Abstract
Background
The SARS-CoV-2 virus pandemic is primarily transmitted by direct contact between infected and uninfected people, though, there are still many unknown factors influencing the survival and transmission of the virus. Air temperature is one of the main susceptible factors. This study aimed to explore the impact of air and land surface temperatures on Covid-19 transmission in a region of Iran.
Method
Daily Land Surface Temperature (LST) measured by satellite and Air Temperature measured by weather station were used as the predictors of Covid-19 transmission. The data were obtained from February 2020 to April 2021. Spatio-temporal kriging was used in order to predict LST in some days in which no image was recorded by the satellite. The validity of the predicted values was assessed by Bland-Altman technique. The impact of the predictors was analyzed by Distributed Lag Non-linear Model (DLNM). In addition to main effect of temperature, its linear as well as non-linear interaction effect with relative humidity were considered using Generalized Additive Model (GAM) and a bivariate response surface model. Sensitivity analyses were done to select models’ parameters, autocorrelation model and function of associations.
Results
The dose-response curve revealed that the impact of both predictors was not obvious, though, the risk of transmission tended to be positive due to low values of temperatures. Although the linear interaction effect was not statistically significant, but joint patterns showed that the impact of both LST and AT tended to be different when humidity values were changed.
Conclusion
However the findings suggested that both LST and AT were not statistically important predictors, but they tended to predict the Covid-19 transmission in some lags. Because of local based evidence, the wide confidence intervals and then non-significant values should be cautiously interpreted.
Keywords: Ambient temperature, Covid-19, Transmission, Iran
1. Introduction
COVID-19, caused by the SARS-CoV-2 is a respiratory infectious disease. The SARS-CoV-2 virus pandemic was started through all countries since 2019. At the beginning of the pandemic, many issues were unknown about the pathogen, origin of the virus, transmission, prevention and treatment of the disease (Chaudhuri et al., 2020, Christophi et al., 2021). In addition to direct contact between infected and uninfected people, it is also transmitted through respiratory droplets from infected people with or without symptoms (Gupta, 2020; O'Reilly et al., 2020). However, there are still many unknown factors influencing survival and transmission of the viruses. Air temperature is one of the main susceptible factors (Rashed et al., 2020). When temperature is low, spread of the virus in the nasal mucosa tends to be increased, because mucociliary clearance is slowed down and the virus spreading into the respiratory tract can accordingly be easier. Also, low temperatures enhance survivability of the coronaviruses on surfaces (Azuma et al., 2020; Zhu et al., 2021) which result in high chance of its transmission.
The SARS-CoV pandemic which occurred at the beginning of 21st century and was spread from China in 2002 (Casanova et al., 2010) had similar genomes to SARS-CoV-2. Several laboratory studies investigated the effect of temperature on transmission and survival of the SARS-CoV. They found that high temperatures and low humidity decreased the virus's survival on surfaces (Demongeot et al., 2020; Tan et al., 2005; Yuan et al., 2006). Therefore, risk of the virus transmission was higher at low temperatures. Because of the similarity mentioned, these findings support the hypothesis that risk of the Covid-19 transmission at low temperatures might be higher than high temperatures. There are few evidences about the impact of environmental factors including temperature and humidity on spread of the COVID-19. Their findings are not fully consistent; some of them reported positive association (Bashir et al., 2020; Menebo, 2020; Xie and Zhu, 2020) but some found a negative association (Li et al., 2020; Méndez-Arriaga, 2020; Prata et al., 2020). Therefore, role of the ambient temperature on the virus transmission is still a question.
As shown by previous studies (Lee et al., 2016; Weinberger et al., 2019; Shi et al., 2016), Land Surface Temperature (LST) measured by satellites is a strong predictor of mortality. This predictor might be an important predictor of the Covid-19 transmission as well. However, previous time-series studies about Covid-19 used station temperature data as exposure. Therefore, the present study assessed the impact of two measurements including LST measured by satellite Terra and Air Temperature (AT) measured by weather stations on the Covid-19 transmission in a region of Iran, North Khorasan, Bojnurd. North Khorasan province, located in north east of Iran, has different climatic conditions; the south counties have hot desert and north counties have cold semi-arid climate based on the Köppen climate classification (Climatic classification o, 2020).
2. Methods
2.1. Data
In this study, two datasets, including Land Surface Temperature (LST) measured by satellite Terra, and Air Temperature (AT) measured in a weather station were used as exposures. The Covid-19 cases measured by health deputy of North Khorasan were the outcome of this study. The region of under study was Bojnurd which is located in North Khorasan province (Fig. 1 ). Based on Köppen climate classification, Bojnurd has a cold semi-arid climate with mean annual air temperature of 13.3 °C. In this region. the most wet month is March with the average of 42.4 mm, and the driest month is August with 6.0 mm. Also, the average annual precipitation is 272.4 mm (Climatic classification, 2020).
Fig. 1.
Geographic location of the region under study; Bojnurd, North Khorasan, Iran.
2.2. Exposure measurement
The first predictor used in the study was air mean temperature measured by a weather station in the region. It was obtained from Iran meteorological organization. In addition, wind speed and relative humidity were obtained from the organization in order to control their confounding effect. There was no missing in the data, thereby having no need for any imputation method for the variables.
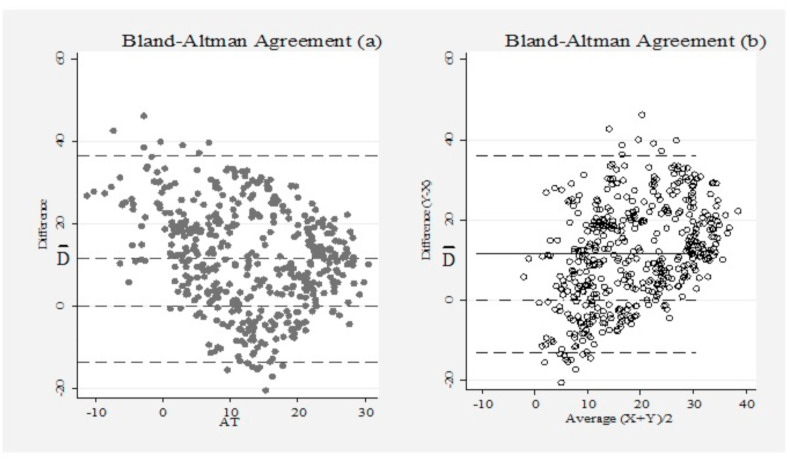
The daily air mean temperature has been used as the predictor of Covid-19 transmission in some studies (Xie and Zhu, 2020; Li et al., 2020; Méndez-Arriaga, 2020; Tosepu et al., 2020), though, LST might be an important predictor as well. In this study, MODIS/Terra LST&E Daily L3 Global Coarse Resolution (MOD11B1) was used as another exposure. The LST is produced in day/night at 6 km spatial resolution in the sinusoidal projection. The images were freely downloaded from NASA's Level 1 and Atmospheric Archive and Distribution System (https://search.earthdata.nasa.gov/) from 20 February 2020 when the covid-19 became epidemic in Iran. The daytime LST was used in this study, because most people are exposed to outdoor temperature in daytime. Although the area of under study was the province center (Bojnurd), but the images were downloaded for whole area of North Khorasan. The LST from other locations (Out of Bojnurd) were used in spatio-temporal kriging in order to predict LST for Bojnourd in the days when there were no measured observations by the satellite. The reason for lack of LST in some days might be some obstacles such as clouds which make the satellite unable to measure the LST. In the spatio-temporal kriging method, a parametric function was fitted to a semivariogram in which both latitude and longitude were used as predictors. Therefore, universal spatio-temporal kriging was used in this study. In order to assess the model performance and prediction validity, the variance of predicted values and Bland-Altman technique were used. In the Bland-Altman method, a plot of difference between the two predictors (LST and AT) against their mean was used. It allows us to investigate any possible relationship between the measurement error and the true value. However, because we do not know the true value, the mean of the two measurements was a good estimate in the method (Bland and Altman, 2010).
The agreement between the two predictors can be summarized by calculating the bias which is estimated by average of the difference ( in vertical axes of Fig. 2 ) and the confidence interval of the differences. It is expected that most of the differences lie between 95% confidence interval. In the method, the more distance between average of the difference () and zero, the more biased values might exist. The Bland-Altman plot has been presented in Fig. 2. In the plot, most of the differences have been lied between 95% confidence interval (Fig. 2, the highest and lowest dashed lines). It shows that the differences have been normally distributed (Bland and Altman, 2010). This normal distribution suggests that the variation between temperatures value are negligible. It should be mentioned that in Fig. 2,a, the average of the two measurements was superseded by the AT itself, since it can be seen as standard value in our study, and it seems that such replacement makes results more validated (Krouwer, 2008). In this case, most of observations lied between the confidence interval and almost similar bias to the plot b was seen. Therefore, however some bias exists in the spatio-temporally predicted values, but it can be used as an exposure in our model.
Fig. 2.
Bland-Altman agreement between kriged Land Surface Temperature (LST) and Air Temperature (AT); in plot a and b the AT and the average values of AT and LST were used as standard measurement, respectively.
It should be mentioned that the impact of cold, very cold, heat and very hot values were assessed in this study. They were defined as percentiles 5th, 1st, 95th and 99th, respectively.
2.3. Outcome measurement
The Covid-19 data were collected by health deputy of North Khorasan from the beginning of the COVID-19 pandemic. In the present study, new confirmed outpatients were included in analysis from February 2020 to April 2021. The date of symptoms onset was measured for every case by health workers. Given that the present study aimed to see the impact of temperature on Covid-19 transmission, the date of symptoms onset was less likely to be the date of transmission. Indeed, we assumed that the transmission had already happened some days ago. Therefore, we matched temperature and Covid-19 cases by the date of transmission. This distance between the transmission date (i.e., exposure to temperature) and the date of symptoms onset, named incubation period or lag, should be therefore addressed in the analysis. Most of the previous researches showed that the incubation period (i.e. lag in the concept of this study) was variable from the median of 5–8 days (Alene et al., 2021; McAloon et al., 2020; Quesada et al., 2020; Qin et al., 2020). However, symptoms onset occurs within about 14 days for more than 95% of infected persons (Lauer et al., 2020), showing variability in the incubation period. Therefore, in this study, dose-response association was reported for lags 5, 6, 7 and 8. In addition, the impact of cold and heat values of both LST and AT was estimated for maximum lag of 14 (0–14).
2.4. Statistical analysis
In order to see the impact of both LST and AT by different lags, Distributed Lag Non-linear Model (DLNM) was applied. In this model, the impact of temperature is defined in two dimensions, named exposure-response and lag-response associations. In the first dimension (exposure-response), we used natural cubic spline function with three knots located in percentiles 25, 75 and 90. However, we did sensitivity analysis to choose the best function and location of the knots based on Quassi-Akaike Information Criteria (Q-AIC). The best function for the second dimension (lag-response) was natural cubic spline with three knots placed in percentiles 25, 50 and 75. The two dimensions were incorporated by a cross-basis function in DLNM. The cross-basis function of the associations was then entered in Quassi-Poisson regression model in which overdispersion was considered. The regression model was as following:
| (1) |
Where is the number of Covid-19 cases in day t. A link function, named Log link which is suitable to model relative risk was used in the regression model. In the model, is intercept, Cb is the crossbasis function made in DLNM. The is lagged disease number in logarithmic scale to control autocorrelation. The autocorrelation in infectious diseases is likely to be stronger than non-infectious diseases. This is because of true contagion autocorrelation which is need to be controlled (Imai et al., 2015). The logarithm of the number was used because previous studies suggested that past cases as predictor can result in overadjustment (Nottmeyer and Sera, 2021). This can be explained by time series susceptible-infectious-recovery (SIR) models. The models suggest that for communicable diseases, using logarithm scale (i.e. log (Yt−l)), can more accurately match the mechanisms of disease transmission (Imai et al., 2015). Indeed, autocorrelation of residuals in the case of communicable disease is pathogen-specific that needs to be accounted for (Nottmeyer and Sera, 2021). Because of the similarity between the link function used for the outcome as dependent variable and the logarithmic scale of the lagged outcome as exposure, the issue can be negligible. In addition, previous studies (Imai et al., 2015; Nottmeyer and Sera, 2021) as well as our study showed that the function can improve the models fitness. We did sensitivity analysis based on partial autocorrelation to choose the best lagged outcome.
In the model, NS is natural cubic spline function. The df = 3 was chosen for the confounders (humidity and wind speed) based on model fit using Q-AIC and literatures (Yang et al., 2015; Stafoggia et al., 2008). The seasonality, trend and unmeasured confounders (e.g. change in diagnostic tests) were controlled for using an artificial variable (i.e., Time). The df for the variable was chosen based on sensitivity analysis and literatures as well. In addition, public holidays in Iran including any national festival or mourning as well as days of week were controlled for in the model. The holiday and days of week (DOW) were indicator variables in which the non-holidays and Friday were chosen as reference value, respectively.
In order to calculate relative risk in each lag, percentiles 5th (cold), 1st (very cold), 95th (heat) and 99th (very hot) were compared to Minimum Transmission Temperature (MTT). The MTT was a value with the lowest risk of transmission.
The analysis was done in both univariate (single effect of predictors) and multiple regressions. In both regressions, the time-related variables (i.e., time, DOW and holiday) were controlled. So, in addition to temperature, the dose-response association between humidity and wind speed with the Covid-19 cases were reported.
2.5. Interaction effect between humidity and temperature
Interaction effect between temperature and humidity was assessed in both linear and non-linear ways by Generalized Additive Model (GAM). In order to assess the linear interaction, humidity was categorized to three levels named dry, comfortable, and sultry. The comfortable condition was chosen as reference (main effect) and the temperature effect on Covid-19 transmission in the others two were compared to the reference. In order to assess non-linear interaction effect, bivariate response surface model was used in the GAM. In this model, both univariate and bivariate spline functions of two types of exposures can be applied (Ruppert et al., 2003). In other words, we can fit s (x1, x2) in addition to s (x3) and s (x4), for example. Thus, we used the following model to graphically see the joint pattern of temperature and humidity on Covid-19 transmission:
| (2) |
In which, the TS is thin-plate spline. It should be mention that the model was applied to lags 5, 6, 7 and 8.
3. Results
The average daily number of covid-19 cases was about 30 that most of them were male (about 18 males vs 12 females). The majority of the cases were young (with the maximum number of 200). In Table 1 , the average daily number of covid-19 cases along its distribution statistics has been provided. In the table, descriptive statistics of weather parameters have been provided as well; the daily mean temperatures were 24.32 and 12.82 for LST and AT, respectively.
Table 1.
Descriptive statistics of daily Covid-19 cases and weather parameters in Bojnourd during February 2020 to April 2021.
| Sub Groups | Mean (±SE) | Minimum | Maximum | Percentiles |
|||
|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | |||||
| Covid-19 Cases | Male | 18.01 (1.04) | 1 | 120 | 4 | 10 | 25 |
| Female | 12.92 (0.75) | 1 | 93 | 3 | 8 | 17 | |
| Young | 28.83 (1.66) | 0 | 203 | 7 | 16 | 39 | |
| Elderly | 0.95 (0.08) | 0 | 10 | 0 | 0 | 1 | |
| Total | 29.78 (1.71) | 1 | 213 | 7 | 17 | 41 | |
| Weather Parameters | LST | 24.32 (0.62) | −5.95 | 49.6 | 13.93 | 24.22 | 36.2 |
| AT | 12.82 (0.42) | −11.2 | 30.5 | 6.1 | 13 | 20.2 | |
| Humidity | 53.43 (0.9) | 11.5 | 90.88 | 36.75 | 55.38 | 68.38 | |
| Wind speed | 2.1 (0.06) | 0 | 6.38 | 1.25 | 2 | 2.88 | |
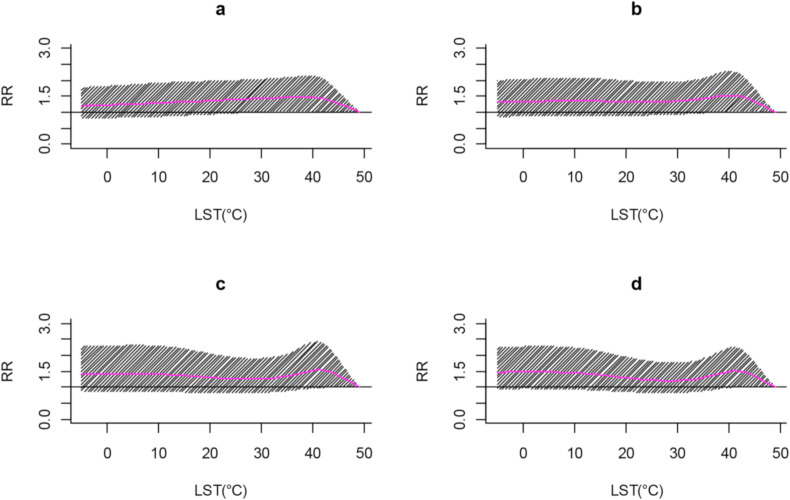
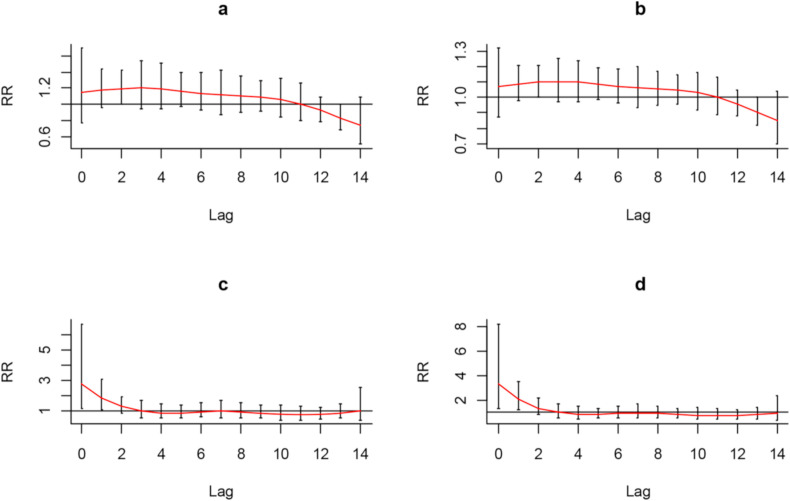
The dose-response effect (exposure-outcom association) of all LST values has been shown by lags 5, 6, 7 and 8 in the Fig. 3 . No values of the predictor had statistically significant impact on Covid-19 transmission in the lags. Fig. 4 represents lag-outcom association. In the figure, impact of temperature has been specifically presented for low (cold and very cold) and high (heat and very hot) values of LST by all 14 lags. As seen, the impact of both cold and very cold temperatures was not statistically significant, though, the relative risks of transmission were higher than 1 (RR > 1) in most of lags for the values. The same pattern was roughly seen for heat and very hot values (Fig. 4c and d). The univariate results of the plot have been provided in supplementary file (Fig. S1). The only significant adverse impact of the predictor was seen at low values and lag 10.
Fig. 3.
Dose-response curve of Land Surface Temperature (LST) effect on Covid-19 transmission; a, b, c and d represent impact of LST in lags 5, 6, 7 and 8, respectively.
Fig. 4.
The nonlinear effect of Land Surface Temperature (LST) on Covid-19 transmission by different lags. In plots a, b, c and d, the cold (percentile 5th), very cold (percentile 1st), heat (percentile 95th) and very hot (percentile 99th) temperatures were compared to minimum transmission risk value (49 °C).
Fig. 5 shows exposure-outcom association of AT and Covid-19 transmission in lags 5, 6, 7 and 8. Apparently, like LST, no values of AT had statistically significant impact on the transmission in the lags. In the Fig. 6 , impact of AT has been specifically provided for the low and high values in all lags (lag-outcom association). It revealed that, excepting lag 0, nighter low (cold and very cold) nor high (heat and very hot) values had significant effect, as well. The result of univariate analysis for this variable has been shown in Fig. S2.
Fig. 5.
Dose-response curve of Air Temperature (AT) effect on Covid-19 transmission; a, b, c and d represent impact of AT in lags 5, 6, 7 and 8, respectively.
Fig. 6.
The nonlinear effect of AT on Covid-19 transmission by different lags. In plots a, b, c and d, the cold (percentile 5th), very cold (percentile 1st), heat (percentile 95th) and very hot (percentile 99th) temperatures were compared to minimum transmission risk value (-11 °C).
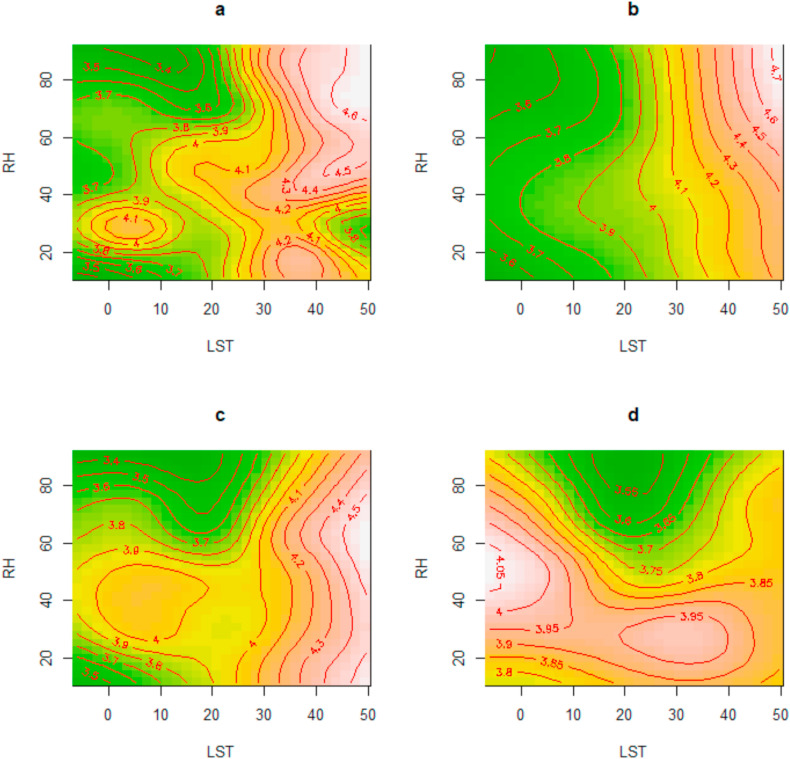
Both linear and non-linear interaction effect between temperature and humidity were assessed in this study. There was no linear interaction effect between both LST and AT and humidity (the results have been provided for lags 5, 6, 7 and 8, in Table S1 in supplementary file). However, humidity tended to non-lineary modify the temperature effect on total new cases. For example, in the plot d in Fig. 7 , low values of LST had the highest impact when the values of humidity were at comfortable level (middle values). In the other hand, low values of AT tended to have the highest effect when the humidity was at low level (dry condition). As seen in Fig. 8 , the low values of AT in plot a, b and c had the highest effect when humidity was at the lowest level (dry condition). When we considered higher incubation period (lag 8), the pattern was changed (Fig. 8, d). Hawever, we found no significant impact of humidity itself. The results of both univariate an multiple regression of this variable as well as wind speed have been shown in supplementary file (Figs. S3, S4, S5 and S6).
Fig. 7.
Contour plots of Land Surface Temperature (LST) effect on Covid-19 daily cases by different levels of Relative Humidity (RH). The values represent estimated covid-19 cases and the graded colors from green to red and light shows the estimations from low to high, respectively. The plots a, b, c and d represent the effect for lags 5, 6, 7, and 8, respectively. . (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 8.
Contour plots of Air Temperature (AT) effect on Covid-19 daily cases by different levels of Relative Humidity (RH). The values represent estimated covid-19 cases and the graded colors from green to red and light shows the estimations from low to high, respectively. The plots a, b, c and d represent the effect for lags 5, 6, 7, and 8, respectively. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
4. Discussion
The results of this study showed that neither LST nor AT had statistically significant effect on Covid-19 transmission. However, the relative risk of transmission due to cold values, especially the cold values of AT, tended to be higher than 1 in most of the lags. The results of previous studies showed that there is still controversy about the impact of AT. For example, a study conducted by Briz-Redón et al. in Spain showed that there was no evidence of association between air temperature and the diseases (Briz-Redón et al. 2020). Also, a study conducted in 8 cities in US revealed that the air temperature was a week predictor of Covid-19 transmission, with particularly no significant impact in Albany (Runkle et al., 2020). In addition, in the study conducted by To et al. (2021) in Canada, there was no significant impact of air temperature on the diseases. They also found no significant impact of the predictor on reproductive number of Covid-19. Meanwhile, there are some studies showing significant effect of air temperature on Covid-19; a study conducted by Shi et al. (2020) in China showed that the intensity of Covid-19 epidemy decreased slightly by higher temperatures (the relative risk along its 95% confidence interval were 0.96 and 0.93–0.99, respectively). In the study, they used meta-analysis of data from 28 provinces and found statistically significant association between air temperature and the diseases incidence. Also, another study in Bangladesh found that high temperatures can significantly reduce the number of new cases. The controversy can be highly explained by different methodology and exposure/outcome measurement used by previous studies. For example, in the study conducted in Canada (To et al., 2021), effective reproductive number and cumulative incidence were the outcome of the study. In addition, linear regression was applied to the data in the study. While, Shi et al. (2020) used DLNMs in their study. In addition to methodology, time period of the studies might be another reason for the heterogenicity of the results. Because of power issue, it is hard to show any significant associations in a short period of time. It is also hard to control for some time-varying unmeasured confounders (i.e., seasonality or trend) when the period of the study is short. Indeed, some measurements such as diagnostic tests have been changed during time. This changes which might not be seen in a short time lead to a trend in Covid-19 cases that needs to be accounted for. Therefore, any inference about the previous evidences as well as our results should be cautiously used.
In addition to air temperature, land surface temperature was used as the predictor of the diseases in this study. The results revealed that it was not a strong predictor. Few studies have assessed the impact of daily LST on Covid-19. Most of the previous evidences such as the studies conducted by Parida et al. (2021) and Maithani et al. (2020) assessed the impact of lockdown on LST during Covid-19 epidemy. Because of the outcome used in the studies, they can not be compared to our results. While the LST was not a strong predictor in our study, but there are many evidences, showing its strong effect on human mortality (Lee et al., 2016; Shi et al., 2016; Xu et al., 2014). Because of the effect and high resolution of the data, it might be a good predictor of the diseases. Therefore, we suggest that more efforts need to be done about the impact of daily LST on Covid-19.
This was a local study and the statistically nonsignificant impact of both predictors might highlight the low power of the study, though, but the positive effect (RR > 1) of cold temperature supports the hypothesis that risk of Covid-19 transmission at low temperatures might be higher than high temperatures. There are some mechanisms to explain the hypothesis. For example, the low temperatures hinder humans' innate immunity, resulting in decrease blood supply and then reduce the provision of immune cells to the nasal mucosa (Wu et al., 2020). In addition, the SARS-CoV-2 tolerates more low temperatures than high, thereby having more chance to find new host.
Depending on lag, another finding of the study was that humidity tended to non-laniary modify the impact of both LST and AT. For example, cold values of AT had the highest effect when humidity was at low level (plots a, b and d in Fig. 8). Few studies controlled for the interaction effect. Qi et al. (2020) considered the effect in their study which was conducted in China. Similar to our findings, they found interaction effect between air temperature and the relative humidity. This effect might be explained by the hypothesis that a combination of low AT and humidity results in the nasal mucosa prone to small ruptures, thereby making more chance to the virus invasion (Qi et al., 2020). Meanwhile, most of the previous studies have assessed the main effect of humidity and temperature, and strong evidences are still need to explore the interaction effect. However, our results can give a useful clue to policymakers as well as researchers to address the issue when any preventive programs are made.
A strength of this study was to use kriged LST as the predictor of Covid-19. It had almost similar impact to AT. In addition, we did several sensitivity analyses in which the same results were seen. These makes the results more robust. However, the study was accomplished in a small region of Iran. A probable reason for the statistically non-significant effects might be therefore the low power of this study. This is a limitation of our study and, thus, a multy-center study is suggested to be done in Iran. Another limitation of the present study was not to predict air temperature using LST. The predicted air temperature might be an important predictor of the diseases. So, we suggest that the predicted air temperature (using LST) be used in multi-center or multi-country studies.
5. Conclusion
The results showed that the impact of both LST and AT on Covid-19 transmission was not statistically significant in most of lags, though, the risk of transmission was positive. Also, the linear interaction between the predictors and humidity was not significant, though, but humidity seemed to non-liniary modify the temperature effect. Because of local-based study, the findings should be cautiously interpreted. However, they give a clue to health policymakers as well as researchers to prevent the disease spreading.
Funding
This study was supported by the Deputy of research and technology, North Khorasan University of Medical Sciences.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was financially supported by North Khorasan University of Medical Sciences by Grant No. 990175. We thank the Deputy of Health of North Khorasan University of Medical Sciences for providing the data.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2022.112887.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alene M., Yismaw L., Assemie M.A., Ketema D.B., Gietaneh W., Birhan T.Y. Serial interval and incubation period of COVID-19: a systematic review and meta-analysis. BMC Infect. Dis. 2021;21(1):1–9. doi: 10.1186/s12879-021-05950-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Á Briz-Redón, Serrano-Aroca Á. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728:138811. doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azuma K., Kagi N., Kim H., Hayashi M. Impact of climate and ambient air pollution on the epidemic growth during COVID-19 outbreak in Japan. Environ. Res. 2020;190:110042. doi: 10.1016/j.envres.2020.110042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. vol. 728. Science of The Total Environment; 2020. p. 138835. (Correlation between Climate Indicators and COVID-19 Pandemic in New York, USA). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Int. J. Nurs. Stud. 2010;47(8):931–936. [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri S., Basu S., Kabi P., Unni V.R., Saha A. 2020. Modeling Ambient Temperature and Relative Humidity Sensitivity of Respiratory Droplets and Their Role in Covid-19 Outbreaks. arXiv preprint arXiv:200410929. [Google Scholar]
- Christophi C.A., Sotos-Prieto M., Lan F.-Y., Delgado-Velandia M., Efthymiou V., Gaviola G.C., et al. Ambient temperature and subsequent COVID-19 mortality in the OECD countries and individual United States. Sci. Rep. 2021;11(1):1–9. doi: 10.1038/s41598-021-87803-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Climatic Classification of North Khorasan Province. General Meteorological Department of North Khorasan; 2020. http://www.nkhmet.ir [Available from: [Google Scholar]
- Demongeot J., Flet-Berliac Y., Seligmann H. Temperature decreases spread parameters of the new Covid-19 case dynamics. Biology. 2020;9(5):94. doi: 10.3390/biology9050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta D. 2020. Effect of Ambient Temperature on COVID-19 Infection Rate. Available at SSRN 3558470. [Google Scholar]
- Imai C., Armstrong B., Chalabi Z., Mangtani P., Hashizume M. Time series regression model for infectious disease and weather. Environ. Res. 2015;142:319–327. doi: 10.1016/j.envres.2015.06.040. [DOI] [PubMed] [Google Scholar]
- Krouwer J.S. Why Bland–Altman plots should use X, not (Y+ X)/2 when X is a reference method. Stat. Med. 2008;27(5):778–780. doi: 10.1002/sim.3086. [DOI] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M., Shi L., Zanobetti A., Schwartz J.D. Study on the association between ambient temperature and mortality using spatially resolved exposure data. Environ. Res. 2016;151:610–617. doi: 10.1016/j.envres.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Xu X.-L., Dai D.-W., Huang Z.-Y., Ma Z., Guan Y.-J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maithani S., Nautiyal G., Sharma A. Investigating the effect of lockdown during COVID-19 on land surface temperature: study of Dehradun city, India. Journal of the Indian Society of Remote Sensing. 2020;48(9):1297–1311. [Google Scholar]
- McAloon C., Collins Á., Hunt K., Barber A., Byrne A.W., Butler F., et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open. 2020;10(8) doi: 10.1136/bmjopen-2020-039652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735:139560. doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737:139659. doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nottmeyer L.N., Sera F. Influence of temperature, and of relative and absolute humidity on COVID-19 incidence in England-A multi-city time-series study. Environ. Res. 2021;196:110977. doi: 10.1016/j.envres.2021.110977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. The Lancet Planetary Health. 2020;4(5):e172. doi: 10.1016/S2542-5196(20)30106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parida B.R., Bar S., Kaskaoutis D., Pandey A.C., Polade S.D., Goswami S. Sustainable Cities and Society; 2021. Impact of COVID-19 Induced Lockdown on Land Surface Temperature, Aerosol, and Urban Heat in Europe and North America; p. 103336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J., You C., Lin Q., Hu T., Yu S., Zhou X.-H. Estimation of incubation period distribution of COVID-19 using disease onset forward time: a novel cross-sectional and forward follow-up study. Sci. Adv. 2020;6(33) doi: 10.1126/sciadv.abc1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quesada J., López-Pineda A., Gil-Guillén V., Arriero-Marín J., Gutiérrez F., Carratala-Munuera C. English Edition. Revista Clínica Española; 2020. Incubation Period of COVID-19: A Systematic Review and Meta-Analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashed E.A., Kodera S., Gomez-Tames J., Hirata A. Influence of absolute humidity, temperature and population density on COVID-19 spread and decay durations: multi-prefecture study in Japan. Int. J. Environ. Res. Publ. Health. 2020;17(15):5354. doi: 10.3390/ijerph17155354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runkle J.D., Sugg M.M., Leeper R.D., Rao Y., Matthews J.L., Rennie J.J. Short-term effects of specific humidity and temperature on COVID-19 morbidity in select US cities. Sci. Total Environ. 2020;740:140093. doi: 10.1016/j.scitotenv.2020.140093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruppert D., Wand M.P., Carroll R.J. Cambridge university press; 2003. Semiparametric Regression; p. 386. [Google Scholar]
- Shi L., Liu P., Wang Y., Zanobetti A., Kosheleva A., Koutrakis P., et al. Chronic effects of temperature on mortality in the Southeastern USA using satellite-based exposure metrics. Sci. Rep. 2016;6(1):1–8. doi: 10.1038/srep30161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafoggia M., Schwartz J., Forastiere F., Perucci C. Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. Am. J. Epidemiol. 2008;167(12):1476–1485. doi: 10.1093/aje/kwn074. [DOI] [PubMed] [Google Scholar]
- Tan J., Mu L., Huang J., Yu S., Chen B., Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community. 2005;59(3):186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To T., Zhang K., Maguire B., Terebessy E., Fong I., Parikh S., et al. Correlation of ambient temperature and COVID-19 incidence in Canada. Sci. Total Environ. 2021;750:141484. doi: 10.1016/j.scitotenv.2020.141484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger K.R., Spangler K.R., Zanobetti A., Schwartz J.D., Wellenius G.A. Comparison of temperature-mortality associations estimated with different exposure metrics. Environmental Epidemiology (Philadelphia, Pa) 2019;3(5) doi: 10.1097/EE9.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Liu Y., Ma Z., Toloo G.S., Hu W., Tong S. Assessment of the temperature effect on childhood diarrhea using satellite imagery. Sci. Rep. 2014;4(1):1–8. doi: 10.1038/srep05389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Yin P., Zhou M., Ou C.-Q., Guo Y., Gasparrini A., et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart. 2015;101(24):1966–1972. doi: 10.1136/heartjnl-2015-308062. [DOI] [PubMed] [Google Scholar]
- Yuan J., Yun H., Lan W., Wang W., Sullivan S.G., Jia S., et al. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Control. 2006;34(4):234–236. doi: 10.1016/j.ajic.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu G., Zhu Y., Wang Z., Meng W., Wang X., Feng J., et al. The association between ambient temperature and mortality of the coronavirus disease 2019 (COVID-19) in Wuhan, China: a time-series analysis. BMC Publ. Health. 2021;21(1):1–10. doi: 10.1186/s12889-020-10131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.