Abstract
Hoffa's fat pad (HFP) is the most commonly afflicted among all the knee fat pads. Anterior knee pain is common in various pathologies of HFP, as it is richly innervated. A potpourri of the intrinsic and extrinsic pathologies and the tumors and tumor-like conditions affect HFP, and MRI remains the fundamental modality to assess them and provide a specific diagnosis.
Keywords: fat pads around knee joint, Hoffa's fat pad, infrapatellar fat pad lesions, MRI, MRI knee, radiology
Anatomy of Hoffa's Fat Pad
Fat pads around the knee joint have been a significant area of research, with the infrapatellar fat pad or HFP being the major one. Other anterior fat pads are the anterior suprapatellar (quadriceps) and posterior suprapatellar (prefemoral) fat pads ( Fig. 1 ). 1
Fig. 1.
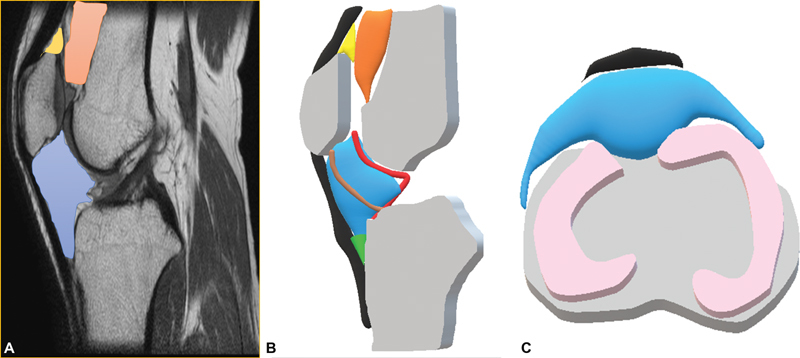
Fat pads around knee joint. Sagittal proton density (PD) images ( A ) and graphical sagittal ( B ) and axial ( C ) images depicting suprapatellar fat pad (yellow), prefemoral pad fat (orange), Hoffa's fat pad (HFP) (blue), infrapatellar plica (brown), deep infra-patellar recess (green), menisci (pink), and synovial lining (red lining).
The borders of HFP are formed by the joint capsule and patellar tendon anteriorly, the synovium-lined joint cavity posteriorly, the inferior pole of the patella superiorly, and the proximal tibia and deep infrapatellar bursa inferiorly. It is made up of fat lobules with interspersed fibrous septa attached posteriorly to the menisci with the most prominent septa being the infrapatellar plica ( Fig. 2 ). Arterial branches from the superior and inferior genicular arteries connected by the horizontal anastomotic branches supply the HFP. Femoral and common peroneal and saphenous nerves richly innervate the HFP. 2
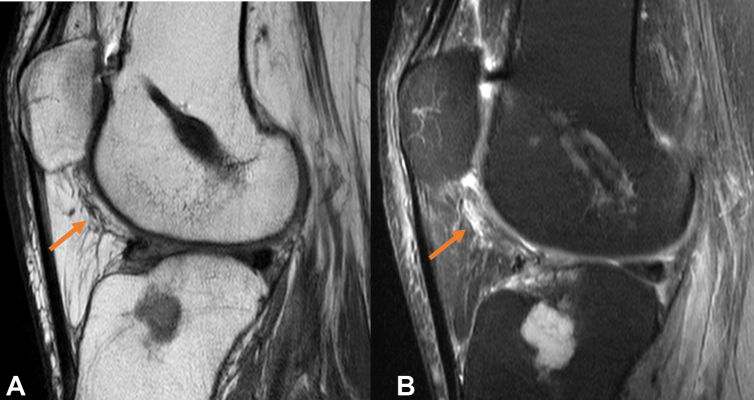
Fig. 2.
Synovial recesses around Hoffa's fat pad (HFP). Proton density fat-suppressed (PDFS) sagittal images depicting normal HFP and distended supra-Hoffitic recess with fluid (red margin) in image ( A ). Note made of anterior cruciate ligament tear ( A ). Infra-Hoffitic recess (green) noted in image ( B ) and image ( C ) reveals the communication between the two recesses around HFP (depicted in image C ).
Imaging of Hoffa's Fat Pad
Usually, the basic imaging sequences for MRI knee are used for the evaluation of HFP. These include proton density images with fat suppression (PDFS) in the axial and sagittal planes, T2-weighted coronal images, and sagittal T1W fast spin echo images with an approximate field of view of 140 to 150 mm and a slice thickness of 2.5 mm with no gap. The MR protocol may need to be tailored for the evaluation of HFP lesions, depending upon the pathology suspected. Additional gradient echo (GRE) images should be obtained to evaluate the possibility of hemorrhage or calcification, wherever required. The mass-like lesions of the HFP may require contrast evaluation and precontrast T1 weighted images in a plane that best evaluates the pathology should be performed (usually the sagittal plane). The postgadolinium contrast T1W fat-suppressed images were obtained in all three planes. HFP is hyperintense on T1- and T2-weighted images following signal intensity as the adjacent subcutaneous fat with hypointense intrinsic fibrous septae. The biomechanics of HFP relies upon the flexibility of HFP, which moves in varying degrees during the extension of the knee joint and reduces friction between the patella, patellar tendon, and synovium and deep-seated structures. Many studies have documented HFP to be a reservoir of cytokines, adipokines, and lipid mediators with the presence of inflammatory and mesenchymal stem cells in it. 3 4 5 6
Trauma and Trauma-related Pathologies
Hoffa's Disease
The impingement of the infrapatellar fat pad results from repetitive or acute microtrauma, leading to Hoffa's disease. The knee joint movement causes alterations at the tissue level with subsequent inflammation, edema, and hemorrhage. This, in turn, leads to hypertrophy and predisposes to crushing or impingement between the femur and tibia. Further mechanical stress may lead to fibrous scar tissue formation, necrosis, and eventually metaplastic cartilage or progress to ossification.
Fat pad impingement may also occur in the absence of prior injury secondary to joint space narrowing, attributable to other causes like patella alta. In the initial stages, poorly marginated T2 hyperintense and T1 hypointense areas are seen ( Fig. 3 ), which may cause mass effect over the patellar tendon.
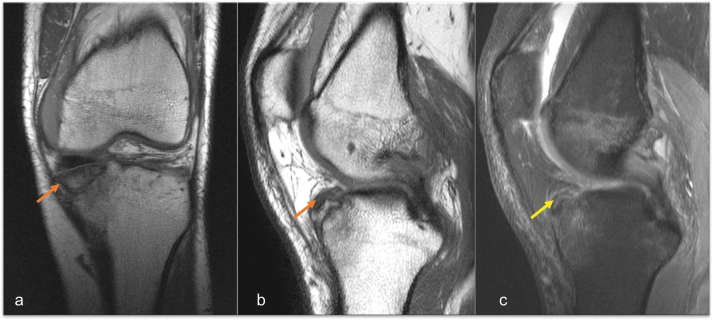
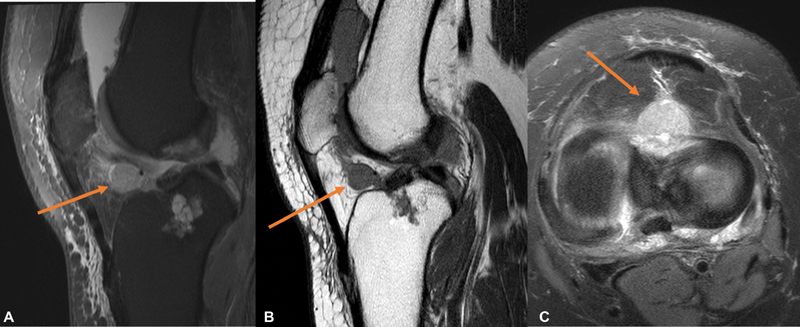
Fig. 3.
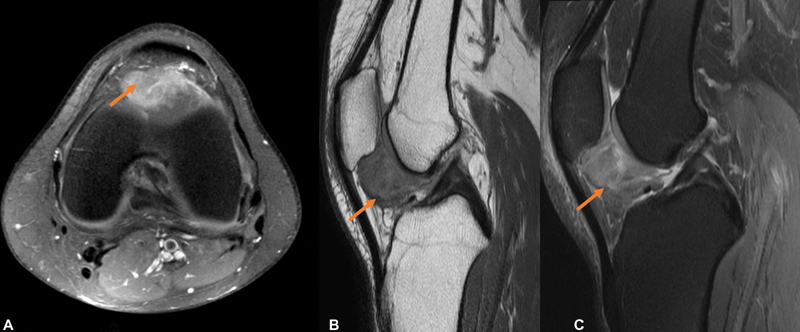
Hoffa's disease . Axial proton density fat-suppressed magnetic resonance imaging (PDFS MRI) ( A ), sagittal T2 fat suppressed ( B ), and sagittal PDFS ( C ) images reveal globular hyperintense signal intensity lesion along HFP, which is abutting the patella superiorly.
Further, in chronic stages, there can be fibrosis (appears hypointense on all sequences) which gradually progress to osteochondral metaplasia. 7 8 Depending upon the stage of the disease, it needs to be differentiated from inflammatory changes due to other causes in the early stages, and lesions presenting as heterogeneous masses and fibrosis in HFP in the chronic stages.
Posttraumatic
Fractures in the vicinity of HFP show reactive edematous changes due to shear injury or direct impact including patellar, tibial, and femoral condylar fractures. Anterior cruciate ligament (ACL) injuries are known to be associated with shear injury in HFP. The imaging appearances may range from subtle PD/T2 hyperintensity/edema to extensive hemorrhage. ( Fig. 4 ). Displaced torn ligaments may be seen along the HFP, mimicking a small tumor. ( Fig. 5 ).
Fig. 4.
Posttraumatic Hoffa's fat pad (HFP) edema. Proton density (PD) coronal ( A ), sagittal ( B ), and PD fat-suppressed (PDFS) sagittal magnetic resonance imaging (MRI) images ( C ) depict anterior tibial plateau fracture with mild displacement of the fracture fragment (orange arrow) and reactive edema involving infrapatellar fat pad (yellow arrow).
Fig. 5.
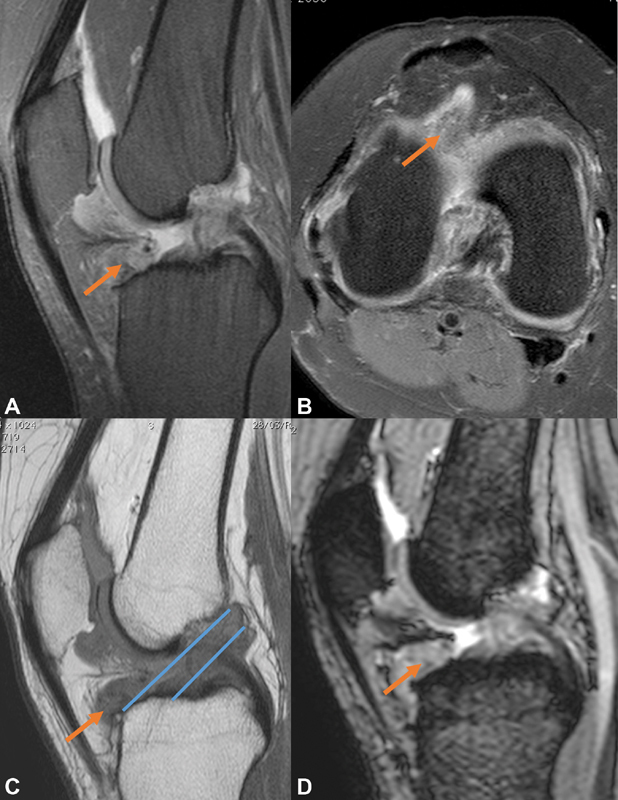
Torn anterior cruciate ligament (ACL) fibers in Hoffa's fat pad (HFP) mimicking a lesion: Proton density fat suppressed (PDFS) sagittal ( A ), PDFS axial ( B ), sagittal T1 images ( C ), and gradient echo (GRE) sagittal images show torn hyperintense ACL fibers along the HFP (orange arrow), which appear hyperintense on PDFS images and hypointense on T1WI, with nonvisualization of normal ACL hypointense band (parallel blue lines along the Blumensaat's line).
Postoperative Changes
The initial postarthroscopy appearances can be a typically linear and horizontal fibrotic reaction along the arthroscopic portal site through the HFP ( Fig. 6 ). It may produce a more extensive fibrotic reaction within the fat pad. Metal fragments remaining after the surgery demonstrate low-signal intensity on all sequences and show “blooming” on GRE images due to metallic susceptibility artifacts ( Fig. 7 ).
Fig. 6.
Postarthroscopy fibrosis. Sagittal T1 ( A ) and sagittal proton density fat-suppressed (PDFS) ( B ) magnetic resonance imaging (MRI) images demonstrating linear fibrosis coursing through the infrapatellar fat pad along the arthroscopic portal with linear hypointense screw markings along distal femur. Incidentally detected, chondroid lesion along proximal tibial epimetaphysis.
Fig. 7.
Postsurgical changes in Hoffa's fat pad (HFP). Case 1: Proton density fat-suppressed (PDFS) sagittal and PD sagittal images ( A and B ) showing extensive susceptibility artifacts (orange arrows) in HFP in a case of autologous osteochondral grafting. Case 2: PDFS sagittal and PD images ( C and D ) reveal a small susceptibility artifact in HFP in a case of post-anterior cruciate ligament (ACL) reconstruction.
A cyclops lesion represents localized arthrofibrosis occurring after ACL reconstruction. The reaction to exposed ACL graft material or operative debris has been postulated as the etiology implicated in the postoperative loss of knee extension 9 ( Fig. 8 ).
Fig. 8.
Cyclops lesion. Sagittal proton density (PD) ( A ), sagittal ( B ), and axial ( C ) PD fat-suppressed magnetic resonance imaging (PDFS MRI) images reveal the presence of nodular soft-tissue mass, which extends into the intercondylar region and the apex of the infrapatellar fat pad and appears intermediate to hypointense indicative of fibrosis. Arthroscopy still image ( D ) confirms the presence of the cyclops lesion.
Secondary to Adjacent Disorders
Meniscal and ACL tears, patellar tendinopathies, and cysts are commonly associated with HFP pathologies in the form of edema, tear, or fibrosis. Focal edema is commonly associated with the impingement of the HFP between the tibia and femur. 10 Patellar tendon pathologies may cause mechanical impingement of HFP 7 between the femur and tibia and usually manifest in the form of focal HFP edema along the inferior aspect ( Fig. 9 ).
Fig. 9.
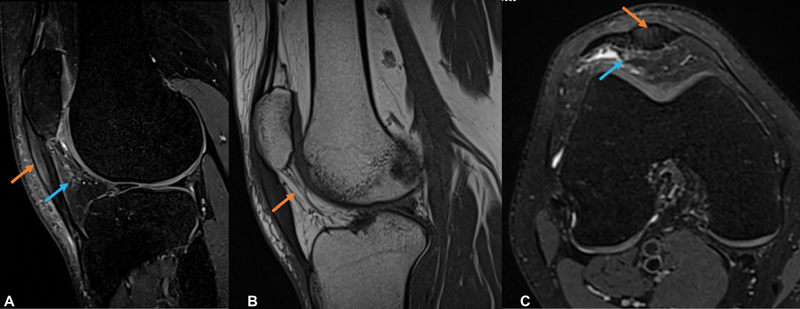
Patellar tendinosis with Hoffa's fat pad (HFP) edema: ( A ) Proton density fat suppressed (PDFS), ( B ) T1 sagittal PD, and ( C ) axial PDFS images reveal bulky hyperintense patellar tendon along its proximal and mid aspect (orange arrow) with edema along the superior aspect of HFP (blue arrow).
Meniscal and Ganglion Cysts
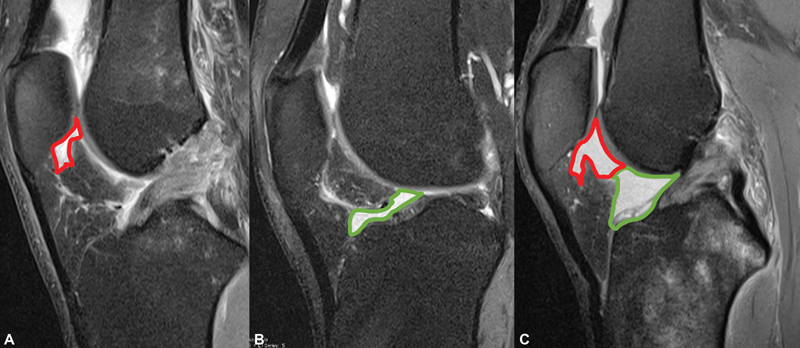
Synovial fluid extrusion secondary to complex and horizontal meniscal tears (lateral more than medial) results in meniscal cyst formation, which may project into HFP. MRI reveals a T2 hyperintense marginated cystic structure contiguous with the meniscal tear margin of a horizontal or a complex tear and can be multiseptated. It has been postulated that the leakage of fluid across the meniscal cyst wall may contribute to HFP edema. It has to be differentiated from the loculations of joint effusion which are commonly observed as the two normal synovial clefts along the posterior aspect of the HFP get distended; one located superiorly in a vertical orientation and the other located anterior to the menisci in a horizontal orientation ( Fig. 10 ).
Fig. 10.
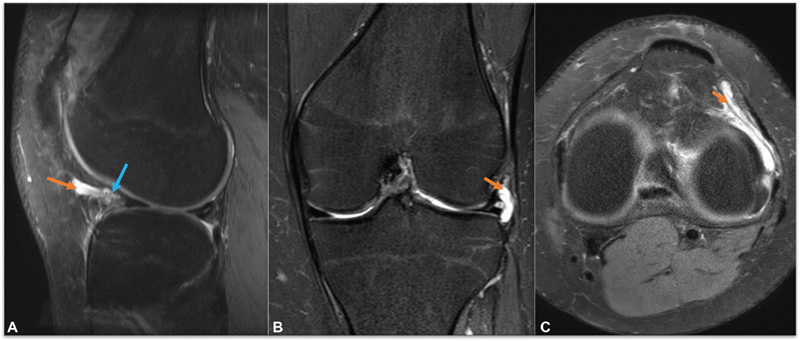
Parameniscal cyst in Hoffa's fat pad (HFP). Proton density fat-suppressed (PDFS) sagittal ( A ), coronal ( B ), and axial images ( C ) show a small loculated fluid intensity lesion in the infrapatellar fat pad anterior to the anterior horn of lateral meniscus, which shows intrinsic hyperintensity (orange arrow-cyst). Communication with the tear at the capsular surface of body of adjacent meniscus confirms the diagnosis (blue arrow).
Ganglion cysts, primarily containing viscous dense fluid, are encapsulated by fibrous tissues and lack the synovial lining. They can be solitary or multiple, round or globular, multi- or uniloculated, and may demonstrate a neck or communication with adjacent joint spaces ( Fig. 11 ). Both the cysts may frequently present as asymptomatic swellings, around the joints, cause mass effect on the adjacent structures, and be a constant source of pain. Asymptomatic patients can be followed-up, whereas painful cysts can be treated by ultrasound-guided local steroid and local anesthetic injections. Surgical resection is rarely indicated in nonresponsive cases. 2 11
Fig. 11.
Benign ganglion cyst of Hoffa's fat pad (HFP). Sagittal proton density fat-suppressed (PDFS) ( A ) and PD ( B ) magnetic resonance imaging (MR) images depicting a well-defined, homogeneous multiloculated cyst arising from anterior synovial alar fold and projecting into the infrapatellar fat.
Displaced Osteochondral Fragments
Following trauma, osteochondral and bony fragments may be lodged along the HFP, along the intra-articular aspect, maybe a significant cause of anterior knee pain, and may cause symptoms of locking. MRI helps in the identification of the origin of the fragment, its constitution, associated injuries, and acts as a road map for surgical repair ( Figs. 12 - 14 ). 2
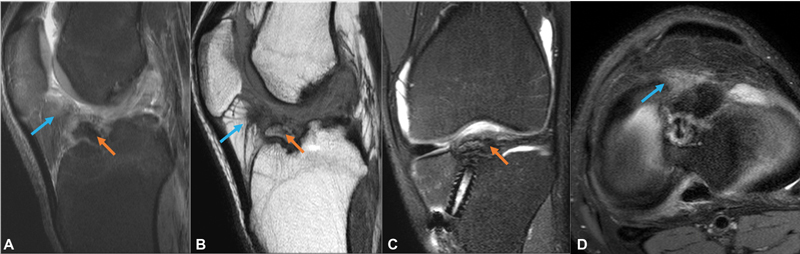
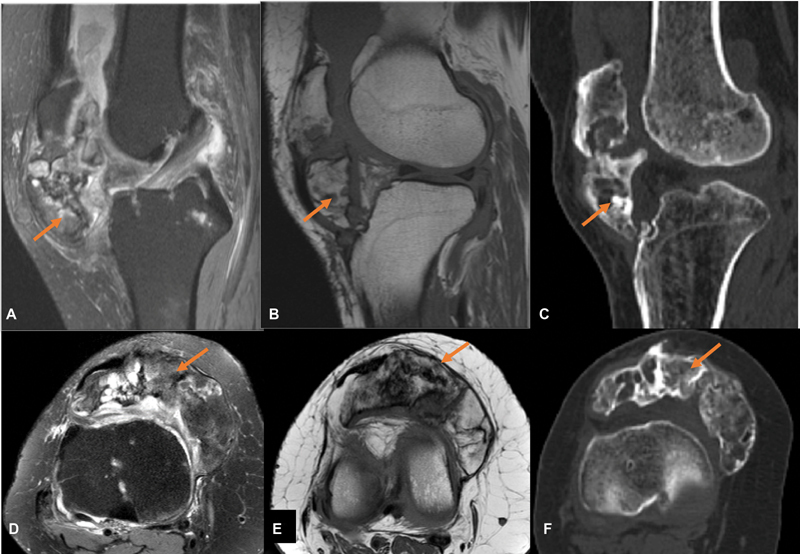
Fig. 12.
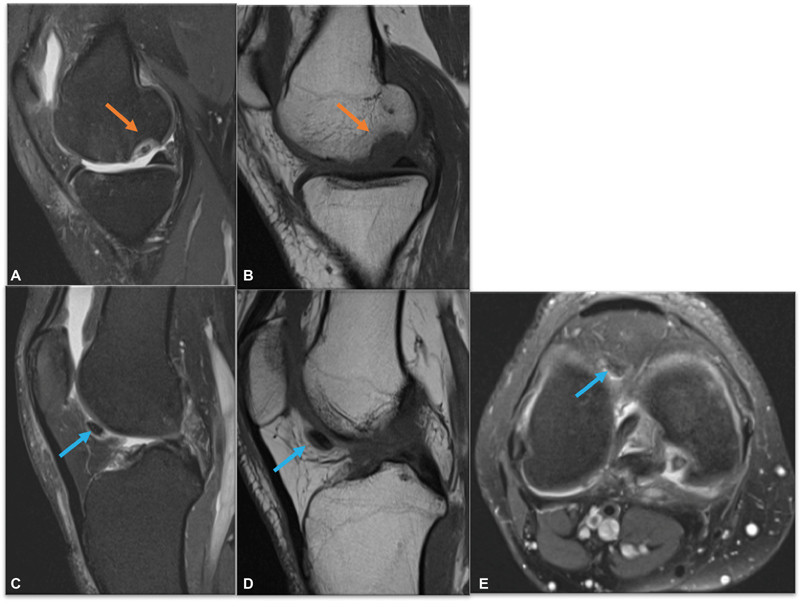
Osteochondral fragment in Hoffa's fat pad (HFP). Proton density fat-suppressed (PDFS) sagittal images ( A and C ), PD sagittal images ( B and D ), and axial PDFS ( E ) images show an osteochondral defect at posterior of the medial femoral condyle (orange arrow) with a displaced osteochondral fragment in the synovial recess along infrapatellar fat pad (blue arrow).
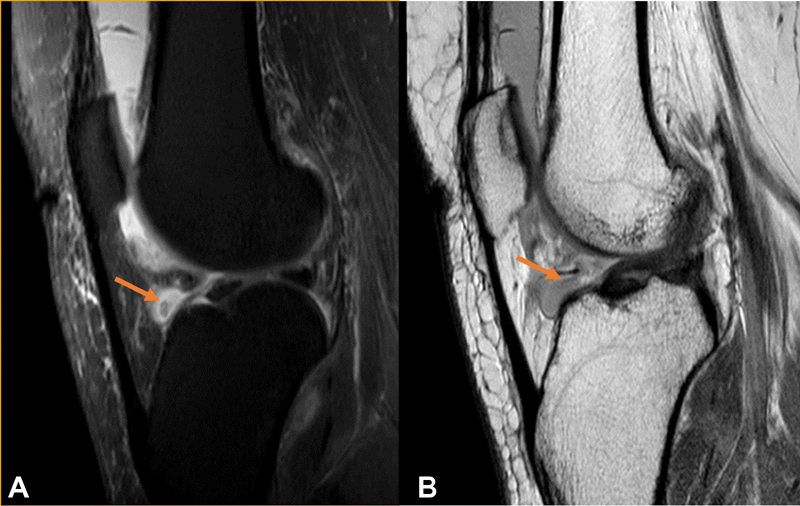
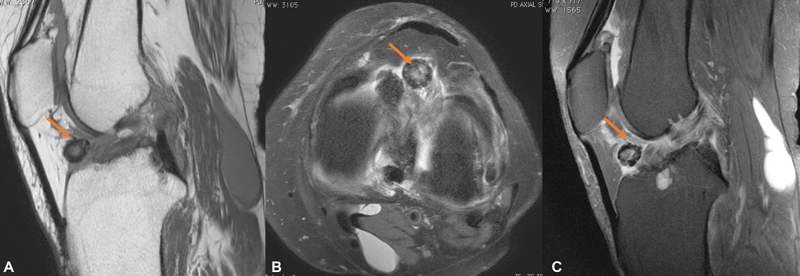
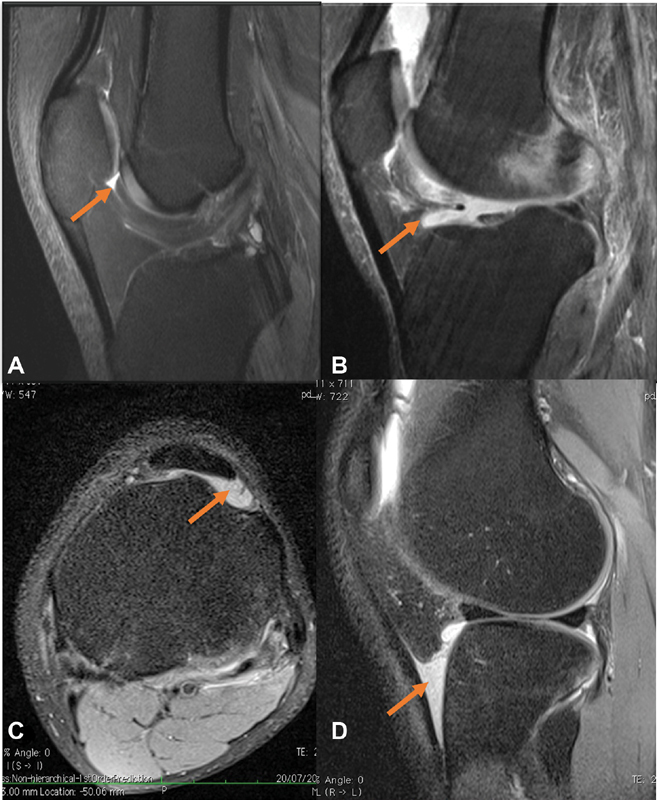
Fig. 14.
Displaced bony fragment in Hoffa's fat pad (HFP). Proton density fat-suppressed (PDFS) sagittal ( A ), PD sagittal ( B ), coronal PDFS ( C ), axial PDFS and ( D ) magnetic resonance (MR) images showing anterior intercondylar tibial eminence fracture with mild displacement of avulsed fracture fragment (orange arrow) and reactive edema (blue arrow) involving infrapatellar fat pad in a post-anterior cruciate ligament (ACL) reconstruction case.
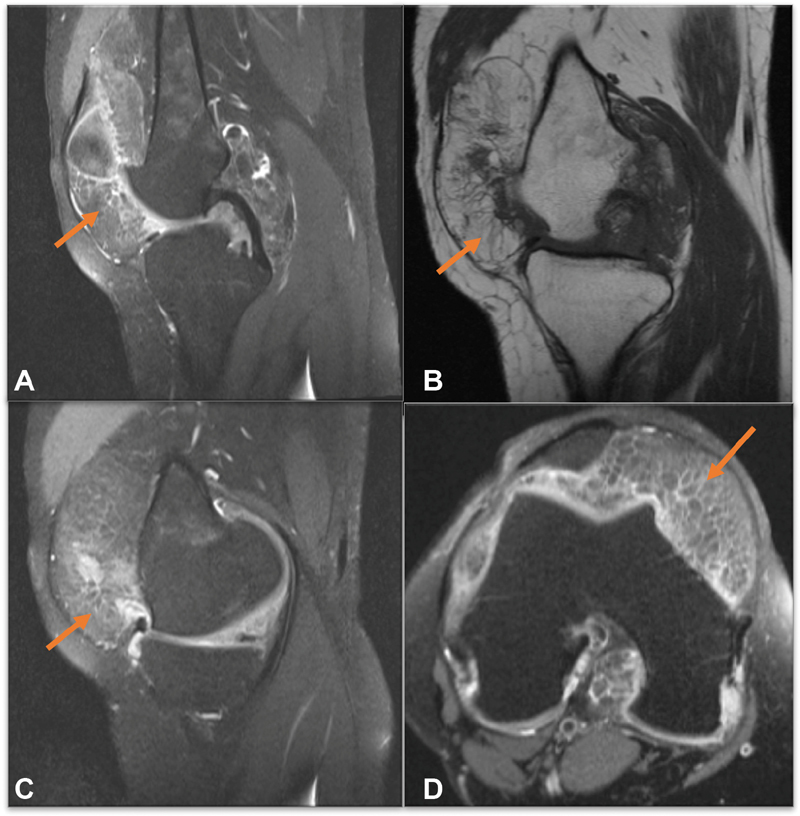
Fig. 13.
Loose body in Hoffa's fat pad (HFP). Proton density (PD) sagittal ( A ), PD fat-suppressed (PDFS) axial, ( B ) and sagittal PDFS images ( C ) reveal a well-defined hypointense loose body along the HFP. Incidentally noted, Baker's cyst along the posteromedial aspect of knee ( C ).
Osgood–Schlatter Disease
Osgood–Schlatter disease is conventionally seen in young patients (age 10–15 years). It is caused by repetitive friction created by gliding of the patellar tendon over immature apophysis of the tibial tubercle, resulting in microtrauma-induced changes in the form of swelling of cartilage, tibial tubercle fragmentation culminating into patellar tendon inflammation, and bursitis of superficial and tibial infrapatellar bursae, which may be associated with adjacent HFP edema. MRI helps in delineating the respective findings with soft-tissue swelling anterior to the tibial tuberosity, thickening, and edema of the inferior patellar tendon with subjacent bone marrow edema at the tibial tubercle with or without HFP edema and deep infrapatellar bursitis 2 12 ( Fig. 15 ).
Fig. 15.
Osgood–Schlatter disease with secondary Hoffa's fat pad (HFP) edema. A young boy with pain along the anterior knee joint, ( A ) sagittal proton density fat-suppressed (PDFS) and ( B ) PD magnetic resonance (MR) images reveal soft-tissue swelling anterior to the tibial tuberosity with loss of the sharp inferior angle of the HFP (orange arrow). There is thickening and edema of the inferior patellar tendon with bone marrow edema at the tibial tubercle. Sagittal computed tomography (CT) scan bone window ( C ) reveals focal cortical erosion of tibial apophysis (blue arrow).
Intrinsic Tumors
Lipomas and Fibrolipomas
Intra-articular or synovial lipomas are usually slow-growing and are considered rare along the knee joint. They usually have well-defined borders and fairly delineated fibrous capsules. The most common symptom is vague anterior knee pain, palpable swelling, and larger swellings that may limit the range of knee movements. Occasionally, severe pain has been reported in patients with strangulation of the lesion. Upon imaging, a lipoma follows fat signal intensity on all sequences ( Fig. 16 ), whereas fibrolipoma may have a variegated appearance, depending upon the fibrotic content. The treatment of fibrolipomas involves surgical excision along with their pseudocapsule. 13 It is important to differentiate lipomas from liposarcoma.
Fig. 16.
Lipoma in Hoffa's fat pad (HFP). Proton density fat-suppressed (PDFS) sagittal ( A ), axial ( B ), and PD sagittal magnetic resonance imaging (MRI) images ( C ) reveal a well-encapsulated fat intensity lesion in HFP.
The features favoring liposarcoma are larger size (which are usually more than 10 cm), a recent change in size or aggravation of symptoms in a previously known long-standing swelling, and heterogeneous signal intensity within the fat intensity lesion, possibly related to hemorrhage or associated soft-tissue component. Also, any lipomatous lesion located anywhere in the body with nonfatty components having prominent thickened septa > 2 mm and the presence of nodular to globular foci that may be associated with contrast enhancement are considered to be well-differentiated liposarcoma. The imaging differentials of fibrolipomas include synovial osteochondroma, synovial sarcoma, and para-articular chondroma 14 due to their variegated appearance. Correlation with radiographs or computed tomography (CT) scans can show the calcification or ossification in these lesions and aid differentiation.
Extrinsic Lesions
A myriad synovial pathologies involve HFP, ranging from pigmented villonodular synovitis (PVNS) and synovial osteochondromatosis to rarely synovial sarcomas.
Pigmented Villonodular Synovitis
PVNS is most commonly seen around the knee joint. Many theories have been postulated, ranging from idiopathic inflammatory synovial hyperplasia to benign neoplastic pathogenesis; however, a precise etiology remains unclear. It can be diffuse involving the entire joint, which is more common or can be a focal periarticular proliferation of synovial tissue, with focal PVNS having a predilection for HFP. There is an extensive proliferation of synovial membrane in PVNS, which histopathologically mimics giant cell tumor of the tendon sheath and is characterized by deposits of hemosiderin and fibrous stroma with infiltration by histiocytes and giant cells. 15
The patient may present with symptoms of joint locking in cases of focal synovitis, and in diffuse forms, the patients present with a history of recurrent joint swellings, mechanical pain, and occasionally give the history of repeated joint aspirations which are serosanguinous. Radiographs may demonstrate articular erosions in diffuse long-standing cases with fullness along the suprapatellar recess. MRI is considered as a superlative diagnostic modality with hypointense, thickened synovium in all sequences, primarily due to the paramagnetic effect of hemosiderin. There are susceptibility/blooming artifacts due to the same and a spectrum of synovitis, synovial thickening, and effusion coexist in these patients. Radiographs or CT scans aid in differentiating calcification from hemosiderin, as both show “blooming” on GRE images. The fluid suppression sequences help document bone marrow edema and erosions. 16 Differential considerations of synovial sarcoma, 17 hemosiderotic synovitis, hemophilic arthropathies, and rarely malignant fibrous histiocytoma must be considered. 18
Localized Nodular Synovitis
Localized nodular synovitis, also termed as “synovial giant cell tumor,” is a benign synovial proliferative lesion, most commonly presenting in the infrapatellar fat pad. Intra-articular localized nodular synovitis has a variable MR imaging appearance. Typically, it is presented as a well-defined, small ovoid lesion or as a large multilobulated soft-tissue mass with iso- or hyperintense signal intensity relative to skeletal muscles on T1-weighted images and variable signal intensity on T2-weighted images. Intrinsic circular hypointense areas may be present related to the high-hemosiderin concentration. An internal cleft-like hyperintense signal on T2-weighted images has been reported within the lesion, possibly related to tissue necrosis. MRI features that help distinguish localized nodular synovitis from PVNS include the appearance of a smooth surface (compared with diffuse frond-like projections of PVNS), the involvement of a small region of synovium, smaller hemosiderin deposition, and the absence of a hemorrhagic joint effusion ( Fig. 17 ). They show different growth patterns: PVNS tends to constrict the joint as it enlarges, whereas localized nodular synovitis tends to grow outward, becoming pedunculated. The torsed peduncle of localized nodular synovitis may present as acute knee pain. 19
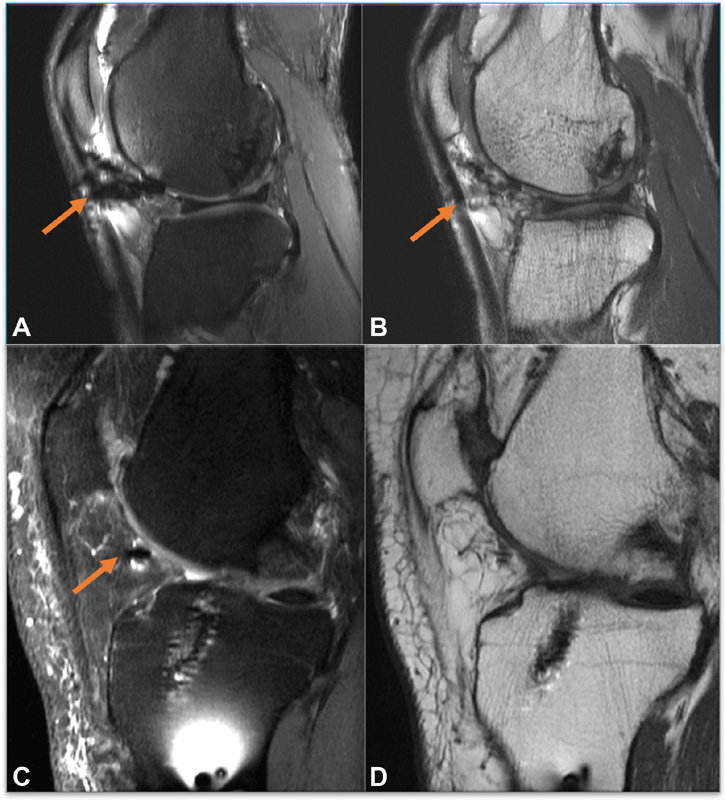
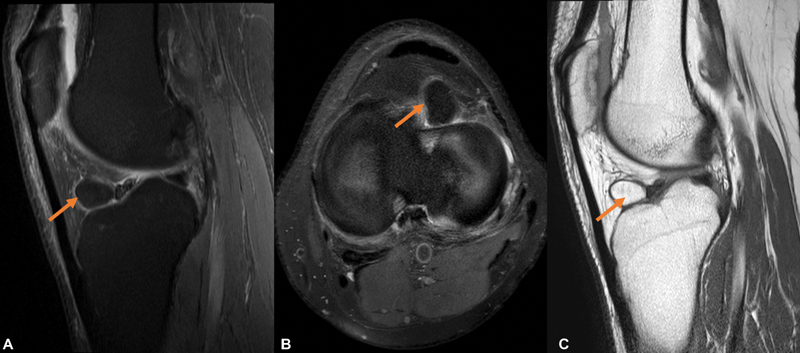
Fig. 17.
Localized nodular synovitis. A 26-year-old male complaining of anterior knee pain, proton density fat-suppressed (PDFS) sagittal images ( A ), PD sagittal ( B ) and PDFS axial magnetic resonance imaging (MRI) images reveals intermediate signal intensity focal mass with adjacent inflammatory fat stranding in Hoffa's fat pad (HFP). It is a localized variant of pigmented villonodular synovitis (PVNS) but may lack typical “black” signal from hemosiderin.
Various differential diagnoses of heterogeneous nodular mass in the infrapatellar fat pad include chronic Hoffa's disease, chondroma or osteochondroma of HFP (lacks hemosiderin), tophus from gout, and focal arthrofibrosis.
Synovial Hemangioma
It is a vascular malformation of the synovium, is benign, and commonly occurs in children and in earlier decades, that is, the first and second decades of life. Patients present with recurrent joint swelling and pain, restricted range of motion, and tenderness. On aspiration, hemarthrosis is commonly encountered. It has a predilection for HFP. 20 Radiographs may demonstrate soft-tissue opacity and joint effusions, osteopenia secondary to recurrent hemarthrosis, and uncommonly periosteal reaction. CT scan and radiographs may also demonstrate the presence of phleboliths. USG may be used to demonstrate intrinsic vascularity in the lesion. MRI best depicts the extent of the lesion. It presents as a poorly defined lobulated mass lesion with intermediate signal on T1WI and markedly hyperintense on T2W/PDFS images. Phleboliths are relatively uncommon in synovial hemangioma and are seen as small foci of blooming on GRE. Other features identified within the lesion include T1 hyperintense intralesional fat, linear T2 hypointense fibrotic bands, serpiginous vessels of fluid signal intensity or flow voids due to vascular channels ( Fig. 18 ). Postcontrast MRI images reveal intense enhancement of the lesion. 21
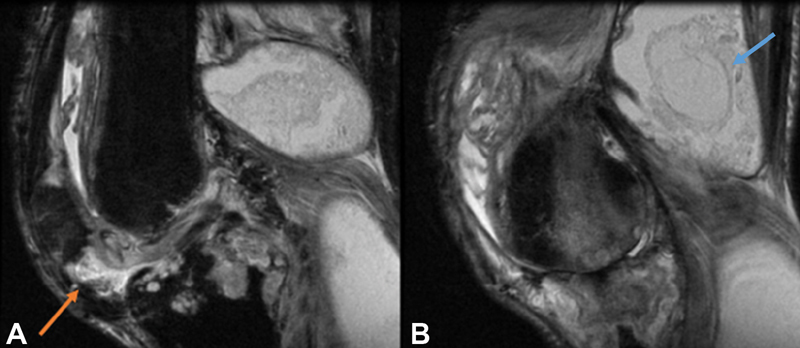
Fig. 18.
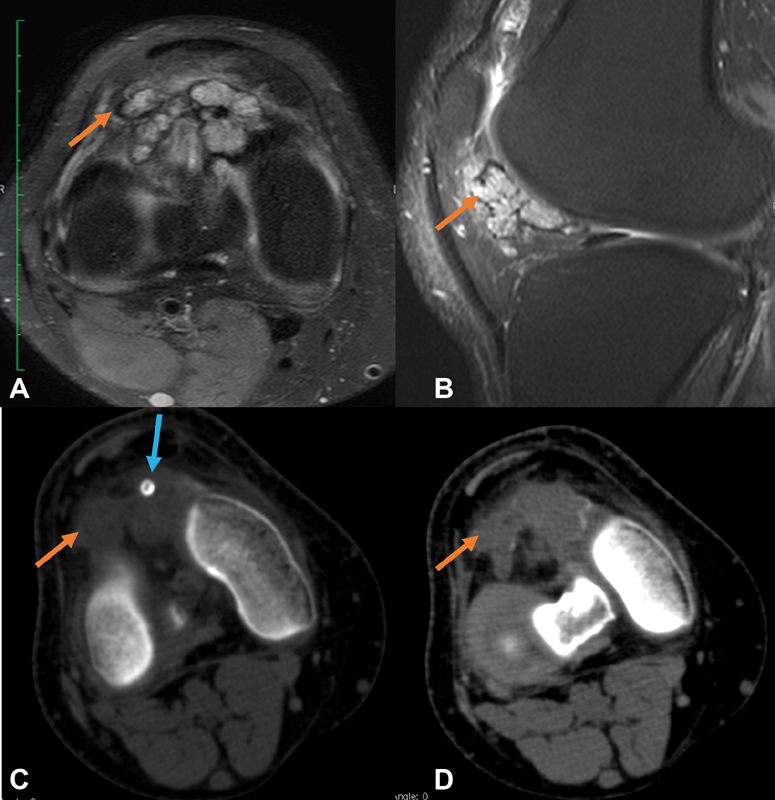
Hemangiolipoma of Hoffa's fat pad (HFP). Proton density fat suppressed (PDFS) axial ( A ) and sagittal ( B ) images reveal lobulated hyperintense lesion with hemosiderin rim and small flow voids within. Computed tomography (CT) scan axial images ( C and D ) shows evidence of ill-defined isodense lesion intermixed with fat density along HFP. A phlebolith is also seen with a central lucency within that clinches the diagnosis (blue arrow).
Hemangioma is the most common soft-tissue mass lesion of HFP in children and adolescents and should be suspected in children with nonspecific symptoms and long-standing knee pain. Differential considerations include hemosiderotic synovitis (secondary to trauma or hemophilia), hemophilic arthropathies, and PVNS. Hemosiderin deposition can also be seen in rheumatoid arthritis. GRE images classically show “blooming” along the synovial lining with diffuse T2 hypointensities in these cases due to hemosiderin residues, whereas the synovial hemangiomas show phleboliths as well-defined foci of blooming or vascular flow voids within.
Synovial Osteochondromatosis
It is another idiopathic condition that is characterized by metaplastic alterations of the synovial membrane, which results in the formation of multiple osseous and chondroid loose bodies. It can be classified into primary or secondary type. Primary synovial chondromatosis is commonly seen in middle-aged individuals, whereas secondary synovial chondromatosis occurs mostly in elderly people due to the enlargement of the detached articular cartilage or osteophyte fragments in patients with underlying joint diseases, most commonly with degenerative osteoarthritis. Standard radiographs can depict multiple similar-sized intra-articular calcifications diffusely distributed throughout the joint with typical “ring and arc” internal chondroid matrix mineralization. MRI shows a variable appearance depending on the degree of mineralization. Most commonly, it depicts intermediate- to high-signal intensity proliferative synovium involving suprapatellar pouch and/or popliteal fossa with multiple T2 hypointense calcified bodies. Focal adjacent bony erosions are commonly encountered. 22 ( Fig. 19 ). Enhancement may be helpful to differentiate T2 hyperintense uncalcified cartilage nodules from synovial fluid. 23 The former typically shows a peripheral and septal pattern of enhancement as commonly observed in hyaline cartilage neoplasms.
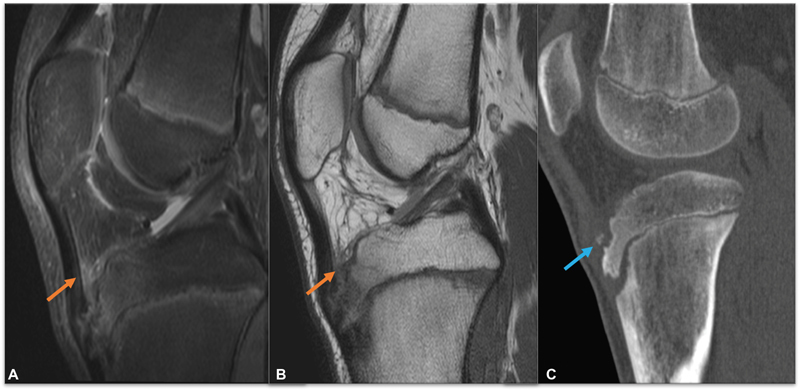
Fig. 19.
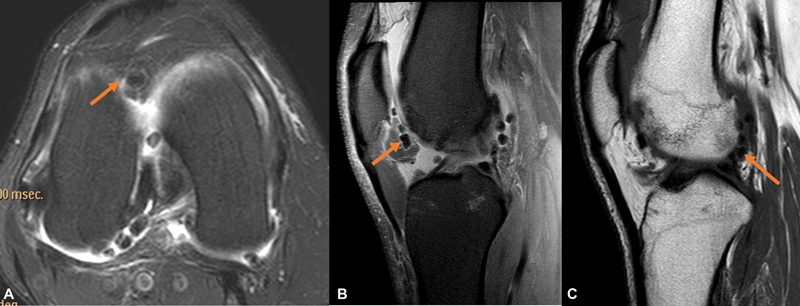
Synovial osteochondromatosis in Hoffa's fat pad (HFP). A middle-aged female with chronic knee pain. Proton density fat-suppressed (PDFS) axial ( A ) and sagittal images ( B ) and sagittal T1 magnetic resonance (MR) images reveal multiple loose bodies in HFP extending posterior to the knee joint with associated moderate joint effusion and mild synovial inflammatory changes.
Secondary synovial osteochondromatosis can be differentiated by the presence of the underlying articular disease and fewer chondral bodies of varying shapes and sizes. HFP involvement in the form of ossification is rare and comprises a list of differential diagnoses including crystal deposition arthropathies, para-articular osteochondroma, synovial sarcoma, myositis ossificans and, rarely, extraskeletal osteosarcoma and chondrosarcomas. 24
Synovial chondrosarcoma is a rare event associated with primary or secondary synovial chondromatosis. MRI imaging features may be overlapping with both entities having similar imaging findings, including diffuse synovial proliferation, cartilaginous nodules, and masses invading adjacent structures. 7 It can be difficult to differentiate recurrent disease from malignant transformation as an extension into the adjacent soft-tissue and deep bone erosions may be present in both entities. However, the presence of true cortical and permeative destruction and bone marrow invasion, which are better delineated on T1 weighted images, can be considered as a sign of malignancy. Features that should raise the suspicion of malignant transformation include a rapid increase in the size of the lesion in a known case of primary synovial osteochondromatosis or a rapidly deteriorating clinical course and should prompt biopsy evaluation.
Synovial Sarcoma
Intra-articular synovial sarcomas are rare and most of the cases have been documented along the knee joint. Fat pad calcification is noted in 30% of cases and its presence on initial radiographic examination may help to suspect a tumoral pathology and consider a possibility of malignant etiology. MRI aids in the accurate depiction of size, extension, and adjacent invasion and acts as a road map for surgical planning. The lesions are multilobulated, can be septated, and show variable T2 hyperintensity. In lesions > 5 cm in size, “triple signal intensity” has been described with a “bowl of grapes” appearance of intermixed iso, hypo, and hyperintense areas ( Fig. 20 ). Postcontrast T1WI may aid in delineating benign versus malignant nature, depending upon the degree of enhancement. 7 17 The possibility of synovial sarcoma should be considered in the presence of a juxta-articular soft-tissue mass in an adolescent with calcification or ossification. Differential considerations would be of pigmented villonodular synovitis, extraskeletal chondrosarcoma, synovial osteochondroma, or para-articular chondroma.
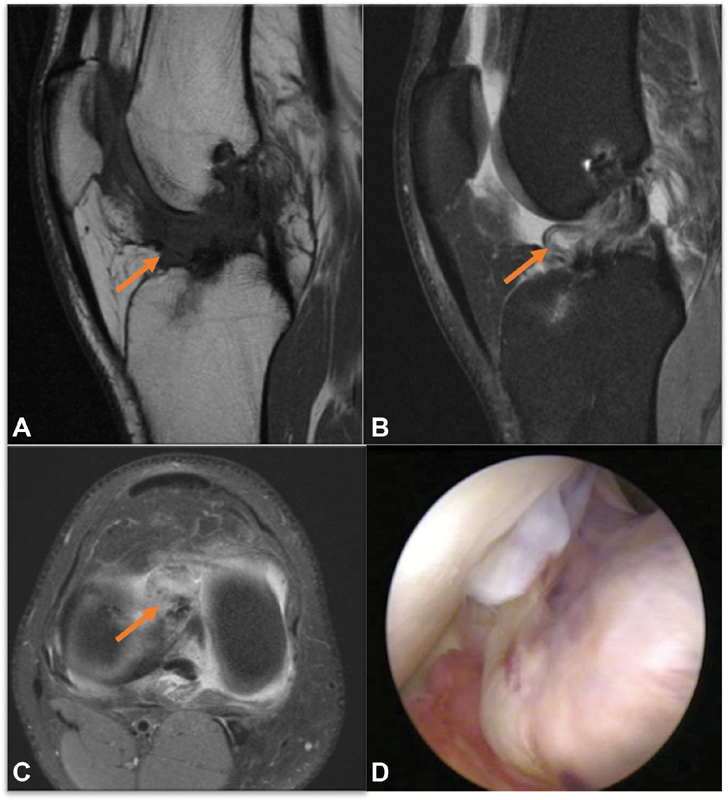
Fig. 20.
Synovial sarcoma involving Hoffa's fat pad (HFP). T1 sagittal images ( A ), proton density fat-suppressed (PDFS) axial ( B ) and PD axial images ( C ) reveals lobulated confluent T1 hypointense, T2 hyperintense altered signal intensity lesions along the suprapatellar recess, anterior and posterior joint recesses and extending along HFP (with encasement of intra-articular ligaments).
Para-articular Chondroma or Osteochondroma
Three variants of extraskeletal chondroma are recognized, namely, soft-tissue chondroma, synovial chondromatosis (see above), and para-articular osteochondroma. Para-articular or intracapsular chondroma arise from the joint capsule and/or connective tissue adjacent to the capsule due to cartilaginous metaplasia. The term para-articular osteochondroma is used when this chondral metaplasia progresses to ossification. It is postulated that repetitive and chronic trauma triggers a cycle of inflammation, fibrosis, and hemorrhage which is gradually replaced by further hemosiderin and an increase in fibrosis. In a few cases, fibrocartilaginous metaplasia may lead to ossification along the HFP as in the case of chronic Hoffa's disease. 25 26 It causes obliteration of normal fat of HFP with varying degrees of mineralization ranging from a few calcific specks to large ossifying masses. Chondromas show T2 hyperintense signals with varying degrees of heterogeneity related to mineralization. Para-articular osteochondroma of HFP ( Fig. 21 ) presents as a large central or less commonly eccentric, predominantly intra-articular, lobulated ossified mass lesion, causing capsular distension and may be associated with the erosion of the inferior pole of the patella or anterosuperior tibial cortex. Contrast administration shows the peripheral enhancement of the cartilage lobules. Imaging differential diagnosis of a para-articular chondroma in HFP would be of synovial sarcoma. Osteochondroma can be readily differentiated from the more anteriorly located patellar tendon ossification.
Fig. 21.
Osteochondroma in Hoffa's Fat pad (HFP). Magnetic resonance imaging (MRI) proton density fat-suppressed (PDFS) sagittal ( A ) T1WS sagittal ( B ), computed tomography (CT) scan (sagittal), PDFS axial ( D ) images, and PD axial ( E ) MR images reveal a large predominantly intraarticular lobulated mass lesion involving HFP with the erosion of the inferior aspect of patella and the anterosuperior aspect of the upper end of tibia. CT scan ( F ) reveals dense ossification along the HFP.
Lipoma Arborescence
It is a rare condition, commonly involving the knee joint. Lipoma arborescens is nearly always associated with underlying degenerative joint disease, chronic rheumatoid arthritis, or prior trauma. It is characterized by diffuse villous proliferation of the synovium which is histopathologically characterized by the replacement of subsynovial tissue. It usually affects the knee joint; however, few cases have been reported around the hip, elbow, and shoulder joints. Patients usually present with one or more of the following symptoms including pain, a gradual increase in swelling with limited range of motion, and locking. 27
MRI is the diagnostic imaging modality of choice and can demonstrate the entire spectrum with classical imaging pattern, showing a large “frond-like mass” arising from the synovium following fat signal intensity on all sequences. It may show mixed signal intensities. The presence of fat intensity and absence of susceptibility artifacts helps in differentiating it from pigmented villonodular synovitis and synovial osteochondromatosis 28 29 ( Fig. 22 ). Other differential considerations for long-standing chronic joint swellings showing fat intensity within include intra-articular or synovial lipoma, liposarcoma, and synovial hemangiolipoma.
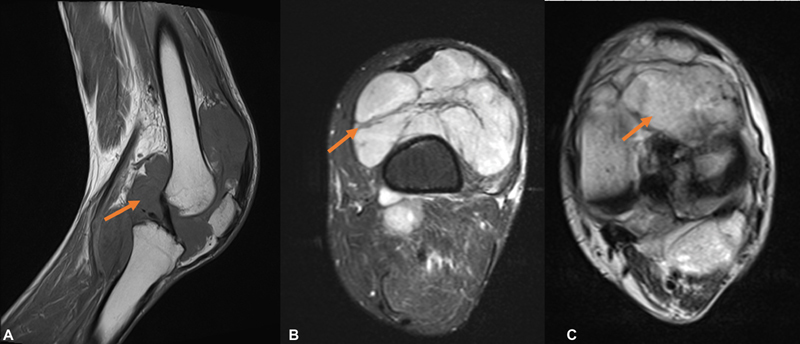
Fig. 22.
Lipoma arborescence involving the Hoffa's fat pad (HFP). A middle-aged male with long-standing painless knee swelling. Proton density fat-suppressed (PDFS) sagittal images ( A and C ), PD sagittal ( B ) images, and PDFS axial ( D ) Magnetic resonance (MR) images reveal frond-like proliferations showing fat intensity with coexisting joint effusion and inflammatory edematous changes involving suprapatellar bursa and infrapatellar fat pad.
Nonspecific Synovial Proliferative Pathologies and Joint Effusions
A diverse group of synovial proliferative pathologies may extrinsically involve infrapatellar pad fat which primarily affects the joint. This includes a wide differential list of seronegative arthritis, rheumatoid arthritis, gouty arthritis, infective arthritis including septic and tubercular etiology, as well as degenerative primary osteoarthritis. Contrast-enhanced MRI helps in delineating the true extent of synovial proliferation from the joint fluid. However, an extensive history, multiple joint involvements, array of biochemical tests, and occasionally synovial biopsy is needed for final confirmation. Joint effusions may insinuate along the various recesses around the HFP and can replicate synovial pathologies and HFP edema 2 ( Figs. 23 and 24 ).
Fig. 23.
Septic arthritis with secondary Hoffa's pad fat (HFP) involvement. Proton density fat-suppressed (PDFS) sagittal images ( A and B ) reveal mild synovial effusion with abnormal marrow edema and subchondral erosions. Irregular contour of the HFP is seen with synovial inflammatory changes (orange arrow). A large loculated collection is seen in the popliteal fossa consistent with abscess (blue arrow).
Fig. 24.
Joint fluid along synovial recesses in three different cases. Proton density fat-suppressed (PDFS) sagittal ( A, B , and D ) and axial ( C ) images ( A —case 1, B—case 2, and C and D —case 3) reveals minimal fluid in supra-Hoffitic recess in ( A ), mild joint fluid with synovial inflammatory changes ( B ), and distension of infra-Hoffitic recess—infrapatellar bursitis ( C and D ).
Miscellaneous Lesions
Other rare differential diagnosis of HFP masses reported in the literature include glomus tumors and schwannoma. The glomus tumor shows typical features of T1 low to intermediate and T2WI/PDFS hyperintense signal with characteristic intense postcontrast enhancement. Histopathological evidence of glomus cells, smooth muscles, and vascular channels with positive immunohistochemistry (IHC) tests for myosin, vimentin, and desmin is confirmatory. 30 31 A case of HPF schwannoma reported in the literature presented as a well-circumscribed, well-encapsulated, and solitary heterogeneously hyperintense lesions on IHC findings of S100 and CD34 32 . Tumoral calcinosis associated with chronic renal disease may also present as periarticular soft tissue in the HFP. 33
Conclusion
Cross-sectional imaging including CT and MRI are the ultimate problem solver tools in cases with anterior knee pain, attributed to a spectrum of pathologies affecting the infrapatellar fat pad of Hoffa. As their imaging appearances are varied and distinctive and the list of differentials is exhaustive, an algorithmic-based approach helps the radiologist to identify the abnormalities, thereby enabling the clinician to provide necessary and appropriate care based on the correct diagnosis ( Fig. 25 ).
Fig. 25.
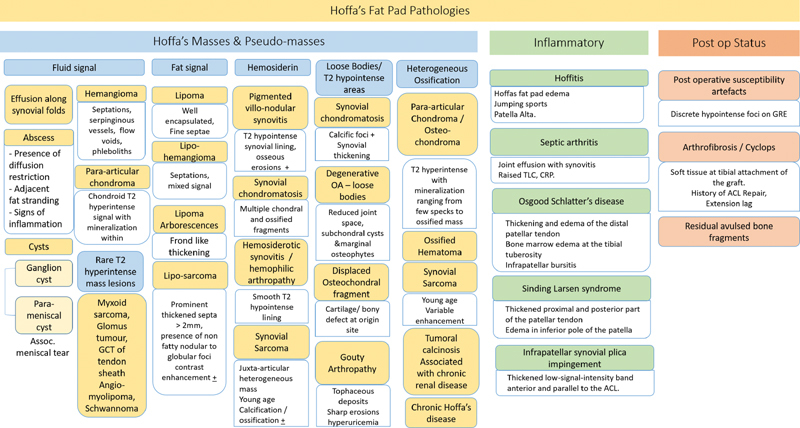
Diagnostic algorithm for Hoffa's fat pad (HFP) pathologies.
Conflict of Interest None declared.
Financial Support and Sponsorship
Nil.
References
- 1.Jacobson J A, Lenchik L, Ruhoy M K, Schweitzer M E, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997;17(03):675–691. doi: 10.1148/radiographics.17.3.9153705. [DOI] [PubMed] [Google Scholar]
- 2.Draghi F, Ferrozzi G, Urciuoli L, Bortolotto C, Bianchi S. Hoffa's fat pad abnormalities, knee pain and magnetic resonance imaging in daily practice. Insights Imaging. 2016;7(03):373–383. doi: 10.1007/s13244-016-0483-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orita S, Koshi T, Mitsuka T et al. Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord. 2011;12:144. doi: 10.1186/1471-2474-12-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conde J, Scotece M, López V et al. Differential expression of adipokines in infrapatellar fat pad (IPFP) and synovium of osteoarthritis patients and healthy individuals. Ann Rheum Dis. 2014;73(03):631–633. doi: 10.1136/annrheumdis-2013-204189. [DOI] [PubMed] [Google Scholar]
- 5.Klein-Wieringa I R, Kloppenburg M, Bastiaansen-Jenniskens Y M et al. The infrapatellar fat pad of patients with osteoarthritis has an inflammatory phenotype. Ann Rheum Dis. 2011;70(05):851–857. doi: 10.1136/ard.2010.140046. [DOI] [PubMed] [Google Scholar]
- 6.Wickham M Q, Erickson G R, Gimble J M, Vail T P, Guilak F. Multipotent stromal cells derived from the infrapatellar fat pad of the knee. Clin Orthop Relat Res. 2003;(412):196–212. doi: 10.1097/01.blo.0000072467.53786.ca. [DOI] [PubMed] [Google Scholar]
- 7.Helpert C, Davies A M, Evans N, Grimer R J. Differential diagnosis of tumours and tumour-like lesions of the infrapatellar (Hoffa's) fat pad: pictorial review with an emphasis on MR imaging. Eur Radiol. 2004;14(12):2337–2346. doi: 10.1007/s00330-004-2491-1. [DOI] [PubMed] [Google Scholar]
- 8.Larbi A, Cyteval C, Hamoui M et al. Hoffa's disease: a report on 5 cases. Diagn Interv Imaging. 2014;95(11):1079–1084. doi: 10.1016/j.diii.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Bradley D M, Bergman A G, Dillingham M F. MR imaging of cyclops lesions. AJR Am J Roentgenol. 2000;174(03):719–726. doi: 10.2214/ajr.174.3.1740719. [DOI] [PubMed] [Google Scholar]
- 10.Abreu M R, Chung C B, Trudell D, Resnick D. Hoffa's fat pad injuries and their relationship with anterior cruciate ligament tears: new observations based on MR imaging in patients and MR imaging and anatomic correlation in cadavers. Skeletal Radiol. 2008;37(04):301–306. doi: 10.1007/s00256-007-0427-y. [DOI] [PubMed] [Google Scholar]
- 11.Marra M D, Crema M D, Chung M et al. MRI features of cystic lesions around the knee. Knee. 2008;15(06):423–438. doi: 10.1016/j.knee.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Saddik D, McNally E G, Richardson M. MRI of Hoffa's fat pad. Skeletal Radiol. 2004;33(08):433–444. doi: 10.1007/s00256-003-0724-z. [DOI] [PubMed] [Google Scholar]
- 13.Sezgin E A, Atik OŞ. Tumors and tumor-like lesions of infrapatellar fat pad and surrounding tissues: A review of the literature. Eklem Hastalik Cerrahisi. 2018;29(01):58–62. doi: 10.5606/ehc.2018.002. [DOI] [PubMed] [Google Scholar]
- 14.Gigis I, Gigis P. Fibrolipoma with osseous and cartilaginous metaplasia of hoffa's fat pad: a case report. Case Rep Orthop. 2012;2012:547963. doi: 10.1155/2012/547963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dorwart R H, Genant H K, Johnston W H, Morris J M. Pigmented villonodular synovitis of synovial joints: clinical, pathologic, and radiologic features. AJR Am J Roentgenol. 1984;143(04):877–885. doi: 10.2214/ajr.143.4.877. [DOI] [PubMed] [Google Scholar]
- 16.Larbi A, Viala P, Cyteval Cet al. Imaging of tumors and tumor-like lesions of the knee Diagn Interv Imaging 201697(7-8):767–777. [DOI] [PubMed] [Google Scholar]
- 17.Albergo J I, Gaston C L, Davies M et al. Hoffa's fat pad tumours: what do we know about them? Int Orthop. 2013;37(11):2225–2229. doi: 10.1007/s00264-013-2041-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu L, Gao J, Wang C. Localized tenosynovial giant cell tumor in the infrapatellar fat pad: a very rare location. Int J Clin Exp Med. 2016;9(07):14453–14456. [Google Scholar]
- 19.Huang G S, Lee C H, Chan W P, Chen C Y, Yu J S, Resnick D. Localized nodular synovitis of the knee: MR imaging appearance and clinical correlates in 21 patients. AJR Am J Roentgenol. 2003;181(02):539–543. doi: 10.2214/ajr.181.2.1810539. [DOI] [PubMed] [Google Scholar]
- 20.Choudhari P, Ajmera A. Haemangioma of knee joint: a case report. Malays Orthop J. 2014;8(02):43–45. doi: 10.5704/MOJ.1407.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maheshwari S, Chatterjee S, Rajesh U, Khandelwal P V. A case report of synovial hemangioma: a rare cause of opacity in Hoffa's fat pad. Indian J Musculoskelet Radiol. 2019;1:127–130. [Google Scholar]
- 22.Narváez J A, Narváez J, Aguilera C, De Lama E, Portabella F. MR imaging of synovial tumors and tumor-like lesions. Eur Radiol. 2001;11(12):2549–2560. doi: 10.1007/s003300000759. [DOI] [PubMed] [Google Scholar]
- 23.Lee D H, Jeong T W. Uncommon primary synovial chondromatosis involving only the infrapatellar fat pad in an elderly patient. Knee Surg Relat Res. 2016;28(01):79–82. doi: 10.5792/ksrr.2016.28.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oshigiri T, Watanabe K, Otsubo H et al. Arthroscopic resection of multiple ossifying tumors in the infrapatellar fat pad. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(01):43. doi: 10.1186/1758-2555-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hashimoto K, Nishimura S, Yamagishi K et al. Extra-articular synovial osteochondroma of the Hoffa's fat pad involving the patellar tendon: A case report and literature review. Mol Clin Oncol. 2020;12(04):355–357. doi: 10.3892/mco.2020.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eymard F, Chevalier X. Inflammation of the infrapatellar fat pad. Joint Bone Spine. 2016;83(04):389–393. doi: 10.1016/j.jbspin.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 27.De Vleeschhouwer M, Van Den Steen E, Vanderstraeten G, Huysse W, De Neve J, Vanden Bossche L. Lipoma arborescens: review of an uncommon cause for swelling of the knee. Case Reports in Orthopedics. 2016;2016:9.538075E6. doi: 10.1155/2016/9538075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsifountoudis I, Kapoutsis D, Tzavellas A-N, Kalaitzoglou I, Tsikes A, Gkouvas G. Lipoma arborescens of the knee: report of three cases and review of the literature. Case Rep Med. 2017;2017:3.569512E6. doi: 10.1155/2017/3569512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphey M D, Arcara L K, Fanburg-Smith J. From the archives of the AFIP: imaging of musculoskeletal liposarcoma with radiologic-pathologic correlation. Radiographics. 2005;25(05):1371–1395. doi: 10.1148/rg.255055106. [DOI] [PubMed] [Google Scholar]
- 30.Hustings N, Vanhoenacker F, De Backer A. Glomangiomyoma of the knee: a rare juxtasynovial presentation: juxtasynovial glomangiomyoma in the joint capsule is a rare location for glomus tumors that should be considered in the differential diagnosis of hypervascular synovial-based tumors. J Belg Soc Radiol. 2020;104(01):12. doi: 10.5334/jbsr.2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prabhakar S, Dhillon M S, Vasishtha R K, Bali K. Glomus tumor of Hoffa's fat pad and its management by arthroscopic excision. Clin Orthop Surg. 2013;5(04):334–337. doi: 10.4055/cios.2013.5.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caballero Martel J R, Estévez Sarmiento S. Schwannoma: a rare Hoffa's fat pad tumor. Surg J (N Y) 2019;5(02):e62–e64. doi: 10.1055/s-0039-1692996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Narváez J A, Narváez J, Ortega R, De Lama E, Roca Y, Vidal N. Hypointense synovial lesions on T2-weighted images: differential diagnosis with pathologic correlation. AJR Am J Roentgenol. 2003;181(03):761–769. doi: 10.2214/ajr.181.3.1810761. [DOI] [PubMed] [Google Scholar]