Abstract
Purpose
To report preliminary experience of single-port robotic surgery using the da Vinci SP surgical system in gynecologic tumors.
Materials and Methods
This was a retrospective study on 100 consecutive patients who underwent da Vinci SP single-port robotic surgery between November 2018 and January 2021. All procedures were performed by an experienced gynecologic surgeon using a single 2.5-cm umbilical incision.
Results
Of the 100 cases, the procedures included myomectomy (n=76), hysterectomy (n=2), endometrial cancer surgical staging (n=14), radical hysterectomy (n=3), radical trachelectomy (n=3), and ovarian cystectomy (n=2). None of the cases was converted to robotic multiport or open surgery. The median docking time was 5.0 minutes [interquartile range (IQR), 3.0–7.0], the median console time was 107.5 minutes (IQR, 78.7–155.8), and the median total operation time was 250.0 minutes (IQR, 215.0–310.0). The median estimated blood loss was 50.0 mL (IQR, 30.0–100.0), and the median change in hemoglobin level was 0.8 g/dL (IQR, 0.3–1.3). The median pain scores rated on a numerical rating scale immediately after and at 6, 12, and 24 hours after surgery were 5, 2, 2, and 2, respectively. The mean duration of postoperative hospitalization was 2.8 days.
Conclusion
Da Vinci SP single-port robotic surgery was successfully performed in various gynecologic tumors without significant complications. Therefore, this surgical system could be applied in patients who want precise gynecologic surgery while minimizing surgical incision.
Keywords: da Vinci SP surgical system, single-port surgery, gynecologic tumor
INTRODUCTION
Minimally invasive surgery, including laparoscopic and robotic surgery, is an increasingly common treatment for gynecologic tumors.1,2 The advantages of minimally invasive surgery include decreases in postoperative pain and length of hospital stay.2 Single-port surgery is a major advance that provides better cosmetic outcomes and improved patient satisfaction. However, single-port laparoscopic surgery presents technical challenges, such as limited movement of instruments, collisions between instruments, and poor visualization.3,4,5
Robot surgical systems with optimized ergonomics and endo-wristed instruments can compensate for the limitations of conventional laparoscopic surgery by improving visualization.6 In 2010, the da Vinci single-site platform (Intuitive Surgical, Sunnyvale, CA, USA) was developed to combine the advantages of single-port surgery and robotic surgery.7 As robotic surgery became more popular in gynecologic surgery, robotic single-site surgery has been performed and many studies have shown it to be safe, effective, and feasible.6,8,9,10 However, this platform has less instrument variety and no EndoWrist technology. In June 2018, the da Vinci SP surgical system (Intuitive Surgical) was approved by the FDA for urologic operations. The da Vinci SP surgical system contains four instrument drives that control the articulating camera and up to three robotic instruments that can be positioned simultaneously through a 25-mm SP multichannel port. Unlike previous models of the da Vinci single-site surgical system, the EndoWrist SP instruments have two joints. The wrist joint allows for 7 degrees of freedom, and the elbow joint maintains intracorporeal triangulation in 6-mm fully wristed, elbowed instruments. The 12-mm oval EndoWrist SP camera has a 73-degree field of view. This new single-port robotic surgical system can be very useful in various gynecologic surgery and overcome the limitations of the single-site robotic system.11
There have been very few studies detailing the surgical experiences of using the da Vinci SP surgical system in gynecology. Therefore, we hereby report our initial clinical experience with 100 cases of single-port robotic surgery using the da Vinci SP surgical system in benign and malignant gynecologic tumors.
MATERIALS AND METHODS
We retrospectively reviewed 100 consecutive patients who underwent da Vinci SP single-port robotic surgery for benign or malignant gynecologic tumors between November 2018 and January 2021 at the Women’s Cancer Center, Yonsei Cancer Center in Seoul, Korea. All procedures were performed by one surgeon with more than 10-years of experience in minimally invasive surgery and robotic surgery. This study was approved by an Institutional Review Board (IRB No. 4-2020-0824 dated September 4, 2020).
Patient demographic data, previous medical conditions, previous abdominal surgery, pathology, postoperative course, and follow-up were retrieved from the patients’ medical records. We noted patient characteristics including age, gravidity, parity, body mass index, previous history of abdominal surgery, and diagnosed disease.
Perioperative surgical outcome variables were recorded including the following: robot docking time (defined as time to advance the column to the operating table, fasten the robotic arms to the inserted trocars, and introduce the laparoscope and robotic instruments), console time (defined as time surgeon spent sitting at the console and performing the operation),12 total operation time (defined as the time from the initial umbilical skin incision to the final skin closure), estimated blood loss (EBL), postoperative hemoglobin change, number of conversions to robotic multiport or open surgery, and the number of administered intravenous patient-controlled analgesia and additional intravenous analgesics. Finally, intra- and post-operative complications were reviewed. Data for the length of postoperative hospitalization, defined as the days from operation to discharge, was recorded. The postoperative pain intensity was rated using a numeral rating scale from 0–10 and obtained immediately after surgery and then at 6, 12, and 24 hours after surgery.
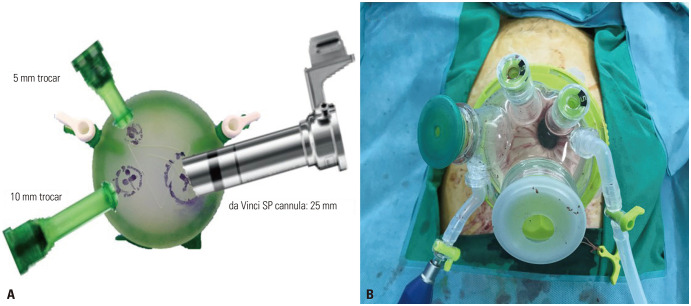
All cases employed the single-port entry system, which offers a 360-degree atraumatic retraction and protection for enhanced exposure, access, and cosmetic results.13,14 We used two types of single-port entry systems: GelPOINT Mini (Applied Medical, Rancho Santa Margarita, CA, USA) and Uni-Port (Dalim, Mapo, Seoul, Korea) (Fig. 1). In the beginning, there was no single-port entry system suitable for the da Vinci SP system, so we used the GelPOINT Mini; however, there were problems such as gas leakage and gel breakdown during the operation. The Uni-Port was designed only for the da Vinci SP system, and had four entry ports of different sizes that can accommodate one da Vinci SP cannula, one 10–15 mm, and two 5 mm-sized laparoscopic instruments at the same time. The GelPOINT Mini was used in 53 cases from November 2018 to April 2020, and the Uni-Port was used in 47 cases from January 2020 to January 2021.
Fig. 1. Single-port entry system for da Vinci SP surgical system. (A) GelPOINT Mini (Applied Medical). (B) Uni-Port (Dalim).
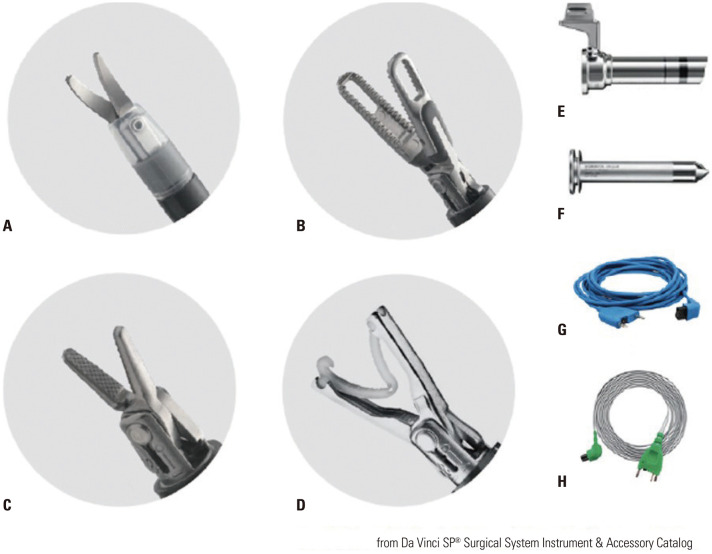
We used the da Vinci SP surgical system to perform single-port robotic surgery in benign and malignant gynecologic tumors. The patients were placed in the dorsal lithotomy position. A 2.5-cm vertical umbilical skin incision was made, and the fascia layer was opened in the same direction using the open Hasson technique. The single-port entry system was inserted into the wound opening. After it was fixed in the incision site, pneumoperitoneum was made through CO2 gas insufflation to 10–12 mm Hg. Then, the patients were placed in the maximum Trendelenburg position. While the da Vinci SP robot surgical system was placed on the right side of the patient, the da Vinci SP cannula (25×100 mm) with four channels was inserted into the single-port entry system. A 12-mm SP camera and three 6-mm robotic instruments were inserted into each channel of the da Vinci SP cannula. The docking was completed by properly positioning each instrument while looking at the camera. We employed the following articulating instruments: da Vinci SP monopolar curved scissor, fenestrated bipolar forceps, needle driver, and medium-large clip applier (Fig. 2). Through the remaining trocar of the single-port entry system, the surgical assistant performed endoscopic suction, put suture materials into the pelvic cavity, and took out the specimen or performed counter-traction with a laparoscopic grasper.
Fig. 2. The da Vinci SP Instruments. (A) Monopolar curved scissors. (B) Fenestrated bipolar forceps. (C) Needle driver. (D) Medium-large clip applier. (E) Cannula. (F) Obturator. (G) Bipolar cautery cord. (H) EnergyShield monopolar cautery cord.
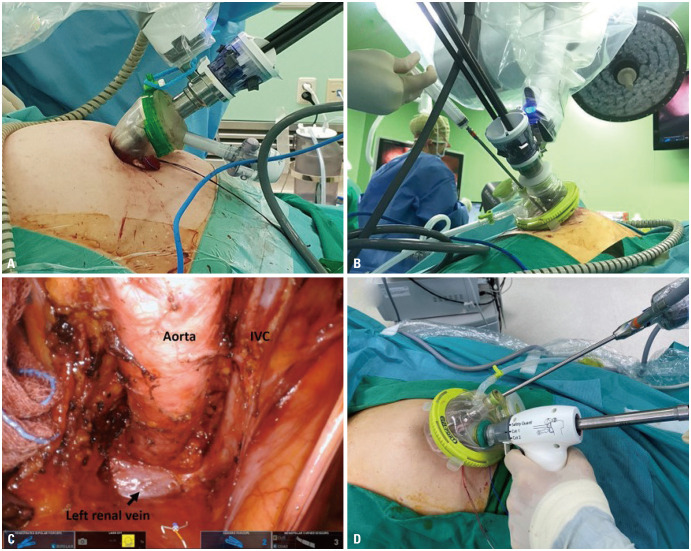
In all surgeries performed using the da Vinci SP surgical system, the overall procedures were the same as that performed by laparoscopy. In myomectomy, vasopressin was administered to the myoma of the uterus. While the surgeon performed the myomectomy, the assistant did traction the myoma using a myoma screw. After surgery, the myoma was placed in a laparoscopic bag, morcellated, and removed through the umbilicus (Fig. 3A, B, and D). In hysterectomy cases, the uterus was inserted into a laparoscopic bag and removed through the vagina. The malignant tumor cases included endometrial cancer and cervical cancer estimated to be at early-stages prior to surgery. In the endometrial cancer surgical staging surgeries (Fig. 3C) and radical hysterectomy cases, we performed bilateral salpingo-oophorectomy and sentinel lymph node dissection using fluorescent image-guided sentinel lymph node mapping with conventional fluorescent laparoscope and indocyanine green. In radical trachelectomy cases, bilateral pelvic sentinel lymph node mapping and dissection were also performed.
Fig. 3. Photographs of da Vinci SP surgical system. (A) External view of the instruments and camera docked through SP cannula fixed to GelPOINT Mini (Applied Medical). (B) External view of injecting vasopressin into the myoma with the instruments and camera docked through SP cannula fixed to Uni-Port (Dalim). (C) Inside view of the paraaortic lymph node dissection in endometrial cancer surgical staging surgery. (D) Morcellation of myomas in an endoscopic bag.
RESULTS
The characteristics for the 100 patients are described in Table 1. The median age of the patients was 37 years (range, 25–61), and the median body mass index was 21.5 kg/m2 (range, 16.0–41.5). Of the 100 cases, 14 patients had a history of abdominal or pelvic surgery. The patients received the following diagnoses: myoma of the uterus (n=76), adenomyosis (n=1), benign ovarian cyst (n=2), endometrial cancer (n=14), and cervical cancer (n=7) by pathologic confirmation. The procedures included myomectomy (n=76), hysterectomy (n=2), endometrial cancer surgical staging (n=14), radical hysterectomy (n=3), radical trachelectomy (n=3), and ovarian cystectomy (n=2).
Table 1. Characteristics of the 100 Patients Who Underwent da Vinci SP Single-Port Robotic Surgery.
| Characteristics | Value | |
|---|---|---|
| Age (yr) | 37 (25–61) | |
| Gravidity | 0 (0–5) | |
| Parity | 0 (0–3) | |
| Body mass index (kg/m2) | 21.5 (16.0–41.5) | |
| Previous abdominal surgery | 14 | |
| Disease | ||
| Myoma | 76 | |
| Adenomyosis | 1 | |
| Ovarian cyst (benign) | 2 | |
| Endometrial cancer | 14 | |
| Cervical cancer | 7 | |
| Procedures | ||
| Myomectomy | 76 | |
| Hysterectomy | 2 | |
| Endometrial cancer surgical staging | 14 | |
| Radical hysterectomy | 3 | |
| Radical trachelectomy | 3 | |
| Ovarian cystectomy | 2 | |
Data are presented as median (range) or n (%).
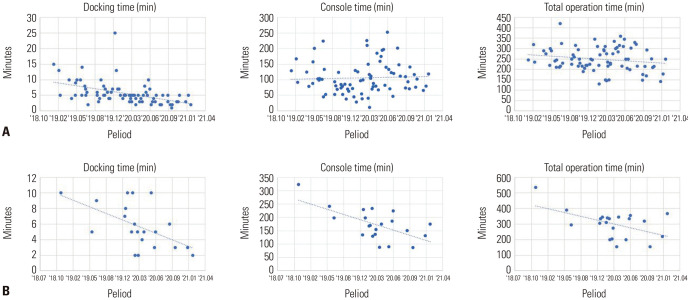
Table 2 shows the perioperative surgical outcomes categorized by benign disease (n=79) and malignant disease (n=21). The median docking time was 5.0 minutes [interquartile range (IQR), 3.0–7.0] for all cases, 5.0 minutes (IQR, 3.5–6.5) for benign disease, and 5.0 minutes (IQR, 3.0–8.0) for malignant disease. The median console time was 107.5 minutes (IQR, 78.7–155.8) for all cases, 97.0 minutes (IQR, 71.5–129.5) for benign disease, and 170.0 minutes (IQR, 135.0–198.0) for malignant disease. The median total operation time was 250.0 minutes (IQR, 215.0–310.0) for all cases, 245.0 minutes (IQR, 215.0–294.0) for benign disease, and 319.0 minutes (IQR, 221.0–345.0) for malignant disease. The median EBL was 50.0 mL (IQR, 30.0–100.0) for all cases, 50.0 mL (IQR, 30.0–100.0) for benign disease, and 30.0 mL (IQR, 30.0–50.0) for malignant disease. The median change in hemoglobin level was 0.8 g/dL (IQR, 0.3–1.3) for all cases, 0.9 g/dL (IQR, 0.4–1.3) for benign disease, and 0.3 g/dL (IQR, 0.0–1.2) for malignant disease. No case required additional assistant port or open surgery. Fig. 4 shows the incision size after closing the umbilicus in da Vinci SP robot surgery. The incision size was less than 2.5 cm. Fig. 5 shows a learning curve graph of docking time, console time, and total operation time for benign disease and malignant disease, respectively. These times generally decreased over time as surgical experience increased. In the benign disease cases, the total operation time shows a slight change over time, and the console time is rather long over time. However, all times in the malignant disease cases are shortened over time. Therefore, technical proficiency and familiarity with the system should predictably decrease total operation times.
Table 2. Perioperative Surgical Outcomes of da Vinci SP Gynecologic Surgery (n=100).
| Surgical outcomes | Benign disease (n=79) | Malignant disease (n=21) | Total (n=100) | |
|---|---|---|---|---|
| Docking time, min | 5.0 (3.5–6.5) | 5.0 (3.0–8.0) | 5.0 (3.0–7.0) | |
| Console time, min | 97.0 (71.5–129.5) | 170.0 (135.0–198.0) | 107.5 (78.7–155.8) | |
| Total operation time, min | 245.0 (215.0–294.0) | 319.0 (221.0–345.0) | 250.0 (215.0–310.0) | |
| Estimated blood loss, mL | 50.0 (30.0–100.0) | 30.0 (30.0–50.0) | 50.0 (30.0–100.0) | |
| Postoperative hemoglobin change, g/dL | 0.9 (0.4–1.3) | 0.3 (0.0–1.2) | 0.8 (0.3–1.3) | |
| Conversion to multiport or open surgery | 0 (0) | 0 (0) | 0 (0) | |
| Patient-controlled analgesia | 0 (0) | 1 (4.8) | 1 (1) | |
| Intravenous analgesics | 28 (35.4) | 8 (38.1) | 36 (36) | |
| Intraoperative complications | ||||
| Transfusion | 0 (0) | 0 (0) | 0 (0) | |
| Others | 0 (0) | 1 (4.8) | 1 (1) | |
| Postoperative complications | ||||
| Transfusion | 0 (0) | 0 (0) | 0 (0) | |
| Wound complications | 1 (1.3) | 0 (0) | 1 (1) | |
| Postoperative hospital stay, day | 2.5±0.7 | 3.6±0.9 | 2.8±0.9 | |
Data are presented as median (interquartile range), n (%) or mean±standard deviation.
Fig. 4. Incision size after closing the umbilicus in da Vinci SP robot surgery to remove a gynecological tumor. The incision size was less than 2.5 cm.
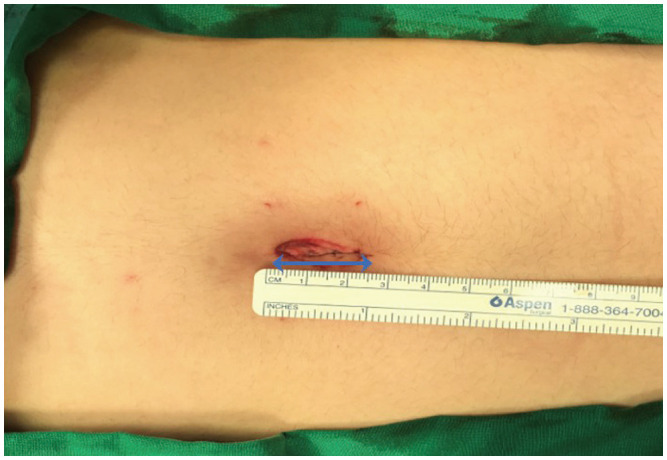
Fig. 5. Docking time, console time, and total operation time for (A) benign tumors and (B) malignant tumors.
Enhanced Recovery After Surgery (ERAS) guidelines recommend that a multimodal approach to analgesia should be adopted, including the use of nonsteroidal anti-inflammatory drugs (NSAIDs)/acetaminophen, gabapentin, and dexamethasone.15 We have been implementing the ERAS protocol since 2019, and all patients received NSAIDs intravenously three times a day on the day of surgery and the day after surgery. At that point, the injected analgesics were changed to oral analgesics. Intravenous patient-controlled analgesia and additional intravenous analgesics (tramadol, pethidine) were needed in one patient and 36 patients, respectively. The median pain scores immediately after surgery and then at 6, 12, and 24 hours following surgery were 5, 2, 2, and 2, respectively (Table 3 and Supplementary Fig. 1, only online).
Table 3. Postoperative Pain Score in Patients Who Underwent da Vinci SP Gynecologic Surgery (n=100).
| Pain score* | Benign disease (n=79) | Malignant disease (n=21) | Total (n=100) |
|---|---|---|---|
| Immediate postoperative | 5.0 (4.0–6.0) | 5.0 (4.0–5.0) | 5.0 (4.0–6.0) |
| At 6 hours | 2.0 (2.0–3.0) | 2.5 (2.0–3.0) | 2.0 (2.0–3.0) |
| At 12 hours | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) |
| At 24 hours | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) |
*numeral rating scale, median (interquartile range).
Intraoperative complications occurred in one patient. A patient who underwent endometrial cancer staging experienced a superficial bowel laceration due to severe adhesion from prior surgery. The patient had a history of myomectomy and the laceration was repaired with an interrupted Vicryl 3-0 suture. The patient did not require any other treatment after the operation and was discharged without any problems. No blood transfusion was needed during and after surgery in all cases.
Postoperative wound complications occurred in one patient who underwent myomectomy. The patient visited the outpatient clinic about a week after discharge with a small amount of yellow discharge from the umbilical wound. The wound was healed cleanly by dressing the site with betadine and the patient taking oral antibiotics for 5 days. There were no other serious postoperative complications, such as wound dehiscence, surgical site hematoma, umbilical hernia, urinary track, or bowel injury. The mean duration of postoperative hospitalization was 2.8±0.9 days for all cases. None of the patients was readmitted after discharge.
DISCUSSION
Robotic single-site surgery still has some challenges of using the semi-rigid, single-site instruments which come with restricted range of motion. Additionally, the robotic arm can cause crowding, especially in conjunction with the bulkiness of the complete robotic system.7,16 The da Vinci SP surgical system was designed to overcome these limitations. EndoWrist instruments of the da Vinci SP surgical system with two joints endows the system with sufficient articulation, proper power, and less crowding. Using this system, it is possible to effectively perform surgery in a narrow space without colliding instruments.
Until now, there are only two studies worldwide reporting clinical gynecologic experiences with the da Vinci SP surgical system. Shin, et al.17 presented their initial experience performing the da Vinci SP single-port robotic surgery in benign gynecologic diseases in 31 cases. Misal, et al.18 presented a total of eight cases of hysterectomy performed successfully with the da Vinci SP surgical system for benign gynecologic diseases. Together, these studies have demonstrated that da Vinci SP single-port robotic surgery is feasible and safe for various benign gynecologic diseases.
The present study reports the initial experience with 100 cases of the da Vinci SP single-port robotic surgery in benign and malignant gynecologic tumors that were performed by an experienced robotic surgeon. The single-port robotic surgeries were successfully performed in all cases without any serious problems. There were no instances of conversion to robotic multiport or open surgery. We performed various single-port robotic surgeries including myomectomy, hysterectomy, endometrial cancer surgical staging, radical hysterectomy, radical trachelectomy, and ovarian cystectomy. In this study, the total operation times seemed to be longer than those reported in previous studies.17,18 However, since the types of gynecologic procedures performed differed from previous studies, it is not reasonable to directly compare the operation times.
A key advantage of single-port surgery is improved cosmetic outcomes due to the small incision. To perform the da Vinci SP single-port robotic surgery, we made a 2.5-cm vertical umbilical skin incision. This incision size is larger than the 1.5-cm incision size commonly used for single-port laparoscopic surgery. The larger incision was needed to accommodate the special single-port entry system as well as the assistant instruments. However, the umbilical wound following single-port robotic surgery appeared similar to what we have observed for single-port laparoscopic surgery (Fig. 4).
Other important advantages of minimally invasive surgery are minimized pain and short hospital stays. In the present study, the median pain score at 6 hours postoperatively was 2, indicating mild pain, and patients were discharged from the hospital on an average of 2.8 days after surgery. Therefore, patients experienced minimal pain and short hospital stays following surgery with the da Vinci SP surgical system.
The present study has several notable features. To our knowledge, this study includes the largest number of da Vinci SP single-port robotic surgery cases reported to date by a single surgeon in gynecologic tumors. Also, this is the first study to include da Vinci SP single-port robotic surgeries for gynecologic malignant tumors. We have successfully performed most gynecologic cancer surgeries, including radical hysterectomy, radical trachelectomy, pelvic lymph node dissection, and paraaortic lymph node dissection, using the da Vinci SP single-port robotic surgery. In a study using a different da Vinci single-site robotic surgery system for benign gynecologic tumors (n=1) and early stage gynecologic cancers (n=5), Yoo, et al.9 reported a median total operative time of 211 minutes, median EBL of 125 mL, and median postoperative hospital stay of 4 days. In comparison, our study had longer total operation time; however, the EBL was low, and the postoperative hospital stay was short.
The total operation time in our study was relatively longer than that previously reported, especially in malignant cases. The total operation time in malignant cases included the time for Indocyanine Green injection and sentinel lymph node mapping in paraaortic and pelvic area, as well as tissue removal using laparoscopic tissue retrieval bag. In sentinel lymph node mapping, conventional fluorescent laparoscopic camera was used, and it usually takes quite a long time to explore the sentinel lymph node with laparoscope.
In the learning curve of Fig. 5, the operation time was much shorter compared to benign cases, although malignant cases were not large in number. The first case of malignancy surgery was the endometrial cancer surgical staging operation in a very obese woman. After skin incision, we found that the operation table was too high for the patient to get the da Vinci SP robotic surgery, and it did not get lowered enough for docking the robotic system. The total operation time of the first case was prolonged to change the table with a new one that can be lowered enough to accommodate the SP system. In the total operation time graph, the effect of the first case seemed to be quite significant in malignant cases. In addition, the more experienced the surgeon became with the da Vinci SP system, the shorter the total operation time was. However, in benign cases, as the surgeon became more experienced with the da Vinci SP single-port robotic system, the total operation time was not significantly reduced by operating on more complicated cases.
The present study was limited by the heterogeneity of the performed procedures. The specific preferences of surgeon may have influenced the characteristics of patients deemed fit for robotic surgery, potentially causing a selection bias. There were also limitations due to the retrospective design and short follow-up period.
Over the past 5 years, the number of robotic surgeries performed worldwide has increased by 20% every year. In a study examining the trend of robotic surgery in Korean gynecology, Lee, et al.19 reported that since the introduction of robotic surgical platforms in Korea, gynecologic robotic surgeries for benign and malignant gynecologic diseases have been rapidly developing, and that they expect the use of robotic surgery in gynecologic diseases to develop continuously.
In addition to this momentum, the current study demonstrated that the da Vinci SP single-port robotic surgery was feasible in most benign and malignant gynecologic tumors when it was performed by an experienced robotic surgeon. The da Vinci SP surgical system may be ideal for most gynecological tumor patients who want minimized surgical incision while maintaining surgical dexterity. This robotic system may be more widely used in the near future with improvements in the surgical instruments and surgical techniques of gynecologic surgeons.
ACKNOWLEDGEMENTS
This work was supported by research funding by Intuitive Surgical.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Young Hwa Kwak, Hwajung Lee, and Sang Wun Kim.
- Data curation: Young Hwa Kwak, Hwajung Lee, Kieun Seon, and Sang Wun Kim.
- Formal analysis: Young Hwa Kwak, Kieun Seon, Young Joo Lee, and Sang Wun Kim.
- Investigation: Young Hwa Kwak, Kieun Seon, Young Joo Lee, and Sang Wun Kim.
- Methodology: Young Hwa Kwak, Hwajung Lee, Yong Jae Lee, and Sang Wun Kim.
- Project administration: Young Hwa Kwak, Yong Jae Lee, and Sang Wun Kim.
- Resources: Yong Jae Lee and Sang Wun Kim.
- Software: Young Hwa Kwak, Hwajung Lee, Young Joo Lee, and Sang Wun Kim.
- Supervision: Yong Jae Lee and Sang Wun Kim.
- Validation: Yong Jae Lee and Sang Wun Kim.
- Visualization: Young Hwa Kwak, Kieun Seon, Young Joo Lee, and Sang Wun Kim.
- Writing—original draft: Young Hwa Kwak.
- Writing—review & editing: Sang Wun Kim.
- Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIAL
Postoperative pain score in patients who underwent da Vinci SP gynecologic surgery (n=100). NRS, numeral rating scale.
References
- 1.Conrad LB, Ramirez PT, Burke W, Naumann RW, Ring KL, Munsell MF, et al. Role of minimally invasive surgery in gynecologic oncology: an updated survey of members of the Society of Gynecologic Oncology. Int J Gynecol Cancer. 2015;25:1121–1127. doi: 10.1097/IGC.0000000000000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Von Gruenigen VE, Sawyer MD, Ponsky LE, Hurd WW. Recent innovations in minimally invasive surgery and implications for gynecology. J Gynecol Surg. 2009;25:67–72. [Google Scholar]
- 3.Kaouk JH, Autorino R, Kim FJ, Han DH, Lee SW, Yinghao S, et al. Laparoendoscopic single-site surgery in urology: worldwide multiinstitutional analysis of 1076 cases. Eur Urol. 2011;60:998–1005. doi: 10.1016/j.eururo.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010;203:26.e1–26.e6. doi: 10.1016/j.ajog.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 5.Nelson RJ, Chavali JSS, Yerram N, Babbar P, Kaouk JH. Current status of robotic single-port surgery. Urol Ann. 2017;9:217–222. doi: 10.4103/UA.UA_51_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nam EJ, Kim SW, Lee M, Yim GW, Paek JH, Lee SH, et al. Robotic single-port transumbilical total hysterectomy: a pilot study. J Gynecol Oncol. 2011;22:120–126. doi: 10.3802/jgo.2011.22.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morelli L, Guadagni S, Di Franco G, Palmeri M, Di Candio G, Mosca F. Da Vinci single site© surgical platform in clinical practice: a systematic review. Int J Med Robot. 2016;12:724–734. doi: 10.1002/rcs.1713. [DOI] [PubMed] [Google Scholar]
- 8.Cela V, Freschi L, Simi G, Ruggiero M, Tana R, Pluchino N. Robotic single-site hysterectomy: feasibility, learning curve and surgical outcome. Surg Endosc. 2013;27:2638–2643. doi: 10.1007/s00464-012-2780-8. [DOI] [PubMed] [Google Scholar]
- 9.Yoo HN, Kim TJ, Lee YY, Choi CH, Lee JW, Bae DS, et al. Single-site robotic surgery in gynecologic cancer: a pilot study. J Gynecol Oncol. 2015;26:62–67. doi: 10.3802/jgo.2015.26.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogliolo S, Mereu L, Cassani C, Gardella B, Zanellini F, Dominoni M, et al. Robotic single-site hysterectomy: two institutions’ preliminary experience. Int J Med Robot. 2015;11:159–165. doi: 10.1002/rcs.1613. [DOI] [PubMed] [Google Scholar]
- 11.Garisto JD, Bertolo R, Kaouk J. Technique for docking and port placement using a purpose-built robotic system (SP1098) in human cadaver. Urology. 2018;119:91–96. doi: 10.1016/j.urology.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 12.Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008;109:86–91. doi: 10.1016/j.ygyno.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Reid K, Pockney P, Draganic B, Smith SR. Barrier wound protection decreases surgical site infection in open elective colorectal surgery: a randomized clinical trial. Dis Colon Rectum. 2010;53:1374–1380. doi: 10.1007/DCR.0b013e3181ed3f7e. [DOI] [PubMed] [Google Scholar]
- 14.Horiuchi T, Tanishima H, Tamagawa K, Matsuura I, Nakai H, Shouno Y, et al. Randomized, controlled investigation of the anti-infective properties of the Alexis retractor/protector of incision sites. J Trauma. 2007;62:212–215. doi: 10.1097/01.ta.0000196704.78785.ae. [DOI] [PubMed] [Google Scholar]
- 15.Nelson G, Altman AD, Nick A, Meyer LA, Ramirez PT, Achtari C, et al. Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations--Part II. Gynecol Oncol. 2016;140:323–332. doi: 10.1016/j.ygyno.2015.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi EJ, Rho AM, Lee SR, Jeong K, Moon HS. Robotic single-site myomectomy: clinical analysis of 61 consecutive cases. J Minim Invasive Gynecol. 2017;24:632–639. doi: 10.1016/j.jmig.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Shin HJ, Yoo HK, Lee JH, Lee SR, Jeong K, Moon HS. Robotic single-port surgery using the da Vinci SP® surgical system for benign gynecologic disease: a preliminary report. Taiwan J Obstet Gynecol. 2020;59:243–247. doi: 10.1016/j.tjog.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 18.Misal M, Magtibay PM, Yi J. Robotic LESS and reduced-port hysterectomy using the da Vinci SP surgical system: a single-institution case series. J Minim Invasive Gynecol. 2021;28:1095–1100. doi: 10.1016/j.jmig.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee S, Kim MR, Seong SJ, Paek J, Lee YS, Nam EJ, et al. Trends in robotic surgery in Korean gynecology. Gyne Robot Surg. 2020;1:50–56. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Postoperative pain score in patients who underwent da Vinci SP gynecologic surgery (n=100). NRS, numeral rating scale.