Abstract
Background
Disease prevention is a central aspect of primary care practice and is comprised of primary (eg, vaccinations), secondary (eg, screenings), tertiary (eg, chronic condition monitoring), and quaternary (eg, prevention of overmedicalization) levels. Despite rapid digital transformation of primary care practices, digital health interventions (DHIs) in preventive care have yet to be systematically evaluated.
Objective
This review aimed to identify and describe the scope and use of current DHIs for preventive care in primary care settings.
Methods
A scoping review to identify literature published from 2014 to 2020 was conducted across multiple databases using keywords and Medical Subject Headings terms covering primary care professionals, prevention and care management, and digital health. A subgroup analysis identified relevant studies conducted in US primary care settings, excluding DHIs that use the electronic health record (EHR) as a retrospective data capture tool. Technology descriptions, outcomes (eg, health care performance and implementation science), and study quality as per Oxford levels of evidence were abstracted.
Results
The search yielded 5274 citations, of which 1060 full-text articles were identified. Following a subgroup analysis, 241 articles met the inclusion criteria. Studies primarily examined DHIs among health information technologies, including EHRs (166/241, 68.9%), clinical decision support (88/241, 36.5%), telehealth (88/241, 36.5%), and multiple technologies (154/241, 63.9%). DHIs were predominantly used for tertiary prevention (131/241, 54.4%). Of the core primary care functions, comprehensiveness was addressed most frequently (213/241, 88.4%). DHI users were providers (205/241, 85.1%), patients (111/241, 46.1%), or multiple types (89/241, 36.9%). Reported outcomes were primarily clinical (179/241, 70.1%), and statistically significant improvements were common (192/241, 79.7%). Results were summarized across the following 5 topics for the most novel/distinct DHIs: population-centered, patient-centered, care access expansion, panel-centered (dashboarding), and application-driven DHIs. The quality of the included studies was moderate to low.
Conclusions
Preventive DHIs in primary care settings demonstrated meaningful improvements in both clinical and nonclinical outcomes, and across user types; however, adoption and implementation in the US were limited primarily to EHR platforms, and users were mainly clinicians receiving alerts regarding care management for their patients. Evaluations of negative results, effects on health disparities, and many other gaps remain to be explored.
Keywords: digital technology, primary health care, preventive medicine, telemedicine, clinical decision support systems
Introduction
The Institute of Medicine declared primary care to be “essential health care” and the central feature of an effective health care system [1]. Primary care has the potential to enhance quality, reduce costs, and increase equity and access to care by providing first contact and easy access to comprehensive, continuous, and coordinated medical care for patients [2] and populations, as articulated in the 4Cs framework by Dr Barbara Starfield [3]. Prevention of diseases and their complications ranks among primary care’s most fundamental functions; when performed effectively, primary care prevention can decrease mortality and morbidity in both chronic and acute conditions [4]. Various practitioners, including physicians, nurses, physician assistants, and pharmacists, recognize its value, but preventive services are often underutilized [5], despite guideline recommendations provided by the US Preventive Services Task Force [6].
Many studies have investigated the sources of suboptimal preventive health service delivery. Among the major barriers to preventive care implementation by clinicians is time. Studies have shown that 8.6 hours per working day are needed for a clinician to fully satisfy the US Preventive Services Taskforce preventive care recommendations for their patients [7]. A steady growth in competing demands across the management of acute, chronic, and preventive needs and an aging population with increasing comorbidities make it nearly impossible for a clinician to provide recommended preventive services without support. Innovations in care delivery, such as the patient-centered medical home [8], use of community health workers [9], and integration of primary care with public health [10], can help reduce this burden on clinicians, but with the rapid evolution of information technology, digital health interventions (DHIs) to address prevention are crucial.
DHIs are delivered via digital technologies to support a variety of health system needs and are used both formally and informally by providers, patients, and population stakeholders. Examples of these technologies include mobile wireless health devices (mobile health [mHealth]) using SMS or smartphone apps, telehealth systems for remote clinical services, wireless medical devices, software as a medical device (eg, clinical decision support), medical imaging, health information technology (HIT), and patient portals. Other digital health facets, such as advanced data analytics and artificial intelligence (AI), may be used as standalone interventions or integrated components within digital technologies. Digital health technologies may or may not be regulated by the US Food and Drug Administration (FDA) or recognized by the World Health Organization (WHO).
DHIs can support primary (eg, timely receipt of vaccinations), secondary (eg, completion of indicated screenings), tertiary (eg, routine monitoring of chronic conditions), and quaternary (eg, prevention of overmedicalization) prevention. DHIs have provided meaningful outcomes via the incorporation of care management programs, disease registries, and behavioral change interventions to improve medication adherence, promote weight loss, support smoking and substance abuse cessation, and enhance mental health [11]. Moreover, DHIs have been effectively used to address racial, ethnic, and socioeconomic health disparities [12]. In addition, the COVID-19 pandemic has accelerated the adoption of DHIs, such as telehealth services, and raised the possibility of longer-term incorporation of such technologies by a primary care community that has traditionally lagged hospital and acute care peers.
Although prior studies have examined the impact of individual DHIs on preventive service receipt, no comprehensive review of these modalities exists to date. A scoping review with a subgroup analysis was conducted to understand how DHIs are being used in US primary care settings to enhance and support the delivery of preventive care.
Methods
Study Design
A scoping review was conducted in accordance with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines [13] to identify studies that examined patients/consumers, providers, and/or population stakeholders in primary care settings (eg, limited to outpatient, ambulatory care, and long-term care) that used at least one digital health technology as an intervention for prevention (primary [eg, timely receipt of vaccinations], secondary [eg, completion of indicated screenings], tertiary [eg, routine monitoring of chronic conditions], and quaternary [eg, prevention of overmedicalization]) and reported beneficial outcomes on health, health care performance, and implementation science. The protocol is available upon request.
Search Strategy
Systematic search queries of MEDLINE via PubMed, Embase, and the Cochrane Library were used to identify references published or available online between January 1, 2014, and July 19, 2020 (Multimedia Appendices 1-7). Studies were limited to primary designs or systematic reviews (with the same inclusion criteria) published in English with abstracts. The rationale for this search cutoff time frame was based upon a high threshold of eligible providers achieving meaningful use of certified electronic health record (EHR) technology, whereby 82.8% of office-based physicians had adopted any EHR [14].
Screening Process
To ensure screener alignment, dual review of 20% of randomized titles and abstracts was followed by group resolution of conflicts. All remaining titles and abstracts underwent single review, and full-text articles were examined by 2 independent reviewers for relevance against the inclusion/exclusion criteria (Multimedia Appendix 8), with third-party adjudication provided for any discrepancies in eligibility. Results were tracked in DistillerSR (Evidence Partners).
The eligible population criteria included studies that examined patients/consumers, providers (both licensed and unlicensed), and/or population stakeholders (eg, payers, employers, communities, health systems, and the government) in outpatient care, ambulatory care, and long-term settings of primary care. Interventions had to target primary, secondary, tertiary, or quaternary prevention using at least one FDA/WHO approved or nonregulated digital health technology facet (eg, telehealth, mHealth, HIT, data analytics, and AI). No comparisons were required. Outcomes of interest included health (eg, individual- or population-level outcomes), health care performance (eg, as per the Agency for Healthcare Research and Quality [AHRQ]: access, quality, utilization, and efficiency, with measures categorized as structural, process, or outcomes including clinical/physiological, surrogate/intermediate, patient-centered, or patient-reported), and DHI implementation (eg, taxonomy as per Proctor et al: acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability) [15]. Only English-language primary studies or systematic reviews with the same inclusion criteria published between January 2014 and July 2020 were included. For definitions and descriptions of terms, see Multimedia Appendix 8 and Multimedia Appendix 9. Notable exclusion criteria for interventions included DHIs associated with treatment or diagnosis (except for preventive screenings), medical imaging for diagnosis, and telehealth using only noncellular telephone communication. Studies conducted in critical care (eg, intensive care unit) or inpatient (eg, hospital admission) settings were excluded.
Data Extraction
After a series of data form piloting and discussions by all extractors to identify gaps in data extraction forms and ensure consistency in the application of definitions, data were abstracted into standardized forms within DistillerSR (Multimedia Appendix 10) for synthesis by a single reviewer. All fields of the data extraction forms for each article were examined for completeness by a second reviewer. Many data categorizations were not mutually exclusive, resulting in percentages totaling more than 100%.
Subgroup Analysis and Data Synthesis
Following title and abstract screening, the large scope (>1000 titles) of the remaining included studies prohibited full-text review of all preventive DHIs identified globally. To narrow the scope of the geography and interventions under review, a subgroup analysis was performed; geography limits were set to only include studies conducted in the US. Additionally, it was apparent that a large volume of records focused on data analysis methods tangential to the development of DHIs. As such, studies that only used EHRs as a retrospective data capture tool were excluded. Two examples of excluded studies are a retrospective analysis of EHRs to determine the prevalence of a preventable disease and a study on the use of diagnostic telemedicine referral to a dermatologist.
Content analysis of extracted technology descriptions was performed to identify recurrent topics and more clearly understand the types of DHIs evaluated in the included studies according to a priori research questions in the protocol. This analysis yielded a list of articles selected to represent innovative or unique DHIs and their implementation in the final data set. Selected technologies were then narratively synthesized into 5 topical groups (eg, population-centered, patient-centered, care access expansion, panel-centered [dashboarding], and app-driven) to provide a framework for their analysis. Selected outcome (eg, health, health care performance, and implementation science) results from these articles were then extracted by a single reviewer to provide additional context regarding the impact of these DHIs beyond the directionality of their results. Details presented from this synthesis are not exhaustive, and key use cases have been highlighted in the results.
Study Quality
Study quality was assessed using the Oxford levels of evidence [16], which allow for the categorization of evidence quality across heterogeneous study types. Examples of the study types comprising these evidence levels include (in increasing quality) expert opinion, case series, systematic reviews of case-control studies, individual cohort studies, randomized controlled trials (RCTs) with narrow confidence intervals, and systematic reviews of RCTs.
Results
Literature searches yielded 5274 unique citations, of which 1060 articles were eligible for full-text screening. A subgroup analysis was conducted to limit geography to US–only settings and exclude DHIs that evaluated EHRs as retrospective data capture tools. These applied limits resulted in 310 articles for full-text review, of which 241 articles [17-257] were included for the subgroup analysis (Figure 1). Abstractions of the included articles can be found in Multimedia Appendix 11. An overview of the study design and key findings is provided in Figure 2. The types of DHI articles covered included HIT (166/241, 68.9%), clinical decision support (88/241, 36.5%), telehealth (88/241, 36.5%), mHealth (35/241, 14.5%), patient portals (16/241, 6.6%), wireless medical devices (6/241, 2.5%), medical imaging (2/241, 0.8%), and other DHIs (31/241, 12.9%) (see Multimedia Appendix 9 for a description of each). The integration of multiple types of technologies was commonly applied to support DHIs (154/241, 63.9%) in practice. The most commonly identified combination of technology was the use of clinical decision support algorithms and mHealth to support more advanced care using HIT-related data.
Figure 1.
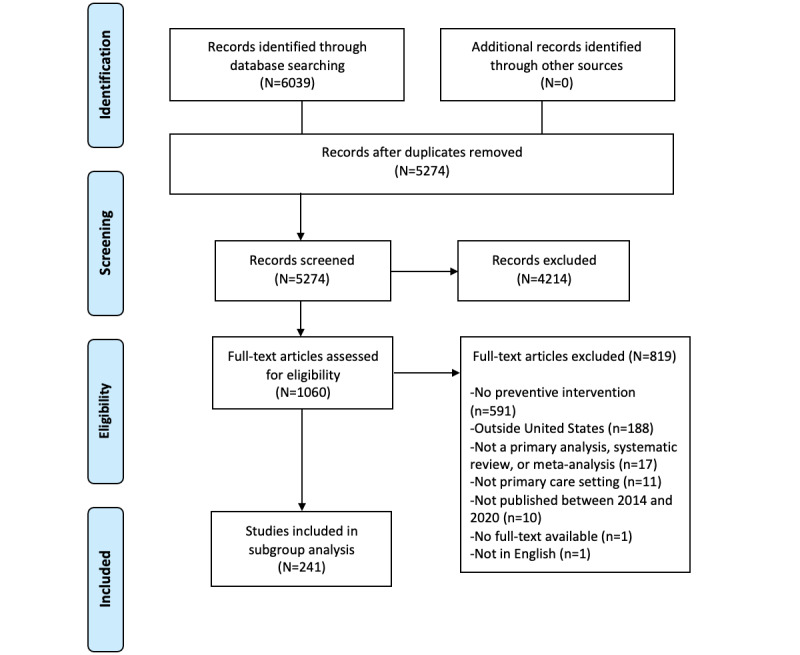
The flow diagram illustrates the flow of information through the different phases of the scoping review, including the number of records identified, included and excluded records, and the reasons for exclusion.
Figure 2.
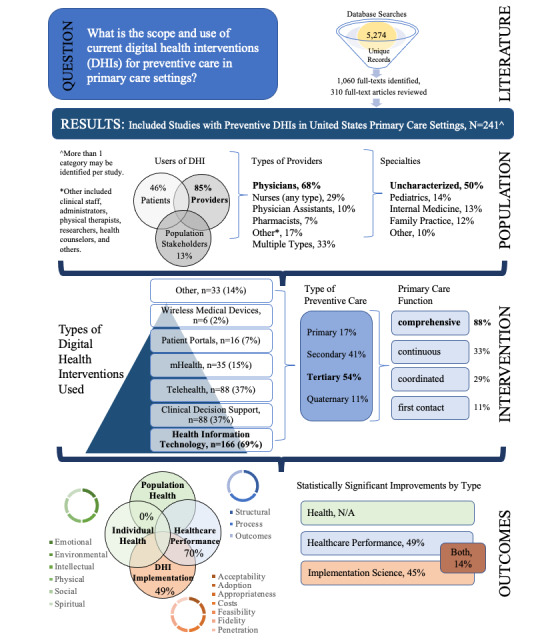
Summary of the study design and key findings. Scoping review study design and summarization of results across the categories of study population, intervention, and outcomes. N/A, not applicable.
The DHIs predominantly addressed tertiary prevention (131/241, 54.4%), followed by secondary (97/241, 40.3%), primary (40/241, 16.6%), and quaternary prevention (27/241, 11.2%), and a combination of prevention levels (43/241, 17.8%). The 4Cs primary care model by Dr Starfield was used as a framework to identify how DHIs supported delivery of preventive care; a large number of articles evaluated DHIs that demonstrated improvements in comprehensiveness of care (213/241, 88.4%), continuous care (76/241, 31.5%), coordinated care (69/241, 28.6%), and first contact care (26/241, 10.8%). The continuum of comprehensive care by DHIs included proactive anticipatory care, self-management support for patients, community resources for patients, longer patient visits to improve communication and clinician documentation, coding practices to improve accuracy, preventive care best practices (eg, immunizations, disease prevention and management, and reduction of overmedicalization), support for the increased scope of clinician practice, and knowledge-seeking practices.
DHI users were identified as providers (205/241, 85.1%), patients/consumers (111/241, 46.1%), others (31/241, 12.9%), or spanning multiple types (89/241, 36.9%). The types of providers using DHIs included physicians (163/241, 67.3%), nurses of any type (71/241, 29.5%), physician assistants (24/241, 10.0%), pharmacists (16/241, 6.6%), others (42/241, 17.4%), and multiple types (79/241, 32.8%). The “others” provider type included various clinic staff, administrators, technicians, physical therapists, researchers, health counselors, etc. The DHI user physician specialty characterization was as follows: uncharacterized (121/241, 50.2%), pediatrics (34/241, 14.1%), internal medicine (32/241, 13.2%), family practice (30/241, 12.4%), and others (25/241, 10.4%). Notably, 27 (11.2%) articles involved study settings with a mix of user types among majority Latino, African American, and Asian American populations, but only 6 (2%) of them discussed health disparities as the primary focus of their DHIs.
Primary and secondary outcomes for DHIs were predominantly clinical; 169 (70.1%) articles addressed clinical (eg, health care performance) outcomes, whereas 119 (49.4%) addressed nonclinical (eg, implementation science) outcomes. No identified studies examined health domain-related (eg, outcomes related to dimensions of wellness such as environmental, emotional, intellectual, physical, social, and spiritual) outcomes. A statistically significant improvement in relevant measured outcomes was identified in 192 (79.7%) articles, with 117 (48.5%) articles reporting improved health care performance outcomes (eg, preventive care/screening rates, validated tool scores, and medication adherence), 109 (45.2%) articles reporting improved implementation science outcomes (eg, intervention acceptability, adoption, and cost), and 34 (14.1%) articles reporting improvement in both. Among articles demonstrating statistically significant improvements in outcomes, 16 (6.6%) and 15 (6.2%) showed benefits for racial/ethnic groups specifically in health care and implementation science outcomes, respectively, with 4 (1.7%) articles identifying benefits for racial/ethnic groups in both. Moreover, 39 (16.2%) articles demonstrated only nonsignificant beneficial findings, while 8 (3.3%) articles provided no beneficial findings and only 1 (0.4%) article reported harm resulting from a DHI (in this case, limited to a portion of a subpopulation, whereas other populations received benefit).
Given that DHIs are frequently implemented as a combination of technologies, a content analysis was conducted to understand how DHIs identified in the included studies are collectively and uniquely being leveraged in care settings to impact prevention. Five topics were identified following content analysis that represent the most novel or distinct DHIs from the reviewed studies as follows: population-centered, patient-centered, care access expansion, panel-centered (dashboarding), and app-driven. Selected abstractions for the articles matching these topics are presented in Tables 1-5.
Table 1.
Population-centered digital interventions for primary care.
| First author, year | Study design | Description of technology | Sample size | Selected outcomes |
| Nagykaldi, 2014 [172] | Pre-post | Linking of a regional health system, hospital organization, and preventive services reminder system via HIEa. | 346 patients (20% ethnic minorities) | 12%-36% increase in preventive service documentation and delivery (P<.001). 9.6% increase in medication reconciliation (P<.001). |
| Nagykaldi, 2017 [171] | Pre-post | Wellness coordinator connection to HIE organizations, PCPsb, county health departments, and hospitals for preventive care outreach for rural communities. | 9138 rural patients | 3%-215% increase in delivery of 10 preventive services over 12 months (P=.004). 80% ROIc for selective preventive services (range, 32%-122%). 40% ROI on wellness coordinator employment cost. |
| Fanizza, 2018 [81] | Open label nonrandomized | Pharmacist connection to the state HIE for comprehensive medication review after discharge and communication with prescribers. | 40 patients | 25.2% decrease in overall 30-day readmission rates (P=.03). 22.7% decrease in 30-day readmission rates for initial diagnosis (P=.009). |
| Shade, 2015 [199] | Pre-post | Clinic link to the state surveillance system providing alerts when out-of-care HIV patients present in the EDd or other settings. | 6 sites serving underserved communities | ORe 2.61 (95% CI 2.11-3.21) for care retention (P=.001). OR 1.24 (95% CI 1.03-1.49) for being on ARTf (P=.02). OR 4.16 (95% CI 2.54-6.80) for undetectable viral load (P<.001). |
aHIE: health information exchange.
bPCP: primary care provider.
cROI: return on investment.
dED: emergency department.
eOR: odds ratio.
fART: antiretroviral therapy.
Table 5.
Selected app-driven digital health interventions for primary care.
| First author, year | Study design | Description of technology | Sample size | Selected outcomes |
| Bennett, 2018 [35] | RCTa | App using IVRb and SMS text messaging to collect patient behavior change data and weight via a smart scale, provide tailored patient feedback based on goal progression, and generate EHRc counseling recommendations for clinicians. | 351 patients | −4.4 kg (95% CI −5.5 to −3.3) weight loss at 6 months (P<.001); −3.8 kg (95% CI −5.0 to −2.5) weight loss at 12 months (P<.001). Participants completing ≥80% of interactions lost significantly more weight than less engaged participants (P<.01). |
| Brayboy, 2016 [45] | Pre-post | iPhone-compatible app for providing trusted, age-appropriate, straightforward sexual health information and resources to teenage girls. | 20 teenage girls | 3.4%-4.2% improvement in sexual health topic knowledge. 58.8% increase in the perception that they or other teenage girls would use the app (P<.001). |
| Dahne, 2019 [64] | RCT | Self-help app adaptation of Brief Behavioral Apptivation, including education, identification of values, daily mood monitoring, and social support including gamification, to reinforce continued use. | 52 patients | 63% greater decrease on BDI-IId assessment after treatment compared with usual care. 70% of participants continued to use the app 1 month after enrollment, and 50% continued to use it at 2 months. |
| Gustafson, 2014 [99] | RCT | Smartphone app to support alcoholism recovery using alerts for trigger locations, audio-guided relaxation, PROe measurement, and clinician notification, as well as a panic button for contacting support persons. | 349 patients | 1.37 (95% CI 0.46-2.27) fewer risky drinking days than controls over 12 months (P=.003). OR 1.65 (95% CI 1.05-2.57) for abstinence prevalence over 12 months (P=.03). |
| Leddy, 2019 [140] | RCT | Home smartphone urinalysis test to complete proteinuria screening for HTNf management. SMS text message link for downloading the app, obtaining the home testing kit, and receiving PCPg notification of abnormal results. | 999 patients | 10.9% increase in proteinuria screening completion (P<.001). 89% of home test patients preferred home testing over a visit to the physician’s office. |
| Lv, 2017 [149] | Pre-post | Dashboard of patient’s personalized action plan, treatment goals, and self-monitoring data combined with a wireless BPh monitor, smartphone, study app, pedometer, and web messaging system. | 147 patients | 55.9% increase in the proportion of patients meeting office BP goals (<140/90 mmHg) at 6 months (P<.001). 46.2% increase in the proportion of patients meeting home BP goals (<135/85 mmHg) at 6 months (P<.001). |
| Ofili, 2018 [176] | Pre-post | App with diabetes curriculum, goal identification and tracking, connectivity to consumer devices (eg, activity monitors), and health coach consultation. | 287 patients | Improvements in SBPi (6 mmHg), blood glucose (15 mg/dL), and physical activity (0.56 miles/day) at 12 weeks (all P<.01), which continued through 52 weeks. |
| Yu, 2018 [249] | Pre-post | App delivering a guided cognitive behavioral program for generalized anxiety disorder along with in-app coach pairing and messaging. | 63 patients | 3.6-point mean reduction on GAD-7j over 2 months for patients with baseline GAD-7 ≥8 (P<.001). |
aRCT: randomized controlled trial.
bIVR: interactive voice response.
cEHR: electronic health record.
dBDI-II: Beck Depression Inventory II.
ePRO: patient-reported outcome.
fHTN: hypertension.
gPCP: primary care provider.
hBP: blood pressure.
iSBP: systolic blood pressure.
jGAD-7: Generalized Anxiety Disorder-7.
Table 4.
Panel-centered digital health interventions for primary care (dashboarding).
| First author, year | Study design | Description of technology | Sample size | Selected outcomes |
| Allen, 2017 [24] | RCTa | Culturally sensitive team model using an electronic diabetes dashboard providing alerts and reports for each patient regarding clinical and behavioral factors and social distress. | 399 Latino patients | Social distress score decrease of 0.6 (controls) vs 1.6 (intervention) over 6 months (P=.01). |
| Duquaine, 2015 [75] | Observational cohort | CDSb for tobacco use and interventions for smoking cessation; quarterly communications with practice-specific and overall program performance. | 19 clinics treating low-income and Medicaid patients | Successful implementation at all sites. Change in EHRc documentation of prevalence and cessation rates (NRd). |
| Fiks, 2015 [85] | Open-label nonrandomized | Quarterly feedback reports summarizing personal, practice, and network rates of missed HPVe vaccine opportunities. | 227 PCPsf | 5.7% (95% CI 3.8-7.7) increase in HPV vaccination compared with controls. |
| Kapoor, 2018 [127] | Observational cohort | Emailed report of the proportion of atrial fibrillation patients receiving anticoagulation therapy compared to peers plus EHR message 1 day before visits with anticoagulation eligible patients. | 5406 patients | Providers reviewed emails (45%) and EHR messages (96%), demonstrating feasibility. No change in the percentage of patients receiving anticoagulation therapy compared with controls after 3 months. |
| Zimmerman, 2017 [255]; Nowalk, 2016 [174]; Zimmerman, 2017 [257]; Lin, 2016 [145]; Zimmerman, 2017 [256] | RCT and pre-post | 4 Pillars Immunization Toolkit and Practice Transformation Program. Web-based dashboard providing and tracking strategies for increasing practice vaccination rates, including EHR prompts, digital outreach, and standing order programs. |
25 clinics [255]; 24 clinics [174]; 11 clinics [257]; 25 clinics [145]; 22 clinics [256] | 2.7% to 10.2% statistically significant increases in vaccination rates for intervention and control sites during RCT studies. −1.9% to 17.1% statistically significant increases in vaccination rates for active intervention groups during year 2 of the pre-post study. |
aRCT: randomized controlled trial.
bCDS: clinical decision support.
cEHR: electronic health record.
dNR: not reported.
eHPV: human papillomavirus.
fPCP: primary care physician.
Primary prevention targets focused on the use of population-centered [171,172] and panel-centered [85,145,175,255-257] DHIs to improve adolescent [256,257] or adult [145,171,172,174,255] vaccination rates for human papillomavirus [256,257], influenza [145,171,172,257], pneumococcal disease [171,172,255,257], and Tdap (tetanus, diphtheria, and pertussis) [174,257].
All the above DHIs that targeted primary prevention had statistically significant health care [145,172,255-257] or implementation [171,174] outcomes following the intervention. Identifying return on investment (ROI) and value on investment can be large barriers for DHI implementation; however, both were satisfied when a community wellness registry was connected to EHRs via a health information exchange (HIE). This pilot study demonstrated the feasibility and cost-effectiveness of technology implementation in a community-based model with a mean ROI of 80% (range, 32% to 122%) for the improved delivery of 10 selective preventive services (mean increase 35%, range 3% to 215%; P=.04) in rural settings [171].
Patient-centered [112,163,211] and population-centered [171,172] DHIs supported secondary prevention by examining measures that led to early diagnosis and treatment using direct-to-patient messaging in an EHR [112,163], decision aids embedded in patient portals [211], and an intelligent HIE using clinical decision support [171,172]. These DHIs improved screening rates for cancer (eg, breast [172] and colorectal [163,171,172]), hepatitis C virus (HCV) [112], and osteoporosis [171,211]. Only 1 study in this grouping did not have significant improvements following the DHI, which may be due to the more invasive and costly colonoscopy procedure itself rather than the ineffectiveness of the EHR portal messaging intervention to improve colorectal cancer screening [163]. However, an advanced EHR that used population analytics and bulk laboratory ordering to directly engage patients for universal HCV screening nearly doubled testing (odds ratio 1.7, 95% CI 1.2-2.1) in the intervention group [112].
Tertiary prevention for chronic disease management was supported primarily by care access expansion [20,58,103,178,181,189], app-driven [35,64,140,149,176,249], and patient-centered [38,97,241,245] approaches. Overall, DHIs decreased disease severity and associated comorbidities; lowered the numbers of emergency department visits, hospitalizations, and 30-day readmissions; increased the receipt of follow-up care; improved medication adherence in the identified studies [20,35,58,64,97,103,149,176,199,245,249]; and improved the quality or effectiveness of health services by technology implementation [24,38,103,140,171,178,186,189,249]. Disease areas targeted by DHIs included diabetes [38,97,171,176], hypertension [97,140,149], asthma [103,181,186], obesity [35,171], cardiovascular disease [123], HIV [199], HCV [245], and hyperlipidemia [97]. Management of behavioral health included smoking cessation support [75,171,189], promotion of physical activity [171], substance abuse management [99,185], and sexual health education [45] using mHealth technology. Mental health [58] (eg, depression [20,64], anxiety [249], posttraumatic stress disorder [178], and social distress [24]) improved following digital interventions. Notably, telehealth and mHealth were leveraged predominantly to support mental health interventions with care access expansion [20,58,178] and app-driven [64,249] technologies to improve patient function, minimize illness impacts, and decrease associated complications. Behavioral and mental health conditions and other chronic diseases often occur concurrently [258]. Two studies [178,185] integrated behavioral or mental health DHIs for chronic condition care, but only 1 study [178] reported outcome measures for both mental and physical health, whereby both improved significantly.
Notably, none of the studies identified by the content analysis examined DHIs for quaternary prevention.
Using the Oxford levels of evidence [16], the quality of the included studies was moderate to low overall due to many studies (101/241, 41.9%) presenting level 4 evidence (eg, case series, poor quality cohort, and case-control studies) and the remainder displaying level 1b (eg, individual RCTs with a narrow CI; 46/241, 19.1%), 2b (eg, individual cohorts including low-quality RCTs; 58/241, 24.1%), 2c (eg, outcomes research and ecological studies; 17/241, 7.1%), 3b (eg, individual case-control studies; 17/241, 7.1%), or 5 (eg, expert opinions; 3/241, 1.2%) evidence.
Discussion
Principal Findings
Amidst the rapid digital transformation of the primary care delivery system in response to the COVID-19 pandemic, this is the first comprehensive summary on DHIs in use by interdisciplinary clinicians (eg, physicians, pharmacists, psychiatrists, etc) in primary care. This scoping review and its subgroup analysis summarized a growing evidence base and rendered a collection of potentially successful strategies for patients, providers, and population stakeholders to improve outcomes for health, health care performance, and implementation science through the use of DHIs. Moreover, important scientific gaps were identified in the contemporary evaluation and knowledge of DHIs leveraged in primary care, particularly the scarcity of the evaluation of DHIs in health disparities and evaluation of the negative effects of DHIs.
A few major themes emerged from our analysis of the extracted data. First, the digital health technologies identified and reviewed were highly concentrated in a narrow range of HIT, most specifically around EHRs/electronic medical records, particularly with the use of alerts to help clinicians make appropriate clinical decisions. Though understandable given their high use and decade-long attention to increasing adoption via “meaningful use” in primary care [259,260], the absence of DHI literature involving other platforms was telling. Despite unprecedented attention to telehealth implementation due to the COVID-19 pandemic response, little evidence of effective implementation of this specific DHI exists to guide primary care telehealth use for health care delivery in the US. A few studies did examine more innovative uses of technology, particularly for the delivery of mental and behavioral health (Tables 1-5). As HIT continues to rapidly evolve and health care is delivered in more innovative ways due to the COVID-19 pandemic, more research should focus on novel DHIs applied to primary care.
Second, despite prevention being 1 of 6 mechanisms underpinning primary care’s beneficial impact on population health [261] and an early target for DHIs, studies evaluating prevention were predominantly focused on secondary or tertiary preventive interventions. Most would agree that disease prevention offers the greatest yield for population health and is amenable to DHIs via mobile and online apps, clinical kiosks, and electronic patient portals [262,263]. Primary prevention interventions, such as immunizations, rely on effective patient counseling and education, which can be difficult and time-consuming to document and capture in EHRs (the predominant type of intervention found in our review). This finding may be a reflection of physician roles in the US. Traditionally, the role of primary prevention has relied on public health professionals [264], and although primary care physicians are increasing their ability to address the needs of the community, most physicians are still focused on the needs of the individual [265]. As the intersection of public health and primary care becomes more urgent to strategically improve individual and population health, future studies should examine the role of DHI adoption and implementation in their integration.
Third, DHIs enhanced core primary care functions by contributing to the comprehensiveness of care provided. This was an unexpected finding given that DHIs are often thought of in the context of first contact through patient portals, coordination through electronic referrals and linked EHRs, and continuity through HIEs and sharing of documents. Many of the articles reviewed discussed the use of DHIs to identify patients in need of services and alert clinicians to provide them. For example, multiple studies described EHR alerts that would prompt clinicians to order viral hepatitis C testing for patients with indications for screening (Multimedia Appendix 11) [83,93,112,116,133,150,164,173,207,246]. Other studies shared examples of how patients could be trained to provide services for themselves (Table 2) or how DHIs could be used to offer additional clinical services (Table 3). Thus, it makes sense that comprehensiveness, or the provision of a robust set of services to a patient, would be improved with DHIs. In an era where comprehensiveness of care is said to be declining in primary care [266-271], DHIs may provide an innovative solution for primary care practices to increase and enhance the services they provide.
Table 2.
Selected patient-centered digital health interventions for primary care (direct engagement).
| First author, year | Study design | Description of technology | Sample size | Selected outcomes |
| Grant, 2015 [97] | RCTa | Informatics surveillance and reminder system connected to EHRb lab test orders that generates mailed letters requesting patient completion of labs for hyperlipidemia, diabetes, and HTNc monitoring. | 4038 patients | aHRd 1.26 (95% CI 0.99-1.62) for decreased time to LDLe goal. aHR 1.15 (95% CI 1.01-1.32) for earlier LDL lab assessment. |
| Hess, 2014 [110] | Observational cohort | PHRf delivering active notifications regarding gaps in preventive chronic disease monitoring until patient logs on to the PHR or closes the prevention gap. | 584 patients | 58% of all prevention gaps were closed over 12 months. 61% of notified patients accessed the PHR or closed the triggering care gap after the 1st message and 73% after the 2nd message. |
| Hojat, 2020 [112] | Controlled trial | EHR bulk-ordered HCVg antibody testing plus automatic PHR messages requesting patients to go to the lab. | 1024 patients | 14% increase in completed HCV tests (P<.001; ORh 1.7, 95% CI 1.2-2.1). Only 3.5% of patients responded to PHR messages, and repeat messaging had no effect on completion. |
| Langford, 2019 [138] | Observational cohort | SMS text message contact to help underserved patients with diabetes find their optimal basal insulin dose. | 113 patients | 84% of patients reached optimal insulin dose. Age, copay status, and initial fasting blood glucose were significantly associated with 100% SMS response (P≤.03). |
| Mehta, 2018 [163] | RCT | Patient portal message containing either opt-in or opt-out for FITi colorectal cancer screening test. | 127 patients | 28% higher FIT completion rate for patients receiving opt-out messages. |
| Quanbeck 2018 [185] | Observational cohort | Patient discussion board, interactive modules for health tracking, and self-management and coping with cravings for addiction management. Clinician web portal for patient-generated data. | 268 patients | 44% reduction in risky drinking days (P=.04), and 34% reduction in illicit drug use days (P=.01), over 12 months. 53%-60% of patients accessed the intervention during the final week of the implementation period. |
| Smallwood, 2017 [211] | RCT | Patient portal decision support tool for fracture risk and prevention. Includes educational information, risk calculation, and a treatment decision values elicitation exercise. | 50 patients | Improved decision quality (P<.001) and conflict (P<.001) scores after the intervention. 25.7% (P=.046) increase in treatment decisions 3 months after the intervention. |
| Turvey, 2016 [234] | RCT | Patient portal link to a downloadable and printable CCDj for sharing with non-VAk providers for continuity of care. | 52 patients | 73% increase in the proportion of patients sharing the CCD with non-VA providers with training on accessing the CCD (P<.001). No improvement in medication reconciliations, but significant reduction in duplicate laboratory tests ordered by non-VA providers (P=.02). |
| Woo, 2016 [241] | Pilot | Daily customized spinal cord injury/disorder disease management questions delivered to patients via a data messaging device. Provider web portal with patient responses and risk level ratings. | 33 patients | Average total response rate of 56%, ranging from 10% to 93%. Nearly 20% decrease in the DUSOIl score over 6 months. |
| Yakovchenko, 2019 [245] | RCT | Customized SMS reminder messages about HCV treatment appointments, labs, adherence, and motivation. | 71 patients | Lower distress about failing treatment (P=.05) and better medication adherence (P=.06). 96% of texters vs 94% of nontexters achieved SVRm. |
aRCT: randomized controlled trial.
bEHR: electronic health record.
cHTN: hypertension.
daHR: adjusted hazard ratio.
eLDL: low-density lipoprotein.
fPHR: personalized health record.
gHCV: hepatitis C virus.
hOR: odds ratio.
iFIT: fecal immunochemical test.
jCCD: continuity of care document.
kVA: Veterans Affairs.
lDUSOI: Duke Severity of Illness Checklist.
mSVR: sustained virologic response.
Table 3.
Selected care access expansion digital health interventions (virtual care/telehealth).
| First author, year | Study design | Description of technology | Sample size | Selected outcomes |
| Aikens, 2015 [20] | Observational cohort | Weekly IVRa calls for depression self-management. Option to designate a lay support person to receive email reports summarizing reported symptoms and providing problem-tailored support guidance. | 221 patients | Increases of 20% in the per-week aORb for medication adherence and 16% for depression remission compared with controls. |
| Coker, 2019 [58] | RCTc | Telehealth-enhanced referral to a CMHCd using informational videos, SMS text messages, and telehealth screening at the primary care clinic. | 342 Latino children | aOR 3.02 (95% CI 1.47-6.22) for completing CMHC visits compared with controls. Telehealth referrals took longer to complete screening but reported greater satisfaction with referral than controls. |
| Halterman, 2018 [103] | RCT | Videoconference telemedicine visit in a school health office for asthma baseline and medication; follow-up telemedicine assessments every 4-6 weeks. | 400 urban students | 0.69 (95% CI 0.15-1.22) more symptom-free days per 2 weeks (P=.01). aOR 0.52 (95% CI 0.32-0.84) for asthma-related EDe visit or hospitalization. |
| Osofsky, 2017 [178] | Pre-experimental time series | Onsite and/or telemedicine behavioral-based trauma treatment delivered in primary care clinics. | 235 patients | 4.5-point decrease in the PCL-Cf score (P=.001), and 1.8-point decrease in the PHQ-15g score (P=.001). |
| Perry, 2018 [181] | RCT | Live video telemedicine asthma education at school for a child, caregiver(s), and school nurse; telemonitoring of patient-reported symptoms; PCPh prompts with guideline-based asthma management. | 393 rural African American students | No change in symptom-free days, quality of life, or lung function. 42% increase in peak flow meter use compared with controls (P<.01) and 19% increase in medication adherence (P=.03) over 6 months. |
| Reeves, 2016 [186] | Pre-post | Implementation of EHRsi in the school system for the asthma care program; messaging connection to PCP EHR systems; school nurse asthma template for PCP messaging. | 33 students | 39.4% decrease in asthma inpatient admissions (P<.001) and 18.2% decrease in exacerbations (P<.05) over 12 months. |
| Richter, 2015 [189] | RCT | Live video telehealth for tobacco cessation delivered in primary care clinics. | 566 patients | No difference in biochemically verified prevalence, prolonged abstinence, quit attempts, or number of cigarettes smoked per day compared with phone counseling. |
aIVR: interactive voice response.
baOR: adjusted odds ratio.
cRCT: randomized controlled trial.
dCMHC: community mental health clinic.
eED: emergency department.
fPCL-C: posttraumatic stress disorder checklist-civilian version.
gPHQ-15: 15-item patient health questionnaire.
hPCP: primary care physician.
iEHR: electronic health record.
Finally, while the development and release of health apps continue to increase, few evaluations of app-driven DHIs were identified in our study (Table 5). This may be in part because many apps lacked integration with primary care or other technology systems or because of the evolving standards for evaluating these types of interventions, as evidenced by the recent establishment of the FDA’s Digital Health Center of Excellence [272]. Most app-driven DHIs included in our study were patient-facing and focused on helping to better involve patients in their care. However, app-driven DHIs are also capable of providing an overwhelming amount of data to providers. Balancing data collection features from apps by adding functionalities, such as thresholds triggering clinical alerts/feedback, designing patient-counseling suggestions based on gathered data, and pairing with timely coaching/contact is important to enhance the clinical relevance and quality of these tools. As the development and clinical adoption of app-driven DHIs continue to expand, rigorous investigation of their safety, efficacy, and value in primary care is urgently needed.
Limitations
These results should be interpreted in the context of a few limitations. The findings are limited to studies conducted in US settings, which prohibits the generalization of their applicability and use at a global scale. Review of the use of DHIs in non-US primary care settings should be prioritized in future work. Further, due to the heterogeneity of identified interventions, it is not possible to provide head-to-head comparisons. The large heterogeneity of DHIs is an additional reason why our synthesis focused on the novel and distinct DHIs that are collectively used in primary care practice rather than presenting evidence collated by distinct DHI technologies. Other limitations include single screening of titles and abstracts, English language restriction, and lack of gray literature evaluation. Data extraction for each article was not confirmed by a secondary reviewer, leaving room for bias in the interpretation of the articles. For example, it was left up to each reviewer to determine the type of prevention the DHI was addressing, or which primary care function (eg, the 4Cs by Dr Starfield: first contact, comprehensiveness, continuity, and coordination) the DHI enhanced. However, careful and collaborative definition of our processes and outcomes prior to extraction (ie, types of prevention or primary care functions) should minimize this bias. Lastly, we intentionally selected a quality assessment tool rather than a risk of bias tool, as we only planned to measure the extent that methodological safeguards (ie, internal validity) against bias were implemented. A risk of bias assessment would have offered a bias judgement (ie, estimation of intervention effects) on such a quality assessment, and judgement of the evidence may have shifted with this approach. It is important to consider that even when a study implements all possible safeguards in a tool, it may not be unbiased, and conversely, a study applying no safeguards is not necessarily biased [273].
Conclusions
Gayle Stephens noted in 1965 that “One of the paradoxes of our time is that the healing relationship seems most in jeopardy at a time when we need it most,” commenting on the range of “forces which threaten to depersonalize the meeting of a doctor and patient” [274]. That paradox remains in an age where technology is often seen as distracting rather than enhancing care. Through further adoption of DHIs with evidence of effectiveness, providers and patients/consumers can enhance primary care by improving the delivery of preventive services and promoting more comprehensive care. Yet, relying solely on EHR alerts may not lead to substantial improvements in health care in the US. Moreover, rigorous and prospective evaluations of the potential negative effects of these DHIs, particularly for clinical end users of these technologies, will be needed to ensure holistic improvement of health care. Innovative DHIs should undergo evaluation in well-designed studies to generate evidence and establish best practices that can be replicated and scaled in diverse primary care settings. Given the ability of technology to amplify existing health disparities and biases, the development of DHIs that can help overcome health disparities and the evaluation of the benefits and harms of current DHIs on health disparities are imperative. In addition, DHIs that allow integration of public health with primary care will be essential for rapid and effective responses to health and health care challenges, such as the COVID-19 pandemic, in an increasingly technology-driven health care environment.
Acknowledgments
We would like to thank Dr Brian Antono for his screening support. Funding was provided by IBM Watson Health.
Abbreviations
- AI
artificial intelligence
- DHI
digital health intervention
- EHR
electronic health record
- FDA
Food and Drug Administration
- HCV
hepatitis C virus
- HIE
health information exchange
- HIT
health information technology
- mHealth
mobile health
- RCT
randomized controlled trial
- ROI
return on investment
- WHO
World Health Organization
Search outline using the PCC (participants, concept, and context) framework.
MEDLINE search via PubMed.
Cochrane Library search.
Embase search.
Updated MEDLINE search via PubMed.
Updated Cochrane Library search.
Updated Embase search.
Inclusion/exclusion criteria.
Description of digital health intervention categories.
Data extraction forms.
Abstracted results from included articles.
Footnotes
Authors' Contributions: Conceptualization: KJTC, YJ, AB, and KBR; formal analysis: KJTC, VCW, YEA, ELS, YJ, and MA; methodology: KJTC; project administration: KJTC; supervision: KJTC; validation: KJTC and VCW; writing–original draft: KJTC, YJ, VCW, and AB; writing–review and editing: all authors.
Conflicts of Interest: VCW was employed by IBM Corporation. KJTC is employed by IBM Corporation. YJ has no conflicts. ELS was employed by IBM Corporation. YEA was employed by IBM Corporation. MA has no conflicts. KBR was employed by IBM Corporation. AB has no conflicts.
References
- 1.Institute of Medicine (US) Committee on the Future of Primary Care . In: Primary Care: America's Health in a New Era. Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, editors. Washington, DC: National Academies Press; 1996. [PubMed] [Google Scholar]
- 2.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. Oxford, United Kingdom: Oxford University Press, USA; 1998. [Google Scholar]
- 3.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. http://europepmc.org/abstract/MED/16202000 .MILQ409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hensrud DD. Clinical preventive medicine in primary care: background and practice: 1. Rationale and current preventive practices. Mayo Clin Proc. 2000 Feb;75(2):165–72. doi: 10.4065/75.2.165.S0025-6196(11)64189-X [DOI] [PubMed] [Google Scholar]
- 5.Rubin HR. Overcoming barriers to preventive care. J Gen Intern Med. 2000 Jun;15(6):434–6. doi: 10.1046/j.1525-1497.2000.115600.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2000&volume=15&issue=6&spage=434 .jgi115600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petitti DB, Teutsch SM, Barton MB, Sawaya GF, Ockene JK, DeWitt T, U.S. Preventive Services Task Force Update on the methods of the U.S. Preventive Services Task Force: insufficient evidence. Ann Intern Med. 2009 Feb 03;150(3):199–205. doi: 10.7326/0003-4819-150-3-200902030-00010.150/3/199 [DOI] [PubMed] [Google Scholar]
- 7.Privett N, Guerrier S. Estimation of the Time Needed to Deliver the 2020 USPSTF Preventive Care Recommendations in Primary Care. Am J Public Health. 2021 Jan;111(1):145–149. doi: 10.2105/AJPH.2020.305967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010 Mar 08;8(2):108–16. doi: 10.1370/afm.1080. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=20212297 .8/2/108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roland KB, Milliken EL, Rohan EA, DeGroff A, White S, Melillo S, Rorie WE, Signes CC, Young PA. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health Equity. 2017;1(1):61–76. doi: 10.1089/heq.2017.0001. http://europepmc.org/abstract/MED/28905047 .10.1089/heq.2017.0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014 Jul 5;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6.S0140-6736(14)60648-6 [DOI] [PubMed] [Google Scholar]
- 11.Thomas Craig KJ, Morgan LC, Chen C, Michie S, Fusco N, Snowdon JL, Scheufele E, Gagliardi T, Sill S. Systematic review of context-aware digital behavior change interventions to improve health. Transl Behav Med. 2021 May 25;11(5):1037–1048. doi: 10.1093/tbm/ibaa099. http://europepmc.org/abstract/MED/33085767 .5934751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas Craig KJ, Fusco N, Lindsley K, Snowdon J, Willis V, Arriaga Y, Dankwa-Mullan I. Rapid review: Identification of digital health interventions in atherosclerotic-related cardiovascular disease populations to address racial, ethnic, and socioeconomic health disparities. Cardiovascular Digital Health Journal. 2020 Nov;1(3):139–148. doi: 10.1016/j.cvdhj.2020.11.001. doi: 10.1016/j.cvdhj.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp ?, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018 Sep 04;169(7):467. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Office-based Physician Electronic Health Record Adoption. HealthIT. [2022-01-03]. https://www.healthit.gov/data/quickstats/office-based-physician-electronic-health-record-adoption .
- 15.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011 Mar;38(2):65–76. doi: 10.1007/s10488-010-0319-7. http://europepmc.org/abstract/MED/20957426 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009) CEBM. [2020-03-27]. https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- 17.Adams WG, Phillips BD, Bacic JD, Walsh KE, Shanahan CW, Paasche-Orlow MK. Automated conversation system before pediatric primary care visits: a randomized trial. Pediatrics. 2014 Sep 04;134(3):e691–9. doi: 10.1542/peds.2013-3759.peds.2013-3759 [DOI] [PubMed] [Google Scholar]
- 18.Afshar AR, Oldenburg CE, Stewart JM. A Novel Hybrid Fixed and Mobile Ultra-Widefield Imaging Program for Diabetic Teleretinopathy Screening. Ophthalmol Retina. 2019 Jul;3(7):576–579. doi: 10.1016/j.oret.2019.03.007.S2468-6530(19)30010-7 [DOI] [PubMed] [Google Scholar]
- 19.Ahern DK, Parker D, Eaton C, Rafferty C, Wroblewski J, Goldman R. Patient-facing Technology for Identification of COPD in Primary Care. J Innov Health Inform. 2016 Jul 15;23(2):824. doi: 10.14236/jhi.v23i2.824. doi: 10.14236/jhi.v23i2.824. [DOI] [PubMed] [Google Scholar]
- 20.Aikens JE, Trivedi R, Heapy A, Pfeiffer PN, Piette JD. Potential Impact of Incorporating a Patient-Selected Support Person into mHealth for Depression. J Gen Intern Med. 2015 Jun 10;30(6):797–803. doi: 10.1007/s11606-015-3208-7. http://europepmc.org/abstract/MED/25666218 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akenroye AT, Kumthekar AA, Alevizos MK, Mowrey WB, Broder A. Implementing an Electronic Medical Record-Based Reminder for Cardiovascular Risk Screening in Rheumatoid Arthritis. Arthritis Care Res (Hoboken) 2017 May 10;69(5):625–632. doi: 10.1002/acr.22966. [DOI] [PubMed] [Google Scholar]
- 22.Albu JB, Sohler N, Li R, Li X, Young E, Gregg EW, Ross-Degnan D. An Interrupted Time Series Analysis to Determine the Effect of an Electronic Health Record-Based Intervention on Appropriate Screening for Type 2 Diabetes in Urban Primary Care Clinics in New York City. Diabetes Care. 2017 Aug 15;40(8):1058–1064. doi: 10.2337/dc16-2133. http://europepmc.org/abstract/MED/28620094 .dc16-2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aleem S, Torrey W, Duncan M, Hort S, Mecchella J. Depression screening optimization in an academic rural setting. International Journal of Health Care Quality Assurance. 2015;28(7):709–25. doi: 10.1108/ijhcqa-01-2015-0012. [DOI] [PubMed] [Google Scholar]
- 24.Allen NA, Zagarins S, Welch G. Reducing Social Distress for Chronic Disease Patients in Primary Care: An Intervention for Latino Type 2 Diabetes Patients Seen at Community Health Centers. Diabetes Spectr. 2017 Nov 27;30(4):288–296. doi: 10.2337/ds16-0031. http://europepmc.org/abstract/MED/29151719 .288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson D, Villagra VG, Coman E, Ahmed T, Porto A, Jepeal N, Maci G, Teevan B. Reduced Cost Of Specialty Care Using Electronic Consultations For Medicaid Patients. Health Aff (Millwood) 2018 Dec;37(12):2031–2036. doi: 10.1377/hlthaff.2018.05124. [DOI] [PubMed] [Google Scholar]
- 26.Apter AJ, Localio AR, Morales KH, Han X, Perez L, Mullen AN, Rogers M, Klusaritz H, Howell JT, Canales MN, Bryant-Stephens T. Home visits for uncontrolled asthma among low-income adults with patient portal access. J Allergy Clin Immunol. 2019 Sep;144(3):846–853.e11. doi: 10.1016/j.jaci.2019.05.030. http://europepmc.org/abstract/MED/31181221 .S0091-6749(19)30752-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bachhuber MA, O'Grady MA, Chung H, Neighbors CJ, DeLuca J, D'Aloia EM, Diaz A, Cunningham CO. Delivery of screening and brief intervention for unhealthy alcohol use in an urban academic Federally Qualified Health Center. Addict Sci Clin Pract. 2017 Dec 07;12(1):33. doi: 10.1186/s13722-017-0100-2. https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-017-0100-2 .10.1186/s13722-017-0100-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bae J, Ford E, Kharrazi H, Huerta T. Electronic medical record reminders and smoking cessation activities in primary care. Addict Behav. 2018 Feb;77:203–209. doi: 10.1016/j.addbeh.2017.10.009. doi: 10.1016/j.addbeh.2017.10.009.S0306-4603(17)30375-1 [DOI] [PubMed] [Google Scholar]
- 29.Bae J, Ford EW, Wu S, Huerta T. Electronic reminder's role in promoting human papillomavirus vaccine use. Am J Manag Care. 2017 Nov 01;23(11):e353–e359. https://www.ajmc.com/pubMed.php?pii=87318 .87318 [PubMed] [Google Scholar]
- 30.Baker JW, Forkum W, McNeal J. Utilizing clinical video telehealth to improve access and optimize pharmacists' role in diabetes management. J Am Pharm Assoc (2003) 2019 Apr;59(2S):S63–S66. doi: 10.1016/j.japh.2019.01.004.S1544-3191(19)30012-3 [DOI] [PubMed] [Google Scholar]
- 31.Bar-Shain DS, Stager MM, Runkle AP, Leon JB, Kaelber DC. Direct messaging to parents/guardians to improve adolescent immunizations. J Adolesc Health. 2015 May;56(5 Suppl):S21–6. doi: 10.1016/j.jadohealth.2014.11.023. doi: 10.1016/j.jadohealth.2014.11.023.S1054-139X(14)00764-2 [DOI] [PubMed] [Google Scholar]
- 32.Barclay C, Viswanathan M, Ratner S, Tompkins J, Jonas DE. Implementing Evidence-Based Screening and Counseling for Unhealthy Alcohol Use with Epic-Based Electronic Health Record Tools. Jt Comm J Qual Patient Saf. 2019 Aug;45(8):566–574. doi: 10.1016/j.jcjq.2019.05.009. https://linkinghub.elsevier.com/retrieve/pii/S1553-7250(19)30101-1 .S1553-7250(19)30101-1 [DOI] [PubMed] [Google Scholar]
- 33.Barton AB, Okorodudu DE, Bosworth HB, Crowley MJ. Clinical Inertia in a Randomized Trial of Telemedicine-Based Chronic Disease Management: Lessons Learned. Telemed J E Health. 2018 Oct;24(10):742–748. doi: 10.1089/tmj.2017.0184. [DOI] [PubMed] [Google Scholar]
- 34.Beasley JM, Kirshner L, Wylie-Rosett J, Sevick MA, DeLuca L, Chodosh J. BRInging the Diabetes prevention program to GEriatric populations (BRIDGE): a feasibility study. Pilot Feasibility Stud. 2019 Nov 11;5(1):129. doi: 10.1186/s40814-019-0513-7. https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-019-0513-7 .513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bennett GG, Steinberg D, Askew S, Levine E, Foley P, Batch BC, Svetkey LP, Bosworth HB, Puleo EM, Brewer A, DeVries A, Miranda H. Effectiveness of an App and Provider Counseling for Obesity Treatment in Primary Care. American Journal of Preventive Medicine. 2018 Dec;55(6):777–786. doi: 10.1016/J.AMEPRE.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Benson GA, Sidebottom A, Sillah A, Boucher JL, Miedema MD, Knickelbine T, VanWormer JJ. Reach and effectiveness of the HeartBeat Connections telemedicine pilot program. J Telemed Telecare. 2017 Feb 13;24(3):216–223. doi: 10.1177/1357633x17692723. [DOI] [PubMed] [Google Scholar]
- 37.Berkley H, Barnes M, Carnahan D, Hayhurst J, Bockhorst A, Neville J. Public Health Surveillance via Template Management in Electronic Health Records: Tri-Service Workflow's Rapid Response to an Infectious Disease Crisis. Military Medicine. 2017 Mar;182(S1):340–345. doi: 10.7205/milmed-d-16-00128. [DOI] [PubMed] [Google Scholar]
- 38.Bhat S, Kroehl ME, Trinkley KE, Chow Z, Heath LJ, Billups SJ, Loeb DF. Evaluation of a Clinical Pharmacist-Led Multidisciplinary Antidepressant Telemonitoring Service in the Primary Care Setting. Popul Health Manag. 2018 Oct;21(5):366–372. doi: 10.1089/pop.2017.0144. http://europepmc.org/abstract/MED/29211661 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bondurant KL, Wheeler JG, Bursac Z, Holmes T, Tilford JM. Comparison of Office-Based Versus Outsourced Immunization Recall Services. Clin Pediatr (Phila) 2017 Jun;56(6):555–563. doi: 10.1177/0009922816673307.0009922816673307 [DOI] [PubMed] [Google Scholar]
- 40.Bose-Brill S, Feeney M, Prater L, Miles L, Corbett A, Koesters S. Validation of a Novel Electronic Health Record Patient Portal Advance Care Planning Delivery System. J Med Internet Res. 2018 Jun 26;20(6):e208. doi: 10.2196/jmir.9203. https://www.jmir.org/2018/6/e208/ v20i6e208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bose-Brill S, Kretovics M, Ballenger T, Modan G, Lai A, Belanger L, Koesters S, Pressler-Vydra T, Holloman C, Wills C. Testing of a tethered personal health record framework for early end-of-life discussions. Am J Manag Care. 2016 Jul 01;22(7):e258–63. https://www.ajmc.com/pubMed.php?pii=86746 .86746 [PubMed] [Google Scholar]
- 42.Bouskill K, Smith-Morris C, Bresnick G, Cuadros J, Pedersen ER. Blind spots in telemedicine: a qualitative study of staff workarounds to resolve gaps in diabetes management. BMC Health Serv Res. 2018 Aug 07;18(1):617. doi: 10.1186/s12913-018-3427-9. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3427-9 .10.1186/s12913-018-3427-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brantley AD, Page KM, Zack B, Friedrich KR, Wendell D, Robinson WT, Gruber D. Making the Connection: Using Videoconferencing to Increase Linkage to Care for Incarcerated Persons Living with HIV Post-release. AIDS Behav. 2019 Jan;23(Suppl 1):32–40. doi: 10.1007/s10461-018-2115-4.10.1007/s10461-018-2115-4 [DOI] [PubMed] [Google Scholar]
- 44.Bratic JS, Cunningham RM, Belleza-Bascon B, Watson SK, Guffey D, Boom JA. Longitudinal Evaluation of Clinical Decision Support to Improve Influenza Vaccine Uptake in an Integrated Pediatric Health Care Delivery System, Houston, Texas. Appl Clin Inform. 2019 Oct;10(5):944–951. doi: 10.1055/s-0039-3400748. http://europepmc.org/abstract/MED/31860114 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brayboy LM, Sepolen A, Mezoian T, Schultz L, Landgren-Mills BS, Spencer N, Wheeler C, Clark MA. Girl Talk: A Smartphone Application to Teach Sexual Health Education to Adolescent Girls. J Pediatr Adolesc Gynecol. 2017 Feb;30(1):23–28. doi: 10.1016/j.jpag.2016.06.011. http://europepmc.org/abstract/MED/27393638 .S1083-3188(16)30092-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Breitenstein SM, Laurent S, Pabalan L, Risser HJ, Roper P, Saba MT, Schoeny M. Implementation findings from an effectiveness-implementation trial of tablet-based parent training in pediatric primary care. Fam Syst Health. 2019 Dec;37(4):282–290. doi: 10.1037/fsh0000447. http://europepmc.org/abstract/MED/31621349 .2019-62241-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown CM, Perkins J, Blust A, Kahn RS. A neighborhood-based approach to population health in the pediatric medical home. J Community Health. 2015 Feb 13;40(1):1–11. doi: 10.1007/s10900-014-9885-z. [DOI] [PubMed] [Google Scholar]
- 48.Brunette MF, Gunn W, Alvarez H, Finn PC, Geiger P, Ferron JC, McHugo GJ. A pre-post pilot study of a brief, web-based intervention to engage disadvantaged smokers into cessation treatment. Addict Sci Clin Pract. 2015 Feb 01;10:3. doi: 10.1186/s13722-015-0026-5. https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-015-0026-5 .s13722-015-0026-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buist DSM, Knight Ross N, Reid RJ, Grossman DC. Electronic health risk assessment adoption in an integrated healthcare system. Am J Manag Care. 2014;20(1):62–9. https://www.ajmc.com/pubMed.php?pii=85342 .85342 [PubMed] [Google Scholar]
- 50.Bulbin D, Denio AE, Berger A, Brown J, Maynard C, Sharma T, Kirchner HL, Ayoub WT. Improved Gout Outcomes in Primary Care Using a Novel Disease Management Program: A Pilot Study. Arthritis Care Res (Hoboken) 2018 Nov;70(11):1679–1685. doi: 10.1002/acr.23544. [DOI] [PubMed] [Google Scholar]
- 51.Burdick T, Kessler R. Development and use of a clinical decision support tool for behavioral health screening in primary care clinics. Appl Clin Inform. 2017 Dec 21;08(02):412–429. doi: 10.4338/aci-2016-04-ra-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carswell SB, Mitchell SG, Gryczynski J, Lertch E. Computerizing NIAAA's Best Practices for Youth Screening and Brief Intervention: A Proof-of-Concept Pilot Study of an Automated Alcohol Screening and Intervention Resource Tool. J Drug Educ. 2020 Dec 16;49(1-2):3–14. doi: 10.1177/0047237919894960. [DOI] [PubMed] [Google Scholar]
- 53.Cawthon C, Mion LC, Willens DE, Roumie CL, Kripalani S. Implementing Routine Health Literacy Assessment in Hospital and Primary Care Patients. The Joint Commission Journal on Quality and Patient Safety. 2014 Feb;40(2):68–76. doi: 10.1016/s1553-7250(14)40008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chambers EC, Wylie-Rosett J, Blank AE, Ouziel J, Hollingsworth N, Riley RW, Selwyn PA. Increasing Referrals to a YMCA-Based Diabetes Prevention Program: Effects of Electronic Referral System Modification and Provider Education in Federally Qualified Health Centers. Prev Chronic Dis. 2015 Nov 05;12:E189. doi: 10.5888/pcd12.150294. https://www.cdc.gov/pcd/issues/2015/15_0294.htm .E189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chouteau WA, Allen SR. Implementation of a Portable Medical Summary for Adolescents and Young Adults With Medical Complexity in Transition to Adult Health Care. J Pediatr Nurs. 2019;48:35–41. doi: 10.1016/j.pedn.2019.05.012.S0882-5963(18)30597-9 [DOI] [PubMed] [Google Scholar]
- 56.Chung E, Gubernick R, LaNoue M, Abatemarco D. Child Abuse and Neglect Risk Assessment: Quality Improvement in a Primary Care Setting. Acad Pediatr. 2019 Mar;19(2):227–235. doi: 10.1016/j.acap.2018.09.011. doi: 10.1016/j.acap.2018.09.011.S1876-2859(18)30640-5 [DOI] [PubMed] [Google Scholar]
- 57.Church E, Banks R, Wilson B, Arfons L, Perez F, Jump R. Improving pneumococcal vaccine uptake in veterans with chronic lymphocytic leukemia through a virtual clinic. Curr Oncol. 2018 Feb 01;25(1):e95–e98. doi: 10.3747/co.25.3756. https://www.mdpi.com/resolver?pii=conc-25-e95 .conc-25-e95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Coker TR, Porras-Javier L, Zhang L, Soares N, Park C, Patel A, Tang L, Chung PJ, Zima BT. A Telehealth-Enhanced Referral Process in Pediatric Primary Care: A Cluster Randomized Trial. Pediatrics. 2019 Mar 15;143(3):e20182738. doi: 10.1542/peds.2018-2738.peds.2018-2738 [DOI] [PubMed] [Google Scholar]
- 59.No authors listed Collins BN, Lepore SJ, Winickoff JP, et al. An Office-Initiated Multilevel Intervention for Tobacco Smoke Exposure: A Randomized Trial. 2018;141(Suppl 1):S75-S86. Pediatrics. 2018 Jun;141(6):e20180894. doi: 10.1542/peds.2018-0894. http://europepmc.org/abstract/MED/29853625 .peds.2018-0894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Condren M, Honey BL, Carter SM, Ngo N, Landsaw J, Bryant C, Gillaspy S. Influence of a systems-based approach to prescribing errors in a pediatric resident clinic. Acad Pediatr. 2014 Sep;14(5):485–90. doi: 10.1016/j.acap.2014.03.018.S1876-2859(14)00101-6 [DOI] [PubMed] [Google Scholar]
- 61.Conklin TM. Addressing alcohol misuse in primary care. J Am Assoc Nurse Pract. 2020 Aug;32(8):583–588. doi: 10.1097/jxx.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 62.Cordova D, Alers-Rojas F, Lua FM, Bauermeister J, Nurenberg R, Ovadje L, Fessler K, Delva J, Salas-Wright CP, Council YL. The Usability and Acceptability of an Adolescent mHealth HIV/STI and Drug Abuse Preventive Intervention in Primary Care. Behav Med. 2018 May 25;44(1):36–47. doi: 10.1080/08964289.2016.1189396. http://europepmc.org/abstract/MED/27223646 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Curtis L, Mullen R, Russell A, Fata A, Bailey S, Makoul G, Wolf MS. An efficacy trial of an electronic health record-based strategy to inform patients on safe medication use: The role of written and spoken communication. Patient Educ Couns. 2016 Sep;99(9):1489–95. doi: 10.1016/j.pec.2016.07.004. http://europepmc.org/abstract/MED/27444235 .S0738-3991(16)30299-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dahne J, Lejuez CW, Diaz VA, Player MS, Kustanowitz J, Felton JW, Carpenter MJ. Pilot Randomized Trial of a Self-Help Behavioral Activation Mobile App for Utilization in Primary Care. Behav Ther. 2019 Jul;50(4):817–827. doi: 10.1016/j.beth.2018.12.003. http://europepmc.org/abstract/MED/31208690 .S0005-7894(18)30157-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dean KM, Hatfield LA, Jena AB, Cristman D, Flair M, Kator K, Nudd G, Grabowski DC. Preliminary Data on a Care Coordination Program for Home Care Recipients. J Am Geriatr Soc. 2016 Sep 10;64(9):1900–3. doi: 10.1111/jgs.14351. [DOI] [PubMed] [Google Scholar]
- 66.DeCamp LR, Godage SK, Valenzuela Araujo D, Dominguez Cortez J, Wu L, Psoter KJ, Quintanilla K, Rivera Rodríguez T, Polk S. A Texting Intervention in Latino Families to Reduce ED Use: A Randomized Trial. Pediatrics. 2020 Jan;145(1) doi: 10.1542/peds.2019-1405. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=31879276 .peds.2019-1405 [DOI] [PubMed] [Google Scholar]
- 67.DeSantes K, Dodge A, Eickhoff J, Peterson AL. Improving Universal Pediatric Lipid Screening. J Pediatr. 2017 Sep;188(5):87–90. doi: 10.1016/j.jpeds.2017.05.030.S0022-3476(17)30651-0 [DOI] [PubMed] [Google Scholar]
- 68.Devries J, Rafie S, Polston G. Implementing an overdose education and naloxone distribution program in a health system. J Am Pharm Assoc (2003) 2017 Apr;57(2S):S154–S160. doi: 10.1016/j.japh.2017.01.002.S1544-3191(17)30002-X [DOI] [PubMed] [Google Scholar]
- 69.Dexter AS, Pope JF, Erickson D, Fontenot C, Ollendike E, Walker E. Cooking Education Improves Cooking Confidence and Dietary Habits in Veterans. Diabetes Educ. 2019 Aug;45(4):442–449. doi: 10.1177/0145721719848429. [DOI] [PubMed] [Google Scholar]
- 70.Diaz MCG, Wysocki T, Crutchfield JH, Franciosi JP, Werk LN. Provider-Focused Intervention to Promote Comprehensive Screening for Adolescent Idiopathic Scoliosis by Primary Care Pediatricians. Am J Med Qual. 2019;34(2):182–188. doi: 10.1177/1062860618792667. [DOI] [PubMed] [Google Scholar]
- 71.Dischinger HR, Cheng E, Mann AD, Grueber TM, Hawk S, Davis LA, Prochazka AV, Hutt E, Caplan L. Decisional support to prevent adverse drug reactions of long latency: pilot randomized controlled intervention for glucocorticoid-induced diabetes. J Eval Clin Pract. 2015 Aug 07;21(4):614–9. doi: 10.1111/jep.12351. [DOI] [PubMed] [Google Scholar]
- 72.Dixon BE, Simonaitis L, Perkins SM, Wright A, Middleton B. Measuring agreement between decision support reminders: the cloud vs. the local expert. BMC Med Inform Decis Mak. 2014 Apr 10;14:31. doi: 10.1186/1472-6947-14-31. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-14-31 .1472-6947-14-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dombkowski KJ, Cowan AE, Reeves SL, Foley MR, Dempsey AF. The impacts of email reminder/recall on adolescent influenza vaccination. Vaccine. 2017 May 25;35(23):3089–3095. doi: 10.1016/j.vaccine.2017.04.033.S0264-410X(17)30511-X [DOI] [PubMed] [Google Scholar]
- 74.Donovan JL, Kanaan AO, Gurwitz JH, Tjia J, Cutrona SL, Garber L, Preusse P, Field TS. A Pilot Health Information Technology-Based Effort to Increase the Quality of Transitions From Skilled Nursing Facility to Home: Compelling Evidence of High Rate of Adverse Outcomes. J Am Med Dir Assoc. 2016 Apr 01;17(4):312–7. doi: 10.1016/j.jamda.2015.11.008.S1525-8610(15)00708-2 [DOI] [PubMed] [Google Scholar]
- 75.Duquaine D, Farley SM, Sacks R, Mandel-Ricci J, Silfen SL, Shih SC. Designing a quality improvement program with electronic health records: New York City's Health eQuits. Am J Med Qual. 2015 Jan 29;30(2):141–8. doi: 10.1177/1062860613520406.1062860613520406 [DOI] [PubMed] [Google Scholar]
- 76.Dwinnells R, Misik L. An Integrative Behavioral Health Care Model Using Automated SBIRT and Care Coordination in Community Health Care. J Prim Care Community Health. 2017 Oct 16;8(4):300–304. doi: 10.1177/2150131917740245. https://journals.sagepub.com/doi/10.1177/2150131917740245?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eckman MH, Lip GY, Wise RE, Speer B, Sullivan M, Walker N, Kissela B, Flaherty ML, Kleindorfer D, Baker P, Ireton R, Hoskins D, Harnett BM, Aguilar C, Leonard A, Arduser L, Steen D, Costea A, Kues J. Using an Atrial Fibrillation Decision Support Tool for Thromboprophylaxis in Atrial Fibrillation: Effect of Sex and Age. J Am Geriatr Soc. 2016 May 25;64(5):1054–60. doi: 10.1111/jgs.14099. http://europepmc.org/abstract/MED/27225358 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eckman MH, Lip GY, Wise RE, Speer B, Sullivan M, Walker N, Kissela B, Flaherty ML, Kleindorfer D, Baker P, Ireton R, Hoskins D, Harnett BM, Aguilar C, Leonard AC, Arduser L, Steen D, Costea A, Kues J. Impact of an Atrial Fibrillation Decision Support Tool on thromboprophylaxis for atrial fibrillation. Am Heart J. 2016 Jun;176:17–27. doi: 10.1016/j.ahj.2016.02.009.S0002-8703(16)00056-9 [DOI] [PubMed] [Google Scholar]
- 79.Emerson JF, Welch M, Rossman WE, Carek S, Ludden T, Templin M, Moore CG, Tapp H, Dulin M, McWilliams A. A Multidisciplinary Intervention Utilizing Virtual Communication Tools to Reduce Health Disparities: A Pilot Randomized Controlled Trial. Int J Environ Res Public Health. 2015 Dec 22;13(1):ijerph13010031. doi: 10.3390/ijerph13010031. https://www.mdpi.com/resolver?pii=ijerph13010031 .ijerph13010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Engel CC, Litz B, Magruder KM, Harper E, Gore K, Stein N, Yeager D, Liu X, Coe TR. Delivery of self training and education for stressful situations (DESTRESS-PC): a randomized trial of nurse assisted online self-management for PTSD in primary care. Gen Hosp Psychiatry. 2015 Jul;37(4):323–8. doi: 10.1016/j.genhosppsych.2015.04.007. https://linkinghub.elsevier.com/retrieve/pii/S0163-8343(15)00074-2 .S0163-8343(15)00074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fanizza FA, Ruisinger JF, Prohaska ES, Melton BL. Integrating a health information exchange into a community pharmacy transitions of care service. J Am Pharm Assoc (2003) 2018;58(4):442–449. doi: 10.1016/j.japh.2018.02.012.S1544-3191(18)30077-3 [DOI] [PubMed] [Google Scholar]
- 82.Federman A, Sarzynski E, Brach C, Francaviglia P, Jacques J, Jandorf L, Munoz AS, Wolf M, Kannry J. Challenges optimizing the after visit summary. Int J Med Inform. 2018 Dec;120:14–19. doi: 10.1016/j.ijmedinf.2018.09.009. http://europepmc.org/abstract/MED/30409339 .S1386-5056(18)30359-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Federman A, Kil N, Kannry J, Andreopolous E, Toribio W, Lyons J. An Electronic Health Record-based Intervention to Promote Hepatitis C Virus Testing Among Adults Born Between 1945 and 1965: a Cluster-randomized Trial. Medical Care. 2017;55(6):590–597. doi: 10.1097/mlr.0000000000000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fiks AG, DuRivage N, Mayne SL, Finch S, Ross ME, Giacomini K, Suh A, McCarn B, Brandt E, Karavite D, Staton EW, Shone LP, McGoldrick V, Noonan K, Miller D, Lehmann CU, Pace WD, Grundmeier RW. Adoption of a Portal for the Primary Care Management of Pediatric Asthma: A Mixed-Methods Implementation Study. J Med Internet Res. 2016 Jun 29;18(6):e172. doi: 10.2196/jmir.5610. https://www.jmir.org/2016/6/e172/ v18i6e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fiks AG, Luan X, Mayne SL. Improving HPV Vaccination Rates Using Maintenance-of-Certification Requirements. Pediatrics. 2016 Mar 03;137(3):e20150675. doi: 10.1542/peds.2015-0675.peds.2015-0675 [DOI] [PubMed] [Google Scholar]
- 86.Fiore M, Adsit R, Zehner M, McCarthy D, Lundsten S, Hartlaub P, Mahr T, Gorrilla A, Skora A, Baker T. An electronic health record-based interoperable eReferral system to enhance smoking Quitline treatment in primary care. J Am Med Inform Assoc. 2019 Aug 01;26(8-9):778–786. doi: 10.1093/jamia/ocz044. http://europepmc.org/abstract/MED/31089727 .5489464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fitzpatrick SL, Dickins K, Avery E, Ventrelle J, Shultz A, Kishen E, Rothschild S. Effect of an obesity best practice alert on physician documentation and referral practices. Transl Behav Med. 2017 Dec 26;7(4):881–890. doi: 10.1007/s13142-017-0514-0. http://europepmc.org/abstract/MED/28653221 .10.1007/s13142-017-0514-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Flocke S, Seeholzer E, Lewis S, Gill I, Ordillas E, Rose J, Albert E, Love TE, Kaelber DC. Designing for Sustainability: An Approach to Integrating Staff Role Changes and Electronic Health Record Functionality Within Safety-Net Clinics to Address Provision of Tobacco Cessation Care. Jt Comm J Qual Patient Saf. 2019 Dec;45(12):798–807. doi: 10.1016/j.jcjq.2019.09.003. doi: 10.1016/j.jcjq.2019.09.003.S1553-7250(19)30391-5 [DOI] [PubMed] [Google Scholar]
- 89.Flynn DM, Eaton LH, McQuinn H, Alden A, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. TelePain: Primary Care Chronic Pain Management through Weekly Didactic and Case-based Telementoring. Contemp Clin Trials Commun. 2017 Dec;8:162–166. doi: 10.1016/j.conctc.2017.10.004. http://europepmc.org/abstract/MED/29497708 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Frank JW, Carey EP, Fagan KM, Aron DC, Todd-Stenberg J, Moore BA, Kerns RD, Au DH, Ho PM, Kirsh SR. Evaluation of a telementoring intervention for pain management in the Veterans Health Administration. Pain Med. 2015 Jun;16(6):1090–100. doi: 10.1111/pme.12715. [DOI] [PubMed] [Google Scholar]
- 91.Fried TR, Niehoff KM, Street RL, Charpentier PA, Rajeevan N, Miller PL, Goldstein MK, O'Leary JR, Fenton BT. Effect of the Tool to Reduce Inappropriate Medications on Medication Communication and Deprescribing. J Am Geriatr Soc. 2017 Oct;65(10):2265–2271. doi: 10.1111/jgs.15042. http://europepmc.org/abstract/MED/28804870 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ganz DA, Kim S, Zingmond DS, Ramirez KD, Roth CP, Jennings LA, Mori T, Keeler EB, Wenger NS, Reuben DB. Effect of a falls quality improvement program on serious fall-related injuries. J Am Geriatr Soc. 2015 Jan 17;63(1):63–70. doi: 10.1111/jgs.13154. http://europepmc.org/abstract/MED/25597558 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Geboy AG, Nichols WL, Fernandez SJ, Desale S, Basch P, Fishbein DA. Leveraging the electronic health record to eliminate hepatitis C: Screening in a large integrated healthcare system. PLoS One. 2019 May 23;14(5):e0216459. doi: 10.1371/journal.pone.0216459. https://dx.plos.org/10.1371/journal.pone.0216459 .PONE-D-18-31217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gill JM, Chen YX, Grimes A, Klinkman MS. Using electronic health record-based tools to screen for bipolar disorder in primary care patients with depression. J Am Board Fam Med. 2012 May 08;25(3):283–90. doi: 10.3122/jabfm.2012.03.110217. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=22570391 .25/3/283 [DOI] [PubMed] [Google Scholar]
- 95.Gold J, Reyes-Gastelum D, Turner J, Pediatric Asthma Quality Team. Davies HD. A quality improvement study using fishbone analysis and an electronic medical records intervention to improve care for children with asthma. Am J Med Qual. 2014;29(1):70–7. doi: 10.1177/1062860613484171.1062860613484171 [DOI] [PubMed] [Google Scholar]
- 96.Goleman MJ, Dolce M, Morack J. Quality Improvement Initiative to Improve Human Papillomavirus Vaccine Initiation at 9 Years of Age. Acad Pediatr. 2018 Sep;18(7):769–775. doi: 10.1016/j.acap.2018.05.005.S1876-2859(18)30309-7 [DOI] [PubMed] [Google Scholar]
- 97.Grant RW, Ashburner JM, Jernigan MC, Chang J, Borowsky LH, Chang Y, Atlas SJ. Randomized trial of a health IT tool to support between-visit-based laboratory monitoring for chronic disease medication prescriptions. J Gen Intern Med. 2015 May 6;30(5):619–25. doi: 10.1007/s11606-014-3152-y. http://europepmc.org/abstract/MED/25560319 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Greene BR, McManus K, Redmond SJ, Caulfield B, Quinn CC. Digital assessment of falls risk, frailty, and mobility impairment using wearable sensors. npj Digit. Med. 2019 Dec 11;2(1):125. doi: 10.1038/s41746-019-0204-z. http://europepmc.org/abstract/MED/31840096 .204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gustafson DH, McTavish FM, Chih M, Atwood AK, Johnson RA, Boyle MG, Levy MS, Driscoll H, Chisholm SM, Dillenburg L, Isham A, Shah D. A Smartphone Application to Support Recovery From Alcoholism. JAMA Psychiatry. 2014 May 01;71(5):566–72. doi: 10.1001/jamapsychiatry.2013.4642. http://europepmc.org/abstract/MED/24671165 .1847578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ha B, O’Sullivan DL, Diamond CA, Plumb AJ, Sleeth JS, Greer FR, Kling PJ. Improving Rates of Screening for Anemia in Infancy. Clin Pediatr (Phila) 2017 Nov 28;57(9):1064–1068. doi: 10.1177/0009922817744608. [DOI] [PubMed] [Google Scholar]
- 101.Haas JS, Baer HJ, Eibensteiner K, Klinger EV, St. Hubert S, Getty G, Brawarsky P, Orav EJ, Onega T, Tosteson AN, Bates DW, Colditz G. A Cluster Randomized Trial of a Personalized Multi-Condition Risk Assessment in Primary Care. American Journal of Preventive Medicine. 2017 Jan;52(1):100–105. doi: 10.1016/j.amepre.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Haas JS, Linder JA, Park ER, Gonzalez I, Rigotti NA, Klinger EV, Kontos EZ, Zaslavsky AM, Brawarsky P, Marinacci LX, St Hubert S, Fleegler EW, Williams DR. Proactive Tobacco Cessation Outreach to Smokers of Low Socioeconomic Status. JAMA Intern Med. 2015 Feb 01;175(2):218–26. doi: 10.1001/jamainternmed.2014.6674. http://europepmc.org/abstract/MED/25506771 .2020290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Halterman JS, Fagnano M, Tajon RS, Tremblay P, Wang H, Butz A, Perry TT, McConnochie KM. Effect of the School-Based Telemedicine Enhanced Asthma Management (SB-TEAM) Program on Asthma Morbidity. JAMA Pediatr. 2018 Mar 01;172(3):e174938. doi: 10.1001/jamapediatrics.2017.4938. http://europepmc.org/abstract/MED/29309483 .2667559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hark L, Acito M, Adeghate J, Henderer J, Okudolo J, Malik K, Molineaux J, Eburuoh R, Zhan T, Katz LJ. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: Ocular Findings at Two Health Centers. Journal of Health Care for the Poor and Underserved. 2018;29(4):1400–1415. doi: 10.1353/hpu.2018.0103. [DOI] [PubMed] [Google Scholar]
- 105.Hark LA, Katz LJ, Myers JS, Waisbourd M, Johnson D, Pizzi LT, Leiby BE, Fudemberg SJ, Mantravadi AV, Henderer JD, Zhan T, Molineaux J, Doyle V, Divers M, Burns C, Murchison AP, Reber S, Resende A, Bui TDV, Lee J, Crews JE, Saaddine JB, Lee PP, Pasquale LR, Haller JA. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: Methods and Screening Results. American Journal of Ophthalmology. 2017 Sep;181:114–124. doi: 10.1016/j.ajo.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 106.Hark LA, Myers JS, Pasquale LR, Razeghinejad MR, Maity A, Zhan T, Hegarty SE, Leiby BE, Waisbourd M, Burns C, Divers M, Molineaux J, Henderer JD, Haller JA, Katz LJ. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study. Journal of Glaucoma. 2019;28(4):294–301. doi: 10.1097/ijg.0000000000001207. [DOI] [PubMed] [Google Scholar]
- 107.Hatef E, Alexander M, Vanderver B, Fagan P, Albert M. Assessment of annual diabetic eye examination using telemedicine technology among underserved patients in primary care setting. Middle East Afr J Ophthalmol. 2017;24(4):207. doi: 10.4103/meajo.meajo_19_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hay JW, Lee P, Jin H, Guterman JJ, Gross-Schulman S, Ell K, Wu S. Cost-Effectiveness of a Technology-Facilitated Depression Care Management Adoption Model in Safety-Net Primary Care Patients with Type 2 Diabetes. Value in Health. 2018 May;21(5):561–568. doi: 10.1016/j.jval.2017.11.005.S1098-3015(17)33714-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hayek S, Nieva R, Corrigan F, Zhou A, Mudaliar U, Mays D, Massoomi M, Ilksoy N. End-of-Life Care Planning: Improving Documentation of Advance Directives in the Outpatient Clinic Using Electronic Medical Records. Journal of Palliative Medicine. 2014 Dec;17(12):1348–1352. doi: 10.1089/jpm.2013.0684. [DOI] [PubMed] [Google Scholar]
- 110.Hess R, Fischer GS, Sullivan SM, Dong X, Weimer M, Zeith C, Clark S, Roberts MS. Patterns of Response to Patient-Centered Decision Support Through a Personal Health Record. Telemedicine and e-Health. 2014 Nov;20(11):984–989. doi: 10.1089/tmj.2013.0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Heyworth L, Kleinman K, Oddleifson S, Bernstein L, Frampton J, Lehrer M, Salvato K, Weiss TW, Simon SR, Connelly M. Comparison of interactive voice response, patient mailing, and mailed registry to encourage screening for osteoporosis: a randomized controlled trial. Osteoporos Int. 2014 Feb 25;25(5):1519–1526. doi: 10.1007/s00198-014-2629-1. [DOI] [PubMed] [Google Scholar]
- 112.Hojat L, Avery A, Greco PJ, Kaelber DC. Doubling Hepatitis C Virus Screening in Primary Care Using Advanced Electronic Health Record Tools—A Non-Randomized Controlled Trial. J GEN INTERN MED. 2019 Dec 02;35(2):498–504. doi: 10.1007/s11606-019-05536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Honaker SM, Dugan T, Daftary A, Davis S, Saha C, Baye F, Freeman E, Downs SM. Unexplained Practice Variation in Primary Care Providers' Concern for Pediatric Obstructive Sleep Apnea. Academic Pediatrics. 2018 May;18(4):418–424. doi: 10.1016/j.acap.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 114.Honaker SM, Street A, Daftary AS, Downs SM. The Use of Computer Decision Support for Pediatric Obstructive Sleep Apnea Detection in Primary Care. Journal of Clinical Sleep Medicine. 2019 Mar 15;15(03):453–462. doi: 10.5664/jcsm.7674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hoopes M, Angier H, Raynor L, Suchocki A, Muench J, Marino M, Rivera P, Huguet N. Development of an algorithm to link electronic health record prescriptions with pharmacy dispense claims. Journal of the American Medical Informatics Association. 2018;25(10):1322–30. doi: 10.1093/jamia/ocy095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jain M, Rich N, Ahn C, Turner B, Sanders J, Adamson B, Quirk L, Perryman P, Santini NO, Singal AG. Evaluation of a Multifaceted Intervention to Reduce Health Disparities in Hepatitis C Screening: A Pre‐Post Analysis. Hepatology. 2019 May 31;:A. doi: 10.1002/hep.30638. doi: 10.1002/hep.30638. [DOI] [PubMed] [Google Scholar]
- 117.Jani PD, Forbes L, Choudhury A, Preisser JS, Viera AJ, Garg S. Evaluation of Diabetic Retinal Screening and Factors for Ophthalmology Referral in a Telemedicine Network. JAMA Ophthalmol. 2017 Jul 01;135(7):706. doi: 10.1001/jamaophthalmol.2017.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jenssen BP, Bryant-Stephens T, Leone FT, Grundmeier RW, Fiks AG. Clinical Decision Support Tool for Parental Tobacco Treatment in Primary Care. Pediatrics. 2016 Apr 14;137(5):e20154185. doi: 10.1542/peds.2015-4185. [DOI] [PubMed] [Google Scholar]
- 119.Jenssen BP, Muthu N, Kelly MK, Baca H, Shults J, Grundmeier RW, Fiks AG. Parent eReferral to Tobacco Quitline: A Pragmatic Randomized Trial in Pediatric Primary Care. American Journal of Preventive Medicine. 2019 Jul;57(1):32–40. doi: 10.1016/j.amepre.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jetelina KK, Woodson TT, Gunn R, Muller B, Clark KD, DeVoe JE, Balasubramanian BA, Cohen DJ. Evaluation of an Electronic Health Record (EHR) Tool for Integrated Behavioral Health in Primary Care. J Am Board Fam Med. 2018 Sep 10;31(5):712–723. doi: 10.3122/jabfm.2018.05.180041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jones Q, Johnston B, Biola H, Gomez S, Crowder C. Implementing standardized substance use disorder screening in primary care. Journal of the American Academy of Physician Assistants. 2018;31(10):42–5. doi: 10.1097/01.jaa.0000795888.70937.34. [DOI] [PubMed] [Google Scholar]
- 122.Kamo N, Williams B, Smith D, Blackmore C. Improving the Electronic Capture of Advance Care Directives in a Healthcare Delivery System. J Am Geriatr Soc. 2017 Feb 09;65(5):973–979. doi: 10.1111/jgs.14695. doi: 10.1111/jgs.14695. [DOI] [PubMed] [Google Scholar]
- 123.Kapoor A, Amroze A, Golden J, Crawford S, O'Day K, Elhag R, Nagy A, Lubitz SA, Saczynski JS, Mathew J, McManus DD. SUPPORT‐AF: Piloting a Multi‐Faceted, Electronic Medical Record‐Based Intervention to Improve Prescription of Anticoagulation. JAHA. 2018 Sep 04;7(17):e009946. doi: 10.1161/jaha.118.009946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Karas D, Sondike S, Fitzgibbon J, Redding M, Brown M. Using a Clinical Decision Support Tool to Increase Chlamydia Screening Across a Large Primary Care Pediatric Network. Clin Pediatr (Phila) 2018 Sep 28;57(14):1638–1641. doi: 10.1177/0009922818803397. [DOI] [PubMed] [Google Scholar]
- 125.Kavanagh P, Sobota A, McClure E, Sprinz P, Adams W. Using an Electronic Health Record-Based Registry to Improve Pediatric Sickle Cell Care. Journal of Clinical Outcomes Management. 2014;21(4):159–68. [Google Scholar]
- 126.Keck JW, Roper KL, Hieronymus LB, Thomas AR, Huang Z, Westgate PM, Fowlkes JL, Cardarelli R. Primary Care Cluster RCT to Increase Diabetes Prevention Program Referrals. American Journal of Preventive Medicine. 2020 Jul;59(1):79–87. doi: 10.1016/j.amepre.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kershaw C, Taylor JL, Horowitz G, Brockmeyer D, Libman H, Kriegel G, Ngo L. Use of an electronic medical record reminder improves HIV screening. BMC Health Serv Res. 2018 Jan 10;18(1):14. doi: 10.1186/s12913-017-2824-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kim RH, Day SC, Small DS, Snider CK, Rareshide CAL, Patel MS. Variations in Influenza Vaccination by Clinic Appointment Time and an Active Choice Intervention in the Electronic Health Record to Increase Influenza Vaccination. JAMA Netw Open. 2018 Sep 14;1(5):e181770. doi: 10.1001/jamanetworkopen.2018.1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kinahan KE, Kircher S, Altman J, Rademaker A, Salsman JM, Didwania A, O'Brien B, Patel AC, Sanford SD. Promoting the Shared-Care Model for Adolescent and Young Adults With Cancer: Optimizing Referrals and Care Coordination With Primary Care Providers. J Natl Compr Canc Netw. 2016 Dec 31;15(1):38–44. doi: 10.6004/jnccn.2017.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Knierim KE, Hall TL, Dickinson LM, Nease DE, de la Cerda DR, Fernald D, Bleecker MJ, Rhyne RL, Dickinson WP. Primary Care Practices’ Ability to Report Electronic Clinical Quality Measures in the EvidenceNOW Southwest Initiative to Improve Heart Health. JAMA Netw Open. 2019 Aug 07;2(8):e198569. doi: 10.1001/jamanetworkopen.2019.8569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Krishnan A, Finkelstein EA, Levine E, Foley P, Askew S, Steinberg D, Bennett GG. A Digital Behavioral Weight Gain Prevention Intervention in Primary Care Practice: Cost and Cost-Effectiveness Analysis. J Med Internet Res. 2019 May 17;21(5):e12201. doi: 10.2196/12201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kroenke K, Baye F, Lourens SG, Evans E, Weitlauf S, McCalley S, Porter B, Matthias MS, Bair MJ. Automated Self-management (ASM) vs. ASM-Enhanced Collaborative Care for Chronic Pain and Mood Symptoms: the CAMMPS Randomized Clinical Trial. J GEN INTERN MED. 2019 Jun 21;34(9):1806–1814. doi: 10.1007/s11606-019-05121-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kruger DL, Rein DB, Kil N, Jordan C, Brown KA, Yartel A, Smith BD. Implementation of Birth-Cohort Testing for Hepatitis C Virus. Health Promotion Practice. 2016 Aug 19;18(2):283–289. doi: 10.1177/1524839916661495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kukafka R, Fang J, Vanegas A, Silverman T, Crew KD. Pilot study of decision support tools on breast cancer chemoprevention for high-risk women and healthcare providers in the primary care setting. BMC Med Inform Decis Mak. 2018 Dec 17;18(1):134. doi: 10.1186/s12911-018-0716-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kukafka R, Jeong IC, Finkelstein J. Optimizing Decision Support for Tailored Health Behavior Change Applications. Stud Health Technol Inform. 2015;216:108–12. [PubMed] [Google Scholar]
- 136.Ladapo JA, Lyons H, Yau M, Rich P, Newton D, Bruce-Mensah K, Johnson A, Zhou Y, Stemkowski S, Monane M. Enhanced Assessment of Chest Pain and Related Symptoms in the Primary Care Setting Through the Use of a Novel Personalized Medicine Genomic Test. Am J Med Qual. 2014 May 05;30(4):345–352. doi: 10.1177/1062860614532517. [DOI] [PubMed] [Google Scholar]
- 137.Landis SE, Galvin SL. Implementation and Assessment of a Fall Screening Program in Primary Care Practices. J Am Geriatr Soc. 2014 Dec 17;62(12):2408–2414. doi: 10.1111/jgs.13137. [DOI] [PubMed] [Google Scholar]
- 138.Langford AT, Wang B, Orzeck-Byrnes NA, Aidasani SR, Hu L, Applegate M, Moloney DN, Sevick MA, Rogers ES, Levy NK. Sociodemographic and clinical correlates of key outcomes from a Mobile Insulin Titration Intervention (MITI) for medically underserved patients. Patient Education and Counseling. 2019 Mar;102(3):520–527. doi: 10.1016/j.pec.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 139.Lanpher MG, Askew S, Bennett GG. Health Literacy and Weight Change in a Digital Health Intervention for Women: A Randomized Controlled Trial in Primary Care Practice. Journal of Health Communication. 2016 Apr 04;21(sup1):34–42. doi: 10.1080/10810730.2015.1131773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Leddy J, Green JA, Yule C, Molecavage J, Coresh J, Chang AR. Improving proteinuria screening with mailed smartphone urinalysis testing in previously unscreened patients with hypertension: a randomized controlled trial. BMC Nephrol. 2019 Apr 18;20(1) doi: 10.1186/s12882-019-1324-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lepore S, Collins B, Coffman D, Winickoff J, Nair U, Moughan B, Bryant-Stephens T, Taylor D, Fleece D, Godfrey M. Kids Safe and Smokefree (KiSS) Multilevel Intervention to Reduce Child Tobacco Smoke Exposure: Long-Term Results of a Randomized Controlled Trial. IJERPH. 2018 Jun 12;15(6):1239. doi: 10.3390/ijerph15061239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Levy S, Henderson L, McAlpine C. Growing up with confidence: using telehealth to support continence self-care deficits amongst young people with complex needs. jhi. 2014 May 27;21(3):113–117. doi: 10.14236/jhi.v21i3.58. [DOI] [PubMed] [Google Scholar]
- 143.Lewis KH, Skelton JA, Hsu F, Ezouah P, Taveras EM, Block JP. Implementing a novel electronic health record approach to track child sugar-sweetened beverage consumption. Preventive Medicine Reports. 2018 Sep;11:169–175. doi: 10.1016/j.pmedr.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Liebschutz JM, Xuan Z, Shanahan CW, LaRochelle M, Keosaian J, Beers D, Guara G, O’Connor K, Alford DP, Parker V, Weiss RD, Samet JH, Crosson J, Cushman PA, Lasser KE. Improving Adherence to Long-term Opioid Therapy Guidelines to Reduce Opioid Misuse in Primary Care. JAMA Intern Med. 2017 Sep 01;177(9):1265. doi: 10.1001/jamainternmed.2017.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lin CJ, Nowalk MP, Pavlik VN, Brown AE, Zhang S, Raviotta JM, Moehling KK, Hawk M, Ricci EM, Middleton DB, Patel S, South-Paul JE, Zimmerman RK. Using the 4 pillars™ practice transformation program to increase adult influenza vaccination and reduce missed opportunities in a randomized cluster trial. BMC Infect Dis. 2016 Nov 3;16(1):623. doi: 10.1186/s12879-016-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Litke J, Spoutz L, Ahlstrom D, Perdew C, Llamas W, Erickson K. Impact of the clinical pharmacy specialist in telehealth primary care. American Journal of Health-System Pharmacy. 2018;75(13):982–6. doi: 10.2146/ajhp170633. [DOI] [PubMed] [Google Scholar]
- 147.Liu Y, Zupan NJ, Swearingen R, Jacobson N, Carlson JN, Mahoney JE, Klein R, Bjelland TD, Smith MA. Identification of barriers, facilitators and system-based implementation strategies to increase teleophthalmology use for diabetic eye screening in a rural US primary care clinic: a qualitative study. BMJ Open. 2019 Feb 18;9(2):e022594. doi: 10.1136/bmjopen-2018-022594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Looman W, Antolick M, Cady R, Lunos S, Garwick A, Finkelstein S. Effects of a Telehealth Care Coordination Intervention on Perceptions of Health Care by Caregivers of Children With Medical Complexity: A Randomized Controlled Trial. Journal of Pediatric Health Care. 2015 Jul;29(4):352–363. doi: 10.1016/j.pedhc.2015.01.007. doi: 10.1016/j.pedhc.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lv N, Xiao L, Simmons ML, Rosas LG, Chan A, Entwistle M. Personalized Hypertension Management Using Patient-Generated Health Data Integrated With Electronic Health Records (EMPOWER-H): Six-Month Pre-Post Study. J Med Internet Res. 2017 Sep 19;19(9):e311. doi: 10.2196/jmir.7831. https://www.jmir.org/2017/9/e311/ v19i9e311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.MacLean CD, Berger C, Cangiano ML, Ziegelman D, Lidofsky SD. Impact of electronic reminder systems on hepatitis C screening in primary care. J Viral Hepat. 2018 Mar 30;25(8):939–944. doi: 10.1111/jvh.12885. [DOI] [PubMed] [Google Scholar]
- 151.Maddali MV, Mehtani NJ, Converse C, Kapoor S, Pham P, Li JZ, Shah M. Development and Validation of HIV-ASSIST, an Online, Educational, Clinical Decision Support Tool to Guide Patient-Centered ARV Regimen Selection. J Acquir Immune Defic Syndr. 2019 Oct 01;82(2):188–194. doi: 10.1097/QAI.0000000000002118.00126334-201910010-00012 [DOI] [PubMed] [Google Scholar]
- 152.Mahabee-Gittens EM, Dexheimer JW, Tabangin M, Khoury JC, Merianos AL, Stone L, Meyers GT, Gordon JS. An Electronic Health Record−Based Strategy to Address Child Tobacco Smoke Exposure. American Journal of Preventive Medicine. 2018 Jan;54(1):64–71. doi: 10.1016/j.amepre.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mahoney MC, Erwin DO, Twarozek AM, Saad-Harfouche FG, Rodriguez EM, Sun X, Underwood W, Fox C. Leveraging technology to promote smoking cessation in urban and rural primary care medical offices. Preventive Medicine. 2018 Sep;114:102–106. doi: 10.1016/j.ypmed.2018.06.016. http://europepmc.org/abstract/MED/29953897 .S0091-7435(18)30205-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mainous AG, Carek PJ, Lynch K, Tanner RJ, Hulihan MM, Baskin J, Coates TD. Effectiveness of Clinical Decision Support Based Intervention in the Improvement of Care for Adult Sickle Cell Disease Patients in Primary Care. J Am Board Fam Med. 2018 Sep 10;31(5):812–816. doi: 10.3122/jabfm.2018.05.180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Mann DM, Palmisano J, Lin JJ. A pilot randomized trial of technology-assisted goal setting to improve physical activity among primary care patients with prediabetes. Preventive Medicine Reports. 2016 Dec;4:107–112. doi: 10.1016/j.pmedr.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mansberger SL, Sheppler C, Barker G, Gardiner SK, Demirel S, Wooten K, Becker TM. Long-term Comparative Effectiveness of Telemedicine in Providing Diabetic Retinopathy Screening Examinations. JAMA Ophthalmol. 2015 May 01;133(5):518. doi: 10.1001/jamaophthalmol.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Marcelin JR, Tan EM, Marcelin A, Scheitel M, Ramu P, Hankey R, Keniya P, Wingo M, Rizza SA, North F, Chaudhry R. Assessment and improvement of HIV screening rates in a Midwest primary care practice using an electronic clinical decision support system: a quality improvement study. BMC Med Inform Decis Mak. 2016 Jul 4;16(1):76. doi: 10.1186/s12911-016-0320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Maxwell LG, McFarland MS, Baker JW, Cassidy RF. Evaluation of the Impact of a Pharmacist-Led Telehealth Clinic on Diabetes-Related Goals of Therapy in a Veteran Population. Pharmacotherapy. 2016 Mar 11;36(3):348–356. doi: 10.1002/phar.1719. [DOI] [PubMed] [Google Scholar]
- 159.McAdam-Marx C, Tak C, Petigara T, Jones NW, Yoo M, Briley MS, Gunning K, Gren L. Impact of a guideline-based best practice alert on pneumococcal vaccination rates in adults in a primary care setting. BMC Health Serv Res. 2019 Jul 10;19(1):474. doi: 10.1186/s12913-019-4263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.McGrath K, Foster K, Doggett P, Altshuler M, Osborne-Wu J, Castellan C, Lopez K, Askie P, Chung D, Parente L, Parra Y. EMR-Based Intervention Improves Lead Screening at an Urban Family Medicine Practice. Fam Med. 2016 Nov;48(10):801–804. http://www.stfm.org/FamilyMedicine/Vol48Issue10/McGrath801 . [PubMed] [Google Scholar]
- 161.McLendon SF, Wood FG, Stanley N. Enhancing diabetes care through care coordination, telemedicine, and education: Evaluation of a rural pilot program. Public Health Nurs. 2019 Mar 13;36(3):310–320. doi: 10.1111/phn.12601. [DOI] [PubMed] [Google Scholar]
- 162.Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, Knight TK, Hay JW, Doctor JN. Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices. JAMA. 2016 Feb 09;315(6):562. doi: 10.1001/jama.2016.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Mehta S, Khan T, Guerra C, Reitz C, McAuliffe T, Volpp K. A Randomized Controlled Trial of Opt-in Versus Opt-Out Colorectal Cancer Screening Outreach. American Journal of Gastroenterology. 2018;113(12):1848–1854. doi: 10.1038/s41395-018-0151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Mera J, Vellozzi C, Hariri S, Carabin H, Drevets DA, Miller A, Reilley B, Essex W, Gahn D, Lyons L, Leston J, Ward JW. Identification and Clinical Management of Persons with Chronic Hepatitis C Virus Infection — Cherokee Nation, 2012–2015. MMWR Morb. Mortal. Wkly. Rep. 2016 May 13;65(18):461–466. doi: 10.15585/mmwr.mm6518a2. [DOI] [PubMed] [Google Scholar]
- 165.Militello L, Diiulio J, Borders M, Sushereba C, Saleem J, Haverkamp D, Imperiale T. Evaluating a Modular Decision Support Application For Colorectal Cancer Screening. Appl Clin Inform. 2017 Dec 20;26(01):162–179. doi: 10.4338/aci-2016-09-ra-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mitchell SL, Shaffer ML, Cohen S, Hanson LC, Habtemariam D, Volandes AE. An Advance Care Planning Video Decision Support Tool for Nursing Home Residents With Advanced Dementia. JAMA Intern Med. 2018 Jul 01;178(7):961. doi: 10.1001/jamainternmed.2018.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Molleda L, Bahamon M, St. George SM, Perrino T, Estrada Y, Correa Herrera D, Pantin H, Prado G. Clinic Personnel, Facilitator, and Parent Perspectives of eHealth Familias Unidas in Primary Care. Journal of Pediatric Health Care. 2017 May;31(3):350–361. doi: 10.1016/j.pedhc.2016.11.001. http://europepmc.org/abstract/MED/28012799 .S0891-5245(16)30322-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mundt MP, Zakletskaia LI. Putting the pieces together: EHR communication and diabetes patient outcomes. Am J Manag Care. 2018 Oct;24(10):462–468. https://www.ajmc.com/pubMed.php?pii=87746 .87746 [PMC free article] [PubMed] [Google Scholar]
- 169.Mussman GM, Vossmeyer MT, Brady PW, Warrick DM, Simmons JM, White CM. Improving the reliability of verbal communication between primary care physicians and pediatric hospitalists at hospital discharge. J. Hosp. Med. 2015 May 29;10(9):574–580. doi: 10.1002/jhm.2392. [DOI] [PubMed] [Google Scholar]
- 170.Mussulman L, Ellerbeck EF, Cupertino AP, Preacher KJ, Spaulding R, Catley D, Cox LS, Lambart L, Hunt JJ, Nazir N, Shireman T, Richter KP. Design and participant characteristics of a randomized-controlled trial of telemedicine for smoking cessation among rural smokers. Contemporary Clinical Trials. 2014 Jul;38(2):173–181. doi: 10.1016/j.cct.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Nagykaldi ZJ, Scheid D, Zhao D, Mishra B, Greever-Rice T. An Innovative Community-based Model for Improving Preventive Care in Rural Counties. J Am Board Fam Med. 2017 Sep 18;30(5):583–591. doi: 10.3122/jabfm.2017.05.170035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Nagykaldi Z, Yeaman B, Jones M, Mold J, Scheid D. HIE-i-health information exchange with intelligence. Journal of Ambulatory Care Management. 2014;37(1):20–31. doi: 10.1097/jac.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 173.Nitsche B, Miller SC, Giorgio M, Berry CA, Muir A. Improving Hepatitis C Identification: Technology Alone Is Not the Answer. Health Promotion Practice. 2017 Sep 11;19(4):506–512. doi: 10.1177/1524839917725501. [DOI] [PubMed] [Google Scholar]
- 174.Nowalk MP, Lin CJ, Pavlik VN, Brown AE, Zhang S, Moehling KK, Raviotta JM, South-Paul JE, Hawk M, Ricci EM, Middleton DB, Patel SA, Ahmed F, Zimmerman RK. Using the 4 Pillars™ Practice Transformation Program to increase adult Tdap immunization in a randomized controlled cluster trial. Vaccine. 2016 Sep;34(41):5026–5033. doi: 10.1016/j.vaccine.2016.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.O'Connor PJ, Magid DJ, Sperl-Hillen JM, Price DW, Asche SE, Rush WA, Ekstrom HL, Brand DW, Tavel HM, Godlevsky OV, Johnson PE, Margolis KL. Personalised physician learning intervention to improve hypertension and lipid control: randomised trial comparing two methods of physician profiling. BMJ Qual Saf. 2014 Sep 16;23(12):1014–1022. doi: 10.1136/bmjqs-2014-002807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ofili EO, Pemu PE, Quarshie A, Mensah EA, Rollins L, Ojutalayo F, McCaslin A, Clair BS. Democratizing Discovery Health with N=Me. Trans Am Clin Climatol Assoc. 2018;129:215–234. http://europepmc.org/abstract/MED/30166716 . [PMC free article] [PubMed] [Google Scholar]
- 177.Okah A, Williams K, Talib N, Mann K. Promoting Oral Health in Childhood: A Quality Improvement Project. Pediatrics. 2018 Jun 25;141(6):e20172396. doi: 10.1542/peds.2017-2396.peds.2017-2396 [DOI] [PubMed] [Google Scholar]
- 178.Osofsky HJ, Osofsky JD, Hansel TC, Flynn T. The Louisiana Mental and Behavioral Health Capacity Project Trauma-Informed Integrated Care Model and Improved Posttraumatic Stress Outcomes. J Public Health Manag Pract. 2017 Dec;23 Suppl 6 Suppl, Gulf Region Health Outreach Program:S25–S31. doi: 10.1097/PHH.0000000000000652.00124784-201711001-00006 [DOI] [PubMed] [Google Scholar]
- 179.Ozanne EM, Howe R, Omer Z, Esserman LJ. Development of a personalized decision aid for breast cancer risk reduction and management. BMC Med Inform Decis Mak. 2014 Jan 14;14(1):4. doi: 10.1186/1472-6947-14-4. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-14-4 .1472-6947-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Peralta CA, Frigaard M, Rolon L, Seal K, Tuot D, Senyak J, Lo L, Powe N, Scherzer R, Chao S, Chiao P, Lui K, Shlipak MG, Rubinsky AD. Screening for CKD To Improve Processes of Care among Nondiabetic Veterans with Hypertension. CJASN. 2020 Feb 07;15(2):174–181. doi: 10.2215/cjn.05050419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Perry TT, Halterman JS, Brown RH, Luo C, Randle SM, Hunter CR, Rettiganti M. Results of an asthma education program delivered via telemedicine in rural schools. Ann Allergy Asthma Immunol. 2018 Apr;120(4):401–408. doi: 10.1016/j.anai.2018.02.013. http://europepmc.org/abstract/MED/29471032 .S1081-1206(18)30122-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Peters KM, Sadler G, Miller E, Radovic A. An Electronic Referral and Social Work Protocol to Improve Access to Mental Health Services. Pediatrics. 2018 Nov;142(5) doi: 10.1542/peds.2017-2417.peds.2017-2417 [DOI] [PubMed] [Google Scholar]
- 183.Petersen A, Mermelstein R, Berg KM, Baker TB, Smith SS, Jorenby D, Piper ME, Schlam TR, Cook JW. Offering smoking treatment to primary care patients in two Wisconsin healthcare systems: Who chooses smoking reduction versus cessation? Prev Med. 2017 Dec;105:332–336. doi: 10.1016/j.ypmed.2017.10.015. http://europepmc.org/abstract/MED/28988997 .S0091-7435(17)30365-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Phillips LS, Barb D, Yong C, Tomolo AM, Jackson SL, Olson DE, Rhee MK, Duva IM, He Q, Long Q. Translating What Works: A New Approach to Improve Diabetes Management. J Diabetes Sci Technol. 2015 Jul 09;9(4):857–64. doi: 10.1177/1932296815576000. http://europepmc.org/abstract/MED/25759182 .1932296815576000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Quanbeck A, Gustafson DH, Marsch LA, Chih M, Kornfield R, McTavish F, Johnson R, Brown RT, Mares M, Shah DV. Implementing a Mobile Health System to Integrate the Treatment of Addiction Into Primary Care: A Hybrid Implementation-Effectiveness Study. J Med Internet Res. 2018 Jan 30;20(1):e37. doi: 10.2196/jmir.8928. https://www.jmir.org/2018/1/e37/ v20i1e37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Reeves K, Taylor Y, Tapp H, Ludden T, Shade L, Burton B, Courtlandt C, Dulin M. Evaluation of a Pilot Asthma Care Program for Electronic Communication between School Health and a Healthcare System’s Electronic Medical Record. Appl Clin Inform. 2017 Dec 18;07(04):969–982. doi: 10.4338/aci-2016-02-ra-0022. https://europepmc.org/articles/PMC5228138?pdf=render . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Regan ME. Implementing an evidence-based clinical decision support tool to improve the detection, evaluation, and referral patterns of adult chronic kidney disease patients in primary care. J Am Assoc Nurse Pract. 2017 Dec;29(12):741–753. doi: 10.1002/2327-6924.12505.01741002-201712000-00006 [DOI] [PubMed] [Google Scholar]
- 188.Richardson LP, Zhou C, Gersh E, Spielvogle H, Taylor JA, McCarty CA. Effect of Electronic Screening With Personalized Feedback on Adolescent Health Risk Behaviors in a Primary Care Setting: A Randomized Clinical Trial. JAMA Netw Open. 2019 May 03;2(5):e193581. doi: 10.1001/jamanetworkopen.2019.3581. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.3581 .2733175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Richter KP, Shireman TI, Ellerbeck EF, Cupertino AP, Catley D, Cox LS, Preacher KJ, Spaulding R, Mussulman LM, Nazir N, Hunt JJ, Lambart L. Comparative and cost effectiveness of telemedicine versus telephone counseling for smoking cessation. J Med Internet Res. 2015 May 08;17(5):e113. doi: 10.2196/jmir.3975. https://www.jmir.org/2015/5/e113/ v17i5e113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ripley-Moffitt C, Neutze D, Gwynne M, Goldstein AO. Patient care outcomes of a tobacco use registry in an academic family practice. J Am Board Fam Med. 2015 Mar 06;28(2):205–13. doi: 10.3122/jabfm.2015.02.140121. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=25748761 .28/2/205 [DOI] [PubMed] [Google Scholar]
- 191.Rollman BL, Belnap BH, Mazumdar S, Abebe KZ, Karp JF, Lenze EJ, Schulberg HC. Telephone-Delivered Stepped Collaborative Care for Treating Anxiety in Primary Care: A Randomized Controlled Trial. J Gen Intern Med. 2017 Mar;32(3):245–255. doi: 10.1007/s11606-016-3873-1. http://europepmc.org/abstract/MED/27714649 .10.1007/s11606-016-3873-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Rose BL, Leung S, Gustin J, Childers J. Initiating Advance Care Planning in Primary Care: A Model for Success. J Palliat Med. 2019 Apr;22(4):427–431. doi: 10.1089/jpm.2018.0380. [DOI] [PubMed] [Google Scholar]
- 193.Satre DD, Leibowitz AS, Leyden W, Catz SL, Hare CB, Jang H, Lam JO, Bryant KJ, Weisner CM, Sterling SA, Horberg M, Volberding P, Silverberg MJ. Interventions to Reduce Unhealthy Alcohol Use among Primary Care Patients with HIV: the Health and Motivation Randomized Clinical Trial. J Gen Intern Med. 2019 Oct 11;34(10):2054–2061. doi: 10.1007/s11606-019-05065-9. http://europepmc.org/abstract/MED/31187344 .10.1007/s11606-019-05065-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Scheuner MT, Hamilton AB, Peredo J, Sale TJ, Austin C, Gilman SC, Bowen MS, Goldzweig CL, Lee M, Mittman BS, Yano EM. A cancer genetics toolkit improves access to genetic services through documentation and use of the family history by primary-care clinicians. Genet Med. 2014 Jan 13;16(1):60–9. doi: 10.1038/gim.2013.75.gim201375 [DOI] [PubMed] [Google Scholar]
- 195.Schiff GD, Klinger E, Salazar A, Medoff J, Amato MG, John Orav E, Shaykevich S, Seoane EV, Walsh L, Fuller TE, Dykes PC, Bates DW, Haas JS. Screening for Adverse Drug Events: a Randomized Trial of Automated Calls Coupled with Phone-Based Pharmacist Counseling. J Gen Intern Med. 2019 Feb;34(2):285–292. doi: 10.1007/s11606-018-4672-7. http://europepmc.org/abstract/MED/30291602 .10.1007/s11606-018-4672-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Schlittenhardt M, Smith SC, Ward-Smith P. Tele-Continence Care: A Novel Approach for Providers. Urol Nurs. 2016;36(5):217–23. [PubMed] [Google Scholar]
- 197.Senft N, Everson J. eHealth Engagement as a Response to Negative Healthcare Experiences: Cross-Sectional Survey Analysis. J Med Internet Res. 2018 Dec 05;20(12):e11034. doi: 10.2196/11034. https://www.jmir.org/2018/12/e11034/ v20i12e11034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sequist TD, Holliday AM, Orav EJ, Bates DW, Denker BM. Physician and patient tools to improve chronic kidney disease care. Am J Manag Care. 2018 Apr 01;24(4):e107–e114. https://www.ajmc.com/pubMed.php?pii=87521 .87521 [PubMed] [Google Scholar]
- 199.Shade SB, Steward WT, Koester KA, Chakravarty D, Myers JJ. Health information technology interventions enhance care completion, engagement in HIV care and treatment, and viral suppression among HIV-infected patients in publicly funded settings. J Am Med Inform Assoc. 2015 Apr;22(e1):e104–11. doi: 10.1136/amiajnl-2013-002623. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=25030033 .amiajnl-2013-002623 [DOI] [PubMed] [Google Scholar]
- 200.Shah SD, Prine L, Waltermaurer E, Rubin SE. Feasibility study of family planning services screening as clinical decision support at an urban Federally Qualified Health Center network. Contraception. 2019 Jan;99(1):27–31. doi: 10.1016/j.contraception.2018.10.004.S0010-7824(18)30463-3 [DOI] [PubMed] [Google Scholar]
- 201.Shaibi GQ, Kullo IJ, Singh DP, Sharp RR, De Filippis E, Cuellar I, Hernandez V, Levey S, Radecki Breitkopf C, Olson JE, Cerhan JR, Mandarino LJ, Thibodeau SN, Lindor NM. Developing a Process for Returning Medically Actionable Genomic Variants to Latino Patients in a Federally Qualified Health Center. Public Health Genomics. 2018;21(1-2):77–84. doi: 10.1159/000494488. https://www.karger.com?DOI=10.1159/000494488 .000494488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Shaikh U, Nettiksimmons J, Joseph JG, Tancredi D, Romano PS. Collaborative practice improvement for childhood obesity in rural clinics: the Healthy Eating Active Living Telehealth Community of Practice (HEALTH COP) Am J Med Qual. 2014 Oct 29;29(6):467–75. doi: 10.1177/1062860613506252.1062860613506252 [DOI] [PubMed] [Google Scholar]
- 203.Shane-McWhorter L, Lenert L, Petersen M, Woolsey S, McAdam-Marx C, Coursey JM, Whittaker TC, Hyer C, LaMarche D, Carroll P, Chuy L. The Utah Remote Monitoring Project: improving health care one patient at a time. Diabetes Technol Ther. 2014 Oct;16(10):653–60. doi: 10.1089/dia.2014.0045. http://europepmc.org/abstract/MED/24991923 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Sharifi M, Adams WG, Winickoff JP, Guo J, Reid M, Boynton-Jarrett R. Enhancing the electronic health record to increase counseling and quit-line referral for parents who smoke. Acad Pediatr. 2014 Sep;14(5):478–84. doi: 10.1016/j.acap.2014.03.017.S1876-2859(14)00100-4 [DOI] [PubMed] [Google Scholar]
- 205.Sharifi M, Franz C, Horan CM, Giles CM, Long MW, Ward ZJ, Resch SC, Marshall R, Gortmaker SL, Taveras EM. Cost-Effectiveness of a Clinical Childhood Obesity Intervention. Pediatrics. 2017 Nov 31;140(5):e20162998. doi: 10.1542/peds.2016-2998. http://europepmc.org/abstract/MED/29089403 .peds.2016-2998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Shuen JA, Wilson MP, Kreshak A, Mullinax S, Brennan J, Castillo EM, Hinkle C, Vilke GM. Telephoned, Texted, or Typed Out: A Randomized Trial of Physician-Patient Communication After Emergency Department Discharge. J Emerg Med. 2018 Oct;55(4):573–581. doi: 10.1016/j.jemermed.2018.07.023. http://europepmc.org/abstract/MED/30181075 .S0736-4679(18)30741-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sidlow R, Msaouel P. Improving Hepatitis C Virus Screening Rates in Primary Care: A Targeted Intervention Using the Electronic Health Record. Journal for Healthcare Quality. 2015;37(5):319–323. doi: 10.1097/jhq.0000000000000010. [DOI] [PubMed] [Google Scholar]
- 208.Sigel E, Harpin SB, Tung G. Increasing documentation and referral for youth at risk for violence through the primary health care setting. Clin Pediatr (Phila) 2015 May 09;54(5):451–7. doi: 10.1177/0009922814553431.0009922814553431 [DOI] [PubMed] [Google Scholar]
- 209.Siminerio L, Ruppert K, Huber K, Toledo FGS. Telemedicine for Reach, Education, Access, and Treatment (TREAT): linking telemedicine with diabetes self-management education to improve care in rural communities. Diabetes Educ. 2014 Sep;40(6):797–805. doi: 10.1177/0145721714551993.0145721714551993 [DOI] [PubMed] [Google Scholar]
- 210.Skolarus LE, Piette JD, Pfeiffer PN, Williams LS, Mackey J, Hughes R, Morgenstern LB. Interactive Voice Response-An Innovative Approach to Post-Stroke Depression Self-Management Support. Transl Stroke Res. 2017 Feb 9;8(1):77–82. doi: 10.1007/s12975-016-0481-7. http://europepmc.org/abstract/MED/27394917 .10.1007/s12975-016-0481-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Smallwood AJ, Schapira MM, Fedders M, Neuner JM. A pilot randomized controlled trial of a decision aid with tailored fracture risk tool delivered via a patient portal. Osteoporos Int. 2017 Feb;28(2):567–576. doi: 10.1007/s00198-016-3767-4.10.1007/s00198-016-3767-4 [DOI] [PubMed] [Google Scholar]
- 212.Smania M. Use of a Point-of-Care Tool to Improve Nurse Practitioner BRCA Knowledge. CJON. 2016 Jun 1;20(3):327–331. doi: 10.1188/16.cjon.327-331. [DOI] [PubMed] [Google Scholar]
- 213.Smith KJ, Kuo S, Zgibor JC, McTigue KM, Hess R, Bhargava T, Bryce CL. Cost effectiveness of an internet-delivered lifestyle intervention in primary care patients with high cardiovascular risk. Prev Med. 2016 Jun;87:103–109. doi: 10.1016/j.ypmed.2016.02.036.S0091-7435(16)30017-2 [DOI] [PubMed] [Google Scholar]
- 214.Smith NM, Satyshur RD. Pediatric Diabetes Telemedicine Program Improves Access to Care for Rural Families: Role of APRNs. Pediatr Nurs. 2016;42(6):294–9. [PubMed] [Google Scholar]
- 215.Sobota AE, Kavanagh PL, Adams WG, McClure E, Farrell D, Sprinz PG. Improvement in influenza vaccination rates in a pediatric sickle cell disease clinic. Pediatr Blood Cancer. 2015 Apr 24;62(4):654–7. doi: 10.1002/pbc.25390. http://europepmc.org/abstract/MED/25545967 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sood A, Watts SA, Johnson JK, Hirth S, Aron DC. Telemedicine consultation for patients with diabetes mellitus: a cluster randomised controlled trial. J Telemed Telecare. 2018 Jul;24(6):385–391. doi: 10.1177/1357633X17704346. [DOI] [PubMed] [Google Scholar]
- 217.Sperl-Hillen J, Crain A, Margolis K, Ekstrom H, Appana D, Amundson G, Sharma R, Desai JR, O'Connor PJ. Clinical decision support directed to primary care patients and providers reduces cardiovascular risk: a randomized trial. J Am Med Inform Assoc. 2018 Sep 01;25(9):1137–1146. doi: 10.1093/jamia/ocy085. http://europepmc.org/abstract/MED/29982627 .5048778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Stading JA, Phan L, Walter A, Bilslend L, White R, Qi Y. Initial Experience of Clinical Pharmacy Services Delivered by Computer Communication via Cisco Jabber Video in a US Veterans Administration Medical Center. J Pharm Technol. 2014 Jun 01;30(3):76–80. doi: 10.1177/8755122513505744. http://europepmc.org/abstract/MED/34860870 .10.1177_8755122513505744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Steinberg DM, Levine EL, Lane I, Askew S, Foley PB, Puleo E, Bennett GG. Adherence to Self-Monitoring via Interactive Voice Response Technology in an eHealth Intervention Targeting Weight Gain Prevention Among Black Women: Randomized Controlled Trial. J Med Internet Res. 2014 Apr 29;16(4):e114. doi: 10.2196/jmir.2996. https://www.jmir.org/2014/4/e114/ v16i4e114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Stevens MB, Hastings SN, Powers J, Vandenberg AE, Echt KV, Bryan WE, Peggs K, Markland AD, Hwang U, Hung WW, Schmidt AJ, McGwin G, Ikpe-Ekpo E, Clevenger C, Johnson TM, Vaughan CP. Enhancing the Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department (EQUiPPED): Preliminary Results from Enhancing Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department, a Novel Multicomponent Interdisciplinary Quality Improvement Initiative. J Am Geriatr Soc. 2015 May;63(5):1025–9. doi: 10.1111/jgs.13404. [DOI] [PubMed] [Google Scholar]
- 221.Stockwell MS, Marchant CD, Wodi AP, Barnett ED, Broder KR, Jakob K, Lewis P, Kattan M, Rezendes AM, Barrett A, Sharma D, Fernandez N, LaRussa P. A multi-site feasibility study to assess fever and wheezing in children after influenza vaccines using text messaging. Vaccine. 2017 Dec 15;35(50):6941–6948. doi: 10.1016/j.vaccine.2017.10.073. http://europepmc.org/abstract/MED/29089191 .S0264-410X(17)31481-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Stulberg DB, Dahlquist IH, Disterhoft J, Bello JK, Hunter MS. Increase in Contraceptive Counseling by Primary Care Clinicians After Implementation of One Key Question® at an Urban Community Health Center. Matern Child Health J. 2019 Aug;23(8):996–1002. doi: 10.1007/s10995-019-02754-z.10.1007/s10995-019-02754-z [DOI] [PubMed] [Google Scholar]
- 223.Sudhanthar S, Lapinski J, Turner J, Gold J, Sigal Y, Thakur K, Napolova O, Stiffler M. Improving oral health through dental fluoride varnish application in a primary care paediatric practice. BMJ Open Qual. 2019 May 31;8(2):e000589. doi: 10.1136/bmjoq-2018-000589. https://bmjopenquality.bmj.com/lookup/pmidlookup?view=long&pmid=31259286 .bmjoq-2018-000589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Szilagyi PG, Serwint JR, Humiston SG, Rand CM, Schaffer S, Vincelli P, Dhepyasuwan N, Blumkin A, Albertin C, Curtis CR. Effect of provider prompts on adolescent immunization rates: a randomized trial. Acad Pediatr. 2015 Mar;15(2):149–57. doi: 10.1016/j.acap.2014.10.006. http://europepmc.org/abstract/MED/25748976 .S1876-2859(14)00388-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Talmi A, Bunik M, Asherin R, Rannie M, Watlington T, Beaty B, Berman S. Improving developmental screening documentation and referral completion. Pediatrics. 2014 Oct 01;134(4):e1181–8. doi: 10.1542/peds.2012-1151.peds.2012-1151 [DOI] [PubMed] [Google Scholar]
- 226.Taveras EM, Marshall R, Sharifi M, Avalon E, Fiechtner L, Horan C, Gerber MW, Orav EJ, Price SN, Sequist T, Slater D. Comparative Effectiveness of Clinical-Community Childhood Obesity Interventions: A Randomized Clinical Trial. JAMA Pediatr. 2017 Aug 07;171(8):e171325. doi: 10.1001/jamapediatrics.2017.1325. http://europepmc.org/abstract/MED/28586856 .2630628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Taylor AM, Bingham J, Schussel K, Axon DR, Dickman DJ, Boesen K, Martin R, Warholak TL. Integrating Innovative Telehealth Solutions into an Interprofessional Team-Delivered Chronic Care Management Pilot Program. J Manag Care Spec Pharm. 2018 Aug;24(8):813–818. doi: 10.18553/jmcp.2018.24.8.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Tetrault J, Holt S, Cavallo D, O'Connor P, Gordon M, Corvino J, Nich C, Carroll K. Computerized Cognitive Behavioral Therapy for Substance Use Disorders in a Specialized Primary Care Practice: a Randomized Feasibility Trial to Address the RT Component of SBIRT. Journal of Addiction Medicine. 2020;14(6):e303–e309. doi: 10.1097/adm.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 229.Tetuan C, Axon DR, Bingham J, Boesen K, Lipsy R, Scovis N, Taylor AM, Warholak T, Lott BE, Leal S. Assessing the Effect of a Telepharmacist's Recommendations During an Integrated, Interprofessional Telehealth Appointment and Their Alignment with Quality Measures. J Manag Care Spec Pharm. 2019 Dec;25(12):1334–1339. doi: 10.18553/jmcp.2019.25.12.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Thomas KE, Kisely S, Urrego F. Electronic Heath Record Prompts May Increase Screening for Secondhand Smoke Exposure. Clin Pediatr (Phila) 2018 Jan 30;57(1):27–30. doi: 10.1177/0009922816688261. [DOI] [PubMed] [Google Scholar]
- 231.Tieu C, Chaudhry R, Schroeder DR, Bock FA, Hanson GJ, Tung EE. Utilization of Patient Electronic Messaging to Promote Advance Care Planning in the Primary Care Setting. Am J Hosp Palliat Care. 2017 Aug 17;34(7):665–670. doi: 10.1177/1049909116650237.1049909116650237 [DOI] [PubMed] [Google Scholar]
- 232.Tsoh JY, Quach T, Duong TB, Sa Nan Park E, Wong C, Huang SM, Nguyen TT. Interactive Mobile Doctor (iMD) to Promote Patient-Provider Discussion on Tobacco Use among Asian American Patients in Primary Care: A Pilot Study. J Am Board Fam Med. 2018 Nov 09;31(6):869–880. doi: 10.3122/jabfm.2018.06.180018. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=30413543 .31/6/869 [DOI] [PubMed] [Google Scholar]
- 233.Turner JC, Keller A, Wu H, Zimmerman M, Zhang J, Barnes LE. Utilization of primary care among college students with mental health disorders. Health Psychol. 2018 Apr;37(4):385–393. doi: 10.1037/hea0000580.2018-03573-001 [DOI] [PubMed] [Google Scholar]
- 234.Turvey CL, Klein DM, Witry M, Klutts JS, Hill EL, Alexander B, Nazi KM. Patient Education for Consumer-Mediated HIE. A Pilot Randomized Controlled Trial of the Department of Veterans Affairs Blue Button. Appl Clin Inform. 2016 Aug 03;7(3):765–76. doi: 10.4338/ACI-2016-01-RA-0014. http://europepmc.org/abstract/MED/27484821 .2016-01-RA-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wagholikar KB, Hankey RA, Decker LK, Cha SS, Greenes RA, Liu H, Chaudhry R. Evaluation of the effect of decision support on the efficiency of primary care providers in the outpatient practice. J Prim Care Community Health. 2015 Jan;6(1):54–60. doi: 10.1177/2150131914546325. https://journals.sagepub.com/doi/10.1177/2150131914546325?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .2150131914546325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Walsh KE, Bacic J, Phillips BD, Adams WG. Misuse of Pediatric Medications and Parent-Physician Communication: An Interactive Voice Response Intervention. J Patient Saf. 2017 Feb 22;17(3):e207–e213. doi: 10.1097/pts.0000000000000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Werk LN, Diaz MC, Cadilla A, Franciosi JP, Hossain MJ. Promoting Adherence to Influenza Vaccination Recommendations in Pediatric Practice. J Prim Care Community Health. 2019 Jun 11;10:2150132719853061. doi: 10.1177/2150132719853061. https://journals.sagepub.com/doi/10.1177/2150132719853061?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Wise K, Sebastian S, Haas-Gehres A, Moore-Clingenpeel M, Lamberjack K. Pharmacist impact on pediatric vaccination errors and missed opportunities in the setting of clinical decision support. J Am Pharm Assoc (2003) 2017;57(3):356–361. doi: 10.1016/j.japh.2017.02.025. doi: 10.1016/j.japh.2017.02.025.S1544-3191(17)30124-3 [DOI] [PubMed] [Google Scholar]
- 239.Wolin KY, Steinberg DM, Lane IB, Askew S, Greaney ML, Colditz GA, Bennett GG. Engagement with eHealth Self-Monitoring in a Primary Care-Based Weight Management Intervention. PLoS One. 2015 Oct 15;10(10):e0140455. doi: 10.1371/journal.pone.0140455. https://dx.plos.org/10.1371/journal.pone.0140455 .PONE-D-14-38415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Wolver SE, Stultz JS, Aggarwal A, Thacker L, Banas C. Provider and Patient Perceptions of an External Medication History Function. J Patient Saf. 2018 Dec;14(4):234–240. doi: 10.1097/PTS.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 241.Woo C, Seton JM, Washington M, Tomlinson SC, Phrasavath D, Farrell KR, Goldstein B. Increasing specialty care access through use of an innovative home telehealth-based spinal cord injury disease management protocol (SCI DMP) The Journal of Spinal Cord Medicine. 2014 Mar 12;39(1):3–12. doi: 10.1179/2045772314y.0000000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Wood SM, McGeary A, Wilson M, Taylor A, Aumaier B, Petsis D, Campbell K. Effectiveness of a Quality Improvement Intervention to Improve Rates of Routine Chlamydia Trachomatis Screening in Female Adolescents Seeking Primary Preventive Care. J Pediatr Adolesc Gynecol. 2019 Feb;32(1):32–38. doi: 10.1016/j.jpag.2018.10.004. http://europepmc.org/abstract/MED/30394335 .S1083-3188(18)30338-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wu RR, Myers RA, Sperber N, Voils CI, Neuner J, McCarty CA, Haller IV, Harry M, Fulda KG, Cross D, Dimmock D, Rakhra-Burris T, Buchanan AH, Ginsburg GS, Orlando LA. Implementation, adoption, and utility of family health history risk assessment in diverse care settings: evaluating implementation processes and impact with an implementation framework. Genet Med. 2019 Feb 6;21(2):331–338. doi: 10.1038/s41436-018-0049-x. http://europepmc.org/abstract/MED/29875427 .10.1038/s41436-018-0049-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Yadav S, Hartkop S, Cardenas PY, Ladkany R, Halalau A, Shoichet S, Maddens M, Zakalik D. Utilization of a breast cancer risk assessment tool by internal medicine residents in a primary care clinic: impact of an educational program. BMC Cancer. 2019 Mar 14;19(1):228. doi: 10.1186/s12885-019-5418-6. https://bmccancer.biomedcentral.com/articles/10.1186/s12885-019-5418-6 .10.1186/s12885-019-5418-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Yakovchenko V, Hogan TP, Houston TK, Richardson L, Lipschitz J, Petrakis BA, Gillespie C, McInnes DK. Automated Text Messaging With Patients in Department of Veterans Affairs Specialty Clinics: Cluster Randomized Trial. J Med Internet Res. 2019 Aug 04;21(8):e14750. doi: 10.2196/14750. https://www.jmir.org/2019/8/e14750/ v21i8e14750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Yeboah-Korang A, Beig M, Khan M, Goldstein J, Macapinlac D, Maurer D, Sonnenberg A, Fimmel CJ. Hepatitis C Screening in Commercially Insured U.S. Birth-cohort Patients: Factors Associated with Testing and Effect of an EMR-based Screening Alert. J Transl Int Med. 2018 Jun;6(2):82–89. doi: 10.2478/jtim-2018-0012. http://europepmc.org/abstract/MED/29984203 .jtim-2018-0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Yeung A, Martinson MA, Baer L, Chen J, Clain A, Williams A, Chang TE, Trinh NT, Alpert JE, Fava M. The Effectiveness of Telepsychiatry-Based Culturally Sensitive Collaborative Treatment for Depressed Chinese American Immigrants. J. Clin. Psychiatry. 2016 Aug 24;77(08):e996–e1002. doi: 10.4088/jcp.15m09952. [DOI] [PubMed] [Google Scholar]
- 248.Young HM, Miyamoto S, Dharmar M, Tang-Feldman Y. Nurse Coaching and Mobile Health Compared With Usual Care to Improve Diabetes Self-Efficacy for Persons With Type 2 Diabetes: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2020 Mar 02;8(3):e16665. doi: 10.2196/16665. https://mhealth.jmir.org/2020/3/e16665/ v8i3e16665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Yu JS, Szigethy E, Wallace M, Solano F, Oser M. Implementation of a Guided, Digital Cognitive Behavioral Program for Anxiety in Primary Care: Preliminary Findings of Engagement and Effectiveness. Telemed J E Health. 2018 Nov 26;24(11):870–878. doi: 10.1089/tmj.2017.0280. [DOI] [PubMed] [Google Scholar]
- 250.Zera CA, Bates DW, Stuebe AM, Ecker JL, Seely EW. Diabetes Screening Reminder for Women With Prior Gestational Diabetes. Obstetrics & Gynecology. 2015;126(1):109–114. doi: 10.1097/aog.0000000000000883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Zhao L, Stinnett SS, Prakalapakorn SG. Visual Acuity Assessment and Vision Screening Using a Novel Smartphone Application. J Pediatr. 2019 Oct;213:203–210.e1. doi: 10.1016/j.jpeds.2019.06.021.S0022-3476(19)30715-2 [DOI] [PubMed] [Google Scholar]
- 252.Zhong X, Liang M, Sanchez R, Yu M, Budd PR, Sprague JL, Dewar MA. On the effect of electronic patient portal on primary care utilization and appointment adherence. BMC Med Inform Decis Mak. 2018 Oct 16;18(1):84. doi: 10.1186/s12911-018-0669-8. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-018-0669-8 .10.1186/s12911-018-0669-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Zieve GG, Richardson LP, Katzman K, Spielvogle H, Whitehouse S, McCarty CA. Adolescents' Perspectives on Personalized E-Feedback in the Context of Health Risk Behavior Screening for Primary Care: Qualitative Study. J Med Internet Res. 2017 Jul 20;19(7):e261. doi: 10.2196/jmir.7474. https://www.jmir.org/2017/7/e261/ v19i7e261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Zimet G, Dixon BE, Xiao S, Tu W, Kulkarni A, Dugan T, Sheley M, Downs SM. Simple and Elaborated Clinician Reminder Prompts for Human Papillomavirus Vaccination: A Randomized Clinical Trial. Acad Pediatr. 2018 Mar;18(2S):S66–S71. doi: 10.1016/j.acap.2017.11.002.S1876-2859(17)30563-6 [DOI] [PubMed] [Google Scholar]
- 255.Zimmerman RK, Brown AE, Pavlik VN, Moehling KK, Raviotta JM, Lin CJ, Zhang S, Hawk M, Kyle S, Patel S, Ahmed F, Nowalk MP. Using the 4 Pillars Practice Transformation Program to Increase Pneumococcal Immunizations for Older Adults: A Cluster-Randomized Trial. J Am Geriatr Soc. 2017 Jan;65(1):114–122. doi: 10.1111/jgs.14451. http://europepmc.org/abstract/MED/27755655 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zimmerman RK, Moehling KK, Lin CJ, Zhang S, Raviotta JM, Reis EC, Humiston SG, Nowalk MP. Improving adolescent HPV vaccination in a randomized controlled cluster trial using the 4 Pillars™ practice Transformation Program. Vaccine. 2017 Jan 03;35(1):109–117. doi: 10.1016/j.vaccine.2016.11.018. http://europepmc.org/abstract/MED/27876200 .S0264-410X(16)31065-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zimmerman RK, Raviotta JM, Nowalk MP, Moehling KK, Reis EC, Humiston SG, Lin CJ. Using the 4 Pillars™ Practice Transformation Program to increase adolescent human papillomavirus, meningococcal, tetanus-diphtheria-pertussis and influenza vaccination. Vaccine. 2017 Oct 27;35(45):6180–6186. doi: 10.1016/j.vaccine.2017.09.039. http://europepmc.org/abstract/MED/28947346 .S0264-410X(17)31268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Daré LO, Bruand P, Gérard D, Marin B, Lameyre V, Boumédiène F, Preux P. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. 2019 Mar 13;19(1):304. doi: 10.1186/s12889-019-6623-6. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6623-6 .10.1186/s12889-019-6623-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Casey MM, Moscovice I, McCullough J. Rural primary care practices and meaningful use of electronic health records: the role of Regional Extension Centers. J Rural Health. 2014;30(3):244–51. doi: 10.1111/jrh.12050. [DOI] [PubMed] [Google Scholar]
- 260.Cross DA, Cohen GR, Nong P, Day A, Vibbert D, Naraharisetti R, Adler-Milstein J. Improving EHR Capabilities to Facilitate Stage 3 Meaningful Use Care Coordination Criteria. AMIA Annu Symp Proc. 2015;2015:448–55. http://europepmc.org/abstract/MED/26958177 . [PMC free article] [PubMed] [Google Scholar]
- 261.Shi L, Starfield B. Primary Care, Income Inequality, and Self-Rated Health in the United States: A Mixed-Level Analysis. Int J Health Serv. 2016 Jun 22;30(3):541–555. doi: 10.2190/n4m8-303m-72ua-p1k1. [DOI] [PubMed] [Google Scholar]
- 262.Krist AH, Aycock RA, Etz RS, Devoe JE, Sabo RT, Williams R, Stein KL, Iwamoto G, Puro J, Deshazo J, Kashiri PL, Arkind J, Romney C, Kano M, Nelson C, Longo DR, Wolver S, Woolf SH. MyPreventiveCare: implementation and dissemination of an interactive preventive health record in three practice-based research networks serving disadvantaged patients--a randomized cluster trial. Implement Sci. 2014 Dec 11;9:181. doi: 10.1186/s13012-014-0181-1. https://implementationscience.biomedcentral.com/articles/10.1186/s13012-014-0181-1 .s13012-014-0181-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Lee M, Lee H, Kim Y, Kim J, Cho M, Jang J, Jang H. Mobile App-Based Health Promotion Programs: A Systematic Review of the Literature. Int J Environ Res Public Health. 2018 Dec 13;15(12) doi: 10.3390/ijerph15122838. https://www.mdpi.com/resolver?pii=ijerph15122838 .ijerph15122838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Prunuske J, Chang L, Mishori R, Dobbie A, Morley CP. The extent and methods of public health instruction in family medicine clerkships. Fam Med. 2014;46(7):544–8. http://www.stfm.org/FamilyMedicine/Vol46Issue7/Prunuske544 . [PubMed] [Google Scholar]
- 265.Institute of Medicine. Board on Population Health and Public Health Practice. Committee on Integrating Primary Care and Public Health . Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 266.Bazemore AW, Makaroff LA, Puffer JC, Parhat P, Phillips RL, Xierali IM, Rinaldo J. Declining numbers of family physicians are caring for children. J Am Board Fam Med. 2012;25(2):139–40. doi: 10.3122/jabfm.2012.02.110203. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=22403191 .25/2/139 [DOI] [PubMed] [Google Scholar]
- 267.Carek PJ. Potentially Alarming Trends in the Scope of Practice for Family Physicians. J Am Board Fam Med. 2018;31(2):178–180. doi: 10.3122/jabfm.2018.02.180022. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=29535232 .31/2/178 [DOI] [PubMed] [Google Scholar]
- 268.Coutinho AJ, Cochrane A, Stelter K, Phillips RL, Peterson LE. Comparison of Intended Scope of Practice for Family Medicine Residents With Reported Scope of Practice Among Practicing Family Physicians. JAMA. 2015 Dec 08;314(22):2364–72. doi: 10.1001/jama.2015.13734.2474423 [DOI] [PubMed] [Google Scholar]
- 269.Jetty A, Jabbarpour Y, Petterson S, Eden A, Bazemore A. The Declining Presence of Family Physicians in Hospital-Based Care. J Am Board Fam Med. 2019 Nov 08;32(6):771–772. doi: 10.3122/jabfm.2019.06.190152. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=31704744 .32/6/771 [DOI] [PubMed] [Google Scholar]
- 270.Tong STC, Makaroff LA, Xierali IM, Parhat P, Puffer JC, Newton WP, Bazemore AW. Proportion of family physicians providing maternity care continues to decline. J Am Board Fam Med. 2012 May 08;25(3):270–1. doi: 10.3122/jabfm.2012.03.110256. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=22570387 .25/3/270 [DOI] [PubMed] [Google Scholar]
- 271.Xierali IM, Puffer JC, Tong STC, Bazemore AW, Green LA. The percentage of family physicians attending to women's gender-specific health needs is declining. J Am Board Fam Med. 2012 Jul 05;25(4):406–7. doi: 10.3122/jabfm.2012.04.110290. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=22773707 .25/4/406 [DOI] [PubMed] [Google Scholar]
- 272.Digital Health Center of Excellence. FDA. [2022-01-03]. https://www.fda.gov/medical-devices/digital-health-center-excellence .
- 273.Furuya-Kanamori L, Xu C, Hasan SS, Doi SA. Quality versus Risk-of-Bias assessment in clinical research. J Clin Epidemiol. 2021 Jan 13;129(2):172–175. doi: 10.1016/j.jclinepi.2020.09.044. https://linkinghub.elsevier.com/retrieve/pii/S0895-4356(20)31138-0 .S0895-4356(20)31138-0 [DOI] [PubMed] [Google Scholar]
- 274.Stephens GG. The Personal Touch: The Physician As Healer In Modern Society. J Kans Med Soc. 1965 May;66:237–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search outline using the PCC (participants, concept, and context) framework.
MEDLINE search via PubMed.
Cochrane Library search.
Embase search.
Updated MEDLINE search via PubMed.
Updated Cochrane Library search.
Updated Embase search.
Inclusion/exclusion criteria.
Description of digital health intervention categories.
Data extraction forms.
Abstracted results from included articles.


