Abstract
Background:
After new cancer data are released in April 2021, it is important to update the incidence trend in breast cancer from 2000 to 2018 and focus on ethnic disparities in the risk of developing breast cancer.
Methods:
We identified 1,129,564 women who were diagnosed with incident breast cancer at age ≥20 in 2000–2018 from 18 SEER (Surveillance, Epidemiology, and End Results) registries. We utilized the SEER*Stat software to calculate age-adjusted incidence rates.
Results:
Overall age-adjusted incidence rate of breast cancer was the highest in non-Hispanic white (NHW) women (190.4 cases per 100,000 women), followed by NH-black (NHB) (178.4), Asian/Pacific-Islanders (API) (141.3), Hispanic (133.3) and American-Indians/Alaska-Native (AIAN) women (128.8). Annual percentage change (APC) from 2000 to 2018 showed that annual increase was statistically significant for API (APC: 1.0, 95% CI: 0.8–1.3), NHB (APC: 0.5, 0.2–0.7), AIAN (1.6, 1.1–2.2), and Hispanic women (0.4, 0.2–0.7), but annual percentage of incidence did not significantly decrease for NHW (−0.1, −0.4 to −0.1). Incidence rates of hormone-receptor positive breast cancer increased from 2000 to 2018 in all ethnic women, while incidence rates of hormone-receptor negative breast cancer decreased. NHW and NHB women had a significantly higher risk of having breast cancer than API women. In 2012–2018, the risks of having local stage and distant stage breast cancer for NHW (1.31, 1.29–1.33 and 1.19, 1.16–1.21) and NHB (1.09, 1.07–1.11 and 1.31, 1.28–1.35) women were significantly higher than that of API women.
Conclusions:
The incidence of hormone-receptor positive breast cancer increased in all ethnic women from 2000 to 2018 while the incidence of hormone-receptor negative breast cancer decreased. There were still substantial racial disparities in breast cancer incidences.
Keywords: breast cancer, incidence rate, incidence trend, racial disparities, SEER areas
International studies have shown consistently that the incidence of female breast cancer was much higher in women of Europe and north America than in Asian women.1–11 For example, age-standardized female breast cancer incidence rates in 2006–2007 were 95.3, 94.5 and 88.6 cases per 100,000 women for the Netherland, France and USA as compared to 43.3, 43.2, and 25.6 cases per 100,000 women for Japan, China, and Thailand, respectively.2 These higher incidence rates were attributed to multiple factors, including low parity, delayed marriage and childbirth, low breast feeding, increased cancer screening, work and life related stress, lack of exercise, higher obesity rate, higher alcohol consumption and smoking, and differential food intakes.12–28 However, the increasing incidence in breast cancer in Asian women have been observed over the past 3 decades,2,29–35 largely due to adaption of western-style diets and lifestyle.2 Some international and migration studies found that those Asian women who immigrated to Europe or north America had higher breast cancer incidence rates than those women who continued to live in Asia,1 supporting the importance of environmental and lifestyle factors in the etiology of breast cancer. For example, Gomez and colleagues31 reported that age-adjusted incidence rates of invasive breast cancer increased for both US-born and foreign-born Asians from 1988 to 2004. The incidence rate was 120.6 cases per 100,000 person-years for US-born Asians and 76.3 cases for foreign-born Asians with the incidence rate ratio between US-born and foreign-born Asians at 1.58 (95% confidence interval of 1.53–1.63).31 A recent analysis based on the 18 SEER registries data showed that overall breast cancer incidence rates increased among Asian/Pacific Islander (1.7% per year), non-Hispanic black (0.4% per year), and Hispanic women (0.3% per year) but were stable in non-Hispanic white and American Indian/Alaska Native women between 2005 and 2014.9 From 2012 to 2016, the overall increase in breast cancer incidence in women was observed, which largely reflected a rise in local (early) stage disease.10 Our current study aimed to not only provide more detailed analyses on more recent breast cancer incidence trends from 2000 to 2018 by time periods, age groups and tumor stages, but also examine racial disparities in the risk of developing breast cancer by adjusting for age and stage in the regression models.
Methods
Data sources
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Public Use Data Set released in November 2020 were used for this study.36 The SEER program supports population-based tumor registries in nine areas (San Francisco/Oakland, San Jose-Monterey, Los Angeles, Greater California, Detroit, Seattle, Atlanta, Rural Georgia, and Greater Georgia) and 9 states (Alaska, Connecticut, Iowa, New Mexico, Utah, Hawaii, Louisiana, Kentucky, and New Jersey), accounting for 28% of the U.S. population. The estimated completeness of cancer case reporting in SEER areas was 97.7%.37 The SEER registries ascertain all newly diagnosed (incident) cancer cases from multiple reporting sources such as hospitals, outpatient clinics, laboratories, private medical practitioners, nursing/convalescent homes/hospices, autopsy reports and death certificates. Information includes tumor location and size; lymph node and distant organ metastases; histologic type and grade of tumor; demographic characteristics such as age, gender, race and marital status; and type of treatments provided in the first course of therapy within four months of initial therapy after diagnosis. This study was considered exempt for Institutional Review Board (IRB) review because it did not involve any patient contact and only had the analysis of de-identified SEER Public Use Data.
Study Population
Our study identified 1,129,564 women who were diagnosed with incident breast cancer at age 20 or older between 2000 and 2018 in 18 SEER registries. The denominator of population data included all women aged 20 or older in the same SEER areas that were provided in the SEER*Stat package.36 Of the 1,129,564 women with breast cancer, 802,790 were non-Hispanic whites (NHW), 119,175 were non-Hispanic blacks (NHB), 86,461 were non-Hispanic Asians/Pacific Islanders (API), 115,309 were Hispanic women, and 5,829 were American Indians and Alaska Natives (AIAN).
Study Variables
Race/ethnicity variable was classified into NHW, NHB, API, Hispanics, and AIAN. The patient socio-demographics included age at diagnosis (20–44, 45–54, 55 or older), year of diagnosis (2000 to 2018), and geographic areas (18 SEER registries). Tumor stage included local, regional, or distant stage. Hormone receptor positive breast cancer was defined if estrogen or progesterone receptor was positive.
Statistical Analysis
We utilized the SEER*Stat software (version 8.3.9) that was provided by the National Cancer Institute together with the SEER Data for analyses in cancer incidence rates and trends. Incidence of breast cancer in women was defined as a ratio of the number of women with a new breast cancer over the number of total female population at risk in the same SEER areas by year, which was presented in number of cases per 100,000 persons. Because age is a significant risk factor for cancer incidence, the incidence rates of breast cancer in all comparison groups by race/ethnicity or time periods that may consist of different age compositions should be standardized by age. Therefore, in this study the incidence rates were adjusted to the year 2000 standard US population by age. The age-adjusted incidence rates, 95% confidence intervals for incidence rates, incidence rate ratios ((IRR) and their 95% confidence intervals and annual percentage change (APC) of incidence rates were calculated from the SEER*Stat software. A p value <0.05 was considered statistically significant.
Results
Table 1 presents the number of total female population, number of incident breast cancer cases, and unadjusted and age-adjusted incidence rates in Asian women and other racial/ethnic women aged 20 or older in all 18 SEER areas in 2000–2018. The overall age-adjusted incidence rate of breast cancer was the highest in NHW women (190.4 cases per 100,000 women), followed by NHB (178.4), API (141.3), Hispanic (133.3) and AIAN women (128.8). The incidence rate ratio was statistically significantly higher in NHW (rate ratio: 1.35, 95% CI: 1.34–1.36) and NHB women (1.26, 1.25–1.27), but was significantly lower in Hispanic women (0.94, 0.94–0.95) and AIAN women (0.91, 0.89–0.94) as compared to API women.
Table 1.
Number of population, number of incident breast cancer cases, and breast cancer incidence in Asian women and other racial/ethnic women in all SEER areas, 2000–2018
| Race/Ethnicity | Number of population | Number of breast cancer cases | Unadjusted Incidence rates (N of cases per 100,000) (95% CI) | Age-adjusted* incidence rates (N of cases per 100,000) (95% CI) | Rate ratio (between age-adjusted incidence rates) (95% CI) |
|---|---|---|---|---|---|
| Non-Hispanic Asians and Pacific Islanders | 61,849,358 | 86,461 | 139.8 (138.9–140.7) | 141.3 (140.3–142.2) | 1.00 (reference) |
| Non-Hispanic white | 356,020,637 | 802,790 | 225.5 (225.0–226.0) | 190.4 (190.0–190.8) | 1.35 (1.34–1.36) |
| Non-Hispanic black | 69,761,330 | 119,175 | 170.8 (169.9–171.8) | 178.4 (177.4–179.4) | 1.26 (1.25–1.27) |
| American Indians and Alaska Natives | 4,779,347 | 5,829 | 122.0 (118.9–125.1) | 128.8 (125.4–132.3) | 0.91 (0.89–0.94) |
| Hispanics | 110,049,635 | 115,309 | 104.8 (104.2–105.4) | 133.3 (132.5–134.1) | 0.94 (0.94–0.95) |
| Total | 602,460,307 | 1,129,564 | 187.5 (187.1–187.8) | 176.9 (176.5– 177.2) |
Incidence rates were age adjusted to the 2000 US population.
Trend analyses showed that only NHW women had a decreasing trend in overall breast cancer incidence rates from 2000 to 2018, whereas all other ethnic women had a slightly increasing trend in breast cancer incidence rates (Figure 1). Table 2 presents the incidence rates and their changes by three time periods in calendar years for various ethnic women. Overall, annual percentage change (APC) from 2000 to 2018 showed that annual increase was statistically significant for API (APC: 1.0, 95% CI: 0.8–1.3), NHB (APC: 0.5, 0.2–0.7), AIAN (1.6, 1.1–2.2), and Hispanic women (0.4, 0.2–0.7) (see last column in Table 2). Overall annual percentage of incidence decreased but not significantly for NHW (−0.1, −0.4 to −0.1). Because the incidence appeared to increase after 2009, we also showed the most recent and available data on the trends from 2010 to 2018 by race/ethnicity in Supplement Figure S1 and Supplement Table S1, indicating significant increasing trend for API, NHW, and Hispanic women, but no significant change for NHB and AIAN. Table 3 presents the age-adjusted incidence rates by race/ethnicity that was stratified by hormone receptor status. The age-adjusted incidence rates of hormone receptor positive breast cancer increased over time from 2000 to 2018 in all race/ethnic women with no exception. The annual percentage change of incidence increase was greater in AIAN and NHB women, followed by API, Hispanic and NHW women. For hormone receptor negative breast cancer or hormone receptor unknown or at borderline, the incidence rates were decreasing over time in all ethnic women. The largest annual percentage decrease was observed in NHW women with hormone receptor unknown or at borderline breast cancer (−13.1%).
Figure 1.
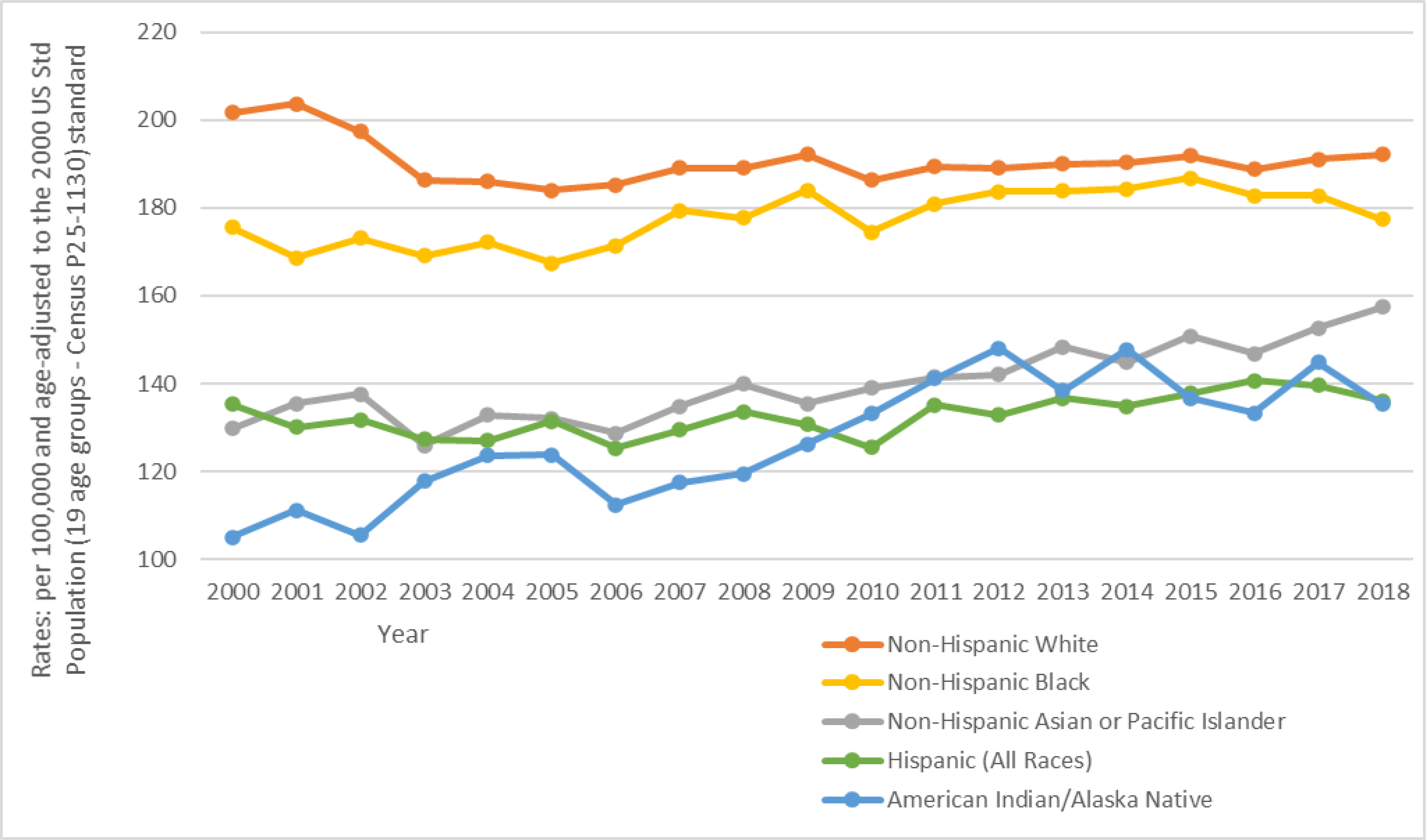
Trends in age-adjusted incidence rates (number of breast cancer cases per 100,000 population) in women by race/ethnicity in SEER areas from 2000 to 2018
Table 2.
Annual percentage change (APC) in age-adjusted incidence rates* (number of breast cancer cases per 100,000 population) in women by time period and race/ethnicity
| Race/Ethnicity | 2000–2005 | 2006–2011 | 2012–2018 | APC (95% CI) | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N. Population | N. Cases | Incidence rate (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | |||
| Non-Hispanic Asians and Pacific Islanders | 15,862,213 | 19,459 | 132.2 (130.3–134.1) | 19,186,258 | 25,720 | 136.8 (135.1–138.5) | 22,800,887 | 41,282 | 149.2 (147.7–150.7) | 1.0 (0.8, 1.3) | < 0.05 |
| Non-Hispanic white | 111,747,980 | 243,792 | 193.0 (192.3–193.8) | 112,106,666 | 249,339 | 188.6 (187.9–189.4) | 132,163,991 | 309,659 | 190.5 (189.8–191.2) | −0.1 (−0.4, −0.1) | 0.2 |
| Non-Hispanic black | 20,115,429 | 30,973 | 171.0 (169.0–172.9) | 21,705,448 | 36,874 | 178.1 (176.3–180.0) | 27,940,453 | 51,328 | 183.1 (181.5–184.8) | 0.5 (0.2, 0.7) | < 0.05 |
| American Indians and Alaska Natives | 1,403,381 | 1,407 | 114.7 (108.5–121.1) | 1,492,543 | 1,773 | 125.5 (119.3–131.7) | 1,883,423 | 2,649 | 139.9 (134.5–145.5) | 1.6 (1.1, 2.2) | < 0.05 |
| Hispanics | 28,316,058 | 26,214 | 130.3 (128.6–131.9) | 34,412,281 | 34,460 | 130.1 (128.7–131.5) | 47,321,296 | 54,635 | 137.0 (135.9–138.2) | 0.4 (0.2, 0.7) | < 0.05 |
| Total | 177,445,061 | 321,845 | 179.1 (178.5–179.7) | 188,905,196 | 348,166 | 174.9 (174.3–175.5) | 236,110,050 | 459,553 | 177.1 (176.6–177.6) | −0.1 (−0.3, −0.1) | 0.3 |
Incidence rates were age adjusted to the 2000 US population.
Table 3.
Annual percentage change (APC) in age-adjusted incidence rates (number of breast cancer cases per 100,000 population) in women in 2000–2018 by hormone receptor status and race/ethnicity
| Race/Ethnicity | Hormone-receptor positive | Hormone-receptor negative | Hormone-receptor status unknown or borderline | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2000 to 2018 | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2000 to 2018 | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2000 to 2018 | |
| Non-Hispanic Asians and Pacific Islanders | 66,990 | 109.5 (108.7, 110.4) | 2.5 (2.2, 2.7) | 13,786 | 22.3 (21.9, 22.7) | −0.6 (−1.1, 0.0) | 5,685 | 9.4 (9.2, 9.7) | −10.5 (−11.8, −9.1) |
| Non-Hispanic white | 620,197 | 146.6 (146.2, 147.0) | 1.4 (1.2, 1.7) | 113,751 | 28.0 (27.9, 28.2) | −1.3 (−1.9, −0.7) | 68,842 | 15.8 (15.6, 15.9) | −12.7 (−13.8, −11.6) |
| Non-Hispanic black | 75,918 | 114.1 (113.3, 115.0) | 2.8 (2.3, 3.3) | 31,706 | 46.5 (46.0, 47.1) | −0.3 (−1.0, 0.4) | 11,551 | 17.7 (17.4, 18.1) | −11.9 (−13.0, −10.8) |
| American Indians and Alaska Natives | 4,474 | 96.5 (93.5, 99.5) | 3.0 (2.2, 3.8) | 1,004 | 21.9 (20.5, 23.3) | −0.3 (−1.7, 1.1) | 451 | 10.5 (9.5, 11.5) | −6.3 (−8.6, −4.0) |
| Hispanics | 83,682 | 97.7 (97.0, 98.4) | 2.2 (1.9, 2.6) | 21,316 | 23.3 (22.9, 23.6) | −0.8 (−1.6, −0.1) | 10,311 | 12.3 (12.1, 12.6) | −10.1 (−11.5, −8.6) |
| Total | 851,161 | 133.1 (132.8,133.4) | 1.5 (1.2, 1.7) | 181,563 | 28.8 (28.7, 28.9) | −1.1 (−1.6, −0.5) | 96,840 | 15.0 (14.9, 15.1) | −12.1 (−13.3, −10.9) |
Incidence rates were age adjusted to the 2000 US population. Hormone-receptor positive was defined as estrogen-receptor was positive OR progesterone receptor was positive.
Table 4 presents the age-adjusted incidence rates by race/ethnicity that was stratified by 3 age groups and 3 time periods. In all age groups regardless of young (20–44 years), middle age (45–54), or older age (>=55 years), and in all time periods (2000–2005, 2006–2011, and 2012–2018), NHW and NHB women had a significantly higher risk of having breast cancer than API women. The magnitude of the incidence rate ratio was greater in women aged 55 or older for NHW (1.69, 1.66–1.72) and NHB (1.40, 1.37–1.44) women as compared to APIs, while the incidence rate ratio was smaller in younger women less than 45 years for NHW (1.09, 1.06–1.12) and NHB (1.17, 1.12–1.22) women in the time period of 2000–2005. The risk of having breast cancer in AIAN and Hispanic women was generally significantly lower than that of API women aged 20–44 and 45–54 years. Interestingly, in women aged 55 or older AIAN women had no significantly different risk of breast cancer while Hispanic women had a significantly higher risk of breast cancer than API women in the earlier time periods of 2000–2005 and 2006–2011. However, in 2012–2018, both AIAN and Hispanic women aged 55 or older had no significantly different risks of breast cancer as compared to API women. In middle-age women of 45–54 years, AIAN and Hispanic women still had a significantly lower risk of breast cancer than API women, but in younger women less than 45 years, only Hispanic women but not AIAN women had a significantly lower risk of breast cancer than API women.
Table 4.
Age-adjusted incidence rates (number of breast cancer cases per 100,000 women) by age groups, race/ethnicity, and time period
| Race/Ethnicity | Age 20–44 yrs | Age 45–54 yrs | Age ≥55 yrs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N. Population | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | |
| 2000–2005 | ||||||||||||
| Non-Hispanic Asians and Pacific Islanders | 8,720,162 | 3,663 | 45.3 (43.8, 46.8) | 1.00 (ref) | 3,050,172 | 5,628 | 184.5 (179.7, 189.4) | 1.00 (ref) | 4,091,879 | 10,168 | 247.5 (242.7, 252.4) | 1.00 (ref) |
| Non-Hispanic white | 49,156,031 | 25,126 | 49.2 (48.6, 49.8) | 1.09 (1.05, 1.13) | 22,354,647 | 50,484 | 225.0 (223.1, 227.0) | 1.22 (1.19, 1.25) | 40,237,302 | 168,182 | 418.3 (416.3, 420.3) | 1.69 (1.66, 1.72) |
| Non-Hispanic black | 11,228,415 | 5,656 | 52.9 (51.6, 54.3) | 1.17 (1.12, 1.22) | 3,864,214 | 8,104 | 210.1 (205.5, 214.7) | 1.14 (1.10, 1.18) | 5,022,800 | 17,213 | 347.7 (342.5, 353.0) | 1.40 (1.37, 1.44) |
| American Indians and Alaska Natives | 789,144 | 258 | 34.2 (30.2, 38.7) | 0.76 (0.67, 0.86) | 289,763 | 425 | 146.9 (133.2, 161.5) | 0.80 (0.72, 0.88) | 324,474 | 724 | 231.6 (214.5, 249.8) | 0.94 (0.86, 1.01) |
| Hispanics | 18,853,130 | 5,778 | 36.7 (35.7, 37.6) | 0.81 (0.78, 0.84) | 4,459,288 | 7,188 | 162.2 (158.5, 166.0) | 0.88 (0.85, 0.91) | 5,003,640 | 13,248 | 269.9(265.3, 274.7) | 1.09 (1.06, 1.12) |
| Total (2000–2005) | 88,746,882 | 40,481 | 46.9 (46.5, 47.4) | 34,018,084 | 71,829 | 210.9 (209.4, 212.5) | 54,680,095 | 209,535 | 384.6 (383.0, 386.3) | |||
| 2006–2011 | ||||||||||||
| Non-Hispanic Asians | 9,865,153 | 4,339 | 46.9 (45.5, 48.3) | 1.00 (ref) | 3,677,948 | 6,979 | 189.3 (184.9, 193.8) | 1.00 (ref) | 5,643,157 | 14,402 | 257.1 (252.8, 261.4) | 1.00 (ref) |
| Non-Hispanic white | 44.816,003 | 22,417 | 51.3 (50.7, 52.0) | 1.10 (1.06, 1,13) | 22,828,283 | 50,544 | 220.2 (218.3, 222.1) | 1.16 (1.13, 1.19) | 44,464,380 | 176,378 | 403.0 (401.1, 405.0) | 1.57 (1.54, 1.60) |
| Non-Hispanic black | 11,158,040 | 5,731 | 55.7 (54.2, 57.1) | 1.19 (1.14, 1.24) | 4,421,680 | 9,192 | 207.4 (203.1, 211.7) | 1.10 (1.06, 1.13) | 6,125,728 | 21,951 | 368.8 (363.8, 373.8) | 1.43 (1.40, 1.47) |
| American Indians and Alaska Natives | 763,242 | 254 | 37.5 (33.0, 42.4) | 0.80 (0.70, 0.91) | 320,396 | 462 | 143.9 (131.1, 157.7) | 0.76 (0.69, 0.84) | 408,905 | 1,057 | 264.2 (247.8, 281.4) | 1.03 (0.96, 1.10) |
| Hispanics | 21,536,450 | 6,801 | 36.8 (35.9, 37.7) | 0.78 (0.76, 0.82) | 5,993,616 | 9,515 | 159.2 (156.0, 162.5) | 0.84 (0.82, 0.87) | 6,882,215 | 18,144 | 271.0 (267.0, 275.1) | 1.05 (1.03, 1.08) |
| Total (2006–2011) | 88,138,888 | 39,542 | 48.0 (47.5, 48.5) | 37,241,923 | 76,692 | 205.1 (203.7, 206.6) | 63,524,385 | 231,932 | 372.4 (370.9, 374.0) | |||
| 2012–2018 | ||||||||||||
| Non-Hispanic Asians | 13,058,803 | 6,160 | 49.5 (48.3, 50.8) | 1.00 (ref) | 4,828,472 | 10,180 | 210.5 (206.4, 214.6) | 1.00 (ref) | 8,913,612 | 24,942 | 280.7 (277.2, 284.3) | 1.00 (ref) |
| Non-Hispanic white | 50,295,413 | 24,146 | 52.9 (52.2, 53.5) | 1.07 (1.04, 1.10) | 23,638,499 | 53,601 | 224.4 (222.5, 226.3) | 1.07 (1.04, 1.09) | 58,230,079 | 231,912 | 404.1 (402.4, 405.7) | 1.44 (1.42, 1.46) |
| Non-Hispanic black | 13,690,032 | 6,549 | 55.2 (53.9, 56.6) | 1.12 (1.08, 1.16) | 5,214,970 | 11,247 | 213.8 (209.8, 217.8) | 1.02 (0.99, 1.04) | 9,035,451 | 33,532 | 382.2 (378.0, 386.4) | 1.36 (1.34, 1.38) |
| American Indians and Alaska Natives | 916,560 | 334 | 44.1 (39.5, 49.2) | 0.89 (0.80, 1.00) | 347,538 | 566 | 161.2 (148.1, 175.1) | 0.77 (0.70, 0.83) | 619,325 | 1,749 | 290.0 (276.0, 304.5) | 1.03 (0.98, 1.09) |
| Hispanics | 27,662,537 | 9,644 | 40.5 (39.7, 41.4) | 0.82 (0.79, 0.86) | 8,461,741 | 14,126 | 166.9 (164.2, 169.7) | 0.79 (0.77, 0.81) | 11,197,018 | 30,865 | 282.9 (279.6, 286.2) | 1.01 (0.99, 1.03) |
| Total (2012–2018) | 105,623,345 | 46,833 | 49.6 (49.1, 50.0) | 42,491,220 | 89,720 | 209.5 (208.1, 210.9) | 87,995,485 | 323,000 | 374.3 (373.0, 375.6) | |||
| Total (2000–2018) | 282,509,115 | 126,856 | 48.2 (48.0, 48.5) | 113,751,227 | 238,241 | 208.4 (207.6, 209.3) | 206,199,965 | 764,467 | 376.5 (375.7, 377.4) | |||
Incidence rates were age adjusted to the 2000 US population in each of the 3 age groups.
Table 5 presents the age-adjusted incidence rates by race/ethnicity that was stratified by tumor stages and time periods. In all tumor stages across 3 different time periods, NHW and NHB women had a significantly higher risk of having breast cancer than API women. For example, NHW and NHB women had a significantly higher risk of having local stage breast cancer (1.47, 1.44–1.49, and 1.07, 1.05–1.10) and distant stage breast cancer (1.68, 1.58–1.78 and 2.51, 2.35–2.69) as compared to API women in 2000–2005. In 2012–2018, the risks of having local stage and distant stage breast cancer for NHW (1.31, 1.29–1.33 and 1.19, 1.16–1.21) and NHB (1.09, 1.07–1.11 and 1.31, 1.28–1.35) women were still significantly higher than that of API women. However, there were some different interesting observations in AIAN and Hispanic women, in which both AIAN and Hispanic women had a significantly lower risk of having local stage breast cancer but had a significantly higher risk of having distant stage breast cancer than API women across the 2000–2005 and 2006–2011 periods. For example, the risk of having local stage breast cancer was 0.83 (0.77–0.89) for AIAN and 0.89 (0.87–0.91) for Hispanic women, but the risk of having distant stage breast cancer was 1.40 (1.15–1.70) for AIAN and 1.33 (1.24–1.44) for Hispanic women as compared to API women in 2000–2005. In 2012–2018, AIAN women had a significantly lower risk of having local stage breast cancer (0.90, 0.85–0.95) but had no significant risk of regional or distant stage breast cancer, whereas Hispanic women had a significantly lower risk of having local stage (0.85, 0.83–0.86) and distant stage (0.94, 0.91–0.96) breast cancer but had a significant higher risk of regional stage (1.06, 1.04–1.09) breast cancer as compared to API women.
Table 5.
Age-adjusted incidence rates (number of breast cancer cases per 100,000 population) in women by tumor stage, Asian sub-groups and time period
| Race/Ethnicity | Local stage Breast Cancer | Regional Stage Breast Cancer | Distant Stage or Unknown Breast Cancer | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N. Population | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | N. Cases | Incidence rate (95% CI) | Rate ratio (95% CI) | |
| 2000–2005 | ||||||||||
| Non-Hispanic Asians and Pacific Islanders | 15,862,213 | 11,960 | 81.8 (80.4, 83.3) | 1.00 (reference) | 6,362 | 42.4 (41.4, 43.5) | 1.00 (reference) | 1,137 | 7.9 (7.4, 8.4) | 1.00 (reference) |
| Non-Hispanic white | 111,747,980 | 152,325 | 120.0 (119.4, 120.6) | 1.47 (1.44, 1.49) | 73,938 | 59.8 (59.4, 60.2) | 1.41 (1.37, 1.45) | 17,529 | 13.3 (13.1, 13.5) | 1.68 (1.58, 1.78) |
| Non-Hispanic black | 20,115,429 | 15,764 | 87.9 (86.5, 89.3) | 1.07 (1.05, 1.10) | 11,689 | 63.2 (62.1, 64.4) | 1.49 (1.45, 1.54) | 3,520 | 19.9 (19.2, 20.5) | 2.51 (2.35,2.69) |
| American Indians and Alaska Natives | 1,403,381 | 817 | 67.9 (63.1, 73.0) | 0.83 (0.77, 0.89) | 461 | 35.6 (32.3, 39.2) | 0.84 (0.76, 0.93) | 129 | 11.1 (9.2, 13.3) | 1.40 (1.15, 1.70) |
| Hispanics | 28,316,058 | 14,230 | 72.8 (71.6, 74.1) | 0.89 (0.87, 0.91) | 9,983 | 46.9 (45.9, 47.9) | 1.10 (1.07, 1.14) | 2,001 | 10.6 (10.1, 11.0) | 1.33 (1.24, 1.44) |
| Total (2000–2005) | 177,445,061 | 195,096 | 108.6 (108.1, 109.1) | 102,433 | 57.3 (56.9, 57.6) | 24,316 | 13.3 (13.1, 13.5) | |||
| 2006–2011 | ||||||||||
| Non-Hispanic Asians | 19,186,258 | 16,368 | 87.3 (86.0, 88.7) | 1.00 (reference) | 7,616 | 40.2 (39.3, 41.1) | 1.00 (reference) | 1,736 | 9.2 (8.8, 9.7) | 1.00 (reference) |
| Non-Hispanic white | 112,108,666 | 160,071 | 120.2 (119.6, 120.8) | 1.38 (1.35, 1.40) | 70,887 | 55.1 (54.7, 55.5) | 1.37 (1.34, 1.40) | 18,381 | 13.3 (13.1, 13.5) | 1.44 (1.37, 1.51) |
| Non-Hispanic black | 21,705,448 | 19,653 | 95.6 (94.2, 97.0) | 1.09 (1.07, 1.12) | 13,138 | 62.6 (61.5, 63.7) | 1.56 (1.51, 1.60) | 4,083 | 20.0 (19.3, 20.6) | 2.16 (2.04, 2.29) |
| American Indians and Alaska Natives | 1,492,543 | 1,009 | 71.9 (67.4, 76.7) | 0.82 (0.77, 0.88) | 615 | 42.8 (39.4, 46.5) | 1.07 (0.98, 1.16) | 149 | 10.7 (9.0, 12.7) | 1.16 (0.97, 1.38) |
| Hispanics | 34,412,281 | 19,395 | 75.1 (74.0, 76.2) | 0.86 (0.84, 0.88) | 12,253 | 44.2 (43.4 45.0) | 1.10 (1.07, 1.13) | 2,812 | 10.8 (10.4, 11.2) | 1.17 (1.10, 1.25) |
| Total (2006–2011) | 188,905,196 | 216,496 | 108.6 (108.1, 109.0) | 104,509 | 52.9 (52.6, 53.3) | 27,161 | 13.4 (13.2, 13.6) | |||
| 2012–2018 | ||||||||||
| Non-Hispanic Asians | 22,800,887 | 22,476 | 80.9 (79.8, 82.0) | 1.00 (reference) | 9,598 | 34.9 (34.2, 35.6) | 1.00 (reference) | 9,208 | 33.4 (32.7, 34.1) | 1.00 (reference) |
| Non-Hispanic white | 132,163,991 | 176,308 | 106.9 (106.4, 107.4) | 1.31 (1.29, 1.33) | 67,988 | 44.0 (43.7, 44.4) | 1.26 (1.23, 1.29) | 65,363 | 39.6 (39.3, 39.9) | 1.19 (116, 1.21) |
| Non-Hispanic black | 27,940,453 | 24,811 | 88.3 (87.2, 89.5) | 1.09 (1.07, 1.11) | 14,287 | 51.0 (50.1, 51.8) | 1.46 (1.42, 1.50) | 12,230 | 43.8 (43.0, 44.6) | 1.31 (1.28, 1.35) |
| American Indians and Alaska Natives | 1,883,423 | 1,409 | 73.7 (69.8, 77.8) | 0.90 (0.85, 0.95) | 645 | 34.4 (31.8, 37.3) | 0.99 (0.91, 1.07) | 595 | 31.8 (29.2, 34.5) | 0.95 (0.87, 1.04) |
| Hispanics | 47,321,296 | 26,003 | 68.7 (67.8, 69.5) | 0.85 (0.83, 0.86) | 15,325 | 37.1 (36.5, 37.7) | 1.06 (1.04, 1.09) | 12,307 | 31.2 (30.7, 31.8) | 0.94 (0.91, 0.96) |
| Total (2012–2018) | 236,110,050 | 252,007 | 96.2 (95.8, 96.6) | 107,843 | 42.7 (42.4, 42.9) | 99,703 | 38.2 (38.0, 38.5) | |||
| Total (2000–2018) | 602,460,307 | 663,599 | 103.5 (103.2, 103.8) | 314,785 | 50.0 (49.8, 50.2) | 151,180 | 23.4 (23.3, 23.5) | |||
Incidence rates were age adjusted to the 2000 US population.
Discussion
This study examined the most recent breast cancer incidence trends among women in SEER areas from 2000 to 2018 by time periods, age groups and tumor stages, and explored racial disparities in the risk of developing breast cancer by adjusting for multiple confounding factors. Our study found that only NHW women had a decreasing trend in breast cancer incidence rates overall from 2000 to 2018, whereas all other ethnic women had a slightly increasing trend in breast cancer incidence. The decreasing trend in breast cancer incidence rates for NHW women was largely driven by the decreasing number of hormone receptor unknown or at borderline breast cancer. In those with hormone receptor positive breast cancer, there was actually a small increase from 2000 to 2018 in NHW women. The incidence rate ratio was statistically significantly higher in NHW and NHB women as compared to API women, but was significantly lower in Hispanic women an AIAN women. However, although AIAN and Hispanic women had a significantly lower risk of having early stage (local stage) breast cancer, they had a significantly higher risk of having distant stage breast cancer than API women in 2000–2018.
Our study on the most recent cohort of breast cancer cases in SEER areas of the United States supported the findings of previous incidence trend studies.8–10,29–35 For example, DeSantis and colleagues9 found that overall breast cancer incidence rates from 2005 to 2014 increased among API (1.7% per year), NHB (0.4% per year), and Hispanic women (0.3% per year) but were stable among NHW and AIAN women in SEER areas. Gomez and colleagues31 showed that breast cancer incidence rates increased over time from 1988 to 2004 among Asian women in California and the incidence increase was greater in the US-born Asian populations than in those foreign-born Asian women. Tuan and colleagues35 reported an increasing trend of breast cancer incidence among Asian women and in most subgroups of Asians such as Filipina, South Asian, Chinese, Korean, and Vietnamese women from 1990 to 2014 in SEER areas, but incidence rates did not change significantly during this time period for NHW and Japanese women. Several other studies also demonstrated an increasing trend in incidence rates for overall breast cancer and for some subtypes of breast cancer in Asian women in the United States.29–35
The decreasing trend in NHW women was primarily attributed to the decreased use of menopausal hormones following the publication and recommendation of two large clinical trial results in 2002, which concluded that hormone replacement therapy was associated with a higher risk of heart disease and breast cancer.3,8–11 It may also be due to small declines in mammography screening since 2000.3,8–11 The increasing trend in other ethnic women, particularly among API women, may be attributed to adaption of western-style diets and lifestyle, more work and life-related stress, lack of physical exercise, increases in body mass index, and declines in the average number of births per woman.4,13–28,37 The improved technology and accuracy in cancer diagnosis and imaging may also have made the previously undetected metastatic tumors or unknown tumor stages to be defined now, hence leading to an increased incidence.
Our study and many previous studies8–11,38 consistently demonstrated that the risk of developing breast cancer was higher in NHW and NHB women, and lower in API, AIAN and Hispanic women. A particular interesting finding was that AIAN and Hispanic women had a lower risk of having early stage breast cancer but had a higher risk of having distant (late) stage breast cancer than in API women. The reasons for these racial/ethnic disparities in the risk of developing breast cancer are multifactorial and might include the lack of physical exercise, higher body mass index, increased work and life related stress, higher alcohol consumption and smoking, delayed marriage and childbirth, lower breast feeding, lower parity, and higher utilization of hormone birth control pills and postmenopausal hormone medications.11,13–28 Although breast cancer incidence rates are increasing in women in all racial/ethnic women except for NHW women, good news is that the mortality rates for breast cancer are decreasing over the past decades due to improvements in early detection and in treatment.11 However, many challenges are still ahead of us in order to address and narrow substantial disparities in cancer incidence and in mortality.
This study has several limitations to be kept in mind for interpretation. First, because there was no information on the place of birth and time of migration for breast cancer cases and for population denominator, the study cannot address the cancer incidence disparities by U.S.-born or foreign-born women or by the timing of migration for those women who immigrated from other countries. Second, although there were some differences among the subgroups of API women such as Chinese, Korean and Japanese Americans, or among the subgroups of Hispanic women such as Mexican or Cuban Americans, the cancer incidence rates by these subgroups cannot be addressed due to lack of information from the population denominators in SEER*Stats data system. Third, many potential risk factors for breast cancer such as parity, smoking, physical exercise, and hormone use differed substantially by race and ethnicity, but breast cancer incidence rates by race/ethnicity duo to these differences cannot be controlled for in the analyses. Fourth, the study found that AIAN and Hispanic women had a significantly higher risk of having distant stage breast cancer than API women in 2000–2018. This may be related to a lower breast cancer mammogram screening rate, as studies showed that in 2018 only 66% of AIAN women had mammogram screening in last two years as compared to 71% of API women aged 50–74 years.40 However, this association cannot be determined in this study due to lack of screening data. Finally, although there was information on health insurance status for cancer cases, this factor cannot be taken into consideration in the analyses because of lack of such information in population denominators.
In conclusion, we observed a slightly increasing trend in overall breast cancer incidence for all ethnic women except for NHW women who had a decreasing trend from 2000 to 2018, but we also observed a small increase in the incidence of hormone receptor positive breast cancer among NHW women and a decreasing trend of hormone receptor negative or unknown breast cancer for all ethnic women. There were still substantial racial disparities in breast cancer incidence with the higher risk of breast cancer in NHW and NHB women and the lower risk in AIAN, Hispanic and API women. AIAN and Hispanic women had a significantly lower risk of having early stage breast cancer but had a significantly higher risk of having distant stage breast cancer than API women. There are still many challenges ahead for us to mitigate risk factors for decreasing breast cancer incidence and to reduce racial disparities for cancer burden.
Supplementary Material
Highlights.
Hormone-receptor positive breast cancer incidence rates increased in all ethnic women
Decreasing trend of hormone receptor negative or unknown breast cancer in 2000–2018
Breast cancer incidence was higher in white and black women than Hispanics and Asians
Hispanics had a lower risk of early stage but higher risk of distant stage breast cancer
Acknowledgments
Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award Number R01AG058971 and R01AG067498. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures and Declarations, Compliance with Ethical Standards
This study was supported by the NIH grant Number R01AG058971 and R01AG067498. There are no conflicts of interest from all authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bray F, McCarron P, Parkin DM. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004;6(6):229–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International Variation in Female Breast Cancer Incidence and Mortality Rates. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1495–506. [DOI] [PubMed] [Google Scholar]
- 3.Ravdin PM, Cronin KA, Howlader N, Berg CD, Chlebowski RT, Feuer EJ, et al. The decrease in breast cancer incidence in 2003 in the United States. N Engl J Med. 2007;356:1670–4. [DOI] [PubMed] [Google Scholar]
- 4.Porter P "Westernizing" women's risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358:213–6. [DOI] [PubMed] [Google Scholar]
- 5.Shin HR, Joubert C, Boniol M, Hery C, Ahn SH, Won YJ, et al. Recent trends and patterns in breast cancer incidence among Eastern and Southeastern Asian women. Cancer Causes Control. 2010. Nov;21(11):1777–85. [DOI] [PubMed] [Google Scholar]
- 6.Zbuk K, Anand SS. Declining incidence of breast cancer after decreased use of hormone-replacement therapy: magnitude and time lags in different countries. J Epidemiol Community Health. 2012;66:1–7. [DOI] [PubMed] [Google Scholar]
- 7.Youlden DR, Cramb SM, Yip CH, Baade PD. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Biol Med. 2014. Jun;11(2):101–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66(1):31–42. [DOI] [PubMed] [Google Scholar]
- 9.DeSantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017. Nov;67(6):439–448. [DOI] [PubMed] [Google Scholar]
- 10.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438–451. [DOI] [PubMed] [Google Scholar]
- 11.American Cancer Society. Breast Cancer Facts & Figures 2019–2020. Atlanta: American Cancer Society, Inc. 2019. [Google Scholar]
- 12.Linos E, Spanos D, Rosner BA, Linos K, Hesketh T, Qu JD, et al. Effects of reproductive and demographic changes on breast cancer incidence in China: a modeling analysis. J Natl Cancer Inst. 2008;100(19):1352–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neilson HK, Friedenreich CM, Brockton NT, Millikan RC. Physical activity and postmenopausal breast cancer: proposed biologic mechanisms and areas for future research. Cancer Epidemiol Biomarkers Prev. 2009;18(1):11–27. [DOI] [PubMed] [Google Scholar]
- 14.Nelson HD, Zakher B, Cantor A, et al. Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and metaanalysis. Ann Intern Med. 2012;156(9):635–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macacu A, Autier P, Boniol M, Boyle P. Active and passive smoking and risk of breast cancer: a meta-analysis. Breast Cancer Res Treat. 2015;154(2):213–224. [DOI] [PubMed] [Google Scholar]
- 16.Haas JS, Hill DA, Wellman RD, et al. Disparities in the use of screening magnetic resonance imaging of the breast in community practice by race, ethnicity, and socioeconomic status. Cancer. 2016;122(4):611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pizot C, Boniol M, Mullie P, et al. Physical activity, hormone replacement therapy and breast cancer risk: A meta-analysis of prospective studies. Eur J Cancer. 2016;52:138–154. [DOI] [PubMed] [Google Scholar]
- 18.Cao Y, Hou L, Wang W. Dietary total fat and fatty acids intake, serum fatty acids and risk of breast cancer: A meta-analysis of prospective cohort studies. Int J Cancer. 2016;138(8):1894–1904. [DOI] [PubMed] [Google Scholar]
- 19.Moore SC, Lee IM, Weiderpass E, et al. Association of Leisure Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern Med. 2016;176(6):816–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White AJ, D’Aloisio AA, Nichols HB, DeRoo LA, Sandler DP. Breast cancer and exposure to tobacco smoke during potential windows of susceptibility. Cancer Causes Control. 2017;28(7):667–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh GK, Jemal A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950–2014: Over Six Decades of Changing Patterns and Widening Inequalities. J Environ Public Health. 2017;2017:2819372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morch LS, Skovlund CW, Hannaford PC, Iversen L, Fielding S, Lidegaard O. Contemporary Hormonal Contraception and the Risk of Breast Cancer. N Engl J Med. 2017;377(23):2228–2239. [DOI] [PubMed] [Google Scholar]
- 23.Picon-Ruiz M, Morata-Tarifa C, Valle-Goffin JJ, Friedman ER, Slingerland JM. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J Clin. 2017;67(5):378–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kerr J, Anderson C, Lippman SM. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017;18(8):e457–e471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iyengar NM, Arthur R, Manson JE, Chlebowski RT, Kroenke CH, Peterson L, et al. Association of Body Fat and Risk of Breast Cancer in Postmenopausal Women With Normal Body Mass Index: A Secondary Analysis of a Randomized Clinical Trial and Observational Study. JAMA Oncol. 2019. Feb 1;5(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: An updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2018;160:152–182. [DOI] [PubMed] [Google Scholar]
- 27.Pfeiffer RM, Webb-Vargas Y, Wheeler W, Gail MH. Proportion of U.S. trends in breast cancer incidence attributable to longterm changes in risk factor distributions. Cancer Epidemiol Biomarkers Prev. 2018;27:1214–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McTiernan A, Friedenreich CM, Katzmarzyk PT, et al. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med Sci Sports Exerc. 2019;51(6):1252–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hausauer AK, Keegan TH, Chang ET, Clarke CA. Recent breast cancer trends among Asian/Pacific Islander, Hispanic, and African-American women in the US: changes by tumor subtype. Breast Cancer Res. 2007;9(6):R90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keegan TH, Gomez SL, Clarke CA, Chan JK, Glaser SL. Recent trends in breast cancer incidence among 6 Asian groups in the Greater Bay Area of Northern California. Int J Cancer. 2007;120(6):1324–9. [DOI] [PubMed] [Google Scholar]
- 31.Gomez SL, Quach T, Horn-Ross PL, Pham JT, Cockburn M, Chang ET, et al. Hidden breast cancer disparities in Asian women: disaggregating incidence rates by ethnicity and migrant status. Am J Public Health. 2010;100 Suppl 1:S125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hou N, Huo D. A trend analysis of breast cancer incidence rates in the United States from 2000 to 2009 shows a recent increase. Breast Cancer Res Treat. 2013;138(2):633–41. [DOI] [PubMed] [Google Scholar]
- 33.Gomez SL, Von Behren J, McKinley M, Clarke CA, Shariff-Marco S, Cheng I, et al. Breast cancer in Asian Americans in California, 1988–2013: increasing incidence trends and recent data on breast cancer subtypes. Breast Cancer Res Treat. 2017;164(1):139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kong X, Liu Z, Cheng R, Sun L, Huang S, Fang Y, Wang J. Variation in Breast Cancer Subtype Incidence and Distribution by Race/Ethnicity in the United States From 2010 to 2015. JAMA Netw Open. 2020;3(10):e2020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tuan AW, Davis Lynn BC, Chernyavskiy P, Yu M, Gomez SL, Gierach GL, et al. Breast Cancer Incidence Trends by Estrogen Receptor Status Among Asian American Ethnic Groups, 1990–2014. JNCI Cancer Spectr. 2020;4(2):pkaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Data, 18 Registries, Nov 2020 Sub (2000–2018) - National Cancer Institute, DCCPS, Surveillance Research Program, released April 2021, based on the November 2020 submission.
- 37.Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76(11):2343–50. [DOI] [PubMed] [Google Scholar]
- 38.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: Final Data for 2017. Natl Vital Stat Rep. 2018;67(8):1–50. [PubMed] [Google Scholar]
- 39.Davis Lynn BC, Rosenberg PS, Anderson WF, Gierach GL. Black-White Breast Cancer Incidence Trends: Effects of Ethnicity. J Natl Cancer Inst. 2018;110(11):1270–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Cancer Society. Cancer Prevention & Early Detection Facts & Figures, 2021–2022. Atlanta, GA: American Cancer Society, 2021, page 48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


