Abstract
Background
Gender-affirming and supportive relations for transgender youth are considered protective in terms of mental health.
Aim
To describe how transgender youth perceived changes in their gender expression, in the course of the gender-affirming path, and the effect of social connectedness and social support on depression and anxiety during the pandemic.
Methods
In this cross-sectional study, transgender youth completed an online survey developed to evaluate the perceived changes in gender expression and affirmation path that occurred during COVID-19 and the age-stratified lockdown. Furthermore, we aimed to investigate the effect of social connectedness and social support on depression and anxiety in this population during the pandemic. The participants completed the following scales: Social Connectedness Scale Revised (SCS-R), Multidimensional Scale of Perceived Social Support (MSPSS), Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI). The effect of lockdown on life conditions, gender expression, social and medical gender-affirming path, social connectedness, social support, depression, and anxiety levels were examined. Linear regression analyses were performed to evaluate the relationships between BDI and STAI scores and other variables.
Outcomes
The relationship between the levels of perceived social connectedness, and social support, the pandemic-related changes in living conditions and depression and anxiety scores were calculated.
Results
A total of 49 transgender youth with a mean age of 20.53 ± 1.86 years were enrolled. Participants reporting discomfort at the place they live and who had difficulties concerning gender expression and affirmation had higher depression and anxiety scores and perceived lower social support from their family. Social connectedness score was a significant negative predictor of depression severity, whereas social connectedness and social support were both significant negative predictors of anxiety severity.
Clinical Implications
Our results show increased adversity for transgender youth when connectedness with supportive people is diminished. During the COVID-19 pandemic, social connectedness and social support perceived by transgender youth are associated with better mental health.
Strengths and Limitations
This is one of the first studies to evaluate the changes that occurred during the COVID-19 pandemic in transgender youth with relation to social support and connectedness, during an age-stratified lockdown. The main limitations were the small study size, skewed gender ratio and that the study sample came from a single gender clinic.
Conclusion
As social connectedness and social support are significant predictors of depression and anxiety severity, special attention is needed to increase contact and support for transgender youth during the pandemic.
Tüzün Z, Başar K, Akgül S. Social Connectedness Matters: Depression and Anxiety in Transgender Youth During the COVID-19 Pandemic. J Sex Med 2022;19:650–660.
Key Words: Gender Dysphoria, Transgender Youth, Social connectedness, Social Support, COVID-19
INTRODUCTION
The COVID-19 pandemic has reached the size of a global disaster and studies have shown it to have a negative impact on the psychological well-being1 and mental health of individuals due to reasons such as its highly contagious potential, lack of treatment, mortality rate, and economic and psychological losses.2 While social support and connectedness help people in dealing with such risky and uncertain situations, diminishing social contact and distancing due to the pandemic are expected to have negative implications over time.
The first officially confirmed coronavirus case in Turkey was on March 11, 2020.3 Afterward, distinct from other countries an age-stratified lockdown was put into action for all children and young people under age 20 (from April 5, 2020 to June 11, 2020) and those older than 65 (from March 21). This age-specific lockdown meant that 40% of the population was kept at home with the aim of decreasing the spread of the virus and protecting the elderly people who were most at risk.4
Social support is the feeling of being a valued member of a social network in which one feels cared for and expects to receive help when in need.5 Many studies have shown that transgender individuals have lower social support than the general population.6, 7, 8 During mass trauma, when a group of people experience the psychological effects of a trauma that was suffered collectively, social support is especially important. A study with a sample from Turkey has shown that for transgender individuals family is an important source of perceived social support, and higher levels of this support are associated with resilience.9 However, for some individuals, the family home can become a place where the person has to struggle to be accepted, recognized, loved, and sometimes maybe dominated by pressure, verbal and physical violence, and hatred.5 , 6 When all family members have to stay at home because of the lockdown and when there is not enough personal space available, one may be more exposed to oppression. Moreover, individuals may not be able to maintain a social connection with those who support them in the extended family, at work, and school due to the pandemic and outbreak-related measures.
Friends are considered as an essential source of social support, especially for sexual and gender minority populations, who do not have common minority status with their family members.10 Studies with transgender people show that psychological resilience, which is the ability to cope with a crisis or to return to pre-crisis status, depends on the relationship with their peers who have similar characteristics.9 , 11 Along with the pandemic and its measures, the interruption of school and work life, the restriction of social interaction means being deprived of an important source of social support for this group. This situation may increase the risk of negative mental consequences of the pandemic in this group. A recent systematic review revealed an increased risk of anxiety and depression in children and adolescents with social isolation and isolation, both at the time of isolation and later in life.12
Besides social support, emerging evidence has implied that social connectedness is an important source of psychological wellbeing and a useful instrument in affirming one's identity for transgender youth.13 , 14 Social connectedness is considered as an internal sense of closeness toward the social world including relationships with family, friends, community, schools, and neighborhoods.15 , 16 Emerging evidence has suggested that social connectedness has an impact on the wellbeing of LGBT youth and adults.17 , 18 Consequently, it is expected that the maintenance of social connectedness with supporting individuals during the pandemic period will have protective effects in terms of mental strain. However, the measures for “social distancing” made social connectedness very difficult and it took an extra effort to maintain and protect it.
This study aimed to examine how transgender youth perceived changes in their gender expression, in the course of the gender-affirming path, and specifically investigate the effect of social connectedness and social support on depression and anxiety in transgender youth during the pandemic. We believed that evaluating the effects of the break from school and/or work, the deprivation of social relations with peers, and being confined at home will provide us with an understanding of what these young people need during the pandemic period and the methods to be considered during the follow-up period.
METHODS
Participants and Procedure
At Hacettepe University individuals presenting with gender identity-related issues are evaluated by a multidisciplinary team and are assessed with clinical interviews performed by experienced mental health professionals. For individuals younger than 18 the intake interview is conducted at the division of Adolescent Medicine, all individuals are routinely evaluated and followed at the Department of Psychiatry. Youth between the ages of 16–24 years, who met DSM 5 criteria for Gender Dysphoria (GD) and were followed during the year preceding the outbreak of the pandemic were eligible for the study. The Institutional Review Board at Hacettepe University approved the study (GO 20/481).
Participants and parents of participants under 18 years were contacted by telephone and given information concerning the study. Online written consent was obtained from all participants 18 years of age and older. Online written assent and parental consent were obtained for participants under the age of 18. Then the online survey was sent to those who accepted participation.
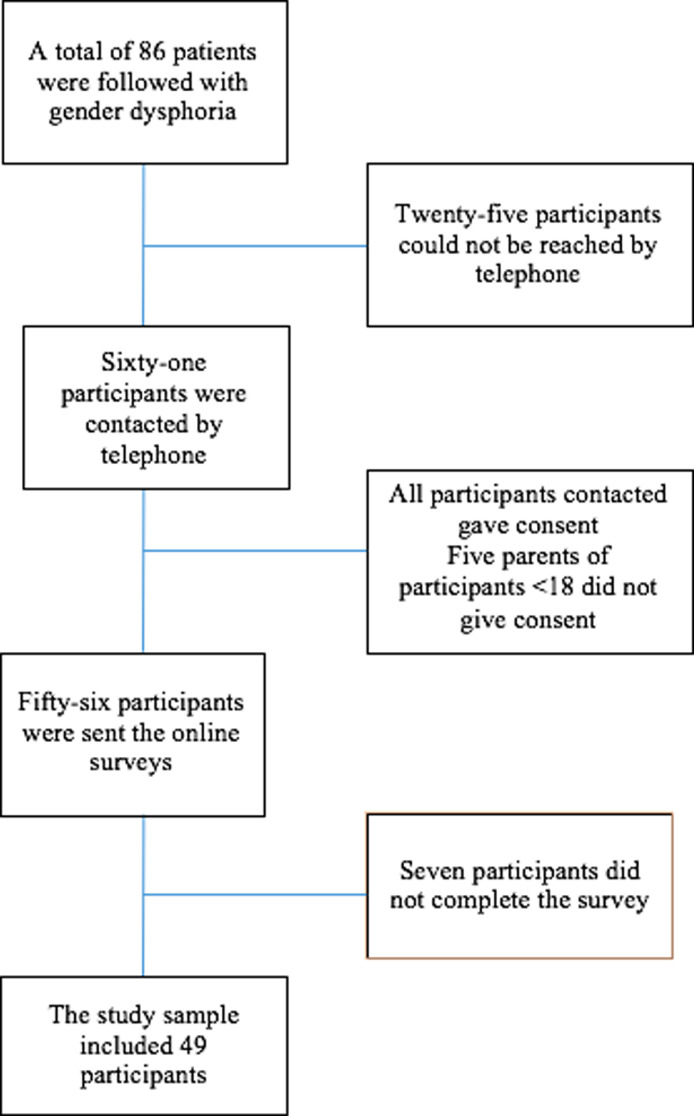
A total of 86 youth were followed between March 2019 and March 2020 for GD and an attempt was made to contact all eligible individuals. As a result, the study sample included 49 individuals. The participants (n = 49) and non-participants (n = 37) were not significantly different for age (U = 827.0, z = −0.701, P = .483) and gender distribution (X2 = 0.850, df = 1, P = .356). Participants were excluded from the study if the surveys were not fully completed or consent was not obtained. A flow chart of study participation has been given in Figure 1 . The survey was administered between June 1st and 30th which was during the lockdown.
Figure 1.
Flow of participants.
Measures
The first part of the online survey, which was developed by researchers, included demographic information, questions related to GD and gender-affirming path, the effects of COVID-19, the public health measures (such as age stratified lockdown, interruption of school etc.) and individual precautions (such as staying at home) gender expression, gender-affirming path, social relationships, and general well-being. Demographic variables included educational and/or occupational status, where and with whom they live and how those conditions were affected by the pandemic, sex assigned at birth and gender identity. Questions related to GD and gender-affirming path included the disclosure of gender identity to family/friends, use of chosen name and clothes considered congruent with the gender identity by the individual in family/friends/school or work environment and how those changed during the pandemic and lockdown period. The questionnaire also included current status related to medical gender-affirming path processes, history of surgical interventions, the use of non-surgical procedures, and whether access to gender care was affected during the COVID-19 pandemic period. They were also asked to report how they felt during the lockdown period, how they handled being isolated from their friends and partners, and how they connected with them. The survey questions that were not open-ended and required participants’ rating were rated using a five-point Likert type scale ranging from 1 (never) to 5 (too much) and from 1 (strongly disagree) to 5 (strongly agree).
Study Measurement Tools
The following measurement tools were conducted on all participants:
-
a)
Social Connectedness Scale-Revised (SCS-R) is a self-report measure that consists of 20 items that evaluate the participant's degree of experiencing a sense of closeness with others in interpersonal contexts and one's experience of distance and isolation from others.19 The scale was asked to be answered in consideration of the pandemic period. Participants rate items using a six-point Likert-type scale ranging from 1 (strongly disagree) to 6 (strongly agree). Ten items are negatively worded and the remaining items are positively worded. Higher scores indicate a strong sense of social connectedness. The range of total points is 20 to 120. The scale was adapted to the Turkish population by Sarıçam and Deveci20 and Cronbach's alpha internal consistency was reported as 0.86. The authors have found a significant negative correlation with loneliness measures. In the present sample, Cronbach's alpha coefficient was calculated as 0.93.
-
b)
Multidimensional Scale of Perceived Social Support (MSPSS) was developed by Zimet et al.21 It is a 12 item self-report scale designed to measure perceived social support from 3 sources: family, friends, and a significant other. Each item is rated using a seven-point Likert-type scale. Four items in each subscale give a subscale score and by adding all subscale scores a total score can be obtained. The range of total points is 12 to 84. Higher scores indicate that perceived social support is high. The psychometric properties for the Turkish population were examined by Eker and Arkar.22 The Cronbach's alpha internal consistency coefficients were reported between 0.80 and 0.95. The authors have reported that MSPSS correlated in the expected direction with measures of loneliness, negative social interaction and a symptom checklist. In the present sample, Cronbach's alpha coefficient was calculated as 0.91.
-
c)
Beck Depression Inventory (BDI) is a widely used 21 item self-report inventory that aims to evaluate the presence of the symptoms of depression.23 The psychometric properties of the instrument (1978 version) were examined in the Turkish population by Hisli24 and Cronbach's alpha was reported as 0.74. In the present sample, Cronbach's alpha coefficient was calculated as 0.90.
-
d)
State-Trait Anxiety Inventory (STAI) is also a widely used 2-scale inventory that provides a separate measure for both state (STAIState, specific to the time of test assessment) and trait (STAITrait, general feeling) anxiety.25 Each scale consists of 20 items that assess the presence of anxiety symptoms. The validity and reliability for the Turkish population were examined by Oner and LeCompte,26 and the inventory have been used in various studies with both healthy and clinical populations. In the present sample, Cronbach's alpha coefficient was calculated as 0.92 for STAIState, 0.88 for STAITrait measures.
Statistical Analysis
Analyses were performed with SPSS version 22.0.27 Descriptive statistics included mean and standard deviation (SD) or median (interquartile range and minimum to maximum). Normal distribution for each variable was checked using statistical (Kolmogorov-Smirnov test, the ratio of standard deviation to mean value, skewness, and kurtosis) and graphical methods (histogram, detrended normal plot). Most of the variables failed in at least some tests of normality. Therefore, nonparametric tests were used in the analyses. Two-tailed Mann-Whitney U-test was used to examine differences in demographic, gender-affirming path related features of the participants and the effect of the COVID-19 pandemic on life conditions, gender expression and social connectedness, social support, depression, and anxiety levels. Spearman correlation was used for analyses of bivariate correlation. Multiple linear regression analyses (enter method) were used to evaluate the relationship between BDI and STAIState scores and other variables. In these analyses, BDI and STAIState scores were considered as dependent variables in two separate analyses; age, gender (binary coded), perceived social support (MSPSS score), and social connectedness (SCS-R score) were included in the analyses as independent variables. In both models, residuals were analyzed for normal distribution; also, bivariate correlations between the residuals and the independent continuous variables included in the models (age, social support, and social connectedness test scores) and the difference between the groups based on the categorical independent variable included in the models (gender) were assessed. Residuals in both models were normally distributed, there was no significant correlation with the variables and the residual values, and the residuals were not different between gender groups. These analyses did not suggest a violation of the assumptions for multiple regression.
A P value < .05 was considered statistically significant in correlation analyses and single comparisons. There are many techniques for correcting the significance level of hypothesis testing that requires multiple comparisons. Since Bonferroni correction is very conservative when the number of comparisons becomes large and when the tests are not independent (eg, as in medical imaging), some alternative approaches have been proposed to make the correction less stringent. One of the methods proposed by Machado28 presented a suitable solution for dealing with high-dimensional problems. This proposed method is a new method for computing the effective number of independent variables used to adjust significance values in multiple comparison testing. The model proposed for computing the number of independent variables is derived from the interpretation of eigen decomposition, that aims at obtaining a lower-dimensional variable space for the problem, in which the new variables (principal components) are uncorrelated.28
The number of independent variables, m, is given as
| (1) |
where n is the number of test, I is the indicator function that returns 1 when the argument is true or 0 otherwise and λi is eigen value.
In our study, using the 8 different scales, the number of eigenvalues, greater than or equal to 1, were determined as 2 by using principal component analysis. The effective number of independent variables, m, computed from Eq. 1., was 3.935. Thus, for multiple comparisons adjusted significance threshold, α was 0.013.
RESULTS
Demographic and Gender-Affirming Path Related Features
The mean age of the study sample (n = 49) was 20.53 (SD = 1.86), genders were not equally represented (83.7% were assigned female at birth). A majority of the participants (91.8%) lived with their families and 98.0 % had already disclosed their gender identity to them. Half of the participants (51.0 %) reported that their family members were using their chosen name, whereas families of 38.8 % used their given name and 10.2 % declared that they had not yet chosen a name. For the majority of the participants (83.7 %), their friends were using their chosen name. Twenty-three (46.9%) individuals reported that they currently had a romantic partner. Of the 22 (44.9%) participants who were using gender-related medical treatments, 3 of them were using a gonadotropin-releasing hormone analogue for puberty suppression and 19 were on gender-affirming hormone treatment. Twelve participants (24.5%) had a history of gender-affirming surgical intervention which was top surgery in all cases. The demographic and gender-affirming path related features of the participants are presented in Table 1 .
Table 1.
Demographic and gender-affirming path-related features of the participants before the pandemic
| N (%) | |
|---|---|
| Final educational attainment | |
| Primary school | 1 (2.0) |
| Secondary school | 6 (12.2) |
| High School | 35 (71.4) |
| University or higher | 7 (14.3) |
| With whom they live | |
| Family | 45 (91.8) |
| Alone | 2 (4.1) |
| Friends | 2 (4.1) |
| Coming out as trans (+) | |
| To family | 48 (98) |
| To friends | 48 (98) |
| At school/work | 45 (91.8) |
| Chosen name (+) | 44 (89.8) |
| Chosen clothes (+) | |
| Alone/home | 42 (85.7) |
| Home with family | 43 (87.8) |
| School/work place | 43 (87.8) |
| In public | 45 (91.8) |
| Medical treatment (+) | 22 (44.9) |
| Gender-affirming hormone treatment | 19 (86.3) |
| GnRHa | 3(13.6) |
| Surgical intervention (+) | 12 (24.5) |
GnRHa = Gonadotrophin releasing hormone agonist; SD = standard deviation.
(+): Present.
Change in Daily Life With the Pandemic
A majority of participants were students (n = 34, 69.4%) and during the COVID-19 pandemic 26 (76.5%) of them were able to continue their education online, 8 (23.5%) could not. Five of the participants (10.2%) reported that they continued to work. There were 11 (22.4%) participants who had to change the place they lived because of the pandemic. Thirteen participants (26.5%) reported discomfort to a degree by the place they currently resided, in addition, 42 (85.7%) reported at least one person within the household they didn't like being together with. The mean level of difficulty experienced by the participants in continuing their work or education was 3.04 (±0.21) on a scale of 1–5, where increasing scores indicated higher difficulty. Due to the pandemic or pandemic-related precautions, 22 (44.9%) reported difficulty in sleeping, 14 (28.6%) reported food insecurity (being without reliable access to a sufficient quantity of affordable, nutritious food) and 24 (29%) had difficulties participating in sports or similar physical activities. On a scale of 1–5, where increasing scores indicated severity, the mean level of fear/anxiety concerning having COVID-19 and any relatives contracting COVID-19 were 2.5 (±0.17) and 3.63 (±0.19), respectively.
Impact of the Pandemic on Medical and Social Gender-Affirming Path
The findings concerning the level of experienced difficulty and change compared to the period before the pandemic concerning the medical and social gender-affirming path are presented in Table 2 . On a scale of 1–5, the mean rate of anticipation of disruption in their plans for gender-affirming hormone treatment due to the pandemic was 4.06 (±0.21), and 3.57 (±0.23) with regards to their plans for gender-affirming surgical interventions. These scores were higher than the levels of difficulty experienced during COVID-19 by the participants in these domains (1.96 ± 0.26 for hormone treatment, 2.42 ± 0.30 for surgical interventions, Table 2).
Table 2.
The effects of the pandemic on the difficulty related to medical and social gender-affirming path
| Severity (rated 1–5) Mean (SD) | Change that occurred with the pandemic n (%) | |
|---|---|---|
| Gender-affirming hormone treatment | 1.92 (0.26) | |
| Gender-affirming surgical interventions | 2.42 (0.30) | |
| Nonmedically assisted gender-affirming procedures (such as binding, tucking, hair removal etc.) | 2.12 (0.21) | |
| Using chosen name with the family (n = 44)* | 2.12 (0.22) | Less/None 32 (72.7) More 12 (27.3) |
| Using chosen name with friends (n = 46)* | 1.15 (0.06) | Less/None 41 (89.1) More 5 (10.9) |
| Wearing chosen clothes when alone (n = 47)* | 1.57 (0.17) | Less/None 39 (83) More 8 (17) |
| Wearing chosen clothes with the family (n = 47)* | 1.50 (0.15) | Less/None 41 (87.2) More 6 (12.8) |
| Overall gender expression (n = 49) | 4.00 (0.16) | Less/None 36 (73.5) More 13 (26.5) |
SD = standard deviation.
Participants who could perform the particular gender-affirming path-related action before the pandemic.
Impact of the Pandemic on Social Relations
The effects of COVID-19, the public health measures and individual precautions against the pandemic on social relationships were evaluated. Results are presented in Table 3 .
Table 3.
Effect of COVID-19 on social connectedness with whom the participant is in a gender-affirming, supportive relationship
| Change with the pandemic n (%) | |
|---|---|
| Any family member (n = 40)* | Less/None 34 (85) More 8 (20) |
| Friends (n = 46)* | Less/None 28 (60.9) More 18 (39.1) |
| Friends from the SGM community (n = 36)* | Less /None 26 (72.2) More 12 (33.3) |
| Partner (n = 23)* | Less/None 10 (43.5) More 13 (56.5) |
SGM = sexual orientation or gender minority.
Participants who report the presence of this kind of relationship before the pandemic.
Life Changes Impact on Depression and Anxiety Severity and Social Support
The median scores of SCS-R, MSPSS, BDI, and STAI and correlations among them are given in Table 4 . None of the scale scores correlated with age, and there was no significant difference between those younger and older than 20 years (P < .05). In addition, the scores of SCS-R, MSPSS, BDI, and STAI were not different with respect to sex assigned-at-birth (P < .05).
Table 4.
Median scores and bivariate correlations among SCS-R, MSPSS, BDI, and STAI
| Scale | Median (IQR) | SCS-R | MSPSSTotal | MSPSSFamily | MSPSSFriend | MSPSSOther | BDI | STAITrait | STAIState | |
|---|---|---|---|---|---|---|---|---|---|---|
| SCS-R | 79 (35.0) |
rs P |
- | 0.696 <0.001 |
0.519 <0.001 |
0.764 <0.001 |
0.359 0.011 |
−0.640 <.001 | −0.697 <.001 | −0.643 <.001 |
| MSPSSTotal | 63 (23.5) |
rs P |
- | 0.770 <0.001 |
0.716 <0.001 |
0.740 <0.001 |
−0.504 <.001 | −0.642 <.001 | −0.627 <.001 | |
| MSPSSFamily | 22 (12.5) |
rs P |
- | 0.402 0.004 |
0.368 0.009 |
−0.624 <.001 | −0.585 <.001 | −0.698 <.001 | ||
| MSPSSFriend | 23 (9.5) |
rs P |
- | 0.342 .016 |
−0.377 .008 | −0.557 <.001 | −0.488 <.001 | |||
| MSPSSOther | 20 (15.0) |
rs P |
- | −0.148 .309 | −0.346 .015 | −0.261 .070 | ||||
| BDI | 14 (16.0) |
rs P |
- | 0.757 <.001 | 0.806 <.001 | |||||
| STAITrait | 46 (13.5) |
rs P |
- | 0.821 <.001 | ||||||
| STAIState | 44 (15.0) |
rs P |
- |
BDI = Beck Depression Inventory; IQR = Interquartile range; MSPSS = Multidimensional Scale of Perceived Social Support; SCS-R = Social Connectedness Scale-Revised; STAI = State-Trait Anxiety Inventory; rs = Spearman's correlation.
There was no significant difference in any scale scores between the participants with respect to the interruption of school or work. There was no difference in the scale scores between the participants who lived with their families and those who did not (n = 4). Those who had to change the place they lived due to the pandemic had similar scores; however, the participants who reported some degree of discomfort about the place they currently live had higher BDI (U = 119, P = .009) and STAIState (U = 97.5, P = .002) scores. Being uncomfortable related to the place they lived was associated with lower scores in MSPSSFamily (U = 86, P = .001).
Effects of the Gender Expression, Social Relations, and Gender-Affirming Path Related Difficulties on Depression and Anxiety Severity, Social Support, and Connectedness
During the pandemic, with regards to anxiety and depression symptom severity, and perceived social support there was no significant difference between participants who reported an increase in the difficulty experienced related to using their chosen name and wearing the clothes they choose and those who did not within the family. However, the participants who could maintain communication with gender-affirming and supportive family members had higher MSPSSFamily (U = 74, P = .005) scores.
Participants who had friends with similar sexual orientation and gender minority status had higher MSPSSFriends (U = 118.5, P = .008) scores. However, there was no significant difference in depression and anxiety symptom severity between those who had greater difficulty (n = 9) and no change (n = 21) in communicating with these peers during the pandemic.
Those who had a partner had significantly higher MSPSSOthers (U = 107, P = .001). With regards to depression and anxiety symptom severity, there was no significant difference between those who had difficulties in communicating with their partner (n = 13) and those who said there was no change (n = 10) during the pandemic.
Participants who were on hormone treatment reported significantly higher belief that they could express their gender identity during the pandemic, compared to those who did not use hormones (U = 170.5, P = .007). The level of perceived difficulty with maintaining hormone therapy during the pandemic (n = 27) inversely correlated significantly with SCS-R (r = −0. 381, P .05), MSPSSFamily (r = −0.420, P .029), and MSPSSFriends (r = −0.482, P .011) scores. There was no such relationship regarding the difficulties associated with surgical interventions during the pandemic. There was no significant relationship between the severity of the concern that hormone and surgical procedures will be interrupted in the future due to the pandemic and any scale scores.
During the pandemic the level of difficulty experienced by participants concerning procedures performed by the individual without the need for medical assistance to make their bodies appear more congruent with their gender identities (such as hair removal or chest-binding) significantly correlated (r = −0.418, P = .003) with the belief that they could express their gender identity.
Predictors of Depression and Anxiety Severity
Two multiple linear regression analyses were employed to develop models for predictors of the participants’ depression and anxiety symptom severity (dependent variables; BDI and STAIState scores, respectively) by age, gender, perceived social support (MSPSS score), and social connectedness (SCS-R score). Significant regression equation was found for both depression (F (4, 44) = 8.176, P < .001, R2 = 0.426, Durbin- Watson value = 2.35) and anxiety (F (4, 44) = 9.166, P < .001, R2 = 0.455, Durbin- Watson value = 2.05) severity. The findings are presented in Table 5 . Analyses indicated that social connectedness was a significant negative predictor of depression symptom severity (t = −3.763, P < .001), social connectedness (t = −2.334, P = .024) and social support (t = −2.224, P = .031) were significant negative predictors of anxiety severity.
Table 5.
Multiple regression analyses predicting anxiety and depression severity of the participants (N = 49)
| Multiple linear regression |
||||
|---|---|---|---|---|
| Independent variables | B (SE) | β | P | |
| BDI | (constant) | 57.075 (15.221) | .001 | |
| R2= 0.426 | Age | −0.625 (0.682) | −0.105 | .365 |
| F4,44 = 8.176 | Gender | −2.017 (3.423) | −0.068 | .559 |
| P = .<001 | MSPSSTotal | −0.018 (0.108) | −0.027 | .871 |
| 42.6 % | SCS-R | −0.320 (0.085) | −0.613 | <.001 |
| STAIState | (constant) | 76.992 (14.611) | <.001 | |
| R2= 0.455 | Age | −0.113 (0.655) | −0.019 | .863 |
| F4,44 = 9.166 | Gender | −0.580 (3.285) | −0.020 | .861 |
| P < .001 | MSPSSTotal | −0.231 (0.104) | −0.355 | .031 |
| 45.5 % | SCS-R | −0.191 (0.082) | −0.371 | .024 |
β: Standardized B coefficient; SE: standard error; BDI: Beck Depression Inventory; STAI: State-Trait Anxiety Inventory; MSPSS: Multidimensional Scale of Perceived Social Support
These significant associations persisted when difficulty in gender expression during the pandemic and gender-affirming hormone/gonadotropin-releasing hormone analogue use were included into the models as dependent variables (for depression, F (6, 42) = 5.126, P < .001, R2 = 0.423, Durbin-Watson value = 2.04; for anxiety, F (6, 42) = 6.142, P < .001, R2 = 0.467, Durbin- Watson value = 1.95).
DISCUSSION
To the best of our knowledge, this is one of the first studies to examine the depression and anxiety symptom severity in transgender youth with relation to perceived social support and connectedness, during an age-stratified lockdown and the COVID-19 pandemic. Transgender youth may be especially vulnerable to the psychosocial impact of the pandemic, since a pre-existing fragile social support system may be disrupted during times of crisis. We found that lower social support and a weaker sense of social connectedness are predictors of depression and anxiety severity.
The pandemic has been shown to have a negative impact on youth mental health, particularly leading to increased anxiety and depression in adolescents.29 Gonzales et al30 reported that 60% of their LGBT college student sample were experiencing anxiety and depression during the COVID-19 pandemic. Similarly, Kidd et al31 found that psychological distress was higher during the pandemic compared to pre-pandemic period among transgender and nonbinary adults. The psychological impact of COVID-19 has been reported to vary with some variables associated with the risk of infection, but some identity-related features appear to be associated with worse outcomes.32 Suen et al33 reported that sexual minority specific stressors contributed significantly to the variance in anxiety and depression in an LGB sample. Previous research shows that depressive and anxiety symptoms, self-harm behavior and suicide attempts are observed with high rates among transgender youth.34 , 35 The minority stress model suggests that the prejudice and discrimination-related stress experienced by sexual and gender minority groups contribute to the poor mental health outcomes reported in these groups.36
In our sample, the perceived level of social support is inversely correlated with depression and anxiety. In further multivariable analysis, higher social support was found to be a significant predictor of lower anxiety. Similar to the general population, social support is considered an important source of psychological resilience in transgender people, furthermore, it is proposed to have a protective role against the mental health impact of adverse life events including minority stress.8 , 37 , 38 Our findings support earlier evidence on the effectiveness of social support in dealing with the stressors experienced by transgender youth.
This study has shown that similar to social support, social connectedness also has an impact on the mental health of transgender youth during the pandemic. Sense of social connectedness predicted both depression and anxiety levels in the sample, despite the inclusion of social support in the analysis. Social connectedness can be conceptualized as the actualized part of social support, like the actual level of connection and relation with their social network. In a prospective study on adolescent mental health during COVID-19, feeling socially connected was found to be a protective factor against poor mental health during follow-up.39 Although we did not know the pre-pandemic status of our participants in terms of the analyzed variables, when we consider this in the context of the pandemic and lockdown lower levels of perceived social support and sense of connectedness were associated with negative mental health consequences.
The COVID-19 pandemic has meant a mandatory lockdown for our participants’ age group. In addition to the general sense of social connectedness, in our sample, we studied the maintenance of connectedness by transgender youth with gender-affirming and supportive individuals. We found that participants who were able to continue to communicate with family members with whom they feel close to, reported significantly higher levels of social support. According to an earlier study during the COVID-19 pandemic, LGBT students who were living with unsupportive families reported a higher amount of psychological distress compared with families supporting the LGBT status.30 Regarding the relationships with friends, participants who had close friends with similar gender minority status reported higher levels of social support. Kidd et al31 similarly reported that decreased transgender and gender nonbinary community support is associated with psychological distress during the pandemic. In terms of family and peer support and connectedness, failure in communication decreases the sense of connectedness and as well as perceived support. The present findings confirm that family and friends are essential sources of support8 , 40 and also show the crucial importance of strengthening these support resources. Fish et al41 showed the importance of online support programs for LGBTQ youth during the COVID-19 pandemic. It is understood that although existing stressors are present, transgender youth can benefit from maintaining connectedness with online mechanisms. Considering the initial negative reactions following the disclosure of the gender incongruence, the families of transgender youth may benefit from the provision of assistance and guidance on how they can accept and support transgender youth.42
During the pandemic, many gender diverse youth have experienced a delay in the course of gender-affirming medical procedures and may have even been told that these interventions can wait or are elective.43 , 44 Similarly, in our study, the pandemic also interfered with access to gender-affirming medical care and treatment. Those participants who reported perceived difficulties with hormone therapy during the pandemic also had a weaker sense of connectedness and lower social support from family and friends. Social support and connectedness may provide the means to overcome the interruptions in access to hormone therapy for some participants. Another possible interpretation is that those lacking support and connection may process similar difficulties with greater apprehension. Gender-affirming treatments have consistently been shown to improve the physical and mental health of gender diverse youth45 and thus it is of great importance that these treatments be prioritized during the pandemic.
This study has certain limitations. First, while our target and study sample were not significantly different for age and gender distribution, the final sample is relatively small with a response rate of 60%. Second, we did not assess if the participants experienced domestic violence because of their gender identity and/or gender expression, which may be correlated with anxiety and depression scores. The assessments in this study consisted of self-report instruments which bear the possibility of social desirability. Additionally, the fact that the study sample consists of individuals followed in a single gender clinic and only one hospital limits generalizability. Finally, pre-pandemic scores of the analyzed variables were unknown and as baseline scores were unavailable it is difficult to solely attribute these results to the effects of the pandemic. Further research is required to address these limitations.
CONCLUSION
In conclusion, this study has shown that during the pandemic failure in access to supportive peers and family members, lower social support and a weaker sense of social connectedness are associated with depression and anxiety in transgender youth. Although it is not possible to suggest that the associations between social connectedness and support and mental health indices are limited to the pandemic period based on our findings, the present findings indicate the necessity for precautions against mental health consequences considering the possibility of prolonged pandemic practices. Mental health professionals should recognize the importance of enhancing means of social support for trans youth, especially from their friends, assisting them in finding alternative ways to maintain connectedness during the pandemic. Additionally, they should work with the families of transgender youth on understanding their difficulties and becoming more affirming. Furthermore, our findings highlight the need for improving and prioritizing access to gender-affirming medical care for trans youth during the pandemic.
Statement of Authorship
Zeynep Tüzün: Conceptualization, Methodology, Investigation, Writing- Review & Editing; Koray Başar: Conceptualization, Methodology, Investigation, Formal Analysis, Writing- Review & Editing; Sinem Akgül: Conceptualization, Methodology, Writing-Review & Editing.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
REFERENCES
- 1.McPherson KE, McAloney-Kocaman K, Mc Glinchey E, et al. Longitudinal analysis of the UK COVID-19 psychological wellbeing study: trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiatric Res. 2021;304 doi: 10.1016/j.psychres.2021.114138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- 3.T.C. Sağlık Bakanlığı. T.C. Sağlık Bakanlığı Korona tablosu. Available at: https://covid19.saglik.gov.tr/ Accessed April 24, 2020.
- 4.Kanbur N., Akgül S. Quaranteenagers: a single country pandemic curfew targeting adolescents in Turkey. J Adolesc Health. 2020;67:296–297. doi: 10.1016/j.jadohealth.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor, SE. “Social support: a review, oxford library of psychology” in The Oxford handbook of health psychology. ed. H. S. Friedman (New York: Oxford University Press), 2011;189–214.
- 6.Başar K, Yüksel Ş. Çocukluktan yetişkinliğe cinsiyet kimliği ile ilgili sorunlar: uygun değerlendirme ve izlem. Psikiyatride Güncel. 2015;4:389–404. [Google Scholar]
- 7.Bariola E, Lyons A, Leonard W, et al. Demographic and psychosocial factors associated with psychological distress and resilience among transgender individuals. Am J Public Health. 2015;105:2108–2116. doi: 10.2105/AJPH.2015.302763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaptan S, Cesur E, Başar K, et al. Gender dysphoria and perceived social support: a matched case-control. J Sex Med. 2021 doi: 10.1016/j.jsxm.2021.01.174. [DOI] [PubMed] [Google Scholar]
- 9.Başar K, Öz G. Resilience in Individuals with Gender Dysphoria: Association with Perceived Social Support and Discrimination. Turk Psikiyatri Derg. 2016;27:225–234. [PubMed] [Google Scholar]
- 10.Budge SL, Katz-Wise SL, Tebbe EN, et al. Transgender emotional and coping processes: facilitative and avoidant coping throughout gender transitioning. Couns Psychol. 2013;41:601–647. doi: 10.1177/0011000011432753. [DOI] [Google Scholar]
- 11.Başar K, Öz G, Karakaya J. Perceived discrimination, social support, and quality of life in gender dysphoria. J Sex Med. 2016;13:1133–1141. doi: 10.1016/j.jsxm.2016.04.071. [DOI] [PubMed] [Google Scholar]
- 12.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austin A, Goodman R. The impact of social connectedness and internalized transphobic stigma on self-esteem among transgender and gender non-conforming adults. J Homosex. 2017;64:825–841. doi: 10.1080/00918369.2016.1236587. [DOI] [PubMed] [Google Scholar]
- 14.DiFulvio GT. Sexual minority youth, social connection and resilience: from personal struggle to collective identity. Soc Sci Med. 2011;72:1611–1617. doi: 10.1016/j.socscimed.2011.02.045. [DOI] [PubMed] [Google Scholar]
- 15.Lee RM, Robbins SB. The relationship between social connectedness and anxiety, self-esteem and social identity. J Couns Psychol. 1998;45:338–345. [Google Scholar]
- 16.Lee RM, Robbins SB. Understanding social connectedness in college women and men. J Couns Dev. 2000;78:484–491. [Google Scholar]
- 17.Ceatha N, Mayock P, Campbell J, et al. The power of recognition: a ualitative study of social connectedness and wellbeing through LGBT sporting, creative and social groups in Ireland. Int J Environ Res Public Health. 2019;16:3636. doi: 10.3390/ijerph16193636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia J, Vargas N, Clark JL, et al. Social isolation and connectedness as determinants of well-being: global evidence mapping focused on LGBTQ youth. Global Public Health. 2019 doi: 10.1080/17441692.2019.1682028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee RM, Draper M, Lee S. Social connectedness, dysfunctional interpersonal behaviors and psychological distress: testing a mediator model. J Couns Psychol. 2001;48:310–318. doi: 10.1037/0022-0167.48.3.310. [DOI] [Google Scholar]
- 20.Sarıçam H, Deveci M. Revize edilmiş sosyal bağlılık Ölçeğinin psikometrik özellikleri. 1.Uluslararası sosyal beşeri ve eğitim bilimleri kongresi. İstanbul, Türkiye 2017;197-198. doi:10.13140/RG.2.2.24940.87688.
- 21.Zimet GD, Dahlem NW, Zimet SG, et al. Multidimensional scale of perceived social support. J Pers Assess. 2018;5:30–41. [Google Scholar]
- 22.Eker D, Arkah H. Çok boyutlu algılanan soayal destek Ölçeği'nin faktör yapısı, geçerlik ve güvenirliği. Türk Psikoloji Dergisi. 1995;10:17–25. [Google Scholar]
- 23.Beck AT, Ward C, Mendelson M., Mock J, Erbaugh J. An İnventory for measuring for depression. Arc Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 24.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Türk Psikoloji Dergisi. 1998;7:3–13. [Google Scholar]
- 25.Spielberger CD, Grosuch RL, Lushene RE. Manual for state-trait anxiety Inventory. Consult Psychol. 1970 [Google Scholar]
- 26.Öner N, Le Compte A. Boğaziçi Üniversitesi Yayınları; İstanbul, Turkey: 1983. Durumluluk Süreklilik Kaygı Envanteri ElKitabı. [Google Scholar]
- 27.IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; Armonk, NY: 2013. [Google Scholar]
- 28.Machado AMC. Multiple testing correction in medical image analysis. J Math Imaging Vis. 2007;29:107–117. [Google Scholar]
- 29.Nearchou F, Flinn C, Niland R, et al. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;16:8479. doi: 10.3390/ijerph17228479. PMID: 33207689; PMCID: PMC7698263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonzales G, Loret de Mola E, Gavulic KA, et al. Mental health needs among lesbian, gay, bisexual and transgender college students during the COVID-19 pandemic. J Adol Health. 2020 doi: 10.1016/j.jadohealth.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kidd JD, Jackman KB, Baruccu R, et al. Understanding the impact of COVID-19 pandemic on the mental health of transgender and gender nonbinary individuals engaged in a longitudinal cohort study. J Homosex. 2021 doi: 10.1080/00918369.2020.1868185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;163:e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suen YT, Chan RCH, Wong EMY. Effects of general and sexual minority-specific COVID-19-related stressors on the mental health of lesbian, gay, and bisexual people in Hong Kong. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spack PN, Edwards-Leeper L, Feldman HA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical centre. Pediatrics. 2012;129:418–425. doi: 10.1542/peds.2011-0907. [DOI] [PubMed] [Google Scholar]
- 35.Holt V, Skagerberg E, Dunsford M. Young people with features of gender dysphoria: demographics and associated difficulties. Clin Child Psychol Psychiatry. 2016;21:108–118. doi: 10.1177/1359104514558431. [DOI] [PubMed] [Google Scholar]
- 36.Meyer IH. Prejudice, social stress and mental health in lesbian, gay and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ryan C, Russell S, Huebner D, et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23:205–213. doi: 10.1111/j.1744-6171.2010.00246.x. [DOI] [PubMed] [Google Scholar]
- 38.Russell ST, Fish JN. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu Rev Clin Psychol. 2016;12:465–487. doi: 10.1146/annurev-clinpsy-021815-093153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magson NR, Freeman JYA, Rapee RM, et al. J. risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bockting WO, Miner MH, Swinburne Romine RE, et al. Stigma, mental health and resilience in an online sample of the US transgender population. Am J Public health. 2013;103:943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fish JN, McInroy LB, Paceley MS, et al. I'm Kinda Stuck at home with unsupportive parents right now”: LGBTQ youths’ experiences with COVID-19 and the importance of online support. J Adolesc Health. 2020;67:450–452. doi: 10.1016/j.jadohealth.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hiller A, Torg E. Parent participation in a support group for families with transgender and gender-nonconforming children: “being in the company of others who do not question the Reality of Our Experience”. Transgend Health. 2019;4:168–175. doi: 10.1089/trgh.2018.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roberts SA, Williams CR, Grimstad FW. Consideration for providing pediatric gender-affirmative care during the COVID-19 pandemic. J Adolesc Health. 2020;67:635–637. doi: 10.1016/j.jadohealth.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van der Miesen AIR, Raaijmakers D, Van de Grift TC. “You have to wait a little longer”: transgender (Mental) health at risk as a consequence of deferring gender‑affirming treatments during COVID‑19. Arch Sex Behav. 2020;49:1395–1399. doi: 10.1007/s10508-020-01754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van der Miesen AIR, Steensma TD, de Vries ALC. Psychological functioning in transgender adolescents before and after gender affirmative care compared to cisgender general population peers. J Adolesc Health. 2020 doi: 10.1016/j.jadohealth.2019.12.018. [DOI] [PubMed] [Google Scholar]