Abstract
Due to the challenges in data collection, there are few studies examining how individuals’ routine mobility patterns change when they experience influenza-like symptoms (ILS). In the present study, we aimed to assess the association between changes in routine mobility and ILS using mobile phone-based GPS traces and self-reported surveys from 1,155 participants over the 2016–2017 influenza season. We used a set of mobility metrics to capture individuals’ routine mobility patterns and matched their weekly ILS survey responses. For a statistical analysis, we used a time-stratified case-crossover analysis and conducted a stratified analysis to examine if such associations are moderated by demographic and socioeconomic factors, such as age, gender, occupational status, neighborhood poverty and education levels, and work type. We found that statistically significant associations existed between reduced routine mobility patterns and the experience of ILS. Results also indicated that the association between reduced mobility and ILS was significant only for female and for participants with high socioeconomic status. Our findings offered an improved understanding of ILS-associated mobility changes at the individual level and suggest the potential of individual mobility data for influenza surveillance.
Keywords: Mobile phone-based GPS, Influenza-like symptoms (ILS), Mobility metrics, Time-stratified case-crossover
1. Introduction
Seasonal flu is a contagious respiratory illness caused by influenza viruses. The health burden associated with influenza has been well-documented (Molinari et al., 2007; Chang et al., 2016). In 2018, for example, the Centers for Disease Control and Prevention (CDC) reported approximately 30 million symptomatic illnesses, 13 million medical visits, and 500 thousand influenza-related deaths nationwide as the annual burden of seasonal flu (Centers for Disease Control and Prevention, 2018a).
Influenza surveillance system tracks the temporal and spatial variations of influenza onset, and uses the collected information to provide effective prevention and control measures against epidemics. However, the current influenza surveillance system underestimates the actual incidence cases and thus fails to provide real-time information (Hayward et al., 2014; Yang et al., 2015). These issues are often associated with reporting lags and their dependence on hospital usage data, such as outpatient visits and hospitalizations, as a primary data source (Lee and Wong, 2014; Yang et al., 2017). To address these issues, attempts have been made to leverage other data sources, such as the records of students’ absences from school (Aldridge et al., 2016), online search trends for flu (Yang et al., 2015; Shin et al., 2016), and portable sensor measurements (Miller et al., 2018; Konty et al., 2019). In their longitudinal study of dengue and influenza, Perkins et al. (2016) demonstrated the utility of individual’ mobility data as a means to infer personal health status, noting that study participants’ mobility patterns changed while they were coping with fever. Similarly, Barlacchi et al. (2017) showed that individuals’ mobility patterns could be used as a predictor of the onset of influenza illness, although their findings were based on the unrepresentative sample (e.g., 27 study participants) over a relatively short period (e.g., a month) that did not cover the full cycle of a typical influenza season.
Traditionally, individuals’ mobility data and disease symptoms have been collected via mail, telephone, or personal observations/interviews, all of which are time-consuming, costly, and labor-intensive. These challenges in traditional data collection have led to a dearth of studies examining the association between mobility and health status. In recent years, however, the widespread use of mobile phones has enabled investigators to tackle these problems by using massive mobile phone data as a proxy of human mobility (Wesolowski et al., 2016). Mobile phone tracking data consists of a series of geographical coordinates collected by Global Positioning System (GPS) technologies, and these GPS traces reflect individuals’ movements and whereabouts at fine scales.
Most previous studies (Schönfelder and Axhausen, 2003; Siła-Nowicka et al., 2016) that captured human mobility patterns from mobile-phone data relied on a few common mobility metrics, such as the number of places visited, duration of stay at each place, and travel distance between visited places. Others quantified the regularity and spatial range of individuals’ mobility using either entropy-based measures (Song et al., 2010; Xu et al., 2018) or radius of gyration (Gonzalez et al., 2008; Barbosa et al., 2018). These metrics are in common to reveal individuals’ routine mobility patterns, which likely change when they experience influenza-like symptoms (ILS) like fever and extreme fatigue. To the best of our knowledge, however, there are no previous studies that have quantified mobility by these multiple mobility metrics to test the association between changes in routine mobility patterns and the onset of influenza illness.
We further hypothesized that the changes in human mobility associated with influenza illness would be more pronounced among individuals with higher risks of experiencing severe symptoms. For instance, the risk of complications of influenza-like pneumonia is higher for the elderly compared to younger persons (Lee et al., 2010; Talbot, 2017). Similarly, the symptoms tend to be more severe for females than males (Lorenzo et al., 2011; Klein et al., 2012). Meanwhile, changes in individuals’ mobility patterns in response to experiencing influenza-like illness may also vary by socioeconomic status (SES). Specifically, individuals with high SES have greater discretion over their work or economic capacity to afford absence from work than individuals with low SES (Gozzi et al., 2021; Lee et al., 2021), and consequently, mobility patterns would be more likely to change for the individuals with high SES compared to the ones with low SES.
In the present study, we tested the hypothesis that individuals’ routine mobility patterns change when they experience ILS using mobile phone tracking data. Specifically, we investigated this question by combining the mobile phone-based GPS traces with weekly self-reported symptom surveys collected from 1,155 study participants in western New York, U.S., over the entire influenza season in 2016–2017. We matched participants’ mobility patterns quantified by multiple mobility metrics with their self-assessed ILS, and conducted statistical analyses to evaluate if the changes in individuals’ routine mobility patterns would be associated with the onset of ILS. We also explored if such associations between mobility changes and onset of ILS are moderated by individuals’ demographic characteristics and socioeconomic status.
2. Materials and Methods
2.1. Study Area and Data
The present study is based on a larger project (Yoo, 2019; Yoo et al., 2020, 2021b; Eum and Yoo, 2021), and focuses on a total of 1,155 study participants who were the residents of Erie and Niagara counties in western New York, US, and had experienced ILS at least once during the study period. We recruited the study participants via invitation letters, flyers, online advertisements using social media, and local news. Each participant began their survey on different days between 10/24/2016 and 12/18/2016 and engaged in the survey for different periods (with a minimum of 129 days to a maximum of 224 days) with an average of 201 days. The survey officially ended on 05/22/2017.
The participants provided home and work addresses, as well as personal information, such as gender and age group (age 13–17, 18–34, 35–64, and over 65 years old). They also provided information about their occupational status whether they were a full-time employee, part-time employee, student, or unemployed. Sensitive information about study participants, such as income and education level, was not collected to protect participants’ privacy.
Each participant installed a mobile phone application (app) developed by the research team and completed weekly surveys using the app. Participants reported if they had at least one of the influenza-like symptoms (e.g., fever, runny nose, sore throat, cough, and nausea) in the past week. The weekly survey questions also included their coping strategies to the ILS in case they experienced ILS, asking them to select any from the following options: going to work or school while sick; staying home sick from work or school; visiting a doctor; or taking over-the-counter-flu medicine. Lastly, participants were asked to report the name and addresses of up to five most frequently visited places (FVPs) during the past week except the home address. While participants were able to initiate the survey anytime at their convenience, the app sent a notification every Monday to maximize their survey participation.
In addition, we collected location information (i.e., geographical coordinates), time, speed, and the accuracy of the GPS traces using the app that relied on the iPhone’s significant-change location service (Apple Inc., 2019). This location service was triggered to record a new location if a movement of a device was detected, typically more than 500 m away from the last recorded location. Although this distance threshold was sometimes too coarse to discern some visited places from others, it was a pre-determined parameter by Apple Inc., and could not be changed. We also used a power-friendly location service to support our data collection because battery drainage can be a major problem of mobile phone-based location tracing. The survey was approved by the Institutional Review Board of the university authors are affiliated with.
During their participation over a six-month period, a small number of participants made trips outside the study area, although these were rare (< 2% of total traces). After we confirmed that those trips outside the study area were not a part of individuals’ routine mobility, we excluded such GPS traces in the subsequent analyses.
As reported by Yoo et al. (2020), GPS traces collected using the iPhone’s significant-change location service suffered from missing data problems. Specifically, no GPS tracing occurred near the places where individuals stayed still or spent substantial amounts of time, and the presence of such missing data in GPS traces led to incorrect inference of individuals’ routine mobility patterns. To address the issue, we imputed the under-reported GPS traces at the locations where the device remained static. We refer readers to Yoo et al. (2020) for details, but a brief description of the algorithm is provided in Appendix A.
In order to determine the land-use type of places at which participants visited, we used parcel data for Erie and Niagara counties obtained from the New York State GIS Clearinghouse (https://gis.ny.gov). The GIS polygon data contains information on property types, as defined by the New York State Department of Taxation and Finance (https://www.tax.ny.gov/research/property/assess/manuals/prclas.htm). We classified the parcels into six property types: residential, commercial, recreational, educational, healthcare, and others.
The socioeconomic status (SES) information was not directly collected from study participants, but it was inferred from their home and workplace addresses. Here, we used the following three variables as a proxy of participants’ SES: (1) neighborhood poverty; (2) neighborhood-level educational attainment; and (3) the type of workplace (Lowcock et al., 2012; Levy et al., 2013; Mingo et al., 2014). We obtained 2011–2016 American Community Survey (ACS) 5-year estimate data (https://data.census.gov/cedsci/) for the two neighborhood-level variables. Specifically, we operationalized neighborhood poverty as the percentage of persons living below the federal poverty level within each census tract. Similarly, we defined neighborhood-level educational attainment as the percentage of people living in census tracts without a high school degree. We further classified these variables into four quartiles of low, mid-low, mid-high, and high, and used them in subsequent analyses. See Appendix B for details on the two neighborhood-level SES variables and their classification scheme. Lastly, we matched the reported workplace address with both the Google Places database (https://developers.google.com/maps/documentation/places/web-service/overview) and tax parcel data and extracted the contextual information about each participant’s workplace. We classified workplaces into one of the two categories: blue-collar (e.g., construction, farming, forestry, fishing, and manual labor) or white-collar occupation (e.g., education, professional, and public administration).
2.2. Quantification of Mobility Patterns: Mobility Metrics
The online survey was conducted on a weekly basis, although GPS traces were collected along with each participant’s movements. To illustrate mobile-phone based GPS trace data, we mapped out the location of visited places for two randomly selected participants on the week of 12/12/2016 – 12/18/2016 (see Figure 1). Here, the size of circles increased in proportion to the dwell time at each visited place, and the lines between two places were drawn according to the sequence of visits. Clearly, we can quantify the differences in the mobility patterns of these two individuals by comparing the number of frequently visited places (2 versus 4 places) and the time spent at home (17.9 versus 15.9 hours).
Figure 1.
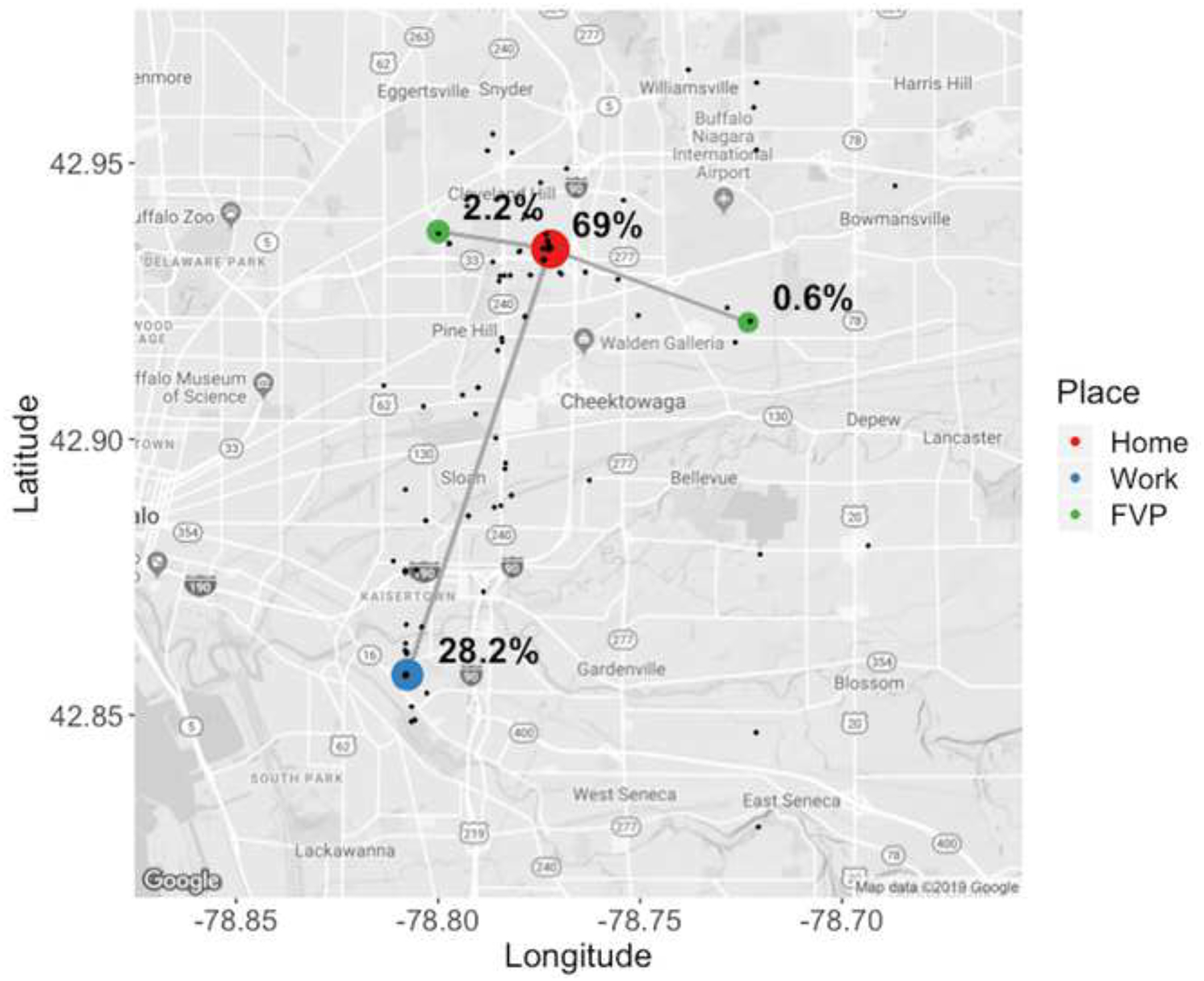
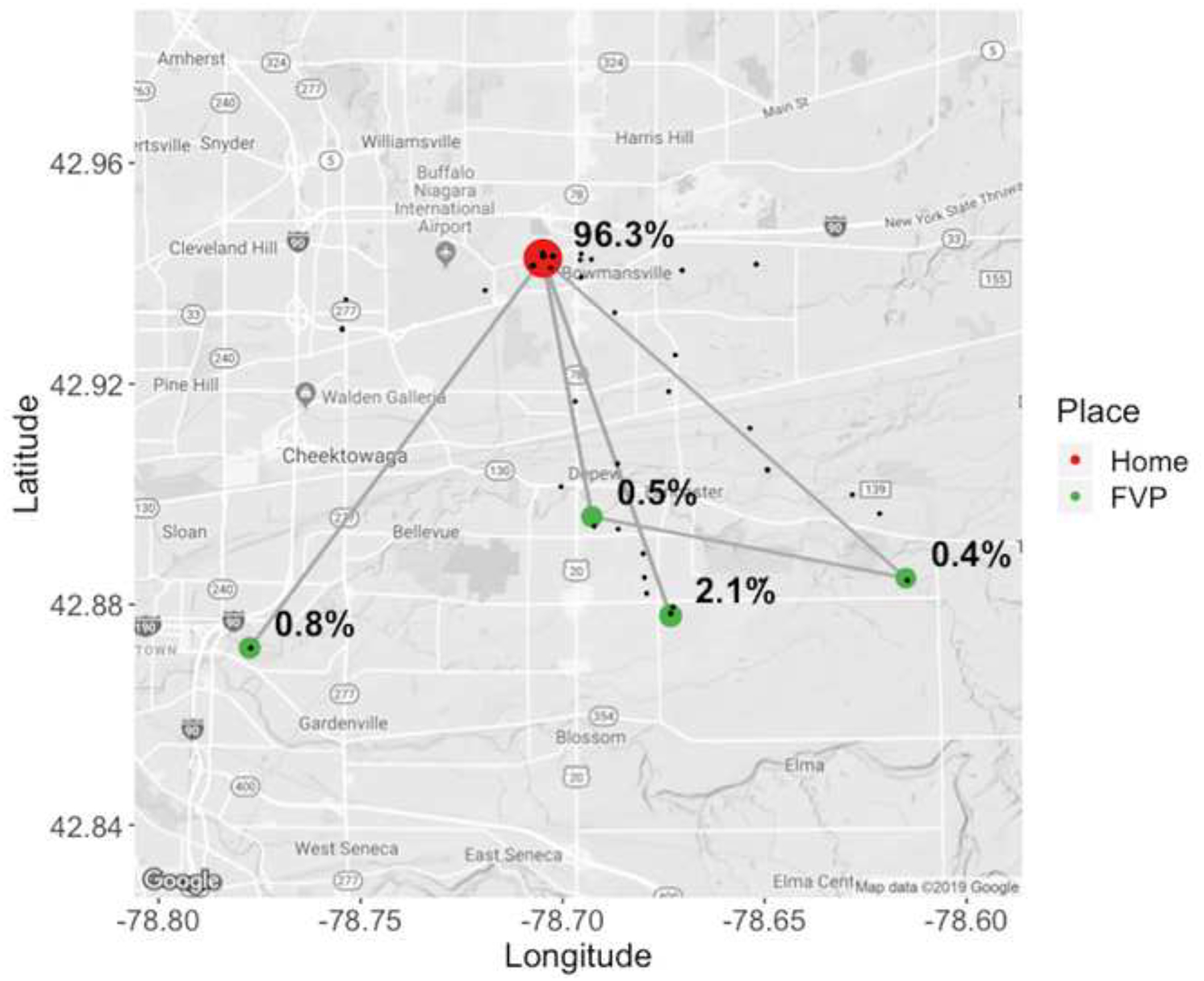
Home, work, and frequently visited places (FVPs) of two randomly selected participants during the week of 12/12/2016 – 12/18/2016: (a) a female employee in the 35–64 age group and (b) an unemployed male aged above 65.
To coordinate the GPS traces with the weekly online survey, we summarized individuals’ GPS traces as weekly mobility pattern metrics using the following mobility metrics (Schönfelder and Axhausen, 2003; Gonzalez et al., 2008; Xu et al., 2018):
Total number of places visited (N)
Number of places visited per property type θ (Nθ ≤ N)
Dwell time at home (Th), work (Tw), and frequently-visited places (Tv)
Activity entropy (E)
Radius of gyration (R), and
Total travel distance (D).
First, we identified a set of frequently visited places (FVPs) based on the weekly online survey. Next, we created a set of weekly visited places by adding participants’ home and work addresses to FVPs. Our research team geocoded these weekly visited places using the Geocoding API of Google Maps Platform (https://developers.google.com/maps/documentation/geocoding/start). Lastly, we combined the geocoded weekly visited places with the GPS traces collected on the same week for each individual to confirm participants’ visits to reported places. We also measured dwell time at visited places as a mobility metric. To account for the positional error that might be present in the GPS traces (Yoo et al., 2020), we used a 1 km buffer centered at each geocoded location while merging the two datasets (DeMers, 2008).
Mobility metrics were calculated from the merged data set (weekly visited places and GPS traces). We calculated the total number of visited places (N) each week and identified the property type of places that participants visited. The property type was determined by overlaying the geocoded FVPs with GIS parcel data. This information was summarized by calculating the number of visited places per property type each week for residential (Nr), commercial (Nc), recreational (Nf), educational (Ne), and healthcare (Nd) facilities, respectively.
We calculated the dwell time at each participant’s known locations, such as home (Th), work (Tw), and FVPs (Tv), using GPS traces on a weekly basis. The total dwell time at each known place was calculated by adding the total dwell time of each GPS trace that was assigned to the place. We assumed that the time interval between consecutive GPS traces represents the dwell time at each GPS position because the location data were collected using the iPhone’s motion-triggered system.
We also calculated activity entropy (Song et al., 2010; Barlacchi et al., 2017; Xu et al., 2018) to capture how each participant allocated time across the places visited. The activity entropy was calculated as based on the proportion of dwell time at each place over the total dwell time at N places, i.e., . The activity entropy is the lowest (i.e., zero) if a participant spent an entire week at one place, and its value increases if N gets larger (i.e., the individual visited more places). That is, if an individual spends more time at home due to ILS, the value of activity entropy decreases. Meanwhile, E increases as an individual spends the same amount of time at multiple places. In summary, E quantifies the predictability or, conversely, the diversity of an individual’s mobility patterns.
The radius of gyration is a standardized measure of the geographical extent of an individual’s mobility (Xu et al., 2015), and calculated as . Here , m = 1, …, M is the geographical coordinates of each GPS trace, where the total number of GPS traces is denoted by M. The mean center of the GPS traces is denoted by .
We also measured the total travel distance D by calculating the sum of the travelled distance between consecutive GPS traces each week.
2.3. Statistical Analysis: Case-crossover Design
We applied a time-stratified case-crossover design with a conditional logistic regression model to study the association between individuals’ mobility patterns and their experience of ILS. For each individual, the mobility metrics of the week when the participant reported one’s experience of ILS (‘case’ week) was compared with the mobility metrics on the other weeks during the same month and the year without ILS (‘control’ weeks). By selecting control weeks from the same month and the year, we assessed the associations between changes in participants’ mobility patterns and their ILS while effectively controlling for potential confounding effects, such as participant’s age, gender, and other fixed participant characteristics (Janes et al., 2005; Carracedo-Martínez et al., 2010).
We developed a conditional logistic regression model for each of the mobility metrics with the self-assessed health status. Here, if a participant experienced ILS during the week of interest, we assigned 1 and 0 otherwise. For the mobility metrics associated with dwell time and travel distance, we used daily average by dividing the weekly metrics by 7 days in order to align with other metrics in the model fit.
In addition, we conducted a stratified analysis to examine the moderation of associations between changes in mobility patterns and ILS by individuals’ age, gender, occupational status. We further assessed the effect modification by individuals’ SES based on their proxy variables. The statistical significance of the difference between each stratum-specific model coefficient was also tested. Specifically, we calculated the z-score of the difference as , where and denote the model coefficients in the conditional logistic regression models, and σ1 and σ2 are the standard errors of the models (Malig et al., 2016; Chen et al., 2019; Yoo et al., 2021a).
All the analyses were conducted in R 3.4.0 (R Core Team, 2017). We used the survival package to fit the conditional logistic regression models.
3. Results
3.1. Study Participants and Survey Data
Among the total of 1,155 participants, the majority were females (68%) and 35 and 64 years old (56%). As summarized in Table 1, a total of 144 participants (12%) were students, and 863 (75%) were either full- or part-time employees who reported their work addresses. Only 148 participants (13%) reported being unemployed at the time of their participation.
Table 1:
Participants by age, gender, and occupational status.
| Gender | Age | Occupational Status | |||
|---|---|---|---|---|---|
| Full-time employee | Part-time employee | Student | Unemployed | ||
| Female | 13–17 | 0 | 1 | 23 | 1 |
| 18–34 | 148 | 32 | 78 | 18 | |
| 35–64 | 300 | 81 | 4 | 61 | |
| ≥ 65 | 5 | 4 | 0 | 31 | |
| Male | 13–17 | 0 | 0 | 17 | 0 |
| 18–34 | 97 | 6 | 21 | 0 | |
| 35–64 | 176 | 5 | 1 | 16 | |
| ≥ 65 | 4 | 4 | 0 | 21 | |
We received a total of 32,252 online survey responses from the 1,155 participants during the study period. On average, participants submitted their surveys for 27.9 weeks (out of a total of 30 weeks). We received a majority (75%) of the survey responses on Mondays, which indicates that potential recall bias in the survey was minimized by the app notification. As shown in Figure 2, the number of participants who experienced ILS increased from the beginning of the influenza season in October, 2016 up to its peak (26.2%) on the last week of December, 2016. The infection rate decreased with some fluctuations in the rest of the study period. Our observation was consistent with the CDC report (Centers for Disease Control and Prevention, 2018b) on the influenza season.
Figure 2.
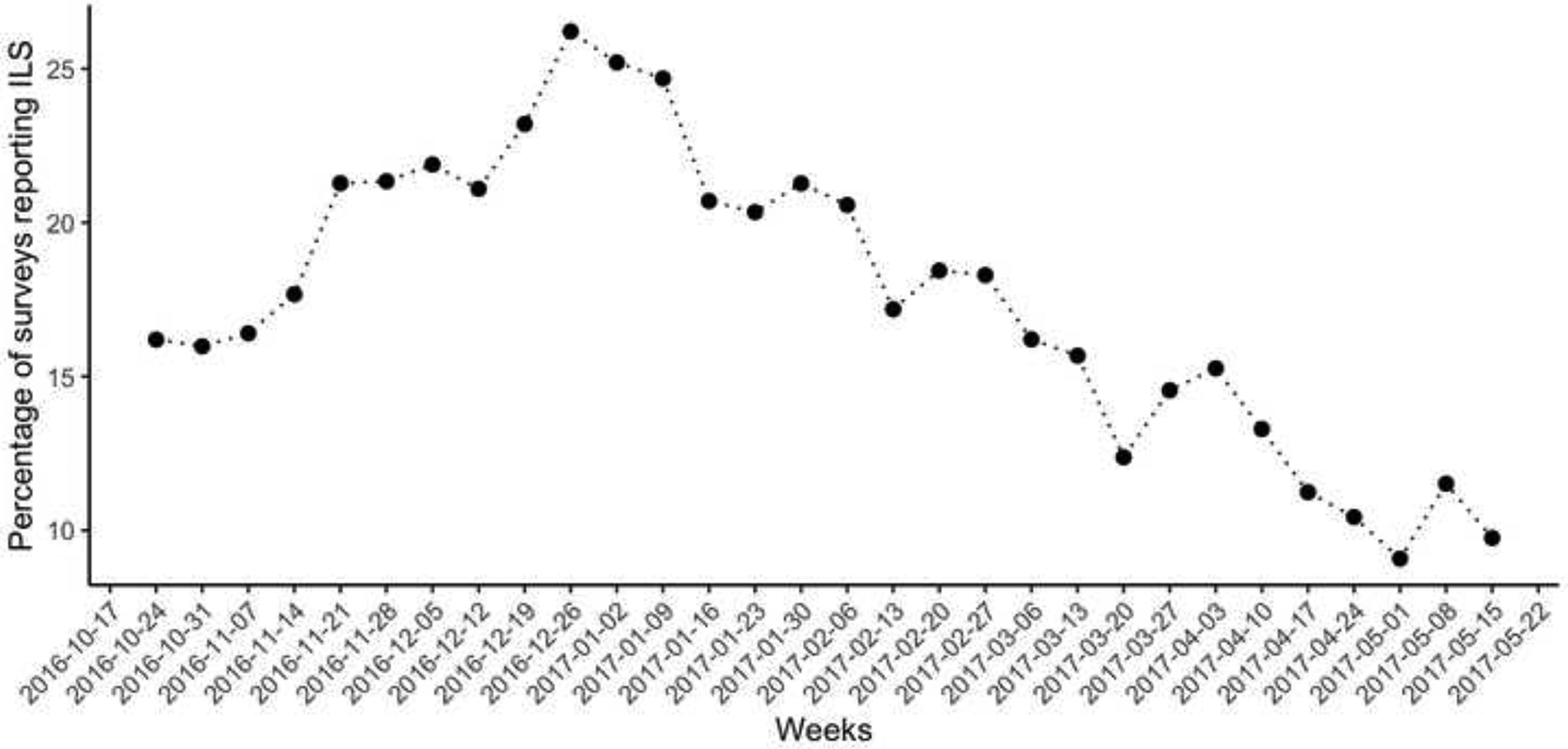
Temporal (weekly) variation of self-assessed influenza illness in the study region.
In terms of their responses to the experiences of ILS, a total of the 5,624 online survey responses (48.7%) of the participants reported that they kept working or went to school. Only 503 responses (8.9%) were associated with the behaviors of seeking medical assistance (i.e., went to see a doctor) while experiencing ILS (Table 2).
Table 2:
Survey responses to influenza-like symptoms.
| Responses | Count (%) |
|---|---|
| Keep working | 2,738 (48.7) |
| Stay at home | 918 (16.3) |
| Go to the doctor | 503 (8.9) |
| Take medicine | 1,949 (34.7) |
| None of the above | 1,624 (28.9) |
| Total | 5,624 (100%) |
3.2. Mobility Metrics
In Table 3, we summarized the study participants’ weekly mobility patterns using the twelve mobility metrics described in Section 2.2. On average, the study participants stayed at home for 101 hours and visited about 4.8 places per week. The average weekly travel distance was 343 km. We also examined mobility metrics by age, gender, and occupational status of each participant. The Welch two-sample t-test suggested that mobility patterns were not significantly different by gender, but they were significantly different from one age group to the other and by their occupational status (p-value < 0.05). Specifically, adults aged 18 to 64 had greater mobility than both teenagers and the elderly (over 65 years old) in terms of the radius of gyration and total travel distance. The mobility patterns of the youngest age group were the least predictable and irregular even though the number of places they visited were fewer than those of other age groups. As expected, the elderly spent most of their time at home (substantially higher than any other age group), and the spatial extent of the youngest age group’s mobility was significantly smaller than the radius of gyration of adults (p-value < 0.05). Full-time workers traveled a greater distance over larger spatial areas than the participants in other occupational statuses, although the differences were significant only from part-time employees. Unemployed individuals spent longer hours at both home and FVPs than any other group of participants. We also found that students had a significantly smaller number of visited places compared to other participants.
Table 3:
Summary of mobility metrics.
| Mobility Metrics* | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | N r | N c | N f | N e | N d | T h | T w | T v | E | R | D | |
| Total | 4.8 (1.2)+ | 0.4 (0.5) | 1.6 (1.0) | 0.1 (0.3) | 0.2 (0.4) | 0.0 (0.2) | 101.4 (15.7) | 19.2 (15.5) | 14.4 (11.9) | 0.7 (0.3) | 6.0 (2.7) | 34.5 (20.1) |
| Gender | ||||||||||||
| Female | 4.8 (1.2) | 0.4 (0.5) | 1.7 (1.0) | 0.1 (0.2) | 0.2 (0.4) | 0.0 (0.1) | 102.4 (15.7) | 18.7 (15.3) | 15.0 (12.1) | 0.7 (0.3) | 5.9 (2.7) | 33.2 (19.8) |
| Male | 4.6 (1.2) | 0.4 (0.5) | 1.4 (1.1) | 0.2 (0.3) | 0.2 (0.4) | 0.0 (0.2) | 99.3 (15.5) | 20.1 (15.8) | 13.2 (11.2) | 0.7 (0.3) | 6.3 (2.8) | 37.2 (20.4) |
| Age group | ||||||||||||
| 13–17 | 4.3 (1.2) | 0.4 (0.6) | 1.1 (1.0) | 0.2 (0.2) | 0.3 (0.4) | 0.0 (0.1) | 99.1 (11.8) | 26.1 (12.9) | 13.9 (16.3) | 0.9 (0.3) | 4.2 (1.8) | 27.1 (16.0) |
| 18–34 | 4.5 (1.3) | 0.4 (0.6) | 1.4 (1.1) | 0.1 (0.2) | 0.2 (0.4) | 0.0 (0.2) | 98.4 (15.6) | 20.2 (14.6) | 14.7 (12.0) | 0.8 (0.3) | 6.2 (2.5) | 35.5 (18.2) |
| 35–64 | 4.9 (1.1) | 0.4 (0.5) | 1.7 (1.0) | 0.2 (0.3) | 0.2 (0.4) | 0.0 (0.2) | 102.4 (15.2) | 19.8 (15.7) | 14.2 (11.6) | 0.7 (0.2) | 6.2 (2.9) | 34.8 (21.4) |
| ≥ 65 | 4.8 (1.1) | 0.3 (0.4) | 2.1 (1.0) | 0.2 (0.3) | 0.1 (0.3) | 0.1 (0.2) | 110.9 (18.2) | 3.6 (9.1) | 15.3 (10.4) | 0.5 (0.2) | 5.2 (2.7) | 29.6 (19.0) |
| Occupational status | ||||||||||||
| Full-time | 4.8 (1.2) | 0.4 (0.5) | 1.6 (1.0) | 0.1 (0.3) | 0.2 (0.4) | 0.0 (0.2) | 97.9 (13.5) | 24.5 (14.4) | 13.2 (11.4) | 0.8 (0.2) | 6.6 (2.8) | 35.9 (18.2) |
| Part-time | 5.0 (1.1) | 0.4 (0.5) | 1.6 (0.9) | 0.1 (0.2) | 0.3 (0.4) | 0.0 (0.1) | 109.7 (14.0) | 12.0 (9.9) | 14.7 (10.5) | 0.6 (0.3) | 5.3 (2.3) | 30.6 (18.9) |
| Student | 4.3 (1.2) | 0.3 (0.5) | 1.1 (0.9) | 0.1 (0.2) | 0.4 (0.5) | 0.0 (0.1) | 97.8 (14.8) | 18.6 (14.2) | 16.0 (12.6) | 0.8 (0.3) | 5.1 (2.2) | 33.1 (18.6) |
| Unemployed | 4.9 (1.1) | 0.4 (0.5) | 2.3 (1.0) | 0.2 (0.3) | 0.2 (0.3) | 0.1 (0.1) | 114.9 (17.7) | - | 18.5 (13.5) | 0.5 (0.2) | 4.8 (2.3) | 32.1 (29.0) |
Mean (Standard Deviation)
Mobility Metrics: Total number of visited places (N); Number of visited places in residential (Nr), commercial (Nc), recreational (Nf), educational (Ne), and healthcare (Nd) areas; Dwell time at home (Th), work (Tw), and frequently visited places (Tv); Activity entropy (E); Radius of gyration (R); Travel distance (D).
3.3. Associations between mobility and influenza-like symptoms
The odds ratios (OR) and the 95% confidence interval (CI) obtained from the conditional logistic regression for each mobility metric are summarized in Figure 3. We found that the dwell time at home (Th) was a significant mobility metric as an hour increase of dwell time at home increased the odds of being sick (OR = 1.01; 95% CI = 1.00–1.04). Similarly, we found that the dwell time at work (Tw) was negatively associated with ILS (OR = 0.95; 95% CI = 0.92–0.98). We also found that a unit decrease of both activity entropy (OR = 0.66; 95% CI = 0.52–0.83) and the total travel distance (OR = 0.94; 95% CI = 0.92–0.95) showed significant associations with increased odds of having ILS. Meanwhile, no statistically significant associations were found for the number of places visited nor the radius of gyration.
Figure 3.
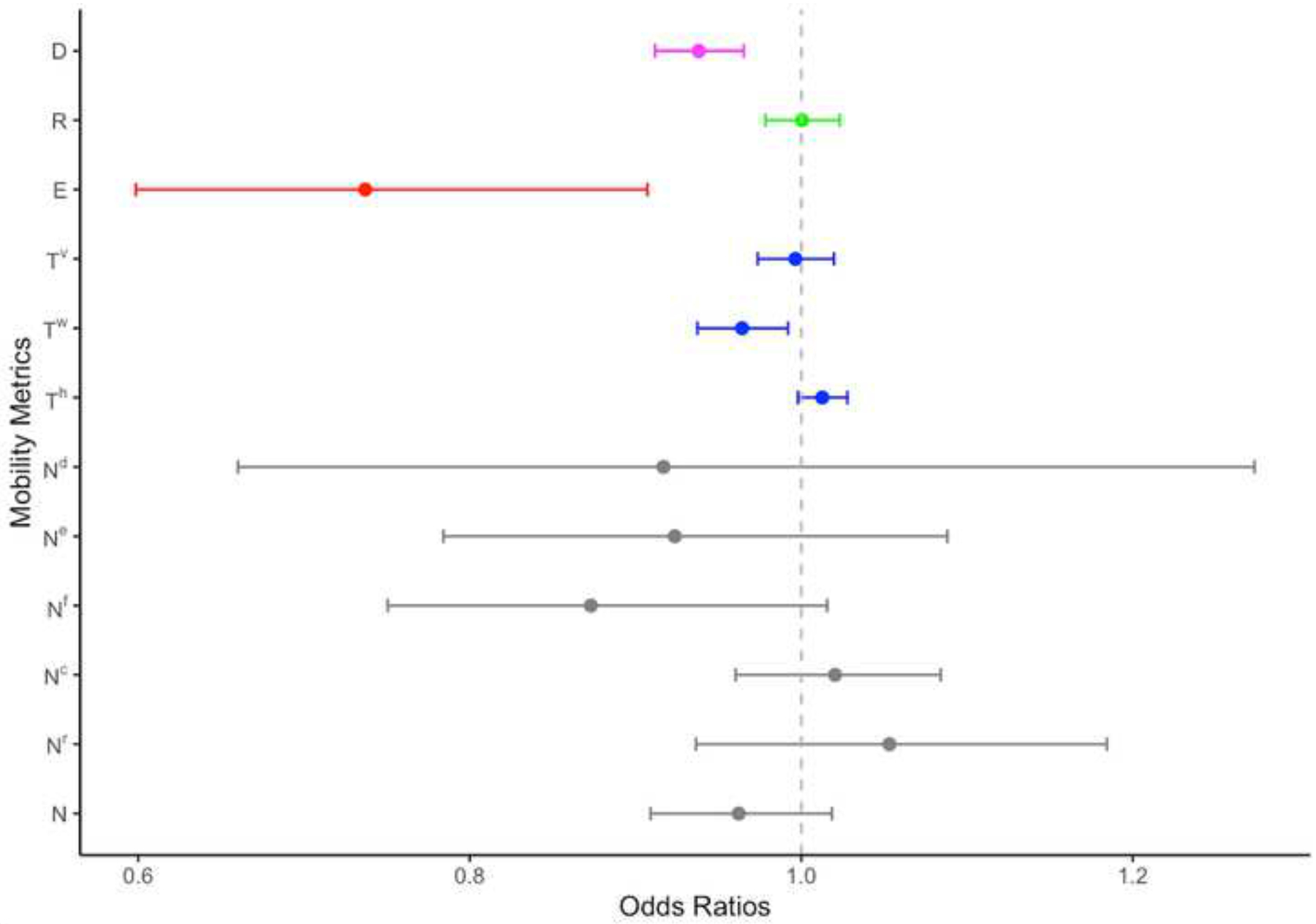
Estimated association between influenza-like symptoms and a unit increase in mobility pattern metrics. The odds ratio (OR) and 95% CI for 12 mobility metrics are summarized using different shades: the number of visited places (N) in gray, dwell time (T) in blue, activity entropy (E) in red, radius of gyration (R) in green, and total travel distance (D) in magenta. The number of visited places is further divided into residential (Nr), commercial (Nc), recreational (Nf), educational (Ne), and healthcare (Nd) based on the property type. Similarly, the dwell time is also categorized into dwell time at home (Th), work (Tw), and FVPs (Tv).
Table 4 presents the summary of estimated associations between changes in mobility patterns and ILS experiences across different age groups, genders, occupational statuses, neighborhood poverty and education levels (categorized into four groups), and work types (two categories). The gender-stratified analysis suggested that decreased dwell time at work was significantly associated with ILS for both males and females. However, the decreased number of visited places, reduced activity entropy, and shortened travel distance were significantly associated with ILS only for females. We found that these gender differences were statistically significant with p-values of 0.01, 0.03, and 0.02 for the number of visited places, activity entropy, and travel distance, respectively.
Table 4:
Subgroup analysis by age, gender, occupational status, and SES.
| Subgroups | Mobility Metrics* | ||||||
|---|---|---|---|---|---|---|---|
| N | T h | T w | T v | E | R | D | |
| Gender | |||||||
| Female | 0.92 (0.86–0.99) | 1.03 (1.01–1.04) | 0.96 (0.92–0.99) | 0.98 (0.95–1.01) | 0.58 (0.50–0.75) | 0.99 (0.96–1.02) | 0.90 (0.86–0.93) |
| Male | 1.08 (0.96–1.21) | 1.01 (0.98–1.04) | 0.94 (0.89–1.00) | 1.00 (0.95–1.05) | 0.90 (0.58–1.38) | 1.02 (0.98–1.07) | 0.97 (0.91–1.02) |
| Age group | |||||||
| 13–17 | 0.96 (0.70–1.33) | 1.02 (0.94–1.09) | 0.98 (0.88–1.09) | 0.95 (0.80–1.13) | 0.56 (0.50–1.46) | 0.98 (0.89–1.08) | 1.01 (0.84–1.22) |
| 18–34 | 0.91 (0.82–1.02) | 1.03 (1.00–1.06) | 0.97 (0.92–1.02) | 0.97 (0.92–1.01) | 0.56 (0.50–0.82) | 0.99 (0.95–1.04) | 0.93 (0.88–0.97) |
| 35–64 | 0.98 (0.90–1.06) | 1.02 (1.00–1.04) | 0.94 (0.90–0.98) | 0.99 (0.96–1.03) | 0.63 (0.50–0.86) | 1.00 (0.97–1.04) | 0.92 (0.88–0.96) |
| ≥ 65 | 1.03 (0.85–1.26) | 1.01 (0.95–1.07) | 0.94 (0.73–1.20) | 1.03 (0.95–1.10) | 2.24 (0.89–2.30) | 1.02 (0.93–1.12) | 0.85 (0.73–0.99) |
| Occupational Status | |||||||
| Full-time | 0.98 (0.90–1.06) | 1.01 (0.98–1.03) | 0.94 (0.91–0.98) | 0.99 (0.96–1.03) | 0.63 (0.47–0.84) | 1.00 (0.97–1.03) | 0.91 (0.87–0.95) |
| Part-time | 0.97 (0.81–1.17) | 1.09 (1.03–1.14) | 0.95 (0.86–1.05) | 0.91 (0.84–0.99) | 0.42 (0.21–0.82) | 1.02 (0.96–1.08) | 0.97 (0.89–1.06) |
| Student | 0.84 (0.71–1.00) | 1.05 (1.01–1.10) | 1.00 (0.92–1.07) | 0.91 (0.84–1.00) | 0.48 (0.27–0.86) | 0.99 (0.93–1.06) | 0.98 (0.90–1.07) |
| Unemployed | 0.98 (0.85–1.12) | 1.00 (0.96–1.04) | - | 1.04 (0.99–1.09) | 1.57 (0.84–2.00) | 0.98 (0.93–1.05) | 0.85 (0.78–0.94) |
| Poverty | |||||||
| Low | 0.98 (0.90–1.07) | 1.03 (1.01–1.06) | 0.97 (0.93–1.02) | 1.01 (0.97–1.05) | 0.65 (0.46–0.91) | 0.94 (0.91–0.98) | 0.91 (0.87–0.95) |
| Mid-low | 1.00 (0.90–1.11) | 0.98 (0.96–1.01) | 0.96 (0.91–1.01) | 1.01 (0.97–1.05) | 1.17 (0.79–1.72) | 1.02 (0.98–1.07) | 0.96 (0.91–1.01) |
| Mid-high | 0.98 (0.88–1.10) | 1.02 (0.99–1.05) | 0.93 (0.87–0.98) | 0.96 (0.92–1.01) | 0.56 (0.37–0.85) | 1.03 (0.98–1.08) | 0.97 (0.91–1.03) |
| High | 0.65 (0.51–0.84) | 1.02 (0.97–1.08) | 1.05 (0.95–1.16) | 0.99 (0.90–1.09) | 0.59 (0.29–1.21) | 1.10 (1.01–1.20) | 0.98 (0.86–1.12) |
| Educational Attainment | |||||||
| Low | 1.06 (0.82–1.36) | 1.04 (0.98–1.11) | 1.03 (0.93–1.14) | 1.02 (0.92–1.13) | 0.71 (0.32–1.59) | 1.04 (0.94–1.14) | 0.98 (0.88–1.10) |
| Mid-low | 1.00 (0.89–1.13) | 1.01 (0.98–1.04) | 0.94 (0.89–1.00) | 1.03 (0.98–1.08) | 0.97 (0.63–1.49) | 1.00 (0.96–1.05) | 0.98 (0.92–1.04) |
| Mid-high | 0.95 (0.87–1.04) | 1.04 (1.01–1.06) | 0.96 (0.92–1.01) | 0.96 (0.92–1.00) | 0.58 (0.41–0.82) | 0.98 (0.94–1.02) | 0.93 (0.89–0.97) |
| High | 0.93 (0.85–1.03) | 0.98 (0.96–1.01) | 0.96 (0.92–1.01) | 1.00 (0.97–1.04) | 0.79 (0.55–1.12) | 1.02 (0.98–1.05) | 0.91 (0.87–0.96) |
| Workplace Categories | |||||||
| Blue-collar | 0.99 (0.85–1.15) | 1.02 (0.98–1.06) | 1.00 (0.93–1.07) | 1.00 (0.94–1.06) | 1.43 (0.81–2.52) | 1.04 (0.98–1.10) | 1.03 (0.95–1.12) |
| White-collar | 0.98 (0.89–1.07) | 1.02 (0.99–1.04) | 0.95 (0.91–0.99) | 0.98 (0.94–1.02) | 0.57 (0.42–0.79) | 1.00 (0.96–1.03) | 0.91 (0.87–0.95) |
Total number of visited places (N); Dwell time at home (Th), work (Tw), and frequently visited places (Tv); Activity entropy (E); Radius of gyration (R); Total travel distance (D)
We did not find statistical differences across different age groups, although a noticeable difference was found among the participants by their occupational status. Decreased working hours were significantly associated with ILS for full-time employees, but not a similar pattern was found for part-time workers and students. In turn, increased dwell time at home and reduced dwell time at FVPs were significant mobility metrics associated with ILS in both students and part-time employees. Lastly, the odds of unemployed and full-time working participants experiencing ILS significantly increased with decreased total travel distance.
We also found that there exist significant differences in the associations between individuals’ mobility and the experiences of ILS by SES of participants. We found that the experience of ILS was significantly associated with increased dwell time at home and a decrease in the radius of gyration among the participants with the lowest poverty level (wealthy neighborhoods), but this association was insignificant among the participants who resided in poor neighborhoods (p < 0.05). Similarly, the total travel distance was negatively associated with the experiences of ILS among the participants with higher educational attainment (OR = 0.91; 95 % CI = 0.87–0.96), but they were not significant for participants with lower educational achievement. Lastly, the mobility patterns of blue-collar workers did not significantly change associated with ILS, whereas the dwell time at work and travel distance significantly reduced for white-collar workers (with a statistically significant difference at a significance level of 0.05).
4. Discussion
We examined associations between individuals’ experience of influenza-like symptoms (ILS) and their routine mobility patterns using both mobile phone-based GPS traces and self-reported health surveys. We matched participants’ mobility patterns quantified by multiple mobility metrics with their self-assessed ILS, and conducted statistical analyses using a time-stratified case-crossover design. The present study is one of a few attempts that have been made to evaluate the changes in individuals’ routine mobility associated with their experience of ILS. Our assessment was based on large-scale data that covered the full cycle of an influenza season, which is rare. Our study further found evidence that the association between mobility and ILS was moderated by individuals’ demographic and socioeconomic characteristics, whereas such effect modification has not been studied sufficiently.
Based on statistical analyses, we identified key mobility metrics inferred from GPS traces that were significantly associated with individuals’ experiences of ILS. These include increased dwell time at home, decreased activity entropy, and shortened travel distance. Our findings on the key mobility metrics suggest mobility data might be useful to improve existing influenza surveillance systems by providing real-time and accurate data on seasonal influenza epidemics. As noted in the previous studies (Lee and Wong, 2014; Yang et al., 2015; Aldridge et al., 2016), traditional surveillance systems often underestimate the actual onset of influenza (or influenza-like illness) because not everyone uses health facilities when he/she experiences ILS. This underutilization of health facilities was also found in our survey on the small percentage of medical visits in response to ILS (Table 2), as well as the statistically insignificant association between the number of health facilities visited (Nd) and ILS (Figure 3). We believe that the use of mobility data has the potential to overcome the discrepancy between hospital record-based surveillance and disease symptoms in public. This is in line with the suggestions from previous studies that used new data sources, such as online search, social media, electronic health records, and crowd-sourced self-reports, to complement the traditional surveillance system and allow reliable real-time estimates of influenza activity (Santillana et al., 2015, 2016; Baltrusaitis et al., 2018). As the availability of individual mobility data increases at a large scale, the accurate inference of influenza illness based on human mobility patterns could provide alternative information for influenza surveillance.
In our stratified analysis, we found that associations between individuals’ ILS and mobility patterns substantially differ by gender. Several mobility metrics representing reduced mobility showed a significant association with ILS among female participants, whereas these were not significant for male participants. Given that ILS-related mobility reduction would be highly dependent upon the severity of the symptom, our findings on the gender differences support the findings of previous studies that symptoms of influenza infection are generally more severe among females (World Health Organization, 2010; Lorenzo et al., 2011; Klein et al., 2012). Although the elderly participants (over 65 years old) are at a greater risk for severe symptoms than other age groups, our results did not indicate any key mobility metric being significant. The routine mobility of this group could be less modifiable than other age groups, but this might be due to its small sample size in that the statistical analysis result for this stratum was highly uncertain. Further investigation is warranted to confirm our findings.
We also found that the reduced dwell time at work was a significant indicator for ILS of full-time employees, but not among part-time workers. According to Bureau of Labor Statistics (2018), approximately 85 to 99 % of full-time employees have access to paid leave, while only 40 to 44 % of part-time employees have the same benefit. Previous studies also showed that workers without access to paid sick leave have a significantly lower probability of calling in sick for influenza illness compared to those with access to paid leave (DeRigne et al., 2016; Piper et al., 2017), which we related to our findings. The statistical analyses also indicated that significantly reduced mobility was associated with ILS among the participants in higher SES, consisting of participants residing in the neighborhood with lower levels of poverty or higher levels of educational attainment, and white-collar workers. That is, our findings on the fact that individuals with high socioeconomic conditions had a higher level of flexibility to modify their mobility when they experience ILS is in line with recent reporting on COVID-19 pandemics where populations with higher SES could decide where to work (home versus workplace) and could afford social distancing (Gauvin et al., 2020; Dueñas et al., 2021; Gozzi et al., 2021; Lee et al., 2021).
We elected not to distinguish mobility patterns observed during weekdays versus weekends based on the results of our preliminary analysis (see Appendix C), where the effect modification by the distinction between weekdays and weekends was not significant. Similarly, we did not include the information on vaccination for influenza among study participants in our analyses due to the relatively short latent period (average 2 days with a range of 1 to 4 days) for influenza symptoms (Hamborsky et al., 2015). Given that about 46% of the participants were vaccinated for influenza throughout the study period, we believe that the effect of vaccination on the short-term mobility changes might have been significant.
The present study has several limitations. First, influenza-like symptoms of participants were based on their self-diagnostics, but not necessarily confirmed by professionals or a medical examination. The findings of our study would be more convincing if the self-reported ILS were validated. Second, participants’ GPS traces contain positional uncertainty from various sources, including the 500 m distance threshold of the iPhone’s significant-change location service. Despite our efforts to minimize the potential bias, some fine-scale mobility metrics might have been affected by the locational error in GPS traces. In addition, we quantified a set of mobility metrics based on Euclidean distance in the present study. To quantify a more realistic measure of mobility, however, a transportation network-based travel distance calculation is warranted. Lastly, our findings were based on weekly surveys and thus not able to capture daily mobility changes. It is possible, thus, that statistical analyses based on daily influenza symptoms and mobility patterns might have led to different results. In summary, we believe that further investigations based on relatively short-term mobility changes associated with the daily onset of influenza-like illness could lead to a better understanding of the relationship between human mobility and individuals’ influenza illness.
5. Conclusion
We assessed the associations between changes in individuals’ mobility patterns and the onset of influenza-like symptoms based on relatively large-scale, fine-grained, individual-level data using a case-crossover design. Our analysis suggests that the incidence of ILS can be inferred from personal location information collected by GPS-enabled mobile phones. Meanwhile, we found that the key mobility indicators significantly associated with symptoms of influenza-like illness, such as increased dwell time at home, decreased number of visited places, shortened travel distance, vary considerably by gender and occupational status. In addition, mobility of the participants in high socioeconomic conditions reduced significantly associated with ILS. Although our findings have implications for public health surveillance, further investigation is warranted to explore the associations between individuals’ mobility patterns and influenza illness at the daily level.
Research Highlights.
We assessed the association between the change in routine mobility and influenza illness.
Reduced and regularized mobility appeared to indicate the onset of influenza illness.
The associations were significantly moderated by gender and socioeconomic status.
People do not necessarily seek for medical care while having influenza-like symptoms.
Individual movement data may complement hospital-based influenza surveillance.
Acknowledgement
This research was supported by the National Institutes of Health [R01GM108731]. The funding organization had no role in study design; collection, analysis or interpretation of data.
Appendix
A. Missing Data Imputation
We collected mobile phone tracking data using the significant-change location service, a motion-triggered system. Thus, the GPS traces entailed missing data around the places where the participants stayed long, and the missing data led to inaccurate inference of mobility patterns. To enhance the data quality by imputing under-reported GPS traces, we first selected two consecutive GPS recordings where the time interval between them was greater than 30 minutes and less than 24 hours if they meet one of three criteria: (1) more than 500 m distant from each other; (2) within the same parcel boundary; or (3) within 500 m from the home, work, and weekly reported FVPs. For the selected GPS recordings, we imputed missing data at a 30-min interval on the firstly recorded location while accounting for moving speed for the last imputed data point. The imputation results significantly improved the performance of quantifying mobility patterns from GPS traces.
B. Neighborhood-level Socioeconomic Status (SES)
We estimated neighborhood-level poverty and educational attainment by merging the home address of each participant with ACS statistics at the census tract level (average population of 3,700; median land area of 2.5 km2). First, we identified the census tract within which participants’ home addresses fall. Next, we calculated the percentage of people below the federal poverty level for each census tract. Lastly, we categorized the census tracts into four quantile groups to represent poverty status in the neighborhood: low (<6%), mid-low (6–11%), mid-high (11–26%), and high (26–64%). We also estimated the neighborhood-level educational attainment by calculating the percentage of people who had not graduated high school among the population over age 25. The census tracts were classified into four quartiles indicating the level of educational attainment: low (15–60%); mid-low (8–15%); mid-high (4–8%); high (<4%). The aforementioned categories of each variable was used to proxy study participants’ neighborhood-level socioeconomic conditions.
C. Sensitivity Analysis: Weekdays versus Weekends
We evaluated the effect of differentiating weekdays from weekends on the association between mobility pattern changes and ILS. Specifically, we calculated mobility metrics, and conducted the time-stratified case-crossover analysis for weekdays and weekends separately. The mobility pattern metrics during the weekdays and weekends were distinguished from each other as found in the literature (Schlich and Axhausen, 2003; Calabrese et al., 2011; Raux et al., 2016). However, the associations between mobility changes and ILS did not show a significant difference between the two temporal periods. Table A.1 demonstrates the OR and 95% CI between a unit increase of each mobility metric and ILS, estimated from the conditional logistic regression models fitted separately for weekdays and weekends. We did not find a statistically significant difference between the associations estimated from weekdays and weekends, except for a more pronounced reduction in travel distance associated with ILS during the weekdays with p < 0.05.
Table A.1:
Estimated association between influenza-like symptoms and a unit increase in mobility pattern metrics by weekdays and weekends.
| Mobility Metrics* | |||||||
|---|---|---|---|---|---|---|---|
| N | T h | T w | T v | E | R | D | |
| Weekdays | 0.96 (0.90–1.02) | 1.01 (1.00–1.03) | 0.96 (0.93–0.98) | 0.98 (0.96–1.01) | 0.62 (0.50–0.79) | 0.99 (0.96–1.01) | 0.93 (0.90–0.95) |
| Weekends | 0.94 (0.88–1.01) | 1.01 (1.00–1.02) | 0.99 (0.96–1.02) | 0.98 (0.96–1.00) | 0.74 (0.60–0.91) | 0.99 (0.98–1.01) | 0.97 (0.95–0.99) |
Total number of visited places (N); Dwell time at home (Th), work (Tw), and frequently visited places (Tv); Activity entropy (E); Radius of gyration (R); Total travel distance (D)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Aldridge RW, Hayward AC, Field N, Warren-Gash C, Smith C, Pebody R, Fleming D, McCracken S, et al. (2016). Are school absences correlated with influenza surveillance data in England? Results from Decipher my Data—a research project conducted through scientific engagement with schools. PLoS One, 11(3):e0146964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apple Inc. (2019). Apple developer documentation. Retrieved June 9, 2020 from https://developer.apple.com/documentation/corelocation/cllocationmanager/1423531-startmonitoringsignificantlocati.
- Baltrusaitis K, Brownstein JS, Scarpino SV, Bakota E, Crawley AW, Conidi G, Gunn J, Gray J, Zink A, and Santillana M (2018). Comparison of crowd-sourced, electronic health records based, and traditional health-care based influenza-tracking systems at multiple spatial resolutions in the United States of America. BMC Infectious Diseases, 18(1):403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa H, Barthelemy M, Ghoshal G, James CR, Lenormand M, Louail T, Menezes R, Ramasco JJ, Simini F, and Tomasini M (2018). Human mobility: Models and applications. Physics Reports, 734:1–74. [Google Scholar]
- Barlacchi G, Perentis C, Mehrotra A, Musolesi M, and Lepri B (2017). Are you getting sick? Predicting influenza-like symptoms using human mobility behaviors. EPJ Data Science, 6(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (2018). Employee benefits in the United States. Retrieved June 9, 2020 from https://www.bls.gov/news.release/pdf/ebs2.pdf.
- Calabrese F, Di Lorenzo G, Liu L, and Ratti C (2011). Estimating origin-destination flows using mobile phone location data. IEEE Pervasive Computing, 10(4):36–44. [Google Scholar]
- Carracedo-Martínez E, Taracido M, Tobias A, Saez M, and Figueiras A (2010). Case-crossover analysis of air pollution health effects: a systematic review of methodology and application. Environmental Health Perspectives, 118(8):1173–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2018a). Past seasons estimated influenza disease burden. Retrieved June 9, 2020 from https://www.cdc.gov/flu/about/burden/past-seasons.html.
- Centers for Disease Control and Prevention (2018b). Summary of the 2016–2017 influenza season. Retrieved June 9, 2020 from https://www.cdc.gov/flu/about/season/flu-season-2016-2017.htm.
- Chang D, Bednarczyk RA, Becker ER, Hockenberry JM, Weiss PS, Orenstein WA, and Omer SB (2016). Trends in US hospitalizations and inpatient deaths from pneumonia and influenza, 1996–2011. Vaccine, 34(4):486–494. [DOI] [PubMed] [Google Scholar]
- Chen K, Breitner S, Wolf K, Hampel R, Meisinger C, Heier M, von Scheidt W, Kuch B, Peters A, Schneider A, et al. (2019). Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. European heart journal, 40(20):1600–1608. [DOI] [PubMed] [Google Scholar]
- DeMers MN (2008). Fundamentals of geographic information systems. John Wiley & Sons. [Google Scholar]
- DeRigne L, Stoddard-Dare P, and Quinn L (2016). Workers without paid sick leave less likely to take time off for illness or injury compared to those with paid sick leave. Health Affairs, 35(3):520–527. [DOI] [PubMed] [Google Scholar]
- Dueñas M, Campi M, and Olmos LE (2021). Changes in mobility and socioeconomic conditions during the COVID-19 outbreak. Humanities and Social Sciences Communications, 8(1):1–10. [Google Scholar]
- Eum Y and Yoo E-H (2021). Imputation of missing daily time-activity data via embedding and stacked long short-term memory network. Computers, Environment and Urban Systems (Under Review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauvin L, Bajardi P, Pepe E, Lake B, Privitera F, and Tizzoni M (2020). Socioeconomic determinants of mobility responses during the first wave of COVID-19 in Italy: from provinces to neighbourhoods. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez MC, Hidalgo CA, and Barabasi A-L (2008). Understanding individual human mobility patterns. Nature, 453(7196):779. [DOI] [PubMed] [Google Scholar]
- Gozzi N, Tizzoni M, Chinazzi M, Ferres L, Vespignani A, and Perra N (2021). Estimating the effect of social inequalities on the mitigation of COVID-19 across communities in Santiago de Chile. Nature communications, 12(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamborsky J, Kroger A, Wolfe S, and Centers for Disease Control and Prevention and others (2015). Epidemiology and prevention of vaccine-preventable diseases. US Department of Health & Human Services, Centers for Disease Control and Prevention, Atlanta, US. [Google Scholar]
- Hayward AC, Fragaszy EB, Bermingham A, Wang L, Copas A, Edmunds WJ, Ferguson N, Goonetilleke N, Harvey G, Kovar J, et al. (2014). Comparative community burden and severity of seasonal and pandemic influenza: results of the Flu Watch cohort study. The Lancet Respiratory Medicine, 2(6):445–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janes H, Sheppard L, and Lumley T (2005). Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology, 16(6):717–726. [DOI] [PubMed] [Google Scholar]
- Klein SL, Hodgson A, and Robinson DP (2012). Mechanisms of sex disparities in influenza pathogenesis. Journal of leukocyte biology, 92(1):67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konty KJ, Bradshaw B, Ramirez E, Lee W-N, Signorini A, and Foschini L (2019). Influenza surveillance using wearable mobile health devices. Online Journal of Public Health Informatics, 11(1). [Google Scholar]
- Lee N, Choi K, Chan P, Hui D, Lui G, Wong B, Wong R, Sin W, Hui W, Ngai K, et al. (2010). Outcomes of adults hospitalised with severe influenza. Thorax, 65(6):510–515. [DOI] [PubMed] [Google Scholar]
- Lee SS and Wong NS (2014). Respiratory symptoms in households as an effective marker for influenza-like illness surveillance in the community. International Journal of Infectious Diseases, 23:44–46. [DOI] [PubMed] [Google Scholar]
- Lee WD, Qian M, and Schwanen T (2021). The association between socioeconomic status and mobility reductions in the early stage of England’s COVID-19 epidemic. Health & Place, 69:102563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy NS, Nguyen TQ, Westheimer E, and Layton M (2013). Disparities in the severity of influenza illness: A descriptive study of hospitalized and nonhospitalized novel H1N1 influenza–positive patients in New York City: 2009–2010 influenza season. Journal of Public Health Management and Practice, 19(1):16–24. [DOI] [PubMed] [Google Scholar]
- Lorenzo ME, Hodgson A, Robinson DP, Kaplan JB, Pekosz A, and Klein SL (2011). Antibody responses and cross protection against lethal influenza A viruses differ between the sexes in C57BL/6 mice. Vaccine, 29(49):9246–9255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowcock EC, Rosella LC, Foisy J, McGeer A, and Crowcroft N (2012). The social determinants of health and pandemic H1N1 2009 influenza severity. American journal of public health, 102(8):e51–e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malig BJ, Pearson DL, Chang YB, Broadwin R, Basu R, Green RS, and Ostro B (2016). A time-stratified case-crossover study of ambient ozone exposure and emergency department visits for specific respiratory diagnoses in California (2005–2008). Environmental health perspectives, 124(6):745–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AC, Singh I, Koehler E, and Polgreen PM (2018). A smartphone-driven thermometer application for real-time population-and individual-level influenza surveillance. Clinical Infectious Diseases, 67(3):388–397. [DOI] [PubMed] [Google Scholar]
- Mingo CA, Martin KR, Shreffler J, Schoster B, and Callahan LF (2014). Individual and community socioeconomic status: impact on mental health in individuals with arthritis. Arthritis, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molinari N-AM, Ortega-Sanchez IR, Messonnier ML, Thompson WW, Wortley PM, Weintraub E, and Bridges CB (2007). The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine, 25(27):5086–5096. [DOI] [PubMed] [Google Scholar]
- Perkins TA, Paz-Soldan VA, Stoddard ST, Morrison AC, Forshey BM, Long KC, Halsey ES, Kochel TJ, Elder JP, Kitron U, Scott TW, and Vazquez-Prokopec GM (2016). Calling in sick: impacts of fever on intra-urban human mobility. Proceedings of the Royal Society of London B: Biological Sciences, 283(1834). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper K, Youk A, James III AE, and Kumar S (2017). Paid sick days and stay-at-home behavior for influenza. PLoS One, 12(2):e0170698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2017). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Raux C, Ma T-Y, and Cornelis E (2016). Variability in daily activity-travel patterns: the case of a one-week travel diary. European Transport Research Review, 8(4):26. [Google Scholar]
- Santillana M, Nguyen A, Louie T, Zink A, Gray J, Sung I, and Brownstein JS (2016). Cloud-based electronic health records for real-time, region-specific influenza surveillance. Scientific Reports, 6:25732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santillana M, Nguyen AT, Dredze M, Paul MJ, Nsoesie EO, and Brownstein JS (2015). Combining search, social media, and traditional data sources to improve influenza surveillance. PLoS Computational Biology, 11(10):e1004513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlich R and Axhausen KW (2003). Habitual travel behaviour: evidence from a six-week travel diary. Transportation, 30(1):13–36. [Google Scholar]
- Schönfelder S and Axhausen KW (2003). Activity spaces: measures of social exclusion? Transport Policy, 10(4):273–286. [Google Scholar]
- Shin S-Y, Kim T, Seo D-W, Sohn CH, Kim S-H, Ryoo SM, Lee Y-S, Lee JH, Kim WY, and Lim KS (2016). Correlation between national influenza surveillance data and search queries from mobile devices and desktops in South Korea. PLoS One, 11(7):e0158539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siła-Nowicka K, Vandrol J, Oshan T, Long JA, Demšar U, and Fotheringham AS (2016). Analysis of human mobility patterns from GPS trajectories and contextual information. International Journal of Geographical Information Science, 30(5):881–906. [Google Scholar]
- Song C, Qu Z, Blumm N, and Barabási A-L (2010). Limits of predictability in human mobility. Science, 327(5968):1018–1021. [DOI] [PubMed] [Google Scholar]
- Talbot HK (2017). Influenza in older adults. Infectious Disease Clinics, 31(4):757–766. [DOI] [PubMed] [Google Scholar]
- Wesolowski A, Buckee CO, Engø-Monsen K, and Metcalf C (2016). Connecting mobility to infectious diseases: the promise and limits of mobile phone data. The Journal of Infectious Diseases, 214(suppl_4):S414–S420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2010). Sex, gender and influenza.
- Xu Y, Belyi A, Bojic I, and Ratti C (2018). Human mobility and socioeconomic status: Analysis of Singapore and Boston. Computers, Environment and Urban Systems, 72:51–67. [Google Scholar]
- Xu Y, Shaw S-L, Zhao Z, Yin L, Fang Z, and Li Q (2015). Understanding aggregate human mobility patterns using passive mobile phone location data: a home-based approach. Transportation, 42(4):625–646. [Google Scholar]
- Yang S, Santillana M, Brownstein JS, Gray J, Richardson S, and Kou S (2017). Using electronic health records and Internet search information for accurate influenza forecasting. BMC infectious diseases, 17(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W, Lipsitch M, and Shaman J (2015). Inference of seasonal and pandemic influenza transmission dynamics. Proceedings of the National Academy of Sciences, 112(9):2723–2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo E-H (2019). How short is long enough?: Modeling temporal aspects of human mobility behavior using mobile phone data. Annals of the American Association of Geographers, 109(5):1415–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo E-H, Eum Y, Roberts JE, Gao Q, and Chen K (2021a). Association between extreme temperatures and emergency room visits related to mental disorders: A multi-region time-series study in New York, USA. Science of The Total Environment, page 148246. [DOI] [PubMed] [Google Scholar]
- Yoo E-H, Pu Q, Eum Y, and Jiang X (2021b). The impact of individual mobility on long-term exposure to ambient pm2.5: Assessing effect modification by travel patterns and spatial variability of pm2.5. International Journal of Environmental Research and Public Health, 18(4):2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo E-H, Roberts JE, Eum Y, and Shi Y (2020). Quality of hybrid location data drawn from GPS-enabled mobile phones: Does it matter? Transactions in GIS, 24(2):462–482. [DOI] [PMC free article] [PubMed] [Google Scholar]


