Abstract
Exposure to stigma, violence, sex work, and substance use are associated with increased HIV risk, but relationships between these factors have not been fully elucidated among transgender women whose data are often aggregated with men who have sex with men and other sexual and gender minorities. Considering this gap, we aimed to identify a serologically confirmed HIV estimate for transgender women and examine the relationships between stigma, sex work, substance use, and HIV among a national sample of transgender women in Dominican Republic. We analyzed biomarkers and self-report data from the third wave of Dominican Republic's Encuesta de Vigilancia y Comportamiento con Vinculación Serológica, employing logistic and negative binomial regression to estimate models (n = 307). HIV rate was 35.8%. Nearly 75% of respondents engaged in sex work. Over 20% reported experiencing violence; 61.6% reported being stigmatized. Participation in sex work was associated with higher levels of stigma [incidence rate ratio (IRR): 1.70, p < 0.05]. Respondents who experienced violence had over three times higher odds of living with HIV relative to respondents who had not been victimized [odds ratio (OR): 3.15, p < 0.05]. Marijuana users were less likely to experience stigma compared with cocaine users (IRR: 1.72, p < 0.05), and a higher risk of alcohol dependency was associated with higher odds of experiencing violence (OR: 1.17, p < 0.001). Findings illustrate the importance of disaggregating data collected from transgender women compared with other sexual and gender minorities to ascertain subpopulation-specific estimates and indicate an urgent need to implement structural interventions and policies to protect transgender women's health and their human rights.
Keywords: transgender, sexual and gender minorities, Dominican Republic, stigma, violence, HIV, Serological Study, vulnerability, Global Health
Introduction
There are few studies on the health and well-being of transgender women in resource-constrained global settings, environments where funds are limited, and stigma against sexual and gender minorities is high.1 Although transgender women are a key population in addressing the global HIV epidemic, there are few serologically confirmed HIV estimates for this population, even though such estimates are necessary for the development and implementation of tailored prevention and treatment efforts.2,3 In response to this scientific knowledge gap, we conducted a serological and behavioral study of transgender women in Dominican Republic, a middle-income nation in the Latin American and Caribbean (LAC) region, a region that holds high rates of HIV, second only to sub-Saharan Africa.4 Our results offer one of the few socioserological national narratives of the transgender experience. Considering the difficulty of obtaining of these data, as well as the potential for our findings to yield high public health impact, we propose two objectives. The first is to characterize the lived experiences and health risks of transgender women in Dominican Republic; this includes reporting on the serologically verified prevalence of HIV in our sample. Our second objective is to test the hypothesis that there is an association between negative exposures and HIV among transgender women in Dominican Republic. Transgender women are at higher risk for contracting HIV, and due to stigma perpetuated by society, transgender women are more likely to struggle to find stable employment, which can facilitate entry into sex work (exacerbating HIV risk) and engagement in high-risk coping mechanisms, such substance use.1,5,6
Sexual and gender minorities in Dominican Republic
Dominican Republic is home to an estimated 124,772 sexual and gender minorities whose sex assigned at birth is male.6,7 Of these 124,772, about 0.3% (∼8000 individuals) identify as transgender women.7,8 Even though sexual and gender minorities only comprise about 1% of the national population, they represent a third of all new HIV infections, with historic estimates of HIV prevalence among sexual and gender minorities being 6.1% (confidence interval: 5.1–7.6).8 In Dominican Republic, rates of HIV incidence and prevalence among transgender women are not fully elucidated due to the nondisaggregation of data from transgender women as compared with men who have sex with men (MSM); transgender women continue to be labeled as MSM in clinical records and in behavioral surveys across the LAC region, leading to the potential for HIV prevalence and incidence rate inflation among MSM, and deflation among transgender women. To our knowledge, only one study in the Dominican Republic was previously able to extrapolate HIV prevalence (collected through self-report) from an exclusively transgender women sample; that study estimated the HIV prevalence among transgender women to be at 17%.8
Although our 2016 study is the first socioserological project to focus exclusively on transgender women in Dominican Republic, prior socioserological research has been conducted with an amalgamation of sexual and gender minorities and populations that are at higher risk for contracting HIV. In 2004, the Proyecto DELTA serobehavioral study was conducted with MSM and reported an HIV prevalence of 11%.9 In 2008, the first Dominican Republic behavioral surveillance survey with serological linkage, Encuesta de Vigilancia y Comportamiento con Vinculación Serológica (EVCVS I in Spanish) was conducted with sex workers, MSM, transgender women, and drug users; then in 2012, a second wave of EVCVS was conducted (continuing to aggregate transgender women with MSM).10 In the 2012 EVCVS II study, the prevalence of HIV among sexual and gender minorities was estimated to be between 3.9% and 6.9%.10,11
HIV and stigma
Stigma refers to the process of devaluing a group of individuals due to their “deeply discrediting” attributes or behaviors.12,13 Stigma's negative effects on well-being, such as reducing medication adherence, increasing rates of mental illness, increasing substance use as a coping mechanism, and lowering quality of life, have been well documented, and a growing body of research details the injurious effects of stigma on sexual and gender minorities globally and across the LAC region. The HIV Stigma Framework by Earnshaw and Chaudoir suggests that three stigma mechanisms affect health, namely enacted stigma, anticipated stigma, and internalized stigma.14,15 Enacted stigma includes experiences of discrimination, devaluation, and violence.14,15 Anticipated stigma encompasses the expectation of repercussions for holding devalued traits. Internalized stigma is the socioemotional acceptance of negative societal characterizations.
HIV research with sexual and gender minorities has drawn direct and indirect pathways between stigma and HIV-related outcomes, indicating that stigma acts as a barrier to HIV prevention and testing and also is associated with poor treatment outcomes across the entire continuum of care, making stigma reduction a high-priority public health target.16 In Dominican Republic, transgender women may experience enacted stigma through direct assault, violence, and discrimination in employment.6,17,18 When stigma is a barrier to employment, it can affect HIV risk (e.g., entrance into sex work when no other work options are available). Understanding the extent to which transgender women experience stigma is critical to addressing the HIV epidemic, since stigma has been shown to be associated with poor HIV-related outcomes across the continuum of care, and experiencing or internalizing stigma is associated with coping mechanisms such as substance use and engagement in high-risk sexual behaviors, such as sex work, among transgender women.17,19
Substance use and sex work
Transgender women can be economically marginalized and socially stigmatized; there is evidence to suggest that these women may opt into sex work out of financial necessity and may concurrently use substances to cope with stigmatizing attitudes and aggressions. In Dominican Republic where a third of transgender women believe it is difficult to access health care services due to stigma and shame, the likelihood of entering into psychiatric care or therapy for substance use is low,19 exacerbating the precarious lives of many of these women.
The World Health Organization reports that residents of Dominican Republic consume an average of 6.9 liters of alcohol per capita annually, and nearly 30% (29.4%) engage in heavy episodic drinking leading to an average of 3 years of life lost;20 according to Dominican Republic's National Council for HIV and AIDS (CONAVIHSIDA), sexual and gender minorities hold significantly higher rates of substance use as compared with the general population.11 Studies suggest a higher prevalence of substance use and abuse among transgender women compared with the general population and a strong association between negative psychosocial exposures, namely transphobia, discrimination, violence, and stigma, with substance use.21–23
While transgender women may use substances to cope, they may also use substances to facilitate sex work. A recent study found that nearly half (48%) of transgender women from a Dominican Republic sample engaged in sex work, and that sex work was associated with stigma and trauma.24 Relative to those in other occupations, sex workers had higher rates of substance use, but sex work may not be the sole contributing factor to substance use. Being poor, previously abused, having limited education, and being transgender, increase the likelihood of engagement in sex work, substance use and abuse, and risk of contracting HIV.
Methods
Data
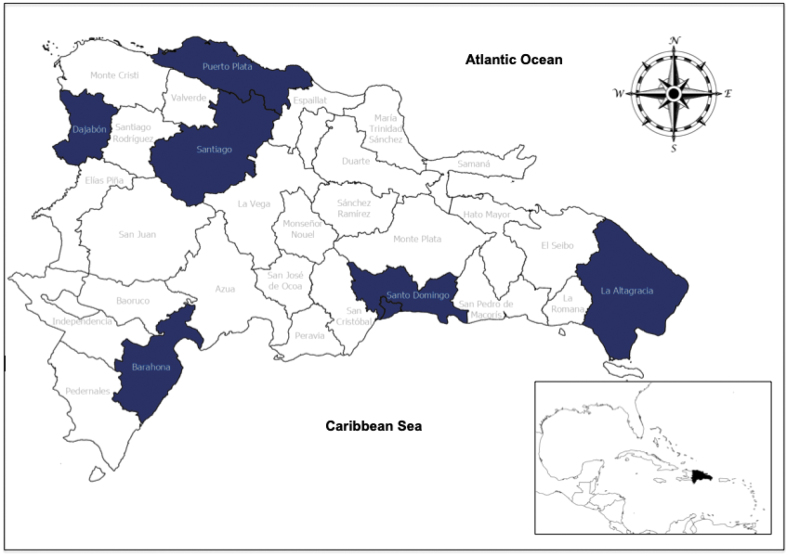
We analyzed data (n = 307) from the third wave of EVCVS III, in which transgender women were disaggregated from the broader sexual and gender minority community in Dominican Republic. This study was funded by CONAVIHSIDA, and was conducted by the Center for Counseling and Integral Research (COIN) and Universidad Iberoamericana (UNIBE). Transgender women were recruited from the Santo Domingo, Santiago, Barahona, Puerto Plata, Dajabón, and La Altagracia provinces. See Fig. 1. Informed consent was obtained verbally; explanatory statements related to informed consent and research considerations were read to the potential participant by a trained interviewer; the potential participant was informed that she could accept or decline to participate without any implications. This process emphasized that participation in EVCVS III was voluntary and that the study participant could refuse to answer any question. Data collection occurred at community settings, such as in parks and nightclubs, between April 2016 and November 2016.
FIG. 1.
Recruitment provinces in Dominican Republic.
Ethics approval
This protocol, including informed consent procedures, was approved by the National Bioethics Council (CONABIOS, #035-2016) and the Institutional Ethics Committee of UNIBE (#CEI2016-04). Approval to analyze data was provided by the University of Alabama at Birmingham Institutional Review Board (#300002551-001).
Patient and public involvement
The Principal Investigator and study team worked closely with transgender women on the refinement of measures. Patients were not directly involved in recruitment, but cisgender and transgender key informants did support recruitment.
Dependent variables: HIV, stigma, and violence
HIV serological status was determined by detection of anti-HIV 1 and 2-specific antibodies. Reactive samples were later confirmed with an immunoassay of antigen and antibodies of p24 structure. Respondents with reactive HIV serological tests were coded as 1 = positive for HIV serostatus; participants with nonreactive tests were coded as 0 = negative.
Stigma was measured on a 0–6 scale (Cronbach's α = 0.77) and captured if the respondent had ever experienced the following events: lied about sexual orientation to get work (internalized stigma), asked to quit work because of trans identity or sexual orientation (enacted stigma), mistreated or refused health services because of trans identity or sexual orientation (enacted stigma), lied about sexual orientation or pretended to be heterosexual to get health care (internalized and perceived stigma), rejected by family for having sex with men (enacted stigma), or refused medical or dental attention because of trans identity or sexual orientation (enacted and perceived stigma). Responses to each of these questions were weighted equally in the summed measure of stigma. Exposure to violence was measured through two questions: respondents were asked if in the last 12 months they had been (1) beaten; and (2) forced to have sex against their will (rape). Respondents answering yes to either question were coded as 1 and the remaining respondents were coded as 0.
Independent variables: demographics and behavioral risk
We included age, educational attainment, income, and salaried employment. Age was measured as a continuous variable in years. Educational attainment was measured with a dichotomous variable (1 = high school education or higher; 0 = less than high school education). Monthly income in pesos was dichotomized to reflect more than 10,001 Dominican pesos a month versus 10,000 or less (1 = more than 10,001 pesos per month, which is equivalent to about $210 USD per month). Respondents reporting engagement in formal salaried work were coded as 1; those who were no engaged in salaried employment were coded as 0.
Sex work was defined as having “ever had sex in exchange for money or other items.” Respondents who reported earnings from sex work were coded as 1, while respondents who did not participate in sex work were coded as 0. Substance use was measured by assessing three indicators: marijuana use, cocaine use, and risk for alcohol dependency. Respondents were asked if they used marijuana or cocaine in the last 6 months. Yes, responses were coded as 1 and no responses as 0. Alcohol dependency was measured with the Alcohol Use Disorders Identification Test (AUDIT) questionnaire, which has been previously validated in Spanish with multiple populations.25–27 The AUDIT questionnaire is scored on a 0–40 scale (Cronbach's α = 0.76) and asked respondents: how often is alcohol consumed; how many alcoholic beverages are usually consumed on a normal day; how often are 6 or more alcoholic beverages consumed in 1 day; how often in the past year has the respondent been unable to stop drinking once starting to drink; how often in the past year could the respondent not do what was expected of them because of drinking alcohol; how often in the past year has the respondent needed to drink on an empty stomach to recover after drinking a lot the day before; how often during the past year has the respondent felt remorse or guilt after drinking; how often in the past year has the respondent been unable to remember what happened the night before due to drinking; how often has the respondent or someone else been injured because the respondent was drunk; and if a family member, friend, doctor, or health professional been concerned about the respondent's drinking or suggested the respondent stop drinking. AUDIT scores in the range of 8–15 represented a medium risk of alcohol problems, scores of 16–20 represent a high risk of alcohol problems,28 and scores above 20 represent likely addiction. We dichotomized the score to indicate high risk of alcohol dependency ( = 1) compared with medium or low risk of dependency ( = 0).
Statistical analyses
We conducted multivariate analyses to evaluate associates of HIV, stigma, and violence. Observations with missing values were deleted using listwise deletion after ensuring missingness was at random. We also developed logistic regression models to examine the statistical relationship among HIV, violence, substance use, and individual characteristics. Since the stigma variable is measured as a count, we employed a negative binomial regression to estimate the relationship among stigma, substance use, and individual characteristics. All models were estimated using Stata 16.1.
Results
Descriptive statistics
Sample characteristics are in Table 1. Respondents' age ranged from 16 to 62 years; average age was 26.6 years old. Approximately 20% had a secondary education or higher (18.2%) and 29.0% of the sample had monthly earnings of 10,000 Dominican pesos or greater. Three quarters (74.2%) of the sample participated in sex work at some point in their lives, and over a third were receiving salaried income (39.4%). Engagement in sex work does not preclude one from also working in a salaried position. Marijuana and cocaine use were limited, with 11.1% of respondents reporting marijuana use and 11.4% reporting cocaine use. Around 42% of the sample was at high risk of alcohol dependency (41.8%). About one fifth of the sample (21.92%) reported experiencing violence, and 61.6% reporting experiencing at least one stigma event. Of note, 35.8% of our national sample of transgender women were living with HIV, indicated by a reactive (positive) HIV serological, laboratory confirmed test.
Table 1.
Study Participant Characteristics (n = 307)
| Respondent characteristic | Frequency (%) |
|---|---|
| Age | |
| Mean | 6.61 |
| SD | 7.69 |
| High school level education | |
| Yes | 26 (18.24) |
| No | 251 (81.76) |
| High income | |
| Yes | 82 (28.98) |
| No | 201 (71.02) |
| Salaried income | |
| Salaried income | 121 (39.41) |
| No salaried sources | 186 (60.59) |
| Ever engaged in sex work | |
| Yes | 219 (74.24) |
| No | 76 (25.76) |
| Marijuana use | |
| Yes | 34 (11.07) |
| No | 273 (88.93) |
| Cocaine use | |
| Yes | 35 (11.40) |
| No | 272 (88.60) |
| AUDIT score | |
| Mean | 9.75 |
| SD | 6.36 |
| Stigma score | |
| Mean | 1.59 |
| SD | 1.78 |
| Exposure to any violence (e.g., physical, sexual) | |
| Yes | 64 (21.92) |
| No | 228 (78.08) |
| HIV serological status | |
| Negative | 197 (64.17) |
| Positive | 110 (35.83) |
AUDIT, Alcohol Use Disorders Identification Test; SD, standard deviation.
Multivariate analyses
Logistic regression models estimated the covariates of experienced violence and HIV. We report that negative binomial fixed-effects regression models were used to estimate the relationships among stigma, individual characteristics, and substance use as shown in Table 2. Respondents who participated in sex work were more likely to have experienced higher levels of stigma [incidence rate ratio (IRR): 1.70, p < 0.05]. Respondents who reported using marijuana were less likely to have experienced higher levels of stigma while respondents who reported using cocaine were more likely to have experienced higher levels of stigma compared with respondents who did not (IRR: 0.54, p < 0.05; IRR: 1.72, p < 0.05; respectively). Respondents reporting high risk of alcohol dependency were slightly less likely to have experienced higher levels of stigma (IRR: 0.97, p < 0.05). Finally, respondents reporting experiencing violence were associated with higher risk to experiencing stigma (IRR: 1.97, p < 0.001).
Table 2.
Multivariate Analysis, Stigma, and Violence as Outcomes of Interest (n = 143)
| Stigma |
Exposure to violence |
|
|---|---|---|
| IRR (95% CI) | OR (95% CI) | |
| Age | 1.005 (0.982–1.029) | 0.993 (0.927–1.063) |
| Education | ||
| ≥High school | 0.799 (0.484–1.329) | 0.854 (0.191–3.816) |
| National median income | ||
| Above median | 0.754 (0.510–1.115) | 1.609 (0.568–4.561) |
| Engaged in sex work | ||
| Yes | 1.697 (1.039–2.770)* | 6.264 (0.754–2.021) |
| Salaried employment | ||
| Yes | 1.058 (0.732–1.528) | 0.775 (0.288–2.084) |
| Marijuana use | ||
| Yes | 0.537 (0.294–0.982)* | 2.734 (0.635–11.768) |
| Cocaine use | ||
| Yes | 1.724 (1.047–2.838)* | 0.839 (0.220–3.195) |
| AUDIT score | 0.963(0.935–0.993)* | 1.166 (1.070–1.270)* |
| Exposure to violence | ||
| Yes | 1.970 (1.311, 2.961)*** | — |
| Stigma score | — | 1.608 (1.237, 2.091)*** |
p < 0.05, **p < 0.01, ***p < 0.001.
CI, confidence interval; IRR, incidence rate ratio; OR, odds ratio.
Models predicting associates of violence were estimated with logistic regression. Respondents with higher risk of alcohol dependency were associated with 1.2 times higher odds of experiencing physical violence or rape compared with those with lower risk of alcohol dependency [odds ratio (OR): 1.17, p < 0.001]. Respondents reporting higher levels of stigma were associated with 1.6 higher odds of experiencing violence (OR: 1.61, p < 0.001).
Respondents with high school level of education or higher were associated with lower odds of living with HIV compared with respondents with less than a high school level of education (OR: 0.26, p < 0.05). Respondents with higher risk of alcohol dependency were associated with lower odds of HIV seropositivity compared with respondents with lower risk of alcohol dependency (OR: 0.92, p < 0.05). Respondents who had experienced violence were associated with over three times higher odds of HIV seropositivity relative to respondents who had not experienced violence (OR: 3.15, p < 0.05) (Table 3).
Table 3.
Multivariate Analysis, HIV as the Outcome (n = 143)
| Living with HIV | |
|---|---|
| OR (95% CI) | |
| Age | 1.08 (1.023–1.141)** |
| Education | |
| ≥High school | 0.26 (0.076–0.889)* |
| National median income | |
| Above median | 1.04 (0.448–2.422) |
| Engaged in sex work | |
| Yes | 1.64 (0.596–4.530) |
| Salaried employment | |
| Yes | 0.61 (0.270–1.381) |
| Marijuana use | |
| Yes | 0.33 (0.079–1.355) |
| Cocaine use | |
| Yes | 3.04 (0.882–10.445) |
| AUDIT score | 0.92 (0.862–0.991)* |
| Exposure to violence | |
| Yes | 3.15 (1.185–8.388)* |
| Exposure to stigma | |
| Yes | 0.66 (0.275–1.566) |
p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
Our first objective was to characterize the lived experiences and health risks of transgender women in Dominican Republic. In addition to finding high rates of stigma and violence, we uncovered an HIV prevalence rate of over one third (35.8%), confirmed through laboratory-based serological testing. This high statistic signals that collecting self-reported HIV status from sexual and gender minorities, particularly in stigmatizing settings, may be subject to underreporting. If confirmed through replication studies, such a high HIV seroprevalence would warrant immediate intervention to ensure transgender women living with HIV in Dominican Republic are aware of their status, understand how HIV transmission occurs, are in care, and are virally suppressed. Since nearly three-quarters (74.1%) of transgender women who participated in our study self-reported engaging in sex work, and sexual contact is a primary mode of HIV transmission, another potential target group for HIV risk reduction are those individuals who purchase or coerce sexual acts from transgender women in Dominican Republic.
Our second objective was to test the hypothesis that we would find significant associations among stigma, experiences of violence, and HIV. We found some support for this hypothesis; stigma was associated with sex work, cocaine use, and higher risk for alcohol use, specifically, violence was associated with higher risk o alcohol use and stigma. Since our stigma scale encompassed measures of enacted, internalized, and perceived stigma, we were unable to parse the effects of each mechanism, but were able to include all three mechanisms of note, as defined in the HIV Stigma Framework.15
HIV seropositivity was associated with age, lower education, violence, and higher risk for alcohol dependency. Findings suggest that our sample of transgender women had high rates of negative exposures, potentially lower quality of life, and those risks were associated with HIV, indicating the need to address HIV risk among transgender women. To do so, researchers, policy makers, and clinical providers should leverage human rights approaches and intersectional frameworks that examine HIV risk considering the social standing of sexual and gender minorities, their lack of power, effects of stigma and discrimination, and socioeconomic status. While, this study was conducted in Dominican Republic, a resource-limited setting, this recommendation also applies to research with transgender populations in wealthier nations, since HIV services have been designed primarily around the needs of cisgender women, not necessarily transgender women.29,30
This study contributes to the growing body of literature on sexual and gender minorities in this region. Logie et al. found that a significant number of Jamaican transgender women and transgender female sex workers experienced events of forced sex, childhood sexual abuse, and incidents of intimate partner violence.31 A series of studies conducted with the Transgender Health National Survey found high rates of sex work, experiences with abuse, suicidal ideation, and even attempted murder against transgender women in Dominican Republic.1,5,17 Thus, while our study is not the first to examine the experiences of transgender women in the Caribbean, it is—to our knowledge—the first to conduct a serological and behavioral study with an exclusively transgender sample in Dominican Republic producing a serologically confirmed HIV estimate of nearly 36%.
Limitations should be considered when extending our findings. First, data are cross-sectional, which precludes any claims of causality and directionality. Transgender women are stigmatized; thus, reaching them, even in community settings, is challenging. During the planning of this study, we intended to collect data from transgender women in the provinces of Elias Piña and Independencia, but when local residents learned that transgender women were our target population, they became physically and verbally aggressive toward our interviewers necessitating that the team abandon data collection plans due to verifiable safety concerns. Because of this, data collectors relied on nonrandom sampling techniques, which restricts generalizability. Self-reported measures are subject to recall and desirability biases. Stigma and violence measures were limited; data on stigma and violence were collected using new scales that were tailored for transgender women in Dominican Republic. Individual measures of enacted, internalized, and anticipated stigma were untested. Current alcohol use appears correlated with prior sex work, but the lack of alignment in time or recall (sex work reporting is over the lifetime while alcohol use is assessed more recently) warrants further investigation.
Limitations notwithstanding, this study offers novel insights into the experiences of transgender women in Dominican Republic. While there may be value in extrapolating findings to other LAC countries to inform their public health efforts, this should be done with care and caution. LAC nations share languages, colloquialisms, and some cultural values, but there are notable differences in national policy, epidemiological profiles, and public health approaches to the HIV epidemic. For example, a recent study found significant differences in HIV knowledge and condom use among female sex workers working at the Haiti and Dominican Republic border.32 A related desk review found widely differing approaches to HIV prevention in the region with Argentina having implemented structural interventions to address societal exclusion, and Brazil and Mexico adopting treatment as prevention strategies.33
Results offers key insights for researchers, advocates, and policymakers working with transgender women to inform structural and behavior interventions, as well as health policy designed to reduce HIV risk, fortify the individual against the deleterious effects of stigma and violence, and improve the well-being of transgender women in Dominican Republic. While future research that validates our findings and attempts to attain a larger sample size by utilizing more comprehensive recruitment designs that can reach into less densely populated regions is warranted, our findings, in and of themselves, justify an urgent public health response to support and protect transgender women in Dominican Republic.
Acknowledgments
The authors thank Rosa Sanchez of CONAVIHSIDA, the monitoring and evaluation technical working group, members of nongovernmental organizations working with transgender populations, and the University of Alabama at Birmingham (UAB) Sparkman Center for Global Health. The authors express their gratitude to Christian King from Trans Amigas Siempre Amigas (TRANSSA) for her leadership and support of this study.
Authors' Contributions
H.B. is the lead author and designed the study presented in this publication. R.P.-R. is the senior author; he designed and implemented the original project, including all data collection; R.P.-R. was supported by L.T. K.R.H. was the lead methodologist, and S.A.B. supported K.R.H. in data management and analyses. S.N. provided senior-level support on framing this study. All authors contributed to the writing and editing processes.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Research reported in this publication was supported by the Dominican Republic Ministry of Health through the National Council of HIV and AIDS (CONAVIHSIDA), the National Institute of Mental Health (NIMH), and Fogarty International Center (FIC) of the National Institutes of Health (NIH) under Award Nos. K01MH116737 (H.B.) and R21TW011761 (H.B. and R.P.-R.).
References
- 1. Budhwani H, Hearld KR, Milner AN, et al. . Transgender women's experiences with stigma, trauma, and attempted suicide in the Dominican Republic. Suicide Life Threat Behav 2018;48:788–796. [DOI] [PubMed] [Google Scholar]
- 2. De Boni R, Veloso VG, Grinsztejn B. Epidemiology of HIV in Latin America and the Caribbean. Curr Opin HIV AIDS 2014;9:192–198. [DOI] [PubMed] [Google Scholar]
- 3. Halperin DT, de Moya EA, Pérez-Then E, et al. . Understanding the HIV epidemic in the Dominican Republic: A prevention success story in the Caribbean? J Acquir Immune Defic Syndr 2009;51 Suppl 1:S52–S59. [DOI] [PubMed] [Google Scholar]
- 4. AVERT. HIV and AIDS in Latin America: The Caribbean Regional Overview. 2018. Available at: https://www.avert.org/professionals/hiv-around-world/latin-america/overview (Last accessed November 9, 2020).
- 5. Budhwani H, Hearld KR, Hasbun J, et al. . Transgender female sex workers' HIV knowledge, experienced stigma, and condom use in the Dominican Republic. PLoS One 2017;12:e0186457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hearld KR, Milner AN, Budhwani H, et al. . Alcohol use, high risk behaviors, and experiences of discrimination among transgender women in the Dominican Republic. Subst Use Misuse 2019;54:1725–1733. [DOI] [PubMed] [Google Scholar]
- 7. Edwards JK, Hileman S, Donastorg Y, et al. . Estimating sizes of key populations at the national level: Considerations for study design and analysis. Epidemiology 2018;29:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ONUSIDA. El Estado epidémico del VIH en la Republica Dominicana, Dirección General de Control de Infecciones de Transmisión sexual y SIDA. Santo Domingo, Dominican Republic, 2014. [Google Scholar]
- 9. UNAIDS. HIV modes of transmission model: Analysis of the distribution of new HIV infections in the Dominican Republic and recommendations for prevention. 2010. Available at: https://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/countryreport/2010/201011_MOT_DominicanRepublic_en.pdf (Last accessed October 23, 2021).
- 10. CONAVIHSIDA. Second Behavioral Surveillance Survey with Serological Linkage in Key Populations: UNFPA. 2012. Available at: http://www.conavihsida.gob.do/ (Last accessed October 23, 2021).
- 11. CONAVIHSIDA. Segunda Encuesta de Vigilancia de Comportamiento con Vinculación Serológica en Poblaciones Claves: Gais, Trans, y Hombres que tienen sexo con hombres (GTH), Trabajadoras sexuales (TRSX), Usuarios de Drogas (UD). Santo Domingo, Dominican Republic, 2014. Available at: https://mcr-comisca.org/actividades-regionales/febrero-2014-curso-de-malaria/encuestas-de-vigilancia-de-comportamiento-evc/87-encuesta-de-vigilancia-de-comportamiento-en-vinculacion-serologica-en-poblaciones-claves-de-republica-dominicana-2012/file (Last accessed October 23, 2021).
- 12. Turan B, Budhwani H, Fazeli PL, et al. . How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav 2017;21:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goffman E. Stigma: Notes on the Management of Spoiled Identity. Upper Saddle River, NJ: Prentice Hall, 1963. [Google Scholar]
- 14. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav 2009;13:1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Earnshaw VA, Smith LR, Chaudoir SR, et al. . HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav 2013;17:1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Budhwani H, Robles G, Starks TJ, et al. . Healthy choices intervention is associated with reductions in stigma among youth living with HIV in the United States (ATN 129). AIDS Behav 2021;25:1094–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Budhwani H, Hearld KR, Milner AN, et al. . Transgender women's drug use in the Dominican Republic. Transgend Health 2017;2:188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hamilton A, Shin S, Taggart T, et al. . HIV testing barriers and intervention strategies among men, transgender women, female sex workers and incarcerated persons in the Caribbean: A systematic review. Sex Transm Infect 2020;96:189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. PAHO. Blueprint for the Provision of Comprehensive Care for Trans Persons and Their Communities in the Caribbean and Other Anglophone Countries. Arlington, VA: John Snow, Inc., 2014. [Google Scholar]
- 20. Hearld KR, Budhwani H, Martínez-Órdenes M, et al. . Female sex workers' experiences of violence and substance use on the Haitian, Dominican Republic border. Ann Glob Health 2020;86:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hotton AL, Garofalo R, Kuhns LM, et al. . Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ Prev 2013;25:62–71. [DOI] [PubMed] [Google Scholar]
- 22. Keuroghlian AS, Reisner SL, White JM, et al. . Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend 2015;152:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reback CJ, Fletcher JB. HIV prevalence, substance use, and sexual risk behaviors among transgender women recruited through outreach. AIDS Behav 2014;18:1359–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Milner AN, Hearld KR, Abreau N, et al. . Sex work, social support, and stigma: Experiences of transgender women in the Dominican Republic. Int J Transgend 2019;20:403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ballester L, Alayo I, Vilagut G, et al. . Validation of an online version of the Alcohol Use Disorders Identification Test (AUDIT) for alcohol screening in spanish university students. Int J Environ Res Public Health 2021;18:5213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. García Carretero M, Novalbos Ruiz JP, Martínez Delgado JM, et al. . Validation of the Alcohol Use Disorders Identification Test in university students: AUDIT and AUDIT-C. Adicciones 2016;28:194–204. [DOI] [PubMed] [Google Scholar]
- 27. Pérula de Torres LA, Fernández-García JA, Arias-Vega R, et al. . Validation of the AUDIT test for identifying risk consumption and alcohol use disorders in women. Aten Primaria 2005;36:499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cut-off score. Addiction 1995;90:1349–1356. [DOI] [PubMed] [Google Scholar]
- 29. Auerbach JD, Moran L, Watson C, et al. . We are all women: Barriers and facilitators to inclusion of transgender women in HIV treatment and support services designed for cisgender women. AIDS Patient Care STDs 2020;34:392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bockting W, MacCrate C, Israel H, et al. . Engagement and retention in HIV care for transgender women: Perspectives of medical and social service providers in New York City. AIDS Patient Care STDs 2019;34:16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Logie CH, Wang Y, Lacombe-Duncan A, et al. . Factors associated with sex work involvement among transgender women in Jamaica: A cross-sectional study. J Int AIDS Soc 2017;20:21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Budhwani H, Hearld KR, Hasbún J, et al. . Assessing human immunodeficiency virus (HIV) prevention through knowledge and condom use among female sex workers at the border of Haiti and Dominican Republic. AIDS Patient Care STDS 2020;34:477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Silva-Santisteban A, Eng S, de la Iglesia G, et al. . HIV prevention among transgender women in Latin America: Implementation, gaps and challenges. J Int AIDS Soc 2016;19(3 Suppl 2):20799. [DOI] [PMC free article] [PubMed] [Google Scholar]