]
- 34.Stromgren A, Groenvold M, Pedersen L, Olsen A, Sjogren P. Symptomatology of cancer patients in palliative care_content validation of self-assessment questionnaires against medical records. Eur J Cancer 2002;38:788–794. [DOI] [PubMed] [Google Scholar]
- 35.Vogl D, Rosenfeld B, Breitbart W, et al. Symptom prevalence, characteristics, and distress in AIDS outpatients. J Pain Symptom Manage 1999;18:253–262. [DOI] [PubMed] [Google Scholar]
- 36.Wolfe J, Orellana L, Cook EF, et al. Improving the care of children with advanced cancer by using an electronic patient-reported feedback intervention: Results from the PediQUEST randomized controlled trial. J clin Oncol 2014;32:1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav 1981;22:337–356. [PubMed] [Google Scholar]
- 38.Semega J, Kollar M, Shrider EA, Creamer J. Income and Poverty in the United States: 2019. US Census Bureau. 2020. Available from: https://www.census.gov/library/publications/2020/demo/p60-270.html. Accessed June 29, 2021. [Google Scholar]
- 39.Pew Research Center. The middle class is losing ground: No longer the majority and falling behind financially. 2015. Available from: https://www.pewresearch.org/social-trends/2015/12/09/the-american-middle-class-is-losing-ground/. Accessed June 29, 2021.
- 40.McCarthy MC, Clarke NE, Ting CL, et al. Prevalence and predictors of parental grief and depression after the death of a child from cancer. Journal of Palliative Medicine 2010;13:1321–1326. [DOI] [PubMed] [Google Scholar]
- 41.Ramsey L, Graves P, Howard Sharp K, et al. Impact of race and socioeconomic status on psychologic outcomes in childhood cancer patients and caregivers. J Pediatr Hematol Oncol 2019;41:433–437. [DOI] [PubMed] [Google Scholar]
- 42.Rosenberg AR, Dussel V, Kang T, et al. Psychological distress in parents of children with advanced cancer. JAMA Pediatr 2013;167:537–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mackenzie C, Smith M, Hasher L, Leach L, Behl P. Cognitive functioning under stress: Evidence from informal caregivers of palliative patients. J Palliat Med 2007;10:749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mackenzie CS, Wiprzycka UJ, Hasher L, Goldstein D. Associations between psychological distress, learning, and memory in spouse caregivers of older adults. J Gerontol B Psychol Sci Soc Sci 2009;64:742–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morris AT, Gabert-Quillen C, Friebert S, Carst N, Delahanty DL. The indirect effect of positive parenting on the relationship between parent and sibling bereavement outcomes after the death of a child. J Pain Symptom Manage 2016;51:60–70. [DOI] [PubMed] [Google Scholar]
- 46.Knapp CA, Madden VL, Curtis CM, Sloyer P, Shenkman EA. Family support in pediatric palliative care: how are families impacted by their children’s illnesses? J Palliat Med 2010;13:421–426. [DOI] [PubMed] [Google Scholar]
- 47.Aoun SM, Gill FJ, Phillips MB, et al. The profile and support needs of parents in paediatric palliative care: comparing cancer and non-cancer groups. Palliat Care Soc Pract 2020;14:2632352420958000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomson J, Shah SS, Simmons JM, et al. Financial and social hardships in families of children with medical complexity. J Pediatr 2016;172:187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Currie ER, Christian BJ, Hinds PS, et al. Parent perspectives of neonatal intensive care at the end-of-life. J Pediatr Nurs 2016;31:478–89. [DOI] [PubMed] [Google Scholar]
- 50.McClung N, Glidewell J, Farr SL. Financial burdens and mental health needs in families of children with congenital heart disease. Congenit Heart Dis 2018;13:554–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baah FO, Teitelman AM, Riegel B. Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health - An integrative review. Nurs Inq 2019;26:e12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst 2017;109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dussel V, Bona K, Heath JA, et al. Unmeasured costs of a child’s death: perceived financial burden, work disruptions, and economic coping strategies used by American and Australian families who lost children to cancer. J Clin Oncol 2011;29:1007–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bona K, London WB, Guo D, et al. Prevalence and impact of financial hardship among New England pediatric stem cell transplantation families. Biol Blood Marrow Transplant 2015;21:312–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


