Abstract
Background
AR based navigation of spine surgeries may not only provide accurate surgical execution but also operator independency by compensating for potential skill deficits. “Direct” AR-navigation, namely superposing trajectories on anatomy directly, have not been investigated regarding their accuracy and operator's dependence.
Purpose of this study was to prove operator independent reliability and accuracy of both AR assisted pedicle screw navigation and AR assisted rod bending in a cadaver setting.
Methods
Two experienced spine surgeons and two biomedical engineers (laymen) performed independently from each other pedicle screw instrumentations from L1-L5 in a total of eight lumbar cadaver specimens (20 screws/operator) using a fluoroscopy-free AR based navigation method. Screw fitting rods from L1 to S2-Ala-Ileum were bent bilaterally using an AR based rod bending navigation method (4 rods/operator). Outcome measures were pedicle perforations, accuracy compared to preoperative plan, registration time, navigation time, total rod bending time and operator's satisfaction for these procedures.
Results
97.5% of all screws were safely placed (<2 mm perforation), overall mean deviation from planned trajectory was 6.8±3.9°, deviation from planned entry point was 4±2.7 mm, registration time per vertebra was 2:25 min (00:56 to 10:00 min), navigation time per screw was 1:07 min (00:15 to 12:43 min) rod bending time per rod was 4:22 min (02:07 to 10:39 min), operator's satisfaction with AR based screw and rod navigation was 5.38±0.67 (1 to 6, 6 being the best rate). Comparison of surgeons and laymen revealed significant difference in navigation time (1:01 min; 00:15 to 3:00 min vs. 01:37 min; 00:23 to 12:43 min; p = 0.004, respectively) but not in pedicle perforation rate.
Conclusions
Direct AR based screw and rod navigation using a surface digitization registration technique is reliable and independent of surgical experience. The accuracy of pedicle screw insertion in the lumbar spine is comparable with the current standard techniques.
Keywords: Augmented reality, pedicle screw navigation, rod bending, pedicle screw accuracy, HoloLens
Abbreviations: AR, Augmented Reality; CT, Computer Tomography; nDD, navigated Direction Deviation or navigated Trajectory Deviation; nED, navigated Entry Point Deviation; pDD, performed Direction Deviation or performed Trajectory Deviation; pED, performed Entry Point Deviation; RMSE, Root Mean Square Error; vs., versus
Introduction
Upcoming augmented reality (AR) based navigation systems promise to be the next-generation navigation technique in spine surgery [1], [2], [3], [4], [5], [6]. Due to the intuitive in situ visualization of important anatomical structures or predefined computer-generated information like planned screw trajectories, AR promises to simplify otherwise difficult and dangerous surgical procedures such as pedicle screw placement. Such simplification would potentially lead to a standardization of surgical procedures and reduce dependence on surgeon's skills or experience.
Complex navigation solutions have been developed to reduce the rate of pedicle screw malpositioning such as optical navigation systems, robotic-assisted pedicle screw placement and patient specific instrumentation. Those technologies provide a significant improvement of pedicle screw accuracy compared to the standard freehand technique [7], [8], [9], [10]. However, they are still not widely used due to their expensive hardware, set-up and maintenance costs. The costs for a robotic navigation system for example are currently around $550,000 USD, not including disposables and implants [11,12]. Additionally, such systems are bulky [12] and despite their sophisticated technology, they are still prone to errors in certain scenarios such as in obese patients or in patients with severe deformities, or osteoporosis [13,14].
AR based spinal navigation systems promise to compensate for many of these shortcomings. They potentially provide a cost-effective and intuitive navigation tool, even for indirect navigation tasks such as rod bending for multilevel spinal fusion surgery [15]. Furthermore, radiation-free registration and navigation of pedicle screw insertion has theoretically become possible through head-mounted AR displays equipped with inside-out-tracking technology [16]. Inside-out-tracking is a technical achievement, which allows the device to spatially locate itself with the environment without requiring additional technical equipment such as external tracking systems. With inside-out-tracking it is possible to pursue a “surgeon-centric” approach where 3D holograms can be visualized directly in-situ on the anatomy and from the surgeon's viewpoint. Studies have shown that such surgeon-centric approaches make cognitively demanding tasks such as pedicle screw placement or rod bending potentially easier [17]. Several years of research and development preceded the here investigated technology of “direct” AR-based navigation.
An important step towards clinical application of AR based surgical navigation is the investigation of reliability and accuracy in cadavers and the dependence of the new technology on surgical skills. We therefore hypothesized that direct AR based spinal navigation allows standardization of performance for certain surgical tasks (e.g. pedicle screw insertion and rod bending), independent of surgeon's skills or experience.
Methods
Ethical approval for this study was obtained from the ethical committee of Canton Zurich (Basec-Nr. 2017-00874). Eight fresh frozen human lumbar spine specimens were acquired from ScienceCare® (Phoenix, Arizona, USA) and used in this study.
The cadavers were freed from soft tissues such as the paravertebral autochthonic muscles in order to expose the dorsal bony anatomy. Two biomedical engineers without any surgical or anatomical education and two experienced spine surgeons were declared as laymen (Layman 1 and Layman 2) and surgeons (Surgeon 1 and Surgeon 2), respectively, to allow comparison between the two experience groups.
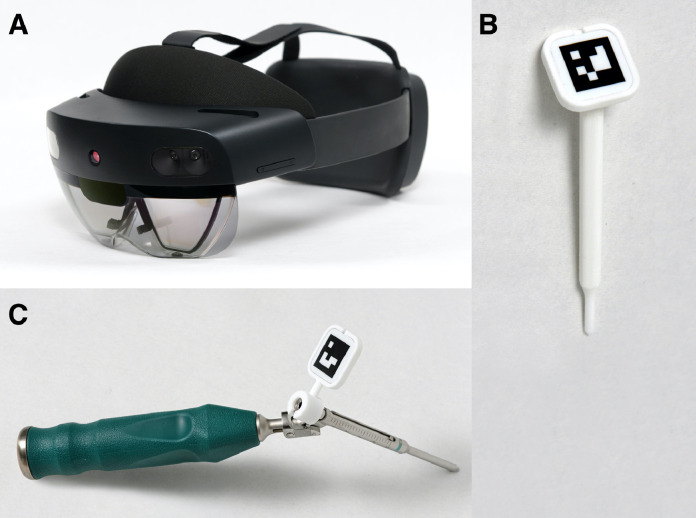
Each operator was assigned to implant AR navigated pedicle screws from L1 to L5 on both sides of two cadavers and, afterwards, to bend a rod implant fitting into the screw heads using AR rod bending. To make the rod bending more challenging, S1 and S2-Ala-Ileum screws were additionally inserted by a surgeon before the rod bending maneuvers. In total, each operator inserted 20 screws and bent 4 rods using the head-mounted device Microsoft Hololens 2 (Microsoft, Redmond, USA; Figure 1).
Fig. 1.
Equipment needed for AR based pedicle screw navigation and rod bending: (A) pointer with fiducial marker, (B) HoloLens 2, (C) trackable drill sleeve guide with 3D printed clamp for marker fixation.
Preoperative planning
Preoperative CT scans (SOMATOM Edge Plus, Siemens Healthcare GmbH, Erlangen, Germany) with a slice thickness of 1 mm were acquired. 3D triangular surface models were reconstructed from the segmented vertebrae using a commercial segmentation software (Mimics 19.0, Materialise NV, Leuven, Belgium).
Pedicle screw insertion points and trajectories were planned in 3D using our in-house developed preoperative planning software (CASPA, University Hospital Balgrist, Zurich, Switzerland). In the planning software, the screw trajectories were represented as cylinder primitives which were brought into the desired positions and orientations by an experienced spine surgeon. The entry points of the screws were defined at the intersection between the superior articular process and the transverse process. The trajectories of the screws were planned to be centrally within the pedicles.
The data about entry points (3D points), trajectories (3D direction vectors) and 3D bone models were loaded on the Hololens 2 application and served as the basis for our navigation approach which is described in the following section.
Registration and pedicle screw navigation
Our approach for registering the preoperative planning to the ex-vivo anatomy is based on an optical process with which the exposed bone surface is digitized and aligned with the bone models of the preoperative plan. The method was validated for the predecessor model of the AR device and published in a previous study [16]. In our experiments, each vertebra was digitized and registered separately and immediately before navigation. A digital representation of the dorsal bony anatomy was generated by sampling the transverse processes, laminae, pars and spinous process of each vertebra with a trackable pointing device (Figure 1).
The resulting 3D point cloud was then automatically registered to the corresponding CT-reconstructed vertebra model of the preoperative plan using iterative closest point (ICP) registration [18]. The registration result was verified and approved by the operator by comparing the in-situ displayed 3D hologram of the vertebra, the planned screw trajectories and the entry points with the real cadaver anatomy.
For navigation, a commercial depth limited drill sleeve guide (∅3.2 mm No. 03.614.010, Synapse System, DePuy Synthes, Johnson & Johnson, Raynham, MA, USA) was equipped with a fiducial marker (Clear Guide Medical, Baltimore MD, USA) on a custom-made, 3D-printed clamp to enable real-time position tracking of the drill sleeve through the Hololens (Figure 1).
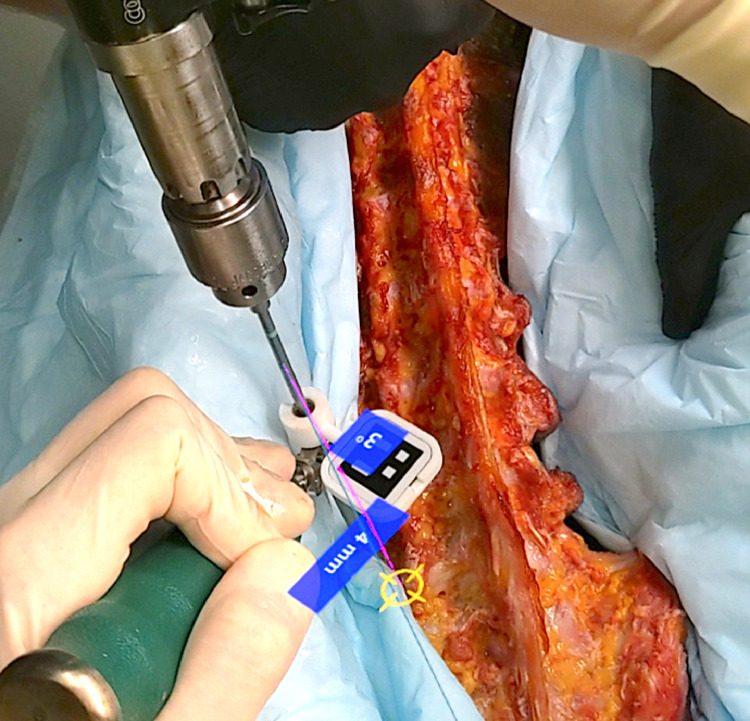
In our visually based navigation approach, the current Euclidean distance from the planned entry point (nED; in millimeters) and the current angular deviation from the planned trajectory (nDD; in degrees) were measured in real-time and displayed directly adjacent to the drill sleeve (Figure 2). Additionally, the current trajectory deviation was visualized graphically by three points forming a triangle; the first one lying on the planned trajectory, the second one on the entry point and the third one on the current trajectory. The operator started drilling when he reached the best match with the preoperative plan. Immediately before drilling, the displayed values of nED and nDD were reported and recorded. Cannulated screws with a 6 mm diameter and a length of 45 mm (M.U.S.T., Medacta SA, Castel San Pietro, Switzerland) were inserted over a K-wire into the pre-drilled hole.
Fig. 2.
Intraoperative operator's view during navigation. Current deviation of the drill sleeve guide from entry point (4 mm) and from planned trajectory (3°) is shown in real time.
The navigation time was recorded as well, which was defined as the time from which the drill sleeve was taken with the hands until the drilling process was started.
Rod bending
A previously validated and published AR based rod bending application [15] was used to bend and insert the rods into the screw heads from L1 to Ileum. The same pointing device as in the registration step was used in a first step to capture the 3D positions of the screw heads.
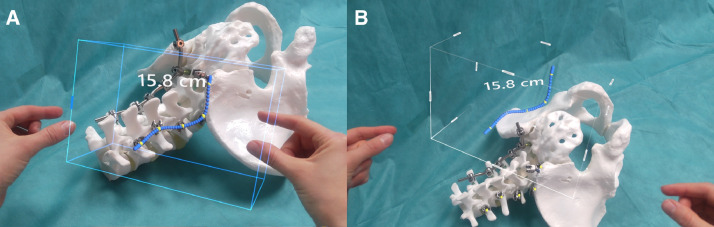
Thereafter, a hologram representing the rod shape that optimally matches patient anatomy and screw heads was calculated by fitting a centripetal Catmull-Rom spline function [19] to the digitized screw positions. The holographic rod could be positioned and rotated in space using gestures (Figure 3).
Fig. 3.
Intraoperative operator's view for rod bending here shown in a saw bone model. (A) virtual rod which optimally matches screw heads is created after capture of the 3D positions of screw heads. Optimal rod length is indicated (15.8 cm). (B) The holographic rod can be moved in space using gestures.
After positioning next to the bending place, the hologram served as a bending template for assisting the real bending maneuver. The bending maneuver was performed using commercial titanium rods (∅5.5 mm, M.U.S.T. Medacta SA, Castel San Pietro, Switzerland) using three optional commercial rod bending devices as to the surgeon's preference (Cat. No. 388.750, USS Rod Cutting and Bending Device / Cat. No. 2770-30-000, French Rod Bender / Cat. No. 2770-30-050 In-situ Rod Bender, Synthes, J&J) as well as a rod clamp (Cat.No. 2770-30-135, Rod Clamp, Synthes, J&J) if necessary.
The rod was implanted and connected with the pedicle screws using a rod reducer (M.U.S.T, Medacta, Castel San Pietro, Switzerland) if necessary. The end of the rod bending process was defined as the moment when the last set screw was tightened with the Torque Limiter Set Screwdriver (M.U.S.T. Medacta, Castel San Pietro, Switzerland).
Outcome evaluation
Postoperatively, a CT of each cadaver was acquired to assess accuracy of the instrumentation. 3D models of the vertebrae and of the implanted screws were created using the same segmentation method as applied preoperatively. Each postoperative 3D bone model was then aligned to the corresponding preoperative vertebra model using ICP registration. A ∅2 mm cylinder was aligned to the implanted screws in order to quantify the screw trajectories. The performed entry points were defined as the intersection between the bony surface and the screw trajectory. Hereinafter, the 3D distance between planned and performed entry points is denoted as the performed entry point deviation (pED). Similarly, the 3D angle between planned and performed trajectories is denoted as the performed trajectory deviation (pDD).
Additionally, pedicle perforations were assessed by a blinded radiologist using the Gertzbein-Robbins Classification [20] (grade A: no perforation / grade B: < 2 mm perforation / grade C: < 4 mm perforation / grade D: < 6 mm perforation / grade E: > 6 mm perforation).
Registration time, number of digitized registration points and the root mean square error (RMSE) of the registration were recorded postoperatively to quantitatively assess the registration performance. The RMSE is a statistical measure of differences of values between a model and observations. The observation was represented here by the intraoperative points sampled using surface digitization. Through the registration process, these points were superimposed with the CT-reconstructed 3D bone model. The "RMSE model" is constructed by finding for each point of the observation the closest point on the 3D bone model. The average distance between all these point pairs is then defined as the RMSE. The formula for RMSE calculation is as follows:
where is the i-th point of the digitized surface having N points and is the point from the preoperative 3D model which is closest to .
Rod bending performance was assessed by recording the screw head detection time (screw heads from L1 to S2-Al-Ileum of one side / for one rod), total bending time for one rod (start of bending until the last screw has been set), time for first bending attempt (from the start of bending until the rod was tried to be placed in screw heads), number and times for any required re-bending attempts, and overall subjective bending satisfaction graded from 1 to 6 with 6 being the best rating.
Statistical analysis
A univariate model (one-way ANOVA) was applied to identify differences between surgeons (Surgeon 1 and Surgeon 2) and laymen (Layman 1 and Layman 2) as well as between operators among themselves. Fisher exact test was applied to identify variation in screw-perforation grading.
To identify correlations between variables either Pearson's correlation coefficient for presumed linear correlation or Spearman's rho for presumed monotone correlation were applied. Correlation coefficient descriptors were considered as small: 0.1–0.3, moderate: 0.3–0.5, and large: >0.5. Statistical significance was set to p < 0.05. Statistical Software for the Social Sciences (IBM SPSS Statistics version 26.0 for Windows, IBM Corp, Armonk, NY, USA, 2018) was used to carry out the analysis.
Continues variables are reported as means with standard deviation, time measures as median with range, categorical variables as proportions.
Results
Pedicle screw placement
The radiological assessment revealed that 97.5% of the screws (78 of 80 screws) were placed within the safe zone of 2 mm pedicle wall perforation (grade A and B). 67 screws (83.8%) were located completely within the pedicle (grade A), while 13 (16.3%) showed some perforation. 11 screws (13.8%) had a perforation smaller than 2 mm (grade B). One screw (1.3%) had a perforation of less than 6 mm (grade D) which had been inserted by a surgeon (Surgeon 2). One screw (1.3%) had a perforation greater than 6 mm (grade E) which had been inserted by a layman (Layman 1). The group comparison between surgeons and laymen showed no significant difference in pedicle perforation (Table 1). Similarly, no significant difference could be found among all operators in pedicle perforation rate (Table 2).
Table 1.
Comparison of registration and navigation performance between surgeons and laymen (nDD: navigated Direction Deviation, nED: navigated Entry Point Deviation, pDD: performed Direction Deviation, pED: performed Entry Point Deviation).
| Parameters | Surgeons | Laymen | p-value |
|---|---|---|---|
| Pedicle perforations | |||
| Grad A and B (<2 mm) | 97.5% (39/40) | 97.5% (39/40) | 0.43 |
| Grad A | 80% (32/40) | 87.5% (35/40) | |
| Grad B | 17.5% (7/40) | 10% (4/40) | |
| Grad C | 0% | 0% | |
| Grad D | 2.5% (1/40) | 0% | |
| Grad E | 0% | 2.5% (1/40) | |
| Deviation from preoperative plan | |||
| nDD | 2.9 ± 1.5° | 2.2 ± 1.0° | 0.04 |
| nED | 3.1 ± 1.5mm | 3.7 ± 2.4mm | 0.25 |
| pDD | 7.0 ± 3.9° | 6.5 ± 3.8° | 0.61 |
| pED | 4.2 ± 2.8mm | 3.8 ± 2.5mm | 0.52 |
| Registration time [min] | 02:06 (00:56 to 06:48) | 02:30 (01:30 to 10:00) | 0.53 |
| Registration points collected | 555 ± 230.3 | 233.4 ± 144.8 | <0.01 |
| Registration RMSE | 2.37 ± 0.73mm | 1.78 ± 1.26mm | 0.012 |
| Navigation time [min] | 01:01 (00:15 to 03:00) | 01:37 (00:23 to 12:43) | <0.01 |
| Satisfaction (0-6) | 5.4 ± 0.7 | 5.4 ± 0.6 | 0.47 |
Table 2.
Comparison of registration and navigation performance among operators (nDD: navigated Direction Deviation, nED: navigated Entry Point Deviation, pDD: performed Direction Deviation, pED: performed Entry Point Deviation).
| Parameters | Surgeon 1 | Surgeon 2 | Layman 1 | Layman 2 | p-value |
|---|---|---|---|---|---|
| Pedicle perforations | |||||
| Grad A and B (<2 mm) | 100% | 95% | 95% | 100% | 0.86 |
| Grad A | 80% (16/20) | 80% (16/20) | 85% (17/20) | 90% (18/20) | |
| Grad B | 20% (4/20) | 15% (3/20) | 10% (2/20) | 10% (2/20) | |
| Grad C | 0% | 0% | 0% | 0% | |
| Grad D | 0% | 5% (1/20) | 0% | 0% | |
| Grad E | 0% | 0% | 5% (1/20) | 0% | |
| Deviation from preoperative plan | |||||
| nDD | 3.4 ± 1.5° | 2.3 ± 1.2° | 2.9 ± 0.7° | 1.9 ± 0.9° | 0.01 |
| nED | 2.7 ± 1.6mm | 3.6 ± 1.3mm | 3.4 ± 1.6mm | 3.8 ± 2.7mm | 0.26 |
| pDD | 7.9 ± 4.3° | 6.1 ± 3.3° | 7.2 ± 4.7° | 5.9 ± 2.7° | 0.32 |
| pED | 3.8 ± 3.0mm | 4.6 ± 2.7mm | 4.9 ± 2.7mm | 2.8 ± 1.9mm | 0.05 |
| Registration time [min] | 03:45 (01:57 to 06:48) | 01:37 (00:56 to 03:11) | 03:54 (01:51 to 10:00) | 02:13 (01:30 to 03:30) | <0.01 |
| Registration points collected | 284.6 ± 154.7 | 715.8 ± 33.4 | 363.2 ± 118.2 | 318.2 ± 52.2 | <0.01 |
| Registration RMSE | 2.64 ± 0.89mm | 2.35 ± 0.08mm | 1.94 ± 0.59mm | 1.19 ± 0.09mm | <0.01 |
| Navigation time [min] | 01:34 (00:32 to 03:00) | 00:50 (00:15 to 02:30) | 03:31 (00:23 to 12::43) | 01:48 (00:23 to 05:30) | <0.01 |
| Satisfaction (0-6) | 5.0 ± 0.7 | 5.9 ± 0.3 | 5.7 ± 0.3 | 5.3 ± 0.6 | <0.01 |
The comparison between postoperative 3D models and preoperative plan showed an average deviation between performed and planned 3D-trajectories of 6.8 ± 3.9° (pDD). The average deviation between performed and planned entry point was 4 ± 2.7 mm (pED). Regarding the performed direction deviation, no significant differences could be found neither between surgeons and laymen nor among all operators. With regard to the performed entry point deviation, all operators showed significantly different performance. In the comparison between the laymen and surgeons groups, this difference was not significant.
The intraoperatively displayed deviation from the planned pedicle screw trajectory immediately before drilling was 2.6 ± 1.3° (nDD). The mean intraoperatively displayed deviation (nED) from the planned entry point was 3.4 ± 1.9 mm.
A significant difference in navigated direction deviation (nDD) could be found when comparing surgeons versus laymen and among the particular operators. Laymen had less deviation than surgeons (2.2 ± 1.0° vs. 2.9 ± 1.5°, p = 0.04, respectively). (Table 1)
While a layman (Layman 2) had the smallest deviation in nDD, a surgeon (Surgeon 1) had the largest deviation (1.9° ± 0.9° vs. 3.4° ± 1.5°, p = 0.01, respectively). (Table 2)
Correlation between deviation parameters (pDD, pED) and pedicle perforations
No correlation was found between deviation from the preoperatively planned trajectory (pDD) and the extent of pedicle screw perforation. There was a weak positive correlation between the performed entry point deviation (pED) with the degree of perforation according to the Gertzbein-Robbins grade (r=0.289, p = 0.007).
Registration
On average, the registration took 2:25 minutes (00:56 to 10:00 min). No significant difference in registration time was found between surgeons and laymen. However, there was a significant difference regarding the registration time between operators. On average, Surgeon 2 needed the least time for registration and Layman 1 the longest (01:37 min (00:56 to 03:11 min) and 03:54 min (1:51 to 10:00 min), p < 0.01 respectively).
Surgeons collected significantly more registration points than laymen (555 ± 230.3 vs. 233.4 ± 144.8, p < 0.01 respectively). An average of 394 ± 250 points were collected per vertebral body.
A significant correlation was neither found between registration time nor between amount of registration points and performed accuracy (pDD, pED) or perforation rate.
The RMSE averaged 2.07 ± 1.06 mm. There were significant differences among the operators regarding the RMSE (F=8.855, p = 0.000, partial η2= 0.259). The lowest average RMSE of 1.19 ± 0.09 mm was measured for Layman 2 and the highest RMSE of 2.64 ± 0.89 mm was measured for Surgeon 1.
Navigation time
On average, the operators navigated 1:07 min (00:15 to 12:43 min) before starting the drilling process. Surgeons had significantly less navigation time than laymen (Table 1). The shortest navigation time was performed by a surgeon (Surgeon 2) and the longest by a layman (Layman 1). No significant correlations were found between navigation time and the deviation from the planned trajectory (pDD, pED) or perforation rate.
Satisfaction of the operator
The overall satisfaction with the whole registration and navigation process was graded as high by all operators, with an average score of 5.4 ± 0.6 (scale range: 1-6, 6 being the best grade). No significant differences were found comparing surgeons and laymen.
Rod bending
The median screw head detection time was 54 seconds (00:29 to 04:30 min). 16 rods were bent in total. In 6 cases one additional re-bending attempt was needed after primary bending. In 3 cases two re-bending attempts were necessary. The median total bending time was 05:53 min (02:37 to 22:08 min) per rod. The time required for the first rod bending attempt was 04:22 min (02:07 to 10:39 min). The first re-bending attempt took additional 02:42 min (00:25 to 07:49 min) and the second re-bending attempt took additional 04:00 min (00:40 to 08:43 min). Across all rod bending maneuvers, satisfaction was graded at 5.38 ± 0.67 (scale range: 1-6, 6 being the best rate).
A significant difference among operators were found in the time required for the first bending attempt with a surgeon having the shortest and a layman having the longest re-bending attempt of 02:47 min (02:07 to 05:55 min) vs. 06:58 min (04:36 to 10:00 min), respectively (p = 0.05). Surgeons were also significantly faster than laymen regarding the first bending attempt in the group analysis, requiring 03:08 min (02:07 to 05:55 min) vs. 06:24 min (03:50 to 10:39 min), respectively (p = 0.004).
Screw head detection time was only significantly different among all operators but not in the comparison between surgeons and laymen. Two laymen had both the shortest and the longest screw head detection time of 00:33 min (00:29 to 00:38 min) and 02:07 min (01:02 to 04:30 min), respectively (p = 0.04) (Tables 3 and 4).
Table 3.
Comparison of rod bending performance between surgeons and laymen.
| Parameters | Surgeons | Laymen | p-value |
|---|---|---|---|
| Screw head detection time [min] | 00:54 (00:31 to 02:45) | 00:50 (00:29 to 02:10) | 0.51 |
| Median total bending time [min] | 04:52 (02:37 to 22:08) | 07:00 (03:50 to 17:00) | 0.74 |
| First bending [min] | 03:08 (02:07 to 05:55) | 06:24 (03:50 to 10:39) | 0.004 |
| Re-bending 1 [min] | 02:43 (02:20 to 07:49) | 00:53 (00:25 to 05:30) | 0.17 |
| Re-bending 2 [min] | 08:43 (08:43 to 08:43) | 02:20 (00:40 to 04:00) | 0.27 |
| Number of re-bends | 6 | 6 | 1 |
| Satisfaction (0-6) | 5.25 ± 0.88 | 5.5 ± 0.42 | 0.30 |
Table 4.
Comparison of rod bending performance among operators.
| Parameters | Surgeon 1 | Surgeon 2 | Layman 1 | Layman 2 | p-value |
|---|---|---|---|---|---|
| Screw head detection time [min] | 01:08 (00:44 to 02:45) | 00:43 (00:31 to 01:15) | 02:07 (01:02 tp 04:30) | 00:33 (00:29 to 00:38) | 0.04 |
| Median total bending time/rod [min] | 03:32 (02:37 to 06:05) | 08:03 (04:49 to 22:08) | 08:13 (05:41 to 17:00) | 06:08 (03:50 to 11:14) | 0.28 |
| First bending [min] | 03:20 (02:37 to 04:09) | 02:47 (02:07 to 05:55) | 06:58 (04:36 to 10:00) | 05:32 (03:50 to 10:39) | 0.05 |
| Re-bending 1 [min] | 02:20 (02:20 to 02:20) | 05:06 (02:42 to 07:49) | 02:57 (00:25 to 05:30) | 00:53 (00:35 to 01:12) | 0.40 |
| Re-bending 2 [min] | none | 08:43 (08:43 to 08:43) | 02:20 (00:40 to 02:20) | none | 0.27 |
| Number of re-bending attempts | 1 | 5 | 4 | 2 | 0.26 |
| Satisfaction (0-6) | 4.9 ± 0.9 | 6 ± 0 | 5.75 ± 0 | 5.38 ± 0.48 | 0.26 |
Discussion
AR-based surgical navigation could be the next step in the evolution of surgical navigation in spine surgery. This is the first study to document reliability and accuracy of “direct” AR navigation of pedicle screws and rod bending using Hololens 2 and inside-out tracking. The experiments were performed in human cadavers by surgeons and laymen and showed independency on surgical skills and experience.
No or minor pedicle perforations of less than 2 mm were achieved in 97.5% of the inserted screws by both the surgeons and the non-anatomically and surgically educated biomedical engineers. This indicates that AR based surgical navigation may be an operator-independent solution for surgical navigation which might be capable of compensating potential skill deficits. In particular, our study was able to show that AR is capable of simplifying the difficult surgical steps of pedicle screw placement and rod implant bending. For the future use of this technology in surgery this could mean that less experienced surgeons may be able to perform these tasks in a more standardized and safer manner. Clearly, this statement is only true for a specific surgical step in an experimental setting and does not apply for overall surgical skills.
The achieved navigation accuracy with respect to pedicle perforation was comparable with other established navigation systems: The accuracy of patient-specific template guided pedicle screw insertion was reported to be 98% within the safe zone of less than 2 mm breach [8]. Computer based navigation techniques have shown to have an accuracy of up to 96% [7] and robotic assisted navigation has an accuracy 95-98% [9,10,14].
The performed deviation from the preoperative plan with 6.8° 3D angular deviation and 4 mm entry point deviation seems to be higher in our study than, for instance, in robotic assisted surgery where deviations of 2.2° have been reported [10]. Similarly, patient-specific template guided pedicle screw insertion has smaller angular deviations of 1.74° on average [21]. However, the deviation measurements in these studies were only performed in two different planes and not with a 3D angular deviation mesaure as in our study. A comparison is therefore only possible to a limited extent as 3D anges report deviations in 3 rather than 2 dimension.
On the other side, since the spatial orientation of Hololens 2 is based on inside-out-tracking, it has, despite clear advantages, a limited accuracy compared to high-end navigation systems or robotic surgery.
Nevertheless, these relatively high deviation parameters seem not to have an influence on the very low pedicle perforation rate in our study. Deviations, as shown in our study, appear to have fewer consequences in the lumbar spine than in the thoracic or cervical spine because the lumbar pedicles are generally larger in diameter [22].
Another interesting finding was that surgeons had a greater navigated direction deviation (nDD) than laymen. It might be possible, that surgeons intuitively relied more on their anatomical knowledge than on navigation and therefore deviated more from the navigation than laymen. This phenomenon is possible with AR navigation, since the holograms only suggest a trajectory while the surgeon is still free to deviate.
The average registration and navigation time was 2:50 min per vertebra and 1:51 min per screw, respectively. This means that the entire AR based navigation process for one vertebra, respectively, for two screws takes around 7 minutes. This is acceptable, because in turn no time for intraoperative image acquisition is necessary. Furthermore, as shown for Surgeon 2, time effort can be reduced to 1:38 mins for registration and 58 sec for navigation while still achieving good accuracy.
Whereas comparison of laymen and surgeons showed no difference in screw accuracy, a significant difference was found in the number of digitized points and navigation time. Laymen collected less registration points as surgeons and they were slower in navigation which may reflect the surgeons’ ability to recognize the relevant bony anatomy easier and safer due to their anatomical knowledge. This explains also why the RMSE of the laymen were significantly lower. The laymen digitized only the regions of the vertebrae which were easiest to identify due to the lack of anatomical knowledge. Within these regions, the RMSE was lower which does, however, not allow to conclude that the registration/superimposition was better. The surgeon tried to capture the entire vertebrae surface by digitizing as much of the visible bone surface as possible. However, the different digitization strategies had no significant influence on the accuracy of pedicle screw insertion.
The results of the rod bending step showed that there were no significant differences between laymen and surgeons. The total bending time was not different between both operator groups, which proves that this application also appears to be operator-independent. Moreover, it has been demonstrated previously that the time for bending can be reduced by 20% using this application compared to the conventional method [15].
Conclusion
Direct AR-based navigation for pedicle screw insertion and rod bending using surface digitization registration technology seems reliable, operator-independent and requires little technical equipment. The accuracy in the lumbar spine is comparable to current, established navigation systems. An in-human clinical study is warranted to investigate the potential merits of the here presented novel method for surgical navigation as the next consequential step toward standard clinical application.
Funding disclosure statement
This work is part of “SURGENT” under the umbrella of University Medicine Zurich.
Informed Patient Consent
The authors declare that informed patient consent was taken from all the patients.
Declaration of Competing Interest
The authors declare no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2021.100084.
Appendix. Supplementary materials
References
- 1.Molina CA, Theodore N, Ahmed AK, Westbroek EM, Mirovsky Y, Harel R, et al. Augmented reality–assisted pedicle screw insertion: a cadaveric proof-of-concept study. J Neurosurg Spine. 2019;31:139–146. doi: 10.3171/2018.12.SPINE181142. [DOI] [PubMed] [Google Scholar]
- 2.Burström G, Nachabe R, Persson O, Edström E, Elmi Terander A. Augmented and virtual reality instrument tracking for minimally invasive spine surgery. Spine. 2019;44:1097–1104. doi: 10.1097/BRS.0000000000003006. [DOI] [PubMed] [Google Scholar]
- 3.Ma L, Zhao Z, Chen F, Zhang B, Fu L, Liao H. Augmented reality surgical navigation with ultrasound-assisted registration for pedicle screw placement: a pilot study. Int J Comput Assist Radiol Surg. 2017;12:2205–2215. doi: 10.1007/s11548-017-1652-z. [DOI] [PubMed] [Google Scholar]
- 4.Elmi-Terander A, Burström G, Nachabe R, Skulason H, Pedersen K, Fagerlund M, et al. Pedicle screw placement using augmented reality surgical navigation with intraoperative 3D imaging: a first in-human prospective cohort study. Spine. 2019;44:517–525. doi: 10.1097/BRS.0000000000002876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edström E, Burström G, Nachabe R, Gerdhem P, Elmi Terander A. A novel augmented-reality-based surgical navigation system for spine surgery in a hybrid operating room: design, workflow, and clinical applications. Oper Neurosurg. 2019 doi: 10.1093/ons/opz236. [DOI] [PubMed] [Google Scholar]
- 6.Wu JR, Wang ML, Liu KC, Hu MH, Lee PY. Real-time advanced spinal surgery via visible patient model and augmented reality system. Comput Methods Programs Biomed. 2014;113:869–881. doi: 10.1016/j.cmpb.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 7.Mason A, Paulsen R, Babuska JM, Rajpal S, Burneikiene S, Nelson EL, et al. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine. 2014;20:196–203. doi: 10.3171/2013.11.SPINE13413. [DOI] [PubMed] [Google Scholar]
- 8.Farshad M, Betz M, Farshad-Amacker NA, Moser M. Accuracy of patient-specific template-guided vs. free-hand fluoroscopically controlled pedicle screw placement in the thoracic and lumbar spine: a randomized cadaveric study. Eur Spine J. 2016;26:1–12. doi: 10.1007/s00586-016-4728-5. [DOI] [PubMed] [Google Scholar]
- 9.Laudato PA, Pierzchala K, Schizas C. Pedicle screw insertion accuracy using O-arm, robotic guidance, or freehand technique. Spine. 2018;43:E373–E378. doi: 10.1097/BRS.0000000000002449. [DOI] [PubMed] [Google Scholar]
- 10.Van Dijk JD, Van Den Ende RPJ, Stramigioli S, Köchling M, Höss N. Clinical pedicle screw accuracy and deviation from planning in robot-guided spine surgery: Robot-guided pedicle screw accuracy. Spine. 2015;40:E986–E991. doi: 10.1097/BRS.0000000000000960. [DOI] [PubMed] [Google Scholar]
- 11.Fiani B, Quadri SA, Farooqui M, Cathel A, Berman B, Noel J, et al. Impact of robot-assisted spine surgery on health care quality and neurosurgical economics: A systemic review. Neurosurg Rev. 2020;43:17–25. doi: 10.1007/s10143-018-0971-z. [DOI] [PubMed] [Google Scholar]
- 12.Malham GM, Wells-Quinn T. What should my hospital buy next?—Guidelines for the acquisition and application of imaging, navigation, and robotics for spine surgery. J Spine Surg. 2019;5:155–165. doi: 10.21037/jss.2019.02.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lieberman IH, Kisinde S, Hesselbacher S. Robotic-assisted pedicle screw placement during spine surgery. JBJS Essent Surg Tech. 2020;10 doi: 10.2106/JBJS.ST.19.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang JN, Fan Y, Hao DJ. Risk factors for robot-assisted spinal pedicle screw malposition. Sci Rep. 2019;9 doi: 10.1038/s41598-019-40057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wanivenhaus F, Neuhaus C, Liebmann F, Roner S, Spirig JMJM, Farshad M. Augmented reality-assisted rod bending in spinal surgery. Spine J. 2019;19:1687–1689. doi: 10.1016/j.spinee.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 16.Liebmann F, Roner S, von Atzigen M, Scaramuzza D, Sutter R, Snedeker J, et al. Pedicle screw navigation using surface digitization on the Microsoft HoloLens. Int J Comput Assist Radiol Surg. 2019 doi: 10.1007/s11548-019-01973-7. [DOI] [PubMed] [Google Scholar]
- 17.Brendle C, Schütz L, Esteban J, Krieg SM, Eck U, Navab N. 12263 LNCS. Springer Science and Business Media Deutschland GmbH; 2020. Can a hand-held navigation device reduce cognitive load? A user-centered approach evaluated by 18 surgeons; pp. 399–408. (Lect. Notes Comput. Sci. (including Subser. Lect. Notes Artif. Intell. Lect. Notes Bioinformatics)). [DOI] [Google Scholar]
- 18.Besl PJ, McKay ND. Method for registration of 3-D shapes. In: Schenker PS, Sens. Fusion IV control paradig. Data struct., vol. 1611, SPIE; 1992, p. 586–606. doi:10.1117/12.57955.
- 19.Barry PJ, Goldman RN. Recursive evaluation algorithm for a class of Catmull-Rom splines. Comput Graph. 1988;22:199–204. doi: 10.1145/378456.378511. [DOI] [Google Scholar]
- 20.Gertzbein S, Robbins S. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Lamartina C, Cecchinato R, Fekete Z, Lipari A, Fiechter M, Berjano P. Pedicle screw placement accuracy in thoracic and lumbar spinal surgery with a patient-matched targeting guide: a cadaveric study. Eur Spine J. 2015;24:937–941. doi: 10.1007/s00586-015-4261-y. [DOI] [PubMed] [Google Scholar]
- 22.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12:160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.