Abstract
Implementation of an infrastructure to support digital pathology began in 2006 at Memorial Sloan Kettering Cancer Center. The public health emergency and COVID-19 pandemic regulations in New York City required a novel workflow to sustain existing operations. While regulatory enforcement discretions offered faculty workspace flexibility, a substantial portion of laboratory and digital pathology workflows require on-site presence of staff. Maintaining social distancing and offering staggered work schedules. Due to a decrease in patients seeking health care at the onset of the pandemic, a temporary decrease in patient specimens was observed. Hospital and travel regulations impacted onsite vendor technical support. Digital glass slide scanning activities onsite proceeded without interruption throughout the pandemic, with challenges including staff who required quarantine due to virus exposure, unrelated illness, family support, or lack of public transportation. During the public health emergency, we validated digital pathology systems for a remote pathology operation. Since March 2020, the departmental digital pathology staff were able to maintain scanning volumes of over 100 000 slides per month. The digital scanning team reprioritized archival slide scanning and participated in a remote sign-out validation and successful submission of New York State approval for a laboratory developed test. Digital pathology offers a health care delivery model where pathologists can perform their sign out duties at remote location and prevent disruptions to critical pathology services for patients seeking care at our institution during emergencies. Development of standard operating procedures to support digital workflows will maintain turnaround times and enable clinical operations during emergency or otherwise unanticipated events.
Keywords: digital pathology, COVID-19, implementation, operations, clinical, telepathology, remote signout
Introduction
Coronavirus disease 2019 (COVID-19) disrupted the world, and with large impact in New York City (NYC), a global travel hub with high population density, at the early days of the pandemic, in March and April 2020. Memorial Sloan Kettering Cancer center (MSKCC) is a large tertiary care center with 514 beds and 560 000 outpatient visits a year in its main hospital in Manhattan and 19 ambulatory sites across the states of New York and New Jersey. The hospital had to respond effectively to the viral spread with leadership needed to quickly adapt operations to support patients and staff. Patients with cancer are among those most vulnerable to severe illness from respiratory viral infections. 1,2 By April 10, 2020, New York State had 9385 reported deaths, and patients with cancer comprised 8.4% of deceased individuals. 3
Memorial Sloan Kettering Cancer center had developed polymerase chain reaction testing for COVID-19 by March 10, 2020. 3,4 From March 10 until May 7, 2020, SARS-CoV-2 was detected in 946 patients at MSKCC. 3 During the peak pandemic days, patient positivity rate had a rate of 4.3% that fell below 0.3% after April 2020. 4
Memorial Sloan Kettering Cancer center utilized the Hospital Incident Command System (HICS) to coordinate essential services and assign responsibilities during emergencies. This system was integrated with local, state, and federal incident command processes and includes representation from all stakeholders in the organization. The system was fully activated in March 2020 with daily staff updates.
The institutional response guided the pathology department’s management of the pandemic in a short period of time. Pathology services continued throughout the months surveyed in this study (eg, March-June 2020). This period included the initial days of the pandemic following the diagnosis of the first case in NYC, the city’s mandated lockdown as well as power outages due to weather and the civilian unrest on the weeks that followed the May 25 killing of George Floyd (See Table 1 for timeline).
Table 1.
Timeline of Study Period (In Bold, MSKCC Hospital Wide Response).
| January 11, 2020 | China reports first COVID-19 death |
| January 21, 2020 | First confirmed COVID-19 case in the United States |
| February 5, 2020 | MSKCC Hospital Incident Command System (HICS) activated |
| March 1, 2020 | First COVID-19 case in New York State |
| March 7, 2020 | NY Governor Andrew Cuomo declares a state of emergency |
| March 8, 2020 | NYC issues guidelines to avoid densely packed buses, subways, or trains |
| March 12, 2020 | Discussions for pathology remote sign-out contingency plan and initiation of validation |
| March 13, 2020 | President Trump declares a national emergency. First 2 COVID-19 deaths in NYS |
| March 14, 2020 | MSK offers commuter assistance |
| March 16, 2020 | NYC public schools close |
| March 19, 2020 | Suspension of research activities and rescheduling noncritical follow-up visits at MSK. |
| March 22, 2020 | NYS on Pause Program begins, all nonessential workers must stay home |
| March 26, 2020 | CMS temporary waiver for CLIA licenses requirement for remote locations |
| March 27, 2020 | MSK Employee Relief Fund assistance to employees. Hotel accommodations offered to employees who are working onsite |
| March 30, 2020 | Face mask mandate at MSK |
| March 31, 2020 | NYC passes 1000 COVID-19 deaths |
| April 3, 2020 | Mandatory online health check for employees |
| April 14, 2020 | Remote digital pathology validation completed |
| April 15, 2020 | New York requires face masks in public places |
| April 24, 2020 | FDA non 510(k) device guidance for remote reviewing and reporting of scanned digital images of pathology slides |
| April 30, 2020 | Nightly NYC subway closures from 1 am to 5 am |
| May 4, 2020 | Conditional approval by New York State for remote digital pathologist review of digital images for digital (remote) pathology |
| May 25, 2020 | George Floyd is killed by Minneapolis police |
| May 27, 2020 | US COVID-19 deaths pass 100 000 |
| June 2-7, 2020 | NYC daily curfew 8 pm-5 am |
| June 8, 2020 | NYC begins Phase 1 reopening |
| June 22, 2020 | NYC begins phase 2 of reopening |
Abbreviations: MSKCC, Memorial Sloan Kettering Cancer center; NYC, New York City; NYS, New York State; CMS, Centers for Medicare & Medicaide Services; CLIA, Clinical Laboratory Improvement Amendments; FDA, Food & Drug Administration.
Unanticipated operations challenges to the pathology department included access to personal protective equipment (PPE) in a state of global shortage. The access to PPE had to be rationed to staff in labs and administration to maintain supply to the patient facing frontline workers.
Implementation of an infrastructure to support digital pathology began over a decade ago at MSKCC. To date, the digitized slide volumes surpasses 3.3 million slides (data not shown). During the pandemic, digital scan operations at MSKCC went uninterrupted while making changes to maintain quality operations and protecting the well-being of staff and their families.
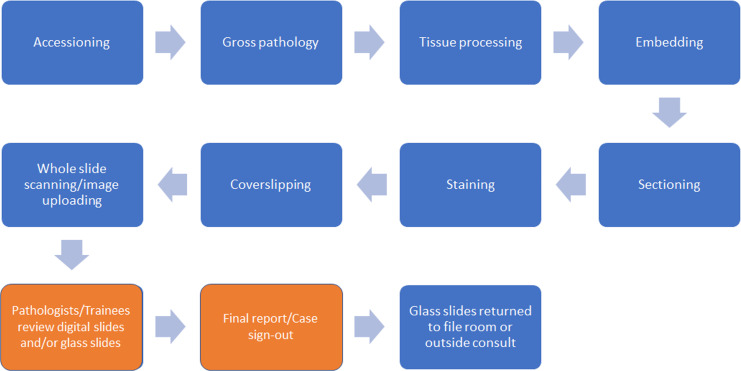
While many pathology staff and pathologists were able to work remotely, a substantial portion of pathology laboratory and digital pathology workflows required on-site presence of staff for the preanalytical and postanalytical steps. These steps (Figure 1) include not only the preanalytic steps of specimen delivery, accession, processing, and digitization (steps 1-4) but also the quality control (QC) steps to ensure the quality of the digital scans before pathologist review (step 5) and the collation and filing of glass slides post the review process (step 7). These steps are all time sensitive and require a coordinated effort of individuals from multiple departments including couriers, accessioning, laboratory, and digital scanning.
Figure 1.
Schematic workflow of pathology glass slides at MSKCC from specimen receiving to pathologist signout. In blue—steps that require on-site support staff whereas only 2 steps shown in orange can be achieved remotely.
A digital scan team, comprised of digital scanning associates and managers at the department of pathology, is responsible for digitization of microscopy glass slides following their generation (ie, sectioning, staining, coverslipping, drying) in the histology lab as well as archival scanning of patient’s cases that were previously reported. The team consists of 21 individuals who are employed at the main hospital in Manhattan as well as in an archival warehouse in the Bronx where accessioned cases from prior years are stored. There are 26 scanners located at 4 disparate locations that are being used in these scanning operations, a few of these scanners are being used solely for research activities. For prospective clinical scanning, 3 Leica Aperio GT450 (Leica Biosystems), 3 Philips Ultra Fast Scanner (Philips Best), and one 3DHistech P1000 (3DHistech Budapest) whole slide scanners were used.
In this report, we describe the response of the department of pathology and the digital scan operations during the months of March to June 2020, the approaches to meeting the pandemic challenges, and the workflow adaptations to ensure continuous patient care in times of emergencies.
Methods
Digital scanning operations data was retrieved from our laboratory information system and scanning records. These data include the number of glass slides scanned each day over the study period by each individual whole slide scanner and scanning location. Vendor service visits and instrument failure were retrieved from laboratory records. Human resources (HR) management software records were used to determine employee attendance during this period, distance from work was collected based on employee residence zip codes, mode of transportation to work, specific employee concerns, and family members health issues were self-reported by employees to their managers. All data was kept confidential, deidentified, and pooled together before analysis. Confidentiality requirements pursuant to the Health Insurance Portability and Accountability Act of 1996 and employment law have limited the ability to share specific information about infected individuals on our team.
Results
Operations
Cancer hospitals have seen a marked decrease in patient visits and in treatment volume during the height of the pandemic 5,6 with most nonurgent surgeries temporary suspended. 7 At MSKCC, SARS-CoV-2 was detected in 946 patients from March 10 to April 7, 2020. 3 Memorial Sloan Kettering Cancer center experienced a temporary decrease peaking on April 19, 2020 which was a ∼75% drop from median normal volumes, however showed a recovery in subsequent weeks in patient specimen accessions and by the end of the summer the department was showing relatively normal number of accessioned cases (data not shown). Despite fluctuations in specimen volume, pathology operations were available and uninterrupted throughout the pandemic.
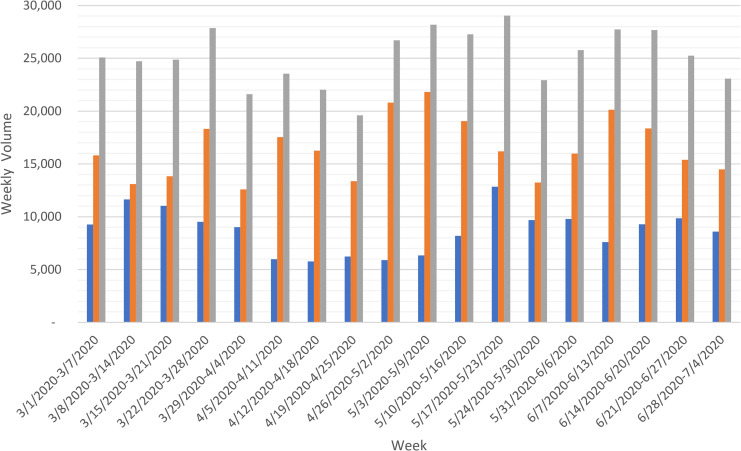
The weekly pathology glass slide scan totals remained mostly unchanged during the month of March, with a 15% decrease in total scan volume during the month of April (Figure 2). During this period, the current slide scan decreased by 35% due to a general decline in hospital visits and elective surgeries. The scanning activities benefited from the flexibility of shifting from current to archival scans using available scanner and staffing capacity.
Figure 2.
Weekly glass slide scans at MSKCC’s department of pathology. Current scanning volumes (blue) indicate prospective digital slide scanning, where archival scanning (orange) refers to digitization of off-site glass slides from prior accessioned years. In gray, combined archival and current slide scans. All whole slide images are interfaced with the anatomic pathology laboratory information system and may be accessed for clinical use.
Scan volumes increased in May and exhibited normal weekly variation that is a result of staffing and technical issues. Of note is the decline in scan operations during the city curfew period from June 1 to 7 following the death of George Floyd on May 28 and the protests that started on May 29. The scanning volumes of over 100 000 slides per month were maintained throughout this period.
The digital scanning team reprioritized archival slide scanning and participated in a remote sign-out validation and successful submission of NY State approval for a laboratory developed test to remotely review and report on patient specimens using digital pathology.
As mentioned, the digital scan team is required to be on-site in close coordination with the laboratory staff to ensure timely scanning of glass slides with sufficient quality checks. Digital pathology is a disruptive technology such that there is an additional time requiring step for each glass slide that is needed before case distribution to the trainees or pathologists. Modifying workflows and training for staff was required to minimize delays in turnaround time. Downtime periods where slides were traditionally being collated with their respective cases or awaiting review overnight were used for digital scanning efforts to show no difference in slide distribution or case reporting turnaround time. As a result, histotechnologists were trained to load and operate basic functionality on the high throughput whole slide scanners, whereas the digital scan team offered troubleshooting and technical support as needed, in addition to both teams providing QC checks on the glass slides and whole slide images. An effort was made to increase the likelihood of successful first time scans. The laboratory histology workflow was modified and staff was provided best practices to facilitate digital scanning efforts, such as centering of tissue during embedding and sectioning, ensuring tissue is not present at the edge or past glass slide coverslips, and allowing time for racks to fully dry before being loaded into the whole slide scanners.
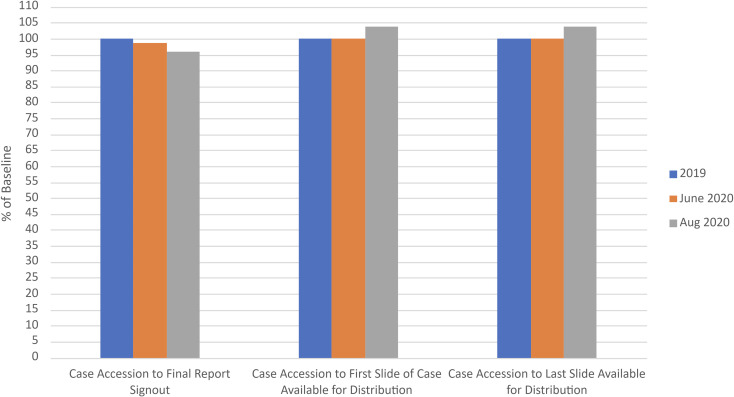
Prospective scanning of biopsy glass slides started in August 2020. The median turnaround time for the cases was assessed in the month following the adoption of the prospective scanning. Three different metrics were used: Case accession to final report signout; case accession to first slide of case available for distribution; and case accession to last slide of case available for distribution (Figure 3). These values were compared to median turnaround time that was measured for the year 2019 and for June 2020, the month preceding prospective biopsy glass slide scanning. The analysis demonstrates there was no significant delay in the time from case accession to first slide of case available for distribution and case accession to last slide of case available for distribution from the laboratory baseline compared to after prospective clinical scanning (3.8% and 3.7%, respectively). The delay was likely due to the incremental time of scanning the glass slides, however altogether, the total time from case accessioning to final report signout decreased by 4.3% from 2019 to August 2020 following the prospective scanning workflow adoption in clinical practice. Not all cases were reported digitally; however, these data show that prospective scanning of glass slides were able to maintain turnaround times even with the additive scanning workflow.
Figure 3.
Median relative turnaround time assessments before and after prospective biopsy scanning of glass slides as percent of 2019 data which was used as baseline (in blue). June 2020 median turnaround time directly preceding prospective scanning began (in orange); August 2020, median turnaround time following prospective scanning implementation (in gray).
Staffing, Scheduling, and Wellness
A major effort was made to maintain staff health at the department. Daily health questionnaires were sent out to all hospital employees to monitor employee symptoms, infections, and allow trace contacting, and prevent further spread of the virus. Frequent COVID-19 testing and sick time accommodations were offered for those who were found to be positive for the infection. When needed, staff were redeployed to meet changing clinical needs and volumes at the hospital.
During the period described in this study (March 2 to June 30, 2020), the digital scan team included 21 full time employees, an additional individual who worked full time from March 2 to May 1, and another individual who was hired on May 5 but was only fully trained after the end of this study period. In addition, we had 2 part time individuals who contributed 45 days of work combined in this period. The MSK work experience of these employees ranged from 6 months to 22.5 years, with a total of 108 years of work experience at MSK.
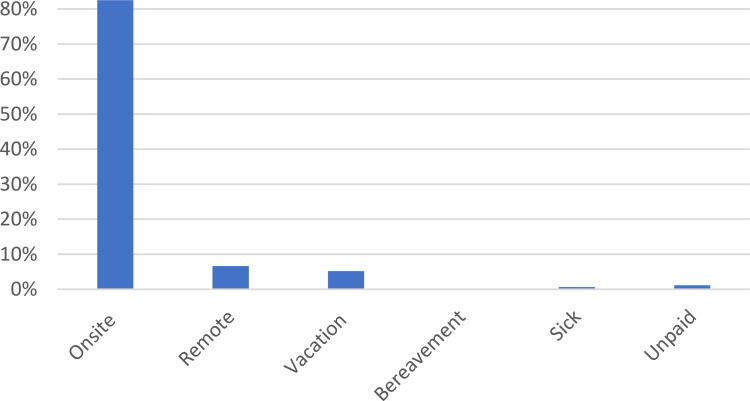
The total number of employed full days in the period was 1761 days. During this time, 5 full time employees worked a total of 117 days remotely, doing image review, planning, research, administration, and other slide scanning operations activities that did not require onsite presence (Figure 4). Four senior-level digital scan team staff members worked additional overtime hours for a total of 85 hours during this period.
Figure 4.
Workday distribution among staff during the study period as % of total work days in period (n = 1761).
All employees expressed concern over their safety of working at a Manhattan hospital with NYC being the epicenter of the pandemic at the United States. Most expressed the conflict of not staying with their families at home. During the study period, 14 individuals took newly requested or previously planned vacation days ranging from 1 day to 22 consecutive days. In total, there were 96 vacation days that were taken by the team members with 3 individuals responsible for 56 of those days. These individuals used their vacation days early on after the lockdown to avoid coming to the hospital for fear of being infected and/or infecting their family members. In an effort to minimize potential employee work exposure to the virus, the team management followed World Health Organization 8 and MSKCC HICS recommendations to modify operations to minimize staff who is present onsite and allow more social distancing for employees. Digital scan team members’ workstations were rearranged with more spacing between stations for social distancing, and the work areas were decluttered to allow better cleaning and sanitation practices. Employee schedules were modified to allow flexible work to all employees based on their family and transportation needs when possible. Two digital scan associates chose to work 12 hour shifts, 3 days a week. Two chose 10 hour shifts, 4 days a week. Tasks that did not require onsite presence were identified and allowed to have a staggered rotation among senior personnel with 1 to 2 individuals working from home every day, and the other starting their workday at 5, 7, or 8 am. As a result of this effort, scanner use was expanded and included late afternoon and evening scans allowing greater use of current equipment.
Improvements were also made in hospital facilities in response to the growing threat of the pandemic. Hospital meeting rooms and break rooms reduced their capacity, and additional lounge areas were offered by the hospital for those employee breaks. All nonclinical activities were minimized and all research labs and activities were shut down. Team meetings were held remotely and most team communication was done by emails and messaging.
Mode of Transportation to Site and Transportation Adjustments
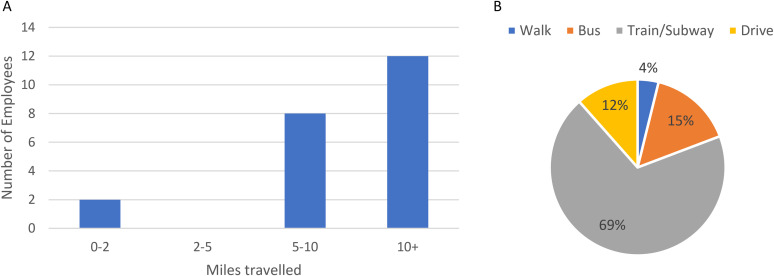
Public transportation in NYC in the study periods was restricted to essential travel only, and some routes were operating on limited schedules. Hospital employees were designated as essential workers in March and all employees had this designation label added to their ID badge per HICS guidance. In addition, all employees were encouraged to carry a hospital letter explaining their role as an essential employee in case they get stopped by law enforcement. The staff’s commute was to 2 main locations. One in the Bronx, where archival scanning takes place, and the second in the main hospital in Manhattan. Twenty-two of the 23 employees were not within walking distance of these 2 working sites and had a 5 mile and more commute to work every day (Figure 5).
Figure 5.
Distance from work of digital scan team members based on reported residence zip codes (A) and mode of transportation to Work (B).
The commute for 18 employees was previously reliant on public transportation and 14 of them had either a subway or train ride as part of their daily commute to the hospital (Figure 5B). These employees’ commute was severely interrupted with reduced subway and train schedules that were imposed by the city and the Metropolitan Transportation Authority (MTA). An additional concern was the unknown infectivity rate and personal safety on the buses and trains in the city. Coverage of personal car or car service expenses for some employees was offered during the early part of the pandemic to assist employees who lost their public transportation routes.
Between June 2 to 7, 2020, NYC imposed daily curfew from 8 pm to 5 am in response to the protests and civil unrest following the killing of George Floyd on May 25. Though essential employees were exempt from this curfew, public transportation was not guaranteed, and steps were taken to ensure that employees would not have to travel during these times. These steps included modified work schedules to guarantee employees abilities to get to their homes before the start of the curfew at 8 pm or leave to work after the curfew was lifted at 5 am.
Adverse Events
Though all staff members were affected by the pandemic, a significant percent of the digital scan team members had either personal or loved ones experience health issues related to the virus. Some team members reported testing positive for SARS-CoV-2 after developing symptoms to the virus in both the main hospital and the Bronx location. Additional team members had experienced a loss of a close family member during this time, and efforts were made to accommodate all their bereavement needs.
Vendor/Technical Support
Another challenge facing both research and clinical operations is a potential disruption in technical support of lab equipment in times of emergencies. In April, MSKCC implemented restricted access and screening measures in order to protect both patients and employees form viral infection, which resulted in a strict no visitor policy. As a result, onsite vendor technical support was disrupted; though remote technical support was able to continue uninterrupted with all our vendor partners. Two of our high throughput Leica Aperio AT2 scanners that were out of order on the first week of April were only able to get services and operational on May 1, following a technical visit from a vendor. The scan team operations shifted to use available capacity on the other scanners during this time.
Validation and Approval of Laboratory Developed Test
The potential use of digital pathology was identified as a priority early on in the lockdown recognizing that the COVID-19 situation is an opportunity to reassess our department’s workflows and improve operations with available digital technologies.
Initial discussions focused on developing support for remote signout, and with the previous investment of digital pathology solutions that were already implemented, 9,10 this validation was performed in an expeditious fashion. The system was validated according to the way it would be clinically utilized. This validation was set up after all coordination of stakeholders, security measures, and technical considerations were reviewed. During March and April, the department achieved a validation of the digital pathology system and operational workflow for remote primary diagnosis, including digitization of glass slides generated from formalin fixed paraffin embedded and frozen tissue; including hematoxylin & eosin stains, immunohistochemical stains, and special stains 11. Twelve pathologists participated in a digital pathology validation from remote sites, covering all surgical pathology subspecialties. In total, 108 patient cases, comprising 254 part diagnoses, and 1196 slides were reported using whole slide images with monitor display and with brightfield microscopy. Digital diagnoses were performed from a remote site using virtual private networks and 2-factor authentication for security, and optical diagnoses were performed at the hospital in the pathologists’ respective offices. There was an overall 98.8% concordance with 100% major diagnostic concordance. 11 Other operational metrics were also recorded to further understand rescan rates as well as tissue types that may be more prone to require rescanning. These data were included as part of developing a standard operating procedure for laboratory and scanning workflows.
The validation documentation and supportive testing of scanners were submitted to the New York State Department of Health as the Clinical Laboratory Improvement Amendments (CLIA)-deemed entity for all laboratories in New York State (NYS) on April 22, 2020. The provisional approval by NYS Department of Health (DOH) was received less than 2 weeks afterward allowing pathologists to use this technology for their own protection, as well as to support continuous care for patients seeking care at our institution. Remote signout capabilities have also allowed pathologists with family care needs that were increasingly disrupted during the pandemic flexibility in supporting work–life balance.
Though the digital pathology system was validated for remote use, our current prospective digital scanning volume is still limited by current laboratory staffing and instrumentation. As of October 2020, remote signout accounts are estimated to be about 10% of the cases in our department (data not shown). Digital and remote signouts became increasingly used for biopsy review, however due to throughput constraints, the laboratory is not able to scan all generated glass slides at this time.
Discussion
The 2020 COVID-19 pandemic resulted in many challenges to health care and pathology. At MSKCC, hospital operations had to undergo adaptations that would allow to address safety concerns without affecting patient care. During the initial months of the 2020 COVID-19 pandemic, processes had to be in place to answer the continuum of hospital operations. Protecting and maintaining staff health and morale were a top priority for managers and administrators at MSKCC throughout this period. Working conditions were monitored as increasing scientific data became available regarding the severity of the airborne infection, and a major team effort approach was required to solve critical questions related to the COVID-19 response. 5
Digital pathology workflows allow faculty workspace flexibility and is an attractive solution for maintaining pathology operations during emergencies. However, as previously described for clinical pathology 12 and cytopathology, 13 pathology laboratory and digital pathology workflows require on-site presence of staff for most of the steps involved (Figure 1) and planning and precautions have to be taken to ensure operations in situations that required minimized onsite staffing. The need to maintain operations in emergencies, motivated us to develop a novel workflow during this period. 11 The digital scan team was involved early on with the conceptualization, development, and validation of the prospective scanning remote signout workflow.
Maintaining safe distancing was a challenge given the nature of the scanning operations, the proximity of the slide prepping stations, and the scanning instrumentation. Slide prepping as well as computer workstations were evaluated and spaced apart while maintaining the scanners in their fixed locations. Staggered work schedules were offered to decrease crowding in work areas and decrease potential exposure. One solution that was offered to employees was flexible work schedules with longer shifts to allow for social distancing and to minimize the frequency of public transportation needs. The scheduling of staggered employee shifts was also introduced to minimize potential cross-exposure between a fewer number of staff members.
The flexibility to implement changes in the schedules of the digital pathology scan team members allowed the use of scanner resources without compromising employee safety because of overcrowding. This also allowed employees to adjust their schedules based on their unique family needs without a change in productivity. There was some resistance from a few employees to come to work, and those employees chose to use their vacation and sick days at the early days of the lockdown. An effort was made to accommodate specific requests for remote work whenever possible.
When NYC went into a state of emergency on March 7, changes were made to public transportation routes and schedules that made the commute of our staff a challenge. Most of the team’s employees rely on public transportation and had to modify their routes which resulted in added longer overall commute for most. Coverage of personal car or car service expenses for some employees were offered during the early part of the pandemic to help employees who experienced this hardship.
Additional benefits were offered through the hospital and included financial assistance through a hospital grant program, temporary lodging for workforce fearing infection of family members, some complimentary food and additional lounge space, and assistance with childcare options for the employees who had to come to work onsite. The financial impact to the department during the shutdown included unanticipated expenses for securing remote work solutions, travel expense reimbursement, overtime payments for staff, structural changes to work areas, accommodating COVID testing for employees while encountering lower specimen, and overall revenue and distribution of PPE. All these MSKCC sponsored assistance resulted in a higher cost of maintaining operations but helped to alleviate staff health concerns and maintained high morale among the staff members.
Browning et al (2020) reported the response of pathology services to the pandemic in the United Kingdom and makes the argument for DP and artificial intelligence playing a key role in resilience for both academic pathology and diagnostic pathology services and how these should form an essential component of future planning. 14 Stathonikos et al described the virtues of digital pathology as their lab in Utrecht adapted to pathology operations during the pandemic. 15 Liscia et al described the continuum of pathology operations with limited staffing using a digital pathology system at Biella hospital in hard hit Northern Italy 16
Investment in digital pathology and the development of a remote signout workflows has the benefits that could help guarantee pathology’s clinical operations in years to come without the challenges of natural or man-made emergencies that would limit pathologists’ availability to practice at the hospital. This along will other benefits of digital pathology 16 -18 make the investment in digital pathology attractive to institutions who have not fully committed to doing so. Reports of using digital pathology has shown overall efficiency gains as well as cost savings. 10,19 -22 There is a clear benefit for use of digital pathology as a means for supporting remote clinical workflows. Processes must be put in place to guarantee the safety and well-being of staff that is involved with the preanalytic and postanalytic phases of pathology operations not only during public health emergencies but for routine daily clinical utility.
Conclusion
The aftermath of COVID-19 has ushered novel operational workflows in hospitals globally. Pathology departments with investments in digital pathology were able to quickly pivot toward delivering safe remote clinical service for pathologists to enable continuous patient care. Implementing and sustaining such efforts requires careful planning and execution, as the laboratory and digital scanning operations require on-site skilled staff presence to perform their clinical roles in the laboratory. The experience at our institution validated the investment in digital pathology and deep engagement of staff toward establishing best practice workflows. The SARS-CoV-2 public health emergency allowed for digital workflows to support patient care during this critical time but will be used as a blueprint to offer novel care delivery models for patients in the future.
Acknowledgments
Research reported in this publication was supported in part by the Warren Alpert Foundation.
Authors’ Note: There are no relevant financial conflicts of interest to the material presented in this manuscript. However in relation to digital pathology: DSK and MGH are consultants to PaigeAI. PJS is a co-founder and equity holder of Paige.AI.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The article processing fee for this article was funded by an Open Access Award given by the Society of ‘67, which supports the mission of the Association of Pathology Chairs to produce the next generation of outstanding investigators and educational scholars in the field of pathology. This award helps to promote the publication of high-quality original scholarship in Academic Pathology by authors at an early stage of academic development.
ORCID iDs: Peter Schueffler  https://orcid.org/0000-0002-1353-8921
https://orcid.org/0000-0002-1353-8921
Matthew G. Hanna  https://orcid.org/0000-0002-7536-1746
https://orcid.org/0000-0002-7536-1746
References
- 1. Hijano DR, Maron G, Hayden RT. Respiratory viral infections in patients with cancer or undergoing hematopoietic cell transplant. Front Microbiol. 2018;9:3097. doi:10.3389/fmicb.2018.03097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Madhusoodhan PP, Pierro J, Musante J, et al. Characterization of COVID-19 disease in pediatric oncology patients: the New York-New Jersey regional experience. Pediatr Blood Cancer. 2021;68:e28843. doi:10.1002/pbc.28843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Robilotti EV, Babady NE, Mead PA, et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020;26:1218–1223. doi:10.1038/s41591-020-0979-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aslam A, Singh J, Robilotti E, et al. SARS CoV-2 surveillance and exposure in the perioperative setting with universal testing and personal protective equipment (PPE) Policies [Published online October 22, 2020]. Clin Infect Dis. 2020:ciaa1607. doi:10.1093/cid/ciaa1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levine RL. Cancer did not stay home for COVID-19. Sci Adv. 2020;6:eabd7487. doi:10.1126/sciadv.abd7487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sinard JH. An analysis of the effect of the COVID-19 pandemic on case volumes in an academic subspecialty-based anatomic pathology practice. Acad Pathol. 2020;7. doi:10.1177/2374289520959788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rusch VW, Wexner SD; American College of Surgeons COVID-19 communications Committee Board of Regents, and officers. The American College of Surgeons responds to COVID-19. J Am Coll Surg. 2020;231:490–496. doi:10.1016/j.jamcollsurg.2020.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Laboratory biosafety guidance related to coronavirus disease (COVID-19). 2020, Accessed December 23, 2020. https://www.who.int/publications/i/item/WHO-WPE-GIH-2021.1
- 9. Hanna MG, Reuter VE, Hameed MR, et al. Whole slide imaging equivalency and efficiency study: experience at a large academic center. Mod Pathol Off J U S Can Acad Pathol Inc. 2019;32:916–928. doi:10.1038/s41379-019-0205-0 [DOI] [PubMed] [Google Scholar]
- 10. Hanna MG, Reuter VE, Samboy J, et al. Implementation of digital pathology offers clinical and operational increase in efficiency and cost savings. Arch Pathol Lab Med. 2019;143:1545–1555. doi:10.5858/arpa.2018-0514-OA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hanna MG, Reuter VE, Ardon O, et al. Validation of a digital pathology system including remote review during the COVID-19 pandemic. Mod Pathol Off J U S Can Acad Pathol Inc. 2020;33:2115–2127. doi:10.1038/s41379-020-0601-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jackson BR, Genzen JR. The lab must go on. Am J Clin Pathol. 2021;155:4–11. doi:10.1093/ajcp/aqaa187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vigliar E, Cepurnaite R, Alcaraz-Mateos E, et al. Global impact of the COVID-19 pandemic on cytopathology practice: results from an international survey of laboratories in 23 countries. Cancer Cytopathol. 2020;128:885–894. doi:10.1002/cncy.22373 [DOI] [PubMed] [Google Scholar]
- 14. Browning L, Colling R, Rakha E, et al. Digital pathology and artificial intelligence will be key to supporting clinical and academic cellular pathology through COVID-19 and future crises: the Pathlake Consortium perspective [Published online July 3, 2020]. J Clin Pathol. 2020. doi:10.1136/jclinpath-2020-206854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stathonikos N, Varsseveld NC, van Vink A, et al. Digital pathology in the time of corona. J Clin Pathol. 2020;73:706–712. doi:10.1136/jclinpath-2020-206845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liscia DS, Bellis D, Biletta E, D’Andrea M, Croci GA, Dianzani U. Whole-slide imaging allows pathologists to work remotely in regions with severe logistical constraints due to Covid-19 pandemic. J Pathol Inform. 2020;11:20. doi:10.4103/jpi.jpi_32_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hanna MG, Parwani A, Sirintrapun SJ. Whole slide imaging: technology and applications. Adv Anat Pathol. 2020;27:251–259. doi:10.1097/PAP.0000000000000273 [DOI] [PubMed] [Google Scholar]
- 18. Pantanowitz L, Sinard JH, Henricks WH, et al. Validating whole slide imaging for diagnostic purposes in pathology: guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med. 2013;137:1710–1722. doi:10.5858/arpa.2013-0093-CP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baidoshvili A, Bucur A, van Leeuwen J, van der Laak J, Kluin P, van Diest PJ. Evaluating the benefits of digital pathology implementation: time savings in laboratory logistics. Histopathology. 2018;73:784–794. doi:10.1111/his.13691 [DOI] [PubMed] [Google Scholar]
- 20. Chong T, Palma-Diaz MF, Fisher C, et al. The California Telepathology Service: UCLA’s experience in deploying a regional digital pathology subspecialty consultation network. J Pathol Inform. 2019;10:31. doi:10.4103/jpi.jpi_22_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ho J, Ahlers SM, Stratman C, et al. Can digital pathology result in cost savings? A financial projection for digital pathology implementation at a large integrated health care organization. J Pathol Inform. 2014;5:33. doi:10.4103/2153-3539.139714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Evans AJ, Vajpeyi R, Henry M, Chetty R. Establishment of a remote diagnostic histopathology service using whole slide imaging (digital pathology) [Published online July 1, 2020]. J Clin Pathol. 2020. doi:10.1136/jclinpath-2020-206762 [DOI] [PubMed] [Google Scholar]