Abstract
Background
Sacroiliac joint dysfunction (SJD) is a known cause of lower back pain. SJD might be due to hypermobility in the Sacroiliac joint (SIJ) in patients with Ehlers Danlos Syndrome (EDS). Stabilization of the SIJ can be a highly successful treatment for lower back pain. No previous literature about EDS and SIJ fusion is available. The purpose of this study was to assess our mid-term results of SIJ fusion surgery in EDS patients suffering from SIJ dysfunction.
Methods
A case series of patients who underwent SIJ fusion for SIJ dysfunction due to EDS between January 2012 and December 2018 were analyzed in retrospect. Patients underwent surgery and the SIJ was stabilized with triangular implants bridging the joint. Pain and functional outcomes were assessed in nine agree/disagree questions and a satisfaction performance scale. Clinical data has been extracted from the patient files and in addition, we reassessed the position of the implants on the CT scans.
Results
A total of 16 patients with EDS completed the questionnaire and were available for analysis. The mean satisfaction score is 78.1 out of 100 and seven patients reported a 100% satisfaction score.
Conclusion
SIJ fusion is a safe and useful procedure to reduce pain and function levels in EDS patients with lower back pain due to SIJ dysfunction.
Keywords: Sacroiliac joint fusion, Ehlers Danlos Syndrome, hypermobility, lower back pain, Sacroiliac joint dysfunction, iFuse implant system
Introduction
Sacroiliac joint (SIJ) fusion can be a highly successful treatment for lower back pain due to sacroiliac joint dysfunction [1,2]. When patients do not sufficiently respond to conservative treatment including analgesics, physiotherapy and corticosteroid injections, fusion can be considered for permanent stabilization of the SIJ [3].
The sacroiliac joint is responsible for energy and force transfers from the pelvis to the spine. A combination of balanced ligamentous compression and articular congruity is required for a proper function [3]. Disbalance in these components results in pathological motion potentially causing pain and disability [4,5]. The diagnosis is mostly based on clinical findings as blood work and imaging often show no significant pathological abnormalities. When SIJ dysfunction is suspected an intra-articular injection of the SIJ can be used to confirm the diagnosis [6,7]
With fusion of the sacrum and ilium the SIJ is stabilized to facilitate effective load transfer across the joint. By reducing micro-movement SIJ fusion is hypothesized to effectively treat SIJ mediated lower back pain [4,6]. This concept has been proven as recent randomized clinical trials showed SIJ fusion to be a successful and safe treatment in SIJ dysfunction [6,8].
Pregnancy, trauma, rheumatoid (sacroiliitis) and arthritis are often reported as causes of SIJ dysfunction and pain. Another lesser-known etiology for disbalance and subsequent pain of the SIJ due to hypermobility is Ehlers Danlos Syndrome (EDS) [9]. EDS constitutes a group of inherited disorders of connective tissue characterized by, among other things, joint and ligament hypermobility [10]. Hypermobility of the ligaments around the SIJ potentially destabilize the SIJ, inducing increased and thereby pathologic movement of the joint causing pain [11].
EDS may be diagnosed clinically or via molecular genetic testing [12]. The clinical diagnosis is based on several criteria such as atrophic scarring, skin hyperextensibility and generalized joint hypermobility. For this hypermobility the Beighton Criteria scale is used, which is a widely accepted grading system for the objective semi-quantification of joint hypermobility [13]. The joint and tissue hypermobility can lead to joint dislocations, early arthritis, fatigue and joint pain. The incidence of Ehlers-Danlos syndrome is best estimated to be roughly between 1 in 2500-5000 [14].
The purpose of the current study was to assess mid-term results of SIJ fusion surgery in EDS patients suffering from SIJ dysfunction.
Patients and methods
Study population
This study evaluated a continuous case series of patients who underwent SIJ fusion for SIJ dysfunction due to EDS at our institution between January 2012 and December 2018. All patients with EDS who underwent SIJ fusion for SIJ dysfunction were selected and asked to participate in the study. Not included were selected patients that refused to participate or did not finish the questionnaires. As this was a retrospective study and did not alter the treatment of patients nor their outcomes, ethical approval was waived by the Institutional Review Board, approval was obtained from the METC. Patient participation was entirely voluntary, with explanation and consent obtained by written informed consent. After providing the written consent a questionnaire was completed. We retrieved the medical history of all included patients from the patient files.
Surgical intervention
The procedures were performed under general anesthesia with the patients in a prone position. The patients were prepped in the usual sterile fashion and IV antibiotics were given before incision. An incision of approximately 4 cm was made and guide wires were placed under fluoroscopic control, passing through the ilium, crossing the SIJ into the sacrum.
The implants used for this study were triangular shaped titanium SIJ fusion devices (iFuse Implant System®, SI-BONE, Inc., San Jose, CA, USA). The implant is coated with a porous titanium plasma spray. The coating allows biological fixation of bone and has been used and proven effective in total joint prostheses over the last decades. The implants are available in sizes ranging from 4-7mm in diameter and 30-70 mm in length.
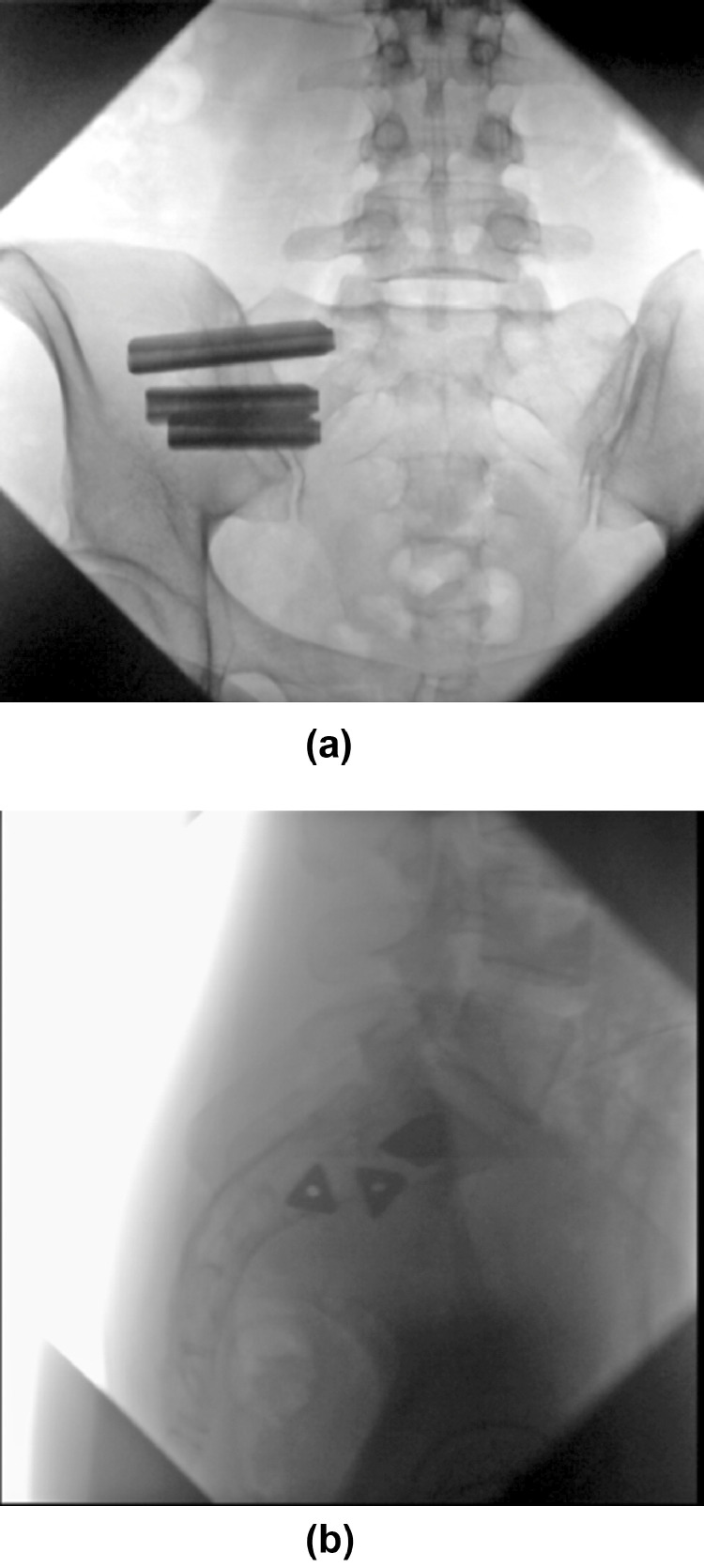
Triangular channels were created using the implant broach. The implant was then inserted and tapped into position. Two or three implants were placed to the proper depth under radiological control (inlet, outlet and lateral view) [Fig. 1a & b]. The implant positions were re-checked under radiologic control. The incision was then irrigated and the tissue layers were sequentially closed.
Fig. 1.
a: Inlet radiological view of iFuse implants; 1b: lateral view of iFuse implants.
Follow up
All patients were observed overnight for pain control and neurological observation. On the first postoperative day, a CT scan was performed to assess the position of the implants. Mobilization started the first postoperative day, initially with crutches. Full weight-bearing was allowed when possible. A physiotherapist was consulted for individualized physical therapy.
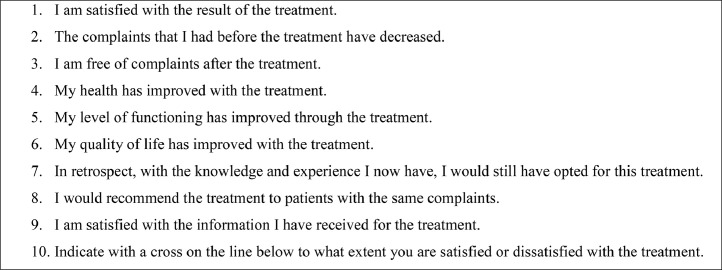
After 6-8 weeks patients returned to the clinic for regular follow-up. For this analysis, all patients were asked to complete a questionnaire [17]. Pain and functional outcomes were assessed in nine agree/disagree (strongly agree, agree, neutral, disagree and strongly disagree) questions and a satisfaction performance scale (NRS, 0-100) (Fig. 2).
Fig. 2.
Questionnaire.
Clinical data has been extracted from the patient files and in addition we reassessed the position of the implants on the CT scans.
Results
Study cohort
All patients operated in the evaluated period were asked to complete a questionnaire. A response rate of the patients questionnaire was 73%. In this group, a total of 16 patients were known with EDS and were available for analysis (Table 1).
Table 1.
Clinical evaluation of the patients.
| Case | Side | Age at time of surgery | Gender | ASA-clasification | BMI | Smoking | Duration of complaints | Block* | Number of implants | Size of implants (mm) | Size of implants (mm) | Size of implants (mm) | Duration of surgery (min) | Revision |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | left | 36.8 | F | 2 | 31.6 | - | - | 1 | 3 | 60 | 45 | 40 | 30 | 1 |
| 2 | left | 60.0 | F | 2 | 17.6 | No | >5y | 1 | 2 | 55 | 40 | 24 | ||
| 3 | left | 56.0 | F | 3 | 20.76 | - | - | 1 | 2 | 55 | 40 | 14 | ||
| right | 56.4 | 20.76 | 2 | 50 | 40 | 22 | ||||||||
| 4 | left | 46.0 | F | 2 | 20.1 | Yes | >5y | 1 | 2 | 55 | 40 | 27 | ||
| right | 44.5 | 20.1 | 2 | 50 | 40 | 24 | ||||||||
| 5 | left | 39.6 | F | 3 | 34.9 | - | - | 1 | 2 | 60 | 40 | 21 | ||
| right | 39.1 | 34.9 | 2 | 55 | 40 | 15 | ||||||||
| 6 | left | 34.9 | F | 2 | 26.0 | No | - | 1 | 2 | 50 | 40 | 30 | ||
| right | 35.7 | 26.0 | 2 | 60 | 45 | 23 | ||||||||
| 7 | left | 53.8 | F | 3 | 28.0 | No | - | 1 | 2 | 60 | 40 | 41 | ||
| right | 53.8 | 28.0 | 2 | 60 | 40 | 41 | ||||||||
| 8 | left | 51.9 | F | 2 | 20.7 | No | - | 1 | 2 | 66 | 45 | 32 | 1 | |
| right | 51.9 | 20.7 | 2 | 55 | 45 | 32 | ||||||||
| 9 | left | 53.6 | F | 2 | 18.7 | Yes | - | 0 | 2 | 60 | 40 | 13 | ||
| right | 54.1 | 18.7 | 2 | 55 | 45 | 19 | ||||||||
| 10 | left | 19.9 | F | 3 | 18.0 | - | >5y | 1 | 2 | 55 | 35 | 15 | ||
| right | 20.5 | 18.0 | 2 | 50 | 35 | 26 | ||||||||
| 11 | left | 44.3 | F | 2 | 22.0 | No | >5y | 1 | 2 | 60 | 40 | 16 | ||
| right | 43.9 | 22.0 | 2 | 60 | 40 | 22 | ||||||||
| 12 | left | 50.8 | F | 3 | 24.9 | - | - | 1 | 2 | 55 | 40 | 65 | ||
| right | 50.8 | 24.9 | 2 | 50 | 40 | 65 | ||||||||
| 13 | left | 52.3 | F | 3 | 28.4 | Yes | - | 1 | 2 | 55 | 40 | 20 | ||
| right | 51.9 | 28.4 | 2 | 55 | 40 | 15 | ||||||||
| 14 | left | 36.8 | F | 2 | 21.2 | - | >5y | 1 | 2 | 50 | 40 | 24 | ||
| right | 37.4 | 21.2 | 2 | 60 | 45 | 21 | ||||||||
| 15 | left | 47.4 | F | 3 | 26.3 | No | >5y | 1 | 2 | 50 | 40 | 14 | ||
| right | 47.7 | 26.3 | 2 | 50 | 40 | 15 | ||||||||
| 16 | left | 36.2 | F | 3 | 15.2 | No | - | 1 | 2 | 60 | 40 | 40 | ||
| right | 36.2 | 15.2 | 2 | 60 | 40 | 40 |
0 = not performed; 1 = good result on block; 2 = no result on block.
All included patients were female. The median age at the time of surgery was 46 years - interquartile range (IQR) 16.5 - ranging from 19 to 60 years. The mean BMI was 23.3 [SD 5.95]. Prior to the operative procedure, a diagnostic SIJ block using lidocaine was done in 15 of the 16 patients. In all these 15 patients, the block yielded significant short time pain relief.
Duration of surgery of the unilateral procedure ranged between 13 and 30 minutes with a mean of 20 [SD 5.3] minutes. In four cases the operation was performed bilaterally during the same procedure (case 7, 8, 12 and 16). The mean duration of surgery in these bilateral procedures was 45 minutes [range 32-65, SD 14.2].
Two patients underwent revision surgery. In one patient (case 1), an implant caused nerve impingement due to malpositioning. The implant was withdrawn several millimeters in additional corrective surgery. After this procedure the neurological complaints diminished.
Another patient (case 8) experienced no pain relief after the first surgery despite adequate positioning of the two implants. It was our believe the complaints were the result of persistent instability possibly due to a lack of total implant surface area (ISA) over the SIJ. Therefore a few months later a third implant was placed providing added stability which resulted in an excellent outcome.
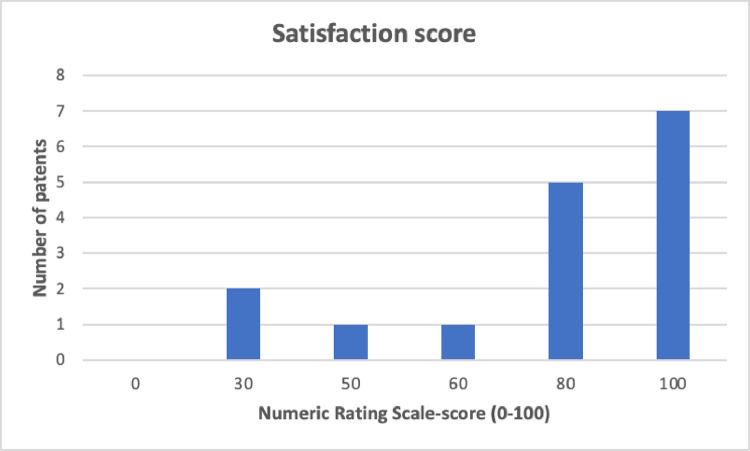
Patient follow up
The mean time between surgery and completion of the questionnaire was 36 months (range 16 – 74 months). 100% satisfaction was reported in seven patients. The mean satisfaction score is 78.1 out of 100 (Table 2). Only three patients score their satisfaction below 50 (Fig. 3). As we analyze the agree/disagree questions we see that these three patients score worse on all questions. These patients indicated that they did not notice any improvement. Their complaints have not improved after surgery and their daily functioning has not improved.
Table 2.
Results.
| Case | Question 1 | Question 2 | Question 3 | Question 4 | Question 5 | Question 6 | Question 7 | Question 8 | Question 9 | Satisfaction performance scale* |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 4 | 4 | 4 | 4 | 4 | 5 | 3 | 2 | 48 |
| 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 77 |
| 3 | 1 | 1 | 2 | 3 | 2 | 2 | 1 | 1 | 1 | 100 |
| 4 | 2 | 2 | 3 | 2 | 2 | 1 | 2 | 2 | 2 | 81 |
| 5 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 2 | 100 |
| 6 | 3 | 3 | 4 | 2 | 2 | 2 | 2 | 2 | 2 | 76 |
| 7 | 1 | 1 | 1 | 2 | 4 | 4 | 1 | 1 | 1 | 100 |
| 8 | 5 | 2 | 5 | 5 | 5 | 5 | 2 | 2 | 1 | 27 |
| 9 | 2 | 2 | 3 | 2 | 2 | 2 | 1 | 1 | 1 | 75 |
| 10 | 3 | 2 | 4 | 3 | 2 | 1 | 2 | 3 | 2 | 61 |
| 11 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 100 |
| 12 | 2 | 1 | 4 | 2 | 2 | 2 | 2 | 2 | 1 | 80 |
| 13 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 100 |
| 14 | 1 | 2 | 4 | 2 | 2 | 2 | 1 | 1 | 1 | 100 |
| 15 | 1 | 1 | 4 | 2 | 2 | 2 | 1 | 1 | 2 | 100 |
| 16 | 4 | 4 | 5 | 5 | 5 | 5 | 3 | 4 | 3 | 25 |
| Mean | 2,1 | 1,8 | 3,3 | 2,4 | 2,4 | 2,3 | 1,7 | 1,7 | 1,5 | 78,1 |
1 Strongly agree * (0-100).
2 Agree.
3 Neutral.
4 Disagree.
5 Strongly disagree.
Fig. 3.
Satisfaction score.
Seven patients strongly confirmed that the complaints that existed before surgery had decreased. But if we see question 3 – I am free of complaints after the treatment – only 2 patients strongly agree and 3 patients agree. This means in most patients the complaints decreased, but do not disappear completely.
In 15 patients two implants were placed and one patient received three implants. Postoperative CT scans were analyzed and in particular the position of the implants of patients who were less satisfied was compared with the position of more satisfied patients.
Notable, the implants in patients who are less satisfied, have less surface contact with the SIJ. Also, in one patient who was less satisfied an iliac fracture was seen nearby an implant.
Discussion
Our findings suggest that SIJ fusion is effective in EDS patients with lower back pain due to SIJ dysfunction. These patients showed improvements in multiple patient-reported parameters, including pain, quality of life and disability after SIJ fusion. These improvements in pain, disability and quality of life in our study were similar to results reported in other studies concerning patients with lower back pain due to SIJ dysfunction without EDS [1,2].
Movements and disbalance in SIJ in EDS patients may cause pain. After stabilizing the SIJ, it is hypothesized that the pain generator is removed [11]. Proper implant position is important in achieving pain relief. A postoperative CT scan for checking implant positioning is recommended, especially when patients show neurological complaints or when pain persists several months after surgery. When the CT scan shows implant malposition in patients with persisting pain, revision surgery may result in a satisfactory outcome.
In this cohort in almost all patient 2 implants were placed. A study by Lindsey et al [15]. demonstrates that placement of 3 implants across the SI joint resulted in the most stable construct, which may imply that 3 implants are more effective [16]. This might influence our results. Additional studies may be required to examine the best position of the implants.
Although the current study sample size is relatively small with 16 cases, the results are encouraging.
To our knowledge, this is the first study showing the results of SIJ fusion in EDS patients. Favorable outcomes in this study clarify the necessity to suspect hypermobility in the SIJ as a pain generator in patients with EDS. Results of SIJ fusion were comparable to patients without EDS [1,2].
Physicians are encouraged to investigate the sacroiliac joint more as a potential pain generator in patients presenting with EDS, hypermobility and lower back pain. Moreover, further studies of minimally invasive SI joint fusion for the relief of lower back pain in EDS patients are warranted.
Conclusion
SIJ-fusion for the treatment of SIJ dysfunction in patients with Ehlers Danlos Syndrome has received limited attention in the literature. This current study suggests that SIJ fusion using triangular implants bridging and stabilizing the joint is a safe and useful procedure to reduce pain and function levels in EDS patients with lower back pain due to SIJ dysfunction.
Informed Patient Consent
The authors declare that informed patient consent was taken from all the patients.
Declaration of Competing Interest
The authors declare no conflict of interest.
Author & funding disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
No relevant financial activities outside the submitted work.
The manuscript submitted does not contain information about medical device(s)/drug(s).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2021.100082.
Appendix. Supplementary materials
References
- 1.Smith-Petersen MN. Arthrodesis of the sacroiliac joint. A new method of approach. J Bone Joint Surg Am. 1921;3(8):400–405. [Google Scholar]
- 2.Martin CT, Haase L, Lender PA, Polly DW. Minimally invasive sacroiliac joint fusion: the current evidence. Int J Spine Surg. 2020;14(Suppl 1):20–29. doi: 10.14444/6072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore MR. Diagnosis and surgical treatment of chronic painful sacroiliac dysfunction: the integrated function of the lumbar spine and sacroiliac joint. (The Integrated Function of the Lumbar Spine and Sacroiliac Joint. ECO Rotter- dam, San Diego, CA, USA. 1995:339–345. [Google Scholar]
- 4.Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006;9(1):61–67. [PubMed] [Google Scholar]
- 5.Pool-Goudzwaard AL, Vleeming A, Stoeckart R, Snijders CJ, Mens JM. Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to 'a-specific' low back pain. Man Ther. 1998;3(1):12–20. doi: 10.1054/math.1998.0311. [DOI] [PubMed] [Google Scholar]
- 6.Polly DW, Cher DJ, Wine KD, Whang PG, Frank CJ, Harvey CF, et al. Randomized controlled trial of minimally invasive sacroiliac joint fusion using triangular titanium implants vs nonsurgical management for sacroiliac joint dysfunction: 12-month outcomes. Neurosurgery. 2015;77(5):674–690. doi: 10.1227/NEU.0000000000000988. discussion 690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac joint pain and its treatment. Clin Spine Surg. 2016;29(2):42–48. doi: 10.1097/BSD.0000000000000359. [DOI] [PubMed] [Google Scholar]
- 8.Dengler J, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Gaetani P, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Joint Surg Am. 2019;101(5):400–411. doi: 10.2106/JBJS.18.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gazit Y, Jacob G, Grahame R. Ehlers-Danlos syndrome-hypermobility type: a much neglected multisystemic disorder. Rambam Maimonides Med J. 2016;7(4):e0034. doi: 10.5041/RMMJ.10261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK) Am J Med Genet. 1998;77(1):31–37. doi: 10.1002/(sici)1096-8628(19980428)77:1<31::aid-ajmg8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 11.Shirley ED, Demaio M, Bodurtha J. Ehlers-Danlos syndrome in orthopaedics: etiology, diagnosis, and treatment implications. Sports Health. 2012;4(5):394–403. doi: 10.1177/1941738112452385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malfait F, Wenstrup RJ, De Paepe A. Clinical and genetic aspects of Ehlers-Danlos syndrome, classic type. Genet Med. 2010;12(10):597–605. doi: 10.1097/GIM.0b013e3181eed412. [DOI] [PubMed] [Google Scholar]
- 13.Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK) Am J Med Genet. 1998;77(1):31–37. doi: 10.1002/(sici)1096-8628(19980428)77:1<31::aid-ajmg8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 14.Miklovic T, Sieg VC. StatPearls Publishing LLC; StatPearls Treasure Island (FL): 2020. Ehlers Danlos syndrome. [PubMed] [Google Scholar]
- 15.Lindsey DP, Kiapour A, Yerby SA, Goel VK. Sacroiliac joint stability: Finite element analysis of implant number, orientation, and superior implant length. World J Orthop. 2018;9(3):14–23. doi: 10.5312/wjo.v9.i3.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dale M, Evans J, Carter K, O'Connell S, Morgan H, Carolan-Rees G. iFuse Implant System for Treating Chronic Sacroiliac Joint Pain: A NICE Medical Technology Guidance. Appl Health Econ Health Policy. 2020;18(3):363–373. doi: 10.1007/s40258-019-00539-7. [DOI] [PubMed] [Google Scholar]
- 17.Knoef RJH, Nellensteijn JM, van Vugt AB, Zeegers AVCM. The development of a tailored health-related outcomes set in patients with sacroiliac joint (SIJ) instability. ICHOM conference. Poster presentation 2020/11.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.