Abstract
Background
Most dementia disorders have a clear genetic background and a number of disease genes have been identified. Mutations in the tau gene (MAPT) lead to frontotemporal dementia (FTD), whereas mutations in the genes for the amyloid-β precursor protein (APP) and the presenilins (PSEN1, PSEN2) cause early-onset, dominantly inherited forms of Alzheimer’s disease (AD).
Even if mutations causing Mendelian forms of these diseases are uncommon, elucidation of the pathogenic effects of such mutations have proven important for understanding the pathogenic processes. Here, we performed a screen to identify novel pathogenic mutations in known disease genes among patients undergoing dementia investigation.
Results
Using targeted exome sequencing we have screened all coding exons in eleven known dementia genes (PSEN1, PSEN2, APP, MAPT, APOE, GRN, TARDBP, CHMP2B, TREM2, VCP and FUS) in 102 patients with AD, FTD, other dementia diagnoses or mild cognitive impairment.
We found three AD patients with two previously identified pathogenic mutations in PSEN1 (Pro264Leu and Met146Val). In this screen, we also identified the recently reported APP mutation in two siblings with AD. This mutation, named the Uppsala mutation, consists of a six amino acid intra-amyloid β deletion.
In addition, we found several potentially pathogenic mutations in PSEN2, FUS, MAPT, GRN and APOE. Finally, APOE ε4 was prevalent in this patient group with an allele frequency of 54%.
Conclusions
Among the 102 screened patients, we found two disease causing mutations in PSEN1 and one in APP, as well as several potentially pathogenic mutations in other genes related to neurodegenerative disorders. Apart from giving important information to the clinical investigation, the identification of disease mutations can contribute to an increased understanding of disease mechanisms.
Keywords: Alzheimer's disease, Frontotemporal dementia, Neurodegenerative disorders, PSEN1, PSEN2, APP, MAPT, APOE, Exome sequencing
Introduction
Mutations in the genes for the amyloid-β precursor protein (APP) and the presenilins (PSEN1 and PSEN2) cause early-onset, dominantly inherited forms of Alzheimer’s disease (AD), whereas mutations in the MAPT gene mainly lead to frontotemporal dementia (FTD). The elucidation of the pathogenic effects of such mutations has proven important for the understanding of the respective disease processes.
Alzheimer’s disease is neuropathologically characterized by the formation and extracellular deposition of insoluble plaques, consisting of the 38–43 amino acid long peptide amyloid-β (Aβ) and intracellular neurofibrillary tangles of the tau protein, as well as a substantial neuronal loss [1]. According to the amyloid cascade hypothesis, AD is initiated by increased levels or a changed conformation of Aβ which can promote the formation of toxic oligomers and protofibrils before the formation of insoluble plaques [2]. We have previously identified and characterized two different APP mutations, the Swedish mutation [3] and the Arctic mutation [4]. Functional analyses of these mutations have significantly increased our understanding of the disease pathogenesis. Whereas the Swedish mutation results in an increased cleavage by β-secretase and thereby elevated levels of all forms of Aβ [5, 6], the Arctic mutation leads to a conformational change of Aβ and increased formation of toxic Aβ protofibrils [7]. Moreover, mutations in PSEN1 and PSEN2 have been shown to increase the generation of the longer and more aggregation prone form of Aβ (Aβ42).
Recently, several new genes causing dementia disorders have been identified. Such discoveries have been important to increase our knowledge of the aetiology behind these disorders. Most notably, the understanding of frontotemporal dementia has been further advanced by the identification of disease causing mutations in the genes for TAR DNA-binding protein-43 (TARDBP), progranulin (GRN) and C9orf72-SMCR8 complex subunit (C9ORF72) [8–12]. Moreover, discoveries of rare variants in the triggering receptor expressed on myeloid cells 2 (TREM2) gene have highlighted the involvement of immunological and inflammatory pathways in AD pathogenesis [13, 14].
The development of next generation sequencing technologies has enabled identification of new mutations in previously known as well as in novel disease genes [15]. Furthermore, there is growing evidence that mutation screening may yield interesting findings also in patients with late onset disease forms [16].
In this study we have performed exome sequencing of eleven potential disease genes (PSEN1, PSEN2, APP, MAPT, APOE, GRN, TARDBP, CHMP2B, TREM2, VCP and FUS) in patients with AD and other neurodegenerative diseases for whom an early disease onset and/or a familial pattern of inheritance had been reported.
Results
Three different disease causing mutations and several mutations with potential pathogenicity were identified in the screened gene regions (Table 1).
Table 1.
Clinical characteristics of patients with known or potentially pathogenic mutations
| Patient No | Diagnosis | Gender | Onset age | Heredity | Protein change (dbSNP) | APOE | Function | Pathogenic | Population frequencya | SIFT scoreb | PolyPhen-2 scoreb |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | AD | F | 50 | Yes | PSEN1 P264L (rs63750301) | ε3/ε4 | Missense | Yes | 0.0000040 | 0 | 1 |
| 2 | AD | M | 42 | Yes | PSEN1 P264L (rs63750301) | ε3/ε4 | Missense | Yes | 0.0000040 | 0 | 1 |
| 3 | AD | M | 34 | No | PSEN1 M146V (rs63750306) | ε3/ε3 | Missense | Yes | - | 0.01 | 0.985 |
| 4 | AD | M | 65 | Yes | PSEN2 I144L (rs764718172) | ε3/ε3 | Missense | Unknown | 0.0000080 | 0.01 | 0.257 |
| 5 | bvFTD | M | 69 | Yes | PSEN2 A252T (rs138836272) | ε3/ε3 | Missense | Unknown | 0.00023 | 0.42 | 0.172 |
| FUS Δ229-231 (rs767564995) | Deletion | Unknown | 0.00021 | - | - | ||||||
| 6 | AD | M | 59 | Yes | FUS Ser57Δ (rs777545405) | ε4/ε4 | Deletion | Unknown | 0.00017 | - | - |
| 7 | svPPA | M | 64 | Yes | FUS Δ166-167 (rs537605135) | ε4/ε4 | Deletion | Unknown | 0.00030 | - | - |
| 8 | AD | F | 57 | Yes | GRN A324V (rs758636128) | ε3/ε3 | Missense | Unknown | 0.000024 | 0.21 | 0.129 |
| 9 | AD | M | 59 | Yes | MAPT V224G (rs141120474) | ε4/ε4 | Missense | Unknown | 0.0021 | 0 | 0.187 |
| 10 | MCI | M | 61 | Yes | MAPT A239T (rs63750096) | ε3/ε4 | Missense | Unknown | 0.00063 | 0.27 | 0.079 |
| 11 | AD | M | 56 | Yes | APOE R269G (rs267606661) | ε3/ε4 | Missense | Unknown | 0.00036 | 0 | 0.533 |
| 12 | AD | M | 44 | Yes | APP Δ690-695 | ε3/ε3 | Deletion | Yes | - | - | - |
| 13 | AD | M | 40 | Yes | APP Δ690-695 | ε3/ε3 | Deletion | Yes | - | - | - |
aPopulation frequency was obtained from gnomAD database, except for rs767564995 for which dbSNP was used
bPolyPhen-2 and SIFT scores were obtained using Ensembl Variant Effect Predictor. These scores are used to predict whether amino acid substitution is likely to affect protein function. The SIFT score ranges from 0.0 (deleterious) to 1.0 (tolerated). The PolyPhen-2 score ranges from 0.0 (tolerated) to 1.0 (deleterious)
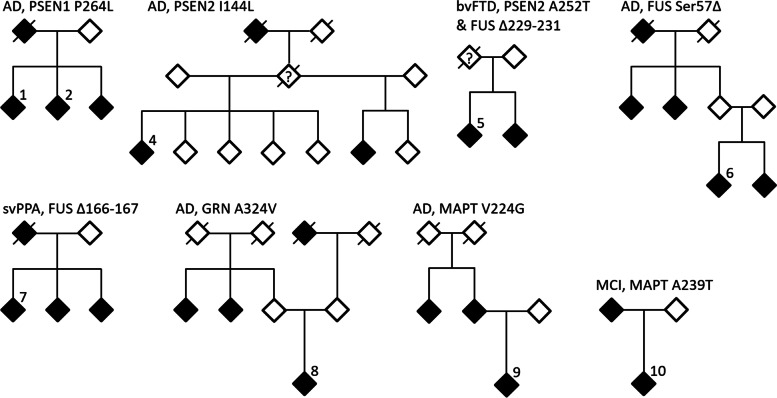
We found two pathogenic mutations in the PSEN1 gene, both of which had been previously reported [17–19]. The PSEN1 P264L (rs63750301) mutation was detected in two siblings with AD. In the same family, the father and another sibling also suffered from the disease, although DNA samples were not available from them (Fig. 1). The age at onset in this family was reported to be 40–50 years. The siblings suffered from global cognitive impairment and early personality changes and both displayed a clear hypometabolism in posterior temporo-parietal cortex on FDG-PET. The other PSEN1 mutation, M146V (rs63750306), was identified in an AD patient who had presented with slight short term memory dysfunction and spatial disorientation already at about 30 years of age. At later disease stages the patient suffered from myoclonic epileptic seizures and gait difficulties. A widespread bilateral parietal hypometabolism with involvement also of temporal and frontal cortices was observed on FDG-PET. Interestingly, no heredity had been reported in this family.
Fig. 1.
Pedigrees of the families in which mutations were identified. The analyzed cases are indicated by numbers. Each pedigee is labeled by diagnosis and the nature of the mutation(s) identified. Filled symbols are affected family members. Slashed symbols are used for individuals known to be deceased. The numbers refer to the screened patients, corresponding to Table 1
In the Aβ coding sequence of the APP gene we identified the recently reported eighteen base pair deletion, which causes a six amino acid deletion in the protein sequence. This in frame deletion, named the Uppsala mutation, was found in two siblings and a cousin suffering from an aggressive early onset form of AD. A typical pattern of autosomal dominant inheritance and age at disease onset of 40–50 years had been reported in earlier generations of the family [20]. We have also analyzed more than 500 DNA samples from Swedish AD patients, older family members, and older healthy control subjects, without finding any other cases with this mutation. Furthermore, we extensively studied clinical and pathological features of this deletion and the data strongly suggest that the Uppsala mutation is the cause of AD in this family [20].
In addition to these pathogenic mutations, several mutations with potential pathogenicity were identified. In one individual with AD and a known family history of dementia we found a Ser57 deletion (rs777545405) in FUS (Fig. 1). This deletion had been previously reported as likely pathogenic in a patient with sporadic amyotrophic lateral sclerosis (ALS) [21]. Our patient had experienced memory problems before the age of 60 years, but no typical ALS symptoms had been reported. In addition, two other deletions in FUS were found in patients with behavioral variant FTD (bvFTD) and semantic variant primary progressive aphasia (svPPA), respectively (Table 1).
In PSEN2, the A252T mutation (rs138836272) was identified in a patient with the behavioral variant of FTD (bvFTD), also carrying the Δ229-231 deletion in FUS (Fig. 1 and Table 1). The PSEN2 A252T mutation had been previously reported in African healthy controls [22] and its pathogenicity is thus unclear. In addition, PSEN2 I144L (rs764718172), which has not been reported in any previous studies, was found in an AD patient with a family history of disease (Fig. 1).
Since APOE was included in our next generation sequencing analysis, we examined all APOE exons for possible mutations. In one patient with early onset AD we identified the R269G (rs267606661) mutation. This APOE mutation had previously been reported as a likely cause of autosomal dominant hypercholesterolemia [23].
Moreover, three rare genetic variants with potential pathogenicity were found in MAPT and GRN (Fig. 1 and Table 1), whereas no variants that are likely to be pathogenic could be identified in TARDBP, CHMP2B and VCP.
Analyses of conventional APOE alleles in the total sample set showed an ε4 allele frequency of 54%. Of the 102 patients, 32 were homozygous for ε4 and 45 had the ε3ε4 genotype. When only including the 77 AD cases in the analysis, a slightly higher APOE ε4 allele frequency was observed (57%) (Table 2).
Table 2.
Description of the study population
| Disease | Number of patients, n | Known heredity, n (%) | Females, n (%) | Age at onset, mean (range) |
|---|---|---|---|---|
| Alzheimer’s disease | 77 | 70 (90.9) | 36 (46.8) | 60.8 (34–76) |
| Behavioral variant of frontotemporal dementia | 7 | 7 (100) | 2 (28.6) | 59.1 (47–69) |
| Other types of frontotemporal dementia | 4 | 3 (75) | 1 (25) | 60.8 (54–71) |
| Semantic variant primary progressive aphasia | 5 | 4 (80) | 2 (40) | 58,2 (49–64) |
| Other dementia related diagnosesa | 2 | 1 (50.0) | 0 (0) | 65.0 (55–75) |
| Mild cognitive impairmentb | 7 | 7 (100) | 4 (57.1) | 59.4 (55–65) |
aIn this group one patient had vascular dementia and one unspecified dementia
bMost patients with MCI had a known heredity for AD
We also included TREM2 in our analyses, since several studies have recently reported that rare variants in this gene could confer an increased AD risk similar to APOE ε4 [13, 24]. We found that eight AD and two patients with mild cognitive impairment (MCI) were carriers of the TREM2 R62H allele (rs143332484), which gives an allele frequency of 4.9%. This is significantly higher than what has been previously reported in European populations [25]. Interestingly, also the two AD patients with the Uppsala mutation were found to carry the TREM2 R62H allele.
Discussion
In this study, we have screened 102 patients with AD or FTD from our Memory clinic and identified several pathogenic mutations causing AD. We also found two PSEN1 mutations, P264L and M146V. Both of these mutations have been previously described as pathogenic, causing autosomal dominantly inherited disease forms [17–19]. The approximate onset age of PSEN1 P264L patients had been reported at 45 years, which corresponds well to the onset ages of our patients. Despite the fact that all individuals with this mutation get dementia at an early age, there is an interindividual variation of symptoms. In the study by Martikainen et al., one of the three patients carrying this mutation displayed spastic paraparesis, whereas the other two patients presented with parkinsonism. With respect to neuropathology, all three cases exhibited abundant cotton wool plaques in the brain at autopsy [18].
The PSEN1 M146V mutation usually causes early onset AD with an onset age at about 40 years [26]. Two mutation-carrying patients from a previously described large Swedish/Finnish family showed global cortical glucose hypometabolism, which was further accentuated over time. Brain examination revealed considerably higher numbers of neuritic plaques and neurofibrillary tangles in all examined brain regions, as compared to sporadic AD patients. Similar to our patient, epileptic seizures were observed in both patients described in this study [27].
The recently reported deletion in APP, resulting in a six amino acid shorter version of the Aβ peptide, is to our knowledge the first dominantly inherited form of AD caused by a large deletion in Aβ [20]. Previously, only a single amino acid deletion within the Aβ sequence has been reported in a Japanese family. This APP mutation was described to have a recessive mode of inheritance and seems to cause disease due to an increased oligomerization and higher resistance to proteolytic degradation of Aβ [28]. As recently described, the Uppsala APP mutation causes increased Aβ generation by altering α-secretase and β-secretase cleavages of APP. Furthermore, the Uppsala Aβ mutant adopts unique polymorphs that accelerate the formation of fibrils and their deposition into amyloid plaques [20].
The Ser57 deletion in FUS and the R269G mutation in APOE have been previously reported, although clinical data from patients and data about functional consequences of these mutations are still limited. Nevertheless, the clinical presentation of the reported cases seems to be very different from our patients [21, 23].
Several other mutations identified in our study have been previously reported in genetic analyses of AD and other dementia disorders. The MAPT A239T variant was described in an FTD patient carrying pathogenic deletion in GRN gene [29]. The MAPT V224G was reported in several studies and found in both AD patients and controls [16, 30]. The PSEN2 A252T mutation, affecting an amino acid residue that is conserved between PSEN1 and PSEN2, was found in two controls from the Mandenka and Yoruba samples [22]. Nevertheless, only very few individuals with these mutations have been reported and further analyses are necessary in order to examine their possible pathogenic role.
The APOE ε4 allele is the strongest risk factor for late onset AD [31]. In the general Caucasian population APOE ε4 frequency is around 10–15% whereas in AD a frequency of 25–35% is usually reported [32, 33]. Thus the high APOE ε4 frequency of over 50% in the patients included in our study, confirms that APOE is of importance also in familial dementia [34–36]. Much more surprising was that the frequency of the TREM2 R62H allele was as high as 4.9%, whereas the allele frequency reported in dbSNP for this variant was just about 1% in most European and American populations. In the first study investigating a potential association of TREM2 R62H to AD, this polymorphism was not associated with disease [14]. However, in another study of 85 133 subjects, a strongly significant association between AD and TREM2 R62H was found, although the allele frequency was low (1.4% in AD cases and 0.9% in controls) [25].
In this study we used a sequence enrichment technology together with next generation sequencing in order to screen target genes. An advantage of this method is its cost efficiency combined with the high quality of sequencing data. The main limitation of the technique is that only already known disease genes can be analyzed. Another limitation is that it cannot be used to analyze the structural variants, like deletions and insertions, and repetitive sequences like the hexanucleotide repeat expansions in C9ORF72 causing FTD [11, 12]. Furthermore, a number of genes associated with increased susceptibility for AD have been identified [37, 38]. Variations in several of these genes, such as CR1, SORL1, BACE1, ABCA7, could also predispose for familial early onset form of the disease [39, 40]. Some of the families included in our study have rather complex patterns of inheritance (Fig. 1) and we can therefore not exclude that combination of variants in several genes can be disease causative. Nevertheless, PSEN1, PSEN2 and APP mutations are the main causes of autosomal-dominant early-onset AD, whereas mutations in MAPT and GRN account for a significant part of genetic FTD [41–43].
In conclusion, in our screen of 102 AD, FTD and MCI patients with early onset and/or signs of heredity we found two previously described PSEN1 mutations, the recently described Uppsala APP deletion and a number of other potentially pathogenic mutations. Screening for mutations in known and putative disease susceptibility genes can aid in the clinical diagnosis of dementia patients. Moreover, such screening could enable us to discover additional disease mechanisms that can be targeted by novel therapeutic strategies.
Methods
Selection of patients and controls
A selection of 102 patients who attended the Memory clinic at Uppsala University Hospital during 2006–2019 were recruited to the study. The included patients had been diagnosed with either AD, FTD, another dementia disorder or mild cognitive impairment. Moreover, they had displayed a disease onset before 65 years of age and/or had reported at least one first degree relative diagnosed with a dementia disorder. The diagnoses were based on established criteria including analysis of cerebrospinal fluid biomarkers of AD in most cases [44–48]. The patient information is summarized in Table 2. Available pedigrees for patients with identified mutations are presented in the Fig. 1. The pedigree for the patients with the Uppsala mutation was recently published [20].
Gene selection
Nine genes with known pathogenic mutations causing familial early onset dementia diseases were included in the analyses (APP, PSEN1, PSEN2, MAPT, GRN, TARDBP, CHMP2B, VCP and FUS). In addition, we analyzed TREM2 in which rare variants have been associated with an increased risk of AD [14, 25]. We also included APOE in order to determine the ε2-4 genotypes. The gene information is summarized in Table 3.
Table 3.
Gene list
| Gene name | Gene symbol | Chromosome | Associated disease |
|---|---|---|---|
| Presenilin 2 | PSEN2 | chr01 | AD, FTD |
| TDP-43, TAR DNA binding protein | TARDBP | chr01 | FTD, ALS |
| Charged multivesicular body protein 2B | CHMP2B | chr03 | FTD, AD |
| Triggering receptor expressed on myeloid cells 2 | TREM2 | chr06 | AD |
| Valosin containing protein | VCP | chr09 | ALS, FTD |
| Presenilin 1 | PSEN1 | chr14 | AD, FTD |
| FUS RNA binding protein | FUS | chr16 | FTD, ALS |
| Granulin | GRN | chr17 | FTD |
| Microtubule-associated protein tau | MAPT | chr17 | AD, FTD |
| Apolipoprotein E | APOE | chr19 | AD |
| Amyloid-β precursor protein | APP | chr21 | AD |
Targeted exome sequencing
Genomic DNA from the whole-blood samples was extracted by a commercially available kit (Chemagen, Germany) at the Karolinska institute biobank or by QIAamp DNA Blood Maxi Kit (Qiagen, Germany). All selected exons, including at least 25 nucleotides surrounding the exonic regions, were amplified either using Agilent SureSelect custom design kit or Life Technologies AmpliSeq sequence enrichment method. The amplified DNA was analyzed by Illumina MiSeq or Life Technologies IonTorrent sequencing, respectively. The average target coverage was over 97% for both methods. Targeted exome sequencing was performed at the Uppsala Genome Center using standardized protocols provided by the manufacturer.
Bioinformatics
Sequenced gene regions were aligned to the human reference genome (assembly hg19). Sequence variations were visualized using Integrated Genome Viewer [49]. Annotation of single nucleotide polymorphisms (SNPs) and small insertions or deletions was performed using Ensembl Variant Effect Predictor (http://grch37.ensembl.org/), NCBI SNP database dbSNP (https://www.ncbi.nlm.nih.gov/snp/), Genome Aggregation Database gnomAD (https://gnomad.broadinstitute.org/) and Alzheimer’s disease mutation database (https://www.alzforum.org/mutations).
Acknowledgements
We would like to thank all study participants and the staff at the Memory clinic at Uppsala University Hospital for their cooperation.
Abbreviations
- AD
Alzheimer’s disease
- ALS
Amyotrophic lateral sclerosis
- APOE
Apolipoprotein E
- APP
Amyloid-β precursor protein
- Aβ
Amyloid-β
- bvFTD
Behavioral variant of FTD
- C9ORF72
C9orf72-SMCR8 complex subunit
- CHMP2B
Charged multivesicular body protein 2B
- FDG-PET
Fluorodeoxyglucose positron emission tomography
- FTD
Frontotemporal dementia
- FUS
FUS RNA binding protein
- GRN
Granulin
- MAPT
Microtubule-associated protein tau
- MCI
Mild cognitive impairment
- PSEN1
Presenilin 1
- PSEN2
Presenilin 2
- SNP
Single nucleotide polymorphism
- svPPA
Semantic variant of primary progressive aphasia
- TARDBP
TDP-43, TAR DNA binding protein
- TREM2
Triggering receptor expressed on myeloid cells 2
- VCP
Valosin containing protein
Authors’ contributions
MI, LL and VG designed the study. RMB, ML, LK and MI were responsible for the patient recruitment and clinical information collection. VG planned and organized DNA preparation and sequencing. MPV, CN and VG were responsible for the sequencing data analysis. All authors participated in the interpretation of data, editing of the manuscript, as well as reading and approving of the final manuscript.
Funding
Open access funding provided by Uppsala University. This work was supported by the Swedish Research Council (#2016–02120); the Swedish Alzheimer Foundation and Uppsala University Hospital.
Availability of data and materials
Amyloid-β precursor protein exon 17 nucleotide sequence for the Uppsala mutation is available from GenBank (https://www.ncbi.nlm.nih.gov/genbank/, accession number MW892394). Gene based sequencing data summary is available from the corresponding author.
Declarations
Ethics approval and consent to participate
The study had been approved by the Regional Ethical Committee in Uppsala, Sweden (2005–244/Ö 48–2205) and the Swedish Ethics Review Authority (2020–03703). All study participants had provided written informed consent for participation and legal guardian/next of kin provided informed consent for patients with psychiatric disorders. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Braak H, Del Trecidi K. Neuroanatomy and pathology of sporadic Alzheimer’s disease. Adv Anat Embryol Cell Biol. 2015;215:1–162. [PubMed]
- 2.Selkoe DJ. Alzheimer’s disease is a synaptic failure. Science. 2002;298:789–791. doi: 10.1126/science.1074069. [DOI] [PubMed] [Google Scholar]
- 3.Mullan M, Crawford F, Axelman K, Houlden H, Lilius L, Winblad B, Lannfelt L. A pathogenic mutation for probable Alzheimer’s disease in the APP gene at the N-terminus of beta-amyloid. Nat Genet. 1992;1:345–7. [DOI] [PubMed]
- 4.Nilsberth C, Westlind-Danielsson A, Eckman CB, Condron MM, Axelman K, Forsell C, Stenh C, Luthman J, Teplow DB, Younkin SG, et al. The “Arctic” APP mutation (E693G) causes Alzheimer’s disease by enhanced Abeta protofibril formation. Nat Neurosci. 2001;4:887–93. [DOI] [PubMed]
- 5.Citron M, Vigo-Pelfrey C, Teplow DB, Miller C, Schenk D, Johnston J, Winblad B, Venizelos N, Lannfelt L, Selkoe DJ. Excessive production of amyloid beta-protein by peripheral cells of symptomatic and presymptomatic patients carrying the Swedish familial Alzheimer disease mutation. Proc Natl Acad Sci U S A. 1994;91:11993–7. [DOI] [PMC free article] [PubMed]
- 6.Johnston JA, Cowburn RF, Norgren S, Wiehager B, Venizelos N, Winblad B, Vigo-Pelfrey C, Schenk D, Lannfelt L, O’Neill C. Increased beta-amyloid release and levels of amyloid precursor protein (APP) in fibroblast cell lines from family members with the Swedish Alzheimer’s disease APP670/671 mutation. FEBS Lett. 1994;354:274–8. [DOI] [PubMed]
- 7.Johansson AS, Berglind-Dehlin F, Karlsson G, Edwards K, Gellerfors P, Lannfelt L. Physiochemical characterization of the Alzheimer’s disease-related peptides A beta 1–42Arctic and A beta 1–42wt. FEBS J. 2006;273:2618–2630. doi: 10.1111/j.1742-4658.2006.05263.x. [DOI] [PubMed] [Google Scholar]
- 8.Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, Snowden J, Adamson J, Sadovnick AD, Rollinson S, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442:916–919. doi: 10.1038/nature05016. [DOI] [PubMed] [Google Scholar]
- 9.Benajiba L, Le Ber I, Camuzat A, Lacoste M, Thomas-Anterion C, Couratier P, Legallic S, Salachas F, Hannequin D, Decousus M, et al. TARDBP mutations in motoneuron disease with frontotemporal lobar degeneration. Ann Neurol. 2009;65:470–473. doi: 10.1002/ana.21612. [DOI] [PubMed] [Google Scholar]
- 10.Cruts M, Gijselinck I, van der Zee J, Engelborghs S, Wils H, Pirici D, Rademakers R, Vandenberghe R, Dermaut B, Martin JJ, et al. Null mutations in progranulin cause ubiquitin-positive frontotemporal dementia linked to chromosome 17q21. Nature. 2006;442:920–924. doi: 10.1038/nature05017. [DOI] [PubMed] [Google Scholar]
- 11.DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J, et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron. 2011;72:245–256. doi: 10.1016/j.neuron.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Renton AE, Majounie E, Waite A, Simon-Sanchez J, Rollinson S, Gibbs JR, Schymick JC, Laaksovirta H, van Swieten JC, Myllykangas L, et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72:257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, Bjornsson S, Huttenlocher J, Levey AI, Lah JJ, et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N Engl J Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, Cruchaga C, Sassi C, Kauwe JS, Younkin S, et al. TREM2 variants in Alzheimer’s disease. N Engl J Med. 2013;368:117–27. [DOI] [PMC free article] [PubMed]
- 15.Pimenova AA, Raj T, Goate AM. Untangling Genetic Risk for Alzheimer’s Disease. Biol Psychiatry. 2018;83:300–310. doi: 10.1016/j.biopsych.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sassi C, Guerreiro R, Gibbs R, Ding J, Lupton MK, Troakes C, Al-Sarraj S, Niblock M, Gallo JM, Adnan J, et al. Investigating the role of rare coding variability in Mendelian dementia genes (APP, PSEN1, PSEN2, GRN, MAPT, and PRNP) in late-onset Alzheimer’s disease. Neurobiol Aging. 2014;35:2881 e2881–2881 e2886. doi: 10.1016/j.neurobiolaging.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campion D, Flaman JM, Brice A, Hannequin D, Dubois B, Martin C, Moreau V, Charbonnier F, Didierjean O, Tardieu S, et al. Mutations of the presenilin I gene in families with early-onset Alzheimer’s disease. Hum Mol Genet. 1995;4:2373–2377. doi: 10.1093/hmg/4.12.2373. [DOI] [PubMed] [Google Scholar]
- 18.Martikainen P, Pikkarainen M, Pontynen K, Hiltunen M, Lehtovirta M, Tuisku S, Soininen H, Alafuzoff I. Brain pathology in three subjects from the same pedigree with presenilin-1 (PSEN1) P264L mutation. Neuropathol Appl Neurobiol. 2010;36:41–54. doi: 10.1111/j.1365-2990.2009.01046.x. [DOI] [PubMed] [Google Scholar]
- 19.Wasco W, Pettingell WP, Jondro PD, Schmidt SD, Gurubhagavatula S, Rodes L, DiBlasi T, Romano DM, Guenette SY, Kovacs DM, et al. Familial Alzheimer’s chromosome 14 mutations. Nat Med. 1995;1:848. doi: 10.1038/nm0995-848a. [DOI] [PubMed] [Google Scholar]
- 20.Pagnon de la Vega M, Giedraitis V, Michno W, Kilander L, Guner G, Zielinski M, Lowenmark M, Brundin R, Danfors T, Soderberg L, et al. The Uppsala APP deletion causes early onset autosomal dominant Alzheimer’s disease by altering APP processing and increasing amyloid beta fibril formation. Sci Transl Med. 2021;13(606):eabc6184. [DOI] [PubMed]
- 21.Belzil VV, Valdmanis PN, Dion PA, Daoud H, Kabashi E, Noreau A, Gauthier J, team SD, Hince P, Desjarlais A, et al. Mutations in FUS cause FALS and SALS in French and French Canadian populations. Neurology. 2009;73:1176–1179. doi: 10.1212/WNL.0b013e3181bbfeef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guerreiro RJ, Baquero M, Blesa R, Boada M, Bras JM, Bullido MJ, Calado A, Crook R, Ferreira C, Frank A, et al. Genetic screening of Alzheimer’s disease genes in Iberian and African samples yields novel mutations in presenilins and APP. Neurobiol Aging. 2010;31:725–731. doi: 10.1016/j.neurobiolaging.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marduel M, Ouguerram K, Serre V, Bonnefont-Rousselot D, Marques-Pinheiro A, Erik Berge K, Devillers M, Luc G, Lecerf JM, Tosolini L, et al. Description of a large family with autosomal dominant hypercholesterolemia associated with the APOE p.Leu167del mutation. Hum Mutat. 2013;34:83–87. doi: 10.1002/humu.22215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou SL, Tan CC, Hou XH, Cao XP, Tan L, Yu JT. TREM2 Variants and Neurodegenerative Diseases: A Systematic Review and Meta-Analysis. J Alzheimers Dis. 2019;68:1171–1184. doi: 10.3233/JAD-181038. [DOI] [PubMed] [Google Scholar]
- 25.Sims R, van der Lee SJ, Naj AC, Bellenguez C, Badarinarayan N, Jakobsdottir J, Kunkle BW, Boland A, Raybould R, Bis JC, et al. Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer’s disease. Nat Genet. 2017;49:1373–1384. doi: 10.1038/ng.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alzheimer’s Disease Collaborative G The structure of the presenilin 1 (S182) gene and identification of six novel mutations in early onset AD families. Nat Genet. 1995;11:219–222. doi: 10.1038/ng1095-219. [DOI] [PubMed] [Google Scholar]
- 27.Scholl M, Almkvist O, Bogdanovic N, Wall A, Langstrom B, Viitanen M, Nordberg A. Time course of glucose metabolism in relation to cognitive performance and postmortem neuropathology in Met146Val PSEN1 mutation carriers. J Alzheimers Dis. 2011;24:495–506. doi: 10.3233/JAD-2011-101563. [DOI] [PubMed] [Google Scholar]
- 28.Tomiyama T, Nagata T, Shimada H, Teraoka R, Fukushima A, Kanemitsu H, Takuma H, Kuwano R, Imagawa M, Ataka S, et al. A new amyloid beta variant favoring oligomerization in Alzheimer’s-type dementia. Ann Neurol. 2008;63:377–387. doi: 10.1002/ana.21321. [DOI] [PubMed] [Google Scholar]
- 29.Pickering-Brown SM, Richardson AM, Snowden JS, McDonagh AM, Burns A, Braude W, Baker M, Liu WK, Yen SH, Hardy J, et al. Inherited frontotemporal dementia in nine British families associated with intronic mutations in the tau gene. Brain. 2002;125:732–751. doi: 10.1093/brain/awf069. [DOI] [PubMed] [Google Scholar]
- 30.Jin SC, Pastor P, Cooper B, Cervantes S, Benitez BA, Razquin C, Goate A, Ibero-American Alzheimer Disease Genetics Group R. Cruchaga C. Pooled-DNA sequencing identifies novel causative variants in PSEN1, GRN and MAPT in a clinical early-onset and familial Alzheimer’s disease Ibero-American cohort. Alzheimers Res Ther. 2012;4:34. doi: 10.1186/alzrt137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 32.Seshadri S, Drachman DA, Lippa CF. Apolipoprotein E epsilon 4 allele and the lifetime risk of Alzheimer’s disease. What physicians know, and what they should know. Arch Neurol. 1995;52:1074–1079. doi: 10.1001/archneur.1995.00540350068018. [DOI] [PubMed] [Google Scholar]
- 33.Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R, Myers RH, Pericak-Vance MA, Risch N, van Duijn CM. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer disease meta analysis consortium. JAMA. 1997;278:1349–1356. [PubMed] [Google Scholar]
- 34.Bonvicini C, Scassellati C, Benussi L, Di Maria E, Maj C, Ciani M, Fostinelli S, Mega A, Bocchetta M, Lanzi G, et al. Next generation sequencing analysis in early onset dementia patients. J Alzheimers Dis. 2019;67:243–256. doi: 10.3233/JAD-180482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giedraitis V, Hedlund M, Skoglund L, Blom E, Ingvast S, Brundin R, Lannfelt L, Glaser A. New Alzheimer’s disease locus on chromosome 8. J Med Genet. 2006;43:931–935. doi: 10.1136/jmg.2006.043000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Duijn CM, de Knijff P, Cruts M, Wehnert A, Havekes LM, Hofman A, Van Broeckhoven C. Apolipoprotein E4 allele in a population-based study of early-onset Alzheimer’s disease. Nat Genet. 1994;7:74–78. doi: 10.1038/ng0594-74. [DOI] [PubMed] [Google Scholar]
- 37.Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, DeStafano AL, Bis JC, Beecham GW, Grenier-Boley B, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, Boland A, Vronskaya M, van der Lee SJ, Amlie-Wolf A, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Abeta, tau, immunity and lipid processing. Nat Genet. 2019;51:414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qiu G, Zhu FQ, Xu C. Identification of two pathogenic mutations in SORL1 in early-onset Alzheimer’s disease. J Clin Neurosci. 2021;89:243–248. doi: 10.1016/j.jocn.2021.05.020. [DOI] [PubMed] [Google Scholar]
- 40.Giau VV, Senanarong V, Bagyinszky E, An SSA, Kim S. Analysis of 50 Neurodegenerative genes in clinically diagnosed early-onset Alzheimer’s disease. Int J Mol Sci. 2019;20:1514. doi: 10.3390/ijms20061514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cacace R, Sleegers K, Van Broeckhoven C. Molecular genetics of early-onset Alzheimer’s disease revisited. Alzheimers Dement. 2016;12:733–748. doi: 10.1016/j.jalz.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 42.Carmona S, Hardy J, Guerreiro R. The genetic landscape of Alzheimer disease. Handb Clin Neurol. 2018;148:395–408. doi: 10.1016/B978-0-444-64076-5.00026-0. [DOI] [PubMed] [Google Scholar]
- 43.Olszewska DA, Lonergan R, Fallon EM, Lynch T. Genetics of frontotemporal dementia. Curr Neurol Neurosci Rep. 2016;16:107. doi: 10.1007/s11910-016-0707-9. [DOI] [PubMed] [Google Scholar]
- 44.Chui HC, Victoroff JI, Margolin D, Jagust W, Shankle R, Katzman R. Criteria for the diagnosis of ischemic vascular dementia proposed by the State of California Alzheimer’s disease diagnostic and treatment centers. Neurology. 1992;42:473–480. doi: 10.1212/wnl.42.3.473. [DOI] [PubMed] [Google Scholar]
- 45.Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–1014. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, van Swieten JC, Seelaar H, Dopper EG, Onyike CU, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–2477. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, Nordberg A, Backman L, Albert M, Almkvist O, et al. Mild cognitive impairment–beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 49.Thorvaldsdottir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14:178–192. doi: 10.1093/bib/bbs017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Amyloid-β precursor protein exon 17 nucleotide sequence for the Uppsala mutation is available from GenBank (https://www.ncbi.nlm.nih.gov/genbank/, accession number MW892394). Gene based sequencing data summary is available from the corresponding author.