History
A boy aged 16 years suffered a close-range shotgun wound to the left groin. A pressure dressing applied in the field by the emergency medical services was saturated with blood when the patient arrived at the trauma center.
Examination
The patient was agitated and uncooperative. His blood pressure was 80/50 mm Hg, heart rate was 140 beats/min, and respiratory rate was 20 breaths/min with audible breath sounds bilaterally. While the patient was being intubated and intravenous catheters were being inserted, an arterial blood gas was drawn and an X-ray of the left groin was performed (figure 1). The results of the arterial blood gas were a pH of 6.89 and a base deficit of −24.8. The pressure dressing over the left groin was reinforced, and the patient was moved to the operating room. He was noted to be moving his left ankle and toes.
Figure 1.
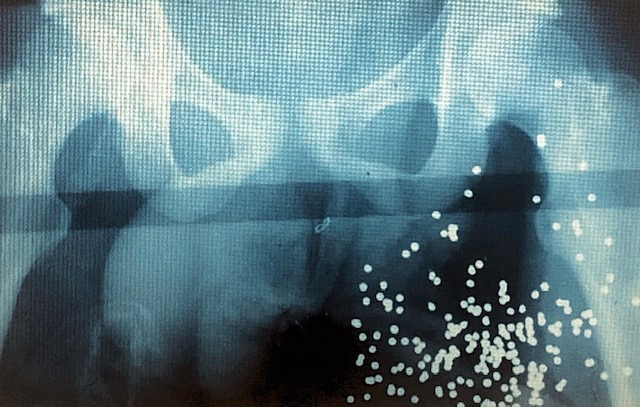
X-ray of close-range shotgun wound of left groin.
First operation
Once the pressure dressing was removed, extensive damage to the soft tissues of the left groin was noted. After a longitudinal incision was made through this area, a quick inspection documented multiple perforations of the common femoral artery (CFA), superficial femoral artery (SFA), and common femoral vein (CFV) with profuse arterial and venous hemorrhage.
Question
After proximal clamp control of the left CFA was attained, your choice for management would be
saphenous vein graft replacement of CFA/SFA, ligation CFV;
intraluminal shunts to CFA/SFA and CFV;
intraluminal shunt to CFA/SFA, ligation CFV;
polytetrafluoroethylene (PTFE) graft replacement of CFA/SFA, ligation CFV.
First operation continued
The injured segment of the left CFA/SFA was resected with sacrifice of the left profunda femoris artery, and a Pruitt-Inahara shunt (Lemaitre Vascular, Burlington, Massachusetts, USA) was inserted to restore arterial inflow to the lower extremity (figure 2). After the left CFV was ligated, the skin edges of the incision and defect in soft tissue in the left groin were reapproximated with towel clips (figure 3). The final step at the first operation was a left below knee two-skin incision four-compartment fasciotomy.
Figure 2.
Pruitt-Inahara intra-arterial shunt connecting left common femoral and superficial femoral arteries in groin wound.
Figure 3.

Towel clip closure to cover open left groin wound and shunt except T-piece.
Second operation
The patient’s metabolic acidosis corrected over 8 hours, and he was returned to the operating room the following day. First, a 6 mm PTFE graft was tunneled medial to the open wound in the left groin. Unfractionated heparin (6000 units) was administered intravenously, vascular clamps were applied to the left CFA and SFA around the shunt, and the shunt was removed. Fogarty balloon catheters were then passed proximally and distally through the left femoropopliteal arterial system, but no thrombus was retrieved. The end of the left CFA was then sewn to the proximal end of the extra-anatomic 6 mm PTFE graft using 6–0 polypropylene suture. After flushing the graft through the open distal end, the blood in the graft was evacuated and the graft was filled with heparinized saline before applying a distal vascular clamp. The end of the PTFE graft was then sewn to the end of the left SFA in an end-to-end fashion using 6–0 polypropylene suture. Appropriate flushing was performed before tying down the last knot on the distal anastomosis. Both left pedal pulses were palpable after the vascular clamp on the distal graft was removed.
Finally, the skin was closed over the two artery-PTFE graft anastomoses to ensure a complete extra-anatomic track.
Third operation
The patient was returned to the operating room on the following day for debridement and open packing of the incision/defect in soft tissue of the left groin.
Fourth operation
The Plastic Surgery Service had been consulted to help with muscle flap coverage of the defect in soft tissue in the left groin. While they were mobilizing a muscle flap in the distal left thigh, the distal SFA beyond the medial extra-anatomic 6 mm PTFE graft was transected inadvertently. This necessitated resecting the prior distal PTFE graft-SFA anastomosis, adding a PTFE graft extension to the end of the original graft, and sewing this extension in an end-to-side fashion to the proximal left popliteal artery.
Fifth through twelfth operations
Eight further operations were performed for debridement of the open wound in the left groin and for the application of split-thickness skin grafts to the open fasciotomy sites on the medial and lateral left leg.
Discharge
The patient was discharged on the 39th postinjury day with a longitudinal granulating open wound in the left groin and mid-anterior proximal left thigh (figure 4). There was 2+ edema of the left lower extremity, and both left pedal pulses were still palpable.
Figure 4.

Granulating open left groin wound at time of discharge on 39th postinjury day.
He was instructed to wear a fitted compressive stocking on the entire left lower extremity, cease smoking, and ingest aspirin 81 mg every 12 hours until re-evaluation in 3 months.
Discussion
Interest in the management of civilian shotgun wounds in the USA is now nearly 75 years old. One of the earliest papers describing a classification system of such injuries (type I—penetrating, over 7 yards; type II—perforating, 3–7 yards; type III—massive, under 3 yards) was coauthored by American Association for the Surgery of Trauma Past President Roger T. Sherman (1978–1979) in 1963.1 Subsequent papers in the 1970s, 1980s, and 1990s described the mechanism of injury,2 principles of management,3 and excellent results when peripheral vascular injuries resulted from a shotgun wound.4 5
In the modern case presented, the trauma team faced the classical dilemma in patients with near-exsanguination from a severe injury to an extremity—namely, salvage of ‘life versus limb’.6 The factors prompting the attempt to save the patient’s left lower extremity despite his precarious hemodynamic status on admission are listed as follows: (1) age of patient; (2) proximal and limited location of injury; (3) easy access to area of hemorrhage; and (4) movement of the left ankle and toes on admission.
The fundamental principles of ‘damage control’ for vascular trauma were all applied in this patient.7 First, bleeding from multiple pellet wounds was controlled by resection of an injured segment of a major artery (CFA/SFA) and ligation of a major vein (CFV). Second, after passage of Fogarty balloon catheters proximally and distally, a temporary intraluminal shunt was inserted to restore arterial inflow into the extremity. Third, with edema of the left lower extremity from ischemia and ligation of the CFV, a ‘prophylactic’ (no compartment pressure measured) two-skin incision four-compartment fasciotomy was performed in the left leg.8 And, fourth, a temporary towel clip closure of the defect in soft tissue/incision in the left groin was performed to cover the intraluminal shunt.
In retrospect, there were several choices for management in this patient which can be criticized. The old Pruitt-Inahara shunt used had the advantages of having inflatable balloons at the ends and a T-piece to allow for postoperative injection of heparin, papaverine, or arteriographic dye. Unfortunately, the outlying diameter was only 9 Fr. In the largest single-center civilian review of temporary intraluminal vascular shunts (91% inserted in peripheral vessels), the most commonly used size was 14 Fr.9 In the modern era, the Pruitt F3 carotid shunt (Lemaitre Vascular) is available in a 10 Fr size resulting in a 10% increase in flow as compared with the original Pruitt-Inahara shunt.
The choice of a small size PTFE graft for the extra-anatomic bypass would be criticized by most vascular trauma surgeons in the current era. The first reason is that PTFE prostheses are known to develop a thick pseudointima over time.10 11 This obviously narrows the luminal diameter so that a 6 mm may become a 4 mm graft over time, thus increasing the risk of thrombosis. In the patient described, a 6 mm rather than an 8 mm graft was chosen presumably to better match the size of the distal open end of the SFA at the second operation. By performing a distal end-to-side anastomosis (graft-to-artery as was done at the fourth operation), a larger PTFE graft could have been inserted at the second operation. This would have been true despite spasm of the left SFA secondary to the presence of a shunt. The third reason is that the patient’s profound shock, significant injury to the soft tissue in the left groin, need for multiple operations, and prolonged stay in the hospital would all contribute to a greater risk of infection in a synthetic conduit as compared with a saphenous vein graft from the contralateral thigh.
As noted above, adherence to the principles of ‘damage control’ for vascular trauma contributed to simultaneous salvage of the patient’s life and limb. The extensive damage to soft tissue in the groin from the shotgun wound and the choice to ligate the injured CFV both contributed to the significant edema of the left lower extremity, the main morbidity of the injury, at discharge.12
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Commissioned; internally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.Sherman RT, Parrish RA. Management of shotgun injuries: a review of 152 cases. J Trauma 1963;3:76–86. 10.1097/00005373-196301000-00007 [DOI] [PubMed] [Google Scholar]
- 2.DeMuth WE Jr.. The mechanism of shotgun wounds. J Trauma 1971;11:219–29. 10.1097/00005373-197103000-00003 [DOI] [PubMed] [Google Scholar]
- 3.Ledgerwood AM. The management of shotgun wounds. Surg Clin North Am 1977;57:111–20. 10.1016/S0039-6109(16)41137-0 [DOI] [PubMed] [Google Scholar]
- 4.Roberts RM, String ST. Arterial injuries in extremity shotgun wounds: requisite factors for successful management. Surgery 1984;96:902–7. [PubMed] [Google Scholar]
- 5.Meyer JP, Lim LT, Schuler JJ, Castronuovo JJ, Buchbinder D, Woelfel GF, Flanigan P. Peripheral vascular trauma from close-range shotgun injuries. Arch Surg 1985;120:1126–31. 10.1001/archsurg.1985.01390340024004 [DOI] [PubMed] [Google Scholar]
- 6.Feliciano DV. Extremity vascular injuries. In: Britt LD, Peitzman AB, Barie PS, Jurkovich GJeds. Acute care surgery. Philadelphia: Lippincott Williams & Wilkins, 2012:426–37. [Google Scholar]
- 7.Shackford SR. Peripheral vessels. In: Feliciano DV, Mattox KL, Moore EE, eds. Trauma. Ninth Edition. New York: McGraw Hill, 2021:919–39. [Google Scholar]
- 8.Moran BJ, Quintana MT, Scalea TM, DuBose J, Feliciano DV. Two Urgency Categories, Same Outcome: No Difference After "Therapeutic" vs. "Prophylactic" Fasciotomy. Am Surg 2021;103. 10.1177/00031348211031860 [DOI] [PubMed] [Google Scholar]
- 9.Subramanian A, Vercruysse G, Dente C, Wyrzykowski A, King E, Feliciano DV. A decade's experience with temporary intravascular shunts at a civilian level I trauma center. J Trauma 2008;65:316–26. 10.1097/TA.0b013e31817e5132 [DOI] [PubMed] [Google Scholar]
- 10.Sottiurai VS, Yao JS, Flinn WR, Batson RC. Intimal hyperplasia and neointima: an ultrastructural analysis of thrombosed grafts in humans. Surgery 1983;93:809–17. [PubMed] [Google Scholar]
- 11.Oblath RW, Buckley FO Jr, Green RM, Schwartz SI, DeWeese JA. Prevention of platelet aggregation and adherence to prosthetic vascular grafts by aspirin and dipyridamole. Surgery 1978;84:37–44. [PubMed] [Google Scholar]
- 12.Kochuba M, Rozycki GF, Feliciano D. Outcome after ligation of major veins for trauma. J Trauma Acute Care Surg 2021;90:e40–9. 10.1097/TA.0000000000003014 [DOI] [PubMed] [Google Scholar]



