Abstract
The coronavirus disease 2019 (COVID-19) pandemic resulted in unprecedented measures across all health services around the globe, including the large-scale cessation of assisted reproductive technology treatment in Europe as clinics closed, causing disruption and delay to the fertility treatment of thousands of patients in the UK alone. This research explores how patients were impacted by the delay and disruption, and their feelings, concerns and reactions. A mixed-methods, anonymous, online questionnaire, live between 19 May and 30 June 2020, was used to target all fertility patients aged >18 years whose treatment had been impacted by COVID-19. In total, 709 people began the questionnaire and 501 completed it in the time available (70.7% completion rate). Patients reported feeling ‘powerless/helpless’ (78.3%), ‘frustrated’ (59.3%) and ‘anxious’ (54.7%) in response to the closure of fertility clinics. The majority were ‘very concerned’ about time passing and not knowing when they could start treatment again (79.0%), and the length of waiting lists when clinics reopened (70.9%). While 76.8% of respondents had some concerns around contracting COVID-19, 42.9% were ‘not at all concerned’ about undergoing in-vitro fertilization treatment during a pandemic. Variables such as funding source, duration of infertility, previous experience of fertility treatment, treatment stage and the presence of children were correlated with significant intragroup differences in the types of concerns reported. The large majority (72.7%) of respondents stated their eagerness to start treatment as soon as possible, and 9.4% said that they had already resumed treatment; only 6.0% of respondents wanted to wait due to concerns related to COVID-19.
Keywords: Assisted reproduction, Coronavirus disease, Counselling, COVID-19, Fertility, Pandemic, Psychology, SARS-COV-2, Sociology
Introduction
On 11 March 2020, deeply concerned by the alarming levels of spread and severity, the Director General of the World Health Organization declared coronavirus disease 2019 (COVID-19) a global pandemic, and called for ‘countries to take urgent and aggressive action’ (World Health Organization, 2020). This resulted in unprecedented measures across health services around the globe, with assisted reproductive technology (ART) treatment in Europe, the USA and elsewhere impacted significantly. Within 1 week, both the American Society for Reproductive Medicine (ARSM) (2020) and the European Society of Human Reproduction and Embryology (ESHRE) (2020a) had provided early independent recommendations for the fertility sector, advising a precautionary approach involving the postponement of all ART pregnancies.
By early April 2020, ESHRE had formed a specialist coronavirus disease 2019 (COVID-19) working group to monitor scientific reports relevant to reproductive medicine (European Society of Human Reproduction and Embryology, 2020b), and released detailed guidance on fertility services during the pandemic (European Society of Human Reproduction and Embryology, 2020c). The guidance advised cessation of new ART treatment for five primary reasons: (i) to avoid complications from ART treatment and pregnancy; (ii) to avoid potential severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)-related complications during pregnancy; (iii) to mitigate the unknown risk of vertical transmission in SARS-CoV-2-positive patients; (iv) to support the necessary reallocation of healthcare resources; and (v) to observe the current recommendations of social distancing. In addition, there was a recommendation that all patients currently undergoing treatment should opt for elective oocyte or embryo freezing to defer embryo transfer and pregnancy. The only exception concerned urgent fertility preservation for oncology patients, with the recommendation that the cryopreservation of gametes, embryos or tissue should still be considered. The ESHRE guidelines reiterated the importance of following ‘local and national government advice’, with most countries either recommending or enforcing the closure of fertility clinics. By 1 April 2020, all European countries reported partial or complete cessation of ART treatment, and fertility clinics remained closed for an average of 7 weeks (ESHRE COVID-19 Working Group, 2020).
In the UK, guidance was published by the British Fertility Society, the Association of Reproductive and Clinical Scientists, the Royal College of Obstetricians and Gynaecologists, and the Human Fertilisation and Embryology Authority (HFEA) (2020a) in March 2020, all urging the cessation of elective ART treatment, both to reduce the risk of viral infections for patients and professionals, and to protect essential medical and National Health Service (NHS) resources to aid in the fight against the pandemic. On 1 May 2020, HFEA wrote to all licensed fertility centres advising that, from 11 May 2020, they could apply to reopen, subject to meeting the steps necessary to protect staff and patients against infection, and ensuring that treatments could proceed in line with social distancing measures (Human Fertilisation and Embryology Authority, 2020b). The announcements, which came earlier than expected, were welcomed by both professionals and patients across the fertility sector (Murray, 2020), but clinics responded at different rates, resulting in continuing uncertainties and anxieties for patients (Gürtin, 2020).
There has already been considerable effort by researchers from a variety of disciplines to understand the impact of the COVID-19 pandemic on fertility patients. At the recent (virtually held) 36th annual ESHRE meeting, three sessions were dedicated to posters and presentations about COVID-19 (Oral Sessions 36 and 67, and Poster Session VI-2140). Regarding the psychological effects of uncertainty and delayed fertility treatment, researchers from the UK and Italy reported a clear negative impact on patients, including increased levels of stress, anxiety and depression (Boivin et al., 2020, Ferrero et al., 2020, Karavadra et al., 2020). These findings echo the reported increases in mental health problems, such as stress, anxiety and depressive symptoms, among the general population in response to concerns about COVID-19 (Nelson et al., 2020, Torales et al., 2020), but are also an important reminder that psychological care needs to be considered a cornerstone of fertility treatment (Gameiro et al., 2015).
As outlined in the joint statement made by ASRM, ESHRE and the International Federation of Fertility Societies (IFFS), ‘Reproductive care is essential and reproductive medicine professionals are in a unique position to promote health and wellbeing’ (Veiga et al., 2020). In order to do this, it is crucial to explore not just the medical implications of the COVID-19 pandemic, but also patients’ experiences, emotional reactions and perceived needs. While it is well established that patients will have a range of psychosocial needs across their treatment pathway (Gameiro et al., 2015), it is noteworthy that additional concerns and support needs may arise as a response to taxing external circumstances, increased uncertainties, unforeseen delays and the health risks that accompany a global pandemic. Given the possibility of a ‘second wave’ of COVID-19, or indeed the outbreak of further disruptive pandemics in the near future, it is particularly important to develop an understanding of the perspectives of fertility patients so that timely lessons can be learnt about how best to respond, or provide support, in similar circumstances.
In the hope of contributing to such an endeavour, this study aims to provide empirical data regarding the profile of patients seeking fertility treatment who were affected by the COVID-19 pandemic and fertility clinic closures, and to develop in-depth insights into their feelings, concerns and self-appraisals regarding the impact of this situation on their lives and wellbeing. The research timing and questionnaire were designed to elucidate the precise concerns that patients had in response to the COVID-19 pandemic and clinic closures, as well as the reopening of clinics, enabling respondents to state whether they were ‘not at all’, ‘slightly’ or ‘very concerned’ by different issues.
Materials and methods
Data were gathered using a mixed-methods, anonymous online questionnaire hosted on the survey platform Qualtrics. The multidisciplinary research team, including a social scientist, two clinicians, a psychologist, a fertility counsellor and a reproductive scientist, compiled the first draft of the questionnaire, developing items based both on personal and clinical experience of patient reactions and concerns, as well as a review of the media coverage, press releases by professional bodies and regulators, and online discussion board content relating to fertility treatment delays due to COVID-19. Subsequently, the questionnaire was tested and improved through two stages of piloting. In the first stage, it was tested for functionality and sensitivity by members of the research team and four volunteers (including two fertility patients). In the second stage, six fertility patients at different stages of disrupted fertility treatment completed the questionnaire, offering detailed feedback on items and making suggestions for clarification and improvement, as well as on the actual phrasing of questions as ‘wording is crucial in survey design’ (Braun et al., 2020).
Ethical approval for the study was obtained from the University College London Research Ethics Committee (Project 9831/001). The ethical review and research development processes were expedited to respond to the extraordinary circumstances surrounding the COVID-19 pandemic in a timely fashion.
The questionnaire was live for 6 weeks from 19 May to 30 June 2020, capturing both the period of clinic closures and the period during which clinics began to reopen in the UK. During this period, study recruitment posters and images including the questionnaire weblink (http://bit.ly/CoronaFertilityStudy) were widely distributed using social media, relevant mailing lists, and personal and professional contacts of the research team. Social media ‘influencers’ with large accounts concentrating on fertility, infertility and fertility treatment, as well as fertility charities and support organizations, shared recruitment materials on their Facebook, Instagram and Twitter accounts, and with their mailing lists where applicable. In addition, the research team contacted every fertility clinic in the UK with information about the research; many posted questionnaire links on their social media platforms, and some displayed study posters on their premises. Members of the British Infertility Counselling Association were also contacted and asked to share study materials with clients, where this was judged to be appropriate. The research received some media coverage during this period, including an article written by the first author (Gürtin, 2020), and a segment discussing the study which aired on BBC Woman’s Hour on 8 and 13 June 2020 enabling the authors to reach a wider audienc (Woman’s Hour, 2020).
The questionnaire weblink directed potential respondents to a detailed information page, outlining the aims and purpose of the research, identifying the research team and institution, emphasizing the anonymous and voluntary nature of participation, and providing a list of resources. Following this information, respondents were asked to provide their consent before proceeding to the questionnaire. At the end of the questionnaire, respondents were asked to confirm the submission of their responses, and those completing submission were directed to a ‘thank you’ page, once again providing a list of resources and the lead researcher’s contact details.
Measures
The questionnaire comprised 10 sections, each concentrating on a different aspect of patients’ context or current experiences: (1) demographic characteristics; (2) fertility history; (3) current fertility treatment circumstances; (4) feelings about the impact of COVID-19 on fertility treatment; (5) impact on relationship with partner (only visible to those in a relationship); (6) concerns regarding clinic closures; (7) concerns regarding clinic reopening; (8) needs, desires and experiences of support from clinics; (9) needs, desires and experiences of support outside clinics; and (10) further thoughts, experiences or recommendations.
Each section, except for Section 10, included a range of quantitative and qualitative items, including Likert scale or multiple-choice questions which enabled a direct comparison across standardized response options, and open-text questions which enabled respondents more freedom to express themselves. Section 10 only included open-ended open-text questions to ensure that respondents had ample opportunity to voice their thoughts and experiences and to raise any particular issues that felt important to them. This mixed-methods design (Braun et al., 2020) was used to maximize openness and flexibility, and to provide a ‘wide angle lens’ (Toerien and Wilkinson, 2004) on the topic, enabling the authors to access a diverse and geographically dispersed group (Braun et al., 2017) in an economical and safe way during the COVID-19 pandemic.
In total, the questionnaire comprised 40 questions; however, the dynamic online format allowed the questionnaire to be tailored to respondents’ answers, developing the flow logic to ensure that each person only viewed questions that were relevant for them. For example, if a respondent ticked that they were ‘single’, subsequent questions pertaining to the impact of clinic closures on their relationship with their partner were not displayed. This was a particularly important consideration when designing the questionnaire, as piloting confirmed the need for sensitivity and attentiveness regarding such issues. Respondents were able to pause and return to the questionnaire multiple times, and could change their answers at any point before submitting their completed questionnaires. This control over key aspects of research participation can be considered an important strength of online questionnaires (Braun et al., 2020).
For most respondents, the questionnaire took approximately 30 min to complete, although respondents were, of course, able to choose how long to spend on the survey or when to complete it (Braun et al., 2017, Terry and Braun, 2017). Respondents were required to answer every question they encountered, except for optional questions in Section 10, in order to submit the completed questionnaire. Almost all submitted questionnaires included detailed and lengthy text responses to open-ended questions. In order to enable transparency and cross-referencing, each qualitative response was given a unique identifier number which appears in parentheses after the quotation; this denotes the question number and the response number to that question.
Study population and respondents
The questionnaire was open to all men and women aged >18 years who were undergoing or waiting to begin fertility treatment, and who experienced treatment delays or disruption due to the COVID-19 pandemic. Although the authors were primarily interested to hear from fertility patients based in the UK, and the recruitment campaigns were focused on UK sites, this was not specified as an inclusion criterion. The questionnaire was only available in English.
In the UK, fertility treatments are offered both through the NHS (for couples or individuals who qualify for state funding) and through the private sector (where they are paid for out of pocket). The authors wanted to include patients from both groups.
In total, 709 people began the questionnaire and 501 people submitted completed questionnaires within the available timeframe, corresponding to a very high completion rate (70.7%). Of the 501 questionnaires received, 37 were from fertility patients living outside of the UK and were excluded from this analysis in order to avoid potential misrepresentations. Non-UK-based submissions comprised eight from Ireland; eight from the USA; three from Australia; three from Canada; two from France; two from the United Arab Emirates; and one each from Belgium, Denmark, Finland, Germany, India, the Netherlands, Norway, South Africa, Spain, Switzerland and Turkey. These responses were excluded in order to minimize confounding variables amongst the respondents. Of the remaining 464 questionnaires, 457 were completed by female fertility patients, only six were completed by male fertility patients, and one was completed by a non-binary patient. Although the authors had hoped to capture responses from all fertility patients, and had not targeted any specific gender in the recruitment materials, the decision was made to concentrate the analysis on the female respondents as they formed the overwhelming majority, and it was felt that there was an insufficient number of responses to represent the experiences of non-female patients.
Analysis
Quantitative data were compiled, and statistical analysis was performed using SPSS Version 26 (IBM Corp., Armonk, NY, USA). Chi-squared test was used to compare categorical data. Statistical significance was set at P < 0.05 for all analyses.
Qualitative data were analysed using reflexive thematic analysis (Braun and Clarke, 2006, Braun and Clarke, 2019). Open-text content was read multiple times by three researchers (ZBG, PDS, CD) to gain familiarity with the data, to assign codes to sections of text, to generate meaningful themes based on codes, and to discuss and review the process together for intercoder variability and reliability. Each response to an open-text question was given a unique identifier, comprised of the question number followed by the response number, and these have been used where quotations are provided.
This paper presents the results from Sections 1–4, 6 and 7 of the questionnaire, concentrating on respondents’ profiles, feelings and concerns around clinic closures and reopenings. The results from the remaining sections will be published as separate papers, focusing on the support needs and experiences of fertility patients during clinic closures (Sections 8–10); the impact of fertility treatment delays on patients’ relationships (Section 5); and a qualitative sociological analysis of patients’ feelings and reactions about the disruption to their fertility treatments.
Results
The results of 457 completed questionnaires from female fertility patients who were living in the UK were analysed. Unless otherwise stated, all percentages were calculated based on the full dataset. All respondents self-identified as having had their fertility treatments disrupted or delayed as a result of the COVID-19 pandemic and clinic closures.
Demographic characteristics
Table 1 provides detailed information regarding respondents’ demographic characteristics, including relationship status, age, partners’ age, residence and ethnicity.
Table 1.
Respondents’ demographic characteristics.
| n | % | ||
|---|---|---|---|
| Relationship status | Heterosexual couple | 416 | 91.0 |
| Same-sex couple | 18 | 3.9 | |
| Single | 21 | 4.6 | |
| Treatment with non-partner | 2 | 0.4 | |
| Total | 457 | 100 | |
| Respondents’ age (years) Range: 21–55 Mean: 34.6 SD: 4.9 |
≤35 | 232 | 50.8 |
| 36–37 | 97 | 21.2 | |
| 38–39 | 57 | 12.5 | |
| 40–42 | 49 | 10.7 | |
| 43–44 | 11 | 2.4 | |
| ≥45 | 11 | 2.4 | |
| Total | 457 | 100 | |
| Partners’ age (years) Range: 24–59 Mean 36.4 SD 5.8 |
≤35 | 171 | 39.7 |
| 36–37 | 99 | 23 | |
| 38–39 | 54 | 12.5 | |
| 40–42 | 54 | 12.5 | |
| 43–44 | 20 | 4.6 | |
| ≥45 | 33 | 7.7 | |
| Total | 431 | 100 | |
| Residence | London | 123 | 26.9 |
| South East England | 96 | 21.0 | |
| South West England | 41 | 9.0 | |
| East Midlands | 26 | 5.7 | |
| West Midlands | 20 | 4.4 | |
| North East England | 13 | 2.8 | |
| North West England | 42 | 9.2 | |
| Yorkshire and the Humber | 21 | 4.6 | |
| Scotland | 38 | 8.3 | |
| Wales | 24 | 5.3 | |
| Northern Ireland | 13 | 2.4 | |
| Total | 457 | 100 | |
| Ethnicity | White | 414 | 90.6 |
| Mixed/multiple ethnicities | 18 | 3.9 | |
| Asian/Asian British | 18 | 3.9 | |
| Black/African/Caribbean/Black British | 1 | 0.2 | |
| Other ethnic group | 5 | 1.1 | |
| I prefer not to say | 1 | 0.2 | |
| Total | 457 | 100 | |
SD, standard deviation.
The average age of respondents was 34.6 years. This compares well with the latest HFEA data, which show that, across the UK, the average age of patients is 35.7 years for in-vitro fertilization (IVF) and 34.5 years for donor insemination (Human Fertilisation and Embryology Authority, 2021). Similarly, 91.0% of the respondents were in heterosexual relationships, compared with 90.4% of all UK cycles of fertility treatment undertaken by heterosexual couples (Human Fertilisation and Embryology Authority, 2021).
Fertility history and current treatment circumstances
Table 2 details all the information regarding respondents’ fertility history and current treatment circumstances including: whether they had any children; number of years they had been trying to conceive; reasons for seeking fertility treatment; whether they had previous experience of fertility treatment and whether they had any eggs/embryos in storage; current stage of treatment; and whether their treatment was privately funded, or partially or fully funded by the NHS.
Table 2.
Respondents’ fertility history and current treatment circumstances.
| n | % | ||
|---|---|---|---|
| Do you have a child or children? | Yes | 59 | 12.9 |
| No | 398 | 87.1 | |
| Total | 457 | 100 | |
| How long have you been trying for a child? | <2 years | 150 | 32.8 |
| 2–4 years | 213 | 46.6 | |
| >4 years | 94 | 20.6 | |
| Total | 457 | 100 | |
| Reason for seeking fertility treatment | No male partner | 41 | 9.0 |
| Unknown/unexplained | 157 | 34.4 | |
| Male-factor infertility | 65 | 14.2 | |
| Female-factor infertility | 111 | 24.3 | |
| Combination of male- and female-factor infertility | 57 | 12.5 | |
| History of miscarriage | 14 | 3.1 | |
| To undertake PGD | 7 | 1.5 | |
| Did not answer | 5 | 1.1 | |
| Total | 457 | 100 | |
| Have you had previous fertility treatment? | Yes | 239 | 52.3 |
| (of these respondents, 120 had frozen eggs/embryos in storage and 119 did not) | |||
| No | 218 | 47.7 | |
| Total | 457 | 100 | |
| Current treatment stage | Undergoing fertility preservation | 3 | 0.7 |
| Hormone treatment/IUI | 37 | 8.1 | |
| Pre-treatment and investigations | 126 | 27.6 | |
| About to start IVF | 132 | 28.9 | |
| During/after IVF cycle | 88 | 19.3 | |
| Between cycles | 53 | 11.6 | |
| Waiting for donor/surrogate | 18 | 3.9 | |
| Total | 457 | 100 | |
| Funding | Fully NHS funded | 198 | 43.3 |
| Partially NHS funded | 26 | 5.7 | |
| Privately funded | 175 | 38.3 | |
| NA/unclear | 58 | 12.7 | |
| Total | 457 | 100 | |
PGD, pre-implantation genetic diagnosis; IUI, intrauterine insemination; IVF, in-vitro fertilization; NHS, National Health Service; NA, not applicable.
Feelings about the closure of fertility clinics
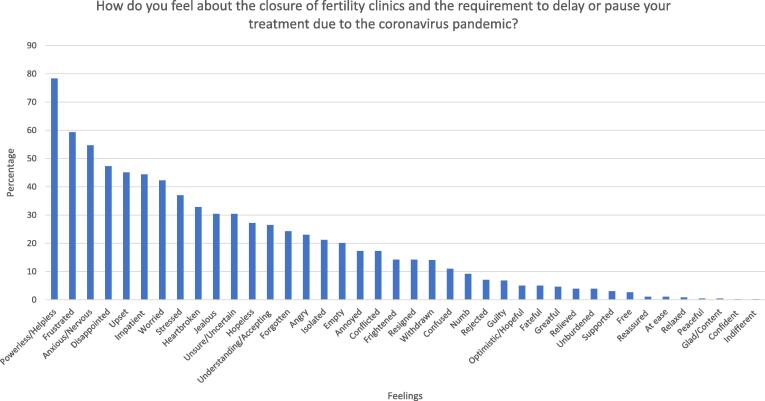
Respondents were asked, ‘How do/did you feel about the closure of fertility clinics and the requirement to delay or pause your fertility treatment due to the COVID-19 pandemic?’ They were provided with a matrix of 40 randomly arranged words, 20 of which could be described as ‘negative’, and 20 as ‘neutral’ or ‘positive’, and asked to tick the words that were most applicable to them. Each respondent had to choose at least one word, but could choose up to a maximum of 10 words.
Fig. 1 shows the words that the respondents picked, from the most commonly chosen to the least commonly chosen. By far the most common word was ‘powerless/ helpless’, chosen by 78.3% of respondents. This was followed by ‘frustrated’ and ‘anxious/nervous’, each chosen by more than half of the respondents (59.3% and 54.7%, respectively). It is noteworthy that all of the most commonly chosen 10 words were negative. In fact, the only three non-negative words that appeared in the top 20 word choices referred to the ambivalent feelings of being ‘unsure/uncertain’, ‘understanding/accepting’ and ‘conflicted’. It is noteworthy that only 3.1% of respondents felt ‘supported’, and only a tiny minority were ‘reassured’ (1.1%) about the clinic closures.
Fig. 1.
Respondents’ feelings.
There were almost no differences in the feeling words chosen by those whose treatment was fully or partially NHS-funded compared with those who were privately funding their treatment, with one important exception. NHS-funded respondents were significantly more likely to report feeling ‘forgotten’ (29.0% versus 17.8%; P < 0.05). This feeling was also reiterated in the open-text answers of many NHS patients. The following highlights a common reaction:
My clinic was closed and staff sent to work in other aspects of the NHS. I feel completely lost. I’m conflicted as what they are doing is amazing but I feel completely forgotten about. (27–384)
Looking at another intragroup comparison, several significant differences were found between the word choices of respondents who had no previous experience of fertility treatment and the word choices of those who had previous experience of fertility treatment. For example, the negative words ‘frustrated’ (64.2% versus 54.8; P < 0.05), ‘anxious/nervous’ (59.6% versus 50.2%; P < 0.05), and ‘stressed’ (41.7% versus 32.6%; P < 0.05) were all chosen by a higher proportion of those who had no previous experience of fertility treatment than those who had previous experience of fertility treatment. Conversely, those who had previous experience of fertility treatment were more likely to report feeling ‘understanding/accepting’ (31.4% versus 21.1%; P < 0.05), ‘unburdened’ (7.1% versus 4.1%; P < 0.01) and ‘relieved’ (6.3% versus 1.4%; P < 0.01). Although chosen by small minorities of respondents, these feelings of relief were also reflected in the open-text responses of some women with previous experience of fertility treatment, who reflected on the benefits of having ‘an enforced break’ from fertility treatments. For example, one respondent wrote:
I felt some relief about the fact that the decision to defer our next cycle had been made for me. I had been nervous about going straight from one failed cycle into another cycle. (27–239)
In general, almost every respondent chose to write lengthy accounts about their feelings in their own words. Many highlighted their sadness in response to clinic closures, using words such as ‘devastated’ and ‘heartbroken’, or described their situation as ‘being stuck’, ‘in limbo’ or ‘shrouded in complete uncertainty’, which led to feeling ‘helpless’, ‘alone’ and ‘isolated’. Some pointed out that while they understood why clinics had to close, they nevertheless felt ‘disappointed’ or ‘let down’, and that they experienced ‘a rollercoaster’ of emotions. While there is not enough space in this paper to do justice to the eloquent and touching qualitative responses received (which will be reported in a separate paper), the following examples give a flavour of the range and intensity of feelings that women articulated:
When I heard the clinic was going to close, I was completely devastated. My partner isn't getting any younger and further delays to our treatment was beyond belief. It was a particularly bitter pill to swallow with all the jokes around lockdown baby boom. (27–111)
It made us feel as though our lives were on hold once again and that our dream of becoming parents was even further out of reach. I was so heartbroken to have come so close to making it happen and then it was whipped away from us. (27–354)
We were just days away from starting the injections. The uncertainty around when clinics would reopen had a significant and profound impact on my already fragile mental health due to years of TTC [trying to conceive]. I was heartbroken and felt completely alone and helpless. (27–182)
I feel panicked and desperate. […] I’m worried that by the time I next get a chance it will be too late. I find the uncertainty of how long the wait will be unbearable. I will be last in the queue after those who were in the middle of treatment. (27–338)
Rollercoaster of emotions. On one hand, I totally get why it had to happen, and on the other, the thing we want most has been delayed. (27–168)
Concerns regarding clinic closures and clinics reopening
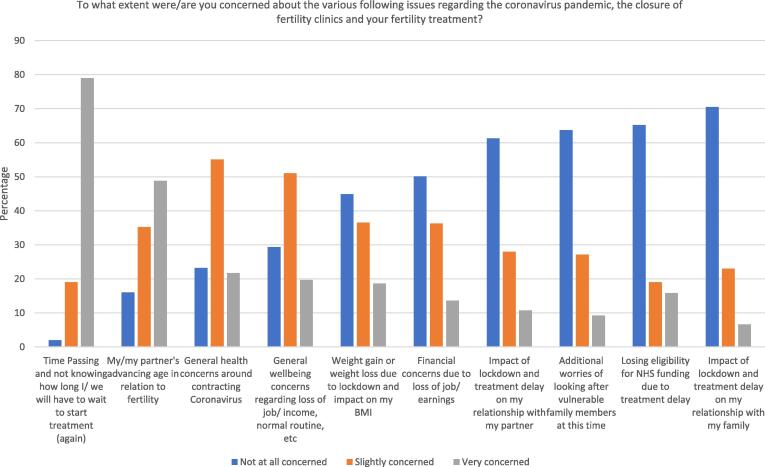
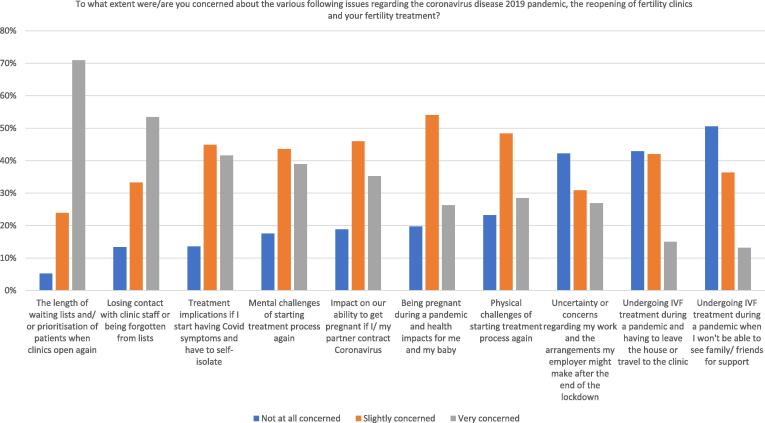
Respondents were provided with a range of 10 potential concerns associated with the COVID-19 pandemic and the closure of fertility clinics, and 10 potential concerns associated with the reopening of fertility clinics. For each item, respondents were asked to rate whether they were ‘not at all concerned’, ‘slightly concerned’ or ‘very concerned’. Fig. 2, Fig. 3 display the results for these questions.
Fig. 2.
Respondents’ concerns regarding the closure of fertility clinics. NHS, National Health Service; BMI, body mass index.
Fig. 3.
Respondents’ concerns regarding the reopening of fertility clinics. IVF, in-vitro fertilization.
Regarding the closure of fertility clinics, by far the biggest concern was ‘time passing and not knowing how long I/we will have to wait to start treatment again’, with 79.0% of respondents stating that they were ‘very concerned’ about this issue. The second largest concern was ‘my/my partner’s advancing age in relation to fertility’, with just under 50% of respondents feeling ‘very concerned’. Reflecting the specific context, ‘general health concerns around contracting coronavirus’ and ‘general wellbeing concerns regarding loss of job/income, normal routine, etc.’ were both of similar concern for the respondents, with 76.8% and 70.7%, respectively, feeling either ‘slightly concerned’ or ‘very concerned’ about these issues.
Regarding the reopening of fertility clinics, by far the biggest concern was ‘the length of waiting lists and/or the prioritization of patients when clinics open again’, with 70.9% feeling ‘very concerned’ about this. On a similar theme, 53.4% were ‘very concerned’ about ‘losing contact with clinic staff or being forgotten from lists’. Interestingly, the respondents were less concerned about undergoing IVF treatment during a pandemic, with 50.6% stating they were ‘not at all concerned’ about not being able to ‘see family/friends for support’, and 42.9% feeling ‘not at all concerned’ about ‘having treatment during a pandemic and having to leave the house or travel to the clinic’.
Intragroup differences regarding potential concerns were also examined When comparing responses across different variables, there were some significant differences between the levels of concern reported by respondents based on: patient age; whether they were NHS-funded or privately funding their treatment; the number of years they had been trying to conceive; whether or not they had previous experience of fertility treatment; the stage of treatment they were at when lockdown was announced; and whether they already had children. The following sections report the results of these intragroup differences.
Patient age
Patient age was strongly correlated with increased concerns about age. While only 30.6% of those aged ≤35 years were ‘very concerned’ about their advancing age in relation to fertility, this was true of significantly higher percentages of those aged 36–37 years (59.8%), 38–39 years (71.9%), 40–42 years (73.5%), 43–44 (81.8%) years and ≥45 years (72.7%; P < 0.001).
Funding source
Whether respondents were NHS-funded or privately funded was correlated with the types of concerns they expressed. In comparison with privately funded respondents, respondents whose treatment was funded by the NHS were more likely to be ‘very concerned’ about losing eligibility for NHS funding (P < 0.001), losing contact with clinic staff or being forgotten (93.3% versus 80.6%; P < 0.001), and the length of waiting lists (97.8 versus 90.3%; P < 0.001).
Conversely, privately funded respondents reported higher concerns about contracting COVID-19 (82.9% versus 70.1%; P < 0.05), having to leave the house during the pandemic to undergo fertility treatment (69.1% versus 47.3%; P < 0.001), treatment implications if they started having COVID-19 symptoms and had to self-isolate (90.3 versus 83.5; P < 0.05), and being pregnant during a pandemic (84.6% versus 76.3; P < 0.05).
Duration of infertility
Those respondents who had been trying to conceive for >4 years were more likely to be concerned about the physical challenges of starting treatment again compared with respondents who had been trying to conceive for 2–4 years or <2 years (85.1% versus 77.5% and 70.7%, respectively; P < 0.05).
Those who had been trying to conceive for 2–4 years were more concerned about losing eligibility for NHS funding than those who had been trying to conceive for <2 years (32.7%) or >4 years (41.3% versus 32.7% and 23.4%, respectively; P < 0.01).
Previous experience of fertility treatment
There were many significant differences between the levels of concern amongst those who did and did not have previous experience of fertility treatment. Those without any previous experience of fertility treatment were more concerned than participants who did have previous experience of fertility treatment about the impact of lockdown and treatment delay on their relationship with their partner (45.4% versus 32.6%; P < 0.05), losing eligibility for NHS funding (41.7% versus 28.5%; P < 0.001), weight gain or loss (61.0% versus 49.8%; P < 0.05), and losing contact with clinic staff (90.4% versus 83.3%; P < 0.05)
On the other hand, those who had previous experience of fertility treatment were significantly more concerned about having treatment during a pandemic and having to leave the house to travel to the clinic (64.9% versus 48.6%; P < 0.001), and the treatment implications if they caught COVID-19 and had to self-isolate (89.5% versus 83%; P < 0.05).
Stage of treatment
The stage of treatment that respondents were at when clinic closures were announced had an impact on their levels of concern about various issues. Amongst the respondents, 70.9% were ‘very concerned’ about the length of waiting lists and/or prioritization of patients when clinics reopened. This concern was more prominent amongst those who were at the initial stages of having pre-treatment investigations (79.4%), and those who were waiting for a donor or surrogate (83.3%) when clinics closed (P < 0.05).
Although 57.1% of all respondents were concerned about undergoing IVF during a pandemic and leaving the house to travel to the clinic, this was true for significantly higher percentages of those who were about to start an IVF cycle (62.9%), those whose treatments were paused mid-cycle (63.6%), and those who were in between IVF cycles (67.9%), compared with those who were having hormone treatments (40.5%), pre-treatment investigations (46.8%), or awaiting a donor or surrogate (50.0%; P < 0.05).
Having a child/children
Respondents who were childless were more likely to be ‘very concerned’ about time passing and not knowing how long they would have to wait to start treatment again (81.2% versus 64.4%; P < 0.05), losing contact with clinic staff (56.3% versus 33.9%; P < 0.05), and the length of waiting lists (73.4% versus 54.2%; P < 0.05) than respondents who already had a child or children.
However, those with children were more concerned about the additional worries of looking after vulnerable family members during lockdown (49.2% versus 34.4%; P < 0.05) and financial concerns due to losing job/earnings (62.7% versus 48.0%; P < 0.05).
Respondents’ concerns – In their own words
Many respondents took the opportunity to record their concerns in their own words. In these open-text responses, many reiterated their concerns surrounding the uncertainties around clinic closures and reopenings, and highlighted a range of worries and anxieties which were categorized into seven overarching categories of concerns regarding: time and/or ageing; communication with clinics; treatment practicalities; health and infection risks; finances; job and/or employer; and a second wave and longer-term impact of COVID-19. Below, illustrations are provided from each category, followed by examples of the positive aspects of lockdown reported by respondents.
Time and/or ageing
Concerns about time passing, ageing, longer waiting lists, and having to wait to attempt conception weighed heavily on respondents’ minds. In addition to concerns about age-related fertility decline, some respondents were also anxious that delays could worsen their existing conditions (endometriosis, fibroids), and reduce the chances of treatment success. As one woman explained:
The delays could ultimately take away our chance to become parents. Fertility is time sensitive and each delay has a knock-on effect. (33–82)
For many patients, their worst fear was ‘that purely due to the delays in treatment from the pandemic, I may never have the chance to conceive’ (33–108), meaning ‘that we missed our chance to become parents’ (33–67).
Communication with the clinics
Communication with clinics and clinic staff was a central concern which permeated responses across different questions, with some reflecting on the negative impacts of poor communication on their mental health and on their sense of trust in the clinic. The following responses were echoed across the dataset:
I’ve had no contact since my cycle was cancelled and no update whatsoever. It’s been 6 weeks since they updated information on their website. I feel really let down. (33–4)
The total lack of clarity and communication from my clinic makes me not trust them as much with our treatment when it eventually happens. (33–88)
The hardest part has been not knowing. We had very little/no contact during the lockdown. A general email on health/wellness/mental health periodically would have helped. Email accounts just bounced out-of-office replies which I felt was not good enough. (33–44)
I don’t know how the clinic will contact me – so I have been anxiously checking the post, for emails and missed calls. (33–32)
Treatment practicalities
Respondents articulated a wide range of practical concerns regarding access to treatments, the delivery of care, and further health services. These included concerns about negotiating virtual appointments and new social distancing guidelines in the midst of uncertainty regarding new arrangements. As one respondent noted:
Apparently I need an appointment with an embryologist before frozen embryo transfer but they have no idea when this will be or how it will take place. Surely, they had to submit their plant to the HFEA including how they would deliver appointments? What value is there in the HFEA’s approval process if this wasn’t covered? How did Primark open before a facility providing time-sensitive medical treatment?! (33–2)
Many patients were particularly concerned that their partners would no longer be able to accompany them:
Going through treatment and my partner not being able to be there with me. […] If I fall pregnant, how long will it be before he can join me for scans? I don’t want him to miss out on the joyful moments of finally being pregnant. It’s been hard getting there so I’d want him to enjoy them too. (33–144)
In one case, the respondent expressed concerns that she and her husband would not be able to accompany their surrogate:
My husband and I are not permitted to attend the embryo transfer, scans, and there is some question as to whether we would be able to attend the birth. (33–141)
As can be expected, practical concerns were particularly exacerbated for those seeking treatment overseas, and those requiring third-party reproductive assistance. While the former were understandably worried about travel restrictions, the latter were concerned about the added burdens impacting donors and their willingness to donate:
Our embryos are in Spain, so we need to be able to travel there early July and hope that the quarantine will indeed be lifted as planned in Spain from 1 July. (33–23)
Our main concern was our donor. Would she lose heart? Would she be scared for her health? Would the whole complex and difficult process be made one step too much? (33–36)
Some respondents raised the ‘indirect impacts […] of COVID on midwifery services, other health services (if I have any pregnancy complications); labour and delivery’ (33–6), as well as general practice clinic closures, and one women pointed out that while she was not concerned about SARS-CoV-2, she ‘would definitely want staff to feel safe while giving treatment’ (33–3).
Health and infection risks
A few respondents discussed either their own or their partner’s pre-existing conditions, which made them feel vulnerable; a few respondents discussed concerns relating to the potential impacts of vertical transmission and ‘the impact of COVID on pregnancies, infants, etc.’ (33–140), and a few respondents worried about negotiating travel to the clinic and clinic appointments safely. One respondent wrote:
I am actually most concerned by the very lax measures the clinic is taking in relation to COVID-19. Clearly social distancing is not possible when having scans or taking bloods. […] Neither the doctor nor the nurse has been wearing their face-mask over their nose. (33–33)
For many of those who noted concerns around catching COVID-19, the main worry was that this would lead to further delays in their treatment. In fact, the majority of respondents noted that they were much less concerned about the various health risks associated with COVID-19 than they were with delays to their treatment. This attitude was fairly typical:
I am more concerned about my clinic NOT reopening or being forgotten about at the bottom of a long waiting list than I am about fertility treatment during a pandemic. (33–103)
Mental health concerns were included in this category, which ranged from concerns that ‘being stressed will make it harder to get pregnant!’ (33–135) to reports of deteriorating mental health: ‘I suffer from anxiety and depression which have both been exacerbated during this time’ (33–34).
Finances
As can be expected, respondents reiterated concerns about losing their NHS funding, but they also worried about the more general financial repercussions on the NHS:
Concerned about the cost of the pandemic to the NHS under the Conservative government. The impact of the cost and whether NHS fertility would be cut. (33–87)
With the amount of money this country has lost, [I worry that] IVF funding would be taken away completely, or if this round didn’t work, they wouldn’t let us have our other two tries. (33–137)
Some respondents raised concerns about having to pay for private treatment to beat waiting lists, having to pay for additional storage of embryos, and losing money if treatment cycles got cancelled due to contracting COVID-19. As one respondent explained:
If we catch it, the cycle gets cancelled without a refund. It feels like investing all our savings into something that may get cancelled due to the pandemic. (33–106)
Job and/or employer
Many respondents relayed specific work-related concerns in relation to their fertility treatment, which were heightened due to the demands of the pandemic or the increased precarity of employment. One nurse, an ‘essential worker’ in the NHS, explained:
IVF is not considered essential and there is no HR [human resources] policy for IVF. I was told I could not be redeployed, take unpaid leave or work from home at the moment, so working at the ‘non COVID site’ is my only option. (33–90)
Many others relayed their worries about disclosing fertility treatment or early pregnancy to employers to enable risk assessments or home-working arrangements. The following response was echoed by several women:
Huge increase in stress and anxiety in relation to work/job security and IVF treatment. I have a very unsympathetic employer, and I had been worried to tell them about my fertility treatment before lockdown. Now job security is threatened due to the pandemic, the idea of informing them that I am going through IVF seems impossible and very likely to cost me my job. (33–93)
A second wave and the longer-term impact of COVID-19
Concerns regarding a second wave were raised frequently:
My main concern is around a second wave. […] What I fear is starting up treatment again, getting just about ready for transfer, and the same thing happens all over again. (33–61)
Some women wondered how long the pandemic would continue, wondering if they would be able to see their families once pregnant, and musing that ‘the world I’m bringing a child into seems very different’ (33–97). One respondent stated:
It seems plausible the pandemic could continue for over a year in England as it’s been handled so disastrously by the government. (33–43)
Positive aspects
Although all respondents felt clinic closures to be negative, it is worth noting that a few respondents also reflected on the benefits of lockdown. The following three quotes are a testament to these women’s resilience and positivity:
One slight positive of the lockdown is that my husband recently started medication which might improve his semen parameters […] he’s been on it for 3 months at this point so we will at least (hopefully soon) see whether it has had an effect before we decide on next steps (33–114)
I have been seeing lockdown as a positive opportunity for my wider health as working at home means I can get better sleep and be less stressed, which I hope will impact my fertility for the better. (33–56)
My professional role ordinarily involves frequent travel, including to countries that pregnant women are advised to avoid […] now it seems likely that I will be able to recommence treatment soon while not having to travel for work until at least the end of 2020, which is a relief. (33–138)
Resuming treatment
Respondents had an opportunity to discuss their feelings and opinions regarding the reopening of clinics in their own words. A large majority (72.7%) of those who took this opportunity (n = 417) said that they wanted to start treatment ‘as soon as possible’. While some respondents stated that they had no concerns, others voiced a range of worries or ambivalent feelings, but reiterated that, on balance, their desire to restart treatment outweighed these concerns:
Keen to start ASAP. I have no concerns regarding treatment or pregnancy during the corona epidemic so happy to continue! (39–409)
I want to start treatment ASAP. I am more concerned about my dwindling fertility than anything to do with coronavirus. I am nervous about having to go to appointments alone, but I am more than willing to do that if it means I get to restart treatment. (39–209)
Of the remainder, 9.6% discussed various mixed or conflicted feelings, or raised other issues (regarding, for example, shielding family members); 9.4% reported that they had already resumed treatment; and 1.9% lamented the fact that they could not resume treatment even if they wanted to (e.g. due to restrictions of traveling abroad). Only a very small minority (6.0%) of respondents expressed wanting to wait before resuming treatment due to concerns about COVID-19:
I would wish to delay currently as although I am desperate to start treatment, I would worry so much that contracting COVID would cause a miscarriage. (39–182)
There were also two respondents who knew that they would not be returning for fertility treatment: one had decided to adopt instead, and the other conceived naturally during lockdown.
Discussion
The COVID-19 pandemic has been associated with increased anxiety for the general population (Cowan, 2020, Holmes et al., 2020, Torales et al., 2020), and professionals have warned of pervasive mental health effects in the present and the future (Holmes et al., 2020). Patients seeking fertility treatment have significantly increased levels of baseline anxiety and depression (De Berardis et al., 2014), and the present findings highlight the additional burdens, anxieties and concerns experienced by them as a result of clinic closures and reopenings during this time. This is an important response to the joint call released by ASRM, ESHRE and IFFS to improve understanding of the impact of the COVID-19 pandemic on patients, and to learn lessons about how best to deal with future pandemics (Veiga et al., 2020).
The results show that delays and disruptions to fertility treatments were highly concerning, upsetting and anxiety-inducing for patients, corroborating the early response results from Boivin et al., 2020, Ferrero et al., 2020, Karavadra et al., 2020, Turocy et al., 2020. Overall, the results demonstrate that female fertility patients felt powerless/helpless, frustrated and anxious in response to clinic closures, and were especially concerned about time delays to accessing fertility treatment, length and prioritization of waiting lists, and losing contact with clinic staff. In open-text responses, many wrote about their primary fear of losing the opportunity to become a parent due to delays associated with the COVID-19 pandemic, echoing the UK media coverage surrounding patients’ stories (e.g. Butterly, 2020, Ferguson, 2020, Kale, S., 2020, Tanner, 2020, Webber, 2020), and reiterating Boivin et al.’s (2020) finding that patients perceived clinic closures as ‘a significant threat to the attainability of parenthood goals’. The communication of recent research findings, which show that delays of up to 180 days do not impact the IVF pregnancy outcomes of women, including those with diminished ovarian reserve (Romanski et al., 2020), could prove very reassuring for some of these patients.
This study also found, for the first time, intragroup differences showing that patients with different circumstances have different types and/or levels of concern, and that patient age, funding source, years of infertility, previous experience of fertility treatment, treatment stage and existing children are all relevant variables. While some of these details confirm what one would intuitively expect – for example, that older patients are more concerned about ageing in relation to treatment delays, and NHS patients are more concerned about losing eligibility for funding – there were also a range of unexpected findings which can be usefully interpreted by regulators, clinicians and counsellors to provide the most appropriate support for each patient group. For example, it is worth being aware that patients, especially NHS patients, and those yet to begin a cycle of treatment, are particularly concerned about losing contact with their clinics or being forgotten; for these patients, even the briefest of communications aimed at staying in touch would be a reassurance. It would also be invaluable to provide updates to patients as greater clarity is achieved around a range of issues, from the potential health and pregnancy impacts of COVID-19 to the expected length of waiting lists at each clinic. Although it is important to acknowledge that many fertility professionals, ‘who are passionate about the care that they give to patients and are emotionally entwined with their fertility journeys’ (Balen, 2020), also faced a range of increased difficulties and challenges during the pandemic, it is regrettable that so many of the respondents felt ‘let down’ and ‘disappointed’ about the difficulties of establishing communication with clinics.
The respondents repeatedly articulated the high priority that fertility treatment holds in their lives. While some of the respondents expressed concerns about SARS-CoV-2, and the various medical, financial and practical implications of having treatment during a pandemic, it is noteworthy that only a tiny percentage (6.0%) wished to wait before resuming treatment. The great majority (72.7%) were keen to resume as soon as possible, and patients echoed in their own words the assessment of the ESHRE Working Group, arguing for ‘the importance for continued reproductive care during the COVID-19 pandemic’ (Veiga et al., 2020).
Strengths and limitations
This research has several key strengths. The anonymous online questionnaire was developed by a multidisciplinary team, bringing a range of insights into the research design. The format helped the authors to reach a large number of respondents at a critical time, enabling them to capture reactions to the COVID-19 pandemic, fertility clinic closures and the re-opening of fertility clinics in real time. The sample included a variety of respondents with different fertility profiles and at different stages of fertility treatment, and some aspects of the respondents’ demographic characteristics (particularly relationship status, age and geographical location) were very similar to those of UK fertility patients in general (Human Fertilisation and Embryology Authority, 2019), leading to the greater generalizability of the findings. The exceptionally high (70.7%) completion rate was indicative of the functionality of the software used, the suitability and sensitivity of questions, and the motivation of respondents. The mixed-methods approach led to the collection of both quantitative data, used to develop categories and comparisons, and qualitative data, which enabled the authors to represent thematic insights into patients’ perspectives in their own words. Moreover, to the authors’ knowledge, this is the first study to report differences in the feelings and concerns of fertility patients based on a range of variables, including the stage of treatment they were at when closures were announced, whether their treatment was privately funded or funded by the NHS, and whether they had previous experience of fertility treatment. Many respondents noted their appreciation for this research in open-text questions, which was rewarding for the research team.
The limitations of this research include an exclusive focus on patients resident in the UK, and the over-representation of white, female respondents. In particular, despite explicit efforts to target all fertility patients, there was a dearth of responses from men, which is both problematic and indicative of wider social attitudes that designate reproduction as predominantly a female issue, and result in women in heterosexual relationships identifying themselves as ‘fertility patients’ (regardless of the cause of infertility) while their male partners may not. While women are known to experience higher levels of infertility-related stress and anxiety than men (Peterson et al., 2014), it would have been valuable to also represent men’s perspectives and to be able to include their first-hand responses. Another limitation of the research was the inability to calculate a response rate, as it cannot be known how many relevant people saw the research invitation (online or through social media), nor what proportion of them responded.
Recommendations
The importance of providing up-to-date information (Cowan, 2020) and including patients in policy making around COVID-19 (Richards and Sowcroft, 2020) has been asserted previously, and the authors would argue that reproductive medicine is a key area in which to apply these principles. Listening to patients’ feelings, concerns and priorities can help to mitigate some of the short- and longer-term anxieties associated with this pandemic and with similar situations that may arise in the future. The results show that patients felt powerless, frustrated and anxious about clinic closures, and were very concerned about time passing and not knowing when they could resume treatment or the length of waiting lists when clinics reopened. Many patients also expressed concerns about losing contact with staff members or being forgotten by clinics, and were keen to resume treatment as soon as possible. COVID-19 has been an unprecedented global event, but many commentators are already warning about potential future pandemics which may present similar challenges; we can be better prepared for the occurrence of future pandemics if we learn lessons now.
Based on the study findings, the authors have three key recommendations:
-
–
Clinics and regulators should strive for the timely provision of information to patients regarding both practical matters (e.g. which modes of communication will be used by clinics; when and how clinics will reopen; or how patients on waiting lists would be prioritized) and medical uncertainties (e.g. the impact of COVID-19 on fertility and pregnancy, or the consequences of delay on IVF success rates).
-
–
Clinics and regulators should note that patients are not a homogenous entity; variables such as funding source, stage of treatment and previous experience of fertility treatment will be associated with different types of concerns which can usefully be addressed by more tailored approaches.
-
–
Clinics and regulators should be aware that the large majority of patients are keen to resume their treatment as soon as possible, and this should be facilitated. Clinics that are yet to open should consider making arrangements for their patients to receive treatment elsewhere.
Declaration
The author reports no financial or commercial conflicts of interest.
Acknowledgements
The authors wish to thank all fertility patients who contributed to this study. The authors are also grateful to Jessica Hepburn and Fertility Fest; Sarah Norcross and Bionews; Katy Lindemann at Uberbarrens Club; Natalie Silverman at The Fertility Podcast; Dr Anita Mitra at Gynae Geek; Tracey Sainsbury; The Fertility Hub; Secondary Infertility Matters, and all fertility charities, support organizations, patient advocates and activists, fertility clinics, counsellors, and others who helped to distribute the questionnaire.
Biography

Dr Zeynep Gürtin is a Lecturer at the Institute for Women’s Health at University College London (UK). She is a sociologist of reproduction interested in the social, ethical and relational issues surrounding fertility, infertility, assisted reproductive technology and new family forms. Her current research focuses on single women’s fertility options, including egg freezing and solo motherhood; motherhood after 40; and reproductive anxiety and choices. Her work provides insights about contemporary reproduction and relationships; in addition to her academic work, she hosts regular outreach seminars and events, and is a regular contributor to media debates.
References
- American Society for Reproductive Medicine, 2020. Patient Management and Clinical Recommendations During The Coronavirus (COVID-19) Pandemic. 17 March 2020. https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/covid-19/covidtaskforce.pdf (Accessed: 25 August 2020).
- Balen, A., 2020. Reflections of a fertility doctor through the Covid-19 crisis. Bionews: 18 May 2020. https://www.bionews.org.uk/page_149773 (Accessed: 25 August 2020).
- Boivin J., Harrison C., Mathur R., Burns G., Pericleous-Smith A., Gameiro S. Patient experiences of fertility clinic closures during the Covid-19 pandemic: Appraisals, coping, emotions. Hum. Reprod. 2020 doi: 10.1093/humrep/deaa218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qualitat. Res. Psychol. 2006;3(2):77–101. [Google Scholar]
- Braun V., Clarke V. reflecting on reflexive thematic analysis. Qualitat. Res. Sport Exercise Health. 2019;11(4):589–597. [Google Scholar]
- Braun V., Clarke V., Gray D. In: The Palgrave Handbook of Critical Social Psychology. Gough B., editor. Palgrave Macmillan; 2017. Innovations in qualitative methods; pp. 243–266. [Google Scholar]
- Braun V., Clarke V., Boulton E., Davey L., McEvoy C. The online survey as a qualitative research tool. Int. J. Soc. Res. Methodol. 2020 doi: 10.1080/13645579.2020.1805550. [DOI] [Google Scholar]
- Butterly, A., 2020. Coronavirus: ‘I’m scared my dream of becoming a mother are gone’. BBC News. 16 April 2020. https://www.bbc.co.uk/news/health-52279391 (Accessed: 25 August 2020).
- Cowan K. MQ: Transforming Mental Health and the Academy of Medical Sciences; 2020. Survey results: Understanding people’s concerns about the mental health impacts of the COVID-19 pandemic. https://acmedsci.ac.uk/file-download/99436893 (Accessed: 25 August 2020) [Google Scholar]
- De Berardis D., Mazza M., Marini S., Del Nibletto L., Serroni N., Pino M.C., Valchera A., Ortolani C., Ciarrocchi F., Martinotti G., Di Giannantonio M. Psychopathology, emotional aspects and psychological counselling in infertility: a review. Clin. Ter. 2014;165(3):163–169. doi: 10.7417/CT.2014.1716. [DOI] [PubMed] [Google Scholar]
- ESHRE COVID-19 Working Group A picture of medically assisted reproduction activities during the COVID-19 pandemic in Europe. Hum. Reprod. Open. 2020 doi: 10.1093/hropen/hoaa035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Society for Human Reproduction and Embryology, 2020a. Coronavirus Covid-19: ESHRE statement on pregnancy and conception. 19 March 2020. https://www.eshre.eu/Press-Room/ESHRE-News (Accessed: 25 August 2020).
- European Society for Human Reproduction and Embryology, 2020b. ESHRE Covid-19 working group to monitor scientific reports relevant to reproductive medicine. 25 March 2020. https://www.eshre.eu/Press-Room/ESHRE-News (Accessed: 25 August 2020).
- European Society for Human Reproduction and Embryology, 2020c. Assisted Reproduction and Covid-19. A statement from ESHRE for phase 1 – Guidance on fertility services during pandemic. 2 April 2020. https://www.eshre.eu/Press-Room/ESHRE-News (Accessed: 25 August 2020).
- Ferguson, D., 2020. Thousands lose last hope of having a baby as lockdown closes IVF clinics. The Guardian. 12 April 2020. https://www.theguardian.com/world/2020/apr/12/thousands-lose-last-hope-of-having-a-baby-as-lockdown-closes-ivf-clinics (Accessed: 25 August 2020).
- Ferrero, S., Scala C., Altieri, M., Barra, F., 2020. Impact of COVID-19 pandemic on the psychological status of infertile patients who had in vitro fertilization treatment interrupted or postponed. Presentation number: 0-279. ESHRE abstract. [DOI] [PubMed]
- Gameiro S., Boivin J., Dancet E.A.F., de Klerk C., Emery M., Lewis-Jones C., et al. ESHRE Guideline: Routine psychosocial care in infertility and medically assisted reproduction - A guide for fertility staff. Hum. Rep. 2015;30(11):2476–2485. doi: 10.1093/humrep/dev177. [DOI] [PubMed] [Google Scholar]
- Gürtin, Z., 2020. Fertility clinics are reopening but for many patients this won’t end the anxiety. The Guardian. 22 May 2020. https://www.theguardian.com/commentisfree/2020/may/22/fertility-clinics-reopening-patients-anxiety-coronavirus (Accessed: 25 August 2020).
- Holmes E.A., O’Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the Covid-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Fertilisation and Embryology Authority, 2019. Fertility treatment 2017: Trends and figures. HFEA, London, May 2019. https://www.hfea.gov.uk/media/3189/fertility-treatment-2017-trends-and-figures.pdf (Accessed: 25 August 2020).
- Human Fertilisation and Embryology Authority, 2020a. Coronavirus (Covid-19) Update: Updated statement for all clinics. 18 March 2020. https://www.hfea.gov.uk/treatments/covid-19-and-fertility-treatment/coronavirus-covid-19-previous-updates-for-professionals/ (Accessed: 25 August 2020).
- Human Fertilisation and Embryology Authority, 2020b. Coronavirus (Covid-19) Update: Restarting treatment. 1 May 2020. https://www.hfea.gov.uk/treatments/covid-19-and-fertility-treatment/coronavirus-covid-19-previous-updates-for-professionals/ (Accessed: 25 August 2020).
- Human Fertilisation and Embryology Authority, 2021. Fertility treatment 2019: Trends and figures. HFEA, London, May 2019. https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2019-trends-and-figures/ (Accessed: 11 November August 2020).
- Kale, S., 2020. Time is Precious in IVF: the women who fear they have lost their chance to have children. The Guardian. 27 April 2020. https://www.theguardian.com/society/2020/apr/27/time-precious-ivf-women-fear-lost-chance-to-have-children (Accessed: 25 August 2020).
- Karavadra B., Balen, A., Morris, E., 2020. A study to explore participants experiences of fertility services during the Covid-19 lockdown; a biphasic mixed methods study. Presentation number: 0-317. ESHRE abstract.
- Murray, J., 2020. IVF clinics set to reopen across UK. The Guardian. 1 May 2020. https://www.theguardian.com/society/2020/may/01/ivf-clinics-set-to-reopen-across-uk (Accessed: 25 August 2020).
- Nelson, Benjamin W., Pettitt, Adam K., Flannery, Jessica, Allen, Nicholas B., 2020. Rapid Assessment of Psychological and Epidemiological Correlates of COVID-19 Concern, Financial Strain, and Health-related Behavior Change in a Large Online Sample. PsyArXiv. April 13. doi: 10.31234/osf.io/jftze. [DOI] [PMC free article] [PubMed]
- Peterson B.D., Sejbaek C.S., Pirritano M., Schmidt L. Are severe depressive symptoms associated with infertility-related distress in individuals and their partners? Hum. Reprod. 2014;29(1):76–82. doi: 10.1093/humrep/det412. [DOI] [PubMed] [Google Scholar]
- Richards T., Sowcroft H. Patient and public involvement in covid-19 policy making. BMJ. 2020;2020(370) doi: 10.1136/bmj.m2575. [DOI] [PubMed] [Google Scholar]
- Romanski P.A., Bortoletto P., Rosenwaks Z., Schattman G.L. Delay in IVF treatment up to 180 days does not affect pregnancy outcomes in women with diminished ovarian reserve. Hum. Reprod. 2020:deaa137. doi: 10.1093/humrep/deaa137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner, C., 2020. ‘Lockdown may mean we never have children’: Hertbreak for thousands as coronavirus halts IVF. iNews. 15 April 2020. https://inews.co.uk/news/coronavirus-uk-latest-ivf-pregnant-fertility-418642 (Accessed: 25 August 2020).
- Terry G., Braun V. In: Collecting Qualitative Data: A Practical Guide to Textual, Media and Virtual Techniques. Braun V., Clarke V., Gray D., editors. Cambridge University Press; 2017. Short but often sweet: The surprising potential of qualitative survey methods; pp. 15–44. [Google Scholar]
- Toerien M., Wilkinson S. Exploring the depilation norm: A qualitative questionnaire study of women’s body hair removal. Qualitat. Res. Psychol. 2004;1(1):69–92. [Google Scholar]
- Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Turocy, J.M., Robles, A., Hercz, D., D'Alton, M., Forman, E.J., Williams, Z., 2020. The emotional impact of the SRM Guidelines on fertility patients during the COVID-19 pandemic. medRxiv.
- Webber, E., 2020. Lockdown makes us fear we’ll never be parents. Mail Online. 8 April 2020. https://www.dailymail.co.uk/femail/article-8197269/Couples-IVF-stopped-coronavirus-share-fear-theyll-never-parents.html (Accessed: 25 August 2020).
- Woman’s Hour, 2020. Fertility clinics during Covid-19. BBC Radio 4. 8 June 2020. https://www.bbc.co.uk/sounds/play/m000jvqx (Accessed: 25 August 2020).
- World Health Organization, 2020. Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (Accessed: 25 August 2020).
- Veiga A., Gianaroli L., Ory S., Horton M., Feinberg E., Penzias A. Assisted reproduction and COVID-19: a joint statement of ASRM, ESHRE and IFFS. Hum. Reprod. Open. 2020;3:hoaa033. doi: 10.1093/hropen/hoaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]