From 2015 to 2019, the incidence of syphilis more than doubled in Greenland. Incidence is high, especially among young females; thus, demographic characteristics are different from other Western populations.
Supplemental digital content is available in the text.
Abstract
Background
An increase in the incidence of syphilis was reported in Greenland from 2011 to 2014, and notification rates kept rising in the following years in spite of focused efforts. To better understand the syphilis epidemic, this study was conducted to describe the syphilis epidemic in Greenland from 2015 to 2019.
Methods
Syphilis cases and their characteristics were identified through reviews of electronic medical records and laboratory results in 3 different data sets: notifications to the National Board of Health, electronic prescriptions for benzathine penicillin, and the national laboratory database. Annual incidences were calculated stratified by sex, age, and region.
Results
The incidence of syphilis in Greenland increased from 107.4 to 246.8 cases per 100,000 inhabitants from 2015 to 2019. The incidence increased in both sexes and in nearly all regions, although with large regional differences. Especially the age group 15 to 29 years showed a substantial increase in incidence in 2018 and 2019. More females than males were infected (245 female cases vs. 178 male cases).
Conclusions
The burden of syphilis in Greenland is high, primarily among the age group 15 to 29 years. A higher incidence among females than among males was found, suggesting mainly heterosexual transmission, as seen for other sexually transmitted infections in Greenland.
In Greenland, the first syphilis case was noted in 1872,1 and in the 1970s and 1980s, 2 larger epidemics occurred in Greenland, reaching incidences between 1000 and 1500 cases per 100,000 inhabitants.1–3 The latter epidemic ended in the mid-1990s, most likely because of focused efforts from the healthcare authorities, combined with a stop-AIDS campaign.2,4 After nearly 2 decades with almost no cases of syphilis in Greenland, an increase in incidence from 5.3 to 85.3 cases per 100,000 inhabitants from 2011 to 2014 was reported.5 Because of this concerning increase, notification of syphilis to the National Board of Health (NBH) in Greenland became mandatory in 2012 and existing guidelines were updated, first in summer 2015 and second in autumn 2018. These guidelines provide prevention strategies including empirical treatment of all primary contacts, contact tracing with provider referral, and follow-up blood samples (at least 3, 6, and 12 months after diagnosis). The 2018 update included an option for polymerase chain reaction (PCR) analysis for Treponema pallidum infection in lesions and a change in the T. pallidum screening tests' cutoff value from 12 to 1 sample/cutoff (S/CO).
Regardless of these efforts, the number of notified cases of syphilis further increased in the following years,6,7 suggesting a syphilis epidemic on the rise. In Greenland, routine surveillance of sexually transmitted infections (STIs) is performed by the NBH. Both chlamydia and gonorrhea have been and still are highly prevalent, whereas HIV, although on the rise, is not a common infection.1,8–10 Surveillance of chlamydia and gonorrhea is based on positive test results from the national laboratory database supplied to the NBH, who cannot access this database or electronic medical records, whereas surveillance of syphilis and HIV relies on notifications to the NBH only. Unfortunately, not all cases of syphilis are notified,5 which may lead to an underestimation of incidence, and no sufficient validation of syphilis notifications is performed.
To better understand the impact of this public health concern in Greenland, it is crucial to know more about the characteristics, risk factors, diagnosis, treatment, and follow-up of cases, because these parameters have not been formally assessed on a large scale in Greenland. Considering the demography of Greenland, it is hypothesized that the follow-up shows large regional differences, which may contribute to a continuing epidemic.
Therefore, the aim of this study was to describe the syphilis epidemic in Greenland from 2015 to 2019 in terms of demographic, clinical and laboratory characteristics, treatment, and follow-up to provide basis for improved prevention strategies.
MATERIALS AND METHODS
Study Design
The study was carried out as a register-based study including all known cases of syphilis (T. pallidum infection) in Greenland from January 1, 2015, to December 31, 2019.
Setting
Greenland is an autonomous self-ruled country within the Kingdom of Denmark. The majority of the population of approximately 56,000 are Inuit (89%), and the remaining are mainly Danish.11 Universal tax paid health care insures all inhabitants, resulting in no financial barriers to accessing public health care in Greenland, including prescription medications. Private health care is not available. The population lives along the coastline in 16 towns with adjacent settlements separated by great distances, with no roads connecting the towns. The healthcare system is divided into 5 regions with one regional hospital in each and health care centers in the remaining towns. The national hospital, Queen Ingrid's Hospital, is located in the capital Nuuk, a city of 18,000 inhabitants, in the Sermersooq region.11 In Nuuk, living conditions (e.g., income and educational level) are generally higher (especially compared with settlements, where the unemployment rate is almost double as high as in towns),11,12 and specialized healthcare services are easier to access than for the rest of Greenland. Thus, for this study, we divided the Sermersooq region, which spans the inland ice from the west to the east coast, into Sermersooq West (including the capital Nuuk) and Sermersooq East (Fig. 1). To the authors' knowledge, no formal reference is found in Greenland with regard to sexual orientation, but no restrictive laws exist, and same-sex marriage is legal. Injection drugs and hard narcotics are very unusual in Greenland.
Figure 1.

Healthcare regions in Greenland. In this study, Sermersooq West: Nuuk, Paamiut, and adjacent settlements and Sermersooq East: Tasiilaq, Ittoqortoormiit, and adjacent settlements.
In the Kingdom of Denmark, every inhabitant is given a unique identification number at birth or when receiving permanent residency through the Civil Registration System (CPR number). Persons without permanent residency are given a temporary CPR number if seeking any kind of health care. The CPR number provides information on date of birth and sex and uniquely identifies the person in different registers.
Syphilis Testing in Greenland
In Greenland, indications for testing for T. pallidum infection include clinical suspicion of syphilis, primary contacts to syphilis cases, and certain patient groups (pregnant women, persons investigated for dementia, patients admitted to psychiatric ward, HIV positives, and occasionally, patients admitted for surgery). Since 2009, a chemiluminescent microparticle immunoassay detecting antibodies to T. pallidum (ARCHITECT Syphilis TP assay Abbott Laboratories; Abbott Park, IL) has been performed on blood samples at the Central Laboratory at the Queen Ingrid's Hospital, as a screening test for syphilis. If positive (≥1 S/CO), the sample is forwarded to Statens Serum Institut (SSI) in Copenhagen, Denmark, for further serological testing with nontreponemal Wassermann reaction (WR), rapid plasma reagin (RPR), and treponemal antiflagellum IgM and IgG antibodies (AF-IgM and AF-IgG). Thus, the reverse algorithm for syphilis serology testing is used.13 Serological analyses of spinal fluid and PCR analysis for T. pallidum infection in skin and mucosal lesions are also performed at the SSI. All syphilis laboratory results for Greenland from 2007 and onward, including those from the SSI, can be accessed in the national laboratory database.
Data Sources
Syphilis cases for the study period were identified through 3 data sets: (1) notifications to the NBH, (2) electronic prescriptions for benzathine penicillin in the electronic medical record system, and (3) individuals with an RPR >0 in the national laboratory database. However, because of an update in software in the national laboratory database, data extraction before March 15, 2016, was unsuccessful, why cases in the third data set were only included from hereon. Data sets were extracted in the aforementioned order, and duplicates of the same case within and between the data sets were excluded (Figure, Supplemental Digital Content 1, http://links.lww.com/OLQ/A764). For each potential case, a review of the electronic medical records from 2000 and onward, as well as laboratory results, was done. To define cases and syphilis stages, both clinical signs,14 past and present serology results,13,15 and medical history (e.g., presumed time of transmission) were assessed, after which cases where either included or excluded, according to study definitions below.
Definitions
All cases of congenital syphilis were excluded. A syphilis case was defined as an individual with a positive T. pallidum PCR test result, or a positive treponemal screening test result in combination with a positive test result in a subsequent nontreponemal test (either WR or RPR and optionally AF-IgM and AF-IgG), or, in case of lack of reference serology results, a positive screening test result in combination with clinical signs of syphilis and relevant recent exposure as noted in the medical record. In daily clinical work before 2018, only a screening value ≥12 S/CO was considered positive and elicited further analysis, but in this study, a value of ≥1 S/CO was considered positive.
An individual with a history of a previous treated infection in combination with a negative or very low RPR was considered as having had a past infection and resulted in exclusion of the case. Individuals with reinfections, defined as previously treated individuals with a primary sufficient clinical and serological response experiencing a ≥3-step increase in WR, ≥4-fold increase in RPR and/or ≥3-step increase in AF-IgG titers, or new clinical characteristics highly suggestive of syphilis, were included as new cases.
The definition of syphilis stage according to serology and clinical characteristics was based on national guidelines for Greenland and from SSI (Definitions, Supplemental Digital Content 2, http://links.lww.com/OLQ/A765). If a case could not be sufficiently accounted for in a specific stage, it was regarded as “unclassified.” The date of diagnosis was defined as the date of the blood sample with a nonspecific treponemal test (WR or RPR) or, if missing, the date of a screening or PCR test. Cases with date of diagnosis outside the study period were excluded. Region of the case was defined as the region in which sampling was performed. Medical treatment was defined as sufficient if prescribed according to Greenlandic and Danish guidelines; the latter included doxycycline in case of penicillin allergy.16
In this study, we used 4 different modes of follow-up, each evaluated individually for each case: (1) notification to the NBH, (2) tracing of contacts, (3) serological follow-up after treatment, and (4) HIV testing. Contact tracing was defined as performed when stated in the medical record. Serological follow-up was defined as performed in case of one or more subsequent blood samples (WR + RPR) after the initial diagnosis and treatment. A sufficient serological response was defined as an either ≥3-step or ≥4-fold decrease in WR or RPR titers, respectively, after treatment. If the initial RPR titer was ≤4, a subsequent decrease or stable value with no clinical indications of ongoing infection was also considered a sufficient response.
Statistical Analysis
Annual incidence of syphilis was calculated as the number of syphilis cases divided by the total population of Greenland by January 1 for the relevant year, stratified by age, sex, and region.17
Ethical Considerations
The study fulfills the Helsinki Declaration II and was approved by The Ethics Committee for Scientific Research in Greenland (no. KVUG-2018-21) and reported to the Data Protection Agency. Furthermore, approval for data extraction was given from both the Agency for Health and Prevention and the NBH in Greenland.
RESULTS
Syphilis Cases and Annual Incidence, 2015 to 2019
In the study period, 409 cases of syphilis were notified to the NBH. According to the inclusion criteria, 64 cases were excluded, but 12 nonnotified reinfections were included, leaving 357 cases in this study. The electronic prescriptions revealed an additional 23 nonnotified cases of syphilis, and the national laboratory database revealed 43 cases not previously identified (Figure, Supplemental Digital Content 1, http://links.lww.com/OLQ/A764). Thus, the total number of syphilis cases in Greenland from 2015 to 2019 was 423, 178 males and 245 females. Twenty-seven individuals were identified as cases twice, and 1 individual thrice, because of reinfections.
Median age at time of diagnosis was 26 years (range, 13–76 years), higher among male cases (29 years) than among female cases (25 years). Sixty percent of cases were tested for syphilis because of symptoms or contact tracing. Most cases were in the early stages of syphilis (primary, secondary or early latent), and all cases in the late stages were late latent cases. No cases were classified as tertiary. The majority of cases (92%) were treated with benzathine penicillin alone. Of these, 76% of cases in early stages were treated correctly with one injection (2.4 MIU), 18% were treated with 2 injections, and 6% were treated with 3 or more injections, whereas 57% of cases in late stages were treated correctly with 3 or more injections (total of 7.2 MIU) within the defined interval. Of 137 cases (32%) with information on sexual transmission, 12 (9%) were reported as men who have sex with men (MSM), and the rest as heterosexual (Table 1).
TABLE 1.
Demographic and Clinical Characteristics of Syphilis Cases (n) in Greenland, 2015 to 2019
| Years | (25%–75% Quartiles) | |
|---|---|---|
| Median age | ||
| Total | 26 | (21.0–34.5) |
| Male | 29 | (23.0–41.0) |
| Female | 25 | (20.0–31.0) |
| Demographics and clinical characteristics | n | (%) |
| Total | 423 | (100.0) |
| Sex | ||
| Male | 178 | (42.1) |
| Female | 245 | (57.9) |
| Indication for syphilis testing | ||
| Symptoms | 140 | (33.1) |
| Primary contact | 114 | (27.0) |
| Pregnancy | 20 | (4.7) |
| Surgery | 4 | (0.9) |
| Other* | 78 | (18.4) |
| Unknown | 67 | (15.8) |
| Sexual transmission | ||
| Heterosexual | 125 | (29.6) |
| MSM | 12 | (2.8) |
| Unknown | 286 | (67.6) |
| Laboratory results, blood samples | ||
| Cases with only a positive screening test available† | 12 | (2.8) |
| Cases with only a positive screening test and a positive WR or RPR available‡ | 25 | (5.9) |
| Cases with all serological results (screening test, WR + RPR and IgM + IgG) available regardless of status§¶ | 385 | (91.0) |
| Laboratory results, other | ||
| Positive intrathecal tests | 0 | (0.0) |
| Negative intrathecal tests | 6 | (1.4) |
| Positive PCR from lesion | 20 | (4.7) |
| Negative PCR from lesion | 4 | (0.9) |
| Stage of syphilis | ||
| Primary | 179 | (42.3) |
| Secondary | 38 | (9.0) |
| Tertiary | 0 | (0.0) |
| Early latent | 128 | (30.3) |
| Late latent | 66 | (15.6) |
| Unclassified | 12 | (2.8) |
| Treatment | ||
| Benzathine penicillin | 390 | (92.2) |
| 2.4 MIU | 384 | (98.5) |
| 1.2 MIU | 4 | (1.0) |
| Unknown dose | 2 | (0.5) |
| 1 injection | 267 | (68.5) |
| 2 injections | 70 | (17.9) |
| 3 injections or more | 53 | (13.6) |
| Doxycycline | 4 | (0.9) |
| Other∥ | 5 | (1.2) |
| Combination** | 9 | (2.1) |
| Unknown | 6 | (1.4) |
| None | 9 | (2.1) |
| Insufficient treatment according to guideline | 61 | (14.4) |
*For example, infection with another STI (primarily), individual's own wishes, admission to psychiatric ward, and investigation of dementia or during follow-up of already diagnosed syphilis (reinfections).
†Symptoms, medical history, and earlier laboratory results gave the diagnosis and stage when possible. One case was also PCR positive from lesion.
‡Three cases were also PCR positive from lesion.
§Giving a total of 422 cases instead of 423 cases, because one case was diagnosed by only positive PCR from lesion, no further serology (blood/sera) was positive.
¶Eight cases had a positive screening test result, negative WR + RPR, and a positive IgM (optionally IgG) at primary blood samples before treatment.
∥Regular benzylpenicillin (penicillin G) or ceftriaxone (cephalosporin).
**Benzathine penicillin + doxycycline, benzathine penicillin + other, or benzathine penicillin + doxycycline + other.
From 2015 to 2019, incidence increased from 107.4 to 246.8 cases per 100,000 inhabitants, but the incidence in 2017 was markedly lower than in previous or later years (Table 2). The increase occurred among both males and females, but for all years, incidence was higher among females than males. Average female/male incidence rate ratio over the period was 1.49 (range, 1.34–1.63). Incidence varied among the regions but increased in all, except for Sermersooq East, where the incidence was lower in 2019 than in 2015, however with an increasing trend in the later years. For persons younger than 35 years, incidence was higher in females than in males, but in persons older than that, almost similar among sexes (Fig. 2). For all years, incidence was higher in age groups younger than 30 years than in older age groups, and highest in the age group 15 to 29 years. This difference was markedly higher for the years 2018 and 2019 than for the years 2015 to 2017 (Fig. 3).
TABLE 2.
Sex- and Region-Specific Annual Incidence (I) of Syphilis Cases (n) in Greenland, 2015 to 2019, Per 100,000 Inhabitants
| Population Size* | 2015 | 2016 | 2017 | 2018 | 2019 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | I | (95% CI) | n | I | (95% CI) | n | I | (95% CI) | n | I | (95% CI) | n | I | (95% CI) | ||
| Total | 55,801 | 60 | 107.4 | (80.3–134.6) | 66 | 118.4 | (89.9–147.0) | 33 | 59.2 | (39.0–79.4) | 126 | 225.9 | (186.5–265.3) | 138 | 246.8 | (205.7–288.0) |
| Sex | ||||||||||||||||
| Male | 29,438 | 25 | 84.9 | (51.6–118.2) | 30 | 101.9 | (65.5–138.3) | 15 | 51.0 | (25.2–76.8) | 52 | 176.8 | (128.8–224.9) | 56 | 189.9 | (140.2–239.6) |
| Female | 26,363 | 35 | 132.6 | (88.7–176.5) | 36 | 137.0 | (92.3–181.7) | 18 | 68.3 | (36.8–99.9) | 74 | 280.6 | (216.8–344.5) | 82 | 310.4 | (243.3–377.4) |
| Region | ||||||||||||||||
| Avannaa | 10,572 | <5 | 18.9 | (0.0–45.0) | <5 | 9.5 | (0.0–28.2) | 0 | 0 | — | 12 | 113.4 | (49.3–177.5) | 18 | 171.1 | (92.1–250.0) |
| Disko | 6538 | <5 | 15.2 | (0.0–45.1) | 16 | 245.9 | (125.5–366.2) | 8 | 123.1 | (37.8–208.3) | 11 | 168.4 | (69.0–267.8) | 20 | 303.6 | (170.8–436.5) |
| Kujataa | 6708 | <5 | 14.3 | (0.0–42.5) | <5 | 14.7 | (0.0–43.5) | <5 | 44.8 | (0.0–95.5) | 0 | 0 | — | 10 | 155.2 | (59.1–251.4) |
| Qeqqa | 9353 | 10 | 106.4 | (40.5–172.3) | 8 | 84.9 | (26.1–143.7) | 18 | 54.1 | (6.7–101.5) | 18 | 193.7 | (104.3–283.0) | 16 | 170.0 | (86.8–253.3) |
| Sermersooq East | 3333 | 24 | 692.8 | (416.6–969.1) | 23 | 684.3 | (405.6–963.0) | 11 | 303.9 | (115.8–491.9) | 11 | 339.3 | (139.1–539.5) | 16 | 484.1 | (247.5–720.8) |
| Sermersooq West | 19,298 | 22 | 116.7 | (68.0–165.4) | 17 | 88.9 | (46.7–131.2) | 74 | 36.1 | (9.4–62.9) | 74 | 379.6 | (293.2–465.9) | 58 | 295.3 | (219.4–371.2) |
*Average population size in January 1, 2015 to 2019, but population size for each year per January 1, is used in the calculations of incidence.
Figure 2.
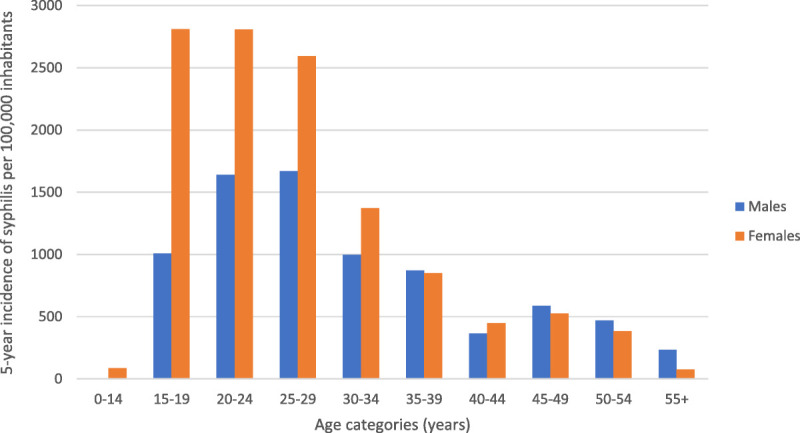
Five-year incidence of syphilis per 100,000 inhabitants by age and sex in Greenland, 2015 to 2019.
Figure 3.

Annual incidence of syphilis per 100,000 inhabitants by age in Greenland, 2015 to 2019.
Follow-Up
Table 3 shows performed follow-up by region. The overall proportion of cases notified to the NBH was 82%, with great variation among regions (range, 47%–91%). Contact tracing was performed in 76% of cases, again with regional differences (range, 27%–87%), and resulted in identification of 27% of cases (Table 1). Ninety-one percent of cases were followed up with serological follow-up, and of these, 95% had a sufficient treatment-related reduction in nontreponemal antibodies. Also, 91% had an HIV test done in relation to syphilis testing or at follow-up. In total, 4 syphilis cases were identified as HIV positive in the study period, with no difference in sex.
TABLE 3.
Region-Specific Proportion of Syphilis Cases (n) With Follow-Up in Greenland, 2015 to 2019
| Region | Total No. Cases (N) | Notification of Case to the National Board of Health | Tracing of Contacts to Case | Serological Follow-Up | HIV Testing of Case | ||||
|---|---|---|---|---|---|---|---|---|---|
| % | (n) | % | (n) | % | (n) | % | (n) | ||
| Avannaa | 33 | 81.8 | (27) | 72.7 | (24) | 75.8 | (25) | 100 | (33) |
| Disko | 56 | 66.1 | (37) | 62.5 | (35) | 91.1 | (51) | 98.2 | (55) |
| Kujataa | 15 | 46.7 | (7) | 26.7 | (<5) | 66.7 | (10) | 100 | (15) |
| Qeqqa | 57 | 89.5 | (51) | 75.4 | (43) | 93.0 | (53) | 100 | (57) |
| Sermersooq East | 84 | 90.5 | (76) | 72.6 | (61) | 96.4 | (81) | 54.0 | (47) |
| Sermersooq West | 178 | 82.6 | (147) | 86.5 | (154) | 91.6 | (163) | 99.4 | (177) |
| Total | 423 | 81.6 | (345) | 75.9 | (321) | 90.5 | (383) | 90.8 | (384) |
DISCUSSION
This study documents an overall increase in the incidence of syphilis in Greenland from 107.4 cases per 100,000 inhabitants in 2015 to 246.8 cases per 100,000 in 2019. The increase in incidence was seen in both sexes, but in all years, incidence was higher among females than males. From 2017 to 2019, a particular steep increase in incidence was caused by an increase in cases in the younger age groups (15–29 years). The incidence increased in nearly all regions, yet with large regional differences also in case follow-up.
The increase in the incidence of syphilis from 2015 to 2019 continued the increase seen from 2011 to 2014.5 Compared with Denmark, the United States, and Canada, the incidence of syphilis is high in Greenland,18–20 but similar to incidences from 2012 to 2015 in Nunavut, Canada, a region where the vast majority of the population is Inuit.19 Like in Greenland, the increase in Nunavut followed a period of low incidence. The most recent study of syphilis among Alaska Natives found no cases of primary or secondary syphilis in 2007 to 2010,21 but an increasing incidence hereafter. In 2018 in Alaska, an outbreak of syphilis was officially declared to be affecting both heterosexual men and women and MSM.22,23 In addition, Greenland, Nunavut, and Alaska have high incidence of other STIs such as chlamydia and gonorrhea,8,21,24 which indicates general challenges with sexual health.
In Greenland, incidences of chlamydia and gonorrhea are highest among young females,8,9,25 indicating mainly heterosexual transmission. This is in line with our findings for syphilis, where females between 15 and 29 years old were most frequently diagnosed. HIV transmission in Greenland is also reported to be mainly heterosexual,10,26 supported by this study, but the low number of syphilis cases with HIV indicates that HIV is not found in parallel with the syphilis epidemic in Greenland. In comparison, syphilis in Denmark, the United States, and Canada generally occurs in males and in an older age group than those infected with chlamydia and gonorrhea, and the very low proportion of infected males reporting MSM transmission in Greenland stands in direct contrast with those Western countries in general.18–20,27,28 However, for specific areas in Canada, including Nunavut, heterosexual transmission is the most common route of transmission, and in the later years, both the United States and Canada are experiencing increasing incidence among females.27,29 The higher observed incidence of syphilis among females in this study may reflect that females are routinely tested in pregnancy and more likely to be tested when seeking healthcare services for gynecological/prevention-related issues. With this in mind and the indication of mainly heterosexual transmission of syphilis and other STIs, it could be suspected that syphilis in males is underdiagnosed in Greenland, which may sustain the epidemic.
It is reassuring that only one case of congenital syphilis was revealed in the study period (Figure, Supplemental Digital Content 1, http://links.lww.com/OLQ/A764), emphasizing the value of testing in pregnancy, which provided diagnosis of 20 infected women. No cases of tertiary syphilis including neurosyphilis were diagnosed in this study, but only 1.4% of cases had cerebrospinal fluid examined; thus, neurosyphilis may be underdiagnosed.
Treatment of the early stages of syphilis was more often sufficient than for the late stages, but although many cases in late stages were treated insufficiently according to guidelines, our results show that a high percentage of cases with serological follow-up had sufficient serological responses. To our surprise, a large proportion of cases were treated with 2 injections of benzathine penicillin, which does not comply with guidelines for neither early nor late syphilis. Furthermore, a few cases were treated with single injections of regular benzylpenicillin instead of benzathine penicillin, a serious error easy to make for non–venerology-specialized healthcare professionals.30 The treatment-related issues were primarily restricted to specific regions (data not shown), and the degree of follow-up also varied among the regions, which, in combination with regionally low total numbers of syphilis cases, indicate a need for a more uniform case handling through, for example, centralization. This suggestion is supported by the fact that the region with the absolute highest annual incidence, Sermersooq East, has managed to reduce incidence for the years 2017 to 2019 compared with 2015 to 2016, probably because of expertise acquired over time, focused efforts, and strict follow-up.31s
The main strength of this study is the use of national registers with unique personal identifiers (the CPR number), electronic medical records, and a national laboratory database to ensure optimal conditions for diagnosis and staging to validate treatment and follow-up. The use of 3 different data sets to identify syphilis cases has minimized the risk of overlooking cases, although it may have led to a minor underestimation of the incidence in the early years as the data set for RPR results was not available before March 15, 2016. In addition, potential nonnotified cases with negative RPR and no prescription of benzathine penicillin are missed in this study, but because benzathine penicillin is registered as the only treatment for syphilis in Greenland guidelines during the study period, and alternative treatments, including doxycycline, were only present in 2% of cases in this study, these limitations are considered as an absolute minor risk of underestimating the incidence.
With the previous epidemics in the 1970s and 1980s in Greenland, there is a risk of falsely diagnosing a previous case as a current case with diagnosis based on serology. This challenge is illustrated by the high number of excluded notified syphilis cases in this study, which in daily clinic were considered to have a current syphilis infection. However, a risk of false-positive diagnosis and false staging in our study remains in the 9% of cases who lacked complete serology, as an estimate of diagnosis and stage was made by combining results with previous serology results, symptoms, and patient history. This limitation is mainly considered to have an impact on staging of these cases and less on diagnosis, because the medical records provided extensive information for ensuring correct diagnosis. However, it must be noted that median age of the 9% who lacked full serology was slightly higher (33 years of age) than for the total of cases, and about two-thirds of these cases were males.
The change in the treponemal screening tests' cutoff value from 12 to 1 in 2018 elicited more potential cases with complete serology, ensuring more precise diagnosis and staging, and 91% of the included cases were identified with a treponemal screening test, a nontreponemal test, and an additional treponemal antibody test. Use of this reverse algorithm for syphilis testing in Greenland is considered an advantage because the traditional algorithm has the potential to overlook cases of early primary syphilis,32s supported by results from this study (Table 1). Mandatory notification in Greenland in 2012 and changes in national guidelines during the study period might potentially have created a false increase in incidence, but the increase continued in subsequent years. Also, the change in the screenings tests' cutoff value cannot have falsely caused the increase because the increase in incidence began before the change was implemented. It may, however, have resulted in an underestimation of the incidence in the early years of the epidemic.
The estimate of the low percentage of MSM among syphilis cases in Greenland must be considered in the light of a very low coverage of reporting on sexual transmission (32% of cases).
Like chlamydia and gonorrhea, the burden of syphilis in Greenland is high; thus, improvements in sexual health are warranted. The incidence of syphilis has increased since 2011 and is for the study period highest among females and the age group 15 to 29 years. The high incidence among females, the relatively young age among the male cases, and the data on mode of transmission, although limited, suggest mainly heterosexual transmission. This is in line with other STIs in Greenland and rises suspicion on a potentially high number of undiagnosed males. Results from this study also suggest challenges with regional differences in awareness and expertise of syphilis in Greenland. Screening for syphilis should be performed with a low threshold and directed more toward the younger age groups, especially males.
Supplementary Material
For further references, please see “Supplemental References,” http://links.lww.com/OLQ/A766.
Footnotes
Acknowledgment: The authors would like to thank Silvia Isidor, Health Consultant, and the National Board of Health in Greenland for collaboration with data on notified cases of syphilis and for supporting the corresponding author with a workplace. They also thank Inge-Lise Kleist, Head of the Laboratory at Queen Ingrid's Hospital, Nils Skovgaard, PhD, IT Consultant, and the Greenland Agency for Health and Prevention for giving access and permission to use laboratory data and data from medical files.
This study was supported by Greenland Research Council (NIS) and Steno Diabetes Center Greenland (grant number NNF20SA0064190).
Conflict of Interest and Sources of Funding: No potential conflict of interest relevant for this study is reported by the authors.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
Contributor Information
Mila Broby Johansen, Email: milabroby@gmail.com.
Karen Bjorn-Mortensen, Email: karenbjorn@gmail.com.
Michael Lynge Pedersen, Email: milp@peqqik.gl.
Jørgen Skov Jensen, Email: jsj@ssi.dk.
Anders Koch, Email: ako@ssi.dk.
REFERENCES
- 1.From E. Some aspects of venereal diseases in Greenland. Sex Transm Infect 1980; 56:65–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Misfeldt JC. Dramatic decline in the incidence of gonorrhea and syphilis in Greenland—result of an intervention strategy? Ugeskr Laeger 1994; 156:4690–4694. [In Danish]. [PubMed] [Google Scholar]
- 3.Statistics Greenland . Greenland in figures 2005 (Statistics Greenland Web Site). Available at: https://stat.gl/publ/en/GF/2005/content/Greenland%20in%20Figures%202005.pdf. Accessed November 27, 2020.
- 4.Berntsen S Karlsen APH Pedersen ML, et al. Gonorrhoea in Greenland, incidence and previous preventive measures: A review to improve future strategies. Int J Circumpolar Health 2017; 76:1350092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albertsen N, Mulvad G, Pedersen ML. Incidence of syphilis in Greenland 2010–2014: The beginning of a new epidemic? Int J Circumpolar Health 2015; 74:28378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The National Board of Health in Greenland . Appendix—Notified numbers of syphilis (The National Board of Health in Greenland Web Site). Available at: https://nun.gl/-/media/landslaegeembedet/udgivelser/nyheder/nyheder-2018/alle-maa-goere-en-indsats-for-at-bekaempe-syfilis-oktober-2018/dk_bilag_anmeldte-tilflde-af-syfilis.pdf?la=da. Accessed December 1, 2020. [In Danish].
- 7.The National Board of Health in Greenland . Note—Syphilis 2019 (The National Board of Health in Greenland Web Site). Available at: https://nun.gl/-/media/landslaegeembedet/udgivelser/sundhedsfaglig-data/notat-til-rsstatistik-om-syfilis-2019_defd3a4f-3f20-44bf-817d-a3c5c2f2e476.pdf?la=da. Accessed December 1, 2020. [In Danish].
- 8.Johansen MB Koch A Wohlfahrt J, et al. Increased incidence of gonorrhoea and chlamydia in Greenland 1990–2012. Int J Circumpolar Health 2017; 76:1324748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics Greenland . Sexually transmitted diseases by disease (chlamydia and gonorrhea), gender and time (2015–2019) (Statistics Greenland Web Site). Available at: https://bank.stat.gl/pxweb/en/Greenland/Greenland__SU__SU01__SU0120/SUXLSKS1.px/table/tableViewLayout1/. Accessed September 24, 2021.
- 10.The National Board of Health in Greenland . Infectious diseases in Greenland 2019 (The National Board of Health in Greenland Web Site). Available at: https://nun.gl/-/media/landslaegeembedet/udgivelser/sundhedsfaglig-data/smitsomme-sygdomme-i-grnland-2019_dk.pdf?la=da. Accessed September 22, 2021. [In Danish].
- 11.Statistics Greenland . Greenland in figures 2020 (Statistics Greenland Web Site). Available at: https://stat.gl/publ/en/GF/2020/pdf/Greenland%20in%20Figures%202020.pdf. Accessed November 20, 2020.
- 12.Statistics Greenland . Unemployment rate among permanent residents aged 18–65 years by time (2019) and place of residence (town, settlements etc.) (Statistics Greenland Web Site). Available at: https://bank.stat.gl/pxweb/en/Greenland/Greenland__AR__AR40/ARXLED4.px/table/tableViewLayout1/?rxid=ARXLED426-09-2021%2017%3A21%3A49. Accessed September 26, 2021.
- 13.Association of Public Health Laboratories (APHL) . Suggested reporting language for syphilis serological testing (APHL Web Site). Available at: https://www.aphl.org/programs/infectious_disease/std/Documents/ID-2020Aug-Syphilis-Reporting-Language.pdf. Accessed December 10, 2020.
- 14.Centers for Disease Control and Prevention (CDC) . Syphilis—CDC fact sheet (detailed) (CDC Web Site). Available at: https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm. Accessed November 23, 2020.
- 15.Statens Serum Institut (SSI) . Standard test syphilis (full examination) (intrathecal synthesis inclusive) (R-nr. 322) (SSI Web Site). Available at: https://www.ssi.dk/produkter-og-ydelser/diagnostik/diagnostiskhaandbog/s/322. Accessed November 23, 2020.
- 16.Danish Health Authority . Recommendations on prevention, diagnosis and treatment of sexually transmitted infections. Available at: https://www.sst.dk/-/media/Udgivelser/2015/Anbefalinger-om-forebyggelse-diagnose-og-behandling-af-seksuelt-overf%C3%B8rbare-infektioner.ashx?la=da&hash=F9A750E13E3ED96401C870174E5416EBAEA6612D. Accessed November 24, 2020. [In Danish].
- 17.Statistics Greenland . Population in districts and municipalities January 1st by age, district, gender and time (2015–2019) (Statistics Greenland Web Site). Available at: https://bank.stat.gl/pxweb/en/Greenland/Greenland__BE__BE01__BE0120/BEXST3.px/. Accessed November 6, 2020.
- 18.Statens Serum Institut (SSI) . Syphilis 2018 (SSI Web Site). Available at: https://en.ssi.dk/surveillance-and-preparedness/surveillance-in-denmark/annual-reports-on-disease-incidence/syphilis-2018. Accessed December 4, 2020.
- 19.Choudhri Y Miller J Sandhu J, et al. Infectious and congenital syphilis in Canada, 2010–2015. Can Commun Dis Rep 2018; 44:43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spicknall IH, Kreisel KM, Weinstock H. Estimates of the prevalence and incidence of syphilis in the United States, 2018. Sex Transm Dis 2021; 48:247–252. [DOI] [PubMed] [Google Scholar]
- 21.Walker FJ Llata E Doshani M, et al. HIV, chlamydia, gonorrhea, and primary and secondary syphilis among American Indians and Alaska natives within Indian health service areas in the United States, 2007–2010. J Community Health 2015; 40:484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cecere D, Jones SA. State of Alaska Epidemiology Bulletin: Syphilis outbreak update—Alaska, 2011–2013 (Alaska Department of Health and Social Services Web Site). Available at: http://epibulletins.dhss.alaska.gov/Document/Display?DocumentId=79. Accessed March 8, 2021.
- 23.Jones S, Smith T. State of Alaska Epidemiology Bulletin: Syphilis update—Alaska, 2019 and recommendations for care (Alaska Department of Health and Social Services Web Site). Available at: http://epibulletins.dhss.alaska.gov/Document/Display?DocumentId=2045. Accessed March 8, 2021.
- 24.Law DG Rink E Mulvad G, et al. Sexual health and sexually transmitted infections in the north American Arctic. Emerg Infect Dis 2008; 14:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Homøe AS, Berntsen S, Pedersen ML. Gonorrhoea in Greenland: Geographic differences in diagnostic activity and incidence of gonorrhoea in 2015. Int J Circumpolar Health 2018; 77:1445938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bjorn-Mortensen K Ladefoged K Obel N, et al. The HIV epidemic in Greenland--a slow spreading infection among adult heterosexual Greenlanders. Int J Circumpolar Health 2013; 72:19558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Government of Canada . Syphilis in Canada: Technical report on epidemiological trends, determinants and interventions (Government of Canada Web Site). Available at: https://www.canada.ca/en/services/health/publications/diseases-conditions/syphilis-epidemiological-report.html#3. Accessed September 24, 2021.
- 28.Centers for Disease Control and Prevention (CDC) . Syphilis Statistics—Figure 39: primary and secondary Syphilis—Distribution of cases by sex and sex of sex partners, United States, 2018 (CDC Web Site). Available at: https://www.cdc.gov/std/syphilis/stats.htm. Accessed March 21, 2021.
- 29.Centers for Disease Control and Prevention (CDC) . National Overview—Sexually Transmitted Disease surveillance, 2019—Syphilis (CDC Web Site). Available at: https://www.cdc.gov/std/statistics/2019/overview.htm#Syphilis. Accessed September 24, 2021.
- 30.Nieuwenburg S Rietbergen N van Zuylen D, et al. Erroneous treatment of syphilis with benzyl penicillin in an era with benzathine benzylpenicillin shortages. Sex Transm Infect 2020; 96:552–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


