Abstract
Background
Geographical setting is seldomly taken into account when investigating out-of-hospital cardiac arrest (OHCA). It is a common notion that living in rural areas means a lower chance of fast and effective helpwhen suffering a time-critical event. This retrospective cohort study investigates this hypothesis and compares across healthcare-divided administrative regions.
Methods
We included only witnessed OHCAs to minimize the risk that outcome was predetermined by time to caller arrival and/or recognition. Arrests were divided into public and residential. Residential arrests were categorized according to population density of the area in which they occurred. We investigated incidence, EMS response time and 30-day survival according to area type and subsidiarily by healthcare-divided administrative region.
Results
The majority (71%) of 8,579 OHCAs were residential, and 53.2% of all arrests occurred in the most densely populated cell group amongst residential arrests. This group had a median EMS response time of six minutes, whereas the most sparsely populated group had a median of 10 minutes. Public arrests also had a median response time of six minutes. 30-day survival was highest in public arrests (38.5%, [95% CI 36.9;40.1]), and varied only slightly with no statistical significance between OHCAs in densely and sparsely populated areas from 14.8% (95% CI 14.4;15.2) and 13.4% (95% CI 12.2;14.7).
Conclusion
Our study demonstrates that while EMS response times in Denmark are longer in the rural areas, there is no statistically significant decrease in survival compared to the most densely populated areas.
Keywords: Out-of-hospital cardiac arrest, OHCA, Survival, Geography, Population density, EMS response time
Abbreviations: OHCA, Out of Hospital Cardiac Arrest; EMS, Emergency Medical Services; HEMS, Helicopter Emergency Services; BLS, Basic Life Support; ALS, Advanced Life Support; AED, Automated External Defibrillator; IQR, Interquartile Range; GPS, Global Positioning System
Introduction
Out-of-hospital cardiac arrest (OHCA) is a well known time-critical condition, and has for a long time received great attention from both clinicians, prehospital administration and mainstream media. This partly results from the use of survival after OHCA as a proxy to benchmark the performance of the Emergency Medical Services (EMS). Worldwide, a culture of excellence has spread, encouraging friendly competition in increasing survival.1
This way of benchmarking has spread to the political and economic debate, and is used whenever a new hospital is to be built, as there is a general conception that experiencing an OHCA far away from an established hospital, with potentially longer EMS response times, decreases the chance of survival. Nevertheless, it remains debated whether specific geographical parameters influence important factors such as EMS response time and survival.
In Denmark, the EMS are obliged by contract to live up to a certain median EMS response time. This mechanism can work either of two ways: It could incline the EMS to station ambulances scattered across the country, but innately, remote areas are prone to longer response times if the vehicle which was originally stationed in the given area is otherwise occupied. It could also invoke a strategy of centralization to a certain degree, as most medical events will inevitably happen where most of the population is settled. This way, the EMS can keep the median response time down by reaching the majority of the events rapidly, and downgrade more remote areas with fewer events. It is a constant worry of politicians and citizens alike that more remote, thinly populated areas have a lower chance of a rapid response and lower odds of favourable outcome when an acute event like an OHCA occurs. This registry based, follow-up study aims to investigate whether living in rural, sparsely populated, areas comes at the cost of a lower chance of survival and simultaneously benchmark the five healthcare-divided administrative regions in Denmark.
Methods
Study setting
Denmark comprises 4,345,831 cells of 100 m by 100 m of mixed population density. The geography is divided into five healthcare-divided administrative regions as shown in supplementary, eFigure 1.
Each region is an administrative unit, responsible for the in- and out-of-hospital systems and services within itself. In each region the EMS consists of a dispatch center (one per region), ambulances providing basic life support (BLS) and physician-staffed cars and helicopters providing advanced life support (ALS). Furthermore, some regions employ paramedic-staffed cars providing ALS. Ambulance services providing BLS are either public (and thus administered by the region) or provided by private contractors. All physician-staffed cars (which are dispatched to all suspected OHCAs) and helicopters (HEMS) are public. Paramedic-staffed cars can be either.
The specific number of vehicles available to each region is largely undisclosed, and in part determined by the private contractors. Notable interregional differences between regions are that while the Central Denmark Region employs the largest amount of physcician staffed vehicles, the Zealand Region does not uliize this response form. HEMS is cross-regionally administrated, and three of such vectors were available from 2016 to 2018 where a fourth was implemented.2
Multiple volunteer responder programes were active in the time period, and while no one, national system was implemented until 2020, all regions had a form of volunteer responder programme in the period, either by SMS- or app activation.
All regions utilized a nationwide criterion-based emergency medical dispatch system (Danish Index) throughout the period, and there was one acute, percutan cardiac intervention center in each region except the Zealand Region from which patients are brought to Rigshospitalet in The Capital Region.3
Regardless of the administrative setup, the EMS services are publicly financed, and in each region, there is a political council which, on the basis of professional counseling and political considerations, determines the highest acceptable median EMS response time.4 Population density and comprisement varies across regions and geography.
Data collection
Inclusion data was based on OHCAs registered in the Danish Cardiac Arrest registry.
All initiated resuscitative efforts in Denmark are required to be registered by the EMS by filing a case report form to this registry. To allow geographical analysis, only reports filed after logging of GPS coordinates began in 2016 were collected, and subsequently matched to a geographical hectare by the coordinates of the ambulance on arrival.
Data on geographical extents of healthcare-divided administrative regions was gathered using data from the Danish Map Supply. Further, data on population density was acquired on a square hectare (cell) level, defined by the coordinate of the lower-left corner from a private data supplier.
Each cell is re-evaluated once per year, and as such the total number of hectares does not vary between years, but the population density of the cells might. In order to avoid person-sensitive data, the population density data received on sparsely populated areas was a mean over an area to a minimum of 1.8 people per cell.
Data analysis
Cell groups
Each cell has one representation for each year between 2016 and 2019. The pool of cells was divided into three groups with an approximately equal number of cells in each group according to population density. Population was defined as night-time population to reflect the amount of people residing in the cell and thereby correspond to residential arrests. Cells with a population of zero and a population so dense that it was not represented in all regions were not included in analysis. In addition, cells containing airports were not included in the analysis due to the mismatch between living population and actual flow of people.5 A cell was allowed to change groups each year. OHCAs that happened in public were treated as a separate group regardless of population and were not included in population and cell analysis.
Population was summed over the years and presented as an absolute number. Residential OHCAs were summarized according to population density group and subsequently, along with public OHCAs according to healthcare-divided administrative region. When presenting population density intervals, inclusion of af number in a group is denoted by a bracket [or] and exclusion of the number from the group is denoted by a parenthesis ().
Incidence
Arrests without valid GPS data or with missing data on the arrest site were excluded. Only bystander witnessed arrests were included. This was done in order to minimize pre-recognition time bias and optimize regional comparability. Incidence was summed for each cell across years according to the healthcare-divided administrative region and reported as raw numbers with column percentages.
OHCAs were categorized according to the case file as being either residential or any three of “Trafficked area”, “Nature area” or “Other”. OHCAs happening in nursing homes are defined as residential if the patient suffering the OHCA is registered as a permanent resident. All but residential arrests were categorized as public.
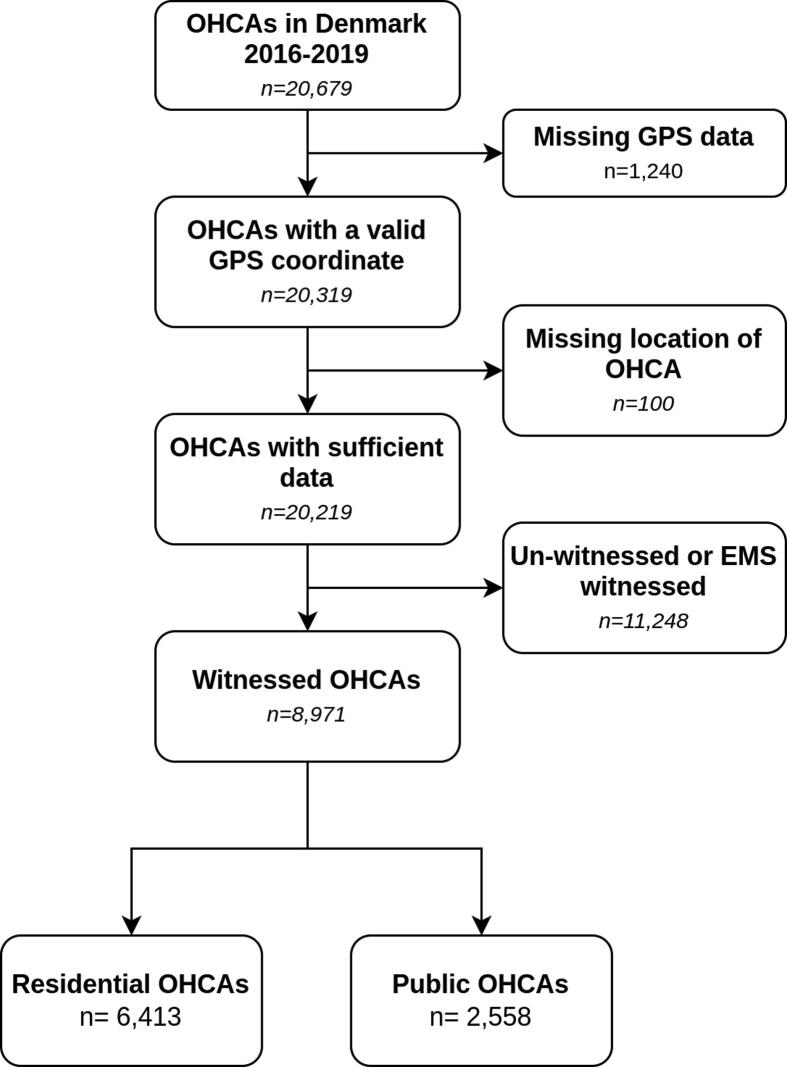
Inclusion and exclusion process is depicted in Fig. 1.
Fig. 1.
Inclusion flowchart.
EMS response times
Response times were treated univariately as time in minutes from the call received at the emergency medical dispatch center to the first EMS-vehicle at the scene. It was received from the registry as integers, and reported as medians with 25% and 75% quartiles and interquartile ranges (IQR) according to cell group.
Survival
Survival was reported unadjusted in univariate analysis as the percentage of patients with valid survival data who survived to day 30 after OHCA and 95% confidence intervals for rates (CI) were calculated and presented in brackets [;]. Survival was stratified according to cell group and healthcare-divided administrative region.
Data analysis was conducted using R statistical software version 4.1.1 and RStudio v. 1.4.1103 with attached packages for the data analysis.6., 7., 8., 9., 10., 11., 12., 13.
Data permissions
The study was approved by the Danish Data Protection Agency. The Danish National Committee on Health Research Ethics does not require ethical approval for registry-based studies. The use of the Danish Cardiac Arrest Registry used for the conduct of this study was approved in the North Denmark Region (2008-58-0028).
Results
Cell groups
The analysis included data for four years, and as such, the distribution of accumulated cells is shown in eTable 1 according to population density and region. 1,318 (0,008%) cells had a population so dense that it was not represented in all regions (greater than 311), 27,792 (0.16%) cells were airports, and 15,671,533 (90,2%) had no population. A total of 178,132 (1.0%) cells were not assigned to a region of which 4,307 (0.02%) had a population of 311 or less and above zero with no airport. The geographical distribution is depicted on a map in supplementary eFigure 2. For the purpose of this illustration, population data for 2019 is chosen.
The accumulated population in each cell group is shown in Table 1, stratified by region. Notably, the Capital Region had the largest span, with 28,663 and 140,941 cells in the least- and most densely populated cell group respectively. Correspondingly, these areas contributed 87,400 and 5,940,000 inhabitants respectively summed across four years. The other health-care administrative regions have a quite different distribution, with 60%-70% of the population living in the most densely populated cell groups compared to 93% in the Capital Region of Denmark and accordingly 28%-31% of the area being densely populated, as opposed to 64% in the Capital Region.
Table 1.
Population in 100,000 according to population density and region, 2016–2019*
| Cell group | Missing Region | Capital Region of Denmark | Central Denmark Region | North Denmark Region | Region of Southern Denmark | Region Zealand | Total |
|---|---|---|---|---|---|---|---|
| [1.8–4) | 0.03 | 0.87 | 4.73 | 3.39 | 3.95 | 4.96 | 17.9 |
| (4.2%) | (1.4%) | (9.3%) | (14.5%) | (12%) | (10.3%) | (8.2%) | |
| [4–12) | 0.1 | 3.35 | 10.51 | 5.24 | 7.1 | 10.79 | 37.1 |
| (13.9%) | (5.3%) | (20.7%) | (22.4%) | (21.6%) | (22.5%) | (16.9%) | |
| ≥12 | 0.6 | 59.41 | 35.65 | 14.75 | 21.79 | 32.3 | 164.5 |
| (83.3%) | (93.4%) | (70.1%) | (63.1%) | (66.4%) | (67.2%) | (74.9%) | |
| Total | 0.72 | 63.64 | 50.89 | 23.38 | 32.84 | 48.05 | 219.5 |
| (100%) | (100%) | (100%) | (100%) | (100%) | (100%) | (100%) |
[]denotes inclusion of number, () denotes exclusion.
Rounding errors occur.
Incidence
Table 2 shows the distribution of OHCAs stratified by cell group and healthcare-divided administrative region. A total of 392 (4.4%) OHCAs were witnessed, but happened in a cell that was not included in the analysis (eg. population of zero, more than 311 or in an airport). More than half of all the arrests (53.2%) occurred in the most densely populated cell group. OHCAs that took place in residential areas accounted for 6,021 (70,2%).
Table 2.
Distribution of OHCA according to cell group and region.
| Cell group | Capital Region | Central Denmark Region | North Denmark Region | South Denmark Region | Zealand Region | Total |
|---|---|---|---|---|---|---|
| [1.8–4) | 39 | 111 | 84 | 87 | 115 | 436 |
| (1.6%) | (6.0%) | (7.8%) | (4.8%) | (8.6%) | (5.1%) | |
| [4–12) | 108 | 250 | 173 | 276 | 215 | 1022 |
| (4.3%) | (13.6%) | (16.0%) | (15.4%) | (16.0%) | (11.9%) | |
| ≥12 | 1549 | 956 | 495 | 928 | 635 | 4563 |
| (61.5%) | (51.9%) | (45.8%) | (51.7%) | (47.3%) | (53.2%) | |
| Public | 822 | 525 | 329 | 504 | 378 | 2558 |
| (32.6%) | (28.5%) | (30.4%) | (28.1%) | (28.1%) | (29.8%) | |
| Total | 2518 | 1842 | 1081 | 1795 | 1343 | 8579 |
| (100%) | (100%) | (100%) | (100%) | (100%) | (100%) |
[]denotes inclusion of number, () denotes exclusion.
EMS response times
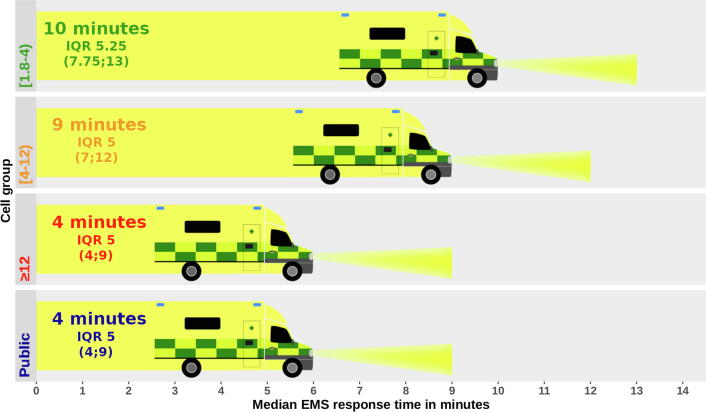
A total of 732 (8.2%) arrests had missing values for EMS response time. Median EMS response times in cell groups ranged from 10 (IQR 5.25) minutes in the least densely populated cell group to 6 (IQR 5) minutes in the most populated cell group and public arrests as depicted in Fig. 2. Overall, EMS response time shortened as population density increased, while the spread of the interquartile range was uniformly between two minutes less and three minutes more than the median. Individual EMS response times spanned from 1 to 240 minutes.
Fig. 2.
Median EMS response time in minutes according to population density. Front end of ambulances showing median response time, end of headlight depicting 3rd quartile and IQR presented under the median as text on to the left.
Survival
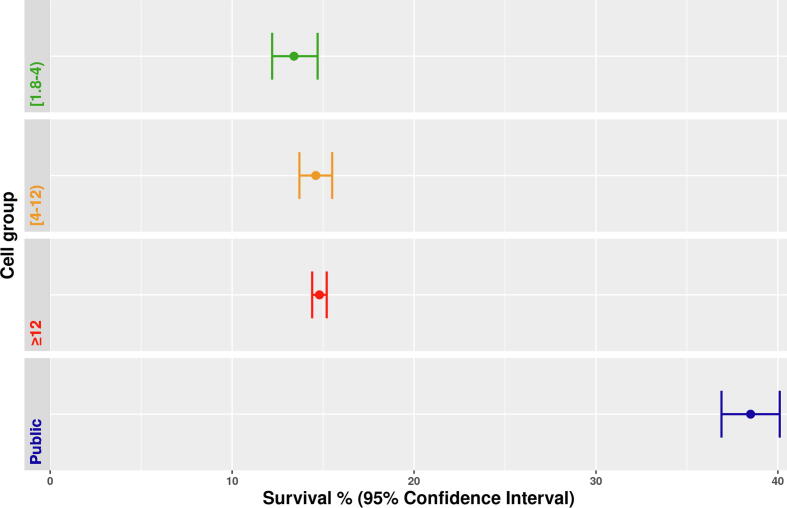
Survival data was missing in 430 (4.8%) of included OHCAs. Of the remaining, a total of 1,802 (21.1%) survived to 30 days after OHCA. Of the survivors, 66 (3.7%) happened in areas not included in analysis (eg. population of zero, more than 311 or in an airport). Fig. 3 depicts survivors in percentages according to cell group as a dot with 95% CI. In the least populated cell group survival was 13.4% (95% CI 12.2;14.7). In the medium populated cell group survival was 14.6% 95% CI13.7;15.5), and in the most densely populated cell group 14.8% (95% CI 14.4;12.2). OHCAs that occurred in public had the highest survival with a rate of 38.5% (95% CI 36.9;40.1).
Fig. 3.
Survival in % according to cell group. Dot represents survival percentage and lines indicate 95% confidence interval (CI). Colouring of dots and lines are according to cell group.
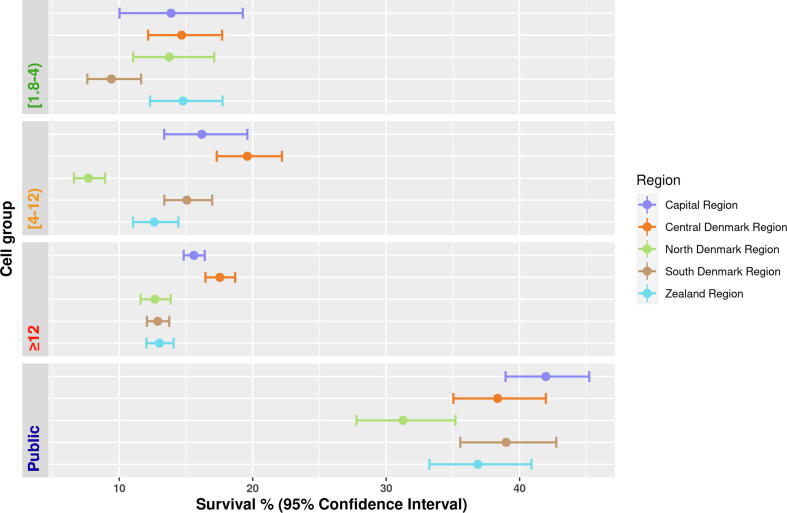
When further stratifying on healthcare-divided administrative region, as is depicted in Fig. 4, the overall picture remains the same, with significantly higher survival rate in public arrests, and generally overlapping 95% CIs. In the least densely populated cell group, the South Denmark Region stands out with a survival rate of 9.41% (95% CI 7.6;11.6) but with 95% CI overlapping with both North Denmark Region and Capital Region. In the medium densely populated cell group, the North Denmark Region falls behind with a survival rate of 7.7% (95% CI 6.6;8.9) with no overlaps of 95% CI. In the most densely populated cell group, the Capital Region and the Central Denmark Region have the highest survival rates of 15.6% (95% CI 14.3;16.4) and 17.5% (95% CI 16.5;18.7). The remaining three regions have lower survival rates with 95% CIs that do not overlap with the two first. For public arrests, survival rates are lowest in the North Denmark Region at 31.3% (95% CI27.8;35.2) and highest in the Capital Region at 42.0% (95% CI 39.0;45.2), both with 95% CIs overlapping other regions.
Fig. 4.
Survival in % according to cell group and healthcare-divided administrative region. Dot represents survival percentage and lines indicate 95% confidence interval (CI). Colouring of dots and lines are according to healthcare-divided.
Discussion
This study aimed to investigate differences in residential OHCAs across different geographical areas, compare them to public OHCAs and further stratify by healthcare-divided administrative region. In summary, by far the largest proportion of OHCAs occurred in the most densely populated third of Denmark, but surprisingly the survival rate was not significantly lower in less populated areas. Survival rates after public OHCAs were found to be significantly higher than all residential arrests, in accordance with previous findings.14., 15.
Looking at differences across the healthcare-divided administrative regions, it is clear that not one region stands out across cell groups. While some particular administrative regions do perform either better or worse in specific cell groups, the same administrative regions have survival rates comparable to the other regions in other cell groups. This indicates that the actual pre-hospital effort does not vary significantly between regions, and considering that each healthcare-divided administrative region only has one primary intervention center it would seem that differences in geography and demographic composition between the regions are determinants of specific survival rates in different cell groups.
Concerning the consequences of having a cardiac arrest in a rural area in Denmark, the disparities in the EMS response time are relatively high with a difference in median times between the most densely populated and rural areas of four minutes. Although the response times in general may not be long, there is still a rough 50% increase between the highest and the lowest median, thus long enough for single-person cardiopulmonary resuscitation (CPR) quality and survival to decrease significantly.16., 17.
Previous similar studies have shown an apparent increase in OHCA survival in more densely populated areas compared to less densely populated areas.18., 19., 20., 21. However, other studies find no significant differences.22., 23. One study found, in line with our finding, that while in crude analysis survival-rate depended on rurality, it was not an independent prognostic factor.24 Most previous studies included both witnessed and unwitnessed arrests. Doing so factors that are non-modifiable by the EMS plays a pivotal role in determining outcome and is, by extension, less relevant to the political debate.
When examining witnessed arrests only, on the other hand, the only parameters that are not in the healthcare providers' hands are delay from discovery of OHCA to phone call which we assume to be short, and the actual quality of CPR provided by the witness which is actively sought to be improved by dispatcher assisted CPR.25., 26.
Previous studies have used the actual number of survivors pr. 100,000 inhabitants not taking geographical variance into account. This is, as depicted in Fig. 2, associated with a large difference in EMS response time, a key parameter in securing long-term survival.17., 27., 28., 29. To adjust for or stratify by EMS response is an irrelevant strategy when benchmarking administrative regions, as it is one of the key parameters of interest that the healthcare-divided administrative regions can influence in order to improve outcome.
When comparing with previous studies of rural versus urban another aspect to consider is the definition of rurality, which is innately relative, and followingly applicability of both present study and previous depends on this very definition. There is no uniform standard for defining rurality, and present study uses a definition based on the Danish geography and a granulation of hectare level, allowing a minimum population density corresponding to 180 per km2. Correspondingly, categories were set to [180–400), [400–1200) and ≥1200 pr km2 where previous studies have defined the most rural categories with a maximum of between 10 and 663.18., 19., 20., 22., 23., 30.
The choice to live rurally alone might not entirely be a matter of choice, as it is influenced by both social and economic capabilities, but it is a parameter that the healthcare-divided administrative regions and the EMS cannot be held accountable for. Interestingly, the hermitization is most common in the most densely populated healthcare-divided administrative region, the Capital Region.31
The health care system is already trying to mitigate the possible consequences of potential prolonged EMS response times in more rural areas by initiating a number of citizen responder programs. This is true both in Denmark and internationally.32., 33., 34., 35. Whether or not this is part of the explanation for the absence of difference in survival despite the longer EMS response times as uncovered in this study remains to be explored.
Strengths
This study was performed on a national scale, with inclusion criteria that is uniform across all healthcare-divided administrative regions. Furthermore, each patient chart is subsequently manually validated by health care professionals to ensure correctness of inclusion and each variable. As such, not only is capture as complete as can be, but data is also of high quality.
Limitations
First, only including witnessed arrests limits the study population. We do, however, argue that this exact population, regardless of size, is the one best suited for the purpose of this study.
Second, what happens at the site of arrest during the EMS response time is unaccounted for, and might influence outcome.
Third, some cells were defined by a coordinate in a south-eastern shoreline and thus could not be linked to a healthcare-divided administrative region, as shoreline has no such geographical definition. This will, however, only affect the summation of cells within each healthcare-divided administrative region and not OHCA data, as these allow tying each OHCA to a region and a cell.
Fourth, the health-care system in Denmark is not to be directly compared to the health-care system in every other setup, neither in terms of pre-hospital setup nor post-resuscitative care. This is especially true when comparing to other countries that might not have a publicly-fininanced health care systems, and comparative research is required in diffrerent healt-care in before assuming applicability.
Fifth, this study did not include analysis of population-centered data, which could in part introduce bias. Further studies should explore the impact difference in age, socioeconimic status and burden of comobidity across area categories.
Sixth, while Danish Society of Cardioligsts publish nationwide recommandation for post-resuscitative care, cross-regional differences in specific practices for which we have not accounted may occur.
Conclusion
Our study shows that in Denmark, despite longer EMS response times to residential OHCAs in rural areas, survival is not significantly different from OHCAs in urban areas of Denmark, and regional differences across cell groups was absent. Only arrests that happened in public locations had a significantly higher survival rate.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We would like to extend our sincerest thanks to the Emergency Medical Services personnel in Denmark who have completed the case report forms for the Danish Cardiac Arrest Register and to the board of the Danish Cardiac Arrest Registry for facilitating the data collection and usage. Further thanks to Ambition for facilitating use of geographical data.
Funding sources
The Danish Cardiac Arrest registry and this study are supported by the Danish Foundation TrygFonden.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100208.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Ten Programs – Global Resuscitation Alliance https://www.globalresuscitationalliance.org/ten-programs/ [accessed July 6, 2021].
- 2.Bases. https://www.akutlaegehelikopter.dk/en/about-us/bases/ [accessed January 10, 202].
- 3.Andersen M.S., Johnsen S.P., Sørensen J.N., Jepsen S.B., Hansen J.B., Christensen E.F. Implementing a nationwide criteria-based emergency medical dispatch system: a register-based follow-up study. Scand J Trauma Resusc Emerg Med. 2013;21:53. doi: 10.1186/1757-7241-21-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danske Regioner - Regional Denmark. https://www.regioner.dk/services/in-english/regional-denmark [accessed August 10, 2021]
- 5.Gantzel Nielsen C., Andelius L.C., Hansen C.M., et al. Bystander interventions and survival following out-of-hospital cardiac arrest at Copenhagen International Airport. Resuscitation. 2021;162:381–387. doi: 10.1016/j.resuscitation.2021.01.039. [DOI] [PubMed] [Google Scholar]
- 6.R Core Team. R. R Foundation for Statistical Computing; 2021. https://www.R-project.org/.
- 7.Kahle D, Wickham H. R Package “Ggmap.”; 2005. http://journal.r-project.org/archive/2013-1/kahle-wickham.pdf.
- 8.Harrell Jr Frank E. With contributions from Charles Dupont and many others. R Package “Hmisc.”; 2021. https://CRAN.R-project.org/package=Hmisc.
- 9.Hadley Wickham and Evan Miller. R Package “Haven.”; 2021. https://CRAN.R-project.org/package=haven.
- 10.Dowle Matt, Srinivasan Arun. R Package “Data.Table.”; 2021. https://CRAN.R-project.org/package=data.table.
- 11.Pebesma EJ, Bivand RS. R Package “Sp.”; 2005. https://cran.r-project.org/doc/Rnews/.
- 12.Bivand Roger, Keitt Tim, Rowlingson Barry. R Package “Rgdal.”; 2021. https://CRAN.R-project.org/package=rgdal.
- 13.RStudio Team. RStudio. RStudio; 2021. http://www.rstudio.com/.
- 14.Folke F., Gislason G.H., Lippert F.K., et al. Differences Between Out-of-Hospital Cardiac Arrest in Residential and Public Locations and Implications for Public-Access Defibrillation. Circulation. 2010;122:623–630. doi: 10.1161/CIRCULATIONAHA.109.924423. [DOI] [PubMed] [Google Scholar]
- 15.Sondergaard K.B., Wissenberg M., Gerds T.A., et al. Bystander cardiopulmonary resuscitation and long-term outcomes in out-of-hospital cardiac arrest according to location of arrest. Eur Heart J. 2019;40:309–318. doi: 10.1093/eurheartj/ehy687. [DOI] [PubMed] [Google Scholar]
- 16.Hightower D., Thomas S.H., Stone C.K., Dunn K., March J.A. Decay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26:300–303. doi: 10.1016/s0196-0644(95)70076-5. [DOI] [PubMed] [Google Scholar]
- 17.Shahzleen R., Mads W., Fredrik F., et al. Association of Bystander Cardiopulmonary Resuscitation and Survival According to Ambulance Response Times After Out-of-Hospital Cardiac Arrest. Circulation. 2016;134:2095–2104. doi: 10.1161/CIRCULATIONAHA.116.024400. [DOI] [PubMed] [Google Scholar]
- 18.Møller S.G., Rajan S., Møller-Hansen S., et al. Pre-hospital factors and survival after out-of-hospital cardiac arrest according to population density, a nationwide study. Resusc Plus. 2020;4 doi: 10.1016/j.resplu.2020.100036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nehme Z., Andrew E., Cameron P.A., et al. Population density predicts outcome from out-of-hospital cardiac arrest in Victoria, Australia. Med J Aust. 2014;200:471–475. doi: 10.5694/mja13.10856. [DOI] [PubMed] [Google Scholar]
- 20.Yasunaga H., Miyata H., Horiguchi H., et al. Population density, call-response interval, and survival of out-of-hospital cardiac arrest. Int J Health Geogr. 2011;10:26. doi: 10.1186/1476-072X-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Masterson S., Wright P., O’Donnell C., et al. Urban and rural differences in out-of-hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42–47. doi: 10.1016/j.resuscitation.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Mathiesen W.T., Bjørshol C.A., Kvaløy J.T., Søreide E. Effects of modifiable prehospital factors on survival after out-of-hospital cardiac arrest in rural versus urban areas. Crit Care. 2018;22 doi: 10.1186/s13054-018-2017-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strömsöe A., Svensson L., Claesson A., Lindkvist J., Lundström A., Herlitz J. Association between population density and reported incidence, characteristics and outcome after out-of-hospital cardiac arrest in Sweden. Resuscitation. 2011;82:1307–1313. doi: 10.1016/j.resuscitation.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 24.Hsu Y.C., Wu W.T., Huang J.B., Lee K.H., Cheng F.J. Association between prehospital prognostic factors and out-of-hospital cardiac arrest: Effect of rural-urban disparities. Am J Emerg Med. 2020:30950–30955. doi: 10.1016/j.ajem.2020.10.054. Published online October 27, 2020:S0735-6757(20)30950-5. [DOI] [PubMed] [Google Scholar]
- 25.Hardeland C., Claesson A., Blom M.T., et al. Description of call handling in emergency medical dispatch centres in Scandinavia: recognition of out-of-hospital cardiac arrests and dispatcher-assisted CPR. Scand J Trauma Resusc Emerg Med. 2021;29:88. doi: 10.1186/s13049-021-00903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rasmussen S.E., Nebsbjerg M.A., Krogh L.Q., et al. A novel protocol for dispatcher assisted CPR improves CPR quality and motivation among rescuers-A randomized controlled simulation study. Resuscitation. 2017;110:74–80. doi: 10.1016/j.resuscitation.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 27.Holmén J., Herlitz J., Ricksten S., et al. Shortening Ambulance Response Time Increases Survival in Out-of-Hospital Cardiac Arrest. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2020;9 doi: 10.1161/JAHA.120.017048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bürger A., Wnent J., Bohn A., et al. The Effect of Ambulance Response Time on Survival Following Out-of-Hospital Cardiac Arrest. Dtsch Arzteblatt Int. 2018;115:541–548. doi: 10.3238/arztebl.2018.0541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park J.H., Song K.J., Shin S.D., Hong K.J. Does second EMS unit response time affect outcomes of OHCA in multi-tiered system? A nationwide observational study. Am J Emerg Med. 2021;42:161–167. doi: 10.1016/j.ajem.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Park J.H., Ro Y.S., Shin S.D., Song K.J., Hong K.J., Kong S.Y. Dispatcher-assisted bystander cardiopulmonary resuscitation in rural and urban areas and survival outcomes after out-of-hospital cardiac arrest. Resuscitation. 2018;125:1–7. doi: 10.1016/j.resuscitation.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 31.Wanscher AHM. Andelen af danskere på mindst 65 år, der bor alene, er historisk lav. https://www.dst.dk/da/Statistik/bagtal/2019/2019-23-12-aeldre-der-bor-alene [accessed August 31, 2021].
- 32.Andelius L., Malta Hansen C., Lippert F.K., et al. Smartphone Activation of Citizen Responders to Facilitate Defibrillation in Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol. 2020;76:43–53. doi: 10.1016/j.jacc.2020.04.073. [DOI] [PubMed] [Google Scholar]
- 33.Metelmann C., Metelmann B., Kohnen D., et al. Smartphone-based dispatch of community first responders to out-of-hospital cardiac arrest - statements from an international consensus conference. Scand J Trauma Resusc Emerg Med. 2021;29:29. doi: 10.1186/s13049-021-00841-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scquizzato T., Pallanch O., Belletti A., et al. Enhancing citizens response to out-of-hospital cardiac arrest: A systematic review of mobile-phone systems to alert citizens as first responders. Resuscitation. 2020;152:16–25. doi: 10.1016/j.resuscitation.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pijls R.W.M., Nelemans P.J., Rahel B.M., Gorgels A.P.M. A text message alert system for trained volunteers improves out-of-hospital cardiac arrest survival. Resuscitation. 2016;105:182–187. doi: 10.1016/j.resuscitation.2016.06.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.