Abstract
Blood eosinophils are a potentially useful biomarker for guiding inhaled corticosteroid (ICS) treatment decisions in COPD. We investigated whether existing blood eosinophil counts predict benefit from initiation of ICS compared to bronchodilator therapy.
We used routinely collected data from UK primary care in the Clinical Practice Research Datalink. Participants were aged ≥40 years with COPD, were ICS-naïve and starting a new inhaled maintenance medication (intervention group: ICS; comparator group: long-acting bronchodilator, non-ICS). Primary outcome was time to first exacerbation, compared between ICS and non-ICS groups, stratified by blood eosinophils (“high” ≥150 cells·µL−1 and “low” <150 cells·µL−1).
Out of 9475 eligible patients, 53.9% initiated ICS and 46.1% non-ICS treatment with no difference in eosinophils between treatment groups (p=0.71). Exacerbation risk was higher in patients prescribed ICS than those prescribed non-ICS treatment, but with a lower risk in those with high eosinophils (hazard ratio (HR) 1.04, 95% CI 0.98–1.10) than low eosinophils (HR 1.19, 95% CI 1.09–1.31) (p-value for interaction 0.01). Risk of pneumonia hospitalisation with ICS was greatest in those with low eosinophils (HR 1.26, 95% CI 1.05–1.50; p-value for interaction 0.04). Results were similar whether the most recent blood eosinophil count or the mean of blood eosinophil counts was used.
In a primary care population, the most recent blood eosinophil count could be used to guide initiation of ICS in COPD patients. We suggest that ICS should be considered in those with higher eosinophils and avoided in those with lower eosinophils (<150 cells·µL−1).
Short abstract
ICS-naïve COPD patients who start on ICS and whose most recent blood eosinophil count is <150 cells·µL−1 have a 15% higher risk of future exacerbation compared to those with a count ≥150 cells·µL−1. ICS should be reserved for those with higher blood eosinophils. https://bit.ly/3CiEFb9
Introduction
Guidelines for pharmacological management of COPD recommend the addition of inhaled corticosteroids (ICS) to bronchodilator therapy for worsening symptoms (frequent exacerbations or persistent breathlessness) [1]. Although there is some benefit in reducing exacerbations, long-term effects of ICS on lung function decline and mortality are unclear. ICS use is associated with adverse effects including pneumonia and osteoporotic fractures, as well as being cumulatively expensive [2, 3]. Nevertheless, ICS compounds are widely used in clinical practice [4]. In UK primary care, almost two in five patients prescribed an ICS did not meet criteria for this treatment [3]. There is therefore an urgent need to improve clarity around when ICS should be prescribed.
Blood eosinophil count has gained interest as a biomarker for identifying COPD patients more likely to benefit from ICS treatment. Many post hoc analyses, using various eosinophil count thresholds, have shown greater response to ICS-containing preparations in patients with a higher baseline blood eosinophil count [5]. In addition, there have been recent prospective evaluations of ICS response and peripheral blood eosinophil count [6, 7]. However, patients included in such trials are not representative of the real-world population, as inclusion is centred around patients already established on inhaled maintenance medication. This is especially important in primary care, where patients are often diagnosed and where step-up or initiation of ICS therapy is most often considered [8, 9].
General practice research databases, which routinely collect anonymised information from patient consultations and are linked at patient level with hospital and national statistics, provide an efficient and well-validated way of answering clinical questions relevant to primary care involving large sample sizes [10].
Using the Clinical Practice Research Datalink (CPRD), we investigated whether the most recent peripheral blood eosinophil count at the point of an inhaled treatment step-up or initiation decision could predict treatment outcomes, in a COPD ICS-naïve primary care population from 2005–2015.
Methods
Study design
We used a new-user active-comparator study design [11] and compared time to first exacerbation of those commencing inhaled maintenance medication containing an ICS (ICS group) with those not containing an ICS (non-ICS group), looking for effect modification by baseline blood eosinophil count. Additional methods are presented in the supplementary material.
Data source and included population
The CPRD, a large database of UK general practice clinical records, individually linked with Hospital Episode Statistics records, was used. Included patients were those with data linkage aged ≥40 years with a COPD diagnosis code, a valid blood eosinophil count (see later for definition), a history of current/past smoking and spirometry diagnostic of COPD (forced expiratory volume in 1 s/forced vital capacity ratio <0.7), who were starting a new inhaled maintenance medication for COPD in the period 1 January 2005 to 31 August 2015 (index date). Our range of index dates were chosen to be after introduction of Quality and Outcomes Framework targets in UK primary care which improved coding of COPD and spirometry [12], but before blood eosinophils were promoted as a potential biomarker, which might have influenced prescribing choices. In addition, recruited patients were ICS-naïve, due to concern that steroid treatment might suppress blood eosinophil values [13], which was defined as no ICS prescriptions and fewer than three oral corticosteroid prescriptions in the previous 12 months. Excluded patients were those with a diagnosis of bronchiectasis, alpha-1 antitrypsin deficiency, interstitial lung disease or cystic fibrosis. Those with an active diagnosis of asthma (coded in the past 2 years versus a historical code on the medical records) were excluded from the primary analysis. Follow-up continued until the earliest of the date the practice stopped providing data to CPRD, the patient died or left the practice or 29 February 2016. Eligible patients were required to have ⩾24 months continuous data, 6 months before and after the index date, to ensure adequate recording of baseline covariates and outcomes.
Exposures
The exposure was a new ICS-containing inhaled maintenance medication (ICS, ICS/long-acting β2-agonist (LABA), or ICS/long-acting muscarinic antagonist (LAMA)), compared with a non-ICS treatment (LABA, LAMA or LAMA/LABA). A new inhaled maintenance medication was defined as a prescription for that drug category that had not been issued in the previous 12 months. Those commencing triple therapy were excluded to enable a better comparison between ICS and non-ICS therapies, and to minimise confounding, as in similar studies [14]. While outside guidelines, prescriptions for ICS monotherapy were included, as this is a common initial treatment for COPD in other database studies [15] and we wanted to reflect real-life practice. Designated prescriptions had to be continued for a minimum of 6 months after the index date (for the primary analysis). Continuous use was defined as treatment duration totalling ⩾90 days’ supply, similar to methods used in a previous study of ICS in COPD [14]. Patients that had a change or addition of another inhaled medication within 30 days of the index date which would result in a change of comparator group were excluded. Sensitivity analyses (supplementary material) explored the effect on results of managing medication adherence and changes of drug class.
To examine a potential dose–response relationship in ICS-containing medications, the strength of ICS prescribed on the index date was stratified into low, medium and high (corresponding to estimated equivalent daily doses of beclomethasone dipropionate of ≤500 µg, >500–1000 µg and >1000 µg, respectively), as used elsewhere [14], but higher than standard clinical categorisations for asthma [16].
Covariates
Baseline information included demographic, disease and general health characteristics. A valid blood eosinophil count was the most recently recorded value in the 2 years prior to the index date, based on simplicity of use for primary care clinicians. For the primary analysis, eosinophil values within 2 weeks of an exacerbation, pneumonia episode or elevated C-reactive protein (>100 mg·L−1) were excluded as these would not reflect baseline state. An eosinophil threshold of <150 cells·µL−1 was used to categorise patients into the low-eosinophil group and ≥150 cells·µL−1 for the high-eosinophil group. This primary threshold was chosen in response to unpublished work at the time of study set-up [17], but with multiple alternative secondary thresholds assessed.
Outcomes
The primary outcome was time to first exacerbation following the index date, which was selected as the outcome of most relevance to patients [18]. Exacerbations were defined as any of the following: code for COPD exacerbation; code for lower respiratory tract infection; prescription of exacerbation-specific antibiotic, e.g. amoxicillin/macrolides/doxycycline and oral steroid for 5–14 days; symptom of exacerbation (cough, breathlessness or sputum) plus prescription of exacerbation-specific antibiotic or oral steroid; hospital admission with COPD or acute respiratory cause as the primary cause of hospitalisation; or a COPD exacerbation code within a hospitalisation episode. Exacerbation events defined by prescriptions alone and occurring on the same date as spirometry, or a code implying rescue-pack administration, were excluded, as this suggested a visit for annual COPD review with provision of standby medication, rather than an exacerbation.
Secondary outcomes analysed were pneumonia episodes, and hospitalisations and death due to COPD, pneumonia or any cause (all time-to-event following index date). A pneumonia episode was defined as a CPRD code for pneumonia, hospital admission with an International Classification of Diseases (ICD)-10 pneumonia code, or a death certificate with pneumonia listed as a cause.
All outcome events occurring within 2 weeks of a previous episode, were counted as the same event. Events within 30 days of the index date were excluded to reduce protopathic bias, as in other studies [14].
Missing data
Handling of missing data is detailed in the supplementary material.
Statistical analysis
Stata (release SE13 64-bit) was used for all analysis. Data are presented as mean±sd, median (interquartile range (IQR)) or hazard ratios (HR) with 95% confidence intervals. Cox proportional hazards models assessed disease outcomes after index date, by drug group (ICS versus non-ICS). Inclusion of an interaction term looked for effect modification by blood eosinophils (due to the difference in response to treatment between eosinophil groups being more relevant than the effect size itself). Covariates were adjusted for if significant (p<0.10) in univariate Cox analysis, to reduce confounding by indication in terms of ICS versus non-ICS group.
Pre-specified subgroup analyses by baseline exacerbation frequency, ICS dose and history of asthma were performed (and by smoking status post hoc). A history of frequent exacerbations was defined as two or more in the year prior to the index date and less-frequent exacerbations defined as fewer than two in the year prior to the index date (exacerbations included hospitalisations for exacerbations, as defined earlier). Multiple sensitivity analyses explored whether different ways of defining the population (e.g. inclusion/exclusion of those with asthma and atopy) and alternative methods for handling medication adherence and outcome timing had any impact on overall results (full details in supplementary material).
Results
Characteristics of included population
There were 30 378 eligible patients, of whom 18 235 (60.0%) had a valid eosinophil count in primary care records. A further 8760 met exclusion criteria, leaving 9475 patients for analysis (supplementary figure S1).
Table 1 shows baseline characteristics and distribution of patients between ICS and non-ICS treatment groups. Patients were more likely to be prescribed ICS therapy if they were younger, female, had previous asthma, more severe airflow limitation, or with a higher baseline exacerbation frequency, oral steroid use or hospital admissions (supplementary table S1). There were 4371 (46%) patients in the non-ICS group (prescribed LABA 19%, LAMA 77%, LAMA/LABA 4%) and 5104 in the ICS group (prescribed ICS 36%, ICS/LABA 62%, ICS/LAMA 3%). Prescriptions for ICS decreased by 81.6% over the decade of the study, whereas non-ICS prescriptions remained constant. A high eosinophil count (≥150 cells·µL−1) occurred in 69.0% of patients. There was no difference in treatment distribution between the ICS and non-ICS groups by eosinophil group (p=0.71).
TABLE 1.
Distribution of patients between inhaled corticosteroid (ICS) and non-ICS groups by baseline characteristics
| Overall | Non-ICS group | ICS group | |
| Patients | 9475 | 4371 | 5104 |
| Age, years | 69.7±10.0 | 70.0±9.7 | 69.4±10.2 |
| Female | 4111 (43.4) | 1809 (41.4) | 2302 (45.1) |
| Current smoker# | 3946 (41.8) | 1836 (42.1) | 2110 (41.6) |
| Airflow limitation severity (most recent FEV1% predicted)¶ | |||
| Mild (≥80%) | 838 (11.9) | 401 (11.3) | 437 (12.5) |
| Moderate (50–80%) | 3878 (55.0) | 2110 (59.4) | 1768 (50.6) |
| Severe (30–50%) | 2010 (28.5) | 914 (25.7) | 1096 (31.4) |
| Very severe (<30%) | 322 (4.6) | 127 (3.6) | 195 (5.6) |
| Asthma >2 years previously | 1098 (11.6) | 269 (6.2) | 829 (16.2) |
| History of atopy+ | 2493 (26.3) | 1107 (25.3) | 1386 (27.2) |
| Exacerbations in previous year | |||
| 0 | 4887 (51.6) | 2433 (55.7) | 2454 (48.1) |
| 1 | 2829 (29.9) | 1250 (28.6) | 1579 (30.9) |
| 2 | 1165 (12.3) | 466 (10.7) | 699 (13.7) |
| ⩾3 | 594 (6.3) | 222 (5.1) | 372 (7.3) |
| Pneumonia episodes in previous year | |||
| 0 | 7484 (79.0) | 3514 (80.4) | 3970 (77.8) |
| 1 | 1500 (15.8) | 660 (15.1) | 840 (16.5) |
| ⩾2 | 491 (5.2) | 197 (4.5) | 294 (5.8) |
| Theophylline in previous 2 years | 97 (1.0) | 17 (0.4) | 80 (1.6) |
| Oxygen use ever | 46 (0.5) | 19 (0.4) | 27 (0.5) |
| Nebulisers in previous 2 years | 157 (1.7) | 48 (1.1) | 109 (2.1) |
| Nonelective hospitalisations§ in previous year | |||
| 0 | 7767 (82.0) | 3663 (83.8) | 4104 (80.4) |
| 1 | 1277 (13.5) | 529 (12.1) | 748 (14.7) |
| ⩾2 | 431 (4.6) | 179 (4.1) | 252 (4.9) |
| GP consultations in previous year | |||
| 0–3 | 2699 (28.5) | 1280 (29.3) | 1419 (27.8) |
| 4–7 | 3381 (35.7) | 1586 (36.3) | 1795 (35.2) |
| ⩾8 | 3395 (35.8) | 1505 (34.4) | 1890 (37.0) |
| Influenza vaccination in previous year | 6710 (70.8) | 3106 (71.1) | 3604 (70.6) |
| Blood eosinophil count (cells·µL−1) | |||
| Geometric mean | 200 | 200 | 201 |
| Median (IQR) | 200 (100–300) | 200 (100–300) | 200 (100–300) |
Data are presented as n, mean±sd or n (%), unless otherwise stated. Percentages are column percentages. FEV1: forced expiratory volume in 1 s; GP: general practitioner; IQR: interquartile range. #: n=9442 for smoking status (only past or current smokers included); ¶: n=7048 for airflow limitation severity; +: atopy defined using presence of codes for allergy, eczema or hay fever; §: for any cause.
Primary analysis
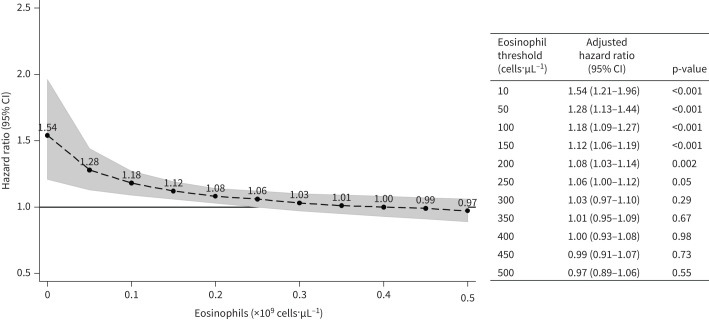
468 patients experienced an exacerbation in the first month after initiating treatment (58.1% in the ICS group) and were excluded from the primary analysis. The remaining 9007 patients provided 38 421 years of follow-up (median 3.8 years per patient, IQR 2.1–6.0 years; range 0.5–11.1 years); 6478 (71.9%) of them experienced an exacerbation during follow-up. The median (95% CI) time to first exacerbation was 645 (95% CI 615–686) days in the non-ICS group and 512 (483–541) days in the ICS group (unadjusted HR ICS versus non-ICS 1.17, 95% CI 1.12–1.23, p<0.001; adjusted HR 1.08, 95% CI 1.03–1.14, p=0.002; figure 1a). Following stratification for baseline eosinophils, the adjusted HR was 1.19 (95% CI 1.09–1.31; p<0.001; figure 1b) in the low-eosinophils group and 1.04 (95% CI 0.98–1.10, p=0.23; figure 1c) in the high-eosinophils group (15% absolute difference; interaction of eosinophil group with treatment group 0.87, 95% CI 0.78–0.97, p=0.01; figure 1).
FIGURE 1.
Kaplan–Meier curves for time to first exacerbation in inhaled corticosteroid (ICS) (red) versus non-ICS (blue) groups, a) overall and b, c) stratified by baseline blood eosinophil group (95% CI shaded). a) Whole group; b) low-eosinophil group (<150 cells·µL−1); c) high-eosinophil group (≥150 cells·µL−1). The interaction between the two eosinophil groups was significant (interaction of eosinophil group with treatment group 0.87, 95% CI 0.78–0.97; p=0.01, 15% absolute difference). Hazard ratios are from Cox regression including the interaction term and adjusted for covariates as follows: age category, sex, smoking status, year of index prescription, socioeconomic status, history of atopy, history of asthma, exacerbations in previous year, pneumonia episodes in previous year, oral steroid prescriptions in previous year, salbutamol inhaler prescriptions in previous year, theophylline in previous 2 years, oxygen use ever, nebulised therapies in previous 2 years, nonelective hospitalisations in previous year, general practitioner consultations in previous year, Charlson comorbidity index [19], influenza vaccination in previous year, pneumococcal vaccination in previous 5 years.
Subgroup and sensitivity analyses of primary analysis
Risk of exacerbations on ICS was lower in those with high eosinophils and history of frequent exacerbations compared to those with low eosinophils and less-frequent exacerbations (HR 0.94, 95% CI 0.82–1.07, p=0.34 versus 1.21, 1.10–1.34, p=0.001; table 2). Multiple sensitivity analyses including using the eosinophil count average of the most recent two, three or all eosinophil counts instead of the most recent value, excluding the highest values (≥500 cells·µL−1), and including eosinophil values close to acute events, made no difference to overall results (supplementary table S2).
TABLE 2.
Subgroup analysis of inhaled corticosteroid (ICS) versus non-ICS treatment, stratified by blood eosinophil group and by baseline exacerbation frequency
|
Low-eosinophil group
(<150 cells·µL−1) |
High-eosinophil group
(≥150 cells·µL−1) |
Interaction HR and p-value | |
| Low exacerbation rate (0 or 1) | 1.21 (1.10–1.34) p=0.001 n=2299 |
1.07 (1.00–1.15) p=0.06 n=5068 |
0.88 (0.78–0.99) p=0.04 |
| Higher exacerbation rate (≥2) | 1.18 (0.97–1.44) p=0.11 n=498 |
0.94 (0.82–1.07) p=0.34 n=1102 |
0.79 (0.62–1.00) p=0.06 |
Data are presented as hazard ratio (HR) (95% CI), unless otherwise stated. HRs are for time to first exacerbation after treatment initiation, for ICS versus non-ICS treatment. HRs are from Cox regression including the interaction term and adjusted for covariates, as listed in figure 1. n=9007.
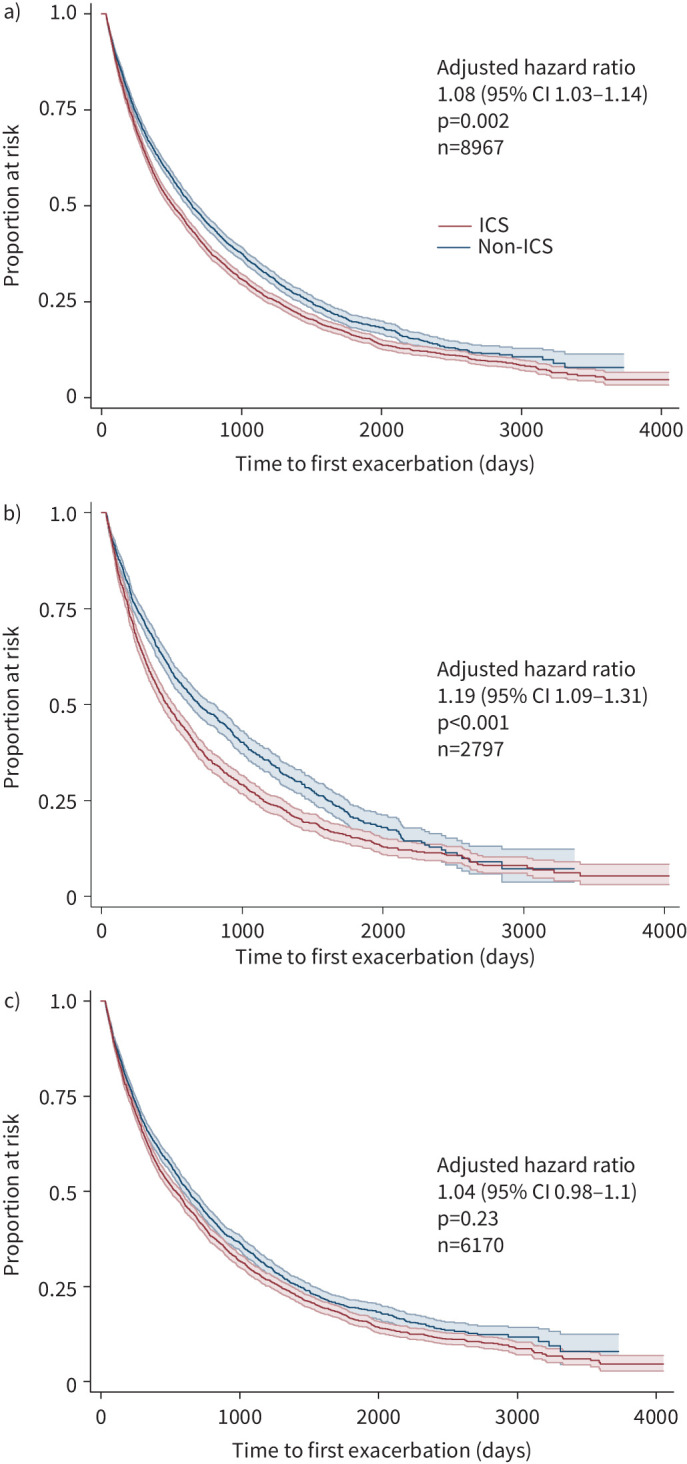
Analysis with different eosinophil thresholds
Using a threshold of 340 cells·µL−1 [20, 21] instead of 150 cells·µL−1, the number of patients in the high-eosinophil group decreased from 69.0% to 19.4% (supplementary table S3). Decreasing HR for ICS treatment as eosinophil count increased was found with increasing eosinophil thresholds, categories, and in continuous analysis (supplementary table S4), and ICS only reduced exacerbations at much higher eosinophil counts (≥450 cells·µL−1) (figure 2).
FIGURE 2.
Hazard ratios for time to first exacerbation for inhaled corticosteroid (ICS) versus non-ICS treatment, at different eosinophil counts. Hazard ratios are from Cox regression including the interaction term and adjusted for covariates as detailed in figure 1, but with eosinophils in the model as a continuous variable (logarithmically transformed). The interaction of eosinophils with ICS treatment group was significant in this model (p=0.004). Deviation of the association from log-linearity was assessed by a likelihood ratio test comparing models with categorical eosinophils (p=0.23). The shaded area shows 95% confidence intervals.
Secondary outcomes
At eosinophil levels <150 cells·µL−1, ICS use was associated with pneumonia, with significant interaction in pneumonia hospitalisations (HR in low-eosinophil group 1.26, 95% CI 1.05–1.50; p-value for interaction p=0.04) (table 3). Time-to-event analyses for different eosinophil thresholds for the pre-specified secondary outcomes are presented in supplementary table S5.
TABLE 3.
Pneumonia outcomes stratified by baseline blood eosinophil group
|
Low-eosinophil group
(<150 cells·µL−1) |
High-eosinophil group
(≥150 cells·µL−1) |
Interaction HR and p-value | |
| Pneumonia episodes | 1.10 (0.99–1.24) p=0.09 n=2832 |
1.05 (0.97–1.13) p=0.24 n=6321 |
0.95 (0.83–1.08) p=0.44 |
| Hospitalisation due to pneumonia | 1.26 (1.05–1.50) p=0.01 n=2910 |
1.00 (0.88–1.14) p>0.99 n=6499 |
0.80 (0.64–0.99) p=0.04 |
| Death due to pneumonia | 1.19 (0.50–2.84) p=0.70 n=2918 |
0.53 (0.27–1.05) p=0.07 n=6517 |
0.44 (0.65–4.42) p=0.14 |
Data are presented as hazard ratio (HR) (95% CI), unless otherwise stated. HRs are for time to first event after treatment initiation, for inhaled corticosteroid (ICS) versus non-ICS treatment. HRs are from Cox regression including interaction term and adjusted for covariates as detailed in figure 1.
Discussion
Summary of main findings
In this real-world study comparing ICS with non-ICS treatment in patients with COPD, there was a statistically significant interaction between ICS treatment and baseline blood eosinophil count. This translated as a 15% lower absolute risk of subsequent exacerbations in patients with higher baseline eosinophil counts who were prescribed an ICS treatment, compared with patients with lower eosinophils who were prescribed ICS. In patients prescribed an ICS there was an eosinophil dose-response with risk of subsequent exacerbation greatest in those with lower eosinophil counts (i.e. <150 cells·µL−1). Results were unchanged when mean of eosinophil counts was used instead of most recent values, or when those taken close to an acute illness were included. In secondary analyses, there was a higher risk of pneumonia hospitalisation in patients receiving ICS treatment with eosinophil counts <150 cells·µL−1.
Contrary to national and international COPD guidelines [22, 23], almost one in five patients were initiated on ICS monotherapy for their COPD, but this has been replicated in other real-life database studies [24, 25]. We found that those prescribed ICS had more “asthma-like” features (e.g. younger, female, previous asthma or oral steroid use), which could suggest that patients with ongoing asthma might be included in the cohort. However, these patients had been coded as COPD and had spirometry diagnostic of COPD, and sensitivity analyses excluding or including all patients with asthma did not change results.
Strengths and weaknesses
We included a large number of patients exposed to routine primary care rather than a highly selected trial population [8]. Other strengths include the new-user cohort study design which avoids immortal time bias that may be present in pharmaco-epidemiological studies [26]; evaluation of steroid-naïve patients, as ICS treatment can affect blood eosinophil values [13]; and use of key variables of interest such as blood results and prescriptions which are generally inputted automatically and so should have virtually complete coverage and accuracy. In this study, missing information is likely to be equally distributed between the eosinophil and treatment groups and should therefore not impact findings.
There is a risk of residual confounding by indication, i.e. there may be unmeasured differences between treatment groups which have not been accounted for. This may partly explain the worse outcome seen with ICS treatment in this study compared to in trials, which have in general found either no or a small benefit of ICS on exacerbation outcomes [2, 27–29], including “real-life” trials in primary care, such as the Salford Lung Study [30]. However, it is the difference in treatment effect size between eosinophil groups, rather than the absolute values, which are important for assessing the role of eosinophils in predicting ICS responsiveness. Importantly, there was no difference in treatment distribution between the ICS and non-ICS groups by eosinophil group.
Our choice of primary eosinophil count threshold of 150 cells·µL−1 is lower than in other studies and is not the threshold for considering initiation in global guidelines [1]. However, this was a pre-specified cut-off based on data available during protocol development. Our observed eosinophil–treatment association was consistent across repeated different thresholds in addition to methodological sensitivity analyses, while a dose–response relationship was seen using continuous analysis of eosinophils.
Our sample size was reduced by almost half due to discontinuation of the new inhaled treatment within 6 months. This may be because of a conscious trialling of medication, a change to an alternative or the patient failing to request prescriptions. However, sensitivity analysis using the full intention-to-treat population, as well as complete on-treatment analysis, made minimal difference to results. Other sensitivity analyses including inclusion of those with an outcome in the first month, and inclusion of covariates with large amounts of missing data, made minimal difference to overall findings.
Comparison with other studies
A systematic review and meta-analysis [5] including 11 post hoc analyses of randomised controlled trials (RCTs), and five retrospective observational studies, found a relative risk of ICS on reducing exacerbation risk of 0.65 (0.52–0.79) with eosinophil counts >150 cells·µL−1 and 0.87 (0.79–0.95) with eosinophil counts <150 cells·µL−1 (four studies used this threshold), and a dose-response of increasing benefit with increasing eosinophil count. However, four out of the five observational studies showed no association. Similar findings have been found in continuous eosinophil analysis of previous trials, except that the benefit of ICS was seen at lower eosinophil counts of 100 cells·µL−1 [31] and 180 cells·µL−1 [32]. Non-ICS treatment appears more favourable in the lowest eosinophil groups [33]. These differences in findings between observational studies and RCTs may be explained by patients who are more unwell being commenced on ICS versus non-ICS treatment, and indeed this was confirmed in the differences between the two groups at baseline, which may relate to other unknown confounders.
Two other studies also used CPRD data to address the same objective. Oshagbemi et al. [34] found a similar HR of exacerbations in patients prescribed ICS versus non-ICS treatment, but that stratification of ICS use by either absolute or relative eosinophil counts did not identify significant differences in risk. However, they excluded all patients with asthma and those who had had any exacerbations in the baseline period. Suissa et al. [35] was a new-user cohort study directly comparing LABA/ICS with LAMA, which found a slightly lower HR for exacerbations than in our study (0.95, 95% CI 0.90–1.01 versus 1.08, 95% CI 1.03–1.14), but a higher HR for pneumonia risk (HR 1.37, 95% CI 1.17–1.60 versus 1.06, 95% CI 1.00–1.13). Despite a number of differences in the methods between our studies, they found a similar association, but with the benefit of ICS seen at lower eosinophil counts.
Our secondary outcomes investigated the relationship of pneumonia events, including severe hospitalised events and pneumonia mortality. We confirm a higher risk of pneumonia in patients with COPD receiving ICS therapy with eosinophils <150 cells·µL−1. This risk was greatest and significant in severe pneumonia events. These findings have been demonstrated before [35, 36], and may relate to an increased bacterial load in ICS-treated patients who have lower (≤2%) blood eosinophils [37].
Application
Our study findings suggest that eosinophil count can be used to predict risk–benefit of ICS treatment: at lower eosinophil levels (especially <150 cells·µL−1) there is a much higher risk of exacerbations and pneumonia hospitalisation with ICS treatment. In this cohort, benefit of ICS treatment was only seen in those with baseline eosinophil counts ≥450 cells·µL−1, and suggests that ICS treatment should particularly be avoided in those with low eosinophil counts. This fits with current Global Initiative for Chronic Obstructive Lung Disease recommendations [38] and National Institute for Health and Care Excellence guidelines [39].
It is not clear whether one or more eosinophil count estimation is required to guide ICS initiation in patients with COPD in clinical practice where often many results are available [40, 41]. Our sensitivity analyses demonstrated that decisions to initiate ICS could be made irrespective of whether the last recorded eosinophil value or an average of multiple results were used.
Conclusions
We recommend considering a more limited approach to ICS prescribing and advise against ICS treatment initiation at low blood eosinophil levels (<150 cells·µL−1), where there is a lower likelihood of treatment benefit and potential harms.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00606-2021.SUPPLEMENT (665.2KB, pdf)
Acknowledgements
Thanks to David McCartney (University of Oxford, Oxford, UK) for assisting with refining code lists; Rebecca Fortescue (St George's, University of London, London, UK) for support; Dan Lasserson (University of Warwick, Warwick, UK), Mike Thomas (University of Southampton, Southampton, UK), David Mant (University of Oxford) and John Stradling (University of Oxford) for input and feedback at the study design stage. We thank the patients who were involved in setting research priorities and input into study design, particularly the Banbury Breathe Easy group.
Footnotes
Provenance: Submitted article, peer reviewed.
Ethical approval: The protocol was reviewed and approval for access to the data was obtained from the Independent Scientific Advisory Committee (ISAC) of the Medicines and Healthcare Products Regulatory Agency (protocol number 16_094), and the approved protocol made available to the journal and reviewers during peer review. Ethical approval for observational research using the Clinical Practice Research Datalink with approval from ISAC has been granted by a National Research Ethics Service committee (Trent MultiResearch Ethics Committee, REC reference number 05/MRE04/87).
Data sharing statement: Requests for data should be directed to the corresponding author; we are happy to share anonymised data within the confines of what is permitted by the CPRD and MHRA.
Author contributions: H.F. Ashdown, I.D. Pavord, C.C. Butler and M. Bafadhel conceived the idea for the study and designed the project, with substantial input from E. McFadden to study design. M. Smith acquired the data and managed it, with some input from H.F. Ashdown. Analysis was mainly performed by H.F. Ashdown with advisory input from M. Smith and E. McFadden. Interpretation of the data was performed by all authors. H.F. Ashdown drafted the manuscript for submission and received critical input from all authors. H.F. Ashdown is guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Conflict of interest: H.F. Ashdown reports support for the present manuscript from National Institute for Health Research; and consulting fees and payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing or educational events received from Boehringer Ingelheim, outside the submitted work. M. Bafadhel reports grants or contracts from AZ; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events received from AZ, GSK, Chiesi, Cipla and Roche; participation on a Data Safety Monitoring Board or Advisory Board for AZ and GSK; and stock or stock options held for Albus Health; all outside the submitted work. I.D. Pavord reports support from Sanofi and Regeneron Pharmaceuticals, Inc., and nonfinancial support from Excerpta Medica, during the conduct of the study; and other support from Aerocrine AB, Almirall, AstraZeneca and Boehringer Ingelheim, grants and other support from Chiesi, other support from GSK, Novartis, Regeneron Pharmaceuticals, Inc., Sanofi, Teva, Circassia, Dey Pharma, Genentech, Knopp Biosciences, Merck, MSD, Napp Pharmaceuticals, RespiVert and Schering-Plough, outside the submitted work. The remaining authors have nothing to disclose.
Support statement: This work was funded by a personal fellowship from the National Institute for Health Research (NIHR) awarded to H.F. Ashdown (DRF 2014-07-052). M. Smith and I.D. Pavord are supported by the NIHR Oxford Biomedical Research Centre. The funder had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The funder will approve the manuscript before publication. The researchers are independent from funders; and all authors had full access to all of the data in the study, and can take responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed are those of the authors and not necessarily those of the National Health Service (NHS), the NIHR or the Department of Health and Social Care. This work used data provided by patients and collected by the NHS as part of their care and support, and would not have been possible without access to these data. The NIHR recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care. This study is based in part on data from the Clinical Practice Research Datalink obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. The interpretation and conclusions contained in this study are those of the authors alone. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J 2019; 53: 1900164. doi: 10.1183/13993003.00164-2019 [DOI] [PubMed] [Google Scholar]
- 2.Kew KM, Dias S, Cates CJ. Long-acting inhaled therapy (beta-agonists, anticholinergics and steroids) for COPD: a network meta-analysis. Cochrane Database Syst Rev 2014; 3: CD010844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White P, Thornton H, Pinnock H, et al. Overtreatment of COPD with inhaled corticosteroids – implications for safety and costs: cross-sectional observational study. PLoS One 2013; 8: e75221. doi: 10.1371/journal.pone.0075221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wurst KE, Punekar YS, Shukla A. Treatment evolution after COPD diagnosis in the UK primary care setting. PLoS One 2014; 9: e105296. doi: 10.1371/journal.pone.0105296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harries TH, Rowland V, Corrigan CJ, et al. Blood eosinophil count, a marker of inhaled corticosteroid effectiveness in preventing COPD exacerbations in post-hoc RCT and observational studies: systematic review and meta-analysis. Respir Res 2020; 21: 3. doi: 10.1186/s12931-019-1268-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med 2018; 378: 1671–1680. doi: 10.1056/NEJMoa1713901 [DOI] [PubMed] [Google Scholar]
- 7.Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med 2020; 383: 35–48. doi: 10.1056/NEJMoa1916046 [DOI] [PubMed] [Google Scholar]
- 8.Kruis AL, Ställberg B, Jones RC, et al. Primary care COPD patients compared with large pharmaceutically-sponsored COPD studies: an UNLOCK validation study. PLoS One 2014; 9: e90145. doi: 10.1371/journal.pone.0090145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herland K, Akselsen JP, Skjønsberg OH, et al. How representative are clinical study patients with asthma or COPD for a larger ‘real life’ population of patients with obstructive lung disease? Respir Med 2005; 99: 11–19. doi: 10.1016/j.rmed.2004.03.026 [DOI] [PubMed] [Google Scholar]
- 10.Herrett E, Thomas SL, Schoonen WM, et al. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 2010; 69: 4–14. doi: 10.1111/j.1365-2125.2009.03537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshida K, Solomon DH, Kim SC. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol 2015; 11: 437–441. doi: 10.1038/nrrheum.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith CJ, Gribbin J, Challen KB, et al. The impact of the 2004 NICE guideline and 2003 General Medical Services contract on COPD in primary care in the UK. QJM 2008; 101: 145–153. doi: 10.1093/qjmed/hcm155 [DOI] [PubMed] [Google Scholar]
- 13.Kreindler JL, Watkins ML, Lettis S, et al. Effect of inhaled corticosteroids on blood eosinophil count in steroid-naive patients with COPD. BMJ Open Respir Res 2016; 3: e000151. doi: 10.1136/bmjresp-2016-000151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DiSantostefano RL, Sampson T, Le HV, et al. Risk of pneumonia with inhaled corticosteroid versus long-acting bronchodilator regimens in chronic obstructive pulmonary disease: a new-user cohort study. PLoS One 2014; 9: e97149. doi: 10.1371/journal.pone.0097149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis 2015; 10: 2207–2217. doi: 10.2147/COPD.S91694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beasley R, Harper J, Bird G, et al. Inhaled corticosteroid therapy in adult asthma. Time for a new therapeutic dose terminology. Am J Respir Crit Care Med 2019; 199: 1471–1477. doi: 10.1164/rccm.201810-1868CI [DOI] [PubMed] [Google Scholar]
- 17.Pascoe S, Locantore N, Dransfield MT, et al. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med 2015; 3: 435–442. doi: 10.1016/S2213-2600(15)00106-X [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Morgan RL, Alonso-Coello P, et al. A systematic review of how patients value COPD outcomes. Eur Respir J 2018; 52: 1800222. doi: 10.1183/13993003.00222-2018 [DOI] [PubMed] [Google Scholar]
- 19.Khan NF, Perera R, Harper S, et al. Adaptation and validation of the Charlson Index for Read/OXMIS coded databases. BMC Fam Pract 2010; 11: 197. 10.1186/1471-2296-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oshagbemi OA, Burden AM, Braeken DCW, et al. Stability of blood eosinophils in patients with chronic obstructive pulmonary disease and in control subjects, and the impact of sex, age, smoking, and baseline counts. Am J Respir Crit Care Med 2017; 195: 1402–1404. doi: 10.1164/rccm.201701-0009LE [DOI] [PubMed] [Google Scholar]
- 21.Vedel-Krogh S, Nielsen SF, Lange P, et al. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am J Respir Crit Care Med 2016; 193: 965–974. doi: 10.1164/rccm.201509-1869OC [DOI] [PubMed] [Google Scholar]
- 22.National Institute for Health and Clinical Excellence Guidance (NICE) . Chronic Obstructive Pulmonary Disease. Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care [CG12]. 2004. Available from: www.nice.org.uk/Guidance/CG12/
- 23.Global Initiative for Chronic Obstructive Lung Disease (GOLD) . Global strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (Updated 2013). 2013. Available from: https://goldcopd.org/
- 24.Price D, Miravitlles M, Pavord I, et al. First maintenance therapy for COPD in the UK between 2009 and 2012: a retrospective database analysis. NPJ Prim Care Respir Med 2016; 26: 16061. doi: 10.1038/npjpcrm.2016.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chalmers JD, Tebboth A, Gayle A, et al. Determinants of initial inhaled corticosteroid use in patients with GOLD A/B COPD: a retrospective study of UK general practice. NPJ Prim Care Respir Med 2017; 27: 43. doi: 10.1038/s41533-017-0040-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol 2008; 167: 492–499. doi: 10.1093/aje/kwm324 [DOI] [PubMed] [Google Scholar]
- 27.Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta2-agonist in one inhaler versus long-acting beta2-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 9: CD006829. doi: 10.1002/14651858.CD006829.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang IA, Clarke MS, Sim EH, et al. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 7: CD002991. doi: 10.1002/14651858.CD002991.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nannini LJ, Cates CJ, Lasserson TJ, et al. Combined corticosteroid and long-acting beta-agonist in one inhaler versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013; 11: CD003794. doi: 10.1002/14651858.CD003794.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vestbo J, Leather D, Diar Bakerly N, et al. Effectiveness of fluticasone furoate-vilanterol for COPD in clinical practice. N Engl J Med 2016; 375: 1253–1260. doi: 10.1056/NEJMoa1608033 [DOI] [PubMed] [Google Scholar]
- 31.Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med 2018; 6: 117–126. doi: 10.1016/S2213-2600(18)30006-7 [DOI] [PubMed] [Google Scholar]
- 32.Siddiqui SH, Guasconi A, Vestbo J, et al. Blood eosinophils: a biomarker of response to extrafine beclomethasone/formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015; 192: 523–525. doi: 10.1164/rccm.201502-0235LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roche N, Chapman KR, Vogelmeier CF, et al. Blood eosinophils and response to maintenance chronic obstructive pulmonary disease treatment. Data from the FLAME Trial. Am J Respir Crit Care Med 2017; 195: 1189–1197. doi: 10.1164/rccm.201701-0193OC [DOI] [PubMed] [Google Scholar]
- 34.Oshagbemi OA, Franssen FME, Braeken DCW, et al. Blood eosinophilia, use of inhaled corticosteroids, and risk of COPD exacerbations and mortality. Pharmacoepidemiol Drug Saf 2018; 27: 1191–1199. doi: 10.1002/pds.4655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suissa S, Dell'Aniello S, Ernst P. Comparative effectiveness of LABA-ICS versus LAMA as initial treatment in COPD targeted by blood eosinophils: a population-based cohort study. Lancet Respir Med 2018; 6: 855–862. doi: 10.1016/S2213-2600(18)30368-0 [DOI] [PubMed] [Google Scholar]
- 36.Pavord ID, Lettis S, Anzueto A, et al. Blood eosinophil count and pneumonia risk in patients with chronic obstructive pulmonary disease: a patient-level meta-analysis. Lancet Respir Med 2016; 4: 731–741. doi: 10.1016/S2213-2600(16)30148-5 [DOI] [PubMed] [Google Scholar]
- 37.Contoli M, Pauletti A, Rossi MR, et al. Long-term effects of inhaled corticosteroids on sputum bacterial and viral loads in COPD. Eur Respir J 2017; 50: 1700451. doi: 10.1183/13993003.00451-2017 [DOI] [PubMed] [Google Scholar]
- 38.Global Initiative for Chronic Obstructive Lung Disease (GOLD) . Global strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2019 report). 2019. Available from: https://goldcopd.org/
- 39.National Institute for Health and Clinical Excellence Guidance (NICE) . Chronic Obstructive Pulmonary Disease in Over-16s: Diagnosis and Management [NG115]. 2018. Available from: www.nice.org.uk/guidance/NG115/
- 40.Brusselle G, Pavord ID, Landis S, et al. Blood eosinophil levels as a biomarker in COPD. Respir Med 2018; 138: 21–31. doi: 10.1016/j.rmed.2018.03.016 [DOI] [PubMed] [Google Scholar]
- 41.Celli BR, Criner GJ. Using the peripheral blood eosinophil count to manage patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc 2019; 16: 301–303. doi: 10.1513/AnnalsATS.201810-729PS [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00606-2021.SUPPLEMENT (665.2KB, pdf)