Abstract
Approximately 25% of patients undergoing transcatheter aortic valve implantation presents significant peripheral arterial disease. The purpose of this case report was to present a feasible approach for transcatheter heart valve in a patient with peripheral arterial disease where the presence of a subclavian stent jutting in the aortic arch made the delivery system passage a challenging procedure.
Keywords: cardiothoracic surgery, cardiovascular disorder
No more limits for TAVI: Severe peripheral arterial disease is no longer a limiting factor for TAVI procedure. The purpose of this case report was to present a feasible and safe approach for THV in a patient with severe peripheral artery disease.

1. BACKGROUND
Transcatheter aortic valve implantation (TAVI) is a well‐recognized treatment option for aortic stenosis in patients with substantial comorbidities. 1 Approximately 25% of patients undergoing TAVI presents significant peripheral arterial disease (PAD) which has been reported as a risk factor for increased procedural complications and worsened clinical outcomes at 1‐year follow‐up. 2 The proper technical planning for a percutaneous procedure should consider and mix cardiac and extracardiac characteristics of the patient, the individual risk of surgery (which is assessed by the judgment of the Heart Team in addition to scores), the feasibility of the TAVI, and local experience. 3 Multimodality imaging is essential for the comprehensive evaluation of the patient and for the correct choice of the procedure access. 4
2. CASE REPORT
We report the case of a 77‐year‐old male patient with symptomatic aortic stenosis. Past medical history includes a prior prostate cancer, chronic obstructive pulmonary disease (COPD), ischemic stroke thrombolysis‐treated, and PAD with prior endarterectomy of the left internal carotid and stenting of the left subclavian artery.
On February 2021, he presented to emergency department complaining syncope. Echocardiography showed a 60% ejection fraction and severe aortic stenosis (AVA 0.6 cm/m2, mean gradient 53 mmHg). Cardiac catheterization revealed a coronary disease of left anterior descending and right coronary arteries treated with stenting. A double antiplatelet therapy was started.
Due to the substantial comorbidities, the patient was elected for transcatheter heart valve (THV) procedure and referred to our department. Preoperative examinations, to plan the safest approach, included a CT scan showing an extensive and multivascular calcified arterial disease (severely calcified aorta and a mild thrombotic vasculopathy of the abdominal aorta). No significant stenoses were reported. Right common femoral artery caliber was appropriate to a transfemoral approach (mean diameter 6 mm). However, the most interesting find was the left subclavian stent jutting in the aortic arch (Figure 1), potentially dangerous for a transfemoral access due to the risk of delivery system hindering or dislocation of the stent itself.
FIGURE 1.

CT scan showed the left subclavian stent jutting in the aortic arch potentially dangerous for a transfemoral access due to the risk of delivery system hindering or dislocation of the stent itself
Therefore, a left transcarotid access was considered and supra‐aortic vessels echo color Doppler ultrasound were performed. Unfortunately, it showed calcification of both common carotid arteries and a 65% right internal carotid stenosis, with a high risk of stroke in case of transcarotid access.
After an accurate evaluation of the CT scan images, the heart team consensus was to attempt THV procedure using a transfemoral access. We have ruled out a transapical approach to avoid mechanical ventilation in a patient with severe COPD. The most challenging aspect of the procedure's planning was how to avoid the subclavian stent dislocation by the delivery system. We decided to stabilize the stent using a 6/30‐mm occlusive balloon inserted through the left radial artery and inflated during the passage of the delivery system (Figure 2A) avoiding any stent dislocation (Figure 2B, Video S1). An Edwards Sapien 29 mm (Edwards Lifesciences, Irvine, California) prosthesis was successfully implanted (Figure 3B, Video S2), after balloon predilation (20/40 mm ZetaMed) (Figure 3A) through angiography‐guided right femoral access. Angiographic (Figure 4, Video S3) and echocardiographic monitoring showed no intraprosthesis regurgitation and low transvalvular gradient.
FIGURE 2.
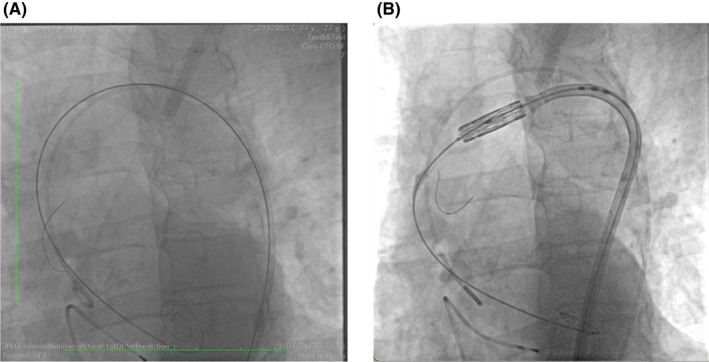
(A) 6/30‐mm occlusive balloon was inserted through the left radial artery and was inflated during the passage of the delivery system. (B) Stent stabilization during the passage of the delivery system, avoiding any stent dislocation
FIGURE 3.
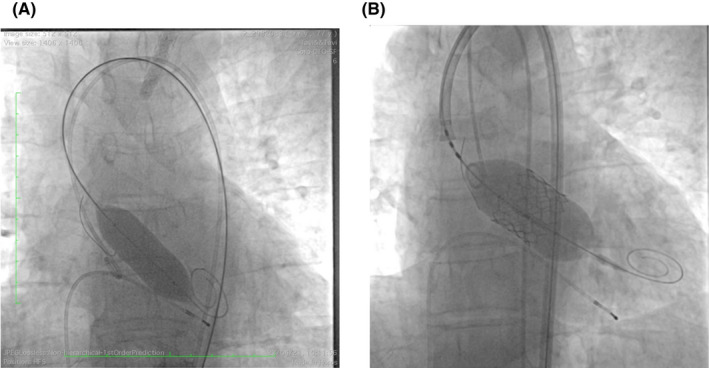
Prosthesis was successfully implanted (B) after balloon predilation (20/40 mm ZetaMed) (A)
FIGURE 4.

Angiographic monitoring showed no intraprosthesis regurgitation and low transvalvular gradient
The patient recovered in five days, and predischarged echocardiography showed a THV mean gradient of 9 mmHg.
At 5 months of follow‐up, the patient presented asymptomatic and in good clinical condition. Echocardiography showed a TVH mean gradient of 10 mmHg.
3. CONCLUSION
Risk factors for aortic valve stenosis have been shown to be similar to atherosclerosis. 5 Consequently, coronary artery disease (CAD) and peripheral vascular artery disease are often found concurrently. The presence of peripheral artery disease not only increases procedural risk but influences also technical approaches. As consequence, an accurate heart team preprocedural evaluation of patients who are candidates for TAVI is mandatory and allows the choice of the best approach for each patient.
The aim of this case report is to present a feasible and safe approach for THV in a patient with severe peripheral artery disease, where a transcarotid access was not possible and the presence of a subclavian stent jutting in the aortic arch made the delivery system passage a challenging procedure.
This is the first case described in literature.
CONFLICTS OF INTEREST
No relationships with industry.
AUTHOR CONTRIBUTIONS
Vittoria Lodo: was the main author. Innocenzo Scrocca and Edoardo Zingarelli: performed the procedure and contributed to the content of the article. Claudio Pietropaolo: carried out anesthesiological management and contributed to the content of the article. Marco Fadde: contributed to the content of the article. Michelangelo Ferri: involved in preoperative planning. Andrea Gaggiano, Gabriella Buono, Giuseppe Musumeci, and Paolo Centofanti: supervised the article and procedure.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Supporting information
Video S1
Video S2
Video S3
ACKNOWLEDGMENTS
All authors contributed significantly to the content of the article. All authors read and approved the submission of the manuscript.
Lodo V, Scrocca I, Zingarelli EM, et al. Another step in transcatheter aortic valve implantation: A challenging transcatheter aortic valve implantation procedure in patient with severe peripheral arterial disease. Clin Case Rep. 2022;10:e05407. doi: 10.1002/ccr3.5407
Funding information
None.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1. Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic‐valve replacement in intermediate‐risk patients. N Engl J Med. 2016;374(17):1609‐1620. doi: 10.1056/NEJMoa1514616 [DOI] [PubMed] [Google Scholar]
- 2. Fanaroff AC, Manandhar P, Holmes DR, et al. Peripheral artery disease and transcatheter aortic valve replacement outcomes: a report from the society of thoracic surgeons/American college of cardiology transcatheter therapy registry. Circ Cardiovasc Interv. 2017;10(10):e005456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Folliguet T, Laurent N, Bertram M, et al. Transcarotid transcatheter aortic valve implantation: multicentre experience in France. Eur J Cardiothorac Surg. 2018;53(1):157‐161. [DOI] [PubMed] [Google Scholar]
- 4. Liu Q, Hahn RT. The role of multimodality imaging in transcatheter aortic valve replacement. Curr Cardiol Rep. 2019;21(8):84. doi: 10.1007/s11886-019-1172-2 [DOI] [PubMed] [Google Scholar]
- 5. Fusini L, Mirea O, Tamborini G, et al. Incidence and severity of atherosclerotic cardiovascular artery disease in patients undergoing TAVI. Int J Cardiovasc Imaging. 2015;31(5):975‐985. doi: 10.1007/s10554-015-0651-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1
Video S2
Video S3
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


