Abstract
Background: Recent data estimate the prevalence of pediatric obesity at 19.3%. Emphasis on primary prevention and early identification is needed to avoid development of serious medical and psychosocial sequelae. The objective of this initiative is to assess baseline knowledge and comfort among trainees at an inner-city pediatric residency program in identifying children with overweight/obesity, evaluating associated risk factors and comorbidities, and providing effective counseling.
Methods: Key topics from 2 major guidelines on pediatric obesity assessment, prevention, and treatment were incorporated into the development of a resident questionnaire, which consisted of 12 knowledge-based questions and a Likert scale evaluating self-perceived knowledge and comfort on 7 skills.
Results: Forty-six percent of eligible residents completed the questionnaire (n = 28). The mean score on the objective knowledge-based section was 44% ± 13%, with no differences by training year. The percentage of residents with correct responses by topic ranged from 14% to 79%. The mean self-perceived knowledge rating was 3.56 ± 0.86. The mean self-perceived comfort rating was 3.53 ± 0.89. Neither the self-perceived knowledge nor comfort rating was a significant predictor of performance on the objective knowledge-based section when controlling for postgraduate year status.
Conclusions: Significant gaps in knowledge were discovered among pediatric residents with regard to appropriate screening, assessment, and counseling practices related to pediatric overweight/obesity. These deficits were not consistently reflected in residents' self-perceived knowledge and comfort ratings. The results of this initiative highlight the need for incorporation of standardized curricula on childhood overweight/obesity into pediatric resident education.
Keywords: obesity, overweight, pediatrics, preventive interventions, primary care, resident education
Introduction
Since 1971, overall rates of childhood obesity in the United States have more than tripled, with the largest increase in the school-aged children. The latest data from the National Health and Nutrition Examination Survey (NHANES) from 2017 to 2018 estimate that currently 35.4% of children and adolescents have either overweight or obesity and 19.3% have obesity. Hispanic, non-Hispanic black, and Mexican American youth are disproportionately affected.1
Studies have shown that obesity established at an early age confers a high risk of obesity in adolescence,2,3 and up to 80%–90% of children with established severe obesity at ages 2–5 continue to have obesity as adults.4 In addition, the risk of cardiometabolic complications, including dysglycemia, dyslipidemia, and hypertension, increases with greater severity of obesity, even when controlling for age, race/ethnicity, and sex.5
Although multiple factors are responsible for these alarming trends, suboptimal training of physicians leading to a lack of knowledge about the implications of obesity is an important contributor that should be considered. As frontline providers, pediatricians are in a unique position for close monitoring of their patients' anthropometric measures, allowing for early identification of overweight/obesity and provision of timely interventions to avoid long-term sequelae. However, previous studies looking at resident education on childhood obesity identified deficits in instructional quality and lack of formal curricula among programs with a pediatric training component.6–9
The objective of our current initiative was to assess baseline knowledge and comfort among trainees at an inner-city pediatric residency program in identifying children with overweight or obesity, evaluating associated risk factors and comorbidities, and providing appropriate counseling. We hypothesized that major gaps in knowledge will be identified due to paucity of a formal educational curriculum on childhood obesity and that trainees will not always be cognizant of their own limitations.
Materials and Methods
Setting
Pediatric trainees at the Icahn School of Medicine at Mount Sinai in New York City, NY, were invited to complete an anonymous questionnaire either in person during their continuity clinic or online over a period of 4 weeks between March and April of 2018. This medium-sized residency program offers pediatric training through the traditional categorical pathway and research track, as well as through preliminary positions for trainees enrolled in advanced subspecialty programs and through a number of combined programs, including medical genetics and pediatrics/psychiatry/child and adolescent psychiatry. Despite the broad clinical, research, and educational experiences and opportunities available to trainees, there is currently no formal curriculum on childhood obesity.
To solidify their educational experience in the general pediatric outpatient setting, all trainees participate in resident continuity clinics throughout the duration of their training. The majority of trainees complete this experience at the Mount Sinai Pediatric Associates Practice. This practice sees an estimated 15,000 preventative visits per year, and a large percentage of patients come from East and Central Harlem, which is comprised predominantly of Hispanic and non-Hispanic black populations and where up to 42% of preschoolers, 46% of public elementary school children, 32% of adolescents, and 60% of adults had either overweight or obesity as of 2007.10
Data Source and Questionnaire Content
Key themes from two major guidelines on childhood obesity assessment, prevention, and treatment published in recent years were incorporated into the development of a resident questionnaire.11,12 The questionnaire consisted of 12 knowledge-based multiple-choice questions on the following topics: diagnostic criteria for pediatric overweight and pediatric obesity; prevalence of childhood obesity in the United States (based on 2013–2014 NHANES data available at the time of the questionnaire development); endocrine/genetic causes of obesity; associated comorbidities; diagnostic criteria for diabetes; diagnostic criteria for pediatric hypertension; recommendations on fruit, vegetable, and fruit juice intake, physical activity, and screen time; and indications for bariatric surgery.
In addition, trainees were asked to rate their self-perceived knowledge and comfort on seven skills using a Likert scale from 1 to 5 (1 = not knowledgeable/not comfortable to 5 = very knowledgeable/very comfortable). These skills included screening for and identifying children with overweight or obesity, discussing the diagnosis of pediatric overweight/obesity with patients and their families, screening for factors contributing to the development of pediatric overweight/obesity, assessing for potential familial or psychosocial factors that contribute to pediatric overweight/obesity, screening for comorbidities associated with pediatric overweight/obesity, counseling families on preventative measures and lifestyle modifications related to pediatric overweight/obesity, and discussing potential pharmacological or surgical options for management of pediatric obesity.
Trainees were asked to indicate their postgraduate year (PGY) status (PGY1, PGY2, or PGY3+) and whether they would be interested in participating in a multidisciplinary, family-focused, group-based obesity clinic that would be built into the continuity practice. A sample questionnaire is provided under Supplementary Data.
Statistical Analyses
Continuous data were assessed for normality using the Shapiro–Wilk test. For normally distributed data and non-normally distributed data with a sample size ≥30 per group, means and standard deviations are reported and an independent two-sample test or one-way analysis of variance with the Tukey post hoc test was used for evaluation of differences in means across groups. For non-normally distributed data with a sample size of <30 in at least one group, the Mann–Whitney U test and Kruskal–Wallis test with pairwise comparisons of mean ranks were utilized; significance values were adjusted by Bonferroni correction to account for multiple comparisons for the latter. For categorical variables, the Pearson chi-square test and adjusted residual post hoc analysis with Bonferroni correction for multiple tests were performed.
Multiple linear regression analyses were conducted between knowledge (independent variable) and comfort (dependent variable) ratings, both as aggregates across all seven skills and then separately for each individual skill, as well as between mean self-perceived knowledge/comfort ratings calculated for each participant (as two separate analyses where each factor acted as an independent variable) and the percentage scores on the objective knowledge-based section (dependent variable); all analyses were controlled for PGY status. A subgroup analysis to assess the latter relationship by PGY status was also performed.
A two-sided p-value of <0.05 was used to define statistical significance for all tests. The Statistical Package for the Social Sciences International Business Machines Corporation (IBM) software package (Version 25.0; IBM, Armonk, NY) was used for all statistical analyses.
The project was determined to be a quality initiative by the Department of Pediatrics Performance Improvement Committee at the Icahn School of Medicine at Mount Sinai and was thus exempt from Institutional Review Board approval.
Results
Twenty-eight trainees (46% of all eligible residents) completed the questionnaire (25 in person and 3 online) (Table 1). Although the percentage of PGY3+ residents who participated was lower (29%) compared with the percentages of PGY1 (55%) and PGY2 (59%) residents, this difference was not statistically significant. The mean score on the objective knowledge-based section was 44% ± 13%, with no significant differences among the PGY groups. The mean self-perceived knowledge rating was 3.56 ± 0.86, and the mean self-perceived comfort rating was 3.53 ± 0.89. The PGY1 group had significantly lower mean ratings for both variables compared with the PGY2 and PGY3+ groups.
Table 1.
Participant Characteristics and Summary of Questionnaire Results
| Characteristic | Result | Test statistic | p |
|---|---|---|---|
| Sample size | 28 (46% of all eligible residents) | ||
| PGY1 | 11 (55%) | ||
| PGY2 | 10 (59%) | ||
| PGY3+ | 7 (29%) | ||
| 0.929a | 0.63 | ||
| Percentage score on objective knowledge-based section | 44% (13%) | ||
| PGY1 | 42% (9%) | ||
| PGY2 | 44% (15%) | ||
| PGY3+ | 46% (17%) | ||
| 0.187b | 0.83 | ||
| Self-perceived knowledge rating, mean (SD) | 3.56 (0.86) | ||
| PGY1 | 3.21 (0.92) | ||
| PGY2 | 3.83 (0.72) | ||
| PGY3+ | 3.71 (0.76) | ||
| 11.828b | < 0.001c | ||
| Self-perceived comfort rating, mean (SD) | 3.53 (0.89) | ||
| PGY1 | 3.27 (0.91) | ||
| PGY2 | 3.71 (0.84) | ||
| PGY3+ | 3.65 (0.83) | ||
| 5.478b | 0.005d |
Pearson chi-square statistic.
F statistic.
On Tukey post hoc analysis, statistically significant differences were found between PGY1 and PGY2 residents (p < 0.001) and PGY1 and PGY3 residents (p = 0.002).
On Tukey post hoc analysis, statistically significant differences were found between PGY1 and PGY2 residents (p = 0.007) and PGY1 and PGY3 residents (p = 0.05).
PGY, postgraduate year; SD, standard deviation.
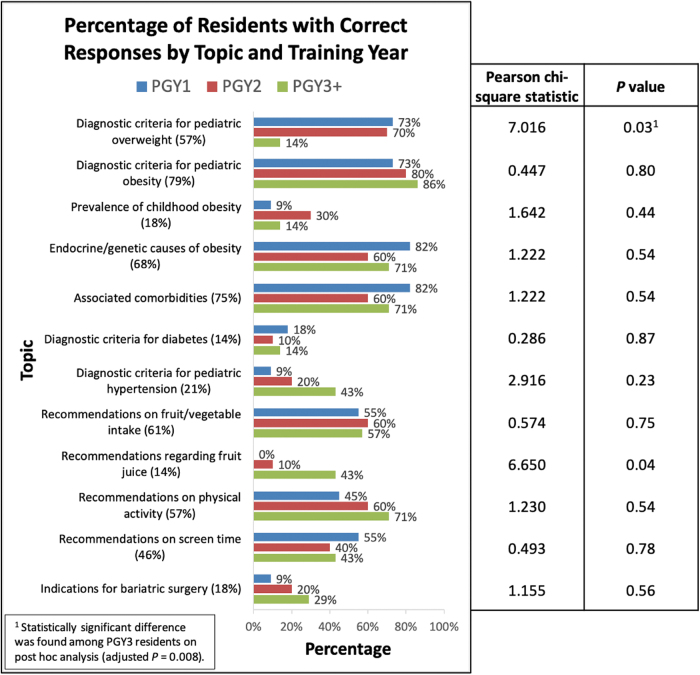
The percentage of residents with correct responses by topic ranged from 14% to 79% (Fig. 1). The topics with the lowest percentage of correct responses (<50%) included prevalence of childhood obesity, diagnostic criteria for diabetes, diagnostic criteria for pediatric hypertension, recommendations on fruit juice, recommendations on screen time, and indications for bariatric surgery. There were no differences among the PGY groups on any topic except the diagnostic criteria for pediatric overweight. The PGY3+ group had the lowest percentage of correct responses (14%) on this topic compared with the PGY1 (73%) and PGY2 (70%) groups.
Figure 1.
Proportion of trainees with correct responses to objective questions by topic and PGY status. In addition, the description of each topic is followed by the total percentage of residents who answered that corresponding question correctly. Results of the Pearson chi-square test are presented in the columns to the right. PGY, postgraduate year.
The mean ranks of self-perceived resident knowledge and comfort ratings were similar across skills, with the exception of discussing potential pharmacological or surgical options for management of pediatric obesity, which had the lowest mean ranks for both variables (data not shown). When evaluating responses by PGY status, the PGY1 group had significantly lower mean rank knowledge ratings in discussing the diagnosis of overweight/obesity and counseling on preventative measures/lifestyle modifications compared with the PGY2 group, but not the PGY3+ group (Table 2). There were no significant differences in the mean rank comfort ratings across the PGY groups on any skill (Table 3).
Table 2.
Comparison of Self-Perceived Knowledge Ratings by Skill and Training Year
| Skill | PGY | Mean rank knowledge rating | H statistic (df 2) | p |
|---|---|---|---|---|
| Screening for overweight/obesity | ||||
| 1 | 13.05 | |||
| 2 | 16.75 | |||
| 3+ | 13.57 | |||
| 3.197 | 0.20 | |||
| Discussing the diagnosis of overweight/obesity | ||||
| 1 | 9.18 | |||
| 2 | 18.50 | |||
| 3+ | 17.14 | |||
| 10.685 | 0.005a | |||
| Screening for contributing factors | ||||
| 1 | 10.50 | |||
| 2 | 17.55 | |||
| 3+ | 16.43 | |||
| 5.974 | 0.05 | |||
| Assessment of familial/psychosocial factors | ||||
| 1 | 11.50 | |||
| 2 | 18.35 | |||
| 3+ | 13.71 | |||
| 5.101 | 0.08 | |||
| Screening for comorbidities | ||||
| 1 | 12.64 | |||
| 2 | 15.00 | |||
| 3+ | 16.71 | |||
| 1.759 | 0.42 | |||
| Counseling on preventative measures/lifestyle modifications | ||||
| 1 | 10.55 | |||
| 2 | 18.00 | |||
| 3+ | 15.71 | |||
| 7.839 | 0.02b | |||
| Discussing pharmacological/surgical treatment options | ||||
| 1 | 11.14 | |||
| 2 | 15.40 | |||
| 3+ | 18.50 | |||
| 4.095 | 0.129 | |||
On pairwise comparisons with Bonferroni correction, a statistically significant difference in mean ranks was found between PGY1 and PGY2 residents (adjusted p = 0.007).
On pairwise comparisons with Bonferroni correction, a statistically significant difference in mean ranks was found between PGY1 and PGY2 residents (adjusted p = 0.02).
df, degrees of freedom; PGY, postgraduate year.
Table 3.
Comparison of Self-Perceived Comfort Ratings by Skill and Training Year
| Skill | PGY | Mean rank comfort rating | H statistic (df 2) | p |
|---|---|---|---|---|
| Screening for overweight/obesity | ||||
| 1 | 12.27 | |||
| 2 | 18.10 | |||
| 3+ | 12.86 | |||
| 4.747 | 0.09 | |||
| Discussing the diagnosis of overweight/obesity | ||||
| 1 | 10.86 | |||
| 2 | 17.15 | |||
| 3+ | 16.43 | |||
| 4.894 | 0.09 | |||
| Screening for contributing factors | ||||
| 1 | 11.18 | |||
| 2 | 17.30 | |||
| 3+ | 15.71 | |||
| 4.920 | 0.09 | |||
| Assessment of familial/psychosocial factors | ||||
| 1 | 12.86 | |||
| 2 | 15.95 | |||
| 3+ | 15.00 | |||
| 1.010 | 0.60 | |||
| Screening for comorbidities | ||||
| 1 | 12.91 | |||
| 2 | 15.40 | |||
| 3+ | 15.71 | |||
| 1.193 | 0.55 | |||
| Counseling on preventative measures/lifestyle modifications | ||||
| 1 | 12.36 | |||
| 2 | 14.20 | |||
| 3+ | 18.29 | |||
| 2.830 | 0.24 | |||
| Discussing pharmacological/surgical treatment options | ||||
| 1 | 13.09 | |||
| 2 | 15.45 | |||
| 3+ | 15.36 | |||
| 0.583 | 0.75 | |||
df, degrees of freedom; PGY, postgraduate year.
The self-perceived knowledge rating was a significant predictor of the comfort rating in general and on all of the seven topics individually, when controlling for PGY status (Table 4). However, neither the mean self-perceived knowledge nor comfort rating was a significant predictor of performance on the objective knowledge-based section, both when controlling for training year (Table 4) and on subgroup analyses by PGY status (data not shown).
Table 4.
Multiple Linear Regression Analyses of Objective and Subjective Data
| Independent variablea | Dependent variable | B [95% CI] | SE B | β | t Statistic | p |
|---|---|---|---|---|---|---|
| Self-perceived knowledge rating | Self-perceived comfort rating | |||||
| Combined | 0.776 [0.676 to 0.876] | 0.051 | 0.754 | 15.345 | <0.001 | |
| Individual skill | ||||||
| Screening for overweight/obesity | 1.006 [0.454 to 1.559] | 0.268 | 0.597 | 3.751 | 0.001 | |
| Discussing the diagnosis of overweight/obesity | 0.811 [0.370 to 1.251] | 0.214 | 0.655 | 3.792 | 0.001 | |
| Screening for contributing factors | 0.627 [0.392 to 0.861] | 0.114 | 0.761 | 5.499 | <0.001 | |
| Assessment of familial/psychosocial factors | 0.402 [0.061 to 0.743] | 0.166 | 0.441 | 2.426 | 0.02 | |
| Screening for comorbidities | 0.953 [0.713 to 1.194] | 0.117 | 0.859 | 8.170 | <0.001 | |
| Counseling on preventative measures/lifestyle modifications | 0.863 [0.490 to 1.236] | 0.181 | 0.698 | 4.764 | <0.001 | |
| Discussing pharmacological/surgical treatment options | 0.841 [0.536 to 1.147] | 0.148 | 0.813 | 5.678 | <0.001 | |
| Mean self-perceived knowledge rating | Percentage score on objective knowledge-based section | −1.870 [−12.887 to 9.147] | 5.349 | −0.076 | −0.350 | 0.73 |
| Mean self-perceived comfort rating | Percentage score on objective knowledge-based section | −2.363 [−11.995 to 7.269] | 4.677 | −0.104 | −0.505 | 0.62 |
All analyses were performed with PGY status added as a covariate.
B, unstandardized beta; CI, confidence interval; SE, standard error; β, standardized beta; PGY, postgraduate year.
Twenty-four respondents (86%) indicated that they would be interested in participating in a multidisciplinary, family-focused, group-based obesity clinic. The characteristics of trainees who indicated “yes” versus “no” are summarized in Table 5. The group that answered “no” had a higher mean rank score on the objective knowledge-based section.
Table 5.
Characteristics of Trainees by Expressed Interest in Obesity Clinic Participation
| Characteristic | Trainee response to whether they would be interested in participating in a multidisciplinary, family-focused, group-based obesity clinic |
Test statistic | p | |
|---|---|---|---|---|
| “Yes” | “No” | |||
| Sample size | 24 (86%) | 4 (14%) | ||
| PGY1 | 10 | 1 | ||
| PGY2 | 9 | 1 | ||
| PGY3+ | 5 | 2 | ||
| 1.559a | 0.46 | |||
| Percentage score on objective knowledge-based sectionb | 42% (13%) | 56% (8%) | ||
| Mean rank score | 13.23 | 22.13 | 17.500c | 0.04 |
| Self-perceived knowledge rating, mean (SD)b | 3.57 (0.86) | 3.46 (0.88) | ||
| Mean rank knowledge rating | 99.40 | 99.07 | 2200.000c | 0.52 |
| Self-perceived comfort rating, mean (SD)b | 3.55 (0.89) | 3.39 (0.88) | ||
| Mean rank comfort rating | 99.85 | 90.38 | 2124.500c | 0.35 |
Pearson chi-square statistic.
Although means and SDs are reported, nonparametric testing was performed for comparison of mean ranks as the data were not normally distributed and the sample size in at least one of the groups was <30.
U statistic.
PGY, postgraduate year; SD, standard deviation.
Discussion
The prevalence of pediatric overweight and obesity in the United States has continued to rise at an alarming rate over the past five decades. Environmental factors, characterized by intake of high amounts of processed carbohydrates prevailing in the Western diet, low levels of physical activity, and increased sedentary behaviors, have undoubtedly contributed to these trends, underscoring the importance of primary prevention. As frontline medical providers for children, pediatricians are ideally positioned to deliver preventative counseling, identify concerning anthropometric trends, and offer appropriate screening and intervention when overweight or obesity is identified.
However, pediatricians must be properly trained to be able to provide the best care possible, and studies have indicated that physician training on the topics of obesity and nutrition, both in adult and pediatric specialties, is often suboptimal.6–9 Multiple barriers have been identified based on interviews and surveys conducted with program directors, including lack of structured training and faculty development within a program, other competing curricular demands and lack of time, unclear evidence base for pediatric obesity treatment and prevention interventions, lack of training sites for seeing pediatric patients with obesity, inadequate financial resources for program development, and lack of insurance reimbursement for obesity interventions.6,7
In response to some of the identified barriers surrounding lack of best practice recommendations, two major guidelines have been published over recent years to help guide pediatric providers on childhood obesity assessment, prevention, and treatment, most recently in 2017.11,12 Several programs and institutions with a pediatric training component have adopted these guidelines and/or other educational materials to design and implement curricula on pediatric obesity in the past 15 years.13–15 These curricula varied in size, length, and format, but all identified positive outcomes, including increases in physician confidence, optimization of physician clinical behavior, positive change in patient behavior, and/or improvements in electronic medical record documentation of topics related to overweight/obesity.14,15
In addition to the efforts described above, both the American Academy of Pediatrics and the United States Preventive Services Task Force have strived to increase awareness of the pediatric obesity epidemic by providing recommendations for prevention, screening, and intervention practices.16,17 Furthermore, the American Board of Pediatrics recognizes nutrition and obesity as important content topics that are tested by the certifying examinations under the domain of “Preventative Pediatrics/Well-Child Care.”18
However, despite these endeavors, to date, there are no standardized recommendations or guidelines provided by the Accreditation Council of Graduate Medical Education (ACGME) to incorporate formal obesity education into the pediatric residency training curriculum. Although the “Frequently Asked Questions” document from the ACGME Review Committee for Pediatrics mentions nutritionists as practitioners who are part of interprofessional teams and may supervise pediatric residents, a review of the most recent ACGME Program Requirements for GME in Pediatrics, effective as of July 1, 2020, did not identify any specific references to weight, obesity, or nutrition under “Educational Program” requirements.19,20 As such, most pediatric residency programs continue to lack in a structured designed curriculum on these topics.
To determine whether the aforementioned educational gaps have tangible consequences on residents' experiences, we surveyed trainees at an inner-city pediatric residency program to assess their objective knowledge on the major themes included in the recently published guidelines cited above and gauge their self-perceived knowledge and comfort ratings on seven skills that pertain to pediatric overweight and obesity. We found suboptimal overall performance on the objective knowledge-based section, notably with no significant differences by training year. Even more disheartening was that only 57% and 79% of residents were able to correctly identify the diagnostic criteria for pediatric overweight and obesity, respectively, with the PGY3+ residents having the worst performance on the former question.
Although the PGY3+ group was the smallest and the trainees' postresidency plans were not assessed, presenting some limitations to the interpretation of results, the poor performance of the PGY3+ group and the overall lack of expected improvement in objective knowledge are nonetheless concerning. As ≥50% of the trainees in this residency program pursue subspecialty training, it is possible that by their third year, these residents' educational focus shifts toward the topics directly pertinent to their chosen career path, resulting in knowledge lapses of topics related to general pediatrics. Furthermore, some PGY3+ residents, whether consciously or subconsciously, may feel that topics such as overweight/obesity may not be as relevant to their future training and practice, resulting in reduced awareness and attention to them.
However, given the importance of childhood overweight/obesity and how it permeates all corners of medical practice, including pediatric subspecialties, it is imperative that all pediatricians, regardless of training and career path, are at least able to correctly identify these children and provide appropriate referrals if necessary. Correctly diagnosing children with overweight/obesity forms the foundational basis for appropriate screening practices and preventative and therapeutic interventions, and the inability to do so likely narrows the window period for effective counseling, putting these patients at risk for further weight gain and metabolic deterioration.
Of even greater interest and significance was the lack of correlation found between self-perceived knowledge and comfort ratings and objective knowledge, both when controlling for training year and on subgroup analysis by PGY status. These findings suggest that while trainees may in fact feel well equipped to address the above topics, with mean self-perceived knowledge and comfort ratings in the upper half of the designated scale, this is not supported by objective data, indicating that residents regardless of their level of training often lack awareness of their gaps. Even residents with the lowest overall scores on the objective knowledge-based section perceived their knowledge and comfort on topics related to pediatric overweight/obesity to be adequate.
This discrepancy could be at least partially explained by the fact that trainees may feel that their exposure to a large population of children with overweight/obesity alone is sufficient to provide them with the tools necessary to care for these patients; however, the lack of a formal curriculum incorporating evidence-based guidelines and thus limited appreciation of the recommended best practices preclude their ability to properly address the relevant issues.
This disconnect between objective knowledge and self-perception of knowledge/comfort may have significant implications directly impacting the care of children with overweight/obesity. The inability to acknowledge one's limitations may contribute to overconfidence and lead to either missed opportunities for appropriate identification and counseling or the delivery of misinformation.
In addition, although residents are always precepted in the continuity clinic by more experienced attending pediatricians, misjudged self-perceived knowledge/comfort may lead to missed opportunities for education if residents feel like they are well equipped to address and manage the issues related to overweight/obesity on their own. This is especially relevant for PGY3+ residents who are typically granted more independence in patient care and decision-making, with less direct oversight by preceptors.
While assessments of baseline knowledge of topics related to pediatric overweight/obesity and trainee perception of their knowledge and comfort are necessary initial steps in highlighting the detrimental effects that lack of a formal curriculum has on the training of future pediatricians, it is equally as important, if not more so, to brainstorm and implement potential solutions. As one solution, we had assembled a working group of residents, faculty, clinic leadership, nutritionists, and social workers to develop a multidisciplinary, group-based family-focused program focused specifically on topics related to overweight/obesity, with the goal of incorporating it into the resident-run clinic. The majority of trainees expressed interest in this program on our questionnaire.
Appreciating the large medical, psychosocial, and financial impacts associated with the unmitigated obesity epidemic, in addition to program-level interventions, it is necessary to optimize physician education on a more large-scale level. One way to ensure this is to mandate formal obesity training in pediatric training programs and highlight proficiency in obesity care as one of the core competencies residents should master before program completion. Basic knowledge of obesity topics is not just relevant to general pediatricians but also to all pediatric subspecialists as they will undoubtedly encounter patients with overweight/obesity throughout their careers and could help reinforce healthy lifestyle practices.
This quality initiative has several limitations. First, this assessment was performed on a limited number of trainees at one residency program and may thus not necessarily be generalizable to the larger population of pediatric residents. However, we believe that by virtue of being part of a medium-sized program that attracts a diverse cohort of trainees of varying backgrounds, educational experiences, and interests, we had a rather representative sample of pediatric residents and can still use the pivotal data acquired through the survey to make broader assumptions about the state of obesity education at large.
Another limitation is that we did not specifically assess whether trainees themselves felt like their obesity training was sufficient or whether they were able to identify any gaps and/or had suggestions for a preferred modality of teaching, although the majority expressed interest in a multidisciplinary, group-based family-focused program.
Nonetheless, our initiative is one of the first of its kind to design a questionnaire that assessed not only subjective knowledge and comfort but also objective resident knowledge on 12 topics borrowed directly from the evidence-based guidelines on pediatric obesity prevention, assessment, and treatment, which are fundamental for providing optimal patient care. In doing so, the questionnaire sheds light on specific deficits in resident obesity education and the concerning lack of concordance between self-perceived knowledge/comfort and objective performance. Our hope is that these findings will motivate individual programs to adopt more rigorous obesity training and provide an impetus for a more global incorporation of formal obesity education into residency curricula.
Conclusions
Pediatric obesity continues to be a major public health issue, with persistently rising prevalence and strong tracking into adulthood, often leading to debilitating health-related complications and considerable medical costs. Pediatricians, as frontline providers, have a critical opportunity to recognize and address this issue early on by providing appropriate screening, assessment, and counseling to those at risk, with the ultimate goal of curbing further weight gain and development of chronic comorbidities. Thus, appropriate education on pediatric overweight/obesity is critical in equipping physicians-in-training with the tools necessary to tackle this issue head on.
However, despite the presence of evidence-based guidelines and program-specific educational endeavors developed over recent years, there is a lack of formal educational curricula on pediatric obesity across residency programs. Our quality initiative showed that as a consequence, residents of all training levels have limited knowledge on the pertinent topics related to pediatric obesity, which are highlighted in the published guidelines, and often lack awareness of their gaps.
Future studies surveying trainees across different programs would help clarify whether these knowledge deficits are in fact present nationally and if there are any discrepancies identified in terms of both program-specific and geographical factors. Furthermore, we invite the assembly of a multidisciplinary working group to develop specific guidelines for a formal education curriculum on pediatric obesity to be incorporated into the pediatric ACGME program requirements, with an associated set of core competencies that residents should be expected to meet by the completion of training.
Supplementary Material
Acknowledgments
The authors would like to thank the Icahn School of Medicine at Mount Sinai Department of Pediatrics Performance Improvement Committee for supporting this quality initiative. They would also like to extend their gratitude to the residents who helped distribute the questionnaires at the Mount Sinai Pediatric Associates Practice and to all of those who completed the survey.
Authors' Contributions
Dr. Azova conceptualized and designed the quality initiative, developed data collection instruments and coordinated data collection, carried out the analyses, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Mogilner assisted with the design of the quality initiative, provided relevant expert input, administered the questionnaires, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding Information
Dr. Azova was supported by a grant, 5T32DK007699-39, from the National Institute of Diabetes and Digestive and Kidney Diseases. The funder/sponsor did not participate in the work.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E Stat 2020. [Epub ahead of print]. [Google Scholar]
- 2. Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med 2014;370:403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Geserick M, Vogel M, Gausche R, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med 2018;379:1303–1312. [DOI] [PubMed] [Google Scholar]
- 4. Ward ZJ, Long MW, Resch SC, et al. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med 2017;377:2145–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med 2015;373:1307–1317. [DOI] [PubMed] [Google Scholar]
- 6. Goff SL, Holmboe ES, Curry L. Barriers to obesity training for pediatric residents: a qualitative exploration of residency director perspectives. Teach Learn Med 2006;18:348–355. [DOI] [PubMed] [Google Scholar]
- 7. Wolff MS, Rhodes ET, Ludwig DS. Training in childhood obesity management in the United States: a survey of pediatric, internal medicine-pediatrics and family medicine residency program directors. BMC Med Educ 2010;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burton AM, Cherrington A, Agne A, et al. 108 Implementing an obesity counseling curriculum in residency training (southern regional meeting abstracts). J Invest Med 2010;58:387. [Google Scholar]
- 9. Lenders CM, Deen DD, Bistrian B, et al. Residency and specialties training in nutrition: a call for action. Am J Clin Nutr 2014;99(5 Suppl):1174S–1183S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matte T, Gordon C, Goodman A, et al. Obesity in East and Central Harlem: A Look Across Generations. New York, NY: New York City Department of Health and Mental Hygiene, 2007. [Google Scholar]
- 11. Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007;120(Suppl 4):S164–S192. [DOI] [PubMed] [Google Scholar]
- 12. Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity-assessment, treatment, and prevention: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2017;102:709–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huang J, Pokala P, Hill L, et al. The Health and Obesity: Prevention and Education (HOPE) curriculum project—Curriculum development. Pediatrics 2009;124:1438–1446. [DOI] [PubMed] [Google Scholar]
- 14. Silber M, Weiss L, Sharaf S, et al. Pediatric residency obesity and overweight training curricula: A systematic review. Glob Pediatr Health 2020;7:2333794X20928215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mastrocola MR, Roque SS, Benning LV, Stanford FC. Obesity education in medical schools, residencies, and fellowships throughout the world: a systematic review. Int J Obes (Lond) 2020;44:269–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Daniels SR, Hassink SG, Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics 2015;136:e275–e292. [DOI] [PubMed] [Google Scholar]
- 17. Force USPST, Grossman DC, Bibbins-Domingo K, et al. Screening for obesity in children and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017;317:2417–2426. [DOI] [PubMed] [Google Scholar]
- 18. General Pediatrics Content Outline. Updated September 1, 2017. Available at https://www.abp.org/sites/abp/files/gp_contentoutline_2017.pdf Last accessed February 13, 2021.
- 19. Frequently Asked Questions: Pediatrics, Review Committee for Pediatrics, ACGME. Updated May, 2017. Available at https://www.acgme.org/Portals/0/PDFs/FAQ/320_pediatrics_FAQs_2017-07-01.pdf?ver=2017-05-18-111047-157 Last accessed February 13, 2021.
- 20. ACGME Program Requirements for Graduate Medical Education in Pediatrics. Updated July 1, 2020. Available at https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/320_Pediatrics_2020.pdf?ver=2020-06-29-162726-647 Last accessed February 13, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.