Abstract
Objective:
Simultaneous alcohol and nonmedical prescription drug use (NMPDU) increases acute risks (e.g., overdose) associated with each; understanding social, substance use, and mental health predictors of same-day use may suggest intervention targets. Method: At an urban emergency department, research assistants recruited youth ages 14–24 reporting past-6-month substance use (n = 599; 58.8% male). Participants self-administered validated measures of alcohol consumption, cannabis use severity (quantity and consequences), mental health symptoms, and social influences at baseline and at four biannual follow-ups. In addition, participants completed Timeline Followback calendars that assessed same-day use of alcohol and prescription drugs. We used negative binomial regression with person-level fixed effects to isolate within-person predictor effects on same-day use frequency.
Results:
Between 6.0% (baseline) and 8.6% (6-month follow-up) of youth reported same-day alcohol use and NMPDU across follow-ups. Within-person increases in alcohol consumption, cannabis use severity, and depression and anxiety symptoms all corresponded to greater same-day alcohol and NMPDU frequency, with consistent findings across genders. Increased positive peer behaviors corresponded to decreased same-day use frequency among males but not females. Decreased parental support and increased delinquent peer exposures corresponded to greater same-day use frequency among females but not males.
Conclusions:
Substance use and mental health symptom escalation are robust predictors of greater same-day use frequency, whereas the roles of social factors appear gender-specific. Interrupting worsening trajectories of substance use and mental health symptoms, and enhancing social support and reducing delinquent peer exposures, may reduce same-day use frequency.
Alcohol is the most commonly used substance in the United States, with initiation and escalation of use often occurring during adolescence and young adulthood (Stone et al., 2012; Substance Abuse and Mental Health Services Administration [SAMHSA], 2020a; Sussman & Arnett, 2014). For example, 18.5% of youth ages 12–20 and 66.2% of those 21–25 years old report past-month alcohol consumption; 11.1% and 41.6%, respectively, report past-month binge drinking, whereas 3.3% and 11.1% endorse symptoms indicative of an alcohol use disorder (SAMHSA, 2020a). In addition, 1.3% of adolescents ages 12–17 and 3.4% of young adults ages 18–25 reported nonmedical prescription drug use (NMPDU) in the past month (past-year: 4.3% and 11.5%, respectively; SAMHSA, 2020a).
Alcohol and NMPDU are associated with increased risk for mental, physical, and social consequences (Baggio et al., 2014; Bonar et al., 2020). NMPDU is associated with both depressive symptoms (Bonar et al., 2020; Lin et al., 2016; Schepis et al., 2018, 2020) and anxiety (Roy et al., 2015; Viana et al., 2012) among youth and, for example, there is evidence that co-ingestion with other substances is associated with seeking mental health treatment among nonmedical sedative/tranquilizer–using youth (Schepis et al., 2016). In addition, mixing alcohol and prescription drugs carries acute health risks. Specifically, co-use of alcohol and prescription opioids can lead to potentially fatal respiratory complications, even with normal-level prescription doses and relatively moderate alcohol co-consumption (van der Schrier et al., 2017). Similarly, sedative/hypnotic co-use with alcohol dramatically increases the risk for overdose death (Garg et al., 2017), whereas prescription stimulant and alcohol co-use may enhance the stimulatory effects, potentially lengthening the duration of a drinking session, increasing related risks (Egan et al., 2013). Thus, it is crucial to understand the prevalence, frequency, and predictors of changes in alcohol and NMPDU co-use, particularly among youth, who show the highest consumption rates of both (Johnston et al., 2014; National Institute on Drug Abuse [NIDA], 2001).
Research on alcohol and NMPDU epidemiology typically involves school-based samples. Among undergraduates, 12.1% reported past-year alcohol and NMPDU co-use, with higher rates among males, White youth, and those reporting earlier alcohol use initiation (McCabe et al., 2006). Past-year NMPDU of prescription stimulants and opioids among high school seniors was 7.3% (McCabe et al., 2015) and 12.3% (McCabe et al., 2012), respectively; roughly half of those reporting nonmedical use also reported co-ingestion with alcohol (McCabe et al., 2012, 2015). The risk of co-use is enhanced by those reporting use in social contexts (McCabe et al., 2015) and with recreational motives (McCabe et al., 2012, 2015). Similarly, other researchers have found more than half of college students reporting NMPDU also report co-use with alcohol, and those individuals generally report higher drinking severity (Garnier et al., 2009).
The current work offers innovations through both the target of the statistical inference and the study population. No prior studies have analyzed co-use among youth in health care settings, such as the emergency department, which is crucial both because (a) urban emergency departments provide an access point for youth who may not attend school or have other health care access and (b) emergency-department youth may be more amenable to behavior change and intervention than those in other settings (Maio et al., 2005). Thus, this work will provide previously unavailable information on a crucial study population that is well-suited to intervention. In addition, although prior studies have identified within-person predictors of changes in substance use (e.g., drug use disorder; Goldstick et al., 2021), no prior research has analyzed what factors are associated with within-person changes over time in alcohol and NMPDU co-use, which may offer crucial information on intervention points and modifiable risk factors.
In this study, we used longitudinal data from youth presenting to an urban emergency department to examine frequency, rates, and predictors of within-person changes in alcohol and NMPDU (stimulants, sedatives, and opioids) co-use (measured as same-day consumption). Given their importance in prior work, we focused principally on time-varying measurements of alcohol consumption, mental health symptoms, and social exposures, as potential predictors, consistent with the inner levels of social-ecological model, which can provide a framework for potential interventions incorporating resiliency-based approaches (Bronfenbrenner, 1994; Garmezy, 1991; Rutter, 1987; Sallis et al., 2008; Sudhinaraset et al., 2016). Given gender-based differences in substance use epidemiology (McHugh et al., 2018), we also conducted gender-stratified analyses. We hypothesized that increased alcohol consumption, worsening depression and anxiety symptoms, and decreased social support would correspond to greater rates of alcohol and NMPDU co-use.
Method
Participants
Youth (ages 14–24) seeking emergency-department treatment for violent injuries in Flint, MI (November 2009–September 2011), were approached for study participation, in addition to a sequentially sampled, age/gender-matched group seeking treatment for other reasons. Those reporting any past-6-month drug use during screening were eligible for a longitudinal study involving a baseline assessment and four biannual follow-ups (all follow-up rates >83%). In total, 599 youth (349 violently injured; 58.8% male; 58.3% Black, 32.6% White, 7.5% multiracial; 5.8% Hispanic) participated in the longitudinal study. Detailed procedures and sample characteristics are described elsewhere (Bohnert et al., 2015; Cunningham et al., 2015a).
Measures
We measured substance consumption (baseline: past-30-days, follow-ups: past-90-days) via the study staff-administered Timeline Followback (TLFB; Hjorthøj et al., 2012; Sobell et al., 1979) recording alcohol quantity (standard drinks) and a binary indicator (yes/no) of nine other substances. Language for the interview guide, including the NMPDU questions (“This means on your own to get high, taken someone else's, or taken more than was prescribed”), was adapted from the NIDA–Alcohol, Smoking and Substance Involvement Screening Test (NIDA-ASSIST; WHO ASSIST Working Group, 2002). TLFB data from this study have been used previously (e.g., Stoddard et al., 2015; Walton et al., 2017). The primary outcome was the number of days on which the participant reported both alcohol use and nonmedical use of one of the following: prescription stimulants, prescription opioids, and/or prescription sedatives.
The focal time-varying explanatory variables in this analysis are self-reported measures of alcohol consumption, cannabis use severity (quantity used; consequences), mental health symptoms, social support/influences, past-6-month violence injury, and demographics (age; public assistance). We assessed past-6-month alcohol use using the Alcohol Use Disorders Identification Test–Consumption (AUDIT-C; Bush et al., 1988; within-sample Cronbach's α = .84) and cannabis use severity by summing the six-item NIDA-Modified ASSIST cannabis subscale (WHO ASSIST Working Group, 2002; α = .75). We used the AUDIT-C rather than the full-length AUDIT because its brevity optimizes usefulness in an emergency-department setting while maintaining strong sensitivity and specificity (Dawson et al., 2005). Participants reported past-week depression and anxiety symptoms (six items each) using the Brief Symptom Inventory (BSI; Piersma et al., 1994; α = .93); we averaged the 12 items into one score.
We measured current positive peer behaviors (four items; e.g., school, community participation; α = .78) and peer delinquency (seven items; e.g., substance use, fighting; α = .82) as the average of scales from the Flint Adolescent Study (Zimmerman et al., 2002), and measured parental support (six items; α = .92) (Procidano & Heller, 1983). Demographics included age, gender, and receipt of public assistance.
Statistical analysis
We calculated the proportion of participants reporting co-use of alcohol and each of prescription stimulants, prescription sedatives, and prescription opioids at each follow-up. Our adjusted analysis was negative binomial regression. Because we were principally interested in within-person associations between the covariates and co-use frequency, all models included person-level fixed effects. Person-level fixed effects ensure the covariate effect estimates are only driven by within-person associations (Gunasekara et al., 2014) and automatically control for time-invariant person-level confounders—both measured and unmeasured. Although typically applied in linear regression models, similar logic applies in negative binomial regression models (Allison & Waterman, 2002); which we chose because of the count outcome. Models included an offset for the log of the number of days assessed in each TLFB (baseline: 30; follow-ups: 90). We hypothesized gender differences in predictors of alcohol and prescription drug co-use, so our models were stratified by gender. Thus, we fit four models in total—one combined model, one with males only, one with females only, and a fourth to explicitly test interactions between gender and each predictor. R version 3.6.0 (www.r-project.org) was used for all data handling and analysis.
Results
The proportions reporting at least 1 alcohol and NMPDU co-use day at baseline and at each follow-up were between 6.0% (baseline) and 8.6% (6-month) across assessments. Supplemental Figure 1 shows the proportion reporting alcohol and NMPDU same-day use at each follow-up, stratified by drug type (stimulants, sedatives, and opioids). (The supplemental material appears as an online-only addendum to this article on the journal's web-site.) Prescription stimulant and alcohol co-use was least common (<1% at all assessments). Across assessments, sedative and alcohol co-use was reported by the largest proportion, ranging between 3.8% (baseline) and 5.5% (18-month follow-up). Between 2.0% (baseline) and 4.7% (6-month) reported at least one alcohol and prescription opioid co-use day. Frequencies stratified by gender are shown in Supplemental Figure 2. Overall, males reported co-use on 1 or more days in 7.9% of all TLFB assessments, whereas the corresponding percentage for females was 6.0%; the difference was not statistically significant (p = .08). Appendix Table 1 shows descriptive statistics for the outcome and each covariate at each follow-up; past-6-month substance use and current mental health symptoms were highest at baseline, and there were comparatively smaller changes in social exposures. The intraclass correlation coefficient of the outcome was .08, suggesting substantial within-person variability in the outcome.
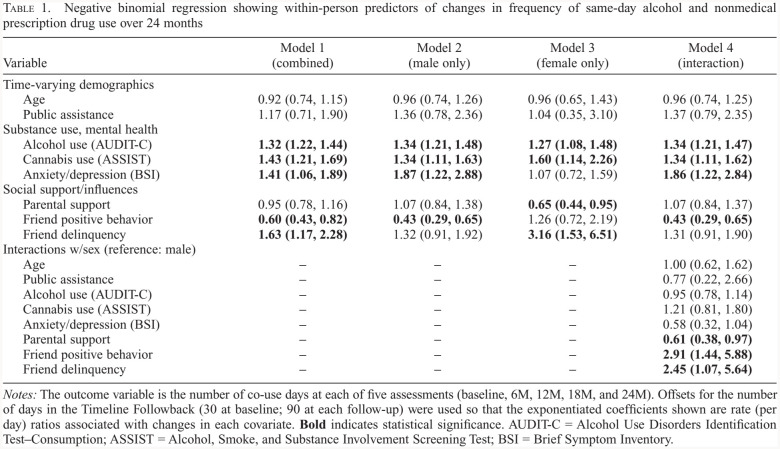
Table 1 shows negative binomial regression examining within-person predictors of changes in alcohol and prescription drug co-use frequency. Among males, increased alcohol consumption (rate ratio [RR] = 1.34), cannabis use severity (RR = 1.34), and anxiety/depression symptoms (RR = 1.87) all corresponded to greater frequency of alcohol and prescription drug co-use, whereas increased positive peer behaviors coincided with less co-use frequency (RR = 0.43). Among females, alcohol consumption (RR = 1.27) and cannabis use severity (RR = 1.60) also showed positive within-person associations with co-use frequency, but, unlike males, peer delinquency (RR = 3.16) also was positively associated with co-use frequency; increased parental support corresponded to lower rates of co-use (RR = 0.65). The joint model confirmed peer delinquency was significantly more risk-enhancing among females, positive peer affiliations were more protective among males, and parental support was more protective among females. As a sensitivity analysis, we re-fit each model using only the 71.3% of participants who completed all five assessments (Appendix Table 2); there were no large changes in the direction or magnitudes of effects, but the parental support findings were no longer significant because of widening of the confidence interval.
Table 1.
Negative binomial regression showing within-person predictors of changes in frequency of same-day alcohol and nonmedical prescription drug use over 24 months
| Variable | Model 1 (combined) | Model 2 (male only) | Model 3 (female only) | Model 4 (interaction) |
|---|---|---|---|---|
| Time-varying demographics | ||||
| Age | 0.92 (0.74, 1.15) | 0.96 (0.74, 1.26) | 0.96 (0.65, 1.43) | 0.96 (0.74, 1.25) |
| Public assistance | 1.17 (0.71, 1.90) | 1.36 (0.78, 2.36) | 1.04 (0.35, 3.10) | 1.37 (0.79, 2.35) |
| Substance use, mental health | ||||
| Alcohol use (AUDIT-C) | 1.32 (1.22,1.44) | 1.34 (1.21, 1.48) | 1.27 (1.08, 1.48) | 1.34 (1.21,1.47) |
| Cannabis use (ASSIST) | 1.43 (1.21,1.69) | 1.34 (1.11, 1.63) | 1.60 (1.14, 2.26) | 1.34 (1.11, 1.62) |
| Anxiety/depression (BSI) | 1.41 (1.06,1.89) | 1.87 (1.22, 2.88) | 1.07 (0.72, 1.59) | 1.86 (1.22, 2.84) |
| Social support/influences | ||||
| Parental support | 0.95 (0.78, 1.16) | 1.07 (0.84, 1.38) | 0.65 (0.44, 0.95) | 1.07 (0.84, 1.37) |
| Friend positive behavior | 0.60 (0.43, 0.82) | 0.43 (0.29, 0.65) | 1.26 (0.72, 2.19) | 0.43 (0.29, 0.65) |
| Friend delinquency | 1.63 (1.17, 2.28) | 1.32 (0.91, 1.92) | 3.16 (1.53, 6.51) | 1.31 (0.91, 1.90) |
| Interactions w/sex (reference: male) | ||||
| Age | - | - | - | 1.00 (0.62, 1.62) |
| Public assistance | - | - | - | 0.77 (0.22, 2.66) |
| Alcohol use (AUDIT-C) | - | - | - | 0.95 (0.78, 1.14) |
| Cannabis use (ASSIST) | - | - | - | 1.21 (0.81, 1.80) |
| Anxiety/depression (BSI) | - | - | - | 0.58 (0.32, 1.04) |
| Parental support | - | - | - | 0.61 (0.38, 0.97) |
| Friend positive behavior | - | - | - | 2.91 (1.44, 5.88) |
| Friend delinquency | - | - | - | 2.45 (1.07, 5.64) |
Notes: The outcome variable is the number of co-use days at each of five assessments (baseline, 6M, 12M, 18M, and 24M). Offsets for the number of days in the Timeline Followback (30 at baseline; 90 at each follow-up) were used so that the exponentiated coefficients shown are rate (per day) ratios associated with changes in each covariate. Bold indicates statistical significance. AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; ASSIST = Alcohol, Smoke, and Substance Involvement Screening Test; BSI = Brief Symptom Inventory.
Discussion
This is the first examination of alcohol and NMPDU couse among youth presenting to an urban emergency department. We found that co-use was relatively common, with up to 8.6% reporting recent co-use days, and co-use was generally more likely among males, which is substantially higher than past-30-day rates in national samples of youth ages 12–25, who report rates under 0.5% for co-use of alcohol and each of stimulants, pain relievers, and tranquilizers/sedatives (SAMHSA, 2020b). In addition, there was within-person variability over time in co-use, with several factors predicting that variability in the context of gender differences in their effects. Furthering knowledge of within-person predictors of changes in alcohol and NMPDU co-use has potential to enhance prevention of co-use and its accompanying risks (e.g., unintentional overdose).
In both males and females, escalating alcohol consumption and cannabis use severity corresponded to greater rates of alcohol and NMPDU co-use. This finding is consistent with prior research showing that those reporting couse have higher drinking severity (Garnier et al., 2009), but this is the first analysis to identify effects driven only by within-person changes. These within-person associations suggest that changes in alcohol use, which are also predictable (Goldstick et al., 2019), and changes in cannabis use, coalesce with changes in higher risk substance use (i.e., misuse of prescriptions, and same-day of prescription drugs with alcohol), and this signal is robust across men and women. Our results suggest that focusing on alcohol and prescription drug co-use for prevention is important, especially among those with indications of escalating alcohol and cannabis use, which could signify a transition into riskier behaviors.
Similar to prior work from this study underscoring the importance of peer influences in substance use trajectories (Goldstick et al., 2018a; Walton et al., 2017), social factors appear related to co-use frequency, with differences across genders. Social exposures primarily affected males through the protective effects of positive peer behaviors, whereas females showed protective effects of parental support. This suggests that social support is important in terms of preventing co-use, but that effect manifests differently by gender. There was a nonsignificant enhanced risk from delinquent peer associations among males, but the effect was more than twice as large (and significant) among females, suggesting greater importance among females; this is consistent with prior research showing that delinquent peer affiliations are a robust predictor of several problem behaviors, including substance use, but their effects are modified by several factors (Marschall-Lévesque et al., 2014), including gender (Goldstick et al., 2018b). Notably, the combined model, without interactions, obscured the protective effects of social variables, highlighting the ongoing importance of examining gender differences in substance use epidemiology (McHugh et al., 2018). Interventions rooted in social ecological theory that incorporate social factors to mitigate co-use risk and negative outcomes could tailor approaches based on the nuances of gender differences in the effects of pro-social factors on co-use. Further, among men, depression/anxiety symptoms were positively associated with co-use, supporting the need to address mental health as well.
This study benefitted from a unique and crucially important study population, time-varying measures of day-level substance use outcomes, and novel predictors, but limitations bear mentioning. The TLFB assessed same-day co-use, which could include—but was not limited to—simultaneous use. Same-day use, even if not simultaneous, of alcohol and NMPDU still confers risk, as many of the substances involved have a fairly long half-life, but future work that measures simultaneous use, potentially with ecological momentary assessment designs, is warranted. Such future studies would also address limitations surrounding the age of the current data set, which ended follow-ups in 2013. Relatedly, amount (e.g., pills, milligrams) of prescription drug ingestion was not assessed, although this would allow a sharper conception of the acute risks of co-use. More general limitations center around lack of assessment of substance use motives in this study (particularly co-use motives, which could reflect desires to address pain or potential suicidality), and the need to replicate this work in other populations (including diverse representation of gender minorities) to increase generalizability and explore other demographic differences (e.g., differences by race/ethnicity).
We demonstrated that alcohol and prescription drug couse is common among emergency-department youth—a population uniquely amenable to intervention—and within-person changes in co-use frequency are both predictable and differ by gender. Prevention of overdose risk behaviors, which include alcohol and prescription drug co-use, could focus on those showing increases in drinking and other substance use severity, which we have shown coalesce with greater co-use risk among both males and females. A first step may be providing education surrounding the risks of alcohol and prescription drug co-use among those at highest risk, as well as motivational interviewing–based interventions to decrease this risky behavior (Cunningham et al., 2015b). We also affirmed the importance of social exposures in the frequency of co-use, but optimization of that information likely requires gender-specific approaches. Overall, enhancing social support and positive social exposures, and lowering delinquent peer affiliations, which are known to modulate substance use rates (Marschall-Lévesque et al., 2014), may also specifically reduce co-use risk. This information is an important step to optimize emergency department–based behavioral interventions to prevent future overdose risk from alcohol and prescription drug co-use, but future work is required with fine-grained assessments to more rigorously evaluate co-use.
Footnotes
This work was funded by Grants R03AA025449 (principal investigator: Jason E. Goldstick), R01DA024646 (principal investigator: Rebecca M. Cunningham), and R49 CE003085 (principal investigator: Rebecca M. Cunningham).
References
- Allison P. D., Waterman R. P. Fixed-effects negative binomial regression models. Sociological Methodology. 2002;32:247–265. doi:10.1111/1467-9531.00117. [Google Scholar]
- Baggio S., Deline S., Studer J., N’Goran A., Mohler-Kuo M., Daeppen J.-B., Gmel G. Concurrent versus simultaneous use of alcohol and non-medical use of prescription drugs: Is simultaneous use worse for mental, social, and health issues? Journal of Psychoactive Drugs. 2014;46:334–339. doi: 10.1080/02791072.2014.921747. doi:10.1080/02791072.2014.921747. [DOI] [PubMed] [Google Scholar]
- Bohnert K. M., Walton M. A., Ranney M., Bonar E. E., Blow F. C., Zimmerman M. A., Cunningham R. M. Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban emergency department. Addictive Behaviors. 2015;41:97–105. doi: 10.1016/j.addbeh.2014.09.019. doi:10.1016/j.addbeh.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar E. E., Coughlin L., Roche J. S., Philyaw-Kotov M. L., Bixler E. A., Sinelnikov S., Walton M. A. Prescription opioid misuse among adolescents and emerging adults in the United States: A scoping review. Preventive Medicine. 2020;132:105972. doi: 10.1016/j.ypmed.2019.105972. doi:10.1016/j.ypmed.2019.105972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecological models of human development. In: Gauvain M., Cole M., editors. International encyclopedia of education. Readings on the development of children. 2nd ed. Vol. 3. Oxford, England: Elsevier; New York, NY: Freeman; 1994. pp. 37–43. Retrieved from https://impactofspecialneeds.weebly.com/uploads/3/4/1/9/3419723/ecologial_models_of_human_development.pdf. [Google Scholar]
- Bush K., Kivlahan D. R., McDonell M. B., Fihn S. D., Bradley K. A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP) Alcohol Use Disorders Identification Test. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. doi:10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Cunningham R. M., Carter P. M., Ranney M., Zimmerman M. A., Blow F. C., Booth B. M., Walton M. A. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: A 2-year prospective cohort study. JAMA Pediatrics. 2015a;169:63–70. doi: 10.1001/jamapediatrics.2014.1900. doi:10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham R. M., Chermack S. T., Ehrlich P. F., Carter P. M., Booth B. M., Blow F. C., Walton M. A. Alcohol interventions among underage drinkers in the ED: A randomized controlled trial. Pediatrics. 2015b;136:e783–e793. doi: 10.1542/peds.2015-1260. doi:10.1542/peds.2015-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Grant B. F., Stinson F. S., Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical and Experimental Research. 2005;29:844–854. doi: 10.1097/01.alc.0000164374.32229.a2. doi:10.1097/01.ALC.0000164374.32229.A2. [DOI] [PubMed] [Google Scholar]
- Egan K. L., Reboussin B. A., Blocker J. N., Wolfson M., Sutfin E. L. Simultaneous use of non-medical ADHD prescription stimulants and alcohol among undergraduate students. Drug and Alcohol Dependence. 2013;131:71–77. doi: 10.1016/j.drugalcdep.2012.12.004. doi:10.1016/j.drugalcdep.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg R. K., Fulton-Kehoe D., Franklin G. M. Patterns of opioid use and risk of opioid overdose death among Medicaid patients. Medical Care. 2017;55:661–668. doi: 10.1097/MLR.0000000000000738. doi:10.1097/MLR.0000000000000738. [DOI] [PubMed] [Google Scholar]
- Garmezy N.1991Resilience in children's adaptation to negative life events and stressed environments Pediatric Annals 20459–460. 463–466doi:10.3928/0090-4481-19910901-05 [DOI] [PubMed] [Google Scholar]
- Garnier L. M., Arria A. M., Caldeira K. M., Vincent K. B., O’Grady K. E., Wish E. D. Nonmedical prescription analgesic use and concurrent alcohol consumption among college students. American Journal of Drug and Alcohol Abuse. 2009;35:334–338. doi: 10.1080/00952990903075059. doi:10.1080/00952990903075059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick J. E., Bohnert K. M., Davis A. K., Bonar E. E., Carter P. M., Walton M. A., Cunningham R. M. Dual trajectories of depression/anxiety symptoms and alcohol use, and their implications for violence outcomes among drug-using urban youth. Alcohol and Alcoholism. 2018a;53:659–666. doi: 10.1093/alcalc/agy036. doi:10.1093/alcalc/agy036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick J. E., Heinze J., Ngo Q., Hsieh H.-F., Walton M. A., Cunningham R. M., Zimmerman M. A. Perceived peer behavior and parental support as correlates of marijuana use: The role of age and gender. Substance Use & Misuse. 2018b;53:521–531. doi: 10.1080/10826084.2017.1342660. doi:10.1080/10826084.2017.1342660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick J. E., Lyons V. H., Myers M. G., Walton M. A., Heinze J. E., Cunningham R. M. Within- and between-person associations with drug use disorder among adolescents and emerging adults presenting to an urban emergency department. Drug and Alcohol Dependence. 2021;221:108605. doi: 10.1016/j.drugalcdep.2021.108605. doi:10.1016/j.drugalcdep.2021.108605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick J. E., Walton M. A., Bohnert A. S. B., Heinze J. E., Cunningham R. M. Predictors of alcohol use transitions among drug-using youth presenting to an urban emergency department. PLoS One. 2019;14:e0227140. doi: 10.1371/journal.pone.0227140. doi:10.1371/journal.pone.0227140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunasekara F. I., Richardson K., Carter K., Blakely T. Fixed effects analysis of repeated measures data. International Journal of Epidemiology. 2014;43:264–269. doi: 10.1093/ije/dyt221. doi:10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- Hjorthøj C. R., Hjorthøj A. R., Nordentoft M. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances—systematic review and meta-analysis. Addictive Behaviors. 2012;37:225–233. doi: 10.1016/j.addbeh.2011.11.025. doi:10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Johnston L. D., O’Malley P., Bachman J., Schulenberg J., Miech R. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2014. Monitoring the Future national survey results on drug use 1975-2013. [Google Scholar]
- Lin L. A., Walton M. A., Bonar E. E., Blow F. C. Trajectories of nonmedical use of prescription opioids among adolescents in primary care. Addiction Research and Theory. 2016;24:514–520. doi:10.1080/1606 6359.2016.1178244. [Google Scholar]
- Maio R. F., Shope J. T., Blow F. C., Gregor M. A., Zakrajsek J. S., Weber J. E., Nypaver M. M. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Annals of Emergency Medicine. 2005;45:420–429. doi: 10.1016/j.annemergmed.2004.10.013. doi:10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Marschall-Lévesque S., Castellanos-Ryan N., Vitaro F., Séguin J. R. Moderators of the association between peer and target adolescent substance use. Addictive Behaviors. 2014;39:48–70. doi: 10.1016/j.addbeh.2013.09.025. doi:10.1016/j.addbeh.2013.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S. E., Cranford J. A., Morales M., Young A. Simultaneous and concurrent polydrug use of alcohol and prescription drugs: Prevalence, correlates, and consequences. Journal of Studies on Alcohol. 2006;67:529–537. doi: 10.15288/jsa.2006.67.529. doi:10.15288/jsa.2006.67.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S. E., West B. T., Schepis T. S., Teter C. J. Simultaneous co-ingestion of prescription stimulants, alcohol and other drugs: A multi-cohort national study of US adolescents. Human Psychopharmacology. 2015;30:42–51. doi: 10.1002/hup.2449. doi:10.1002/hup.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S. E., West B. T., Teter C. J., Boyd C. J. Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug and Alcohol Dependence. 2012;126:65–70. doi: 10.1016/j.drugalcdep.2012.04.017. doi:10.1016/j.drugalcdep.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh R. K., Votaw V. R., Sugarman D. E., Greenfield S. F. Sex and gender differences in substance use disorders. Clinical Psychology Review. 2018;66:12–23. doi: 10.1016/j.cpr.2017.10.012. doi:10.1016/j.cpr.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Prescription drug abuse. 2001 Retrieved from https://www.drugabuse.gov/sites/default/files/rxreportfinalprint.pdf. [Google Scholar]
- Piersma H. L., Reaume W. M., Boes J. L. The Brief Symptom Inventory (BSI) as an outcome measure for adult psychiatric inpatients. Journal of Clinical Psychology. 1994;50:555–563. doi: 10.1002/1097-4679(199407)50:4<555::aid-jclp2270500410>3.0.co;2-g. doi:10.1002/1097-4679(199407)50:4<555::AID-JCLP2270500410>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Procidano M. E., Heller K. Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology. 1983;11:1–24. doi: 10.1007/BF00898416. doi:10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Roy É., Nolin M.-A., Traoré I., Leclerc P., Vasiliadis H.-M. Nonmedical use of prescription medication among adolescents using drugs in Quebec. Canadian Journal of Psychiatry. 2015;60:556–563. doi: 10.1177/070674371506001206. doi:10.1177/070674371506001206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. doi:10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Sallis J., Owen N., Fisher E. B.2008Ecological models of health behavior In Glanz K., Rimer B. K., Viswanath K. (Eds.), Health behavior and health education: Theory, research, and practice (pp. 465–485.)San Francisco, CA: Jossey-Bass; Retrieved from https://edc.iums.ac.ir/files/hshe-soh/files/beeduhe_0787996149.pdf#page=503 [Google Scholar]
- Schepis T. S., Ford J. A., Wilens T. E., Teter C. J., McCabe S. E. Differences in prescription stimulant misuse motives across adolescents and young adults in the United States. Journal of Clinical Psychiatry. 2020;81:20m13302. doi: 10.4088/JCP.20m13302. doi:10.4088/JCP.20m13302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis T. S., Teter C. J., Simoni-Wastila L., McCabe S. E. Prescription tranquilizer/sedative misuse prevalence and correlates across age cohorts in the US. Addictive Behaviors. 2018;87:24–32. doi: 10.1016/j.addbeh.2018.06.013. doi:10.1016/j.addbeh.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis T. S., West B. T., Teter C. J., McCabe S. E. Prevalence and correlates of co-ingestion of prescription tranquilizers and other psychoactive substances by U.S. high school seniors: Results from a national survey. Addictive Behaviors. 2016;52:8–12. doi: 10.1016/j.addbeh.2015.08.002. doi:10.1016/j.addbeh.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L. C., Maisto S. A., Sobell M. B., Cooper A. M. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. doi:10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Stoddard S. A., Epstein-Ngo Q., Walton M. A., Zimmerman M. A., Chermack S. T., Blow F. C., Cunningham R. M. Substance use and violence among youth: A daily calendar analysis. Substance Use & Misuse. 2015;50:328–339. doi: 10.3109/10826084.2014.980953. doi:10.3109/10826084.2014.980953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone A. L., Becker L. G., Huber A. M., Catalano R. F. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. doi:10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) 2019 NSDUH detailed tables. 2020a. Retrieved from https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables.
- Substance Abuse and Mental Health Services Administration (SAM HSA)(2020b2019 National Survey of Drug Use and Health (NSDUH) releases Retrieved from https://www.samhsa.gov/data/release/2019-national-survey-drug-use-and-health-nsduh-releases
- Sudhinaraset M., Wigglesworth C., Takeuchi D. T. Social and cultural contexts of alcohol use: Influences in a social–ecological framework. Alcohol Research: Current Reviews. 2016;38:35–45. [PMC free article] [PubMed] [Google Scholar]
- Sussman S., Arnett J. J. Emerging adulthood: Developmental period facilitative of the addictions. Evaluation & the Health Professions. 2014;37:147–155. doi: 10.1177/0163278714521812. doi:10.1177/0163278714521812. [DOI] [PubMed] [Google Scholar]
- van der Schrier R., Roozekrans M., Olofsen E., Aarts L., van Velzen M., de Jong M., Niesters M. Influence of ethanol on oxycodone-induced respiratory depression: A dose-escalating study in young and elderly individuals. Anesthesiology. 2017;126:534–542. doi: 10.1097/ALN.0000000000001505. doi:10.1097/ALN.0000000000001505. [DOI] [PubMed] [Google Scholar]
- Viana A. G., Trent L., Tull M. T., Heiden L., Damon J. D., Hight T. L., Young J. Non-medical use of prescription drugs among Mississippi youth: Constitutional, psychological, and family factors. Addictive Behaviors. 2012;37:1382–1388. doi: 10.1016/j.addbeh.2012.06.017. doi:10.1016/j.addbeh.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Walton M. A., Epstein-Ngo Q., Carter P. M., Zimmerman M. A., Blow F. C., Buu A., Cunningham R. M. Marijuana use trajectories among drug-using youth presenting to an urban emergency department: Violence and social influences. Drug and Alcohol Dependence. 2017;173:117–125. doi: 10.1016/j.drugalcdep.2016.11.040. doi:10.1016/j.drugalcdep.2016.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. doi:10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Zimmerman M. A., Caldwell C. H., Bernat D. H. Discrepancy between self report and school record grade point average: Correlates with psychosocial outcomes among African American adolescents. Journal of Applied Social Psychology. 2002;32:86–109. doi:10.1111/j.1559-1816.2002.tb01421.x. [Google Scholar]