Abstract
Introduction
Optic capture of sutured scleral fixated posterior chamber intraocular lenses (PC IOLs) is an occasional complication resulting in blurred vision and discomfort.
Methods
A retrospective study of the management of 18 eyes (3.6%) with optic capture out of 495 eyes with scleral fixated IOLs during the study period. 54 procedures were performed in the management of optic capture of sutured scleral fixated PC IOLs. An in-office technique was utilized to relieve the optic capture by repositioning the optic posterior to the iris. This technique was performed after topical anesthesia and topical 5% betadine with the patient stably positioned at the slit lamp. Using a 30-gauge needle, sometimes after a 15-degree paracentesis blade, the needle was advanced in a parallel plane above the iris until the tip reached the edge of the captured optic. The optic is engaged in the inferior periphery away from the central visual axis, and pushed gently posteriorly just enough to reposition the optic posterior to the iris. In some cases, pilocarpine 2% drops were utilized after the procedure to decrease the risk of recapture of the optic.
Results
All 54 procedures were successfully performed in the office without significant pain or discomfort. Vision before optic capture, during optic capture, and at the first office visit after optic capture were comparable. There were not any cases of endophthalmitis, hyphema, iris trauma, iris prolapse or keratitis. While eight patients only had one episode of optic capture, 10 patients had multiple episodes of optic capture, all managed with this in office procedure. Recurrent optic capture occurred more frequently in eyes with fixation at less than 2 mm from the limbus than eyes with scleral fixation at 2 mm from the limbus.
Conclusion
Reposition of the optic after pupillary capture of a scleral fixated PC IOL can be successfully performed in the office without discomfort or significant complications and is an alternative management option to a return to the operating room. This procedure may be especially important when there is poor access to the operating room or restricted access to the operating room as during the COVID19 pandemic.
Keywords: Scleral fixation, PC IOL, Dislocated PC IOL, Optic capture, Pupillary capture, Pars plana vitrectomy, PC IOL reposition, Paracentesis, In office procedure
1. Introduction
Scleral fixation of posterior chamber intraocular lenses (PC IOL) is a commonly used technique for stabilizing or repositioning PC IOLs when there is inadequate capsular support.1, 2, 3, 4, 5While this scleral fixation technique is very successful at fixating the haptics to allow good positioning of the optic, optic capture by the pupil can occur postoperatively and often long after the initial surgery.6, 7, 8, 9 Optic capture can occur after sutured scleral fixation9 or transscleral fixation of the PC IOL.6 Optic capture leads to blurred vision and an eccentric pupil. More severe complications include pain, increased intraocular pressure, uveitis, pupillary block glaucoma, iris chafing, pigment dispersion glaucoma, cystoid macular edema, hyphema or vitreous hemorrhage.
Most cases of optic capture have been managed by a return to the operating room to reposition the optic posterior to the iris. An office procedure was developed to avoid a return to the operating room minimizing both costs and risks of another surgical procedure. This office procedure involves repositioning the optic back into the posterior chamber with a 30-gauge needle at the slit lamp. This procedure is not any more invasive than a paracentesis to relieve elevated intraocular pressure for acute elevations of intraocular pressure, or an intravitreal injection for the treatment of exudative macular degeneration, diabetic retinopathy, or retinal vein occlusions. Both procedures are standard of care and performed in the office.
Herein we present the results of this in office procedure to resolve optic capture in a retrospective study.
2. Methods
A retrospective, interventional cases series was performed at the Hawaii Macula and Retina Institute and Retina Consultants of Hawaii from January 2007 through October 2020 on patients who underwent an in-office paracentesis for resolution of pupillary optic capture. All patients had a past ocular history of a sutured scleral fixated PC IOL. Pupillary optic capture was defined as malposition of any portion of the PC IOL optic anterior to the iris plane. The Western Institutional Review Board (WIRB, Olympia, Washington) exempted this study from IRB approval (1-921364-1). It complied with the Health Insurance Portability and Accountability Act of 1996 and followed the tenets of the Declaration of Helsinki.
2.1. Surgical technique
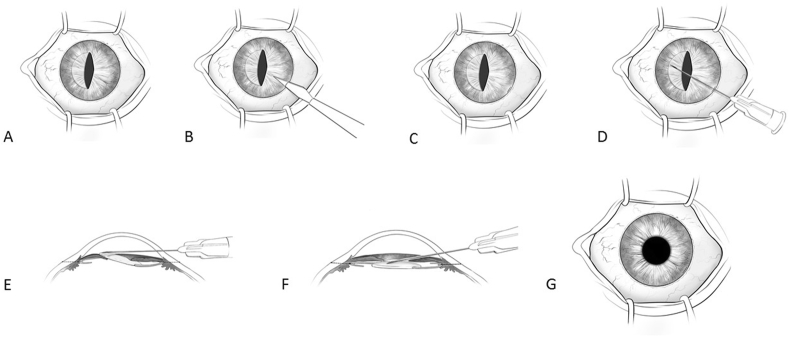
This in-office paracentesis technique was performed after topical anesthesia (0.5% proparacaine) followed by 1–2 drops of 5% povidone-iodine antiseptic solution. A lid speculum was placed, or the upper eyelid was elevated by the assistant. The patient was positioned comfortably at the slit lamp, making sure that their forehead was stably situated against the forehead strap of the slit lamp. A temporal peripheral clear corneal incision was made either using a standard 15° angled paracentesis knife or directly with a 30-gauge needle. The 30-gauge ½ inch needle was mounted on a tuberculin syringe for comfortable handling of the needle. The 30-gauge needle was then advanced in the anterior chamber parallel to the iris plane until engaging the optic in the inferior peripheral part of the optic outside of the visual axis (see Fig. 1).1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 Posterior pressure on the optic was then utilized to push the optic back behind the iris and posterior to the pupil. After the procedure, careful assessment is done to make sure all areas of iris capture have been released and that there is no evidence of anterior chamber shallowing, iris prolapse or wound leakage. Topical broad-spectrum antibiotics are utilized post procedure. In any case of recurrent optic capture pilocarpine 2% drops are utilized at periods when the patient's environment is dark, so often at dinner, before sleep, and waking up if it is dark in the morning.
Fig. 1.
A. Pupillary capture of the optic of this left eye is captured over the nasal iris. B. Paracentesis incision with a 15-degree blade through the temporal clear cornea. C. Paracentesis incision in inferotemporal clear cornea. D. 30-gauge needle placed through paracentesis over the iris and to the peripheral part of the optic away from the visual axis E. 30-gauge needle engaging peripheral optic above the iris plane. F. After posterior pressure the optic is repositioned posterior to the iris. G. After optic reposition PC IOL is in good position and pupil is round.
All consecutive patients undergoing this procedure at Retina Consultants of Hawaii were identified using an office database search of International Classification of Diseases 9 code 996.53 (mechanical complication of ocular lens prosthesis) or International Classification of Diseases 10 code T8529XA (other mechanical complication of intraocular lens, initial encounter), and a procedural database search of 65800 (paracentesis). The following patient data were recorded: age, gender, laterality, PC IOL composition and design, clinical indication for PC IOL fixation, distance of fixation from the limbus (millimeters), location of fixation sclerotomies based on location using a clock hours localization, time interval (months) between scleral fixation surgery and optic capture, time interval (months) between episodes of recurrent optic captures, location of pupil capture of the optic. visual acuity with a Snellen vision chart, intraocular pressure by Tono-Pen (Reichert Inc., Buffalo, New York, USA), and associated symptoms during the office visits. Visual acuities (VA) were converted to logarithm of minimum angle of resolution (logMAR) equivalents for data analysis. We used a value of 2.0 and 3.0 logMAR to represent vision of counting fingers and hand movement, respectively.
The data and analysis were tabulated using Microsoft® Excel® (Redmond, Washington). For numerical data, mean and standard deviation were generated. A paired Student's t-test analysis was used to compare average time and rate of optic capture recurrence when comparing placement of IOL fixation with respect to the limbus. A p-value <0.05 was considered statistically significant.
3. Results
In this study, 18 eyes of 18 patients were identified to have an in-office paracentesis for management of optic capture after scleral fixation of a PC IOL. This study included 14 males and 4 females with an average age of 56 years (range 11–81). Scleral fixation was performed for 8 IOL reposition procedures, 6 secondary IOL procedures, and 4 IOL exchanges. Indications for scleral fixation of the PC IOL was dislocation of PC IOL in 13 eyes, dislocated cataract in 4 eyes, and subluxed crystalline lens in 1 eye. Preexisting ocular conditions included glaucoma in 5 eyes, epiretinal membrane in 4 eyes, and successfully repaired retinal detachment with scleral buckling in 2 eyes, retinal tear successfully repaired with laser in 1 eye, macular hole successfully repaired with pars plana vitrectomy in 1 eye, ocular hypertension in 1 eye, and blunt ocular trauma in 1 eye. All eyes previously underwent a pars plana vitrectomy and scleral fixation of a single piece CZ70BD PMMA PCIOL (Alcon Laboratories, Fort Worth, Texas, USA) using a technique previously published with passing of a long-curved needle through the limbal wound and into a guiding 23-gauge needle placed through the fixation sclerotomy (Alcon Laboratories, Fort Worth, Texas, USA).1,2 Fixation was positioned at 2:00 and 8:00 in 13 eyes, 3:00 and 9:00 in 2 eyes, and 4:00 and 10:00 in 3 eyes. The scleral fixation position posterior to the limbus varied over time with accepted practice guidelines. The position of scleral fixation posterior to the limbus was 1.25 mm in one case and 1.33 mm in one case in 2009, 1.5 mm in one case in 2010, 1.75 mm in 2 cases in 2011, and 2.0 mm in the remaining 13 cases between 2011 and 2019. Cases performed with scleral fixation distances less than 2 mm were in 5 of 18 eyes (28%) and all performed in 2011 or earlier, while cases performed with scleral fixation sutures 2 mm back were in 13 of 18 eyes (72%) and all performed in 2011 or later.
Overall, 18 eyes (3.6%) of 495 scleral fixated PC IOLs during the study period developed optic capture. Patients were asymptomatic in 17 episodes of optic capture, while blurring of vision was noted in 28 episodes, pain and discomfort in 7 episodes, redness in one episode, and scotoma in one episode. The average time interval between the scleral fixated PC IOL surgery and the initial episode of pupillary optic capture was 20 months (range 1 day–108 months). Pupillary capture involved the horizontal meridian more frequently than the vertical meridian of the optic with 52 optic captures in the horizontal meridian and 14 optic captures in the vertical meridian. No relationship was noted regarding optic capture and the location of fixation sclerotomies around the limbus or the distance of scleral fixation from the limbus. None of the pupillary capture episodes were associated with a retraction or concave appearance of the iris consistent with reverse pupillary block. The optic capture was always in the normal position of the iris, but just with the optic captured by the pupil.
All procedures were performed by surgeons at the Hawaii Macula and Retina Institute. All procedures were successful at repositioning the optic posterior to the iris with the in-office procedure. There was not any significant pain or discomfort in any case. Overall, a total of 54 in-office paracentesis procedures for relief of optic capture were performed on 18 eyes (mean 3.00, range 1–10). Recurrent optic capture did occur in ten of the eighteen patients and the average rate of recurrent optic capture for this procedure in these patients was 3.60 ± 2.84 (range 1–9). Mean time interval between optic capture recurrences in the ten patients who required additional treatment after initial corrective paracentesis was 8.0 ± 7.19 months (range 1–33). The average number of IOL reposition procedures via paracentesis was one optic repositioning per year for all cases. For patients with follow-up of 12 months or longer the optic repositioning procedures per year were 0.69 paracenteses per year. This equates to one therapeutic paracentesis every 12 months for all patients and every 17.4 months for patients with follow-up periods of at least 12 months. Thirteen of the eighteen patients with long term follow-up after the last paracentesis procedure did not have repeat optic capture for an average of 3 years (36.08 months; range 2–108 months.) There was a trend towards a lower rate of optic capture recurrence with fixation at 2mm posterior to the limbus compared to those fixated at less than 2mm, but this did not reach statistical significance (p = 0.34). However, the frequency of optic capture recurrence was statistically significantly less with a more posterior scleral fixation at 2mm (9.64; standard deviation = 7.22 mos) than in eyes with a more anterior scleral fixation less than 2 mm (4.26; standard deviation = 6.06 mos)(p = 0.025).
Average BCVA at visits preceding occurrence of optic capture was 20/78 (range 20/20 to HM, 0.59 ± 0.86 logMAR). Average BCVA during the time of optic capture for all cases was 20/69 (range 20/20 to HM, 0.54 ± 0.79 logMAR). Average BCVA was 20/68 (range 20/20 to HM, 0.53 ± 0.85 logMAR) at the subsequent office visit after resolution of optic capture. One eye had an initial visual acuity of hand motion vision which persisted due to pre-existing glaucoma. When we excluded the participant who was HM due to underlying glaucoma, the average BCVA at the visit preceding the event of optic capture was 20/43 (range 20/20 to 20/200, 0.33 ± 0.36 logMAR). The average BCVA during the time of optic capture when excluding the HM patient was about 20/40 (range 20/20 to 20/200, 0.30 ± 0.28 logMAR). The average BCVA at the subsequent office visit after resolution of optic capture when excluding the HM patient was about 20/36 (range 20/20 to 20/200, 0.25 ± 0.26 logMAR) at the subsequent office visit after resolution of optic capture. At the final follow up, mean BCVA for the 18 eyes was 20/46 (0.36 ± 0.71 logMAR), and 20/31 (0.19 logMAR ± 0.20) when omitting the glaucoma patient who was HM. Mean IOP was 16.4 mmHg (range 8–50 mmHg) at the visit preceding presentation of pupillary optic capture. Mean IOP was 17.4 mmHg (range 9–44 mmHg) at presentation of pupillary optic capture and 15.0 mmHg (range 8–30 mmHg) at the subsequent follow-up visit. At the final follow-up period, mean IOP was 16.1 mmHg (range 10–32 mmHg). None of the eyes had endophthalmitis or complications related to the repositioning of the optic posterior to the iris and relieving the optic during the follow-up, which ranged from 2 months to 135 months. All procedures were successfully performed without pain or discomfort under topical anesthesia, and the optic was in good position at final follow-up in all eyes. There were not any cases of IOL subluxation, IOL dislocation or suture breakage utilizing this technique.
4. Discussion
Pupillary optic capture is a well-recognized complication following cataract surgery with IOL implantation,6, 7, 8, 9 and with scleral fixated PC IOL after pars plana vitrectomy (PPV). Johnston10 and Bading et al.11 have found optic capture rates with scleral fixation of PC IOL combined with pars plana vitrectomy to be 14.3% and 7.9% respectively within two weeks after the surgery. In these cases, surgical revision was performed in all cases requiring a return to the operating room. With a mean follow up of 43 months, Cho et al.12 reported the incidence of optic capture to be 23%. In our series there was an optic capture rate of 3.6%, which is lower than previous series.
No definite etiology has been found for optic capture, but it has been proposed that the absence of the vitreous body contributes to IOL instability and its subsequent capture.13 We also speculate that increased mobility of the iris (iridodenesis or a flaccid iris) anteriorly and posteriorly due to loss of support after removal of the crystalline lens or the lens capsule surrounding the PCIOL may contribute to increased movement of the iris forward allowing pupillary capture of the optic. Although reverse pupillary block or iris retraction is another possible hypothesis,13 none of the cases of optic capture had iris retraction or a concave iris. In cases of reverse pupillary block the intact complex of the iris and the optic behind the iris form an continuous platform resulting in blockage of aqueous flow, which causes a reduced distance between the posterior surface of the iris and the optic. These cases can be successfully treated with peripheral iridotomy. However, none of the cases in this series showed iris retraction or a concave appearance of the iris, and optic capture cases occurred in the usual position of the iris.
Different surgical and non-surgical modalities for IOL capture management and prevention have been described in the literature. While pupillary capture can resolve spontaneously or after pupillary dilation in the supine position,12 other nonsurgical maneuvers include external digital percussion of the eyeball through a closed eyelid14 and external compression using cotton-tipped swabs.15 Many of these techniques were tried on the patients in the study but were unsuccessful at relieving the optic capture. Persistent optic capture usually requires surgical intervention and are often successful at release of the optic capture, but there are increased costs, anesthetic risks, and surgical risks with a return to the operating room. This is especially true when there are multiple recurrences of optic capture, as was noted in 10 eyes in this series. This in office procedure may be especially important in clinical situation where there is limited access to the operating room or restricted access to the operating room as what occurred during the COVID19 pandemic.
To our knowledge, this study is the first to describe an in-office procedure that manages pupillary IOL capture for eyes who previously had scleral-fixated PC IOL. A paracentesis was performed and the optic that was captured by the pupil was gently repositioned with posterior pressure on the optic to reposition the optic posterior to the iris and relieve the optic capture. This was not forcefully or abruptly performed, and was not intended to push back on the optic to change the position of the haptics or fixation sutures within the eye. Care should be taken to make sure the patient maintained a stable position with the forehead up against the slit lamp. This in-office procedure offers a potential alternative to surgical intervention in the operating room. With multiple repeat episodes of optic capture, pilocarpine 2% was recommended during hours of relative darkness at home, so usually at dinner time, before going to sleep and in the morning. In one case mydriasis with atropine 1% was well tolerated to prevent recurrence of optic capture. Recapture of the optic often occurred when there was noncompliance with the pilocarpine drops.
This 30-gauge needle repositioning in office technique was safely performed at the slit lamp in all cases without discomfort for the patient just under topical anesthesia. Topical 5% betadine was used prior to the procedure, and topical antibiotics were utilized after the procedure. There were no cases of endophthalmitis in this series of 54 repositioning procedures. However, endophthalmitis is a risk after paracentesis16 and infectious keratitis has also been reported after paracentesis.17 Other in office procedures commonly utilized as standard of care include a paracentesis for reduction of elevated intraocular pressure, a pneumatic retinopexy with injection of gas for retinal detachment repair, or an intravitreal injection for exudative age related macular degeneration or edema from retinal vascular disease. Intravitreal injections may need to be given up to 12 times per year. In patients with long term follow-up of eyes with optic capture the frequency of paracentesis reposition of the optic was less than once per year. This in office procedure to treat optic capture is not any more invasive than other commonly used procedures in the office.
Pilocarpine eyedrops to create miosis may be utilized to prevent optic capture. Dosing can vary, but initially dosing was organized to create the maximum effect during the dark hours, so a common regimen would be at dinner, bedtime and in the early morning. Pilocarpine for pupil constriction has the potential for causing anterior chamber inflammation and headaches,18 but this was not noted in any of the patients in this series. This strategy was often successful at preventing recurrent optic capture. Another approach is to prescribe atropine eyedrops to maintain dilation and prevent capture of the IOL, and some patients can do well with this option without significant side effects from dilation. However, some reports have shown that a miotic pupil appears to cause less IOL capture compared with a large pupil.19 Prior to utilizing this technique, we usually dilated the patient, put the patient in a supine position, and did gentle ocular massage to push posteriorly on the optic. If the optic capture was relieved, miotic drops were placed to bring the pupil down. However, this was not reliably successful at alleviating the optic capture, and the cases which did not resolve were treated with the paracentesis procedure.
In this series, there was minimal change in overall visual acuity after paracentesis and release of optic capture. This indicates that effective IOL reposition with optic capture still allows good vision, even after multiple episodes of optic capture by the pupil. The success of this procedure allows management of optic capture in a very quick and painless in-office procedure without the need for a return to the operating room, which is especially important with multiple cases of recurrent optic capture. This was accomplished in these cases without any cases of endophthalmitis, keratitis, PC IOL subluxation, PC IOL dislocation or suture breakage.
Since this series of patients included cases done over many years, the distance from the limbus varied with clinical experience and publications in the literature. Early on in the study of position for scleral fixation, Lindstrom and colleagues in a cadaver study reported that transscleral sutures should exit the sclera less than 1 mm posterior to the limbus for ciliary sulcus fixation.20 With more clinical experience, studies have shown that a farther fixation point from the limbus can decrease the rate of IOL capture, as consistent with present practice.21 In this study all cases of fixation less than 2 mm were performed in 2011 and earlier, while all cases of fixation 2 mm posterior to the limbus were performed in 2011 and later. There was not any difference in risk of IOL capture between eyes with fixation less than 2 mm, and fixation at 2 mm, but the numbers in this study are relatively small. However, the frequency of optic capture was statistically significantly more in eyes with fixation less than 2 mm than eyes with 2mm fixation from the limbus, which again supports the use of fixation suture no less than 2 mm from the limbus. There were not any other preoperative risk factors for IOL capture in this study. Although surgical intervention can be performed to reposition or exchange a scleral fixated PC IOL more posteriorly, this procedure is complex and requires significant surgical manipulation, and potential complications include macular edema, vitreous incarceration, IOL redislocation, corneal edema due to anterior segment surgical trauma, postoperative astigmatism due to the need for a large limbal wound for IOL exchange, vitreous hemorrhage and retinal detachment.22 This in office relief of optic capture procedure in patients with mostly excellent visual acuity prevents the risk of much more serious complications from a complex surgery to move a scleral fixated PC IOL more posteriorly.
This study is limited by the retrospective design and small number of patients, but does provide good data in regards to multiple episodes of optic capture. To our knowledge this is the first report of this new and useful in-office technique to manage pupillary capture of the optic of the PCIOL. Paracentesis is usually performed in office to relieve intraocular pressure, but this procedure involves this same procedure to relieve optic capture. This procedure can be performed with a topical anesthetic at the slit lamp in the office without pain or discomfort and with good success. Even if multiple procedures were necessary this was infrequent, and much less often that intravitreal injections that are performed in office. This paracentesis procedure to manage optic capture is especially useful when there is poor access to an operating room, or limited access as what recently occurred with the COVID19 pandemic.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patients.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
No conflicting relationship exists for any author.
Acknowledgments
The authors acknowledge the editorial assistance of Maria Won, research coordinator at Hawaii Macula and Retina Institute.
References
- 1.Kokame GT, Yanagihara R, Shantha JG, Kaneko KN. Long-term outcome of pars plana vitrectomy and sutured scleral-fixated posterior chamber intraocular lens implantation. Am J Ophthalmol 189:10-16. [DOI] [PMC free article] [PubMed]
- 2.Kokame G.T., Yamamoto I., Mandel H. Scleral fixation of dislocated posterior chamber intraocular lenses: temporary haptic externalization through a clear corneal incision. J Cataract Refract Surg. 2004;30:1049–1056. doi: 10.1016/j.jcrs.2003.09.065. [DOI] [PubMed] [Google Scholar]
- 3.Abbey A.M., Hussain R.M., Shah A.R., Faia L.J., Wolfe J.D., Williams G.A. Sutureless scleral fixation of intraocular lenses: outcomes of two approaches. The 2014 Yasuo Tano Memorial Lecture. Graefes Arch Clin Exp Ophthalmol. 2015 Jan;253(1):1–5. doi: 10.1007/s00417-014-2834-9. [DOI] [PubMed] [Google Scholar]
- 4.Ma D.J., Choi H.J., Kim M.K., Wee W.R. Clinical comparison of ciliary sulcus and pars plana locations for posterior chamber intraocular lens transscleral fixation. J Cataract Refract Surg. 2011;37:1439–1446. doi: 10.1016/j.jcrs.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 5.McAllister A.S., Hirst L.W. Visual outcomes and complications of scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2011;37:1263–1269. doi: 10.1016/j.jcrs.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Fram N. Consultation Section: cataract. Optic capture after intrascleral fixation. J Cataract Refract Surg. 2020;46:320–324. doi: 10.1097/j.jcrs.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 7.Dong J.K., Kim H.K. Clinical analysis of the factors contributing to pupillary optic capture after transscleral fixation of posterior chamber intraocular lens for dislocated intraocular lens for dislocated intraocular lens. J Cataract Refract Surg. 2016;42:1146–1150. doi: 10.1016/j.jcrs.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Khokhar S., Sethi H.S., Sony P., et al. Pseudophakic pupillary block caused by pupillary capture after phacoemulsification and in-the-bag AcrySof lens implantation. J Cataract Refract Surg. 2002;28:1291Y1292. doi: 10.1016/s0886-3350(02)01305-6. [DOI] [PubMed] [Google Scholar]
- 9.Rahman R., Rosen P.H. Pupillary capture after combined management of cataract and vitreoretinal pathology. J Cataract Refract Surg. 2002;28:1607Y1612. doi: 10.1016/s0886-3350(02)01212-9. [DOI] [PubMed] [Google Scholar]
- 10.Johnston R.L., Charteris D.G., Horgan S.E., Cooling R.J. Combined pars plana vitrectomy and sutured posterior chamber implant. Arch Ophthalmol. 2000;118:905–910. [PubMed] [Google Scholar]
- 11.Bading G., Hillenkamp J., Sachs H.G., et al. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144:371–377. doi: 10.1016/j.ajo.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Cho B.J., Yu H.G. Surgical outcomes according to vitreous management after scleral fixation of posterior chamber intraocular lenses. Retina. 2014;34(10):1977–1984. doi: 10.1097/IAE.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 13.Bang S.P., Choun-ki j, Jun J.H. Reverse pupillary block after implantation of a scleral-sutured posterior chamber intraocular lens: a retrospective, open study. BMC Ophthalmol. 2017;17(1):35. doi: 10.1186/s12886-017-0427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bowman C.B., Hansen S.O., Olson R.J. Noninvasive repositioning of a posterior chamber intraocular lens following pupillary capture. J Cataract Refract Surg. 1991;17:843–847. doi: 10.1016/s0886-3350(13)80421-x. [DOI] [PubMed] [Google Scholar]
- 15.Lindstrom R.L., Herman W.K. Pupil capture: prevention and management. J Am Intraocu Implant Soc. 1983;9:201–204. doi: 10.1016/s0146-2776(83)80049-4. [DOI] [PubMed] [Google Scholar]
- 16.Helbig H., Noske W., Kleineidam M., et al. Bacterial endophthalmitis after anterior chamber paracentesis. Br J Ophthalmol. 1995;79:866. doi: 10.1136/bjo.79.9.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azuara-Blanco A., Katz L.J. Infectious keratitis in a paracentesis tract. Ophthalmic Surg Laser. 1997;28:332–333. [PubMed] [Google Scholar]
- 18.Ritch R. The pilocarpine paradox. J Glaucoma. 1996;5 [PubMed] [Google Scholar]
- 19.Lee V.Y., Tang J.L., Liu D.T., Chan V.C., Li C.L., Lam D.S. Prospective randomized comparative study of the effect of pupil dilation or miosis in intraocular lens pupillary capture after combined phacoemulsification and vitrectomy with intraocular tamponade. Asia Pac J Ophthalmol. 2012 Mar-Apr;1(2):72–76. doi: 10.1097/APO.0b013e31823e4b82. [DOI] [PubMed] [Google Scholar]
- 20.Duffey R.J., Holland E.J., Agapitos P.J., Lindstrom R.L. Anatomic study of transsclerally sutured intraocular lens implanation. Am J Ophthalmol. 1989;108(3):300–309. doi: 10.1016/0002-9394(89)90121-9. [DOI] [PubMed] [Google Scholar]
- 21.Kim D.J., Kim H.K. Clinical analysis of the factors contributing to pupillary optic capture after transscleral fixation of posterior chamber intraocular lens for dislocated intraocular lens. J Cataract Refract Surg. 2016;42:1146–1150. doi: 10.1016/j.jcrs.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Oh S.Y., Lee S.J., Park J.M. Comparison of surgical outcomes of intraocular lens refixation and intraocular lens exchange with perfluorocarbon liquid and fibrin glue-assisted sutureless scleral fixation. Eye(Lond) 2015;29:757–763. doi: 10.1038/eye.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]