Abstract
Objectives
This study aimed to investigate the patterns of pediatric patients visiting emergency departments (EDs) before and after the COVID-19 pandemic and evaluate the interactive effect between the COVID-19 outbreak and age groups.
Methods
We performed a cross-sectional study using the nationwide emergency patient database in Korea from January 2019 to December 2020. Pediatric patients (≤18 years) who visited all 402 nationwide EDs were included. The age- and sex-standardized incidence rates of pediatric ED visits per 1,000,000 person-days were calculated, and the incidence rate ratio (IRR) was calculated. The adjusted odds ratio (aOR) and 95% confidence interval (CI) of in-hospital mortality were calculated by a multivariable logistic regression.
Results
Among 2,808,756 patients, 1,835,045 (65.3%) patients visited before COVID-19, and 973,711 (34.7%) patients visited after the COVID-19 period. The standardized incidence rates of ED visits per 1,000,000 person-days were 589.3 in the before COVID-19 group and 326.9 in the after COVID-19 group (IRR (95% CI): 0.55 (0.53–0.58)). By diagnosis, the IRRs (95% CI) of mental health disorders (0.84 (0.42–1.65)) and self-harm or suicidal attempts (0.99 (0.38–2.59) were not significant, while the incidence rate of infectious disease was significantly decreased (0.48 (0.42–0.54)). The aOR (95% CI) of in-hospital mortality after COVID-19 was 1.58 (1.44–1.73) compared to that before COVID-19.
Conclusions
During the COVID-19 pandemic, the incidence of pediatric ED visits decreased, and these effects differed by age group. Age-specific policies are needed to ensure that children receive the care they need at the right time.
Keywords: COVID-19, Pediatrics, Emergency department utilization
Abbreviations: COVID-19, coronavirus disease 2019; ED, emergency department; IRR, incidence rate ratio; OR, odds ratio; CI, confidence interval
1. Introduction
Coronavirus disease 2019 (COVID-19) spread rapidly to many countries, and the World Health Organization (WHO) declared a pandemic on March 11, 2020 [1,2]. Worldwide, more than 278 million cases of COVID-19 and 5.4 million cumulative deaths were reported by the WHO in December 2021 [3,4]. The Centers for Disease Control and Prevention (CDC) in China and the United States estimated that 1.3% and 1.7% of patients diagnosed with COVID-19 were children, respectively [5,6]. The reported pediatric cases represent 2.2% in Italy (≤18 year-old) and 3.3% and 2.9% in Germany and Austria (<15 year-old), respectively. [7] Although the proportion of children among all COVID-19 patients is known to be relatively small, studies investigating the disease burden of COVID-19 among children are limited.
The COVID-19 outbreak is known to be associated with an unprecedented decline in emergency department (ED) utilization [[8], [9], [10], [11]]. As an effect of the COVID-19 pandemic, there have been daily changes in routine activities and health care delivery [1,12]. Among pediatric patients, health care use has also been affected by policies, such as “stay-at-home” orders and school closures, and the rate of ED visits by children has decreased during the COVID-19 pandemic [13]. Changes in these policies or environments may have different effects depending on the age of the children. Health care delivery for infants and children was mainly related to household and care centers, and delivery for adolescents was affected by school life, education, and social relationships [13,14].
The emergence of infectious disease had different health effects depending on the age of the pediatric patients [13,15]. Differences in the immune capacity with age in pediatrics influence disease patterns. At a young age, the function of the immune system can decrease due to physiological immaturity, and low immunity increases susceptibility to infections [16]. The infectious outbreak and related policies could have caused decreases in health care use in pediatrics; however, there are limited studies concerning age-specific differences in health care use declines among pediatric patients.
We hypothesize that ED utilization among pediatric patients declined during the COVID-19 pandemic and that the pattern of decline might vary by age group. The purposes of this study were to evaluate the patterns of ED visits among children before and after the COVID-19 pandemic and assess age-specific differences in the effects of the COVID-19 outbreak on pediatric ED visits.
2. Methods
2.1. Study design and setting
A cross-sectional study was conducted using a nationwide emergency patient database. Korea has more than 50 million people and 17 administrative divisions. The Ministry of Health and Welfare designed three levels of ED depending on the availability of human resources, facilities, and equipment. There are 402 nationwide EDs classified into three levels as follows: 38 Level I EDs, 128 Level II EDs, and 236 Level III EDs. Level I and Level II EDs provide the highest level emergency care services. The Ministry of Health and Welfare designated specialized emergency medical centers for trauma and pediatric or mental health diseases. In total, 9 pediatric-specialized EDs were designated in 2016, and 7 additional pediatric-specialized EDs were designated in September 2020.
The COVID-19 infection monitoring and surveillance response system in Korea was initiated on December 31, 2019, when patients with pneumonia of an unknown cause were reported in Wuhan, China [12]. The first case of COVID-19 in Korea was detected on January 20, 2020. During the early phase of the COVID-19 outbreak (February and March 2020), there were several shut down events of the EDs because COVID-19 confirmed cases were detected among the patients admitted to the ED [11]. In March 2020, the Ministry of Health and Welfare designated and operated the Severe Emergency Medical Care Centers (SEMC) to treat appropriately suspected and confirmed COVID-19 patients and to protect other uninfected emergency patients from infection. The information on resources, including available isolation units and beds in the SEMC, was shared in real time through the web-based national emergency care information system [17].
To prevent the spread of COVID-19, the government announced a physical distancing policy on March 22, 2020. As the national crisis warning level increased, the Ministry of Education decided to postpone new semester opening dates for kindergartens and schools on February 2, 2020. As an alternative to closures, the government offered emergency childcare services to kindergartens and online classes to schools. Students have taken online or offline classes since May 20, 2020. The Ministry of Education announced plans of physical attendance for all students starting in the second semester of 2021.
2.2. Data source
This study was conducted using the National Emergency Department Information System (NEDIS) database in Korea from January 2019 to December 2020. The NEDIS is a nationwide database operated by the National Emergency Medical Center under the Ministry of Health and Welfare since 2003. All patient-related information is automatically transferred in real time from each hospital to the central government server. Inaccurate data are filtered by a data processing system. The NEDIS includes the demographic and clinical information of all patients who visited EDs across the country, such as patient demographics (such as sex, age, residential area, and insurance), symptoms (chief complaints, onset of symptoms, and reason for visit), prehospital factors (ambulance use and prehospital care), and ED (vital signs, triage, emergency operative procedures, diagnosis codes based on the International Classification of Disease 10th Edition-based (ICD-10), disposition, and final clinical outcomes) information [11,18].
2.3. Study population
Pediatric patients (0–18 years old) who visited any of the 402 nationwide EDs before and after the COVID-19 pandemic (January 1, 2019, to December 31, 2019, as before COVID-19 and January 1, 2020, to December 31, 2020, as after COVID-19) were included to compare the impact of the COVID-19 outbreak after controlling for seasonal variations. We excluded patients who visited EDs for nonmedical purposes and did not meet the emergency physician criteria.
2.4. Study outcomes and measurements
The primary outcome was the incidence of ED visits with specific diagnoses (infectious disease, mental health disorders, and injury) [[19], [20], [21]]. Injury includes self-harm or suicidal attempts and violence or assault. The secondary outcome was in-hospital mortality.
The following demographic and clinical variables were collected from the NEDIS: patient demographics (age and sex) and prehospital ED factors (ambulance use, region of ED, level of ED, initial triage, diagnosis, reason for ED visit, intentionality of injury, and dispositions). The patients' age at the ED visit was categorized into the following four groups: 0–1-, 1–6-, 7–12-, and 13–18-year-old groups. The ED regions were classified into the following three categories according to the population density: metropolitan areas, urban areas, and rural areas.
2.5. Statistical analysis
A descriptive analysis of all pediatric patients visiting EDs was performed by age group and specific diagnosis. The age- and sex-standardized incidence rates of pediatric ED visits per 1,000,000 person-days were calculated using the 2020 mid-year census population in the Korean Statistical Information Service (KOSIS) database from Statistics Korea. We calculated the incidence rate difference (IRD) and incidence rate ratio (IRR) before and after the COVID-19 pandemic to estimate the size of the effect of the COVID-19 pandemic on ED visits among pediatric patients by age group and diagnosis.
The adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were calculated by a multivariable logistic regression after adjusting for age, sex, and ED region, which were potential confounders, and an interaction analysis was conducted with an interaction term (COVID-19 periods × age).
The database construction and statistical analysis were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). The significance level was 0.05.
2.6. Ethics statement
This study was approved by the Institutional Review Board of the National Medical Center (IRB No. NMC-2021-04-044), and the requirement for informed consent was waived due to the retrospective nature of this study.
2.7. Patient and public involvement statement
The National Emergency Medical Center under the Ministry of Health and Welfare was involved in the design and conduct of this research, but it was not possible to involve patients in our research.
3. Results
We identified 2,808,756 pediatric patients who visited EDs from January 1, 2019, to December 31, 2020. Among them, 1,835,045 patients visited EDs before the COVID-19 period, and 973,711 patients visited EDs after the COVID-19 period (Table 1 ). By age group, the 1–6-year-old group was the largest at 903,320 (49.2%) before COVID-19 and 429,441 (44.1%) after COVID-19. Although the overall characteristics after COVID-19 decreased by approximately 50% compared to those before COVID-19, ambulance use (125,383 (6.8%) before COVID-19 vs. 80,942 (8.3%) after COVID-19), intensive care unit (ICU) admission (6360 (0.3%) vs. 5283 (0.5%)), and in-hospital mortality (978 (0.1%) vs. 854 (0.1%)) showed a different pattern. By diagnosis, the number of patients with mental health disorders (6750 (0.4%) vs. 5515 (0.6%)), injury (572,574 (31.2%) vs. 389,974 (40.1%)), and self-harm and suicide attempts (3061 (0.2%) vs. 2962 (0.3%)) also slightly decreased after COVID-19 (Table 1, Supplementary Tables 2 and 3).
Table 1.
Demographic characteristics of pediatric patients visiting emergency departments.
| Before COVID-19 (Jan 2019 – Dec 2019) |
After COVID-19 (Jan 2020 – Dec 2020) |
p-value | |
|---|---|---|---|
| Total | 1,835,045 (100.0) | 973,711 (100.0) | |
| Age groups, years | <0.01 | ||
| 0–1 | 143,987 (7.8) | 74,593 (7.7) | |
| 1–6 | 903,320 (49.2) | 429,441 (44.1) | |
| 7–12 | 402,781 (21.9) | 223,258(22.9) | |
| 13–18 | 384,957 (21.0) | 246,419 (25.3) | |
| Sex | 0.29 | ||
| Male | 1037,173 (56.5) | 550,983 (56.6) | |
| Female | 797,872 (43.5) | 422,728 (43.4) | |
| Region | <0.01 | ||
| Metropolitan | 1,180,715 (64.3) | 603,483 (62.0) | |
| Urban | 556,066 (30.3) | 311,888 (32.0) | |
| Rural | 98,264 (5.4) | 58,340 (6.0) | |
| Ambulance use | 125,383 (6.8) | 80,942 (8.3) | <0.01 |
| Level of ED | <0.01 | ||
| Level 1 | 483,610 (26.4) | 249,105 (25.6) | |
| Level 2 | 870,696 (47.4) | 468,363 (48.1) | |
| Level 3 | 480,739 (26.2) | 256,243 (26.3) | |
| Patient triage (KTAS) | <0.01 | ||
| Emergency (level 1–2) | 47,983 (2.6) | 27,317 (2.8) | |
| Urgent (level 3) | 557,858 (30.4) | 275,560 (28.3) | |
| Less urgent (level 4–5) | 1,130,251 (61.6) | 621,548 (63.8) | |
| Unknown | 98,953 (5.4) | 49,286 (5.1) | |
| Diagnosis | |||
| Infectious disease | 289,728 (15.8) | 133,273 (13.7) | <0.01 |
| Mental health disorders | 6750 (0.4) | 5515 (0.6) | <0.01 |
| Injury | 572,574 (31.2) | 389,974 (40.1) | <0.01 |
| Self-harm or suicidal attempts | 3061 (0.2) | 2962 (0.3) | <0.01 |
| Violence or assault | 5422 (0.3) | 3099 (0.3) | <0.01 |
| Admission | 173,220 (9.4) | 91,625 (9.4) | 0.42 |
| ICU | 6360 (0.3) | 5283 (0.5) | <0.01 |
| Hospital ward | 166,860 (9.1) | 86,342 (8.9) | <0.01 |
| In-hospital mortality | 978 (0.1) | 854 (0.1) | <0.01 |
| ED | 637 (0.0) | 555 (0.1) | <0.01 |
| Hospital ward | 341 (0.0) | 299 (0.0) | <0.01 |
COVID-19, coronavirus disease 2019; Jan, January; Dec, December; ED, emergency department; KTAS, Korean triage and acuity scale; ICU, intensive care unit.
Table 2 shows the demographic characteristics of pediatric patients visiting EDs by age group. After the COVID-19 period, the proportion of ambulance use increased in all four age groups. The decrease in the number of patients with injury was alleviated in the groups aged 0–12 years. A similar pattern was observed in the number of patients diagnosed with mental health disorders in the 13–18-year-old group. The number of patients seen due to violence or assault among infants (under 1 year old) increased from 14 before the COVID-19 period to 29 after the COVID-19 period. For infectious disease, the number of visits was 289,728 before COVID-19 and 133,273 after COVID-19 (Supplementary Table 1). Regarding mental health disorders, the 13–18-year-old group was the largest at 5719 (84.7%) before COVID-19 and 4786 (86.8%) after COVID-19 (Supplementary Table 2). After the COVID-19 period, the proportions of admission and in-hospital mortality increased in all three diagnosis groups during the study period (Supplementary Tables 1–3).
Table 2.
Demographic characteristics of pediatric patients visiting emergency departments by age group.
| Age, 0–1 |
Age, 1–6 |
Age, 7–12 |
Age, 13–18 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before COVID-19 | After COVID-19 | Before COVID-19 | After COVID-19 | Before COVID-19 | After COVID-19 | Before COVID-19 | After COVID-19 | |||||||||
| Total | 143,987 | (100.0) | 74,593 | (100.0) | 903,320 | (100.0) | 429,441 | (100.0) | 402,781 | (100.0) | 223,258 | (100.0) | 384,957 | (100.0) | 246,419 | (100.0) |
| Sex | ||||||||||||||||
| Male | 80,410 | (44.2) | 41,936 | (43.8) | 506,494 | (43.9) | 243,846 | (43.2) | 240,403 | (40.3) | 132,955 | (40.4) | 209,866 | (45.5) | 132,246 | (46.3) |
| Female | 63,577 | (55.8) | 32,657 | (56.2) | 396,826 | (56.1) | 185,595 | (56.8) | 162,378 | (59.7) | 90,303 | (59.6) | 175,091 | (54.5) | 114,173 | (53.7) |
| Region | ||||||||||||||||
| Metropolitan | 110,927 | (77.0) | 56,244 | (75.4) | 602,425 | (66.7) | 276,270 | (64.3) | 239,040 | (59.3) | 127,494 | (57.1) | 228,323 | (59.3) | 143,475 | (58.2) |
| Urban | 31,404 | (21.8) | 17,266 | (23.1) | 265,650 | (29.4) | 133,964 | (31.2) | 133,421 | (33.1) | 77,601 | (34.8) | 125,591 | (32.6) | 83,057 | (33.7) |
| Rural | 1656 | (1.2) | 1083 | (1.5) | 35,245 | (3.9) | 19,207 | (4.5) | 30,320 | (7.5) | 18,163 | (8.1) | 31,043 | (8.1) | 19,887 | (8.1) |
| Ambulance use | 9304 | (6.5) | 6457 | (8.7) | 49,336 | (5.5) | 27,372 | (6.4) | 22,354 | (5.5) | 15,532 | (7.0) | 44,389 | (11.5) | 31,581 | (12.8) |
| Level of ED | ||||||||||||||||
| Level 1 | 62,296 | (43.2) | 31,800 | (42.6) | 269,327 | (29.8) | 125,197 | (29.2) | 84,359 | (20.9) | 46,860 | (21.0) | 67,628 | (17.6) | 45,248 | (18.4) |
| Level 2 | 72,195 | (50.1) | 38,218 | (51.2) | 452,948 | (50.1) | 217,412 | (50.6) | 182,755 | (45.4) | 102,505 | (45.9) | 162,798 | (42.3) | 110,228 | (44.7) |
| Level 3 | 9496 | (6.6) | 4575 | (6.1) | 181,045 | (20.0) | 86,832 | (20.2) | 135,667 | (33.7) | 73,893 | (33.1) | 154,531 | (40.1) | 90,943 | (36.9) |
| Patient triage (KTAS) | ||||||||||||||||
| Emergency (level 1–2) | 18,154 | (12.6) | 10,754 | (14.4) | 19,114 | (2.1) | 8770 | (2.0) | 4341 | (1.1) | 3030 | (1.4) | 6374 | (1.7) | 4763 | (1.9) |
| Urgent (level 3) | 63,358 | (44.0) | 30,039 | (40.3) | 301,318 | (33.4) | 119,007 | (27.7) | 97,150 | (24.1) | 56,923 | (25.5) | 96,032 | (24.9) | 69,591 | (28.2) |
| Less urgent (level 4–5) | 61,044 | (42.4) | 32,837 | (44.0) | 547,629 | (60.6) | 285,115 | (66.4) | 271,616 | (67.4) | 148,595 | (66.6) | 249,962 | (64.9) | 155,001 | (62.9) |
| Unknown | 1431 | (0.1) | 963 | (1.3) | 35,259 | (3.9) | 16,549 | (3.9) | 29,674 | (7.4) | 14,710 | (6.6) | 32,589 | (8.5) | 17,064 | (6.9) |
| Diagnosis | ||||||||||||||||
| Infectious disease | 20,848 | (14.5) | 8246 | (11.1) | 134,418 | (14.9) | 44,660 | (10.4) | 70,121 | (17.4) | 37,379 | (16.7) | 64,341 | (16.7) | 42,988 | (17.4) |
| Mental health disorders | 49 | (0.0) | 50 | (0.1) | 301 | (0.0) | 161 | (0.0) | 681 | (0.2) | 518 | (0.2) | 5719 | (1.5) | 4786 | (1.9) |
| Injury | 26,244 | (18.2) | 19,144 | (25.7) | 269,902 | (29.9) | 198,580 | (46.2) | 144,901 | (36.0) | 91,094 | (40.8) | 131,527 | (34.2) | 81,156 | (32.9) |
| Self-harm or suicidal attempts | 0 | (0.0) | 0 | (0.0) | 6 | (0.0) | 4 | (0.0) | 106 | (0.0) | 85 | (0.0) | 2949 | (0.8) | 2873 | (1.2) |
| Violence or assault | 14 | (0.0) | 29 | (0.0) | 242 | (0.0) | 161 | (0.0) | 1037 | (0.3) | 472 | (0.2) | 4129 | (1.1) | 2437 | (1.0) |
| Admission | 30,100 | (20.9) | 17,634 | (23.6) | 70,830 | (7.8) | 26,939 | (6.3) | 33,028 | (8.2) | 19,494 | (8.7) | 39,262 | (10.2) | 27,558 | (11.2) |
| ICU | 3264 | (2.3) | 2681 | (3.6) | 911 | (0.1) | 661 | (0.2) | 638 | (0.2) | 536 | (0.2) | 1547 | (0.4) | 1405 | (0.6) |
| Hospital ward | 26,836 | (18.6) | 14,953 | (20.0) | 69,919 | (7.7) | 26,278 | (6.1) | 32,390 | (8.0) | 18,958 | (8.5) | 37,715 | (9.8) | 26,153 | (10.6) |
| In-hospital mortality | 254 | (0.2) | 229 | (0.3) | 235 | (0.0) | 171 | (0.0) | 129 | (0.0) | 139 | (0.1) | 360 | (0.1) | 315 | (0.1) |
| ED | 180 | (0.1) | 168 | (0.2) | 137 | (0.0) | 95 | (0.0) | 72 | (0.0) | 76 | (0.0) | 248 | (0.1) | 216 | (0.1) |
| Hospital ward | 74 | (0.1) | 61 | (0.1) | 98 | (0.0) | 76 | (0.0) | 57 | (0.0) | 63 | (0.0) | 112 | (0.0) | 99 | (0.0) |
COVID-19, coronavirus disease 2019; Jan, January; Dec, December; ED, emergency department; KTAS, Korean triage and acuity scale; ICU, intensive care unit.
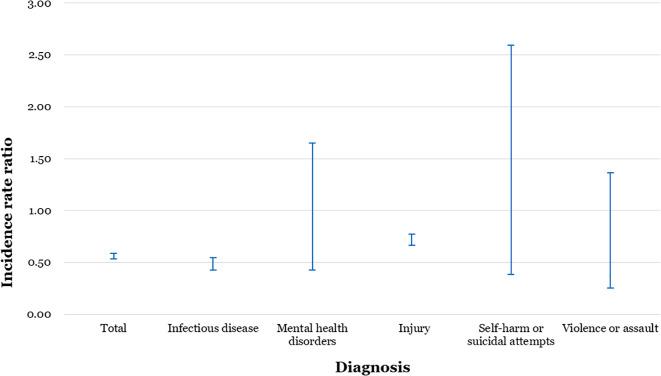
The standardized incidence rates of pediatric ED visits per 1,000,000 person-days were 589.3 before the COVID-19 period and 326.9 after the COVID-19 period (Table 3 ). The IRR (95% CI) of all pediatric ED visits was 0.55 (0.53–0.58). By diagnosis, the IRRs (95% CI) of mental health disorders (0.84 (0.42–1.65)) and self-harm or suicidal attempts (0.99 (0.38–2.59)) were not significant, while the incidence rate of infectious disease was significantly decreased (IRR (95% CI): 0.48 (0.42–0.54)) (Table 3, Figure 1 ).
Table 3.
Standardized incidence rates of pediatric patients visiting emergency departments by age group and diagnosis.
| Before COVID-19 (Jan 2019 – Dec 2019) |
After COVID-19 (Jan 2020 – Dec 2020) |
Rate difference |
Rate ratio |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate⁎ | 95% CI | Rate⁎ | 95% CI | Diff | 95% CI | Ratio | 95% CI | |||||
| Total | 589.3 | 573.0 | 605.6 | 326.9 | 314.5 | 339.3 | −262.4 | −282.9 | −242.0 | 0.55 | 0.53 | 0.58 |
| Age, years | ||||||||||||
| 0–1 | 1336.5 | 1204.6 | 1468.3 | 771.1 | 665.3 | 876.8 | −565.4 | −734.4 | −396.4 | 0.58 | 0.49 | 0.68 |
| 1–6 | 1017.7 | 977.6 | 1057.8 | 512.2 | 482.9 | 541.5 | −505.5 | −555.1 | −455.9 | 0.50 | 0.47 | 0.54 |
| 7–12 | 386.7 | 363.9 | 409.5 | 218.5 | 201.2 | 235.8 | −168.2 | −196.8 | −139.5 | 0.57 | 0.51 | 0.62 |
| 13–18 | 362.8 | 340.9 | 384.7 | 237.4 | 219.5 | 255.4 | −125.3 | −153.6 | −97.0 | 0.65 | 0.59 | 0.72 |
| Diagnosis | ||||||||||||
| Infectious disease | 93.1 | 86.6 | 99.6 | 44.6 | 40.0 | 49.2 | −48.5 | −56.4 | −40.6 | 0.48 | 0.42 | 0.54 |
| Mental health disorders | 2.2 | 1.2 | 3.2 | 1.8 | 0.9 | 2.8 | −0.4 | −1.7 | 1.0 | 0.84 | 0.42 | 1.65 |
| Injury | 184.2 | 175.1 | 193.3 | 130.9 | 123.1 | 138.8 | −53.2 | −65.3 | −41.2 | 0.71 | 0.66 | 0.77 |
| Self-harm or suicidal attempts | 1.0 | 0.3 | 1.7 | 1.0 | 0.3 | 1.7 | 0.0 | −1.0 | 1.0 | 0.99 | 0.38 | 2.59 |
| Violence or assault | 1.8 | 0.9 | 2.7 | 1.0 | 0.3 | 1.7 | −0.7 | −1.9 | 0.4 | 0.59 | 0.25 | 1.36 |
COVID-19, coronavirus disease 2019; Jan, January; Dec, December; Diff, difference; CI, confidence interval.
Age- and sex-standardized incidence rates per 1,000,000 person-days were calculated using the 2020 mid-year census population.
Fig. 1.
Standardized incidence rate ratios of pediatric patients visiting emergency departments by diagnosis.
The aOR (95% CI) of in-hospital mortality after COVID-19 compared to that before COVID-19 was 1.58 (1.44–1.73) (Table 4 ). In the interaction analysis performed to evaluate the effect modification of the COVID-19 period by age, the aORs (95% CIs) of in-hospital mortality were 1.75 (1.46–2.09) in the 0–1-year-old group, 1.54 (1.26–1.87) in the 1–6-year-old group, 1.95 (1.54–2.48) in the 7–12-year-old group, and 1.37 (1.18–1.60) in the 13–18-year-old group (P-for-interaction <0.05).
Table 4.
The risk of in-hospital mortality after COVID-19 compared to that before COVID-19 among pediatric patients visiting emergency departments
| Odds ratio⁎ | 95% CI | ||
|---|---|---|---|
| After COVID-19 vs. before COVID-19 | |||
| Total population | 1.58 | 1.44 | 1.73 |
| Interaction effect between COVID-19 periods and age | |||
| 0–1 | 1.75 | 1.46 | 2.09 |
| 1–6 | 1.54 | 1.26 | 1.87 |
| 7–12 | 1.95 | 1.54 | 2.48 |
| 13–18 | 1.37 | 1.18 | 1.60 |
COVID-19, coronavirus disease 2019; CI, confidence interval.
⁎ Adjustment for COVID-19 periods, age, gender and region of emergency departments, P for interaction <0.05.
4. Discussion
This cross-sectional study used a nationwide emergency patient database and evaluated the impact of the COVID-19 pandemic on pediatric ED visits and whether these effects differed by age group. During the COVID-19 outbreak, the incidence rates of pediatric patients who visited EDs decreased compared with those in the corresponding period (IRR (95% CI): 0.55 (0.53–0.58)), and there was an interaction effect between the COVID-19 outbreak and age groups on in-hospital mortality (P-for-interaction <0.05). During the COVID-19 pandemic, the proportions of ED visits for mental health diseases and self-harm or suicide attempts in the 13–18-year-old group increased, and the number of ED visits for violence or assault among infants also increased. These results emphasize that the COVID-19 pandemic appears to have significantly different impacts on pediatric patients by age. Age-specific policies are needed to ensure that children receive the care they need at the right time to treat potentially preventable diseases.
Several studies have reported a decrease in ED visits in pediatric patients during the COVID-19 pandemic [[22], [23], [24]]. The absolute number of all pediatric ED visits decreased; however, the patterns of decreases differ by the characteristics of illness. In this study, the proportions of patients with high acuity by triage (2.6% and 2.8%, p < 0.01) and those with ambulance use (6.8% and 8.3%, p < 0.01) increased, while the total number of ED visits decreased. EDs have attempted to maintain services for pediatric patients with higher acuity during the pandemic.
COVID-19 has affected various pediatric conditions [25,26]. In terms of infectious illnesses, which are the most common reasons for pediatric ED visits, the prevalence in children younger than 6 years decreased in this study. Interventions, such as using masks, school closures, handwashing, and physical distancing, to reduce the spread of COVID-19 have impacted the reduction in the incidence of other infectious diseases, such as seasonal influenza [25,27]. Self-isolation, quarantine, and worry about COVID-19 transmission in the ED might lead to a decrease in pediatric ED visits [24,25].
There were increases in ED visits for mental health diseases and self-harm or suicidal attempts, especially among the 13–18-year-old group. This result is consistent with the MMWR report from the CDC; the proportion of children's mental health visits increased 44% in 2020 compared with that in 2019 [13]. Many mental disorders occur in childhood, and mental health problems in these groups could be exacerbated by stress and anxiety related to the pandemic, disconnection from school, and sudden disturbances in daily life [28]. This increase also likely occurred because adolescents who usually received mental health care were not receiving services on time due to the mitigation policy of COVID-19 [13].
In terms of injury, changes in children's environment, including stay-at-home orders, could pose various threats, such as injuries in the home or child abuse or neglect [23,29]. For example, there was a report of a threefold increase in ED visits for children bitten by dogs [30]. In this study, the number of ED visits due to violence or assault increased from 14 to 29 among infants (younger than 1 year old) after COVID-19. Uncontrolled emotional stress could increase the risk of young children's exposure to intimate caregiver violence, especially within the family [29,31]. The number of COVID-19 cases has not shown a noticeable decrease, although vaccination has started. There is a strong need to investigate the characteristics of pediatric patients who visit EDs, one of the most vulnerable populations to pandemic disasters, and develop age-specific interventions to correctly utilize the appropriate health care services to treat potentially preventable diseases.
This study has several limitations. First, since this study is an observational study and not a randomized controlled trial, there is a limitation in causal reasoning. Therefore, further studies evaluating causality are needed. Second, patients with mental health diseases were defined based on the diagnosis codes in the NEDIS database. It is impossible to distinguish whether pediatric patients with mental health diseases who visited EDs were previously diagnosed with mental disorders or were newly diagnosed during their visits to the ED. Third, the information concerning self-harm or violence/assault was collected only from Level 1 and Level 2 EDs, and the possibility of underestimation exists.
During the COVID-19 pandemic, the incidence of pediatric ED visits decreased, and these effects differed by age group; the proportions of ED visits for mental health diseases and self-harm or suicidal attempts increased among those aged older than 13 years, and the number of ED visits for violence or assault among infants also increased. Close monitoring and age-specific policies are needed to ensure that children receive the care they need at the right time to treat potentially preventable diseases.
Author contributions
Approval of final manuscript: all authors.
Funding
There was no funding for this study.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2022.02.009.
Appendix A. Supplementary data
Demographics of pediatric patients with diagnosis
References
- 1.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. J Pediatr. 2020;145 [Google Scholar]
- 2.World Health Organization Timeline: WHO's COVID-19 Response 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#! updated 24 Jan, 2021. Available from.
- 3.World Health Organization Weekly epidemiological update on COVID-19: World Health Organization. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---6-april-2021 2021 [updated 6 April. Available from.
- 4.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. Jama. 2020;323:1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 5.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Bialek Stephanie, Gierke Ryan, Michelle Hughes A.L., McNamara Tamara Pilishvili, et al. 2020. Coronavirus disease 2019 in children—United States, February 12–April 2; p. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carroll W., Strenger V., Eber E., Porcaro F., Cutrera R., Fitzgerald D., et al. European and United Kingdom COVID-19 pandemic experience: the same but different. Paediatr Respir Rev. 2020;35:50–56. doi: 10.1016/j.prrv.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodríguez-Leor O., Álvarez B.C., Ojeda S., Moreiras J.M., Cuevas J.R.R., Palop R.L., et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC: Intervent Cardiol. 2020;2(2):82–89. [Google Scholar]
- 10.Thornton J. Covid-19: a&E visits in England fall by 25% in week after lockdown. Br Med J. 2020;369 doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 11.Lee D.E., Ro Y.S., Ryoo H.W., Moon S. Impact of temporary closures of emergency departments during the COVID-19 outbreak on clinical outcomes for emergency patients in a metropolitan area. Am J Emerg Med. 2021;47:35–41. doi: 10.1016/j.ajem.2021.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pak Y.-S., Ro Y.S., Kim S.-H., Han S.-H., Ko S.-k., Kim T., et al. Effects of emergency care-related health policies during the COVID-19 pandemic in Korea: a quasi-experimental study. J Korean Med Sci. 2021;36 doi: 10.3346/jkms.2021.36.e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leeb R.T., Bitsko R.H., Radhakrishnan L., Martinez P., Njai R., Holland K.M. Mental health–related emergency department visits among children aged< 18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. Morb Mort Weekly Report. 2020;69(45):1675. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brady M.T. Infectious disease in pediatric out-of-home child care. Am J Infect Control. 2005;33(5):276–285. doi: 10.1016/j.ajic.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Heiber M., Lou W.W. Effect of the SARS outbreak on visits to a community hospital emergency department. Canadian J Emerg Med. 2006;8(5):323–328. doi: 10.1017/s148180350001397x. [DOI] [PubMed] [Google Scholar]
- 16.Valiathan R., Ashman M., Asthana D. Effects of ageing on the immune system: infants to elderly. Scand J Immunol. 2016;83(4):255–266. doi: 10.1111/sji.12413. [DOI] [PubMed] [Google Scholar]
- 17.Pak Y.S., Ro Y.S., Kim S.H., Han S.H., Ko S.K., Kim T., et al. Effects of emergency care-related health policies during the COVID-19 pandemic in Korea: a quasi-experimental study. J Korean Med Sci. 2021;36(16) doi: 10.3346/jkms.2021.36.e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung E., Ro Y.S., Ryu H.H., Do Shin S., Moon SJJoKms. Vol. 36. 2021. Interaction Effects between COVID-19 Outbreak and Community Income Levels on Excess Mortality among Patients Visiting Emergency Departments; p. 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J., Shin S.D., Im T.H., Lee K.J., Ko S.B., Park J.O., et al. Development and validation of the excess mortality ratio–adjusted injury severity score using the international classification of diseases 10th edition. Acad Emerg Med. 2009;16:454–464. doi: 10.1111/j.1553-2712.2009.00412.x. [DOI] [PubMed] [Google Scholar]
- 20.Lo C.B., Bridge J.A., Shi J., Ludwig L., Stanley R.M. Children’s mental health emergency department visits: 2007–2016. Pediatrics. 2020;145 doi: 10.1542/peds.2019-1536. [DOI] [PubMed] [Google Scholar]
- 21.Smith M.L., Farkas D.K., Sumner J.A., Jiang T., Lash T.L., Galea S., et al. Associations between adjustment disorder and hospital-based infections in the Danish population. J Psychosom Res. 2020;132 doi: 10.1016/j.jpsychores.2020.109976. [DOI] [PubMed] [Google Scholar]
- 22.Angoulvant F., Ouldali N., Yang D.D., Filser M., Gajdos V., Rybak A., et al. Coronavirus disease 2019 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections—a time series analysis. Clin Infect Dis. 2021;72(2):319–322. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaiyachati B.H., Agawu A., Zorc J.J., Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J Pediatr. 2020;226(274–7) doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scaramuzza A., Tagliaferri F., Bonetti L., Soliani M., Morotti F., Bellone S., et al. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020;105(7):704–706. doi: 10.1136/archdischild-2020-319397. [DOI] [PubMed] [Google Scholar]
- 25.Kocher K.E., Macy M.L. Emergency department patients in the early months of the coronavirus disease 2019 (COVID-19) pandemic—what have we learned? JAMA Health Forum. 2020;1(6) doi: 10.1001/jamahealthforum.2020.0705. [DOI] [PubMed] [Google Scholar]
- 26.DeLaroche A.M., Rodean J., Aronson P.L., Fleegler E.W., Florin T.A., Goyal M., et al. Pediatric emergency department visits at US Children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;147(4) doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- 27.Sakamoto H., Ishikane M., Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. Jama. 2020;323(19):1969–1971. doi: 10.1001/jama.2020.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 29.Humphreys K.L., Myint M.T., Zeanah C.H. Increased risk for family violence during the COVID-19 pandemic. Pediatrics. 2020;146(1) doi: 10.1542/peds.2020-0982. [DOI] [PubMed] [Google Scholar]
- 30.Dixon C.A., Mistry R.D. Dog bites in children surge during coronavirus Disease-2019: a case for enhanced prevention. J Pediatr. 2020;225:231–232. doi: 10.1016/j.jpeds.2020.06.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vu N.L., Jouriles E.N., McDonald R., Rosenfield D. Children’s exposure to intimate partner violence: a meta-analysis of longitudinal associations with child adjustment problems. Clin Psychol Rev. 2016;46:25–33. doi: 10.1016/j.cpr.2016.04.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demographics of pediatric patients with diagnosis