Abstract
Objective:
Self-reported alcohol consumption in U.S. public health surveys covers only 30%–60% of per capita alcohol sales, based on tax and shipment data. To estimate alcohol-attributable harms using alcohol-attributable fractions, accurate measures of total population consumption and the distribution of this drinking are needed. This study compared methodological approaches of adjusting self-reported survey data on alcohol consumption to better reflect sales and assessed the impact of these adjustments on the distribution of average daily consumption (ADC) levels and the number of alcohol-attributable deaths.
Method:
Prevalence estimates of ADC levels (i.e., low, medium, and high) among U.S. adults who responded to the 2011–2015 Behavioral Risk Factor Surveillance System (BRFSS; N = 2,198,089) were estimated using six methods. BRFSS ADC estimates were adjusted using the National Alcohol Survey, per capita alcohol sales data (from the Alcohol Epidemiologic Data System), or both. Prevalence estimates for the six methods were used to estimate average annual alcohol-attributable deaths, using a population-attributable fraction approach.
Results:
Self-reported ADC in the BRFSS accounted for 31.3% coverage of per capita alcohol sales without adjustments, 36.1% using indexed-BRFSS data, and 44.3% with National Alcohol Survey adjustments. Per capita sales adjustments decreased low ADC prevalence estimates and increased medium and high ADC prevalence estimates. Estimated alcohol-attributable deaths ranged from approximately 91,200 per year (BRFSS unadjusted; Method 1) to 125,200 per year (100% of per capita sales adjustment; Method 6).
Conclusions:
Adjusting ADC to reflect total U.S. alcohol consumption (e.g., adjusting to 73% of per capita sales) has implications for assessing the impact of excessive drinking on health outcomes, including alcohol-attributable death estimates.
Alcohol consumption is associated with increases in all-cause mortality (Global Burden of Disease 2016 Alcohol Collaborators, 2018; Wood et al., 2018), and excessive drinking is a leading preventable cause of death in the United States (Mokdad et al., 2018) and globally (World Health Organization, 2018). Accurate measures of population-level alcohol consumption and the distribution and pattern of drinking are necessary to estimate the public health impact of excessive drinking. For example, studies that use the population-attributable fraction methodology to estimate deaths attributable to alcohol rely on prevalence estimates of alcohol use at various levels of consumption, and relative risks on the relationship between average daily consumption (ADC) and the risk of death from alcohol-related health conditions (Nelson et al., 2013; Rey et al., 2010). However, self-reported alcohol consumption in U.S. public health surveys generally only accounts for 30%–60% of presumed consumption from per capita alcohol sales, based on tax and shipment data (Kerr & Greenfield, 2007; Nelson et al., 2010; Parish et al., 2017), resulting in conservative estimates of the alcohol-related public health impact.
There are many reasons for underreporting of alcohol consumption in surveys, underscoring the importance of correction. First, respondents may not accurately estimate their consumption using the U.S. definition of a “standard drink” (i.e., 14.0 grams of pure ethanol, which generally equates to a 12 ounce beer, a 5 ounce glass of wine, or a drink with 1.5 ounces of distilled spirits) (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015). Second, accuracy of self-reported consumption may be affected by recall and social desirability biases (Stockwell et al., 2004). Third, population-level alcohol consumption estimated using survey data may be lower than estimates from per capita alcohol sales data because of selection biases in participation (Kopra et al., 2018) and people who decline to participate (Tolonen et al., 2019). Surveys might not capture alcohol consumption by some populations who may drink excessively but are not reached (e.g., persons who are homeless or institutionalized) (Christensen et al., 2015; Karvanen et al., 2016).
Although it is known that surveys tend to underestimate the total amount of alcohol consumed in a population, they are necessary to assess the distribution of alcohol use. The Centers for Disease Control and Prevention's (2020a) Alcohol-Related Disease Impact (ARDI) application estimates alcohol-attributable deaths in the United States and for each state using the population-attributable fraction methodology for 58 different causes of death. In general, the alcohol-attributable fractions for chronic causes of death are based on the prevalence of ADC at three levels of drinking (low, medium, and high) and the condition specific–associated relative risk of dying at that level of consumption (Esser et al., 2020b).
The ADC prevalence estimates in ARDI are based on the Behavioral Risk Factor Surveillance System (BRFSS; Centers for Disease Control and Prevention, 2017). The BRFSS is the only state-based survey used throughout the United States that obtains information on alcohol consumption; however, it yields a lower coverage of per capita alcohol consumption and lower prevalence estimates of higher levels of consumption than other U.S. national surveys (Esser et al., 2020a; Kerr & Greenfield, 2007; Nelson et al., 2010; Parish et al., 2017). BRFSS alcohol data only account for a median of 22%–32% of state alcohol sales, depending on the state (Nelson et al., 2010). To partially correct for the under-reporting of consumption among BRFSS respondents, ADC prevalence estimates in ARDI are adjusted using an indexing method to account for binge drinking episodes, as people tend not to take binge drinking occasions into account when reporting on usual consumption (Stahre et al., 2006).
In contrast to using survey data, estimating population-level alcohol consumption using alcohol sales, tax, and shipment data generally reflects the total alcohol consumed within populations. However, such data do not inform the distribution of ADC or drinking patterns across the population. The World Health Organization and Global Burden of Disease studies correct for survey-based underreporting of alcohol consumption using data on per capita alcohol sales, and adjust survey data to 80% of reported per capita alcohol sales (Rehm et al., 2010; Shield et al., 2020; Stockwell et al., 2018; World Health Organization, 2018). Similar methods have also been used by other researchers. For example, a French study adjusted survey-based alcohol consumption estimates using ratios of per capita alcohol sales and sexspecific alcohol consumption across age groups (Rey et al., 2010).
Sales-based adjustments may be useful when calculating ADC from the BRFSS for generating estimates of alcohol-related harms, including deaths in ARDI. The methods are widely used (Rehm et al., 2010; Rey et al., 2010; Shield et al., 2020), and per capita sales are correlated with population-level harms (Rehm et al., 2020). Therefore, the purpose of this methodological study was to compare approaches for estimating the national prevalence of ADC levels based on U.S. adults’ responses to alcohol consumption questions in the BRFSS, using survey-based adjustments, per capita sales adjustments, or both. This study also examined differences in the national-level distribution of drinks consumed by ADC levels and assessed the impact of ADC adjustments on estimates of the average annual number of alcohol-attributable deaths in the United States.
Method
Data sources
Behavioral Risk Factor Surveillance System
The BRFSS is a state-based telephone survey of non-institutionalized, U.S. adults ages 18 years and older, conducted in all states, the District of Columbia, and U.S. territories. It is conducted monthly via random-digit dialing. Details of the BRFSS methodology have been published (Centers for Disease Control and Prevention, 2017). The BRFSS collects data on a range of health conditions and risk behaviors, including alcohol consumption. The 2011–2015 BRFSS surveys were used in this study to align with the years of data in ARDI, and the median response rates ranged from 45.2% to 49.7% (combined landline and cell phone samples). After excluding U.S. territories, the total BRFSS sample population (respondents with all necessary drinking information) included was 2,198,089. Four BRFSS questions on alcohol consumption during the past 30 days were used, including the number of drinking days, the average number of drinks consumed per drinking day, the frequency of binge drinking (≥4 drinks for women or ≥5 drinks for men, on an occasion), and the largest number of drinks consumed on any occasion.
National Alcohol Survey (NAS)
The NAS is a nationwide survey of non-institutionalized, civilian U.S. adults ages 18 years and older, conducted in all states and the District of Columbia that is administered every 5 years by the Alcohol Research Group of the Public Health Institute in California. The 2015 NAS was conducted via random-digit-dialing, computer-assisted telephone interviews conducted by ICF Macro, Inc. (Fairfax, VA) in 2014–2015, with a response rate of 43.4% (Karriker-Jaffe et al., 2017). Four respondents with incomplete information on alcohol consumption were excluded; the remaining 7,067 NAS respondents were included. The NAS collects detailed data on alcohol consumption and uses methods to reduce the magnitude of the underreporting of alcohol consumption (i.e., the graduated frequency approach) and to improve reports of higher levels of drinking (Greenfield, 2000). This approach removes the need for people to report an average number of drinks consumed across all drinking occasions (Rehm et al., 1999). As a result, previous iterations of the NAS have accounted for about 50% of per capita alcohol sales (Kerr & Greenfield, 2007), and the NAS methods for measuring higher levels of drinking are more sensitive than the BRFSS’ quantity–frequency approach (Esser et al., 2020a). Therefore, NAS drinking distribution estimates were evaluated as possible adjustment factors for the BRFSS ADC prevalence estimates (details below).
Alcohol sales data
Data for annual population-level apparent consumption for the United States (hereinafter referred to as “per capita sales”) were obtained from the National Institute on Alcohol Abuse and Alcoholism's (2017) Alcohol Epidemiologic Data System (AEDS). This system extracts the volume of each beverage type sold annually in each state from sales receipts reports and shipment data from state government and industry sources (National Institute on Alcohol Abuse and Alcoholism, 2017; Slater & Alpert, 2019). Per capita sales were derived by summing beverage-specific consumption and dividing by the number of persons in the United States in 2015 who were at least 18 years old.
ADC adjustment methods
Data from adults who responded to the 2011–2015 BRFSS were used to estimate the prevalence of ADC (Centers for Disease Control and Prevention, 2020b; Esser et al., 2020b). The prevalence of low, medium, and high ADC was calculated overall, by sex, and by four sex–age strata (men and women, ages 18–44 and ≥45 years). Six methods were used to calculate ADC prevalence estimates. The first method used unadjusted BRFSS ADC prevalence estimates, and the other five methods applied adjustments to the ADC prevalence estimates.
(A) METHOD 1, BRFSS UNADJUSTED: In Method 1, the ADC for each BRFSS respondent was determined by multiplying the proportion of days that alcohol was consumed by the average number of drinks consumed on drinking days (i.e., the quantity–frequency method). After calculating each respondent's ADC, the weighted prevalence of low ADC (>0–1 drink of alcohol for women or >0–2 drinks for men), medium ADC (>1–2 drinks for women or >2–4 drinks for men), and high ADC (>2 drinks for women or >4 drinks for men) was calculated by sex and for the four sex–age strata. The cut-points for defining the three ADC levels are consistent with ARDI (Centers for Disease Control and Prevention, 2020b).
(B) METHOD 2, BRFSS ADJUSTED USING INDEXING: In Method 2, the current ARDI indexing method was used to include information on binge drinking episodes in the ADC calculation because binge drinking is often underreported in measures of usual consumption (Centers for Disease Control and Prevention, 2020b; Stahre et al., 2006). First, among each binge drinker, binge drinking days were separated from non–binge drinking days such that the number of binge drinking days was subtracted from the total number of drinking days, and then this recalculated drinking frequency was multiplied by the number of drinks consumed on usual drinking days. Second, the reported binge drinking frequency was multiplied by the largest number of drinks consumed to account for underreporting during binge drinking episodes. The two quantity–frequency measures were then recombined to calculate each binge drinking respondent's ADC. The weighted prevalence estimates by ADC levels were then calculated, as in Method 1.
(C) METHOD 3, BRFSS ADJUSTED TO NAS: In Method 3, BRFSS ADC estimates were adjusted using NAS, allowing for differential adjustments by respondents’ sex and age because the underreporting of alcohol consumption in surveys might vary by these characteristics (Boniface et al., 2014; Northcote & Livingston, 2011). Within each of four sex–age groups, NAS-BRFSS adjustment factors were calculated representing the subgroup's average ADC in NAS divided by the subgroup's average ADC in BRFSS. These adjustment factors were then applied to the BRFSS at the individual level, based on the sex and age group of the respondent. Within each sex–age group, individual-level BRFSS ADC was multiplied by the ratio of NAS to BRFSS ADC estimates, shifting the ADC distribution. For each sex–age group, the weighted prevalence estimates by levels of ADC were then calculated using the same established cut-points for defining each ADC level, as in Method 1.
(D) METHOD 4, BRFSS ADJUSTED TO NAS AND 73% OF PER CAPITA SALES: In Method 4, both NAS and per capita sales data were used to complete a double-step adjustment. The first step was equivalent to Method 3. The second step further adjusted the resulting Method 3 national ADC estimates to 73% of national per capita sales by multiplying each respondent's ADC by the ratio of per capita consumption to NAS-adjusted consumption. The 73% multiplier was selected to match the coverage of per capita sales (from the AEDS) that is achieved in epidemiological cohort studies used to derive condition-specific relative risk estimates (Stockwell et al., 2018). Specifically, data from U.S. cohort studies yield an estimated 6.5 liters per capita annual alcohol consumption, and the AEDS reported an average of 8.9 liters per capita alcohol consumption based on alcohol sales (National Institute on Alcohol Abuse and Alcoholism, 2017; Stockwell et al., 2018). After adjusting for percent alcohol by volume, total annual per capita drinks consumed was 497.6 (Martinez et al., 2019).
(E) METHOD 5, BRFSS ADJUSTED TO 73% OF PER CAPITA SALES: In Method 5, individual-level ADC estimates from the BRFSS were directly adjusted by a factor that corrected the overall ADC to 73% of national per capita sales, without the NAS survey-based adjustment.
(F) METHOD 6, BRFSS ADJUSTED TO 100% PER CAPITA SALES: Finally, in Method 6, individual-level BRFSS ADC estimates were multiplied by a factor that adjusted the overall ADC to 100% of national per capita sales (rather than to 73% as in Method 5).
For all methods, once these ADC adjustments were completed, the weighted prevalence of low, medium, and high ADC were calculated for men and women, resulting in six sets of ADC prevalence estimates for each method. Using each method, the number of annual drinks consumed per capita was calculated overall and within ADC levels, and by sex and among the sex–age strata.
Calculating alcohol-attributable fractions and deaths
Alcohol-attributable fractions, by sex, were calculated for each of 58 alcohol-related conditions in ARDI (Centers for Disease Control and Prevention, 2020b). Deaths from acute conditions included in ARDI (e.g., motor vehicle traffic crashes, other unintentional injuries) are calculated using direct estimates of alcohol involvement from meta-analyses or large surveillance systems (Blair et al., 2016; National Highway Traffic Safety Administration, 2020; Smith et al., 1999). Conditions fully attributable to alcohol (e.g., alcoholic liver cirrhosis) have an alcohol-attributable fraction of 1.0. Alcohol-attributable fractions for both acute and fully attributable conditions are unaffected by the ADC prevalence adjustment methods described above; therefore, the estimated number of alcohol-attributable deaths for these causes are also not affected by ADC prevalence adjustments.
There are 23 chronic conditions in ARDI that are calculated using ADC estimates and alcohol-attributable fractions. The methods used to calculate these alcohol-attributable fractions are detailed elsewhere (Centers for Disease Control and Prevention, 2020b). In brief, alcohol-attributable fractions were based on the six sets of ADC prevalence estimates among U.S. adults (overall, by sex, and among sex–age strata) and the relative risk of dying at corresponding ADC levels (Centers for Disease Control and Prevention, 2020b). The relative risk estimates in this study were consistent with those used in ARDI, based on published meta-analyses of cohort studies of alcohol and causes of death (e.g., cancer [Bagnardi et al., 2015], coronary heart disease [Zhao et al., 2017]). Deaths from excessive alcohol use were estimated in this study (as opposed to deaths from any alcohol use), using corresponding medium and high levels of ADC prevalence estimates and relative risks (RRs). The following alcohol-attributable fraction formula was used:
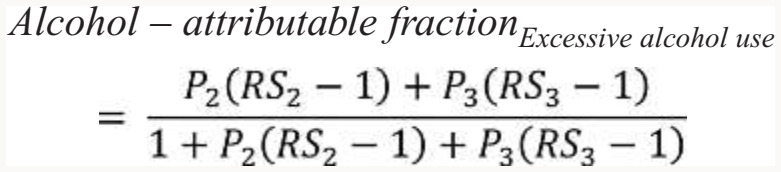 |
P2 is the prevalence of medium ADC, and P3 is the prevalence of high ADC. Condition-specific RR at medium and high levels of ADC were rescaled (RS) relative to the low ADC group (RR1) and calculated for the medium 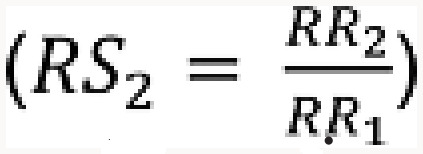 and high consumption groups
and high consumption groups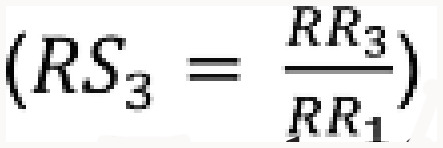 .
.
To estimate the average annual number of deaths from excessive drinking during 2011–2015 overall and by sex, alcohol-attributable fractions were applied to total deaths from alcohol-related causes reported in the National Vital Statistics System (Centers for Disease Control and Prevention, 2020a, 2020b). Alcohol-attributable fractions were applied to the specific causes of death, and alcohol-attributable deaths estimates were grouped, summed, and then reported in the nine categories of causes of death used in ARDI. Estimates of the average annual number of deaths were rounded to the nearest hundred because the results reflect aggregated estimates. Percentage changes in total average annual alcohol-attributable deaths from chronic conditions were estimated relative to the unadjusted BRFSS approach (Method 1). All analyses were conducted using SAS Version 9.4 (SAS Institute Inc., Cary, NC).
Results
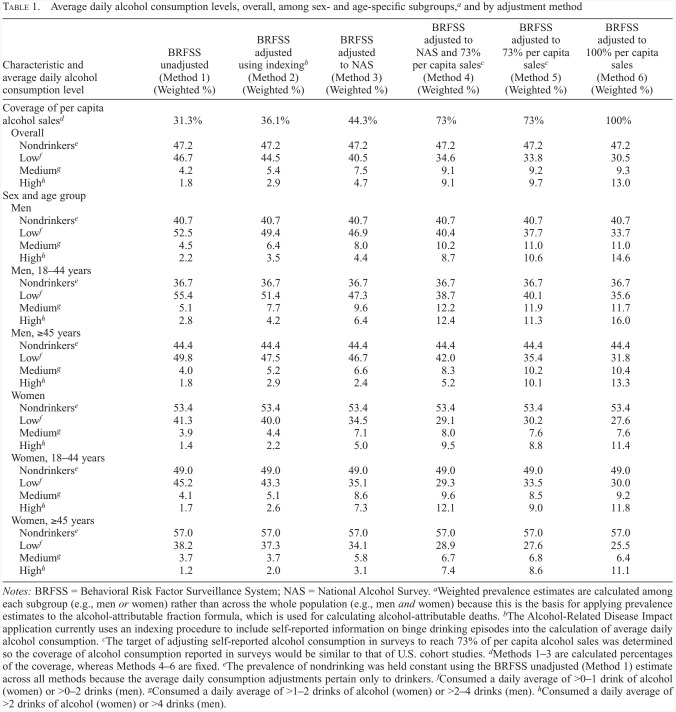
Methods 1–3 estimated ADC from BRFSS using survey data exclusively. BRFSS self-reported ADC data accounted for 31.3% of per capita alcohol sales without adjustments (Method 1), 36.1% using indexing (Method 2), and 44.3% adjusted to NAS (Method 3, Table 1). Compared with ADC estimates based on survey data alone (Methods 1–3), ADC estimates adjusted using per capita sales data (Methods 4–6) generally decreased low ADC prevalence estimates and increased medium and high estimates. For example, using the current ARDI method of indexing (Method 2), the overall prevalence of low ADC was 44.5%, medium ADC was 5.4%, and high ADC was 2.9%. When adjusted to the NAS and 73% of per capita sales (Method 4), the prevalence of low ADC was 34.6%, medium ADC was 9.1%, and high ADC was 9.1%. Similarly, when ADC was adjusted to 73% of per capita sales (Method 5), the prevalence of low ADC was 33.8%, medium ADC was 9.2%, and high ADC was 9.7%.
Table 1.
Average daily alcohol consumption levels, overall, among sex- and age-specific subgroups,a and by adjustment method
| Characteristic and average daily alcohol consumption level | BRFSS unadjusted (Method 1) (Weighted %) | BRFSS adjusted using indexingb (Method 2) (Weighted %) | BRFSS adjusted to NAS (Method 3) (Weighted %) | BRFSS adjusted to NAS and 73% per capita salesc (Method 4) (Weighted %) | BRFSS adjusted to 73% per capita salesc (Method 5) (Weighted %) | BRFSS adjusted to 100% per capita sales (Method 6) (Weighted %) |
|---|---|---|---|---|---|---|
| Coverage of per capita alcohol salesd | 31.3% | 36.1% | 44.3% | 73% | 73% | 100% |
| Overall | ||||||
| Nondrinkerse | 47.2 | 47.2 | 47.2 | 47.2 | 47.2 | 47.2 |
| Lowf | 46.7 | 44.5 | 40.5 | 34.6 | 33.8 | 30.5 |
| Mediumg | 4.2 | 5.4 | 7.5 | 9.1 | 9.2 | 9.3 |
| Highh | 1.8 | 2.9 | 4.7 | 9.1 | 9.7 | 13.0 |
| Sex and age group | ||||||
| Men | ||||||
| Nondrinkerse | 40.7 | 40.7 | 40.7 | 40.7 | 40.7 | 40.7 |
| Lowf | 52.5 | 49.4 | 46.9 | 40.4 | 37.7 | 33.7 |
| Mediumg | 4.5 | 6.4 | 8.0 | 10.2 | 11.0 | 11.0 |
| Highh | 2.2 | 3.5 | 4.4 | 8.7 | 10.6 | 14.6 |
| Men, 18-44 years | ||||||
| Nondrinkerse | 36.7 | 36.7 | 36.7 | 36.7 | 36.7 | 36.7 |
| Lowf | 55.4 | 51.4 | 47.3 | 38.7 | 40.1 | 35.6 |
| Mediumg | 5.1 | 7.7 | 9.6 | 12.2 | 11.9 | 11.7 |
| Highh | 2.8 | 4.2 | 6.4 | 12.4 | 11.3 | 16.0 |
| Men, >45 years | ||||||
| Nondrinkerse | 44.4 | 44.4 | 44.4 | 44.4 | 44.4 | 44.4 |
| Lowf | 49.8 | 47.5 | 46.7 | 42.0 | 35.4 | 31.8 |
| Mediumg | 4.0 | 5.2 | 6.6 | 8.3 | 10.2 | 10.4 |
| Highh | 1.8 | 2.9 | 2.4 | 5.2 | 10.1 | 13.3 |
| Women | ||||||
| Nondrinkerse | 53.4 | 53.4 | 53.4 | 53.4 | 53.4 | 53.4 |
| Lowf | 41.3 | 40.0 | 34.5 | 29.1 | 30.2 | 27.6 |
| Mediumg | 3.9 | 4.4 | 7.1 | 8.0 | 7.6 | 7.6 |
| Highh | 1.4 | 2.2 | 5.0 | 9.5 | 8.8 | 11.4 |
| Women, 18-44 years | ||||||
| Nondrinkerse | 49.0 | 49.0 | 49.0 | 49.0 | 49.0 | 49.0 |
| Lowf | 45.2 | 43.3 | 35.1 | 29.3 | 33.5 | 30.0 |
| Mediumg | 4.1 | 5.1 | 8.6 | 9.6 | 8.5 | 9.2 |
| Highh | 1.7 | 2.6 | 7.3 | 12.1 | 9.0 | 11.8 |
| Women, >45 years | ||||||
| Nondrinkerse | 57.0 | 57.0 | 57.0 | 57.0 | 57.0 | 57.0 |
| Lowf | 38.2 | 37.3 | 34.1 | 28.9 | 27.6 | 25.5 |
| Mediumg | 3.7 | 3.7 | 5.8 | 6.7 | 6.8 | 6.4 |
| Highh | 1.2 | 2.0 | 3.1 | 7.4 | 8.6 | 11.1 |
Notes: BRFSS = Behavioral Risk Factor Surveillance System; NAS = National Alcohol Survey.
Weighted prevalence estimates are calculated among each subgroup (e.g., men or women) rather than across the whole population (e.g., men and women) because this is the basis for applying prevalence estimates to the alcohol-attributable fraction formula, which is used for calculating alcohol-attributable deaths.
The Alcohol-Related Disease Impact application currently uses an indexing procedure to include self-reported information on binge drinking episodes into the calculation of average daily alcohol consumption.
The target of adjusting self-reported alcohol consumption in surveys to reach 73% of per capita alcohol sales was determined so the coverage of alcohol consumption reported in surveys would be similar to that of U.S. cohort studies.
Methods 1–3 are calculated percentages of the coverage, whereas Methods 4–6 are fixed.
The prevalence of nondrinking was held constant using the BRFSS unadjusted (Method 1) estimate across all methods because the average daily consumption adjustments pertain only to drinkers.
Consumed a daily average of >0–1 drink of alcohol (women) or >0–2 drinks (men).
Consumed a daily average of >1–2 drinks of alcohol (women) or >2–4 drinks (men).
Consumed a daily average of >2 drinks of alcohol (women) or >4 drinks (men).
Although the overall prevalence of high ADC was smaller with the NAS adjustment coupled with the 73% of per capita sales adjustment (Method 4) than with the 73% of per capita sales adjustment alone (Method 5), the opposite pattern was found for men and women, ages 18–44 years. That is, among people ages 18–44 years, the prevalence of high ADC was larger with the NAS adjustment coupled with the 73% of per capita sales adjustment (Method 4) than with the 73% of per capita sales adjustment alone (Method 5). However, the high ADC prevalence estimates using per capita sales adjustments were consistently greater than estimates from approaches using survey data alone.
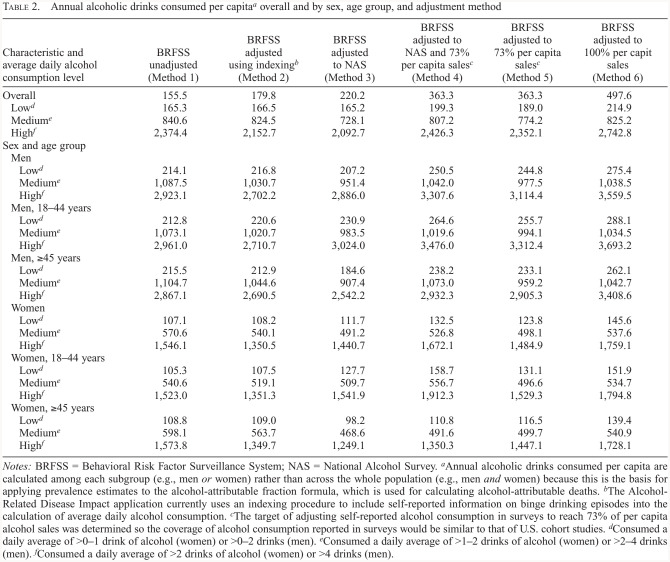
BRFSS unadjusted (Method 1) data corresponded to 155.5 alcoholic drinks consumed annually per capita (≥18 years), and 179.8 drinks consumed per capita using the indexing approach (Method 2), compared with 497.6 drinks per capita based on complete per capita sales data (Method 6) (Table 2). The BRFSS data accounted for 220.2 drinks per capita when ADC was adjusted to the NAS (Method 3) and 363.3 drinks per capita with adjustments to 73% of per capita sales (Methods 4 and 5). Annual per capita consumption among adults who drank at high levels of ADC ranged from 2,092.7 drinks (Method 3) to 2,742.8 (Method 6), or an average of 5.7 drinks/day (Method 3) to 7.5 drinks/day (Method 6).
Table 2.
Annual alcoholic drinks consumed per capitaa overall and by sex, age group, and adjustment method
| Characteristic and average daily alcohol consumption level | BRFSS unadjusted (Method 1) | BRFSS adjusted using indexingb (Method 2) | BRFSS adjusted to NAS (Method 3) | BRFSS adjusted to NAS and 73% per capita salesc(Method 4) | BRFSS adjusted to 73% per capita salesc (Method 5) | BRFSS adjusted to 100% per capit sales (Method 6) | |
|---|---|---|---|---|---|---|---|
| Overall | 155.5 | 179.8 | 220.2 | 363.3 | 363.3 | 497.6 | |
| Lowd | 165.3 | 166.5 | 165.2 | 199.3 | 189.0 | 214.9 | |
| Mediume | 840.6 | 824.5 | 728.1 | 807.2 | 774.2 | 825.2 | |
| Highf | 2,374.4 | 2,152.7 | 2,092.7 | 2,426.3 | 2,352.1 | 2,742.8 | |
| Sex and age group | |||||||
| Men | |||||||
| Lowd | 214.1 | 216.8 | 207.2 | 250.5 | 244.8 | 275.4 | |
| Mediume | 1,087.5 | 1,030.7 | 951.4 | 1,042.0 | 977.5 | 1,038.5 | |
| Highf | 2,923.1 | 2,702.2 | 2,886.0 | 3,307.6 | 3,114.4 | 3,559.5 | |
| Men, 18-44 years | |||||||
| Lowd | 212.8 | 220.6 | 230.9 | 264.6 | 255.7 | 288.1 | |
| Mediume | 1,073.1 | 1,020.7 | 983.5 | 1,019.6 | 994.1 | 1,034.5 | |
| Highf | 2,961.0 | 2,710.7 | 3,024.0 | 3,476.0 | 3,312.4 | 3,693.2 | |
| Men, >45 years | |||||||
| Lowd | 215.5 | 212.9 | 184.6 | 238.2 | 233.1 | 262.1 | |
| Mediume | 1,104.7 | 1,044.6 | 907.4 | 1,073.0 | 959.2 | 1,042.7 | |
| Highf | 2,867.1 | 2,690.5 | 2,542.2 | 2,932.3 | 2,905.3 | 3,408.6 | |
| Women | |||||||
| Lowd | 107.1 | 108.2 | 111.7 | 132.5 | 123.8 | 145.6 | |
| Mediume | 570.6 | 540.1 | 491.2 | 526.8 | 498.1 | 537.6 | |
| Highf | 1,546.1 | 1,350.5 | 1,440.7 | 1,672.1 | 1,484.9 | 1,759.1 | |
| Women, 18-44 years | |||||||
| Lowd | 105.3 | 107.5 | 127.7 | 158.7 | 131.1 | 151.9 | |
| Mediume | 540.6 | 519.1 | 509.7 | 556.7 | 496.6 | 534.7 | |
| Highf | 1,523.0 | 1,351.3 | 1,541.9 | 1,912.3 | 1,529.3 | 1,794.8 | |
| Women, >45 years | |||||||
| Lowd | 108.8 | 109.0 | 98.2 | 110.8 | 116.5 | 139.4 | |
| Mediume | 598.1 | 563.7 | 468.6 | 491.6 | 499.7 | 540.9 | |
| Highf | 1,573.8 | 1,349.7 | 1,249.1 | 1,350.3 | 1,447.1 | 1,728.1 | |
Notes: BRFSS = Behavioral Risk Factor Surveillance System; NAS = National Alcohol Survey.
Annual alcoholic drinks consumed per capita are calculated among each subgroup (e.g., men or women) rather than across the whole population (e.g., men and women) because this is the basis for applying prevalence estimates to the alcohol-attributable fraction formula, which is used for calculating alcohol-attributable deaths.
The Alcohol-Related Disease Impact application currently uses an indexing procedure to include self-reported information on binge drinking episodes into the calculation of average daily alcohol consumption.
The target of adjusting self-reported alcohol consumption in surveys to reach 73% of per capita alcohol sales was determined so the coverage of alcohol consumption reported in surveys would be similar to that of U.S. cohort studies.
Consumed a daily average of >0–1 drink of alcohol (women) or >0–2 drinks (men).
Consumed a daily average of >1–2 drinks of alcohol (women) or >2–4 drinks (men).
Consumed a daily average of >2 drinks of alcohol (women) or >4 drinks (men).
Relative to BRFSS without ADC adjustments (Method 1), the adjustment approaches had differential effects on estimated per capita consumption by ADC level, sex, and age group (Table 2). For example, among men age 45 years and older, BRFSS adjusted using indexing (Method 2) and adjustment to the NAS (Method 3) led to smaller per capita consumption estimates among those who drank at low or high ADC levels. Among women age 45 years and older who drank at high ADC levels, all adjustment approaches except adjustment to 100% of per capita sales led to smaller per capita consumption estimates compared with BRFSS without ADC adjustments (Method 1).
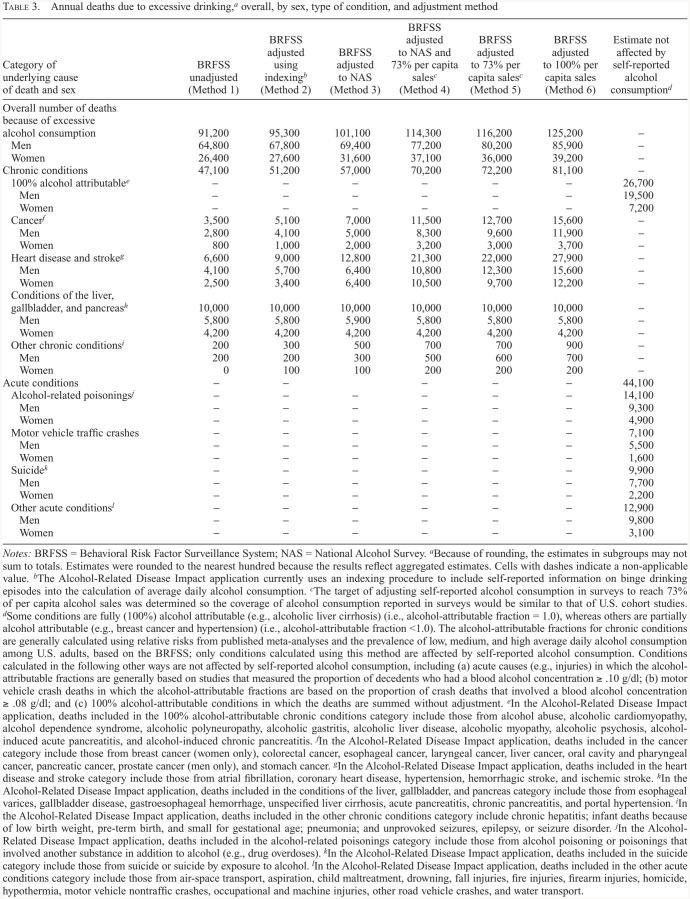
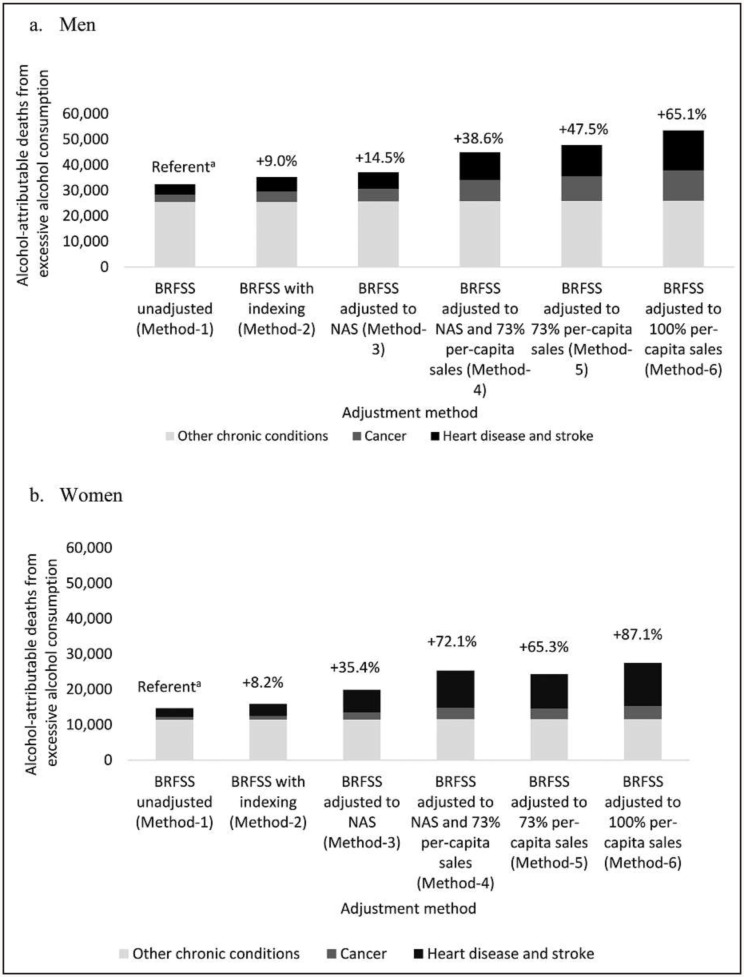
Estimated alcohol-attributable deaths in the United States ranged from approximately 91,200 per year (BRFSS unadjusted; Method 1) to approximately 125,200 per year (100% per capita sales adjustments; Method 6) (Table 3). The average annual number of alcohol-attributable deaths because of chronic conditions accounted for an increasing number and percentage of all alcohol-attributable deaths with each of the adjustment approaches, ranging from approximately 47,100 deaths from chronic conditions with unadjusted BRFSS (51.6% of all alcohol-attributable deaths; Method 1) to approximately 81,100 deaths from chronic conditions when adjusted to 100% of per capita sales (64.8% of all alcohol-attributable deaths; Method 6). Compared with the BRFSS unadjusted approach (Method 1), the percentage change in alcohol-attributable deaths from chronic conditions increased more with the per capita sales–based adjustments (e.g., 47.5% among men and 65.3% among women using Method 5) than with the survey-based adjustments (Figure 1).
Table 3.
Annual deaths due to excessive drinking,a overall, by sex, type of condition, and adjustment method
| Category of underlying cause of death and sex | BRFSS unadjusted (Method 1) | BRFSS adjusted using indexingb(Method 2) | BRFSS adjusted to NAS (Method 3) | BRFSS adjusted to NAS and 73% per capita salesc (Method 4) | BRFSS adjusted to 73% per capita salesc(Method 5) | BRFSS adjusted to 100% per capita sales (Method 6) | Estimate not affected by self-reported alcohol consumptiond |
|---|---|---|---|---|---|---|---|
| Overall number of deaths because of excessive | |||||||
| alcohol consumption | 91,200 | 95,300 | 101,100 | 114,300 | 116,200 | 125,200 | – |
| Men | 64,800 | 67,800 | 69,400 | 77,200 | 80,200 | 85,900 | – |
| Women | 26,400 | 27,600 | 31,600 | 37,100 | 36,000 | 39,200 | – |
| Chronic conditions | 47,100 | 51,200 | 57,000 | 70,200 | 72,200 | 81,100 | – |
| 100% alcohol attributablee | – | – | – | – | – | – | 26,700 |
| Men | – | – | – | – | – | – | 19,500 |
| Women | – | – | – | – | – | – | 7,200 |
| Cancerf | 3,500 | 5,100 | 7,000 | 11,500 | 12,700 | 15,600 | – |
| Men | 2,800 | 4,100 | 5,000 | 8,300 | 9,600 | 11,900 | – |
| Women | 800 | 1,000 | 2,000 | 3,200 | 3,000 | 3,700 | – |
| Heart disease and strokeg | 6,600 | 9,000 | 12,800 | 21,300 | 22,000 | 27,900 | – |
| Men | 4,100 | 5,700 | 6,400 | 10,800 | 12,300 | 15,600 | – |
| Women | 2,500 | 3,400 | 6,400 | 10,500 | 9,700 | 12,200 | – |
| Conditions of the liver, | |||||||
| gallbladder, and pancreash | 10,000 | 10,000 | 10,000 | 10,000 | 10,000 | 10,000 | – |
| Men | 5,800 | 5,800 | 5,900 | 5,800 | 5,800 | 5,800 | – |
| Women | 4,200 | 4,200 | 4,200 | 4,200 | 4,200 | 4,200 | – |
| Other chronic conditionsi | 200 | 300 | 500 | 700 | 700 | 900 | – |
| Men | 200 | 200 | 300 | 500 | 600 | 700 | – |
| Women | 0 | 100 | 100 | 200 | 200 | 200 | – |
| Acute conditions | – | – | – | – | – | 44,100 | |
| Alcohol-related poisoningsj | – | – | – | – | – | – | 14,100 |
| Men | – | – | – | – | – | – | 9,300 |
| Women | – | – | – | – | – | – | 4,900 |
| Motor vehicle traffic crashes | – | – | – | – | – | – | 7,100 |
| Men | – | – | – | – | – | – | 5,500 |
| Women | – | – | – | – | – | – | 1,600 |
| Suicidek | – | – | – | – | – | – | 9,900 |
| Men | – | – | – | – | – | – | 7,700 |
| Women | – | – | – | – | – | – | 2,200 |
| Other acute conditionsl | – | – | – | – | – | – | 12,900 |
| Men | – | – | – | – | – | – | 9,800 |
| Women | – | – | – | – | – | – | 3,100 |
Notes: BRFSS = Behavioral Risk Factor Surveillance System; NAS = National Alcohol Survey.
Because of rounding, the estimates in subgroups may not sum to totals. Estimates were rounded to the nearest hundred because the results reflect aggregated estimates. Cells with dashes indicate a non-applicable value.
The Alcohol-Related Disease Impact application currently uses an indexing procedure to include self-reported information on binge drinking episodes into the calculation of average daily alcohol consumption.
The target of adjusting self-reported alcohol consumption in surveys to reach 73% of per capita alcohol sales was determined so the coverage of alcohol consumption reported in surveys would be similar to that of U.S. cohort studies.
Some conditions are fully (100%) alcohol attributable (e.g., alcoholic liver cirrhosis) (i.e., alcohol-attributable fraction = 1.0), whereas others are partially alcohol attributable (e.g., breast cancer and hypertension) (i.e., alcohol-attributable fraction <1.0). The alcohol-attributable fractions for chronic conditions are generally calculated using relative risks from published meta-analyses and the prevalence of low, medium, and high average daily alcohol consumption among U.S. adults, based on the BRFSS; only conditions calculated using this method are affected by self-reported alcohol consumption. Conditions calculated in the following other ways are not affected by self-reported alcohol consumption, including (a) acute causes (e.g., injuries) in which the alcohol-attributable fractions are generally based on studies that measured the proportion of decedents who had a blood alcohol concentration ≥ .10 g/dl; (b) motor vehicle crash deaths in which the alcohol-attributable fractions are based on the proportion of crash deaths that involved a blood alcohol concentration ≥ .08 g/dl; and (c) 100% alcohol-attributable conditions in which the deaths are summed without adjustment.
In the Alcohol-Related Disease Impact application, deaths included in the 100% alcohol-attributable chronic conditions category include those from alcohol abuse, alcoholic cardiomyopathy, alcohol dependence syndrome, alcoholic polyneuropathy, alcoholic gastritis, alcoholic liver disease, alcoholic myopathy, alcoholic psychosis, alcohol-induced acute pancreatitis, and alcohol-induced chronic pancreatitis.
In the Alcohol-Related Disease Impact application, deaths included in the cancer category include those from breast cancer (women only), colorectal cancer, esophageal cancer, laryngeal cancer, liver cancer, oral cavity and pharyngeal cancer, pancreatic cancer, prostate cancer (men only), and stomach cancer.
In the Alcohol-Related Disease Impact application, deaths included in the heart disease and stroke category include those from atrial fibrillation, coronary heart disease, hypertension, hemorrhagic stroke, and ischemic stroke.
In the Alcohol-Related Disease Impact application, deaths included in the conditions of the liver, gallbladder, and pancreas category include those from esophageal varices, gallbladder disease, gastroesophageal hemorrhage, unspecified liver cirrhosis, acute pancreatitis, chronic pancreatitis, and portal hypertension.
In the Alcohol-Related Disease Impact application, deaths included in the other chronic conditions category include chronic hepatitis; infant deaths because of low birth weight, pre-term birth, and small for gestational age; pneumonia; and unprovoked seizures, epilepsy, or seizure disorder.
In the Alcohol-Related Disease Impact application, deaths included in the alcohol-related poisonings category include those from alcohol poisoning or poisonings that involved another substance in addition to alcohol (e.g., drug overdoses).
In the Alcohol-Related Disease Impact application, deaths included in the suicide category include those from suicide or suicide by exposure to alcohol.
In the Alcohol-Related Disease Impact application, deaths included in the other acute conditions category include those from air-space transport, aspiration, child maltreatment, drowning, fall injuries, fire injuries, firearm injuries, homicide, hypothermia, motor vehicle nontraffic crashes, occupational and machine injuries, other road vehicle crashes, and water transport.
Figure 1.
Sex-specific annual alcohol-attributable deaths from chronic conditions by adjustment method and category of cause of death. BRFSS = Behavioral Risk Factor Surveillance System; NAS = National Alcohol Survey. a The percent change in total alcohol-attributable deaths from chronic conditions indicated above each bar was calculated compared with the BRFSS unadjusted approach (Method 1).
Each subsequent adjustment approach generally led to increases in the estimated number of alcohol-attributable deaths among men and women (Table 3). However, among women, the estimated number of deaths was greater when using adjustments based on the NAS and 73% of per capita sales using Method 4 (37,100 deaths) than with the 73% of per capita sales adjustment alone using Method 5 (36,000 deaths). Increases in the number of alcohol-attributable deaths from various adjustment procedures were driven primarily by increases in deaths because of cancer and heart disease and stroke. For example, there were approximately 9,000 deaths from heart disease and stroke using the indexing approach in Method 2 (17.6% of all alcohol-attributable deaths from chronic conditions) and 22,000 deaths from heart disease and stroke when adjusted to 73% of per capita sales in Method 5 (30.5% of all deaths from chronic conditions).
Discussion
Relative to survey-based adjustments, this study found that the use of per capita sales adjustments, which reflect total alcohol consumed in the U.S. population, generally increased estimates of ADC that are based on usual alcohol consumption. Thus, after categorizing into ADC levels, the survey-based adjustments generally led to increases in the prevalence estimates of medium and high ADC. This resulted in greater proportions of the average annual number of U.S. alcohol-attributable deaths from chronic conditions and increased estimates of the total number of alcohol-attributable deaths in the United States.
The three adjustment methods using only existing survey data each have shortcomings. ADC accounted for less than 45% of per capita alcohol sales in each case, far below the adjustment to 80% of per capita alcohol sales used by the World Health Organization and studies of the Global Burden of Disease (Global Burden of Disease 2016 Alcohol Collaborators, 2018; Shield et al., 2020; Stockwell et al., 2018). Although the indexing method accounts for alcohol consumption during binge drinking episodes in estimates of ADC (Stahre et al., 2006), the underreporting of alcohol consumption during non-binge episodes is not addressed with this approach.
The NAS methodology improves estimates of self-reported alcohol consumption compared with the BRFSS, particularly among adults who drink at higher levels (Esser et al., 2020a). Adjustments to the BRFSS alcohol data using the NAS might be helpful in some contexts because there might be differences in the underreporting of alcohol by respondents’ characteristics. For example, among women, using Method 4 versus Method 5, the prevalence estimates for medium and high ADC were greater, as were the estimated alcohol-attributable deaths. However, correcting BRFSS ADC estimates using the NAS (alone or coupled with the per capita sales adjustments) to generate state-specific estimates of alcohol-attributable deaths is not ideal because NAS data are nationwide, whereas BRFSS and mortality data are available at the state level. Furthermore, the dual-adjustment calculation in Method 4 is complex and burdensome to calculate, which might create barriers for its use in practice.
Adjusting self-reported alcohol consumption in BRFSS to reflect population-level alcohol consumption based on per capita alcohol sales has implications for estimating alcohol-attributable deaths. It results in meaningful differences in estimates of alcohol-attributable deaths (especially deaths from cancer, heart disease, and stroke) compared with using survey data exclusively. As such, adjusting ADC prevalence estimates using per capita alcohol sales data seems to be an appropriate and practical method for estimating U.S. alcohol-attributable deaths. Although the World Health Organization and the Global Burden of Disease studies adjust data to 80% of per capita alcohol sales (Shield et al., 2020), this study conservatively adjusted to 73% of per capita alcohol sales to align with consumption reported among U.S. cohort study participants (Stockwell et al., 2018), thus corresponding with study populations that inform the relative risk of dying from a particular alcohol-related condition (Bagnardi et al., 2015; Patra et al., 2010; Zhao et al., 2017). This correction factor is intentionally conservative because some purchased alcohol is not consumed, as some may be stored, spilled, or used in cooking, or it may be consumed by people younger than 18 years. It is also conservative because unrecorded sales of alcohol and consumption of home-produced alcohol were not included.
Limitations
This study has some limitations. First, ADC adjustments using per capita alcohol sales were based on recorded alcohol sold and do not include unrecorded alcohol sales or home-produced alcohol. However, it is not expected that this inclusion would substantially change the findings because alcohol consumption from unrecorded sources in the United States is relatively low (Lachenmeier et al., 2011). Second, consistent with ARDI, the estimated number of alcohol-attributable deaths were based exclusively on the underlying cause of death from vital statistics to identify alcohol-related causes of death; therefore, contributing causes of death that might also be alcohol related were not included here (Esser et al., 2020b).
Conclusions
Estimates of ADC prevalence and alcohol-attributable deaths can be meaningfully adjusted to reflect total U.S. alcohol consumption more closely. Adjusting self-reported alcohol consumption among BRFSS respondents to 73% of per capita alcohol sales may be an appropriate and practical approach to account for the underreporting in surveys. Estimates generated using this method suggest that the annual number of alcohol-attributable deaths may be substantially greater than current state-specific and national estimates of alcohol-attributable deaths (Esser et al., 2020b). Improved estimates could further inform the rationale for and evaluation of effective population-level strategies for preventing excessive drinking and alcohol-attributable deaths, including those recommended by the Community Preventive Services Task Force (e.g., increasing alcohol taxes, regulating alcohol outlet density) (Campbell et al., 2009; Elder et al., 2010).
Conflict-of-Interest Statement
None of the authors have any conflicts of interest or financial disclosures.
Acknowledgments
The authors thank the Behavioral Risk Factor Surveillance System state coordinators and the National Alcohol Survey fieldwork team at ICF Macro, Inc., for assisting with data collection for those surveys. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Department of Health and Human Services. M. B. Esser, A. Sherk, J. J. Sacks, and T. Naimi conceptualized the study. M. B. Esser and T. Naimi led the drafting of the article. A. Sherk led the data analysis. M. S. Subbaraman and P. Martinez contributed to data analyses. All authors contributed to the interpretation of the findings, reviewed and edited drafts of the article, and approved the final version. K. J. Karriker-Jaffe was affiliated with the Alcohol Research Group as Director of the National Alcohol Survey for most of the duration of the study.
Footnotes
This research was supported in part by Cooperative Agreement numbers NU38OT000225 (for Jeffrey J. Sacks) and NU38OT000307 (for Timothy S. Naimi) from the Centers for Disease Control and Prevention. The National Alcohol Survey was supported in part by a grant from the National Institute on Alcohol Abuse and Alcoholism (P50 AA005595), which had no role in study design, data collection, data analysis, interpretation of results, or the decision to submit the paper for publication. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the U.S. Department of Health and Human Services.
References
- Bagnardi V., Rota M., Botteri E., Tramacere I., Islami F., Fedirko V., La Vecchia C. Alcohol consumption and site-specific cancer risk: A comprehensive dose–response meta-analysis. British Journal of Cancer. 2015;112:580–593. doi: 10.1038/bjc.2014.579. doi:10.1038/bjc.2014.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair J. M., Fowler K. A., Jack S. P., Crosby A. E. The National Violent Death Reporting System: Overview and future directions. Injury Prevention. 2016;22(Supplement 1):i6–i11. doi: 10.1136/injuryprev-2015-041819. doi:10.1136/injuryprev-2015-041819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boniface S., Kneale J., Shelton N. Drinking pattern is more strongly associated with under-reporting of alcohol consumption than socio-demographic factors: Evidence from a mixed-methods study. BMC Public Health. 2014;14:1297. doi: 10.1186/1471-2458-14-1297. doi:10.1186/1471-2458-14-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C. A., Hahn R. A., Elder R., Brewer R., Chattopadhyay S., Fielding J., Middleton J. C., & the Task Force on Community Preventive Services 2009The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms American Journal of Preventive Medicine 37556–569.doi:10.1016/j.amepre.2009.09.028 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2015 BRFSS Survey Data and Documentation. 2017. Retrieved from https://www.cdc.gov/brfss/annual_data/annual_2015.html.
- Centers for Disease Control and Prevention. Alcohol-Related Disease Impact (ARDI) application. 2020a. Retrieved from https://www.cdc.gov/ardi.
- Centers for Disease Control and Prevention 2020bARDI methods. Retrieved from https://www.cdc.gov/alcohol/ardi/methods.html
- Christensen A. I., Ekholm O., Gray L., Glümer C., Juel K. What is wrong with non-respondents? Alcohol-, drug- and smoking-related mortality and morbidity in a 12-year follow-up study of respondents and non-respondents in the Danish Health and Morbidity Survey. Addiction. 2015;110:1505–1512. doi: 10.1111/add.12939. doi:10.1111/add.12939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder R. W., Lawrence B., Ferguson A., Naimi T. S., Brewer R. D., Chattopadhyay S. K., Fielding J. E., & the Task Force on Community Preventive Services 2010The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms American Journal of Preventive Medicine 38217–229.doi:10.1016/j.amepre.2009.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser M. B., Sacks J. J., Sherk A., Karriker-Jaffe K. J., Greenfield T. K., Pierannunzi C., Brewer R. D. Distribution of drinks consumed by U.S. adults by average daily alcohol consumption: A comparison of 2 nationwide surveys. American Journal of Preventive Medicine. 2020a;59:669–677. doi: 10.1016/j.amepre.2020.04.018. doi:10.1016/j.amepre.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser M. B., Sherk A., Liu Y., Naimi T. S., Stockwell T., Stahre M., Brewer R. D. Deaths and years of potential life lost due to excessive alcohol use—United States, 2011–2015. Morbidity and Mortality Weekly Report. 2020b;69:1428–1433. doi: 10.15585/mmwr.mm6939a6. doi:10.15585/mmwr.mm6939a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Burden of Disease 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. doi:10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield T. K. Ways of measuring drinking patterns and the difference they make: Experience with graduated frequencies. Journal of Substance Abuse. 2000;12:33–49. doi: 10.1016/s0899-3289(00)00039-0. doi:S0899-3289(00)00039-0. [DOI] [PubMed] [Google Scholar]
- Karriker-Jaffe K. J., Greenfield T. K., Kaplan L. M. Distress and alcohol-related harms from intimates, friends, and strangers. Journal of Substance Use. 2017;22:434–441. doi: 10.1080/14659891.2016.1232761. doi:10.1080/14659891.2016.1232761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karvanen J., Tolonen H., Härkänen T., Jousilahti P., Kuulasmaa K. Selection bias was reduced by recontacting nonparticipants. Journal of Clinical Epidemiology. 2016;76:209–217. doi: 10.1016/j.jclinepi.2016.02.026. doi:10.1016/j.jclinepi.2016.02.026. [DOI] [PubMed] [Google Scholar]
- Kerr W. C., Greenfield T. K. Distribution of alcohol consumption and expenditures and the impact of improved measurement on coverage of alcohol sales in the 2000 National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2007;31:1714–1722. doi: 10.1111/j.1530-0277.2007.00467.x. doi:10.1111/j.1530-0277.2007.00467.x. [DOI] [PubMed] [Google Scholar]
- Kopra J., Mäkelä P., Tolonen H., Jousilahti P., Karvanen J. Follow-up data improve the estimation of the prevalence of heavy alcohol consumption. Alcohol and Alcoholism. 2018;53:586–596. doi: 10.1093/alcalc/agy019. doi:10.1093/alcalc/agy019. [DOI] [PubMed] [Google Scholar]
- Lachenmeier D. W., Taylor B. J., Rehm J. Alcohol under the radar: Do we have policy options regarding unrecorded alcohol? International Journal on Drug Policy. 2011;22:153–160. doi: 10.1016/j.drugpo.2010.11.002. doi:10.1016/j.drugpo.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Martinez P., Kerr W. C., Subbaraman M. S., Roberts S. C. M. New estimates of the mean ethanol content of beer, wine, and spirits sold in the United States show a greater increase in per capita alcohol consumption than previous estimates. Alcoholism: Clinical and Experimental Research. 2019;43:509–521. doi: 10.1111/acer.13958. doi:10.1111/acer.13958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A. H., Ballestros K., Echko M., Glenn S., Olsen H. E., Mullany E., Murray C. J. L., & the US Burden of Disease Collaborators 2018The state of US health, 1990-2016: Burden of diseases, injuries, and risk factors among US states JAMA 3191444–1472.doi:10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS) 2020. Retrieved from https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars.
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Epidemiologic Data Directory. 2017. Retrieved from https://pubs.niaaa.nih.gov/publications/2017DataDirectory/2017DataDirectory.htm#1.
- Nelson D. E., Jarman D. W., Rehm J., Greenfield T. K., Rey G., Kerr W. C., Naimi T. S. Alcohol-attributable cancer deaths and years of potential life lost in the United States. American Journal of Public Health. 2013;103:641–648. doi: 10.2105/AJPH.2012.301199. doi:10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson D. E., Naimi T. S., Brewer R. D., Roeber J. US state alcohol sales compared to survey data, 1993-2006. Addiction. 2010;105:1589–1596. doi: 10.1111/j.1360-0443.2010.03007.x. doi:10.1111/j.1360-0443.2010.03007.x. [DOI] [PubMed] [Google Scholar]
- Northcote J., Livingston M. Accuracy of self-reported drinking: Observational verification of ‘last occasion’ drink estimates of young adults. Alcohol and Alcoholism. 2011;46:709–713. doi: 10.1093/alcalc/agr138. doi:10.1093/alcalc/agr138. [DOI] [PubMed] [Google Scholar]
- Parish W. J., Aldridge A., Allaire B., Ekwueme D. U., Poehler D., Guy G. P., Jr., Trogdon J. G. A new methodological approach to adjust alcohol exposure distributions to improve the estimation of alcohol-attributable fractions. Addiction. 2017;112:2053–2063. doi: 10.1111/add.13880. doi:10.1111/add.13880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra J., Taylor B., Irving H., Roerecke M., Baliunas D., Mohapatra S., Rehm J. Alcohol consumption and the risk of morbidity and mortality for different stroke types—A systematic review and meta-analysis. BMC Public Health. 2010;10:258. doi: 10.1186/1471-2458-10-258. doi:10.1186/1471-2458-10-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Crépault J. F., Wettlaufer A., Manthey J., Shield K. What is the best indicator of the harmful use of alcohol? A narrative review. Drug and Alcohol Review. 2020;39:624–631. doi: 10.1111/dar.13053. doi:10.1111/dar.13053. [DOI] [PubMed] [Google Scholar]
- Rehm J., Greenfield T. K., Walsh G., Xie X., Robson L., Single E. Assessment methods for alcohol consumption, prevalence of high risk drinking and harm: A sensitivity analysis. International Journal of Epidemiology. 1999;28:219–224. doi: 10.1093/ije/28.2.219. doi:10.1093/ije/28.2.219. [DOI] [PubMed] [Google Scholar]
- Rehm J., Kehoe T., Gmel G., Stinson F., Grant B., Gmel G. Statistical modeling of volume of alcohol exposure for epidemiological studies of population health: The US example. Population Health Metrics. 2010;8:3. doi: 10.1186/1478-7954-8-3. doi:10.1186/1478-7954-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey G., Boniol M., Jougla E. Estimating the number of alcohol-attributable deaths: Methodological issues and illustration with French data for 2006. Addiction. 2010;105:1018–1029. doi: 10.1111/j.1360-0443.2010.02910.x. doi:10.1111/j.1360-0443.2010.02910.x. [DOI] [PubMed] [Google Scholar]
- Shield K., Manthey J., Rylett M., Probst C., Wettlaufer A., Parry C. D. H., Rehm J.2020National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study The Lancet Public Health 5e51–e61doi:10.1016/S2468-2667(19)30231-2 [DOI] [PubMed] [Google Scholar]
- Slater M. E., Alpert H. R. Surveillance Report #113: Apparent per capita alcohol consumption: National, state, and regional trends, 1977–2017. 2019 Retrieved from https://pubs.niaaa.nih.gov/publications/surveillance113/CONS17.htm#top. [Google Scholar]
- Smith G. S., Branas C. C., Miller T. R. Fatal nontraffic injuries involving alcohol: A metaanalysis. Annals of Emergency Medicine. 1999;33:659–668. doi:10.1016/S0749-3797(18)31070-5. [PubMed] [Google Scholar]
- Stahre M., Naimi T., Brewer R., Holt J. Measuring average alcohol consumption: The impact of including binge drinks in quantity-frequency calculations. Addiction. 2006;101:1711–1718. doi: 10.1111/j.1360-0443.2006.01615.x. doi:10.1111/j.1360-0443.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Donath S., Cooper-Stanbury M., Chikritzhs T., Catalano P., Mateo C. Under-reporting of alcohol consumption in household surveys: A comparison of quantity-frequency, graduated-frequency and recent recall. Addiction. 2004;99:1024–1033. doi: 10.1111/j.1360-0443.2004.00815.x. doi:10.1111/j.1360-0443.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Zhao J., Sherk A., Rehm J., Shield K., Naimi T. Underestimation of alcohol consumption in cohort studies and implications for alcohol's contribution to the global burden of disease. Addiction. 2018;113:2245–2249. doi: 10.1111/add.14392. doi:10.1111/add.14392. [DOI] [PubMed] [Google Scholar]
- Tolonen H., Honkala M., Reinikainen J., Härkänen T., Mäkelä P. Adjusting for non-response in the Finnish Drinking Habits Survey. Scandinavian Journal of Public Health. 2019;47:469–473. doi: 10.1177/1403494819840895. doi:10.1177/1403494819840895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. 2015. Retrieved from http://health.gov/dietaryguidelines/2015/guidelines.
- Wood A. M., Kaptoge S., Butterworth A. S., Willeit P., Warnakula S., Bolton T., Danesh J., & the Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group 2018Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies The Lancet 3911513–1523.doi:10.1016/S0140-6736(18)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health, 2018. 2018 Retrieved from https://www.who.int/publications/i/item/9789241565639. [Google Scholar]
- Zhao J., Stockwell T., Roemer A., Naimi T., Chikritzhs T. Alcohol consumption and mortality from coronary heart disease: An updated meta-analysis of cohort studies. Journal of Studies on Alcohol and Drugs. 2017;78:375–386. doi: 10.15288/jsad.2017.78.375. doi:10.15288/jsad.2017.78.375. [DOI] [PMC free article] [PubMed] [Google Scholar]