Abstract
Context:
Oral cancer is one of the ten most common cancers in the world. More than 95% of the carcinomas of the oral cavity are of squamous cell type in nature. Oral Candida is a “yeast-like opportunistic pathogen.” The Candida genus is comprised of over 150 species of asporogenous “yeast-like” fungi.
Aim and Objectives:
The aim of study is to correlate the association of oral fungal infection in progression of oral squamous cell carcinoma (OSCC) and potentially malignant disorders. The current study was undertaken to probe the isolation and identification of oral Candida species in potentially malignant disorder and OSCC versus normal oral mucosa.
Materials and Methods:
Twenty patients for each abovementioned three lesions were randomly selected by using swabs. These swabs were subsequently inoculated in agar medium. Candida grows as white, convex colonies. Samples growing 1–3 colony-forming units (CFUs) were considered normal flora of the oral cavity. The specimens showing moderate to heavy growth were subjected to tests for identification of species of Candida. The chromogenic medium, HiMedia CHROMagar, has chromogenic substances which helps in the quick detection of Candida species, based on the reactions between the extract enzymes of the dissimilar species and the chromogenic substances.
Statistical Analysis:
Chi-square test, one-way analysis of variance test, and post hoc Tukey's test were utilized.
Results:
According to our study, Candida albicans, Candida krusei, Candida tropicalis, and Candida parapsilosis in the culture were found to be in increasing incidence from healthy, OSCC, and oral potentially malignant disorders (OPMDs). These results clearly indicated that Candida species are increasing in the CFUs (P < 0.0001).
Conclusion:
Our study showed a higher intensity of Candida in OPMD and squamous cell carcinoma patients with results. The increasing CFU level and hyphae of Candida species in individual biopsy tissue with oral potentially malignant lesions to OSCC suggest that this pathogen plays a role in disease development and could aid in identifying the pathogenic commensal.
Keywords: Candida, CHROMagar, oral squamous cell carcinoma, potentially malignant disorders, Sabouraud dextrose agar
INTRODUCTION
Oral Candida is a “yeast-like opportunistic pathogen.” Depending on the host defense mechanisms or local oral microenvironment, Candida can transform from a harmless commensal to pathogenic organism causing oral mucosal infection. Among these more important pathogenic species are Candida albicans, Candida tropicalis, Candida parapsilosis, Candida krusei, Candida lusitaniae, and Candida glabrata. C. albicans is the primary cause of oral candidiasis.[1] Oral squamous cell carcinoma (OSCC) accounts for 5% of all cancers in men and 2% in women. Candida is among the etiologic risk factors of OSCC, which is part of normal oral flora. Candida infection may occur probably due to weakening of the immune system. Candida organisms are normal commensals that are found colonizing the oral mucosa frequently.
Oral cancer is a multifactorial disease and besides with many potentially malignant disorders. Chronic oral candidiasis is rarely but can transform into oral cancer. Candida as a pathogen can cause both outward and systemic diseases.
Candida can then produce carcinogenic compounds, such as nitrosamines and N-nitrosobenzylmethylamine. Strains with high nitrosation potential were isolated from lesions with more advanced precancerous changes. The yeast cells in such cases extend from the mucosal surface to the deeper epithelial cell layers representing transport and deposition of precursors like nitrosamines to deeper layers. This showed that certain strains of C. albicans play a key role in the development of dysplasia.[2] The possible association between Candida species and oral neoplasia was first reported in the 1960s (Cawson, 1969, and Williamson, 1969), with later reports suggesting a link between the presence of C. albicans in the oral cavity and the development of OSCC (Bastiaan and Reade, 1982, and Rodriguez et al., 2007).[3]
The ability of C. albicans to colonize, penetrate, and damage host tissues depends on an imbalance between C. albicans virulence factors and host defenses, often due to specific defects in the immune system. C. albicans virulence factors and adherence to mucosal or artificial surfaces in the mouth have been extensively reviewed. Two different mechanisms by which C. albicans can invade keratinocytes have been proposed. One mechanism involves the secretion of degradative enzymes by the fungus, particularly secreted aspartic proteases that can digest epithelial cell surface components and thereby allow the physical movement of hyphae into, or between, host cells. The second proposed mechanism is the induction of epithelial cell endocytosis.[4] Hence, the aim of study is to correlate the association of oral fungal infection in progression of OSCC and potentially malignant disorders.
MATERIALS AND METHODS
The current study was undertaken to probe the isolation and identification of oral Candida species in potentially malignant disorder and OSCC versus normal oral mucosa. Twenty patients for each abovementioned three lesions were randomly selected as provided in institute ethical clearance certificate No. 811718/OP/EC.
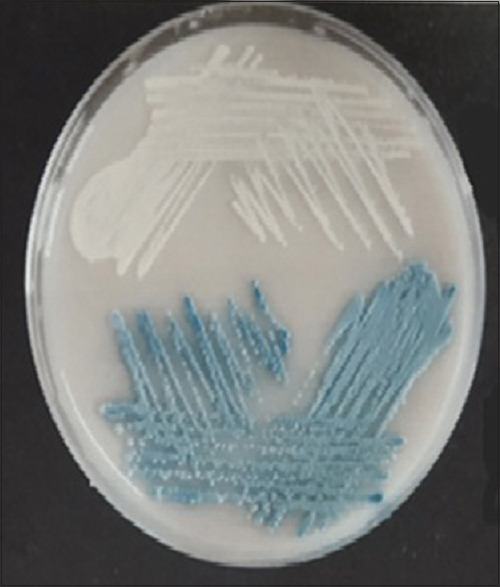
Salivary swab was collected from the patients who have been clinically/histopathologically confirmed with oral potentially malignant disorder (OPMD) and OSCC. These swabs were subsequently inoculated in Sabouraud dextrose agar (SDA) medium. The SDA is inoculated aerobically for 24–48 h. Candida grows as white, convex colonies. Samples growing 1–3 colony-forming units (CFUs) were considered normal flora of the oral cavity. The specimens showing moderate to heavy growth were subjected to tests for identification of species of Candida[5] [Figure 1].
Figure 1.

Candida albicans colonies on Sabouraud agar
The chromogenic medium, HiMedia CHROMagar, has chromogenic substances which helps in the quick detection of Candida species, based on the reactions between the extract enzymes of the dissimilar species and the chromogenic substances[6] [Figure 2].
Figure 2.
Cell culture plate containing Candida parapsilosis, Candida tropicalis
RESULTS
Inferential statistics were performed using Chi-square test and one-way analysis of variance (ANOVA) test. Chi-square test is used to compare categorical data. Intergroup comparison of colony counts is compared using one-way ANOVA test. Post hoc pairwise comparison was done using post hoc Tukey's test.
Demographic distribution of study participants according to gender [Table 1 and Graph 1]
Table 1.
Demographic distribution of study participants according to gender
| Sex | Total | |||
|---|---|---|---|---|
|
| ||||
| Males | Females | |||
| OSCC | n | 17 | 3 | 20 |
| % | 85.0 | 15.0 | 100.0 | |
| PMD | n | 14 | 6 | 20 |
| % | 70.0 | 30.0 | 100.0 | |
| Normal | n | 10 | 10 | 20 |
| % | 50.0 | 50.0 | 100.0 | |
| Total | n | 41 | 19 | 60 |
| % | 68.3 | 31.7 | 100.0 | |
| P value | 0.058, NS | |||
OSCC: Oral squamous cell carcinoma, PMD: Potentially malignant disorder, NS: Not significant
Graph 1.
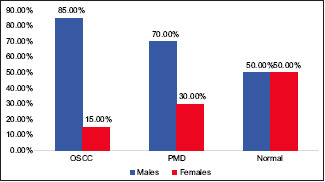
Demographic distribution of study participants according to gender
In this study, 60 cases were included, out of which 20 cases were of OPMD, out of which 14 were males and 6 were females. Out of 20 cases of OSCC, there were more male patients than females that included 17 males and 3 females.
Mean age distribution of study participants [Table 2 and Graph 2]
Table 2.
Mean age distribution of study participates
| Age (years) | |||||
|---|---|---|---|---|---|
|
| |||||
| N | Mean | Sth. deviation | 95% confidence interval for mean | ||
|
| |||||
| Lower bound | Upper bound | ||||
| OSCC | 20 | 55.8000 | 13.50867 | 49.4777 | 62.1223 |
| PMD | 20 | 43.7500 | 11.02091 | 38.5921 | 48.9079 |
| Normal | 20 | 39.3500 | 11.92642 | 33.7683 | 44.9317 |
| P value | <0.0001, S | ||||
| P value of post hoc pairwise comparison | 1>2,3 1*2–0.008 1*3-<0.0001 2*3–0.493 |
||||
OSCC: Oral squamous cell carcinoma, PMD: Potentially malignant disorder, S: Significant, SD: Standard deviation, CI: Confidence interval
Graph 2.
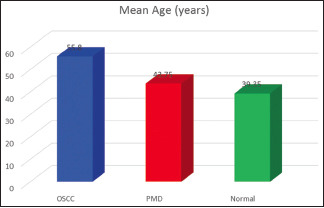
Mean age distribution of study participates
Patients in this study ranged from 14 to 78 years. OPMD patients were in the age range of the 3rd –6th decade of life (mean age: 45 years). OSCC patients were older in their 6th decade of life (mean age: 54 years). This distribution was statistically highly significant with a probability value of 0.001.
Comparison of the presence of Candida species among oral potentially malignant disorder, oral squamous cell carcinoma, and healthy control [Table 3 and Graph 3]
Table 3.
Comparison of the presence of candida species among oral potentially malignant disorder. Oral squamous cell carcinoma, and healthy control
| Growth of C. albicans | Total | ||
|---|---|---|---|
|
| |||
| Present | |||
| OSCC | N | 20 | 20 |
| % | 100.0% | 100.0% | |
| PMD | N | 20 | 20 |
| % | 100.0% | 100.0% | |
| Normal | N | 20 | 20 |
| % | 100.0% | 100.0% | |
| Total | N | 60 | 60 |
| % | 100.0% | 100.0% | |
| P value |
OSCC: Oral squamous cell carcinoma, PMD: Potentially malignant disorder
Graph 3.
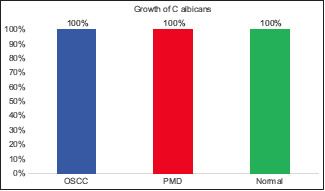
Comparison of the presence of candida species among oral potentially malignant disorder. Oral squamous cell carcinoma, and healthy control
When the presence of Candida species among study groups was compared, the most prevalent Candida species was C. albicans (100.0%) in OSCC patients.
In the OSCC Group, C. albicans was the most commonly cultured species accounting for 100.0%, followed by C. krusei (78.3%), C. tropicalis (55.0%), and C. parapsilosis (35%).
In the OPMD group, the most common cultured species was C. albicans (100.0%), followed by C. krusei (95%), C. tropicalis (60%), and C parapsilosis (30%). In healthy individuals, the most commonly cultured species was C. albicans and C. krusei (40%) followed by C. tropicalis (20%) and C. parapsilosis (10%).
These findings were statistically significant with a probability value of 0.001.
DISCUSSION
C. albicans is the most commonly implicated organism in this condition. C. albicans is carried in the mouths of about 50% of the world's population as a normal commensal component of the oral microbiota. Oral cancer is one of the ten most common cancers in the world. The term oral cancer includes a diverse group of tumors arising from the oral cavity. More than 95% of the carcinomas of the oral cavity are of squamous cell type in nature.[7]
The Candida species are indigenous to the human oral cavity and can produce a variety of oral infections. These findings are consistent with the results of the present study, in which OPMD and OSCC samples gave positive colonies from saliva and swab samples of the oral cavity. Studies have shown that C. albicans is the most commonly isolated pathogen from the oral cavity and that it is the most virulent of the Candida species. This may be because C. albicans is also able to produce various virulence factors.[8] These results clearly indicated that Candida spp. are increasing in the colony forming units. This study showed that Candida is more prevalent in healthy, oral squamous cell carcinoma (OSCC) Potential Malignant Disorders (PMD). Also the fact that healthy case has increasing prevalence of Candida albicans Candida krusei [Figure 3].
Figure 3.

Is Candida krusei
The intergroup comparison of colony counts of C albicans was done using one-way ANOVA. Overall, a statistically significant difference was found in colony counts of C. albicans among cases of OSCC, potentially malignant disorder (PMD), and normal. Post hoc pairwise comparison was done using post hoc Tukey's test, and it was found that mean colony counts of C. albicans among PMD cases were significantly higher than that among PMD, which also showed a statistically significant difference as compared to that among normal controls.
Diagnosis of oral candidiasis is not always performed, and a presumptive diagnosis is often the only one made, based on the patient's history, clinical presentation, and response to antifungal treatment rather than on cultural and histological methods. In the OSCC Group, C. albicans was the most commonly cultured species accounting for 100.0%, followed by C. krusei (78.3%), C. tropicalis (55.0%), and C. parapsilosis (35%). In the OPMD group, the most common cultured species was C. albicans (100.0%), followed by C. krusei (95%), C. tropicalis (60%), and C. parapsilosis (30%). In healthy individuals, the most commonly cultured species was C. albicans and C. krusei (40%), followed by C. tropicalis (20%) and C. parapsilosis (10%).
In case of Candida species, we found that the incidence of Candida albicans is positivity was significantly higher in Squamous Cell Carcinoma group as compared to Oral Potentially Malignant Disorders and healthy groups (p<0.0001). Minimum positivity for Candida species in dish was in Healthy group.
Our results related to counting of colony formation of Candida species in healthy, OSCC, and OPMD were found that Candida species was significantly associated with potentially malignant disorders and oral cancers (OSCC).
CONCLUSION
The aims of our study were to evaluate CFUs of Candida spp. in the healthy, OSCC and OPMD patients.
C. albicans and C. krusei, C. tropicalis, C. parapsilosis were seen on the cultured media petri dish that include HiCrome agar media and CFU is counted by using Chi-square method that included counting of CFU in four segments of petri dish.
In case of Candida species, we found that the incidence of Candida albicans positivity was significantly higher in Squamous Cell Carcinoma group as compared to Oral Potentially Malignant Disorders and healthy groups (P<0.0001). Minimum positivity for Candida species was in Healthy group. Minimum positivity for Candida spp. in dish was in the healthy group.
The present study suggests that the increasing CFU level and hyphae of C. albicans in individual biopsy tissue with oral potentially malignant lesions to OSCC suggest that this pathogen plays a role in disease development and could aid in identifying the pathogenic commensal.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Williams D, Lewis M. Pathogenesis and treatment of oral candidosis. J Oral Microbiol. 2011;3:1–11. doi: 10.3402/jom.v3i0.5771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Grady JF, Reade PC. Candida albicans as a promoter of oral mucosal neoplasia. Carcinogenesis. 1992;13:783–6. doi: 10.1093/carcin/13.5.783. [DOI] [PubMed] [Google Scholar]
- 3.Daftary DK, Mehta FS, Gupta PC, Pindborg JJ. The presence of Candida in 723 oral leukoplakias among Indian villagers. Scand J Dent Res. 1972;80:75–9. doi: 10.1111/j.1600-0722.1972.tb00265.x. [DOI] [PubMed] [Google Scholar]
- 4.Cannon RD, Holmes AR, Mason AB, Monk BC. Oral Candida: Clearance, colonization, or candidiasis? J Dent Res. 1995;74:1152–61. doi: 10.1177/00220345950740050301. [DOI] [PubMed] [Google Scholar]
- 5.Samaranayake LP. Essential Microbiology for Dentistry. 2nd ed. Harcourt Publishers Limited. 2002:144. [Google Scholar]
- 6.Manikandan C, Amsath A. Isolation and rapid identification of Candida species from oral cavity. Int J Pure Appl Biosci. 2013;1:23–7. [Google Scholar]
- 7.Pindborg JJ, Reichart PA, Smith CJ, Van Der Waal I. Histological Typing of the Cancer and Precancer of Oral Mucosa. 2nd ed. Tokyo: Springer; 1997. [Google Scholar]
- 8.Bakri MM, Hussaini HM, Holmes AR, Cannon RD, Rich AM. Revisiting the association between Candidal infection and carcinoma, particularly oral squamous cell carcinoma. J Oral Microbiol. 2010:2. doi: 10.3402/jom.v2i0.5780. doi: 10.3402/jom.v2i0.5780. [DOI] [PMC free article] [PubMed] [Google Scholar]


