Abstract
The coronavirus is naturally mutating over time and producing new variants. Some of them are more contagious and destructive than previous strains. Also, some variants are capable of therapeutic escaping. Earlier SARS-CoV-2 variants proved that some are supercritical, and newly mutated strains are creating new challenges to the global healthcare systems. Here we aimed to evaluate different coronavirus variants and associated challenges for healthcare systems. We searched for information online and on the PubMed, Scopus, and Embase databases. We found the wild-type virus is more sensitive for neutralization and more controllable than newer variants. The Delta and Omicron variants are more highly transmissible than Alpha, Beta, and Gamma variants. Also, few strains are resistant to neutralization. Therefore, there is a chance of reinfection among the vaccinated population. The transmissibility and resistance of the recently identified Omicron variant is still unclear. The Delta variant is the most dangerous among all variants due to its high transmissibility, disease severity, and mortality rate. For poor and developing countries, oxygen supply, medication, vaccination, and device supply are challenging during epidemic waves. Slowing down the transmission, mass vaccination, vaccine redesign, re-compiling action plans, and following safety guidelines can be effective solutions to the new challenges.
Keywords: Coronavirus variants, COVID-19 pandemic, delta variants, public health, healthcare challenge
Background
China experienced a surge in pneumonia cases in December 2019, caused by β-coronavirus. International Committee on Taxonomy of Viruses (ICTV) labeled the virus as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The World Health Organization (WHO) formally designated the viral disease as coronavirus disease-19 (COVID-19) on February 11, 2020. 1 Now the whole world is fighting the deadly COVID-19 as coronavirus has dispersed to almost all over the world. 2 WHO reported more than 349 million confirmed COVID-19 cases and more than 5.5 million related deaths as of January 24, 2022. 3 The coronavirus is continuously changing its character through mutation. Therefore, new variants are sometimes more virulent and transmissible than the previous ones. The severity of symptoms and the performance of vaccines primarily depend on the viral strain involved in the infection. The respiratory distress or pneumonia are common symptoms of all COVID-19 patients. Besides nausea, abdominal pain, vomiting, diarrhea, loss of appetite related to the gastrointestinal tract, and some neurological symptoms we see in most COVID-19 patients. The severity of those symptoms may vary among patients. 4 On the other hand, some infected people can be asymptomatic at the same time. And even for many symptomatic cases, illnesses extent from mild and simple cold-like symptoms to terrible illness and death. 5 On average, it needs 20 to 37 days for virus clearance from the beginning of being infected. 6 How long this virus will exist inside the human body depends on many factors. Also, it varies from person to person. However, a study showed reduced interferon-C production by natural killer cells may favor the long-term existence of coronavirus. 7
Coronavirus Variants
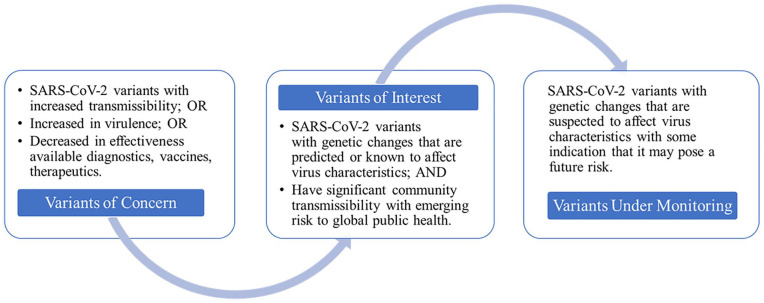
Coronavirus has traveled to every corner of the world and continuously mutates and changes its character. Research shows that the virus responsible for COVID-19 has the most mutations on the targets of various nucleocapsid gene primers and probes. 8 These changes may affect the virus’s properties. The new variants might have a speedy spreading capacity and cause disease severity. Also, new variants might alter the performance of vaccines, diagnostic tools, therapeutic medicines, and other preventive measures. 9 The capacity of changing variants through genomic changes is one of the main characteristics of this virus. In the waves of the COVID-19 pandemic, the world is suffering from Alpha, Beta, Gamma, Delta variants, and most recently Omicron variants of this virus. WHO designated SARS-CoV-2 variants with Greek alphabet letters according to their characteristics and classified them as variants of concern (VOCs) and variants of interest (VOIs) (Figure 1). The WHO defined VOCs and VOIs based on the viral genomic changes, transmissibility, neutralization power, detrimental effects, disease presentation, and emerging health risks on the human being. 10 VOCs are refer to variants with increased transmissibility or increased in virulence or decreased in effectiveness available diagnostics, vaccines, therapeutics. Also, VOIs are refer to those variants with genetic changes that are predicted or known to affect virus characteristics and have significant community transmissibility with emerging risk to global public health. 10 The names are given according to the Greek alphabet that may work as a handy short form for the public, the policymakers, and others. 9 Some recently discovered strains are designated as variants under monitoring for further assessment (Figure 1). This list also includes some former VOIs mutants. The Alpha (B.1.1.7), Beta (B.1.351), Gamma (P.1), Delta (B.1.617.2), and Omicron (B.1.1.529) are classified as VOCs. On the other hand, Lambda (C.37) and Mu (B.1.621) are enlisted as VOIs (Table 1). 11 After Alpha, Beta, Gamma, and Delta variants; Omicron another variant named Delta is the latest concern. However, multiple countries discovered the Omicron variant in Noverber 2021 that is the most infectious variant so far. 11 Till now, this Omicron variant has spread more than 150 countries, and it is spreading faster than others. 12 Moreover, WHO classified some variants as variants under monitoring (VUMs) based on the viral genetic changes that might affect virus characteristics. The Pango lineage of designated SARS-CoV-2 VUMs are B.1.1.318, C.1.2, and B.1.640. 11
Figure 1.
Working definition of SARS-CoV-2 variants. We collected this information from World Health Organization. Tracking SARS-CoV-2 variants. 11
Table 1.
The World Health Organization designated SARS-CoV-2 variants.
| SARS-CoV-2 variants | WHO label | Pango lineage | Earliest documented samples | Date of designation |
|---|---|---|---|---|
| Variants of Concern | Alpha | B.1.1.7 | UK, Sep, 2020 | Dec 18, 2020 |
| Beta | B.1.351 | South Africa, May, 2020 | Dec 18, 2020 | |
| Gamma | P.1 | Brazil, Nov, 2020 | January 11, 2021 | |
| Delta | B.1.617.2 | India, Oct, 2020 | May 11, 2021 | |
| Omicron | B.1.1.529 | Multiple countries, Nov, 2021 | Nov 26, 2021 | |
| Variants of Interest | Lambda | C.37 | Peru, Dec, 2020 | Jun 14, 2021 |
| Mu | B.1.621 | Colombia, Jan, 2021 | Aug 30, 2021 | |
| Variants Under Monitoring | – | B.1.1.318 | Multiple countries, Jan, 2021 | Jun 2, 2021 |
| – | C.1.2 | South Africa, May, 2021 | Sep 1, 2021 | |
| – | B.1.640 | Multiple countries, Sep, 2021 | Nov 22, 2021 |
Source: We obtained data from World Health Organization. Tracking SARS-CoV-2 variants. 11
The Alpha variant
B.1.1.7 variant was renamed as Alpha variant on December 18, 2020. The Alpha variant was found in the earliest documented sample that was found in the United Kingdom in September 2020. It is also noted as lineage B.1.1.7. 13 It is defined by 17 mutations, where 14 mutations are because of the change in amino acids. Three others are deletions of 8 mutations in the spike protein gene that help the virus for viral access to the human cell. Viral functions are potentially affected by at least 3 mutations. 14 Research reported the transmissibility of this variant is 43-90% more than the other variants (early SARS-CoV-2 strains) that were existed in the UK previously. The same transmissibility of this variant has been seen in Switzerland, Denmark, and the United States. 15
The Alpha variant is associated with increased severity of infection regarding hospitalizations and fatality rates, 16 shows no effect on susceptibility when treating with EUA monoclonal antibody,17,18 increased transmission. 19 The most common symptoms in infected people by this variant were chills, loss of appetite, headache and muscle aches, etc. 20 According to a survey, sore throat, fever, myalgia, fatigue, cough, found common symptoms of B.1.1.7 infection. However, loss of smell or taste was reported as a less common symptom; and a higher prevalence of having at least one of the symptoms. 21 Graham et al 22 have studied on UK population and reported evidence of persistent cough, fever, diarrhea, delirium, hoarse voice, headache, unusual muscle pains, loss or change in smell or taste, skipped meals, severe shortness of breath, sore throat, chest pain, abdominal pain, and severe fatigue. Moreover, this strain was found to be resistant to neutralization by antibodies. Planas et al. reported increased resistance to neutralizing antibodies by the strains. They found an escape of neutralization occurred due to mutations. B.1.351 variant had shown more resistance than B.1.1.7, and wild type D614G got neutralized easily.23,24 These escapes from neutralization lead to new complications in the global healthcare system.
The Beta variant
The WHO renamed B.1.351 or 20H/501Y.V2 as a Beta variant on December 18, 2020. It was first reported in South Africa. The earliest documented sample was found in May 2020 in South Africa. The WHO enlisted the Beta variant as a variant of concern. There are 3 mutations on the surface named spike region: K417N, E484K, and N501Y. And there are also 5 spike mutations on the surface of the virus that are a matter of less concern. 25 Compared to a preexisting variant, this variant has a faster spreading quality and causes severe illness in young people more frequently. 26 The main characteristics of this variant are increased transmission than the previous variant, to the combination of bamlanivimab and etesevimab. It shows faded susceptibility, but clinical evince of this decrease is not known. 17 But options of other monoclonal antibody treatments are available against this variant. 18 However, a two-dose regimen of the ChAdOx1 nCoV-19 vaccine did not show protection against mild-to-moderate COVID-19 due to the B.1.351 variant.27 -29 Therefore, the challenge to fight this variant is resistance to neutralization with a higher risk of death.
The Gamma variant
The Gamma variant was designated on January 11, 2021, by WHO. The earliest documented sample was found in November 2020 in Brazil. It is also known as lineage P.1. This variant has 17 amino acid substitutions, in which 10 are present on the surface as spike protein. All of them, are of particular concern: N501Y, E484K, and K417T. Also, 2 mutations are found; one in its ORF8 region and one in its N region. 30 In 2020, a study among 180 samples identified the lineage P.2 of this virus, where the samples are taken from Rio de Janeiro. By genome sequencing, this P.2 was first identified in October 2020 but appeared in early July 2020. 31 The P.2 case can be asymptomatic in some cases. 32 It has been found higher than expected reinfections with Gamma variant among the Brazilian. 33 This variant involves household transmissions and can be traveled in a community without travel history. 32 As of March 30, 2021, this variant has traveled to 45 countries. Reduced neutralization by MOA therapies, post-vaccination sera, and convalescent sera have attributed this variant. It also showed reduced sensitivity to bamlanivimab and etesevimab when they are used for combined MOA treatment. But this variant shows good sensitivity when treated with some EUA monoclonal antibodies.17,18
The Delta variant
The WHO considers the Delta variant as a VOC. The Delta variant was designated on April 4, 2021, as a VOI and designated on May 11, 2011, as a VOC by the WHO. The earliest documented sample was found in October 2020 in India. It is also recognized as lineage B.1.617.2. In India, it was first acknowledged during an aggressive wave of COVID-19 there in April and May 2021. It is rising so fast than the other variants. Now India is facing big trouble because of this variant. Countries that are linked closely economically to India (eg, countries in East Africa) are probably having a huge risk of affecting by the Delta. Cases with Delta variants in these countries are found among shipping crews at different ports. Again, Delta is the biggest risk for the countries having inadequate access to vaccines, especially the countries in Africa- where most nations can vaccinate less than 5% of their populations. This variant is 60% more transmissible than the Alpha variant that is already known as highly infectious. It can be said that this variant is somewhat resistant to vaccines; more especially in those subjects who have received just a first dose of vaccine. 34 A first vaccine dose of either AstraZeneca’s or BioNTech’s vaccine can reduce the risk by 33% for the Delta variant and 50% for the Alpha variant. 35 This Delta variant showed less sensitivity toward neutralizing antibodies inside the body. 36
Another variant has also been identified named as Delta plus. Responsible authorities in India have called it a “VOI,” but WHO hasn’t matched that designation yet. It is also recognized as B.1.617.2.1 or AY.1. It is a sub-lineage of the Delta variant. The difference between these 2 is not so many. For now, only one difference can be known which is an additional mutation in the spike protein found on the surface of the virus. Delta plus shows almost the same transmissibility as the Delta variant. Such mutation has also been found in the Beta and Gamma variants. India’s SARS-CoV-2 Consortium on Genomics reported some attributes of Delta plus variants and that said its binding capacity to the cells of a human lung is stronger and it showed a potential reduction in response while treating with MOA. The response of Delta Plus against a vaccinated body is not still clear to the world. 37
By comparing the variants, it can be stated that the Delta variant is the most dangerous variant of this virus so far. Studies say that it has the most effective transmissibility among all other variants. Delta and Delta plus affect the lungs more as they have transmissibility more than others. A big challenge is that patients are coming to hospitals affected by these variants with a worse lung condition in a very short period. It is a matter of hours to get into deadly conditions from an asymptomatic condition. Healthcare facilities are facing a huge challenge to face these cases as they need more high flow oxygen facilities and intensive care units that may not be enough so far. They are facing increased pressure of a patient with a new strong variant against medication, all of a sudden. These variations emerged as an open challenge to individuals as well as the healthcare system.
The Lambda variant
The Lambda variant was designated on June 14, 2021, by WHO. The WHO considers it to be a VOI that experts suspect it could be more dangerous than the original strain. The earliest documented sample of the Lambda variant was found in December 2020 in Peru. It is also known as lineage C.37. In this country, the number of new cases each day is increasing daily. As said in the attributes of a VOI, the Lambda variant is showing a unique outbreak in the world. It is spreading so fast in South America. The variant is still a mystery. No one knows if it is more contagious than other variants of the virus or if it affects vaccines. The mutation of the Lambda variant resembles those found in several other highly contagious or worrisome variants, which means that it is worth studying. But much remains unknown, and it is not yet clear how much of a risk it poses. Still, no evidence may suggest that Lambda will exceed Delta, which is the highly transmissible variant and that’s now dominating most of the world. The variant contains 8 mutations, where 7 mutations in the gene for the spike protein and are found on the surface of the virus. These mutations may help the variant to be more infectious or to destroy the immune system of the human body. But still, it is not clear that whether this variant has more ability to transmit than the other variants. Some researchers said that Lambda is not found to be worrisome as Delta and does not expect it to become as dominant globally. 38
The Omicron variant
The newly discovered variant “Omicron” of SARS-CoV-2 has heavily mutated to its spike protein, the target of vaccines. 39 The Omicron has raised concerns regarding the transmission of coronavirus, immune system evasion, and vaccine resistance. 40 Many countries have already confirmed the first case of the Omicron variant and the symptoms are mid so far. 40 Several countries have imposed travel restrictions on South African countries to curb the international spread of the Omicron variant. However, it is much difficult to implement health safety guidelines due to several factors. 41 Therefore, the COVID-19 situation may take a drastic turn due to the transmission of the Omicron variant. Thus, we recommend mass immunization for all adults at the earliest possible time. Along with the vaccination programs, avoidance of public gatherings, the unveiling of new genomes, and monitoring of abnormalities should be continued. 42
Other VOIs
The WHO designated several variants of SARS-CoV-2 as VOIs including Eta, Lota, and Kappa strains. The first cases of these mutants were found in multiple countries between the last 2 months of 2020. Later WHO designated these variants as VOIs when their transmissibility, disease severity, immune escape, diagnostic or therapeutic escapes, and their epidemiological impacts meet the criteria although these variants are not significantly as severe and fatal than VOCs. However, VOIs strains also cause mortality and severity of disease in patients of many countries due to immune escape.11,43
New Variants and New Challenges on Global Public Health
The world is facing the worst public health crisis than ever due to the ongoing pandemic. The world is searching for therapeutic and preventative solutions. There are 2 uppermost priorities at this moment: first of all, to revise already-approved pharmacologically active agents or develop therapies to minimize the morbidity and mortality associated with the virus. Secondly, the scientific and pharmaceutical community is to be designated with the invention, testing, and production of a safe and effective vaccine as a longer-term solution to prevent further spreading. 44 Though it sometimes raises the question that if a vaccine can fully protect someone from the virus as it changes its properties so fast and variants come forward with more strong mutations. But there is much evidence that said, vaccination helps in reducing the spread of the virus and protects humans. A study found that people having a single dose and a double dose of the vaccine have respectively 75% and 94% less probability to get into hospital compared to others who have not taken any dose yet. 34 The vaccination procedure helps trigger or boost a long-lasting immune response against the virus responsible for COVID-19. 45 Another study says this emergence can only be avoided by increasing the vaccinated population all over the world and by not relaxing epidemiological containment measures. Besides, it is necessary to revaccinate against new variants. 46 Findings suggest that these vaccines should still work against Lambda, which is the latest variant among all so far. Experts warn that worldwide vaccination rates need to dramatically increase to prevent more variants from arising. 47 So, the vaccinated population is to be increased globally to reduce spreading.
Challenges for Poor and Developing Countries
Poor and developing countries are continuously facing new challenges due to the mutation of coronavirus.48 -54 Developing countries have to make proper planning and road-map to vaccinate their whole population in a period.55 -57 This time, individual needs to aware of the health measures given by WHO to prevent infection and slow transmission. The hospitals should work on how to develop the system of supplying oxygen centrally. Research institutions and universities can work together to develop some advanced systems to face this current situation. Herd immunity can be the only savior for third world countries as a vaccinated population is not an easy thing to make for them. Globally, policymakers should remake their structures of health sectors overall the world. Countries should make themself ready slowly for a further global health crisis. The theory of social distancing must be maintained by individuals. Developing countries may invest more to raise awareness regarding health measures.58 -65 It is a very different scenario the world is going through. No nation was prepared for this deadly situation, but the future world must have to be ready to fight against this kind of emergencies. So, the world needs to gather more possible data and work on it. In the meantime, getting a vaccinated population and maintaining health measures can be the ultimate target for the world.
Initiatives to Protect Public Health During Global Health Emergencies
In the current context, where vaccination campaigns have already begun in COVID-19-affected countries, the emergence of new strains has generated global concerns about their potential impact on the severity of disease and antibody sensitivity. 66 Antibody generation is a time-consuming process, individuals should maintain safety measures even though they are vaccinated.67,68 All the VOCs designated strains are highly transmissible, particularly the Delta and Omicron variants. Gamma and Beta strains escape immunity and generate global public health concerns as they can elevate the rate of mass reinfection. The existing vaccines should be redesigned to prevent reinfection. Prevalence of disease severity of Beta, Delta, and Gamma variants was found very high although any of the VOCs strains have the potential of causing serious disease conditions, in worst case death. COVID-19 affected nations should follow the guidelines provided by WHO. Mass vaccination can be a preventive action wherever several pieces of evidence state that vaccination helps in minimizing severity and transmission. The nations must control the community transmission of viruses and mass vaccination should be carried out at the same time. Extensive genome sequencing should be carried out globally to faster understand and globally control the emerging strains. To prevent the rolling out of oxygen and therapeutic supply during the epidemic surge, the nations should prepare a nationwide systematic guideline and plan of action. Professionals, drugs, and devices for the treatment of severe conditions should be made available at the community level. The nations with VOCs strains should restructure and re-compile their plan of response as immediately as possible to manage the ongoing crisis, and the nations with VOIs and alerts for further monitoring should prepare their plans and infrastructure for possible worst cases.
Conclusions
The global healthcare facilities are facing challenges in rolling out of vaccination programs, ensuring oxygen supply, and treating severe COVID patients during epidemic waves. Implementation of mass vaccination programs, slowing down the transmission, redesign of vaccine, and following safety guidelines are effective solutions to the new challenges of viral mutations.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SI and TI collected data and drafted the manuscript; MRI revised and edited the manuscript, gave intellectual inputs, helped review the manuscript, and provided feedback for improvement. All authors have read and approved the manuscript.
ORCID iDs: Towhidul Islam  https://orcid.org/0000-0002-8402-0740
https://orcid.org/0000-0002-8402-0740
Md. Rabiul Islam  https://orcid.org/0000-0003-2820-3144
https://orcid.org/0000-0003-2820-3144
References
- 1. WHO. Naming the coronavirus disease (COVID-19) and the virus that causes it. 2020. Accessed July 10, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
- 2. Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. 2020;25:278-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO. WHO Coronavirus (COVID-19) Dashboard. 2022. Accessed January 25, 2022. https://covid19.who.int/.
- 4. Chen L, Zheng S. Understand variability of COVID-19 through population and tissue variations in expression of SARS-CoV-2 host genes. Inform Med Unlocked. 2020;21:100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang X, Huang K, Jiang H, et al. Long-Term existence of SARS-CoV-2 in COVID-19 patients: host immunity, viral virulence, and transmissibility. Virol Sin. 2020;35:793-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang R, Hozumi Y, Yin C, Wei GW. Mutations on COVID-19 diagnostic targets. Genomics. 2020;112:5204-5213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nature. Coronavirus variants get Greek names—but will scientists use them? 2021. Accessed July 10, 2021. https://www.nature.com/articles/d41586-021-01483-0. [DOI] [PubMed]
- 10. Aleem A, Akbar Samad AB, Slenker AK. Emerging Variants of SARS-CoV-2 And Novel Therapeutics Against Coronavirus (COVID-19). In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 11. WHO. Tracking SARS-CoV-2 variants. 2021. Accessed January 25, 2022. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/.
- 12. Taylor v. Covid-19: Omicron drives weekly record high in global infections. BMJ. 2022;376:o66. doi:10.1136/bmj.o66. [DOI] [PubMed]
- 13. The Guardian. Here’s what we know about the new variant of coronavirus. 2020. Accessed July 10, 2021. https://www.theguardian.com/commentisfree/2020/dec/22/new-variant-coronavirus-genomic-sars-cov-2-pandemic.
- 14. Harvey WT, Carabelli AM, Jackson B, et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. 2021;19:409-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;372:eabg3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. GOVUK, NERVTAG paper on COVID-19 variant of concern B.1.1.7. 2021. a. Accessed July 10, 2021. https://www.gov.uk/government/publications/nervtag-paper-on-covid-19-variant-of-concern-b117.
- 17. FDA. Fact sheet for health care providers emergency use authorization (eua) of bamlanivimab and etesevimab. 2021. a. Accessed July 10, 2021. https://www.fda.gov/media/145802/download.
- 18. FDA. Fact sheet for health care providers emergency use authorization (eua) of regen-covtm (casirivimab and imdevimab). 2021. b. Accessed July 10, 2021. https://www.fda.gov/media/145611/download.
- 19. Collier DA, De Marco A, Ferreira IATM, et al. Sensitivity of SARS-CoV-2 B.1.1.7 to mRNA vaccine-elicited antibodies. Nature. 2021;593:136-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention. Symptoms of COVID-19. Accessed December 24, 2021. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
- 21. Office for National Statistics. Coronavirus (COVID-19) Infection Survey - Office for National Statistics. 2021. Accessed July 10, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/characteristicsofpeopletestingpositiveforcovid19inengland8april2021.
- 22. Graham MS, Sudre CH, May A, et al. Changes in symptomatology, reinfection, and transmissibility associated with the SARS-CoV-2 variant B.1.1.7: an ecological study. Lancet Public Health. 2021;6:e335-e345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Graham C, Seow J, Huettner I, et al. Neutralization potency of monoclonal antibodies recognizing dominant and subdominant epitopes on SARS-CoV-2 spike is impacted by the B.1.1.7 variant. Immunity. 2021;54:1276-1289.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Planas D, Bruel T, Grzelak L, et al. Sensitivity of infectious SARS-CoV-2 B.1.1.7 and B.1.351 variants to neutralizing antibodies. Nat Med. 2021;27:917-924. [DOI] [PubMed] [Google Scholar]
- 25. Galloway SE, Paul P, MacCannell DR, et al. Emergence of SARS-CoV-2 B.1.1.7 lineage – United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:95-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tegally H, Wilkinson E, Giovanetti M, et al. Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. medRxiv. 2020. doi: 10.1101/2020.12.21.20248640. [Google Scholar]
- 27. Trigueiro-Louro J, Correia V, Figueiredo-Nunes I, Gíria M, Rebelo-de-Andrade H. Unlocking COVID therapeutic targets: a structure-based rationale against SARS-CoV-2, SARS-CoV and MERS-CoV spike. Comput Struct Biotechnol J. 2020;18:2117-2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Irfan N, Chagla Z. In South Africa, a 2-dose Oxford/AZ vaccine did not preventmild to moderate COVID-19 (cases mainly B.1.351 variant). Ann Intern Med. 2021;174:JC50. [DOI] [PubMed] [Google Scholar]
- 29. Madhi SA, Baillie V, Cutland CL, et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 vaccine against the B.1.351 variant. N Engl J Med. 2021;384:1885-1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. COG. Covid-19 Genomic UK Consortium. COG-UK report on SARS-CoV-2 Spike mutations of interest in the UK 15th January 2021. 2021. Accessed July 10, 2021. https://www.cogconsortium.uk/wp-content/uploads/2021/02/Report-2_COG-UK_SARS-CoV-2-Mutations.pdf.
- 31. Voloch CM, da Silva Francisco R, Jr, de Almeida LGP, et al. Genomic characterization of a novel SARS-CoV-2 lineage from Rio de Janeiro, Brazil. J Virol. 2021;95:e00119-e00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Campoy PJS, Buenestado-Serrano S, Pérez-Lago L, et al. Primeras importaciones de las variantes SARS-CoV-2 P.1 y P.2 de Brasil a Madrid y transmisión comunitaria [First importations of SARS-CoV-2 P.1 and P.2 variants from Brazil to Spain and early community transmission] [published online ahead of print, 2021 Jun 3]. Enferm Infecc Microbiol Clin (Engl Ed). 2021. doi:10.1016/j.eimc.2021.05.008. [Google Scholar]
- 33. Taylor L. Covid-19: researchers find higher than expected reinfections with P.1 variant among the Brazilian Amazon. BMJ. 2021;373:n1353. [DOI] [PubMed] [Google Scholar]
- 34. Creech CB, Walker SC, Samuels RJ. SARS-CoV-2 vaccines. JAMA. 2021;325:1318-1320. [DOI] [PubMed] [Google Scholar]
- 35. GOVUK, Vaccines highly effective against B.1.617.2 variant after 2 doses. 2021. b. Accessed July 10, 2021. https://www.gov.uk/government/news/vaccines-highly-effective-against-b-1-617-2-variant-after-2-doses.
- 36. Planas D, Veyer D, Baidaliuk A, et al. Reduced sensitivity of SARS-CoV-2 variant delta to antibody neutralization. Nature. 2021;596:276-280. [DOI] [PubMed] [Google Scholar]
- 37. Kannan SR, Spratt AN, Cohen AR, et al. Evolutionary analysis of the Delta and Delta plus variants of the SARS-CoV-2 viruses. J Autoimmun. 2021;124:102715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Padilla-Rojas C, Jimenez-Vasquez V, Hurtado V, et al. Genomic analysis reveals a rapid spread and predominance of lambda (C.37) SARS-COV-2 lineage in Peru despite circulation of variants of concern. J Med Virol. 2021;93:6845-6849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Saxena SK, Kumar S, Ansari S., et al. Characterization of the novel SARS-CoV-2 Omicron (B.1.1.529) variant of concern and its global perspective [published online ahead of print, 2021 Dec 14]. J Med Virol. 2021. doi:10.1002/jmv.27524. [DOI] [PubMed] [Google Scholar]
- 40. Sohan M, Hossain MJ, Islam MR. The SARS-CoV-2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: What we know so far [published online ahead of print, 2022 Jan 6]. J Med Virol. 2022. doi:10.1002/jmv.27574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Daria S, Bhuiyan MA, Islam MR. Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: associated risk factors and preventive actions. J Med Virol. Published online December 4, 2021 doi: 10.1002/jmv.27503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Islam R, Hossain J. Detection of SARS-CoV-2 omicron (B.1.1.529) variant has created panic among the people across the world: What should we do right now? J Med Virol. Published online December 23, 2021. doi: 10.1002/jmv.27546 [DOI] [PubMed] [Google Scholar]
- 43. Parums V. Editorial: Revised World Health Organization (WHO) terminology for variants of concern and variants of interest of SARS-CoV-2. Med Sci Monit. 2021;27:e933622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Izda V, Jeffries MA, Sawalha AH. COVID-19: a review of therapeutic strategies and vaccine candidates. Clin Immunol. 2021;222:108634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tan Y, Liu F, Xu X, et al. Durability of neutralizing antibodies and T-cell response post SARS-CoV-2 infection. Front Med. 2020;14:746-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cantón R, De Lucas Ramos P, García-Botella A, et al. New variants of SARS-CoV-2. Rev Esp Quimioter. 2021;34(5):419–428. doi:10.37201/req/071.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rahman FI, Ether SA, Islam MR. The “Delta Plus” COVID-19 variant has evolved to become the next potential variant of concern: mutation history and measures of prevention. J Basic Clin Physiol Pharmacol. Published online September 27, 2021. doi: 10.1515/jbcpp-2021-0251. [DOI] [PubMed] [Google Scholar]
- 48. Islam MR, Qusar MMAS, Islam MS. Mental health of children amid COVID-19 pandemic in Bangladesh: an exploratory observation. Asia Pac J Public Health. 2021;33:469-470. [DOI] [PubMed] [Google Scholar]
- 49. Das R, Hasan MR, Daria S, Islam MR. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open. 2021;11:e045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Daria S, Asaduzzaman M, Shahriar M, Islam MR. The massive attack of COVID-19 in India is a big concern for Bangladesh: the key focus should be given on the interconnection between the countries. Int J Health Plann Manage. 2021;36:1947-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Daria S, Islam MR. The use of cow dung and urine to cure COVID-19 in India: a public health concern. Int J Health Plann Manage. 2021;36:1950-1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Daria S, Islam MR. The second wave of COVID-19 pandemic in Bangladesh: an urgent call to save lives. Asia Pac J Public Health. 2021;33:665-666. [DOI] [PubMed] [Google Scholar]
- 53. Repon MAU, Pakhe SA, Quaiyum S, Das R, Daria S, Islam MR. Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: a cross-sectional study. Sci Prog. 2021;104:368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Moona AA, Islam MR. Mucormycosis or black fungus is a new fright in India during covid-19 pandemic: associated risk factors and actionable items. Public Health Pract (Oxf). 2021;2:100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hossain MJ, Soma MA, Islam MR, Emran TB. Urgent call for actionable measures to fight the current co-epidemic of dengue burden during the SARS-CoV-2 delta variant era in South-Asia. Ethics Med Public Health. 2021;19:100726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hossain MJ, Rahman S, Emran TB, Mitra S, Islam MR, Dhama K. Recommendation and roadmap of mass vaccination against COVID-19 pandemic in Bangladesh as a lower-middle-income country (LMIC). Achiev Razi Inst. 2021;76(6):1793–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hossain MJ, Jannat T, Brishty SR, et al. Clinical efficacy and safety of antiviral drugs in the extended use against COVID-19: what we know so Far. Biologics. 2021;1:252-284. [Google Scholar]
- 58. Islam MR, Hossain MJ. Increments of gender-based violence amid COVID-19 in Bangladesh: a threat to global public health and women’s health. Int J Health Plann Manage. 2021;36:2436-2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rahman FI, Islam MR, Bhuiyan MA. Mucormycosis or black fungus infection is a new scare in South Asian countries during the COVID-19 pandemic: associated risk factors and preventive measures. J Med Virol. 2021;93:6447-6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rahman MA, Shanjana Y, Tushar MI, et al. Hematological abnormalities and comorbidities are associated with COVID-19 severity among hospitalized patients: experience from Bangladesh. PLoS One. 2021;16:e0255379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the Covid-19 has worsened the situation. Chronic Stress (Thousand Oaks). 2021;5:24705470211035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Rahman FI, Islam MR. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Womens Health. 2021;17:17455065211043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Islam MR, Daria S, Das R, Hasan MR. A nationwide dataset on the mental health of the Bangladeshi population due to the COVID-19 pandemic. Data Brief. 2021;38:107347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Islam MR, Quaiyum S, Pakhe SA, Repon MAU, Bhuiyan MA. Dataset concerning the mental health of healthcare professionals during COVID-19 pandemic in Bangladesh. Data Brief. 2021;39:107506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Islam R. The COVID-19 pandemic and suicidal behavior in Bangladesh: social stigma and discrimination are key areas to focus on. Alpha Psychiatry. 2021;22:275-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Islam MR. Urgent call for mass immunization against coronavirus in Bangladesh. Sci Prog. 2021;104(4). doi:10.1177/00368504211058562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bari MS, Hossain MJ, Ahmmed F., et al. Knowledge, Perception, and Willingness towards Immunization among Bangladeshi Population during COVID-19 Vaccine Rolling Period. Vaccines (Basel). Published online Decembfer 7, 2021;9(12):1449. doi:10.3390/vaccines9121449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ether SA, Emon FA, Roknuzzaman A., Rakibuzzaman M, Rahman FI, Islam MR. A cross-sectional study of COVID-19-related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh. SAGE Open Med. Published online January 18, 2022;10. doi:10.1177/20503121211073014. [DOI] [PMC free article] [PubMed] [Google Scholar]