Abstract
Background
Herbal medicine is widely used for the treatment of functional dyspepsia (FD) in East Asian countries. We aimed to analyze the prescription patterns of herbal medicine for patients with FD in Korean medicine clinical settings through the analysis of national health insurance claims data over the past 10 years and to check how herbal medicine has been used for FD within the scope of national health insurance.
Methods
All prescription data claimed to the Health Insurance Review and Assessment Service with the diagnosis of FD and herbal medicine prescriptions in 2010–2019 were reviewed. We estimated the demographics, clinical characteristics, and annual prescription amount and cost of each herbal medicine. Frequent comorbidities of FD were investigated by analyzing the frequency of the Korean standard classification of diseases codes used together with FD.
Results
In total, 19,388,248 herbal medicine prescriptions were identified. Herbal medicine prescriptions were mostly claimed by women, the elderly, outpatients at Korean medicine clinics, and national health insurance; the number increased every year. The most frequently prescribed herbal medicine was Pingwei-san (Pyeongwi-san) (31.12%), followed by Xiangshapingwei-san (Hyangsapyeongwi-san) (23.20%), Qiongxia-tang (Gungha-tang) (6.31%), and Banxiaxiexin-tang (Banhasasim-tang) (6.25%). The total cost of herbal medicine prescriptions increased every year, and it was highest for Xiangshapingwei-san (Hyangsapyeongwi-san) (19.37%), followed by Banxiaxiexin-tang (Banhasasim-tang) (17.50%) and then Pingwei-san (Pyeongwi-san) (15.63%). Musculoskeletal and connective tissue diseases including low back pain and myalgia were the commonest comorbidities associated with FD.
Conclusion
This is the first study to investigate the disease burden and actual prescription pattern of herbal medicine for FD using claim data. Future clinical research and related healthcare policies should be established based on our study.
1. Introduction
Functional dyspepsia (FD) comprises troublesome upper gastrointestinal chronic symptoms, including early satiety, postprandial fullness, and epigastric pain or burning sensation [1]. The pathophysiology of FD has not been clearly elucidated and FD has a worldwide prevalence of 5–11% [2, 3]. Although not directly life-threatening, FD can significantly impair quality of life and work productivity [4, 5]. Therefore, FD is extremely important in terms of socioeconomic and national burdens.
In Western medicine, FD involves the administration of various therapeutic agents, either individually or in combination, to alleviate symptoms, but this has limited effectiveness due to the chronicity and variable severity of FD [6, 7]. Thus, there is increasing interest in complementary and integrative medicine such as herbal medicines, which have multicomponent and multitarget characteristics [8]. In particular, statistical data of the Health Insurance Review and Assessment Service (HIRA) in the Republic of Korea indicate that FD ranked 8th among the causes of outpatient consultations at Korean medical institutions in 2020 [9], which indicates that many patients receive traditional Korean medical treatments—such as herbal medicine—for FD. The HIRA, a public institution established in July 2000 in the Republic of Korea, conducts healthcare cost–benefit reviews and adequacy assessments. All citizens of the Republic of Korea are legally obligated to subscribe to National Health Insurance (NHI), and all health insurance claims are reviewed by HIRA. For academic research purposes, the HIRA Health and Medical Big Data Center provides deidentified customized medical care claims data that comprises general prescription details (including patient information such as sex, age, and insurance type and medical information such as disease code, medical institution type, and cost), medical treatment details (including examination, treatment, surgery, and in-hospital dispensing details), diagnosis, and outpatient prescription details. These data are crucial for comprehensively understanding the current status of medical treatments and trends in the Republic of Korea's pharmaceutical market. Recent research using healthcare big data, such as health insurance claims data, has increased. The accessibility and utilization of these data are currently high, thus contributing greatly to policymaking and evidence generation in healthcare [10].
Investigating potential herbal medicines for the treatment of FD, conducting clinical research, and establishing relevant healthcare policies require investigating the current treatment patterns and associated economic burden in actual clinical practice. Such research can lead to the acquisition of relevant political support such as the expansion of NHI coverage and investment in the herbal medicine industry. However, to the best of our knowledge, no study has investigated prescription patterns of herbal medicine for the treatment of FD in a real-world clinical setting. Therefore, this study was conducted with the aim of analyzing the prescription patterns of herbal medicine for FD patients in the Republic of Korea through the analysis of health insurance claims data over the past 10 years to identify evidence that can support healthcare decision-making and policy changes.
2. Materials and Methods
2.1. Data Sources and Research Ethics
This study analyzed big data on health and medical care from HIRA that are anonymized, through the extraction, summarization, and processing of NHI data that are collected, retained, and managed by HIRA to prevent subject identification while facilitating academic research. Our application requesting the use of big data analysis through HIRA's Healthcare Big Data Hub (https://opendata.hira.or.kr/home.do) was reviewed and approved by the Public Data Provision Deliberation Committee of HIRA, and data for analysis that were suitable for research purposes were provided through the remote analysis system (Assigned number: HIRA research data (M20201020802)). The study protocol was exempted from ethical review by the institutional review board of the Korea Institute of Oriental Medicine (I-2010/008-005).
2.2. Study Population
We identified all claims data containing a diagnosis of FD (Korean Standard Classification of Disease [KCD] code: K30 in the primary or first secondary diagnosis, determined with reference to the “Korean Medicine Clinical Practice Guideline for FD”) [11] and herbal medicine prescriptions from Korean medical institutions from January 2010–December 2019, regardless of the subjects' age, sex, episodic order, and types of Korean medical institution (clinic, hospital, and public health center). In the KCD, K30 means FD, which includes indigestion, epigastric pain syndrome, and postprandial distress syndrome and excludes heartburn (R12) and nervous (F45.3), neurotic (F45.3), psychogenic (F45.3), and not-otherwise-specified (R10.19) dyspepsia. Herbal medicine prescriptions were obtained by screening the data for 56 herbal formulas (mixed extracts) that are currently covered by the NHI in the Republic of Korea (Supplement 1).
2.3. Study Variables
We extracted data on patients' demographics and clinical characteristics including age and sex (per person) and type of medical institution, health insurance, hospital visit (inpatient or outpatient), herbal medicine prescription period, and cost (per prescription). Then, the annual prescription amount and cost of each of the 56 herbal medicines were analyzed. Furthermore, we investigated the frequent comorbidities associated with FD by analyzing the frequency of KCD codes—used together with the K30 code indicating FD—for each prescription.
2.4. Data Preprocessing and Analysis
The HIRA provides a data analysis environment through a virtualization server that is based on a preapproved media access control and network address and can be assessed with the SAS Enterprise Guide (SAS EG) analytical tool. Therefore, basic data preprocessing was conducted using SAS EG. For preanalytical processing, first, data on the subjects and their prescription keys with the K30 diagnosis code were obtained for the primary and the first secondary diagnoses. In the prescription table, herbal medicine prescriptions, prescription duration (in days), and prescription costs (in Korean won (₩KRW)) were extracted for each visit. Diagnostic codes registered for each patient's visit were extracted from the diagnosis history table. Frequent comorbidities were extracted and divided alphabetically according to the first letter among the KCD classification criteria. After refining the data set, clinical characteristics, herbal medicine prescriptions, and frequent comorbidities, their trends stratified by sex, age, and year were analyzed. When calculating the number of herbal medicine prescriptions, in cases with more than two herbal medicine prescriptions per visit, each individual prescription was counted as separate. Data such as sex, age, and type of health insurance were extracted based on the date of the subject's first visit during the observation period. We counted the subjects' clinical characteristics based on the patient. In addition, to extract information on the characteristics of prescriptions and comorbidities at the time of prescribing, we counted the events based on prescriptions per visit.
3. Results
3.1. Selection Process of Target Prescriptions
In total, 123,506,249 prescriptions (medications, procedures, etc.) included K30 in either the primary or first secondary diagnosis in Korean medical institutions. Among them, 19,428,028 prescriptions included herbal medicines. After excluding prescriptions of individual herbs, only the prescriptions that corresponded to the predefined 56 herbal formulas (mixed extracts) were selected for analysis. Finally, 19,388,248 herbal medicine prescriptions from 3,687,700 patients were included in the analysis.
3.2. Demographics and Clinical Characteristics
The study population comprising 3,687,700 FD patients—1,105,503 men (29.98%) and 2,582,197 women (70.02%)—showed a mean age (standard deviation) of 49.17 (22.02) years. Regarding the type of medical institution, Korean medical clinics issued most (n = 19,152,474 [98.58%]) of the 19,388,248 herbal medicine prescriptions issued during the study period. Stratification by the type of health insurance showed that the NHI covered most of the herbal medicine prescriptions (n = 18,539,775 [95.62%]). In addition, most hospital visits were made by outpatients (n = 19,341,996, 99.76%). The mean prescription period and cost were 1.68 days and approximately ₩1,880 KRW, respectively (Table 1).
Table 1.
Clinical characteristics of herbal medicine prescriptions.
| Clinical characteristics | N | % |
|---|---|---|
| Type of medical institution (including 39,780 duplicates) | ||
| Korean medical hospital | 269,427 | 1.39 |
| Korean medical clinic | 19,152,474 | 98.58 |
| Public health center | 6,127 | 0.03 |
| Type of health insurance | ||
| National health insurance | 18,539,775 | 95.62 |
| Medical aid | 848,473 | 4.38 |
| Type of administration | ||
| Inpatient | 46,252 | 0.24 |
| Outpatient | 19,341,996 | 99.76 |
| Prescription period (days) | ||
| Mean 1.68 | SD 1.75 | |
| Prescription cost (₩KRW)∗ | ||
| Mean 1,880.04 | SD 2,911.42 | |
KRW, Korean won; SD, standard deviation. ∗$1 USD ≒ ₩1,156.4 KRW (2019).
3.3. Number of Herbal Medicine Prescriptions for FD Stratified by Sex, Age, and Year
A sex-stratified comparison of the number of herbal medicine prescriptions showed that approximately three times more women (n = 14,414,514, 74.3%) than men (n = 4,973,734, 25.7%) received these prescriptions. Age-stratified analysis showed that the number of herbal medicine prescriptions tended to increase proportionally with age: patients in their 70s accounted for the most prescriptions (n = 6,745,042; 34.8%), followed by those in their 60s (n = 4,430,108; 22.8%); thus, subjects in their 60s and 70s accounted for more than half of all herbal medicine prescriptions (Figure 1). The total number of herbal medicine prescriptions steadily increased throughout the study period and, in particular, increased 5.5-fold from 2010 (n = 536,372) to 2019 (n = 2,914,167). A similar trend was observed in the age-stratified analyses; the upward trend was particularly evident in subjects aged 60 or older (Figure 2).
Figure 1.
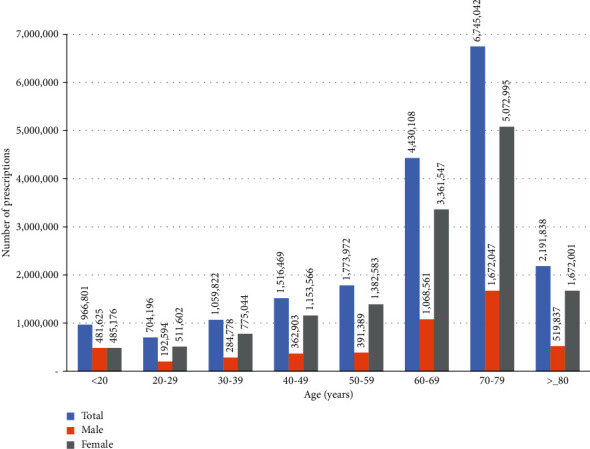
Number of herbal medicine prescriptions for functional dyspepsia based on sex- and age-stratified analyses.
Figure 2.
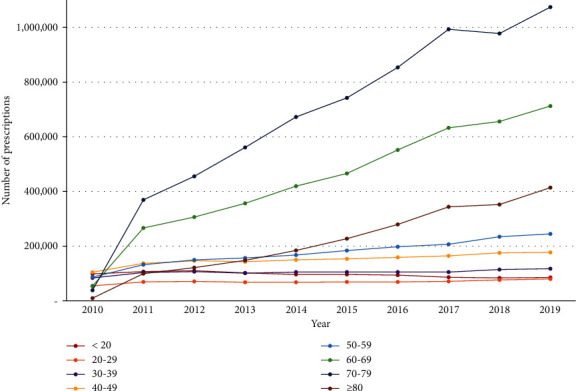
Number of herbal medicine prescriptions for functional dyspepsia based on the year.
3.4. Number and Cost of Frequently Prescribed Herbal Medicines for FD Based on the Year
According to the number of herbal medicine prescriptions for FD that were submitted in claims to the HIRA over 10 years, Pingwei-san (Pyeongwi-san) was the most prescribed medication, accounting for 31.12% (n = 6,033,229) of all prescriptions. Xiangshapingwei-san (Hyangsapyeongwi-san) was the second most prescribed agent (n = 4,497,837; 23.20%), followed by Qiongxia-tang (Gungha-tang; n = 1,222,565; 6.31%), Banxiaxiexin-tang (Banhasasim-tang; n = 1,210,996; 6.25%), and Erchen-tang (Yijin-tang; n = 1,169,238; 6.03%) (Figure 3). The year-wise comparison showed that Pingwei-san (Pyeongwi-san) was the most prescribed medicine across all years during the study period except 2010. The total cost of herbal medicine prescriptions was highest for Xiangshapingwei-san (Hyangsapyeongwi-san) at ₩7,051,079,037 KRW (19.37%), followed by Banxiaxiexin-tang (Banhasasim-tang; ₩6,370,364,917 KRW, 17.50%), Pingwei-san (Pyeongwi-san; ₩5,687,566,199 KRW, 15.63%), Neixiao-san (Naeso-san; 2,335, ₩428,678 KRW, 6.42%), and Buzhongyiqi-tang (Bojungikgi-tang; ₩1,905,819,409 KRW, 5.24%) (Figure 4). The total cost of 56 herbal medicine prescriptions for the treatment of FD during the 10-year study period was ₩36,399,342,776 KRW (Supplement 2).
Figure 3.
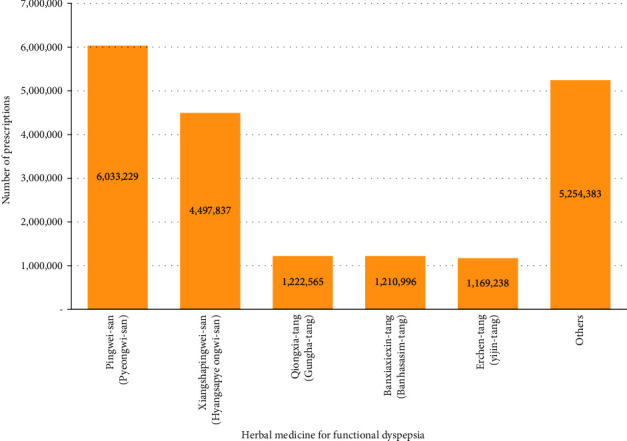
Number of frequently prescribed herbal medicines for functional dyspepsia.
Figure 4.
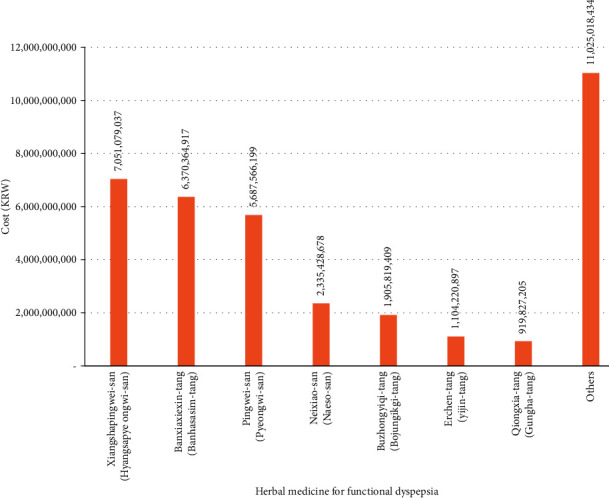
Cost of frequently prescribed herbal medicines for functional dyspepsia.
3.5. Frequent Comorbidities of FD
This study cohort comprised 21,771,403 comorbidities in total that were associated with the FD code (K30). Among them, M code (Diseases of the Musculoskeletal System and Connective Tissue) accounted for most (57.05%; n = 12,420,825) comorbidities, followed by the R code (Symptoms, Signs, and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified; 11.39%), S code (Injury, Poisoning, and Certain Other Consequences of External Causes; 9.82%), U code (Codes for Special Purposes; 8.07%), G code (Diseases of the Nervous System; 4.49%), J code (Diseases of the Respiratory System; 3.89%), and K code (Diseases of the Digestive System; 1.75%). The commonest comorbidity was lower back pain (M545; n = 3,225,059), followed by myalgia (M791; n = 1,390,267), muscle strain (M626; n = 1,118,574), joint pain (M255; n = 870,202), and pain localized to the upper abdomen (R101; n = 796,848) (Table 2). When the K30 code was the primary, secondary, or primary and secondary diagnosis, the ranking of comorbidities showed a similar trend. However, when the K30 code was the primary, the U code (Codes for special purposes, encompassing diseases name in Oriental medicine, disease patterns/syndromes in Oriental medicine, and disease patterns/syndromes of Four-Constitution Medicine) comprised the most frequent comorbidity. In particular, the “spleen qi deficiency pattern (U680)” and “food-retention disorder (U280)” were frequently reported when the K30 code was the primary or secondary diagnosis (Supplement 3).
Table 2.
Frequent comorbidities associated with functional dyspepsia.
| Diagnosis code | N | % | |
|---|---|---|---|
| M (diseases of the musculoskeletal system and connective tissue) | M545 (low back pain) | 3,225,059 | 26.64 |
| M791 (myalgia) | 1,390,267 | 11.48 | |
| M626 (muscle strain) | 1,118,574 | 9.24 | |
| M255 (pain in joint) | 870,202 | 7.19 | |
| M544 (lumbago with sciatica) | 692,076 | 5.72 | |
| Subtotal | 12,420,825 | — | |
|
| |||
| R (symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified) | R101 (pain localized to the upper abdomen) | 796,848 | 33.10 |
| R51 (headache) | 360,327 | 14.97 | |
| R42 (dizziness and giddiness) | 291,311 | 12.10 | |
| R104 (other and unspecified abdominal pain) | 223,702 | 9.29 | |
| R05 (cough) | 116,030 | 4.82 | |
| Subtotal | 2,479,230 | — | |
|
| |||
| S (injury, poisoning, and other consequences from external causes) | S335 (sprain and strain of the lumbar spine) | 435,071 | 20.59 |
| S934 (sprain and strain of the ankle) | 206,398 | 9.77 | |
| S836 (sprain and strain of other and unspecified parts of the knee) | 205,873 | 9.74 | |
| S337 (sprain and strain of other and unspecified parts of lumbar spine and pelvis) | 203,042 | 9.61 | |
| S434 (sprain and strain of the shoulder joint) | 198,715 | 9.40 | |
| Subtotal | 2,137,678 | — | |
|
| |||
| U (codes for special purposes) | U303 (neck-stiffness disorder) | 215,162 | 12.49 |
| U680 (spleen qi-deficiency pattern) | 134,750 | 7.82 | |
| U234 (sequela of wind-stroke disorder) | 115,626 | 6.71 | |
| U238 (joint impediment disorders) | 96,877 | 5.62 | |
| U280 (Food-retention disorder) | 90,571 | 5.26 | |
| Subtotal | 1,757,326 | — | |
|
| |||
| G (diseases of the nervous system) | G442 (tension-type headache) | 182,199 | 19.00 |
| G439 (migraine, unspecified) | 132,424 | 13.81 | |
| G470 (disorders of initiating and maintaining sleep (insomnias)) | 125,029 | 13.04 | |
| G510 (Bell's palsy) | 89,117 | 9.29 | |
| G438 (other migraine) | 56,505 | 5.89 | |
| Subtotal | 977,695 | — | |
|
| |||
| J (diseases of the respiratory system) | J00 (acute nasopharyngitis (common cold)) | 549,195 | 70.09 |
| J310 (chronic rhinitis) | 56,617 | 7.23 | |
| J069 (acute upper respiratory infection, unspecified) | 29,135 | 3.72 | |
| J304 (allergic rhinitis, unspecified) | 27,911 | 3.56 | |
| J303 (other allergic rhinitis) | 16,310 | 2.08 | |
| Subtotal | 847,865 | — | |
|
| |||
| K (diseases of the digestive system) | K590 (constipation) | 99,555 | 27.43 |
| K591 (functional diarrhea) | 60,018 | 16.54 | |
| K297 (gastritis, unspecified) | 31,770 | 8.75 | |
| K210 (gastroesophageal reflux disease with esophagitis) | 22,201 | 6.12 | |
| K076 (temporomandibular joint disorders) | 17,004 | 4.69 | |
| Subtotal | 380,691 | — | |
4. Discussion
This is the first nationwide population-based study to analyze the herbal medicine prescription patterns for FD using NHI data in the Republic of Korea. A total of 19,388,248 herbal medicine prescriptions were included in the analysis based on a review of claims data for the total study period of 10 years. The results showed that the total amount and cost of herbal medicine prescriptions for FD have been continually increasing every year.
According to the findings of our study, women and older adults frequently used herbal medicines to treat FD. This trend is presumably attributable to the higher global prevalence of FD among women and older adults [3, 12] as well as the higher trust in—and usage of—Korean medicines among these populations [13]. Among those who were older than 60 years, the number of FD patients who were prescribed herbal medicines showed a tendency to increase sharply each year. Older adults have a high preference for herbal medicines [14] and as the rate at which the elderly population is expanding in Korea is rapidly progressing [15], this trend is expected to continue. In particular, between 2010 and 2011, the number of prescriptions for patients aged 60 and older increased sharply, which may be attributable to the upward revision of the Korean elderly outpatient copayment system (age ≥65 years) in 2011 that has significantly influenced the medical behavior of Korean medicine practitioners and the number of herbal medicine prescriptions among older adults [16, 17].
Although FD is a chronic disease, the average herbal medicine prescription period was as short as 1.68 days. For FD treatment, in addition to herbal medicine, acupuncture and moxibustion are usually performed once a day and up to three times a week [18]; therefore, the short duration of the prescriptions may be due to the fact that patients frequently visit medical institutions and not only receive herbal medicine prescriptions for short periods but also acupuncture and moxibustion. However, as this study only targeted the number of herbal medicine prescriptions, the results should be interpreted cautiously, because no data are available regarding to the total number and duration of treatment per patient or for the prescription pattern of other treatments, such as acupuncture and moxibustion.
Our analysis showed that, among the herbal medicines prescribed, Pingwei-san (Pyeongwi-san) was the most prescribed, followed by Xiangshapingwei-san (Hyangsapyeongwi-san), Qiongxia-tang (Gungha-tang), Banxiaxiexin-tang (Banhasasim-tang), and Erchen-tang (Yijin-tang). These results are similar to those used in the order of Pingwei-san (Pyeongwi-san; 30%) and Banxiaxiexin-tang (Banhasasim-tang; 27%) for FD treatment in a survey conducted among 349 Korean medicine doctors in 2017 [11]. In particular, Pingwei-san (Pyeongwi-san) comprises six herbs: Cangzhu (Atractylodis Rhizoma), Chenpi (Citri Unshius Pericarpium), Houpu (Magnoliae Cortex), Gancao (Glycyrrhizae Radix et Rhizoma), Shengjiang (Zingiberis Rhizoma Recens), and Dazao (Zizyphi Fructus). In animal models, Pingwei-san (Pyeongwi-san) has been reported to regulate gastric secretion and gastrointestinal motility and protect the gastrointestinal mucosa [19, 20]; its effect on FD treatment has been confirmed in clinical studies [21, 22].
The total cost of herbal medicine prescriptions that were claimed to the NHI for FD treatment during the 10-year study period was ₩36,399,342,776 KRW, and the cost-based rankings of individual prescriptions were as follows: Xiangshapingwei-san (Hyangsapyeongwi-san), Banxiaxiexin-tang (Banhasasim-tang), and Pingwei-san (Pyeongwi-san). In particular, Pingwei-san (Pyeongwi-san), Qiongxia-tang (Gungha-tang), and Erchen-tang (Yijin-tang), which were the first, third, and fifth most prescribed herbal medicines, ranked third, ninth, and 10th, respectively, in terms of total prescription costs. This is because the maximum price for individual herbal medicines is set according to Regulation for Criteria for Providing Reimbursed Services in the NHI in Korea, and the order of the prescription amount and total cost may differ due to differences in the standard pricing of individual herbal medicines.
Most of the frequent comorbidities of FD were identified mainly with regard to the KCD M code, and lower back pain, myalgia, muscle strain, and joint pain were the commonest comorbidities among them. As the majority of this study population were older patients, it can be assumed that musculoskeletal disorders, which often afflict the elderly, were reported frequently [23, 24]. In addition, various comorbidities such as headache, dizziness, common cold, chronic rhinitis, and constipation were reported. Herbal medicine is specifically a typical multitarget multicomponent agent and, thus, has the potential to simultaneously treat various comorbidities. Therefore, it will be meaningful to confirm whether not only FD, but also the accompanying symptoms/comorbidities are improved by herbal medicine treatment through prospective clinical studies.
FD is a chronic disease that significantly impairs quality of life and work productivity [4, 5] and is difficult to treat due to its diverse symptoms and variable course [6, 7]. In this situation, herbal medicine has multicomponent and multitarget characteristics that can target the various pathological mechanisms and symptoms of FD, and studies on the effects of herbal medicines in FD treatment have been actively conducted [25]. Additionally, the present study shows that herbal medicine treatment is being actively administered in actual clinical practice for the treatment of FD, and the prescription amounts increase every year. However, compared to other East Asian countries, the NHI benefit rate for traditional medicine, including herbal medicine, in Korea is relatively low [26, 27], which increases the private medical expenses and disease burden and, consequently, socioeconomic costs. Accordingly, there is increasing demand for the need to expand the items covered by the NHI in Korea. The NHI needs to establish appropriate policies to expand the coverage of traditional medicine by expanding research on the safety and efficacy of herbal medicines and by recognizing the reality that the demand for herbal medicines for FD is increasing in Korea.
Meanwhile, for the treatment of FD, in addition to the 56 herbal medicines covered by the NHI in Korea, Liujunzi-tang (Yukgunja-tang), Zhishixiaopi-wan (Jisilsobi-hwan), and various crude herbal decoctions have been actively used, despite not being covered by the NHI in Korea [11]; their effectiveness has been verified through many clinical trials [28–31]. Nonetheless, their economic evaluation has not yet been undertaken, and when setting a control group for economic evaluation, a frequently used treatment with the same indication should be used [32]. Therefore, when specifying a control group for the economic evaluation of the herbal medicines used in FD treatment that are not covered under insurance, based on the results of this study, this can consist of the frequently used herbal medicines that are covered by the NHI such as Pingwei-san (Pyeongwi-san) and Xiangshapingwei-san (Hyangsapyeongwi-san). These studies provide important fundamental data to support decision-making that enables policymakers to allocate limited resources both efficiently and fairly.
Our study has the following limitations. As this study only targeted herbal medicine prescriptions for FD, it was not possible to confirm the prescription patterns of other interventions such as acupuncture and moxibustion, which can be used for FD in clinical settings. In real-world clinical practice, acupuncture, moxibustion, and chuna are actively used alongside herbal medicine to treat FD. In addition, as only 56 herbal medicines (mixed-extract powders) covered by the NHI were analyzed, the treatment pattern of crude herbal decoctions, which are widely used and not covered by the NHI, could not be confirmed [33]. Therefore, the medical expenditures identified in this study comprise only a part of the actual medical expenses. It would be meaningful to investigate medical behaviors and expenses using surveys and electronic medical record data in the future.
Despite the abovementioned limitations, to the best of our knowledge, this is the first study to use large-scale NHI claim data to investigate the disease burden and actual prescription pattern of herbal medicine, one of the most commonly used interventions in clinical Korean medicine. A 10-year retrospective long-term observation analysis was performed for all herbal medicines covered under the NHI. In the future, based on this study, we hope that evidence-based clinical research will be actively carried out, and related healthcare policies will be established to strengthen the insurance coverage of Korean medicine treatment.
5. Disclosure
The funding source played no role in the interpretation of the study results or the decision to submit these results for publication.
Acknowledgments
This work was supported by the Korea Institute of Oriental Medicine (KSN2021210).
Data Availability
The data that support the findings of this study are available from the Healthcare Big Data Hub of the HIRA. However, restrictions apply with regard to availability as they were used under license for research in the current study; therefore, these data are not publicly available. However, the study-related data are available from the co-author (EKA) upon reasonable request.
Ethical Approval
The study protocol was exempted from ethical review by the Institutional Review Board of the Korea Institute of Oriental Medicine (I-2010/008-005).
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Authors' Contributions
Conceptualization was done by BL. Methodology was done by BL and EKA. The original draft was written by BL. Review and editing were done by EKA and CY. Funding was acquired by CY. Supervision was done by CY.
Supplementary Materials
Supplement 1. List of the 56 herbal medicines used to treat functional dyspepsia in Korea. Supplement 2. Number of prescriptions and cost of 56 herbal medicines by year. Supplement 3. Frequent comorbidities associated with functional dyspepsia when the K30 code was the primary diagnosis.
References
- 1.Stanghellini V., Chan F. K. L., Hasler W. L., et al. Gastroduodenal disorders. Gastroenterology . 2016;150(6):1380–1392. doi: 10.1053/j.gastro.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Aziz I., Palsson O. S., Törnblom H., Sperber A. D., Whitehead W. E., Simrén M. Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study. The Lancet Gastroenterology and Hepatology . 2018;3(4):252–262. doi: 10.1016/S2468-1253(18)30003-7. [DOI] [PubMed] [Google Scholar]
- 3.Ford A. C., Marwaha A., Sood R., Moayyedi P. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut . 2015;64(7):1049–1057. doi: 10.1136/gutjnl-2014-307843. [DOI] [PubMed] [Google Scholar]
- 4.Hantoro I. F., Syam A. F., Mudjaddid E., Setiati S., Abdullah M. Factors associated with health-related quality of life in patients with functional dyspepsia. Health Qual Life Outcomes . 2018;16(1):p. 83. doi: 10.1186/s12955-018-0913-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sander G. B., Mazzoleni L. E., Francesconi C. F., et al. Influence of organic and functional dyspepsia on work productivity: the HEROES-DIP study. Value in Health . 2011;14(5):S126–S129. doi: 10.1016/j.jval.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Talley N. J., Ford A. C. Functional dyspepsia. New England Journal of Medicine . 2020;373(19):1853–1863. doi: 10.1016/S0140-6736(20)30469-4. [DOI] [PubMed] [Google Scholar]
- 7.Olafsdottir L. B., Gudjonsson H., Jonsdottir H. H., Bjornsson E., Thjodleifsson B. Natural history of functional gastrointestinal disorders: comparison of two longitudinal population-based studies. Digestive and Liver Disease . 2012;44(3):211–217. doi: 10.1016/j.dld.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Chiarioni G., Pesce M., Fantin A., Sarnelli G. Complementary and alternative treatment in functional dyspepsia. United European Gastroenterol Journal . 2018;6(1):5–12. doi: 10.1177/2050640617724061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Insurance Review & Assessment Service. Healthcare Bigdata Hub. Statistics of frequent diseases. 2021. https://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do .
- 10.Kim L., Sakong J., Kim Y. Developing the inpatient sample for the National Health Insurance claims data. Health Policy and Management . 2013;23(2):152–161. [Google Scholar]
- 11.National Institute for Korean Medicine Development. Korean medicine clinical practice guideline for functional dyspepsia. 2020;11-14:p. 32. https://nikom.or.kr/nckm/module/practiceGuide/view.do?guide_idx=154&menu_idx=14 . [Google Scholar]
- 12.Kim S. E., Kim N., Lee J. Y. Prevalence and risk factors of functional dyspepsia in health check-up population: a nationwide multicenter prospective study. Journal of Neurogastroenterology and Motility . 2018;24(4):603–613. doi: 10.5056/jnm18068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwon S., Heo S., Kim D., Kang S., Woo J. M. Changes in trust and the use of Korean medicine in South Korea: a comparison of surveys in 2011 and 2014. BMC Complementary and Alternative Medicine . 2017;17(1):p. 463. doi: 10.1186/s12906-017-1969-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sackett K., Carter M., Stanton M. Elders’ use of folk medicine and complementary and alternative therapies: an integrative review with implications for case managers. Professional Case Management . 2014;19(3):113–123. doi: 10.1097/ncm.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 15.Jang I. Y., Lee H. Y., Lee E. Geriatrics fact sheet in Korea 2018 from national statistics. Annals of Geriatric Medicine and Research . 2019;23(2):50–53. doi: 10.4235/agmr.19.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong D. B. Seoul, South Korea: The Graduate School of Seoul National University.; 2017. Analysis of the behavior of Korean medical doctors before and after upward revision of elderly outpatients copayment system. Master’s Thesis. [Google Scholar]
- 17.Kim H., Choi J. Y., Hong M., Suh H. S. Traditional medicine for the treatment of common cold in Korean adults: A nationwide population-based study. Integrative Medicine Research . 2021;10(1) doi: 10.1016/j.imr.2020.100458.100458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kwon C. Y., Ko S. J., Lee B., Cha J. M., Yoon J. Y., Park J. W. Acupuncture as an add-on treatment for functional dyspepsia: a systematic review and meta-analysis. Frontiers of Medicine . 2021;8 doi: 10.3389/fmed.2021.682783.682783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee M. C., Park J. R., Shim J. H., Ahn T. S., Kim B. J. Effects of traditional Chinese herbal medicine Shengmai-san and Pyungwi-san on gastrointestinal motility in mice. Journal of Korean Medicine for Obesity Research . 2015;15(2):68–74. [Google Scholar]
- 20.Chang I. K., Heu I. M. Experimental studies on the efficacy of Pyungwee-san, Hyangsapyungwee-san And Bylwhangumchunggl-san. Kyung Hee Unicersity Oriental Medical Journal . 1990;13:427–461. [Google Scholar]
- 21.Yuan B. Effect of Pingwei powder on gastric dynamics of intractable functional dyspepsia. Clinical Journal of Anhui Traditional Chinese Medicne . 2003;15(5):396–397. [Google Scholar]
- 22.Kim S. Y., Yoon S. H. A selective effect of combined treatment of electroacupuncture at Zusanli(ST36), manual acupuncture, and Pyengwisan in function dyspepsia patients with pyloric valve disturbance and hypoactivity of gastric vagus nerve. The Korean Journal of Internal Medicine . 2009;30(1):191–199. [Google Scholar]
- 23.Loeser R. F. Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clinics in Geriatric Medicine . 2010;26(3):371–386. doi: 10.1016/j.cger.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meucci R. D., Fassa A. G., Faria N. M. X. Prevalence of chronic low back pain: systematic review. Revista de Saúde Pública . 2015;49:p. 1. doi: 10.1590/S0034-8910.2015049005874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chu M. H. K., Wu I. X. Y., Ho R. S. T., et al. Chinese herbal medicine for functional dyspepsia: systematic review of systematic reviews. Therapeutic Advances in Gastroenterology . 2018;11 doi: 10.1177/1756284818785573.1756284818785573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang C. W., Hwang I. H., Yun Y. H., et al. Population-based comparison of traditional medicine use in adult patients with allergic rhinitis between South Korea and Taiwan. Journal of the Chinese Medical Association . 2018;81(8):708–713. doi: 10.1016/j.jcma.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 27.Park H. L., Lee H. S., Shin B. C., et al. Traditional medicine in China, Korea, and Japan: a brief introduction and comparison. Evidence-Based Complementary and Alternative Medicine . 2012;2012 doi: 10.1155/2012/429103.429103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang S., Zhao L., Wang H., et al. Efficacy of modified LiuJunZi decoction on functional dyspepsia of spleen-deficiency and qi-stagnation syndrome: a randomized controlled trial. BMC Complementary and Alternative Medicine . 2013;13:p. 54. doi: 10.1186/1472-6882-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kusunoki H., Haruma K., Hata J. Efficacy of Rikkunshito, a traditional Japanese medicine (Kampo), in treating functional dyspepsia. Internal Medicine . 2010;49(20):2195–2202. doi: 10.2169/internalmedicine.49.3803. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki H., Matsuzaki J., Fukushima Y. Randomized clinical trial: rikkunshito in the treatment of functional dyspepsia--a multicenter, double-blind, randomized, placebo-controlled study. Neuro-Gastroenterology and Motility . 2014;26(7):950–961. doi: 10.1111/nmo.12348. [DOI] [PubMed] [Google Scholar]
- 31.Tominaga K., Sakata Y., Kusunoki H. Rikkunshito simultaneously improves dyspepsia correlated with anxiety in patients with functional dyspepsia: a randomized clinical trial (the DREAM study) Neuro-Gastroenterology and Motility . 2018;30(7) doi: 10.1111/nmo.13319.e13319 [DOI] [PubMed] [Google Scholar]
- 32.Kim J. H., Kwon H. Y., Hong J. H., Lee T. J. A Guideline for Economic Evaluation of Korean Medicine . Seoul, South Korea: Guideline center for Korean Medicine; 2018. [Google Scholar]
- 33.Lim B. Korean medicine coverage in the National health insurance in Korea: present situation and critical issues. Integrative Medicine Research . 2013;2(3):81–88. doi: 10.1016/j.imr.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement 1. List of the 56 herbal medicines used to treat functional dyspepsia in Korea. Supplement 2. Number of prescriptions and cost of 56 herbal medicines by year. Supplement 3. Frequent comorbidities associated with functional dyspepsia when the K30 code was the primary diagnosis.
Data Availability Statement
The data that support the findings of this study are available from the Healthcare Big Data Hub of the HIRA. However, restrictions apply with regard to availability as they were used under license for research in the current study; therefore, these data are not publicly available. However, the study-related data are available from the co-author (EKA) upon reasonable request.


