Abstract
Background:
The best nonsurgical treatment for frozen shoulder is still unclear. Extracorporeal shockwave therapy (ESWT) is an innovative adjunctive treatment for frozen shoulder, but its effect is still unclear.
Purpose:
To evaluate the published literature regarding the potential of ESWT as an adjunctive therapy for frozen shoulder.
Study Design:
Systematic review; Level of evidence, 1.
Methods:
Searches were conducted in the PubMed, EMBASE, Cochrane Library, China National Knowledge Infrastructure (CNKI), and VIP Information databases for relevant studies between inception and November 2020. Included were randomized controlled trials (RCTs) for frozen shoulder that compared ESWT with routine treatments to controls. There were no restrictions on the treatment period, type of ESWT, or severity of symptoms. At least 1 of the following outcome indices was assessed: visual analog scale (VAS) for pain, Constant-Murley score (CMS) for shoulder function assessment, or external rotation range of movement (ER ROM). RevMan 5.3 software was used to evaluate the bias and quality of the included studies. For continuous variables, the mean difference (MD) or standardized MD (SMD) with the 95% CI was extracted. For dichotomous data, event ratios and sample sizes were extracted.
Results:
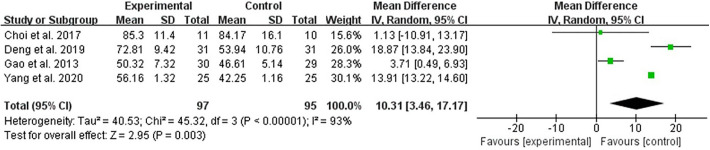
Overall, 20 studies were included. The ESWT used as an adjunct to other interventions had better outcomes compared with control groups regarding immediate and short-term analgesic effects (immediate: MD, –1.10 [95% CI, –1.27 to –0.92], P < .00001; short-term: MD, –0.72 [95% CI, –0.94 to –0.50], P < .00001) as well as immediate function (SMD, 1.54 [95% CI, 1.19 to 1.89], P < .00001], I 2 = 0%). There was significant heterogeneity between studies for long-term analgesia (MD, –0.90 [95% CI, –1.40 to –0.41], P < .00001, I 2 = 89%) and ER ROM (MD, 10.31 [95% CI, 3.46 to 17.17], P < .003, I 2 = 93%).
Conclusion:
ESWT seems to be beneficial to patients with frozen shoulder by alleviating pain and improving function. ESWT could be used as an adjunct therapy to routine treatments, although the quality of the included RCTs was hampered by significant heterogeneity regarding long-term analgesia and joint ROM.
Keywords: extracorporeal shockwave therapy, frozen shoulder, pain, motor function, meta-analysis
Frozen shoulder is a common musculoskeletal disorder characterized by pain, limited joint mobility, and dysfunction, 18 with prevalence rates ranging from <1% to 2%. 19 Frozen shoulder is clinically divided into 3 overlapping phases. The painful freezing phase has a duration of 10 to 36 weeks and is characterized by pain and stiffness around the shoulder, which may worsen at night. The adhesive phase is characterized by restricted range of movement (ROM) with a gradual relief of pain, which occurs at 4 to 12 months. The resolution phase with spontaneous improvement in the ROM takes 12 to 42 months. 7 Frozen shoulder is a self-limited condition, but the recovery may be slow and incomplete, which reduces patients’ activities of daily living and increases their medical burden. 18,26
Because of the uncertainty of the efficacy and risk of surgical treatment, nonsurgical treatments are more likely chosen by patients. 2,17 Among them, intra-articular steroid injection and physical therapy are commonly used nonsurgical treatments and have shown some benefits. 27,40 However, because the 3 stages of frozen shoulder often overlap and the clinical symptoms of patients are complex, adjuvant therapy is often needed throughout the course of treatment. Zhang et al 40 and Dias et al 7 identified that the benefits of steroid injection were specific to the painful freezing phase and not to the adhesive phase of frozen shoulder. Physical therapy provides more obvious benefits in the adhesive phase than in the painful freezing phase. 40
In recent years, extracorporeal shockwave therapy (ESWT) has been increasingly used as an adjunct to other interventions in some randomized controlled trials (RCTs) and has shown satisfactory improvement in multiple aspects. 3,13,30 To date, there is no specialized meta-analysis or systematic review evaluating the effectiveness of ESWT as an adjunctive therapy in treating frozen shoulder. Therefore, the purpose of this study was to perform a meta-analysis to evaluate the effectiveness of ESWT as adjunctive therapy for frozen shoulder. We hypothesized that ESWT would be a positive adjunctive therapy in the treatment of frozen shoulder.
Methods
Search Strategy
A comprehensive search utilizing Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines was performed via PubMed, EMBASE, Cochrane Library, China National Knowledge Infrastructure (CNKI), and VIP Information databases between inception and November 2020. The medical subject headings/keywords were “extracorporeal shockwave therapy,” “frozen shoulder,” “randomized controlled trial,” and “meta-analysis.” Variations of different terms were used to make a systematic search. The complete search strategy used in PubMed is shown in Appendix Table A1. The reference lists of relevant reviews and registered trials were also reviewed to ensure completeness of the search.
Inclusion Criteria
The inclusion criteria were as follows: (1) RCTs; (2) patients who were diagnosed with frozen shoulder and were experiencing pain and restricted joint movement; (3) the experimental groups were treated with ESWT plus routine treatments, the control groups were treated with routine treatments, and the routine treatments were the same in both groups; (4) there were no restrictions on the treatment period, type of ESWT, or severity of symptoms, and the energy intensity was dependent on the tolerance of the patient; (5) the languages were limited to Chinese and English; (6) whether or not to adopt a blinded method was unlimited; and (7) the authors used at least 1 of the following outcome indices: visual analog scale (VAS), Constant-Murley score (CMS), and external rotation ROM (ER ROM).
Exclusion Criteria
The exclusion criteria were as follows: (1) patients experiencing the following comorbidities: rotator cuff disease, fractures, calcifying tendinitis, glenohumeral arthrosis, myofascial pain syndrome, or other diseases that can cause shoulder pain and dysfunction; (2) the original data were not suitable for a meta-analysis, and it was impossible to obtain usable data by contacting the authors; and (3) different types of ESWT were compared with each other.
Data Extraction
Two reviewers (N.Z., J.G.) independently screened the titles and abstracts according to the inclusion and exclusion criteria and thoroughly read the full texts of relevant literature. Studies that met the predefined criteria were included. In the case of a disagreement, a third reviewer (Z.W.) was consulted to assist in the assessment.
Another 2 reviewers (R.L., Y.H.) independently extracted the following data: first author, publication year, sample size, intervention details, follow-up (where available), measurement time, and outcome indices.
Pain intensity was assessed via the VAS (the lower the score, the better the effectiveness). Shoulder function was assessed via CMS (the higher the score, the better the function). The joint ROM was assessed via ER ROM (the higher the degree, the better the curative effect).
The period of assessment was artificially defined as follows: immediate, short-term (<3 months), and long-term (≥3 months). The results at multiple follow-up times from the same study were included in the subgroup analyses by time point. When 2 studies used the same group of participants, the 2 studies were included only when different outcome measures were used.
Bias Assessment and Quality Classification
We evaluated the quality of the included studies using the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials, 11 using RevMan version 5.3 (Nordic Cochrane Centre, The Cochrane Collaboration).
Statistical Processing and Assessment of Heterogeneity
For continuous variables, the mean difference (MD) or standardized MD (SMD) with the 95% CI was extracted. For dichotomous data, event ratios and sample sizes were extracted. Throughout the analyses, a 2-sided test was used, and P values ≤.05 were considered to be statistically significant.
Heterogeneity was evaluated by using the I 2 statistic and the Cochran Q statistic with P values. 26 The data were pooled using the random-effects model if significant heterogeneity was present (I 2 > 50% or PQ < .1); otherwise, a fixed-effects model was used. In the case of significant heterogeneity, subgroup analyses were further conducted to investigate the potential source of heterogeneity on the treatment effect size. 11 The statistical software used was RevMan 5.3 software. A descriptive analysis was performed if data could not be combined.
Results
Study Selection
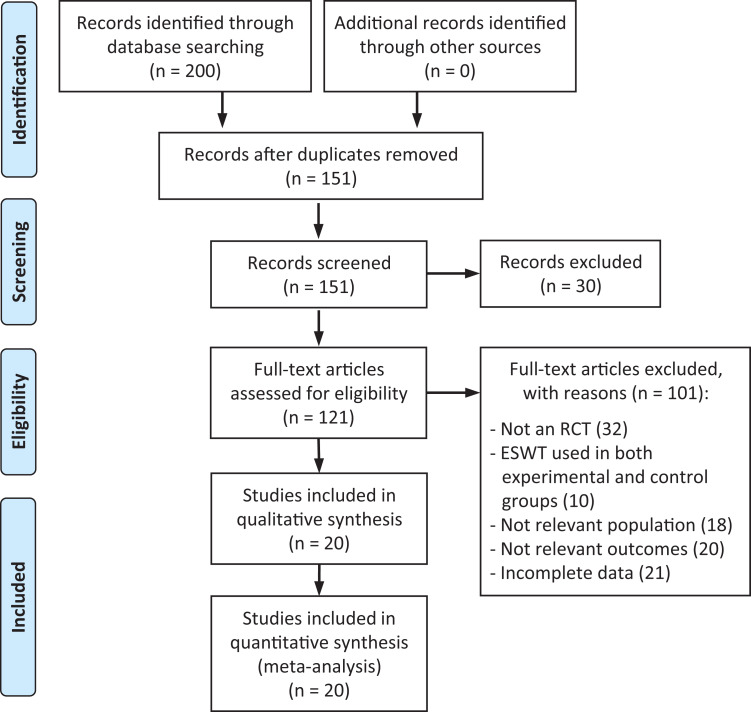
Initially, 200 records were identified via the electronic database search. Of these, we evaluated 121 full texts for eligibility. Ultimately, 20 RCTs § were included in this review. The flow diagram of the selection process is shown in Figure 1.
Figure 1.
Study flow diagram. ESWT, extracorporeal shockwave therapy; RCT, randomized controlled trial.
Study Characteristics
The characteristics of the included studies are listed in Appendix Table A2. Patients in the adhesive phase were identified in 18 studies, ∥ and patients in the remaining 2 studies 8,34 were in the overlap of the painful freezing phase and adhesive phase. Two 1,8 of the included studies were 3-arm studies, and appropriate data were selected for the statistical analysis based on the inclusion and exclusion criteria.
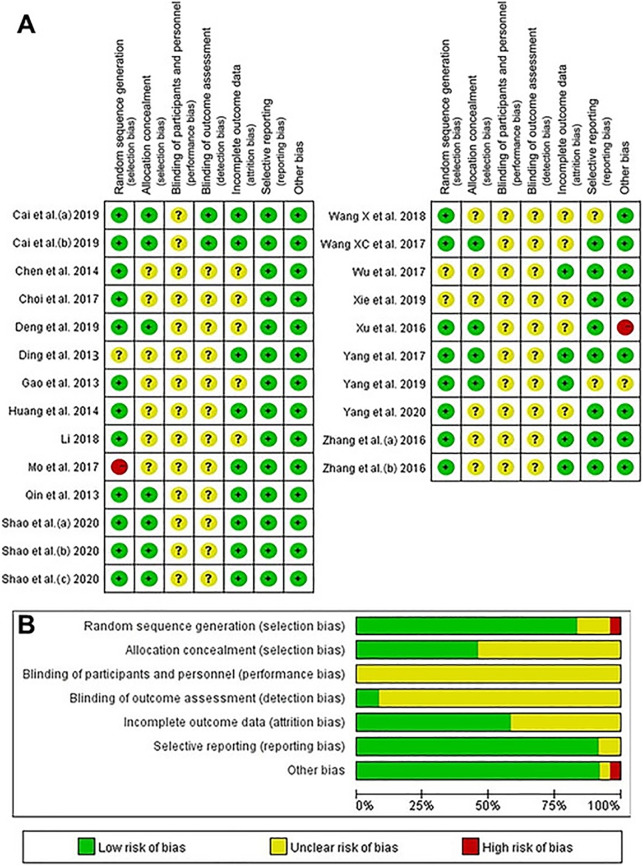
Methodological Quality and the Risk of Bias Within Studies
The risk of bias graph and the risk of bias summary are shown in Figure 2. Of the included studies, 18 ¶ utilized a suitable method to minimize bias and were considered to have a low risk of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases. One 24 of the included studies had a high risk of bias in the randomization scheme, and one 36 of the included studies had a high risk of other biases.
Figure 2.
Risk of bias (A) table and (B) summary. a, sodium hyaluronate + triamcinolone acetonide. Within the figure the three time points were marked as a, b and c, and relate to before treatment, immediately after treatment and 3 months after treatment.
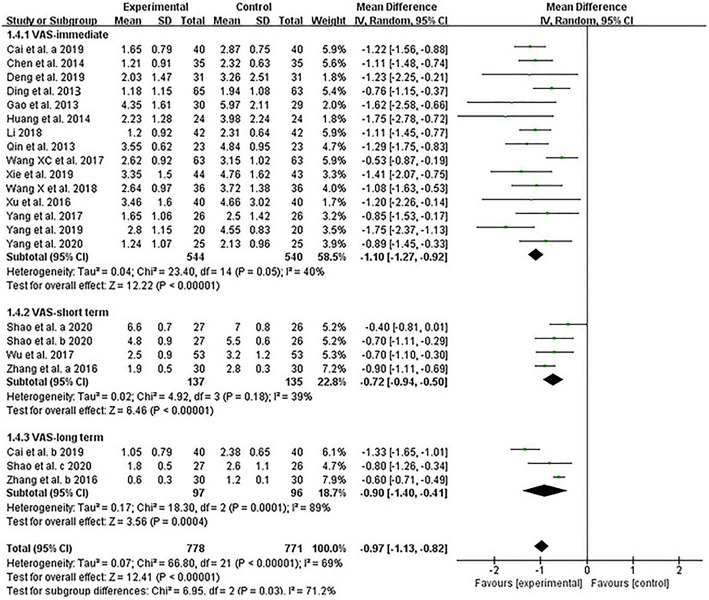
Pain Intensity
Overall, 18 studies # assessed the postintervention effectiveness of ESWT plus routine treatments compared with routine treatments in terms of alleviating pain intensity (MD, –0.97 [95% CI, –1.13 to –0.82], P < .00001, I 2 = 69%). A subgroup analysis was performed based on the assessment time. Compared with routine treatments, both immediate efficacy and short-term efficacy were better. The results were significant and had low heterogeneity (immediate: MD, –1.10 [95% CI, –1.27 to –0.92], P < .00001, I 2 = 40%; short-term: MD, –0.72 [95% CI, –0.94 to –0.50], P < .00001, I 2 = 39%). However, in terms of long-term efficacy, although ESWT plus routine treatments was favored in terms of pain intensity compared with routine treatments, obvious heterogeneity was found, so reliable conclusions could not be drawn (MD, –0.90 [95% CI, –1.40 to –0.41], P < .00001, I 2 = 89%) (Figure 3).
Figure 3.
Forest plot of comparison of visual analog scale (VAS) between extracorporeal shockwave therapy plus routine treatments and routine treatments. Within the figure the three time points were marked as a, b and c, and relate to before treatment, immediately after treatment and 3 months after treatment. IV, Inverse Variance.
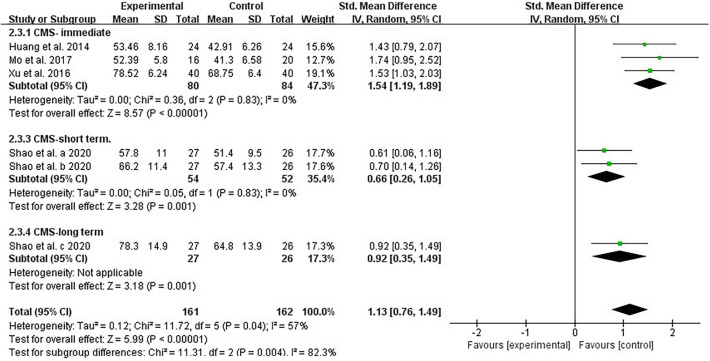
Shoulder Function
Compared with routine treatments, the effectiveness of ESWT plus routine treatments on shoulder function after intervention was assessed in terms of CMS in 4 trials 12,24,29,36 (SMD, 1.13 [95% CI, 0.76-1.49], P < .00001, I 2 = 57%). Strong evidence was detected that ESWT plus routine treatments was more effective for improving shoulder function in terms of immediate efficacy, with no heterogeneity (SMD, 1.54 [95% CI, 1.19–1.89], P < .00001, I 2 = 0%) (Figure 4). However, we could not draw reliable conclusions about short- and long-term efficacy.
Figure 4.
Forest plot of the comparison of Constant-Murley score (CMS) between extracorporeal shockwave therapy plus routine treatments and routine treatments. Within the figure the three time points were marked as a, b and c, and relate to before treatment, immediately after treatment and 3 months after treatment. IV, Inverse Variance; Std, standardized.
Joint Range of Motion
ER ROM was used to reflect the ROM, which was assessed in 4 RCTs. 5,6,9,38 Because of the limited number of studies, ER ROM was measured immediately after treatment in all included studies. The pooled result of the included studies showed that the heterogeneity was high and unacceptable (MD, 10.31 [95% CI, 3.46–17.17], P < .003, I 2 = 93%) (Figure 5).
Figure 5.
Forest plot of the comparison of external rotation range of movement (ER ROM) between extracorporeal shockwave therapy plus routine treatments and routine treatments. IV, Inverse Variance.
Discussion
This is the first meta-analysis comparing the effectiveness of ESWT plus routine treatments and routine treatments in frozen shoulder. We preliminarily found that analgesic effects (immediate and short-term) and function (immediate) were better in the groups where ESWT was used as an adjunct to other interventions (immediate analgesic effects: MD, –1.10 [95% CI, –1.27 to –0.92], P < .00001; short-term analgesic effects: MD, –0.72 [95% CI, –0.94 to –0.50], P < .00001; immediate function: SMD, 1.54 [95% CI, 1.19 to 1.89], P < .00001, I 2 = 0%). However, for the improvement of long-term analgesia (MD, –0.90 [95% CI, –1.40 to –0.41], P < .00001, I 2 = 89%) and external rotation of the shoulder joint (MD, 10.31 [95% CI, 3.46 to 17.17], P < .003, I 2 = 93%), although there was evidence pointing to the effectiveness of ESWT plus routine treatments compared with routine treatments, the data were heterogeneous, and the conclusions were not reliable. In addition, because of the limited number of studies and the fact that data reflecting short-term and long-term improvement in shoulder function relied on the same RCT, 29 we could not prove that ESWT as an adjuvant therapy better promotes the improvement of shoulder function.
The pathophysiology of frozen shoulder remains unclear. Although disagreements exist, cytokine-mediated synovial inflammation with fibroblastic proliferation is the most recognized explanation. 22 Increased expression levels of growth factors, cytokines, and matrix metalloproteinases are found in the patient’s capsular biopsy specimens, suggesting that these substances are involved in the inflammatory and fibrotic cascade of frozen shoulder. 7
ESWT refers to a series of acoustic pulses with a certain energy density transmitted to a specific target area via an appropriate generator, thus achieving therapeutic effect. 28 First, the energy emitted via shockwaves can reach the affected area via body fluid and tissue, improve the distribution of local blood flow, promote the activation of molecular and immunological reactions, stimulate angiogenesis, promote microcirculation, increase cell oxygen carrying, produce anti-inflammatory effects, and alleviate pain. 10,14,15 Second, ESWT can upregulate nitric oxide levels, promote the ingrowth of endothelial nitric oxide synthase activity, and downregulate nuclear factor kappa B expression. 21 Third, shockwave therapy can produce a cavitation effect between tissues, cause intertissue release, promote the separation of adhesion, and release the adhesive tissue. 23 Fourth, this method can change the acceptance frequency of nociceptors to pain, change the composition of chemical mediators around nociceptors, cause changes in free radicals around cells, release substances that inhibit pain, and inhibit the transmission of pain information. 10 Fifth, local high-intensity shockwaves can produce superstimulation to nerve endings, reduce nerve sensitivity, hinder nerve conduction function, and relieve pain. 35 Finally, intensification of tissue regeneration, decrease in tissue apoptosis, and effective recruitment of fibroblasts have been observed in some basic studies. 16
Study Limitations
There are some potential limitations that should be addressed in this study. First, because of the time overlap, the clinical stages of disease were not completely uniform. The vast majority were in the adhesive phase, and a small number were in the overlap of the painful freezing phase and adhesive phase. Second, because of the limited number of studies included, we were not able to perform further subgroup analysis on the results with high heterogeneity, or the studies included in subgroup analysis were insufficient, resulting in incomplete conclusions. Third, the characteristics of each included population were inevitably different, which more or less reduced the reliability and clinical applicability of the results to some extent. Clinical trials should be standardized in the future so that meta-analyses will better elaborate subgroups, including stages of frozen shoulder, main symptoms, comorbidity, and sex.
Conclusion
Although the quality level of the included RCTs was limited, based on this meta-analysis, we can conclude that ESWT seems to be beneficial to patients with frozen shoulder by alleviating pain and improving function. ESWT could be used as an adjunct therapeutic method to routine treatments. Considering methodological imperfections, future multicenter, prospective clinical trials with large sample sizes, placebo control, successful blinding, and effective follow-up are needed.
APPENDIX
Table A1.
Details of the PubMed Search Strategy
| #1 | Search “Frozen shoulder”[MeSH] |
|---|---|
| #2 | Search: (((((((((((((((((((((frozen shoulder[Title/Abstract]) OR (Bursitides[Title/Abstract])) OR (Bursitis[Title/Abstract])) OR (Frozen Shoulders[Title/Abstract])) OR (Shoulder, Frozen[Title/Abstract])) OR (Adhesive Capsulitis of the Shoulder[Title/Abstract])) OR (Shoulder Adhesive Capsulitis[Title/Abstract])) OR (Adhesive Capsulitides, Shoulder[Title/Abstract])) OR (Adhesive Capsulitis, Shoulder[Title/Abstract])) OR (Capsulitides, Shoulder Adhesive[Title/Abstract])) OR (Capsulitis, Shoulder Adhesive[Title/Abstract])) OR (Shoulder Adhesive Capsulitides[Title/Abstract])) OR (Capsulitis[Title/Abstract])) OR (Capsulitides[Title/Abstract])) OR (Pes Anserine Bursitis[Title/Abstract])) OR (Bursitides, Pes Anserine[Title/Abstract])) OR (Bursitis, Pes Anserine[Title/Abstract])) OR (Pes Anserine Bursitides[Title/Abstract])) OR (Adhesive Capsulitis[Title/Abstract])) OR (Adhesive Capsulitides[Title/Abstract])) OR (Capsulitides, Adhesive[Title/Abstract])) OR (Capsulitis, Adhesive[Title/Abstract]) |
| #3 | Search “Extracorporeal Shockwave Therapy”[MeSH] |
| #4 | Search: ((((((((((((((Extracorporeal Shockwave Therapies[Title/Abstract]) OR (Shockwave Therapies, Extracorporeal[Title/Abstract])) OR (Shockwave Therapy, Extracorporeal[Title/Abstract])) OR (Therapy, Extracorporeal Shockwave[Title/Abstract])) OR (Shock Wave Therapy[Title/Abstract])) OR (Shock Wave Therapies[Title/Abstract])) OR (Therapy, Shock Wave[Title/Abstract])) OR (Extracorporeal Shock Wave Therapy[Title/Abstract])) OR (Extracorporeal High-Intensity Focused Ultrasound Therapy[Title/Abstract])) OR (Extracorporeal High Intensity Focused Ultrasound Therapy[Title/Abstract])) OR (HIFU Therapy[Title/Abstract])) OR (HIFU Therapies[Title/Abstract])) OR (Therapy, HIFU[Title/Abstract])) OR (High-Intensity Focused Ultrasound Therapy[Title/Abstract])) OR (High Intensity Focused Ultrasound Therapy[Title/Abstract]) |
| #5 | Search (randomized controlled trial[Publication Type]OR randomized[Title/Abstract] OR placebo[Title/Abstract]) |
| #6 | #1 OR #2 |
| #7 | #3 OR #4 |
| #8 | #5 AND #6 AND #7 |
Table A2.
Basic Features of the Included Studies a
| Lead Author (Year) | Sample Size (ESWT/Control) | ESWT Group | Control Group | Intervention Time | Follow-up | Measurement Time | Outcomes |
|---|---|---|---|---|---|---|---|
| Cai (2019) 1 | 40/40 | ESWT + pain point injection + intra-articular injection b + manual therapy | Pain point injection + intra-articular injection b + manual therapy | 2 wk | 3 mo | Before treatment and 3 mo after treatment | VAS |
| Chen (2014) 4 | 35/35 | ESWT (1500 shockwaves, 10 Hz, 1.5 bar) + manual therapy | Manual therapy | Once every 6 d for 20 d | NR | Before and after treatment | VAS |
| Choi (2017) 5 | 11/10 | ESWT (800 impulses, 5 Hz, 0.129 mJ/mm2) + kinesio taping | Kinesio taping | Twice a wk for 4 wk | NR | Before and after treatment | ER ROM |
| Deng (2019) 6 | 31/31 | ESWT (2000 waves, 8 Hz, 1.0 bar) + ultra-short-wave therapy + joint loosening | Ultra-short-wave therapy + joint loosening | Once every 6 d for 30 d | NR | Before and after treatment | VAS, ER ROM |
| Ding (2013) 8 | 65/63 | ESWT (2000 shockwaves, 4.5 J) + massage | Massage | 3×/wk (10× total) | NR | Before and after treatment | VAS |
| Gao (2013) 9 | 30/29 | ESWT (600-2000 shocks, 12-15 Hz, 1.6-2.5 bar) + routine rehabilitation therapy | Routine rehabilitation therapy | Once a wk for 3 wk | NR | Before and after treatment | VAS, ER ROM |
| Huang (2014) 12 | 24/24 | ESWT (1000 impulses, 0.18-0.25 mJ/mm2) + routine rehabilitation therapy | Routine rehabilitation therapy | Once a wk for 3 wk | NR | Before and after treatment | VAS, CMS |
| Li (2018) 20 | 42/42 | ESWT (1500 shockwaves, 10 Hz, 5 bar) + manual therapy | Manual therapy | Once every 6 d (2× total) | NR | Before and after treatment | VAS |
| Mo (2017) 24 | 16/20 | ESWT (2500-3500 waves, 10-15 Hz, 1.5-2.8 bar) + warming | Warming acupuncture | Once every 5 d for 25 d | NR | Before and after treatment | CMS |
| Qin (2013) 25 | 23/23 | ESWT (1500-2000 shocks, 6.5-11.0 kV) + routine rehabilitation therapy | Routine rehabilitation therapy | Once every 6-7 d for 1 mo | NR | Before and after treatment | VAS |
| Shao (2020) 29 | 27/26 | ESWT (1200 shocks, 0.25 mJ/mm2) + oral corticosteroid + transcutaneous electrical nerve stimulation | Oral corticosteroid + transcutaneous electrical nerve stimulation | Once a wk for 6 wk | NR | Before treatment and 2, 6, and 12 wk after treatment | VAS, CMS |
| Wang (2017) 32 | 63/63 | ESWT (2000 waves, 0.16 mJ/mm2) + intra-articular injection c + manual therapy | Intra-articular injection c + manual therapy | Once every 2 wk for 8 wk | NR | Before and after treatment | VAS |
| Wang (2018) 31 | 36/36 | ESWT (2000-2500 waves, 1.8-2.6 bar, 8-12 Hz) + acupuncture | Acupuncture | 3×/wk for 2 wk | NR | Before and after treatment | VAS |
| Wu (2017) 33 | 53/53 | ESWT (2000 shocks, 0.16-2 mJ/mm2) + intra-articular injection | Intra-articular injection | Once a wk for 3 wk | 6 wk | Before treatment and 6 wk after treatment | VAS |
| Xie (2019) 34 | 43/44 | ESWT (2000 shockwaves, 8 Hz) + manual therapy | Manual therapy | Once every 5 d for 20 d | NR | Before and after treatment | VAS |
| Xu (2016) 36 | 40/40 | ESWT (1000 shockwaves, 10 Hz, 0.18-0.25 mJ/mm2) + manual therapy | Manual therapy | Once a wk (20 d total) | NR | Before and after treatment | VAS, CMS |
| Yang (2017) 37 | 26/26 | ESWT (1000-1500 shocks, 50-60 Hz) + routine rehabilitation therapy | Routine rehabilitation therapy | Once every 5 d (3× total) | NR | Before and after treatment | VAS |
| Yang (2020) 38 | 25/25 | ESWT (1500-2000 shockwaves, 2.5-3.5 bar, 6 Hz) + massage | Massage | Once every 5-7 d (2-3× total | NR | Before and after treatment | VAS, ER ROM |
| Yang (2019) 39 | 20/20 | ESWT (2000 waves, 1.5 bar, 5 Hz) + traditional Chinese medicine (fumigation) | Traditional Chinese medicine fumigation | Once every 6 d for 4 wk | NR | Before and after treatment | VAS |
| Zhang (2016) 41 | 30/30 | ESWT (200-300 waves, 2.5 bar) + pain point injection | Pain point injection | For 4 wk | 6 mo | Before treatment and 1 and 6 mo after treatment | VAS |
a CMS, Constant-Murley shoulder function assessment score; ER ROM, external rotation range of movement; ESWT, extracorporeal shockwave therapy; NR, not reported; VAS, visual analog scale.
b Compound betamethasone injection + mecobalamin + lidocaine + normal saline.
c Sodium hyaluronate + triamcinolone acetonide.
Footnotes
Final revision submitted August 3, 2021; accepted September 3, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by funds from the National Natural Science Foundation of China (NSFC No. 81674066); the Natural Science Foundation of Chongqing Province (No. cstc2017jcyjAX0397); the TCM Foundation of Chongqing Health Committee of China (No. zy201602119); and the Science Foundation, Yongchuan Hospital of Chongqing Medical University (No. YJYJ201603). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Cai ZZ, Lin SZ, Huang ZX. Application of extracorporeal shock wave combined with joint cavity and pain point block in the treatment of severe shoulder periarthritis. Article in Chinese. Contemp Med. 2019;25(24):81–84. [Google Scholar]
- 2. Chaudhury S, Gwilym SE, Moser J, Carr AJ. Surgical options for patients with shoulder pain. Nat Rev Rheumatol. 2010;6:217–226. [DOI] [PubMed] [Google Scholar]
- 3. Chen CY, Hu CC, Weng PW, et al. Extracorporeal shockwave therapy improves short-term functional outcomes of shoulder adhesive capsulitis. J Shoulder Elbow Surg. 2014;23:1843–1851. [DOI] [PubMed] [Google Scholar]
- 4. Chen Y, Peng X, Tang ZW, Lu M. Therapeutic effects of mobilization combined with extracorporeal shock wave treatment on patients with scapulohumeral periarthritis. Article in Chinese. Chin J Rehabil. 2014;3:192–194. [Google Scholar]
- 5. Choi JH, Kim SH, An HJ, Koo JP, Kim NJ. Effects of 6 week kinesiotaping and extracorporeal shock wave therapy on the joint range of motion in patients with frozen shoulder. J Int Acad Phys Ther Res. 2017;8(1):1095–1099. [Google Scholar]
- 6. Deng XZ, Yuan HX. Therapeutic effect of joint mobilization and ultrashort wave combined with extracorporeal shock wave on periarthritis of shoulder. Article in Chinese. Med Inf. 2019;32(11):108–110. [Google Scholar]
- 7. Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005;331(7530):1453–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ding HT, Tang XZ, Jia YF, Chen J. Clinical observation of shock wave combined with massage on periarthritis of shoulder. Article in Chinese. Chin J Rehabil Med. 2013;28(5):468–470. [Google Scholar]
- 9. Gao K, Zhu XC, Yue LH, Feng J, Shen K. Extracorporeal shock wave combined with functional training for the treatment of frozen shoulder. Article in Chinese. China J Orthop Trauma. 2013;26(5):401–403. [PubMed] [Google Scholar]
- 10. Han NH, Liu MY, Chu HZ, et al. Meta-analysis of the clinical effect of extracorporeal shock wave therapy in the treatment of scapulohumeral periarthritis. Article in Chinese. Int J Lab Med. 2020;41(12):1412–1417. [Google Scholar]
- 11. Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huang J, Peng Y, Tang R. Clinical observation of extracorporeal shock wave combined with joint loosening in the treatment of periarthritis of shoulder. Article in Chinese. J Mil Surg Southwest China. 2014;16(6):635–636. [Google Scholar]
- 13. Hussein AZ, Donatelli RA. The efficacy of radial extracorporeal shockwave therapy in shoulder adhesive capsulitis: a prospective, randomised, double-blind, placebo-controlled, clinical study. Eur J Physiother. 2016;18:63–76. [Google Scholar]
- 14. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network metaanalyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. [DOI] [PubMed] [Google Scholar]
- 15. Jain TK, Sharma NK. The effectiveness of physiotherapeutic interventions in treatment of frozen shoulder/adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. 2014;27:247273. [DOI] [PubMed] [Google Scholar]
- 16. Kabbabe B, Ramkumar S, Richardson M. Cytogenetic analysis of the pathology of frozen shoulder. Int J Shoulder Surg. 2010;4:75–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kwaees TA, Charalambous CP. Surgical and non-surgical treatment of frozen shoulder: survey on surgeons treatment preferences. Muscles Ligaments Tendons J. 2014;4:420–424. [PMC free article] [PubMed] [Google Scholar]
- 18. Laslett LL, Burnet SP, Jones JA, Redmond CL, McNeil JD. Musculoskeletal morbidity: the growing burden of shoulder pain and disability and poor quality of life in diabetic outpatients. Clin Exp Rheumatol. 2007;25:422–429. [PubMed] [Google Scholar]
- 19. Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow. 2017;9(2):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li SC. Clinical observation of joint loosening combined with extracorporeal shock wave in the treatment of periarthritis of shoulder. Article in Chinese. Gen J Stomatol. 2018;5(32):179–180. [Google Scholar]
- 21. Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: molecular mechanism that triggers anti-inflammatory action. Curr Med Chem. 2009;16:2366–2372. [DOI] [PubMed] [Google Scholar]
- 22. Mezian K, Coffey R, Chang KV. Frozen shoulder. In: StatPearls[Internet]. StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 23. Min L, Xiao Y, Tang RL, et al. Advances in clinical research on the treatment of periarthritis of shoulder by extracorporeal shock wave. Article in Chinese. World Latest Med Inf. 2017;7(14):87–88. [Google Scholar]
- 24. Mo XX, Zheng RX, Ouyang ZL, Wu RK. Clinical observation of warming acupuncture combined with extracorporeal shock wave in treating periarthritis of shoulder. Article in Chinese. Inner Mongolia Tradit Chin Med. 2017;36(Z1):184–185. [Google Scholar]
- 25. Qin XD, Cao XC, Fu Q, Gao CH. Effect of exogenous shock wave combined with Maitland manipulation on periarthritis of shoulder. Article in Chinese. Chin J Phys Med Rehabil. 2013;7:571–572. [Google Scholar]
- 26. Rangan A, Brealey SD, Keding A, et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicentre, pragmatic, three-arm, superiority randomised clinical trial. Lancet. 2020;396(10256):977–989. [DOI] [PubMed] [Google Scholar]
- 27. Rangan A, Hanchard N, McDaid C. What is the most effective treatment for frozen shoulder? BMJ. 2016;354:i4162. [DOI] [PubMed] [Google Scholar]
- 28. Reilly JM, Bluman E, Tenforde AS. Effect of shockwave treatment for management of upper and lower extremity musculoskeletal conditions: a narrative review. PM R. 2018;10(12):1385–1403. [DOI] [PubMed] [Google Scholar]
- 29. Shao JC, Sun YN, Li J, Zhu HQ, Wang SK, Li JY. The clinical efficiency and safety of extracorporeal shock wave therapy in treatment of diabetes mellitus complicated by periarthritis of shoulder. Article in Chinese. Hebei Med J. 2020;42(8):1192–1195. [Google Scholar]
- 30. Vahdatpour B, Taheri P, Zade AZ, Moradian S. Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J Prev Med. 2014;5:875–881. [PMC free article] [PubMed] [Google Scholar]
- 31. Wang X. Observation on therapeutic effect of acupuncture with extracorporeal shock wave on peripheral-shoulder. Article in Chinese. World Latest Med Inf. 2018;18(76):155–156. [Google Scholar]
- 32. Wang XC, Hao LS, Chen J. Clinical study on divergent type extracorporeal shock wave therapy combined with intra-articular injection and functional exercises in the treatment of periarthritis humeroscapularis. Article in Chinese. Trad Chin Orthop Trauma. 2017;29(8):36–38. [Google Scholar]
- 33. Wu DW, Huang XB, Lyu LM, Tang SS. A clinical research on radial extracorporeal shock wave combined with intra-articular injection for treatment of frozen shoulder. Article in Chinese. Anhui Med Pharm J. 2017;21(12):2274–2277. [Google Scholar]
- 34. Xie G, Yao HY, Wang L, Ouyang PF, Yaxi LV. Effect of joint mobilization combined with extracorporeal shock wave on scapulohumeral periarthritis. Article in Chinese. Med Innov China. 2019;16(26):28–31. [Google Scholar]
- 35. Xing GY, Zhang PG, Shi Z, et al. Extracorporeal shock wave therapy combined with arthroscopy for the treatment of osteochondral lesions of the talus. Orthop J China. 2011;19(12):978–981. [Google Scholar]
- 36. Xu L, Li XP, Gao MX. Effect of extracorporeal shock wave and manipulation treatment in scapulohumeral periarthritis. Article in Chinese. J Clin Exp Med. 2016;15(16):1574–1577. [Google Scholar]
- 37. Yang J, Liao ZB, Zhou RJ, Zhou GH. Effect of extracorporeal shock wave on pain of periarthritis of shoulder. Article in Chinese. Chin Foreign Med Res. 2017;2:22–23. [Google Scholar]
- 38. Yang QX, Tan YS. Treatment of scapulohumeral periarthritis with massage combined with extracorporeal shock wave. Article in Chinese. Chin Manip Rehabil Med. 2020;7:36–38. [Google Scholar]
- 39. Yang Y, Huang GC, Dong M. Observation on extracorporeal shock wave therapy and traditional Chinese medicine fumigation in the treatment of frozen shoulder. Article in Chinese. Mod Med Health. 2019;35(14):2123–2125. [Google Scholar]
- 40. Zhang J, Zhong S, Tan T, et al. Comparative efficacy and patient-specific moderating factors of nonsurgical treatment strategies for frozen shoulder: an updated systematic review and network meta-analysis. Am J Sports Med. 2021;49(6):1669–1679. [DOI] [PubMed] [Google Scholar]
- 41. Zhang TH, Yan RX, Sun TS, Tian YD, Zhou SH. Clinical observation of pain point injection combined with shock wave in treating periarthritis of shoulder. Article in Chinese. Chin J Ctrl Endem Dis. 2016;31(11):1248–1249. [Google Scholar]