Abstract
Background
Traumatic pseudomeningocele are usually a late consequence of cervical root avulsion injury and its occurrence in lumbosacral region is rare. This pathology is mostly due to violent blunt traumatic events and usually develops outside of the spinal canal. Occasionally, a pseudomeningocele may grow inside of the spinal canal causing delayed neurological deficit due to compromise of the adjacent neural structures.
Case description
Evaluation of a delayed left lower extremity weakness in a young man with a history of a gunshot wound injury revealed an extradural pseudomeningocele arising from an S1 root avulsion injury with compressive effect on the adjacent L5 root
Outcome
Excision of the cyst wall and reinstitution of the nerve root sheath resulted in an uneventful recovery
Conclusion
To the best of our knowledge, the presented case with traumatic pseudomeningocele is the first example secondary to high velocity bullet injury. Furthermore, management of traumatic intraspinal pseudomeningocele subsequent to root avulsion injury has not been paid sufficient attention. In this paper, the surgical strategy will be discussed in detail.
Keywords: Bullet injury, Gunshot wound, Lumbosacral spine, Pseudomeningocele; War trauma
Introduction
Lumbosacral root avulsion injury may rarely result in formation of a traumatic pseudomeningocele [1], [2], [3], [4], [5]. The mechanism of pseudomeningocele development is a rupture of the arachnoid cuff of a nerve root with the subsequent expansion of the corresponding root sleeve wall due to free and pulsatile flow of cerebrospinal fluid [6].
The first example of intraspinal traumatic lumbosacral pseudomeningocele secondary to root avulsion was reported by Nosik in 1955 and since that time roughly 30 additional cases have been published within medical literature [7]. All of these cases except one which was due to stab wound were secondary to blunt traumas.
Herein we present a young man with a remote lower leg weakness due to the gradual expansion of a traumatic intraspinal lumbosacral pseudomeningocele which was a late sequel of S1 root avulsion injury caused by a bullet injury.
Case presentation
A 20- year- old Iraqi militia member was referred to our clinic with symptoms of progressive left foot drop. He had a history of a bullet related injury which had occurred 2 years earlier. The bullet had entered in the left paraspinal muscles and was finally embedded in contralateral psoas muscle without causing visceral injury. However, 18 months later he noticed a pin prick needle-like sensation in his left foot that gradually became associated with an accompanying weakness while standing on his heels. His neurological exam was compatible with a 2/5 weakness of the dorsiflexion of his left foot. He also clearly displayed a diminished left ankle jerk. Lumbar MRI disclosed a left sided cystic mass extending from the lower border of L4 to S1 (Figs. 1 and 2).
Fig. 1.
Lumbosacral sagittal MRI, (a) T2 weighted image showing a hyperintense mass at the caudal part of lumbar spine; (b) T1 weighted image with hypointense mass compatible with cystic mass (white arrows).
Fig. 2.
Axial T2-weighted image at L5-S1 level shows a left-sided cyst with extension to the foramen (white arrows).
Operation
After an L4, L5 and upper S1 hemilaminectomy, a left sided cyst with a thickened wall lying alongside the thecal sac was demonstrated (Fig. 3). The cyst wall itself was gradually shrunk with the utilization of bipolar cautery. Subsequently, the left L5 root which had bowed at rostral pole of the cyst, was then meticulously separated from the cysts wall and released. Then, with the continuation of shrinkage, it was found that the cyst in fact has been an expansion of the S1 nerve root sheath. At this stage, the shrunken cyst was incised longitudinally along the direction of the root. Within the space and at the depth of the cavity, intact nerve rootlets with a normal continuity were clearly identified (Figs. 4 and 5). In addition to these findings, the slow flow of the cerebrospinal fluid could be visualized with use of the Valsalva maneuver. The final stage involved the careful excision of the excess cystic wall tissue. and reconstruction of a new root sleeve, with the suturing of the remaining edges of the cyst (Fig. 6).
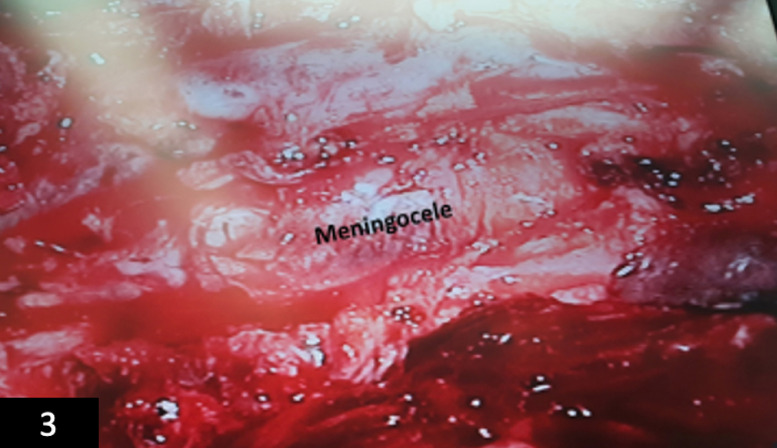
Fig. 3.
Intraoperative image demonstrating the pseudomeningocele.
Fig. 4.
Intraoperative photograph, showing expanded S1 sleeve, note that S1 rootlets are in continuity and are intact.
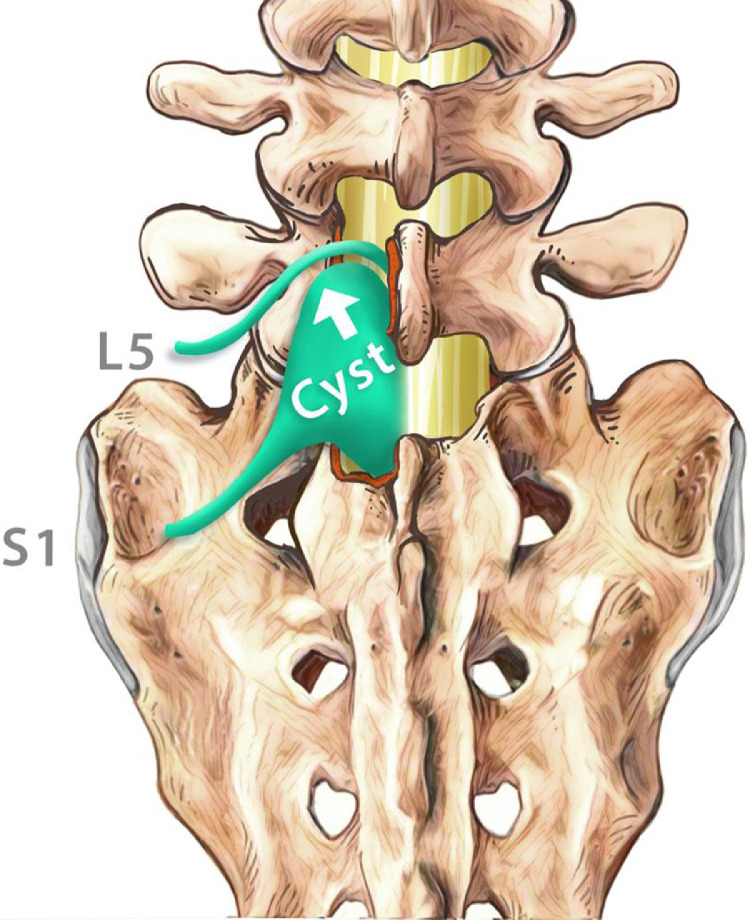
Fig. 5.
Schematic drawing showing that the pseudomeningocele has arisen from left S1 root with compressive effect on L5, note bowing of L5 root.
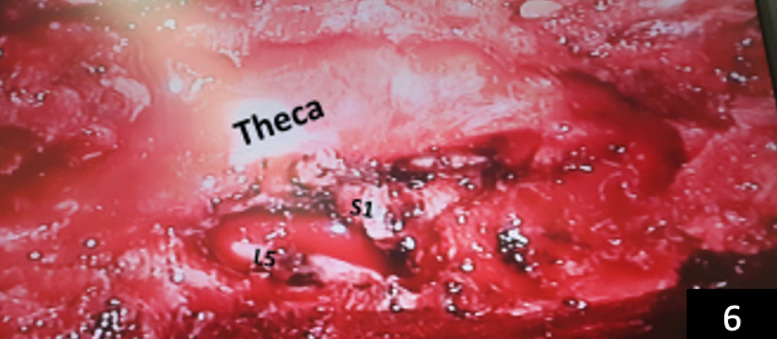
Fig. 6.
Intraoperative image demonstrating L5 root, reconstructed S1 root and decompressed theca.
Postoperative course
During a six-month follow up encounter, the patient's foot strength had improved. MRI at this stage showed no abnormal pathology (Fig. 7). At three- year follow-up, he reports none of the previously mentioned deficits.
Fig. 7.
postoperative T2-weight axial showing hemi-laminectomy (white arrow), note there is no cystic mass.
Discussion
Traumatic intraspinal pseudomeningocele formation secondary to lumbosacral root avulsion injury is a rare medical entity and has seldom been described within medical literature [[1], [2], [3], [4], [5],7].
Pathogenesis
The dura and underlying arachnoid layer extend from the emerging point of the root for about 8–10 mm. The violent vibration of a blunt trauma being directed toward a nerve root may result in the disruption of the nerve root arachnoid sleeve [1], [2], [3], [4], [5]. This causes a subsequent one-way flow of the CSF into the root chamber. When this situation occurs, the nerve rootlets are usually disrupted which results in an immediate neurological deficit [1], [2], [3], [4], [5]. Less frequently, the corresponding rootlets may remain intact and preserve their continuity. In both scenarios, with the one-way entrance of the cerebrospinal fluid and its gradual accumulation within the root chamber, the nerve root sheath eventually expands and a cyst or a pseudomeningocele develops [1], [2], [3], [4], [5], [6], [7]. Such a pseudomeningocele may also gradually create a mass effect on adjacent nerve roots or theca causing a delayed neurological manifestation. These events will vary in time from months to years.
In fact, a very similar scenario had occurred in our patient. However, instead of the vibratory effects being induced by a blunt force trauma, the vibration was created by the bullet itself, in association with the increased abdominal pressure induced by the traversing of the bullet into the retroperitoneal region have been probably the mechanism of the avulsion.
Management: In most frequent scenario where both the arachnoid cuff and the rootlets are torn, in order to relieve the pressure on adjacent neural structures, the base of the pseudomeningocele should be sutured or tied tightly nearest to the theca.
In a less frequent scenario where the rootlets remain intact, partial excision of the cyst wall and reinstitution of the root sleeve should be done.
Conclusion
Both blunt and penetrating lumbopelvic traumatic events may result in formation of a traumatic pseudomeningocele subsequent to root avulsion injury. A pseudomeningocele, is in fact gradual expansion of the root sleeve caused by pulsatile cerebrospinal fluid flow. Traumatic pseudomeningoceles usually develop outside the spinal column, but in rare occasions, their formation may take place in the spinal canal. An expansile pseudomeningocele may cause delayed neurological impairment due to its compressive effect on adjacent neural structures.
Declaration of competing Interest
None to declare.
Acknowledgments
Ethical approval Approved!
Consent Written informed consent was obtained from the patient for publication and corresponding images.
Funding
None!
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2020.100025.
Contributor Information
Abolfazl Rahimizadeh, Email: a_rahimizadeh@hotmail.com.
Seyed Amirhossein Javadi, Email: javadi1978@yahoo.com.
Appendix. Supplementary materials
References
- 1.Banno T., Ohishi T., Suzuki D., Honda Y., Kobayashi S., Matsuyama Y. Traumatic sacral pseudomeningocele with spina bifida occulta: case report. J Neurosurg. 2012;16(1):78–81. doi: 10.3171/2011.8.SPINE11190. [DOI] [PubMed] [Google Scholar]
- 2.Barberá J., Broseta J., Argüelles F., Barcia-Salorio J.L. Traumatic lumbosacral meningocele: case report. J Neurosurg. 1977;46(4):536–541. doi: 10.3171/jns.1977.46.4.0536. [DOI] [PubMed] [Google Scholar]
- 3.Carlson D.H., Hoffman H.B. Lumbosacral traumatic meningocele: report of a case. Neurology. 1971;21(2) doi: 10.1212/wnl.21.2.174. 174-174. [DOI] [PubMed] [Google Scholar]
- 4.Foley J.A., Rao R.D. Traumatic lumbosacral pseudomeningocele associated with spinal fracture. Spine J. 2009;9(11):e5–e10. doi: 10.1016/j.spinee.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Hadley M.N., Carter P.L. Sacral fracture with pseudomeningocele and cerebrospinal fluid fistula: case report and review of the literature. Neurosurgery. 1985;16(6):843–846. doi: 10.1227/00006123-198506000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Rahimizadeh A., Ehteshami S., Yazdi T., Rahimizadeh S. Remote paraparesis due to a traumatic extradural arachnoid cyst developing 2 years after brachial plexus root avulsion injury: case report and review of the literature. J Brachial Plexus Peripheral Nerve Inj. 2015;10(01):e43–e49. doi: 10.1055/s-0035-1558426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nosik W.A. Intracranial hypotension secondary to lumbar nerve sleeve tear. J Am Med Assoc. 1955;157(13):1110–1111. doi: 10.1001/jama.1955.02950300038008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.