Abstract
A 50-year-old patient had presented with recalcitrant right lower extremity venous stasis ulceration, atrial fibrillation, and congestive heart failure. He had a history of a gunshot wound to the right thigh >30 years previously, which had been managed without surgery. Computed tomography angiography indicated a fistulous communication between the right superficial femoral artery and vein with massively dilated right iliofemoral venous and arterial systems. He was treated with stent-graft coverage of the superficial femoral arteriovenous fistula using a bell-bottom iliac limb endoprosthesis. This stent-graft accommodated the diameter asymmetry in the superficial femoral artery caused by the long-standing fistula and ameliorated the symptoms that had afflicted him for decades.
Keywords: Arteriovenous fistula, Stent-graft, Superficial femoral artery
Traumatic arteriovenous fistula (AVF) occur when both an artery and adjacent vein are injured, leading to abnormal flow directly from the artery to the vein. This shunt increases the venous volume and decreases peripheral vascular resistance. Penetrating trauma is the most common cause of traumatic AVFs, followed by percutaneous intervention and blunt trauma. Approximately 50% of all traumatic AVFs are located in the extremities.1 The clinical manifestations of traumatic AVFs vary and depend on the location, size, and duration of the fistula. Traumatic AVFs can be asymptomatic or symptomatic with pain, edema, and varicosities. Delayed presentation after trauma can lead to venous hypertension, high-output heart failure, arterial and venous dilation proximal to the fistula, arterial steal syndrome causing ulceration, and limb length discrepancy.2, 3, 4 The treatment options for traumatic AVF include surgical or endovascular repair.
We have described stent-graft repair of a long-standing superficial femoral AVF using a single bell-bottom iliac limb endoprosthesis designed for abdominal aortic aneurysms. The patient provided written informed consent for the report of his case details and imaging studies.
Case report
A 50-year-old man with hypertension, atrial fibrillation, and congestive heart failure had presented with a long history of right lower extremity swelling, pain, and medial malleolar ulcer present for 7 months. His medical history was pertinent for a gunshot injury of the right medial thigh >30 years previously that had been managed without surgery. He also noted intermittent palpitations and dyspnea on exertion. His physical examination was notable for marked swelling of the right lower extremity with moderate size varicosities and lipodermatosclerosis. A 4-cm ulcer with overlying eschar was present at the medial malleolus. A small linear scar was present at the distal medial thigh, consistent with a prior bullet wound. He had palpable right pedal pulses. The findings from the examination of the left lower extremity were normal. Duplex ultrasound indicated significant ectasia of the right iliofemoral arteries with elevated diastolic velocities. An AVF was noted at the distal superficial femoral artery with arterialization of venous flow. The ankle brachial index was 0.93. An echocardiogram was notable for elevated right atrial pressure. Computed tomography angiography precisely demonstrated the fistulous connection at the right distal superficial femoral artery with an ectatic right iliofemoral arterial system and early filling of the veins (Fig 1). He underwent endovascular repair of the superficial femoral AVF under general anesthesia. The proximal superficial femoral artery was exposed via a transverse incision. Antegrade access was obtained, and an 8F sheath was placed. The fistula was localized with intravascular ultrasound (Fig 2). A large arterial diameter discrepancy was noted between the proximal superficial femoral artery (25 mm) and distal superficial femoral artery (12 mm). Angiography confirmed a fistulous connection between the superficial femoral artery and vein. Opacification of the draining femoral vein was brisk. A 16F sheath was placed antegrade over a 0.035-in. stiff guide wire. We deployed an Excluder iliac bell-bottom limb endoprosthesis (16-mm proximal diameter, 27-mm distal diameter, 10-cm long; W.L. Gore & Associates, Flagstaff, Ariz) from the mid to distal superficial femoral artery. Because of the antegrade deployment, the 27-mm aspect of the limb was situated in the mid-superficial femoral artery, with the 16-mm aspect in the distal superficial femoral artery. Post-stenting balloon angioplasty was performed with a Coda balloon (Cook Medical, Inc, Bloomington, Ind). Completion angiography indicated abrogation of the fistula with prompt filling though the stent-graft (Fig 2). The patient was discharged on postoperative day 2 with rivaroxaban for his atrial fibrillation and aspirin. At follow-up at 2 months, the patient reported resolution of his right lower extremity pain and swelling. His ulcer had healed. An echocardiogram indicated normalization of the right atrial pressure. His atrial fibrillation had persisted despite an attempt at catheter ablation. Computed tomography angiography at 18 months confirmed patency of the stent-graft and closure of the fistula (Fig 3).
Fig 1.
Computed tomography angiogram demonstrating a large arteriovenous fistula (AVF) between the superficial femoral artery and femoral vein. The arrow indicates the fistulous connection. Note is made of dilated and tortuous superficial veins and ectatic arteries.
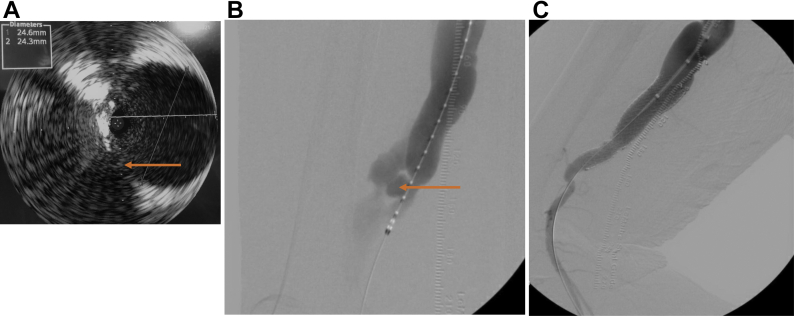
Fig 2.
A, Intravascular ultrasound within the superficial femoral artery was used to delineate the fistulous connection and obtain the diameter measurements. B, Digital subtraction angiogram revealing a pseudoaneurysm in the right distal superficial femoral artery with fistula connection to the femoral vein. C, Post-stenting angiogram indicating exclusion of the arteriovenous fistula (AVF) and pseudoaneurysm. The arrow indicates the fistulous connection.
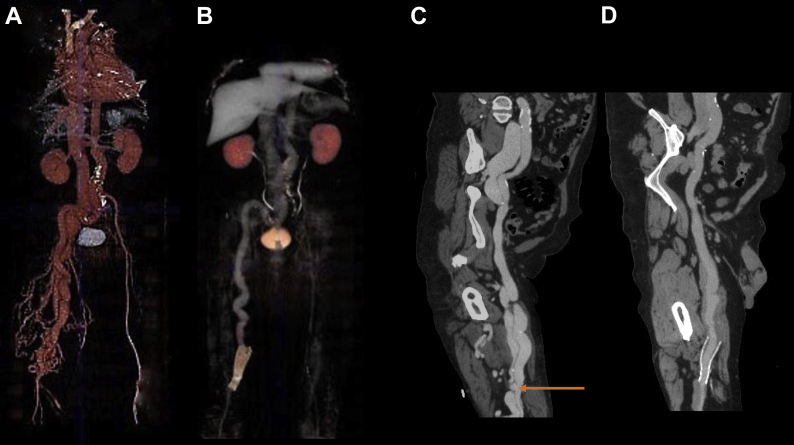
Fig 3.
Three-dimensional computed tomography angiographic reconstructions before (A) and 18 months after (B) superficial femoral artery stent-graft placement. Centerline reconstructions before (C) and 18 months after (D) superficial femoral artery stent-graft placement. The arrow indicates the fistulous connection.
Discussion
The treatment of AVF is based on the principle that the fistulous tract must be disconnected or occluded. The two approaches to repairing AVF are open and endovascular. Open repair involves obtaining proximal and distal control of the fistula and dividing the connection between the artery and vein. Open approaches to treat arteriovenous fistula include ligation, lateral suture repair, and resection with an end-to-end anastomosis or interposition grafting. Surgical repair of an established AVF can be treacherous because massive bleeding can occur from venous hypertension. An endovascular approach has the advantage of being minimally invasive and curtailing blood loss, which is particularly appealing for patients with heart failure. A multitude of reports have endorsed endovascular repair as first-line treatment.5, 6, 7, 8 Catheter-based therapeutic modalities include embolization (using coils, plugs, glue) and stent-graft placement. Embolization requires a slender fistulous tract to avoid embolization to the venous circulation and will not be generally feasible for mature AVFs. Stent-grafts have been used for the treatment of traumatic lower extremity AVFs and require appropriate fixation zones to obtain an effective seal. The stent-grafts used in previous reports have been of uniform diameters proximally and distally. The use of a bell-bottom iliac limb has conventionally been used to secure the seal in an ectatic common iliac artery during endovascular repair of aortoiliac aneurysms, obviating the need for internal iliac artery embolization and docking in the external iliac artery. The bell-bottom iliac limb has also been implemented as a bridging component for the iliac branch device in the setting of complex aortoiliac aneurysmal disease. In the present report, we have described the unique use of a single iliac bell-bottom limb endoprosthesis to secure seal in a superficial femoral artery of differing diameters that had resulted from a long-standing traumatic AVF.
The superficial femoral artery is a dynamic anatomic segment, and flexible stents are needed to avoid external deformation and fracture. Self-expandable stents are preferred in the superficial femoral artery. The Gore Viabahn endoprosthesis (W.L. Gore & Associates) is a self-expanding helical endoprosthesis consisting of heparin-bonded expanded polytetrafluoroethylene with an external nitinol support. Several trials have demonstrated excellent patency with Viabahn stent-grafts within the superficial femoral artery.9, 10, 11 The largest Viabahn stent-graft diameter is 13 mm and would not be able to provide seal in a 25-mm superficial femoral artery, as in our patient. The proximal iliac diameter of the bell-bottom Gore iliac endoprosthesis is standardized at 16 mm; the distal iliac diameters are flared up to 27 mm, which will provide seal for common iliac diameters of up to 25 mm. Similar to the Viabahn endoprosthesis, the graft material of the iliac limb is expanded polytetrafluoroethylene supported by nitinol. We exploited the flared “bell” portion of the iliac endograft and used antegrade deployment to accommodate the mismatch between the diameters of the mid and distal superficial femoral arteries. Other flared iliac limbs in the market include the Zenith Spiral-Z (Cook Medical) and the Endurant (Medtronic, Santa Rosa, Calif) endoprostheses. The anatomic features of a Zenith limb would not have provided seal in our patient because the largest available flared portion is 24 mm. Also, the Endurant limb has unsupported gaps in the stent design, which can be susceptible to kinking and occlusion when placed in the superficial femoral artery.12
We opted for endovascular repair for our patient because venous engorgement in conjunction with heart failure can pose difficulties for an open approach. The Gore iliac bell-bottom endoprosthesis provided an ideal solution. This self-expandable stent was able to provide excellent conformability in the tortuous and elongated superficial femoral artery. We were able to provide rapid symptom resolution for our patient using an endovascular approach. However, we were cognizant of the potential complications that can occur after abrogation of a long-standing AVF. The Branham effect is reflex bradycardia that occurs immediately after repair of an AVF due to the sudden increase in systemic vascular resistance. We performed our procedure with the patient under general anesthesia with vigilant hemodynamic monitoring. The proximal ectasia of the vessels might not be totally reversible after closure of the AVF, and long-term surveillance is mandatory.13 In our patient, the maximal superficial femoral artery diameter proximal to the stent-graft (20 mm) had remained unchanged at 18 months after repair of the AVF. There was nonocclusive mural thrombus within the stent-graft at 18 months with unknown long-term implications. Our patient will remain on long-term anticoagulation therapy for his atrial fibrillation. However, thrombus accumulation within a stent-graft has not been associated with thromboembolic events in multiple studies.14, 15, 16 In the setting of decreased blood flow after repair of an AVF, the massively dilated veins with stagnant flow can also fill with thrombus.17
Conclusions
Endovascular treatment of traumatic AVFs is promising. However, long-term follow-up is needed to determine durable patency. It will be intriguing to monitor the diameter of the arteries proximal to the fistula and assess whether the stent-graft seal will endure over time. Endovascular management can be a temporizing method and will not eliminate the option of a possible delayed conventional bypass graft in the event of stent-graft thrombosis or fistula recanalization.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Branco B.C., DuBose J.J., Zhan L.X., Hughes J.D., Goshima K.R., Rhee P., et al. Trends and outcomes of endovascular therapy in the management of civilian vascular injuries. J Vasc Surg. 2014;60:1297–1307. doi: 10.1016/j.jvs.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 2.Chaudry M., Flinn W.R., Kim K., Neschis D.G. Traumatic arteriovenous fistula 52 years after injury. J Vasc Surg. 2010;51:1265–1267. doi: 10.1016/j.jvs.2009.11.080. [DOI] [PubMed] [Google Scholar]
- 3.Gorsi U., Agarwal V., Savlania A., Behra A., Sandhu M.S. Endovascular management of lower limb arteriovenous fistula presenting 8 years after gunshot injury. Vasc Endovasc Surg. 2019;53:670–673. doi: 10.1177/1538574419870679. [DOI] [PubMed] [Google Scholar]
- 4.Kalender M., Baysal A.N., Dagil M., Gokmengil H. Chronic leg swelling and palpitation as a late complication of post-traumatic arteriovenous fistula: a case report. Trauma Case Rep. 2016;2:16–20. doi: 10.1016/j.tcr.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marin M.L., Veith F.J., Panetta T.F., Cynamon J., Barone H., Schonholz C., et al. Percutaneous transfemoral insertion of a stented graft to repair a traumatic femoral arteriovenous fistula. J Vasc Surg. 1993;18:299–302. [PubMed] [Google Scholar]
- 6.Parodi J.C., Schonholz C., Ferreira L.M., Bergan J. Endovascular stent-graft treatment of traumatic arterial lesions. Ann Vasc Surg. 1999;13:121–129. doi: 10.1007/s100169900230. [DOI] [PubMed] [Google Scholar]
- 7.White R., Krajcer Z., Johnson M., Williams D., Bacharach M., O’Malley E. Results of a multicenter trial for the treatment of traumatic vascular injury with a covered stent. J Trauma. 2006;60:1189–1195. doi: 10.1097/01.ta.0000220372.85575.e2. [DOI] [PubMed] [Google Scholar]
- 8.Glaser J.D., Kalapatpu V.R. Endovascular therapy of vascular trauma-current options and review of the literature. Vasc Endovasc Surg. 2019;53:477–487. doi: 10.1177/1538574419844073. [DOI] [PubMed] [Google Scholar]
- 9.Lammer J., Zeller T., Hausegger K.A., Schaefer P.J., Gschwendtner M., Mueller-Huelsbeck S., et al. Heparin-bonded covered stents versus bare-metal stents for complex femoropopliteal artery lesions: the randomized VIASTAR trial (Viabahn endoprosthesis with PROPATEN bioactive surface [VIA] versus bare nitinol stent in the treatment of long lesions in superficial femoral artery occlusive disease) J Am Coll Cardiol. 2013;62:1320–1327. doi: 10.1016/j.jacc.2013.05.079. [DOI] [PubMed] [Google Scholar]
- 10.Saxon R.R., Dake M.D., Vogelzang R.L., Katzen B.T., Becker G.J. Randomized, multicenter study comparing expanded polytetrafluoroethylene-covered endoprosthesis placement with percutaneous transluminal angioplasty in the treatment of superficial femoral artery occlusive disease. J Vasc Interv Radiol. 2008;19:823–832. doi: 10.1016/j.jvir.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Kedora J., Hohmann S., Garrett W., Munschaur C., Theune B., Gable D. Randomized comparison of percutaneous Viabahn stent grafts vs prosthetic femoral-popliteal bypass in the treatment of superficial femoral arterial occlusive disease. J Vasc Surg. 2007;45:10–16. doi: 10.1016/j.jvs.2006.08.074. [DOI] [PubMed] [Google Scholar]
- 12.Demanget N., Duprey A., Badel P., Orgeas L., Avril S., Geindreau C., et al. Finite element analysis of the mechanical performances of 8 marketed aortic stent-grafts. J Endovasc Ther. 2013;20:523–535. doi: 10.1583/12-4063.1. [DOI] [PubMed] [Google Scholar]
- 13.Melliere D., Hassen-Khodja R., Cormier J.M., Le Bas P., Mikati A., Ronsse H. Proximal arterial dilatation developing after surgical closure of long-standing posttraumatic arteriovenous fistula. Ann Vasc Surg. 1997;11:391–396. doi: 10.1007/s100169900067. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira N.F.G., Bastos Goncalves F.M., Hocks S.E., Ten Raa S., Ultee K.H.J., Rouwet E., et al. Clinical outcome and morphological determinants of mural thrombus in abdominal aortic endografts. J Vasc Surg. 2015;61:1391–1398. doi: 10.1016/j.jvs.2015.01.032. [DOI] [PubMed] [Google Scholar]
- 15.Maleux G., Koolen M., Heye S., Heremans B., Nevelsteen A. Mural thrombotic deposits in abdominal aortic endografts are common and do not require additional treatment at short-term and midterm followup. J Vasc Interv Radiol. 2008;19:1558–1562. doi: 10.1016/j.jvir.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Wegener M., Gorich J., Kramer S., Fleiter T., Tomczak R., Scharrer-Pamler R., et al. Thrombus formation in aortic endografts. J Endovasc Ther. 2001;8:372–379. doi: 10.1177/152660280100800406. [DOI] [PubMed] [Google Scholar]
- 17.Orrapin S., Arworn S., Rerkasem K. Acute deep vein thrombosis in venous aneurysm following closure of the chronic traumatic arteriovenous fistulae of the lower extremities. Case Rep Surg. 2016;2016:1375214. doi: 10.1155/2016/1375214. [DOI] [PMC free article] [PubMed] [Google Scholar]