Abstract
Background
The practice of neurosurgery has been profoundly affected by the coronavirus disease 2019 (COVID-19) pandemic in Kazakhstan. Many elective surgeries were postponed or canceled, which resulted in difficulties in hospitalization. In the present study, we aimed to describe the effects of COVID-19 on neurosurgical practice and to determine whether a discrepancy was present in the effects between metropolises and regional cities in Kazakhstan.
Methods
We performed an electronic internet-based survey among Kazakhstan’s neurosurgeons using the virtual snowball sampling method. The invitation link to complete the questionnaire was sent to neurosurgeons through personal and corporate electronic mail and social networks. The data were analyzed using Excel and Stata.
Results
A total of 43 neurosurgeons completed the survey. The distribution of regional and urban respondents was almost equal. The male neurosurgeons outnumbered the female neurosurgeons (93.02% vs. 6.98%). A decrease in consultations (65.34% ± 28.24%) and surgeries (56.55% ± 26.34%) had been observed by all neurosurgeons, regardless of city type. However, the proportion of neurosurgeons who had attended online educational courses during the pandemic was significantly higher (P = 0.001) for the surgeons from major cities (68.18%) compared with the surgeons from smaller cities (19.05%). The regional neurosurgeons tended to perform urgent surgeries on COVID-19–positive patients 3 times more often than had the metropolitan neurosurgeons (P < 0.001).
Conclusions
The true effect of the pandemic remains unknown for Kazakhstan. A discrepancy between the metropolitan and regional cities was found in the present study. Efforts are required and relevant guidelines must be developed to ensure that the neurosurgical treatment of various conditions continues to be available during health emergencies and that the disparities are addressed.
Key words: COVID-19, Kazakhstan, Neurosurgery, Pandemic
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; PPE, Personal protective equipment
Introduction
In December 2019, an outbreak of the novel coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2), was reported from Wuhan, China.1 Within only 2.5 months, a contagious virus had spread across the world, and the World Health Organization declared a pandemic on March 11, 2020.2 In Kazakhstan, the first case of COVID-19 was reported on March 13, 2020. An infected passenger had arrived in Kazakhstan from Western Europe by air.3 As of September 12, 2021, a total of 224,284,605 COVID-19 cases had been reported worldwide, with ∼912,300 cases in Kazakhstan.4
Kazakhstan is a Central Asian country with an estimated population of 19 million and a population density of 7 persons/1 km2.5 Kazakhstan is geographically divided into 17 administrative areas, with 3 major cities (metropolises), with a population of >1,000,000 (i.e., Nur-Sultan, Almaty, and Shymkent) and 14 regional cities.6 The population is currently served by 356 neurosurgeons, 21 neurosurgical departments within the regional hospitals, and 1 specialized neurosurgical center, which is in the capital (Nur-Sultan; formerly, Astana).7 Complex cases are transmitted from the regional hospitals to larger hospitals located in the metropolises, because the latter are equipped with the necessary technology and equipment.
Neurological disorders were the leading cause of disability and the second leading cause of death in 2016 globally. The number of deaths from neurological disease has increased by 39% in the past 30 years.8 In 2019, the rate of neurological disease in Kazakhstan was 1868.3/100,000 persons.7 Annually, ∼45,000 people will be hospitalized for treatment of neurological diseases and >20,000 neurosurgical interventions will be performed in Kazakhstan.7 The number of newly diagnosed neurological diseases has been increasing each year owing to improvements in the primary health care system and diagnostics. The ongoing COVID-19 pandemic has overwhelmed healthcare systems around the world, and the number of treated neurological diseases in Kazakhstan collapsed during the pandemic.9 The novelty of the disease and the lack of preparedness for a health emergency of this scale resulted in hospital shutdowns and disruption of patients regular access to healthcare. The practice of neurosurgery has also been affected considerably by the COVID-19 pandemic, which has been reported in many previous studies.10, 11, 12, 13
Many elective surgeries were postponed or canceled owing to the restrictions placed on public transportation and travel and the roadblocks and lockdown regimens instituted in Kazakhstan. In the present study, we aimed to describe the effects of the COVID-19 pandemic on neurosurgical practice as reported by practicing neurosurgeons and to determine whether a discrepancy was present in the effects between metropolises and regional cities in Kazakhstan.
Methods
Study Participants
The present cross-sectional study to investigate the effects of the COVID-19 pandemic on the neurosurgical practice in Kazakhstan was conducted from July 22 to July 29, 2020 during the second country-wide lockdown. The survey was based on the SmartSurvey platform (SmartSurvey Ltd., Gloucestershire, United Kingdom) and was distributed among Kazakhstan’s neurosurgeons through personal and corporate electronic mail and neurosurgery-specific groups on the WhatsApp messenger application. The target population for the present study was practicing neurosurgeons. The total number of recipients who had opened the questionnaire was 147. Recruitment was performed using convenient sampling and the virtual snowball sampling method. Because of the small population of practicing neurosurgeons in Kazakhstan (356 as of 2020),7 the absence of access to a database with contact information, and the conditions of lockdown-restricted travel, the method of online snowballing seemed the most appropriate for the present study.
Survey Design
A questionnaire (Appendix 1) was designed based on previous studies and adjusted for the Kazakhstan setting.14 , 15 The questionnaire included 18 questions. The first 5 questions concerned the respondents’ characteristics, including age, sex, the city they worked in (responses were divided into major cities or metropolises [>1,000,000 people] and regional cities), subspecialty, and number of beds at their workplace (≤25 or > 26). Thirteen questions addressed the effect of the pandemic on the respondents’ practice, such as respondent’s perception of the change in the proportion of online consultations, whether they had attended online courses during the pandemic, whether they performed urgent or planned surgery for COVID-19–positive patients, the respondent's perception regarding the availability of personal protective equipment (PPE), whether they had been tested for COVID-19 and the results of the test, the respondent’s perception of the change in the proportion of in-person consultations (patient visits to the neurosurgeon’s office in a hospital [outpatient department]) and surgeries, changes in their salary, and what type of surgery they performed most often. Finally, the respondents had an opportunity to leave comments ad lib.
Ethical Considerations
The institutional review board of the National Center for Neurosurgery approved the questionnaire and method for present study (July 20, 2020; approval no. 114). The written informed consent form included details of the study and explained the anonymity and voluntary nature and the right of the participant to withdraw from the study at any point. No incentives for participation were used. Because the study did not contain clinical studies or patient data, ethical approval was not required.
Statistical Analysis
The data from the survey were downloaded, cleaned, and coded in Excel (Microsoft Office [Microsoft Corp., Redmond, Washington, USA]) and analyzed using STATA software, version 16.0 (StataCorp, College Station, Texas, USA). The analysis of the data included descriptive statistics, such as proportions, frequencies, and mean ± standard deviation. The association between the variables was tested using the Student t test, 1-way analysis of variance, χ2 test, and the Fischer exact test, as appropriate. A P value of < 0.05 was considered statistically significant.
Results
Demographic Characteristics
Of the 147 people who had received the link to the survey, 50 had completed the questionnaire (34.0% response rate). Of the 50 questionnaires, 43 were completed fully and correctly and were included in the final data analysis. The average age of the participants was 38.36 ± 2.05 years. The most common subspecialties were spinal neurosurgery (25.58%), vascular neurosurgery (23.26%), pediatric neurosurgery (20.93%), neuro-oncology (2.33%), and neurotrauma (2.33%). Eleven participants (25.58%) had indicated ≥1 subspecialties and were assigned an unspecified label. The vast majority of neurosurgeons were men (93.02%). The capacity of the hospitals was ≤25 beds for 54.55% and >26 beds for 45.45%. The distribution of neurosurgeons from the metropolises (>1,000,000 residents) and regional cities was almost equal. No statistically significant differences were found between the respondents from the large cities and smaller cities in the demographic characteristics (Table 1 ).
Table 1.
Demographic Characteristics of the Participants
| Variable | Metropolises (n = 22; 51.16%) | Regional Cities (n = 21; 48.84%) | P Value | All (n = 43; 100%) |
|---|---|---|---|---|
| Age (years) | 38.36 ± 2.05 | 39.57 ± 1.74 | 0.66 | 38.95 ± 8.77 |
| Subspecialty | 0.08 | |||
| Unspecified | 3 (13.64) | 8 (38.10) | 11 (25.58) | |
| Pediatric neurosurgery | 3 (13.64) | 6 (28.57) | 9 (20.93) | |
| Neuro-oncology | 1 (4.55) | 0 (0) | 1 (2.33) | |
| Spinal neurosurgery | 8 (36.36) | 3 (14.29) | 11 (25.58) | |
| Neurotrauma | 0 (0) | 1 (4.76) | 1 (2.33) | |
| Vascular neurosurgery | 7 (31.82) | 3 (14.29) | 10 (23.26) | |
| Sex | 0.518 | |||
| Male | 20 (90.91) | 20 (95.24) | 40 (93.02) | |
| Female | 2 (9.09) | 1 (4.75) | 3 (6.98) | |
| No. of beds | 0.86 | |||
| ≤25 | 12 (54.55) | 12 (57.14) | 24 (55.81) | |
| >26 | 10 (45.45) | 9 (42.86) | 19 (44.19) |
Data presented as mean ± standard deviation or n (%).
The average increase in the use of telemedicine among respondents was 29.69% ± 35.45%, with no statistically significant differences between those who practiced in large cities and those who practiced in smaller cities. The proportion of neurological surgeons who attended online educational courses during the pandemic was significantly greater (P = 0.001) for the surgeons from major cities (68.18%) compared with the surgeons from smaller cities (19.05%). However, the number of urgent surgeries on COVID-19–positive patients was the inverse. The surgeons in the regional cities had performed such surgeries ∼3 times more often than had those from large cities (P < 0.001). Elective surgeries for COVID-19–positive patients were much rarer (6.98% overall) and showed no differences between the types of cities. Most of the respondents (69.77%) thought that their workplace had provided enough PPE, and most (74.42%) had been tested for COVID-19 during the pandemic. Almost 30% of the surgeons had tested positive for the virus; however, no significant differences were found between the types of cities. The respondents estimated the change in the number of consultations and surgeries they had performed before and after the pandemic. On average, they reported a 65.34% ± 28.24% decrease in consultations and 56.55% ± 26.34% decrease in surgeries. Approximately 42% of surgeons had had their salary remain the same during the lockdown. The same proportion had had their salary reduced. Finally, ∼16% were left with no salary at all. The effects of the COVID-19 pandemic on neurosurgery practice are presented in Table 2 .
Table 2.
Effect of COVID-19 Pandemic on Neurosurgery Practice
| Variable | Metropolises (n = 22; 51.16%) | Regional Cities (n = 21; 48.84%) | P Value | All (n = 43; 100%) |
|---|---|---|---|---|
| Increased telemedicine use (%) | 38.19 ± 34.79 | 21.19 ± 34.85 | 0.12 | 29.69 ± 35.45 |
| Attended online educational courses | 0.001 | |||
| No | 7 (31.82) | 17 (80.95) | 24 (55.81) | |
| Yes | 15 (68.18) | 4 (19.05) | 19 (44.19) | |
| Performed urgent surgery on COVID-19–positive patients | <0.001 | |||
| No | 17 (77.27) | 5 (23.81) | 22 (51.16) | |
| Yes | 5 (22.73) | 16 (76.19) | 21 (48.84) | |
| Performed elective surgery on COVID-19–positive patients | 1.00 | |||
| No | 20 (90.91) | 20 (9.09) | 40 (93.02) | |
| Yes | 2 (9.09) | 1 (4.76) | 3 (6.98) | |
| Enough PPE at workplace | 0.67 | |||
| No | 6 (6.7) | 7 (6.3) | 13 (30.23) | |
| Yes | 16 (15.3) | 14 (14.7) | 30 (69.77) | |
| Tested for COVID-19 | 0.49 | |||
| No | 7 (31.82) | 4 (19.05) | 11 (25.58) | |
| Yes | 15 (68.18) | 17 (80.95) | 32 (74.42) | |
| COVID-19 test result | 0.74 | |||
| NA | 7 (31.82) | 6 (28.57) | 13 (30.23) | |
| Negative | 8 (36.36) | 10 (47.62) | 18 (41.86) | |
| Positive | 7 (31.82) | 5 (23.81) | 12 (27.91) | |
| Decrease in consultations (%) | 71.02 ± 21.67 | 59.49 ± 33.32 | 0.18 | 65.34 ± 28.24 |
| Decreased consultation group | 0.09 | |||
| ≤50% | 2 (9.09) | 9 (42.86) | 11 (25.58) | |
| >50% to ≤75% | 10 (45.45) | 5 (23.81) | 15 (34.88) | |
| >75% to ≤84% | 5 (22.73) | 4 (19.09) | 9 (20.93) | |
| >84% | 5 (22.73) | 3 (14.29) | 8 (18.6) | |
| Decrease in surgery (%) | 56.02 ± 26.74 | 57.11 ± 26.57 | 0.89 | 56.55 ± 26.34 |
| Decreased surgery group | 0.66 | |||
| <50% | 5 (22.73) | 4 (19.05) | 9 (20.93) | |
| ≥50% to <54% | 5 (22.73) | 8 (38.10) | 13 (30.23) | |
| ≥54% to <75% | 6 (27.27) | 3 (14.29) | 9 (20.93) | |
| ≥75% | 6 (27.27) | 6 (28.57) | 12 (27.91) | |
| Changes in salary | 1.00 | |||
| Left without salary | 4 (18.18) | 3 (14.29) | 7 (16.28) | |
| Reduced salary | 9 (40.91) | 9 (42.86) | 18 (41.86) | |
| Salary stayed the same | 9 (40.91) | 9 (42.86) | 18 (41.86) |
COVID-19, coronavirus disease 2019.
Data presented as mean ± standard deviation or n (%).
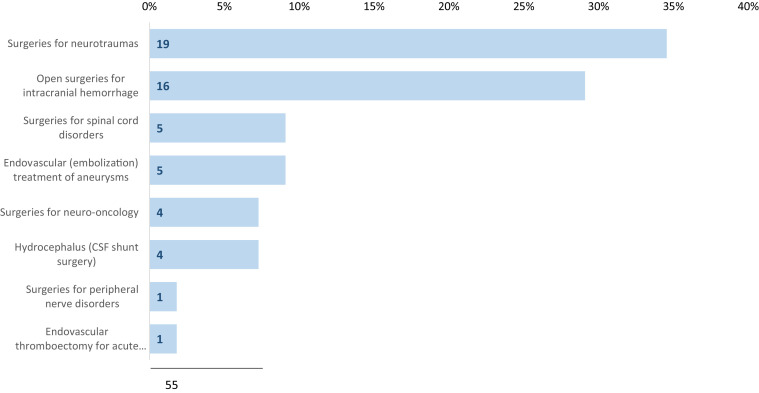
Surgery for neurotrauma and open surgery for intracranial hemorrhage were the most frequently (63.6%) performed neurosurgical interventions. In contrast, emergency interventions for peripheral nerve disorders and endovascular thrombectomies were the least frequent (3.6%). A list of the surgeries performed during the quarantine is shown in Figure 1 .
Figure 1.
Most frequent surgeries performed during the quarantine. CSF, cerebrospinal fluid.
Discussion
The COVID-19 pandemic has remarkably changed healthcare systems worldwide, and Kazakhstan is no exception. Neurosurgery has been profoundly affected by local and central governmental policies. To the best of our knowledge, the present study is the first to evaluate the immediate effects of the pandemic and the lockdowns on neurosurgical performance in Kazakhstan and to assess the discrepancies in the effects in different regions in the country.
As government-sanctioned lockdowns occurred, many hospitals were repurposed to prioritize the treatment of patients with COVID-19 or had been shut down completely to stop the spread of COVID-19 infection.9 This practice is in line with findings reported by Jean et al.,15 which demonstrated that higher income countries were more likely to experience hospital shutdowns owing to a higher number of COVID-19 cases. Kazakhstan, an upper middle-income country according to the World Bank,16 had had, on average, ∼13,000 new cases per week from July 22 to 29, 2020 and was experiencing another peak in the number of cases during the late summer of 2020.4 The results of such measures were directly reflected in the responses provided by our participants. The participants in the present estimated that their telemedicine use during the pandemic had increased by 29.69% ± 35.45%. On average, neurosurgeons across the country estimated that their consultations had decreased by more than one half. Approximately 49% of the neurosurgeons stated that the number of surgeries had decreased by ≥54%. The reduction in the number of operations was similar to the worldwide average of 50% reported by most respondents to a global neurosurgery study.15
Changes in working patterns have affected neurosurgeons’ monthly income considerably, with less than one half of respondents receiving their full salary during the quarantine. In the present study, 42% had had their salary reduced, and 16% received no salary at all. These results are in line with the findings reported by a U.S. study that had surveyed neurosurgeons from April to June 2020,17 with more than one half of respondents reporting that their salaries had been reduced. However, the same study reported that only 4% of neurosurgeons had experienced a complete loss of salary.17 The decrease in income could result in financial stress, as noted by Tsermoulas et al,18 and lead to burnout, which was the case for most of the neurosurgeons from a U.S. study.19 Future studies on the psychological impact of the COVID-19 pandemic on neurosurgeons in Kazakhstan should be conducted.
Surgeries for neurotrauma and intracranial hemorrhages were the most frequent during the quarantine in Kazakhstan, likely owing to the emergency nature of such trauma. Endovascular thrombectomy for acute ischemic stroke was the least frequent intervention in Kazakhstan, which was also reported by other studies.20 It is difficult to determine the reason for the apparent reduction of stroke cases during the pandemic, which has been described in many studies,21, 22, 23, 24, 25, 26 considering that COVID-19 infection itself is a risk factor for stroke.27
When comparing the metropolises with the regional cities, 2 factors became apparent. First, a significantly larger proportion of surgeons from the metropolises had attended some form of online educational program during the pandemic. Although the proportion of surgeons who had experienced a reduction or complete stop of their practice was relatively equal between the city types, the participants from metropolises had had significantly greater access to online education. The lack of opportunity to participate in online studies for the surgeons in the regional cities could reflect the lack of funding and equipment available and the lack of educational material in the Kazakh or Russian language.
A second finding was the inverse situation, regarding the number of urgent surgeries performed for COVID-19–positive patients. The burden of performing urgent surgery was significantly greater for those practicing in regional cities. One of the reasons might have been the lack of personnel at the regional hospitals. These findings could also reflect the practice of sending patients from regional cities to larger hospitals in the capital city or cities of republican importance to undergo complex elective surgery. Therefore, a large number of respondents from the metropolises would have been less likely to perform urgent surgeries that could not be canceled even during the pandemic. This finding might also reflect differences in the disease burden distribution across Kazakhstan. Factors such as lifestyle and healthcare choices could affect the prevalence and severity of different neurological diseases, which has been demonstrated in numerous studies.28, 29, 30 However, no such analysis was available for neurological diseases in Kazakhstan.
Although three quarters of the surgeons responded that their workplace had provided enough PPE, almost 30% of the participants had also reported that they had tested positive for COVID-19. The results were greater than those reported by healthcare workers in Qatar (10.6%) and the United States (5.3%).31 , 32 No correlation was found between PPE sufficiency and city type (metropolis or regional city). Moreover, although the respondents from the regional cities had reported a significantly greater proportion of surgeries for COVID-19–positive patients, the proportion of neurosurgeons with COVID-19–positive results was approximately the same between the metropolises and regional cities. This might imply that the surgeons testing positive for COVID-19 had not contracted it at work.
Study Limitations
One limitation of the present study was the convenience sampling method and self-reporting method of data collection. Because of the ongoing lockdown during data collection, the most efficient method of survey collection was through an online questionnaire distribution. This could have created nonresponse and selection biases, favoring those more proficient in the use of technology. Moreover, exaggeration or underreporting could have resulted from the self-reporting method of data collection. The number of respondents was small, limiting the generalizability of the results to the whole country. Moreover, we did not have information available on the surgeons who did not participate in the survey and, thus, cannot conclude that they were similar or different from the study respondents.
Strength and Future Directions
To the best of our knowledge, the present study is the first to evaluate the effects of the COVID-19 pandemic on neurosurgical practice in Kazakhstan. Our results have revealed the extent of deceleration of neurosurgery in Kazakhstan and some significant differences in the effects on the different city types. Our study showed that smaller cities require better support during health emergencies. Studies with a larger sample size are required, and the experience of neurosurgeons should be evaluated through an in-depth qualitative study. The effect of surgery cancellations could be explored with a focus on the effects on patients.
Conclusions
The COVID-19 pandemic in many ways halted neurosurgical services in Kazakhstan, just as in many other countries. The true effects of the pandemic remains unknown for Kazakhstan. A discrepancy between the metropolitan and regional cities was found in Kazakhstan. Efforts are required and relevant guidelines should be developed to ensure the neurosurgical treatment of various conditions remains available during health emergencies, and that the disparities are addressed.
CRediT authorship contribution statement
Karashash Menlibayeva: Investigation, Formal analysis, Writing – original draft. Aisha Babi: Methodology, Formal analysis, Visualization, Statistical computation, Manuscript preparation. Yerbol Makhambetov: Writing – review & editing. Serik Akshulakov: Writing – review & editing, Supervision.
Acknowledgments
We would like to show our gratitude to Professor Sandro Vento for his comments on an earlier version of our report.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Appendix 1
18-Item Questionnaire
Effect of COVID-19 on Neurosurgical Practice in Kazakhstan
-
1.
City, region (open answer)
-
2.
Age (number)
-
3.
Gender (female/male)
-
4.Subspecialty (with an option to choose several selections)
-
A.Neuro-oncology
-
B.Vascular neurosurgery
-
C.Pediatric neurosurgery
-
D.Spine neurosurgery
-
E.Functional neurosurgery
-
F.Neurotrauma
-
G.Peripheral nervous system surgery
-
H.Acute stroke surgery
-
A.
-
5.Please specify the number of each item listed in your department (number):
- Beds ___
- Neurosurgeons___
- Students (residents on neurosurgery specialty) ___
-
6.Decreases in your medical consultations since the COVID-19 (coronavirus disease 2019) pandemic?
- From 0% (no decrease) to 100% (major decrease) _______
-
7.Decreases in your neurosurgical practice since the COVID-19 pandemic?
- From 0% (no decrease) to 100% (major decrease) ______
-
8.To what extent did you increase telemedicine (online consultations, video sessions)?
- From 0% (no increase) to 100% (major increase)____
-
9.
Have you taken online training courses in your area of specialization during quarantine? Yes/No
-
10.
Have you had to cancel elective surgeries due to COVID-19? Yes/No
-
11.
Did you have to leave for part-time work during the COVID-19 epidemic? Yes/No
-
12.
Did you have to leave without pay during the COVID-19 epidemic? Yes/No
-
13.
Please list the most common surgery during COVID-19 in your practice (open answer) _________
-
14.
Have you operated on emergency cases with COVID-19? Yes/No
-
15.
Have you operated on nonemergency cases with COVID-19? Yes/No
-
16.
Do you think you have enough PPE (personal protective equipment) in your workplace? Yes/No
-
17.
Have you had any symptoms or signs of COVID-19? Yes/No
-
18.Have you been tested for COVID-19?
- If yes, please specify the results ____
- If no, please specify the reason _____
- If you have additional comments, please write them below (open answer) _______________
References
- 1.Zhu H., Wei L., Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5:6. doi: 10.1186/s41256-020-00135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Informburo. Kazakhstan. KazakhstanNews Informburo. https://informburo.kz/ Available at:
- 4.Johns Hopkins Coronavirus Resource Center COVID-19 map. https://coronavirus.jhu.edu/map.html Available at:
- 5.KazStat Department of Statistics of the Republic of Kazakhstan. https://stat.gov.kz/ Available at:
- 6.List of Departments of Statistics of Areas Cities of Nur-Sultan, Almaty and Shymkent. https://stat.gov.kz/region/list Available at:
- 7.KazStat Republican Center for Healthcare. http://rcrz.kz/index.php/en/# Available at:
- 8.Feigin V.L., Vos T. Global burden of neurological disorders: from global burden of disease estimates to actions. Neuroepidemiology. 2019;52:1–2. doi: 10.1159/000495197. [DOI] [PubMed] [Google Scholar]
- 9.Akshulakov S.K., Menlibayeva K.K., Makhambetov Y.T., et al. The COVID-19 Pandemic in Kazakhstan and its impact on neurosurgical practice. J Neurosurg Neurol of Kaz. 2020;4:11–20. [Google Scholar]
- 10.Kondziolka D., Couldwell W.T., Rutka J.T. Introduction. On pandemics: the impact of COVID-19 on the practice of neurosurgery. J Neurosurg. 2020;133:1–2. doi: 10.3171/2020.3.JNS201007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saad H., Alawieh A., Oyesiku N., Barrow D.L., Olsen J. Sheltered neurosurgery during COVID-19: the Emory experience. World Neurosurg. 2020;144:e204–e209. doi: 10.1016/j.wneu.2020.08.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bajunaid K., Alatar A., Alqurashi A., et al. The longitudinal impact of COVID-19 pandemic on neurosurgical practice. Clin Neurol Neurosurg. 2020;198:106237. doi: 10.1016/j.clineuro.2020.106237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee Z.D., Chi Yeu D.L., Ti Ang B., Ng W.H., Seow W.T. Editorial. COVID-19 and its impact on neurosurgery: our early experience in Singapore. J Neurosurg. 2020;133:24–25. doi: 10.3171/2020.4.JNS201026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soriano Sánchez J.A., Perilla Cepeda T.A., Zenteno M., et al. Early report on the impact of COVID-19 outbreak in neurosurgical practice among members of the Latin American Federation of Neurosurgical Societies. World Neurosurg. 2020;140:e195–e202. doi: 10.1016/j.wneu.2020.04.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The World Bank Kazakhstan data. https://data.worldbank.org/country/KZ Available at:
- 17.Caruso J.P., Swartz K., Mazzola C., et al. The financial impact of the COVID-19 pandemic on neurosurgery practice in spring 2020. World Neurosurg. 2021;153:e1–e10. doi: 10.1016/j.wneu.2021.04.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsermoulas G., Zisakis A., Flint G., Belli A. Challenges to neurosurgery during the coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;139:519–525. doi: 10.1016/j.wneu.2020.05.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khalafallah A.M., Lam S., Gami A., et al. Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clin Neurol Neurosurg. 2020;198:106193. doi: 10.1016/j.clineuro.2020.106193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao J., Li H., Kung D., Fisher M., Shen Y., Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Markus H.S., Brainin M. COVID-19 and stroke—a global world stroke organization perspective. Int J Stroke. 2020;15:361–364. doi: 10.1177/1747493020923472. [DOI] [PubMed] [Google Scholar]
- 22.Pop R., Quenardelle V.Q., Hasiu A., et al. Impact of the COVID-19 outbreak on acute stroke pathways—insights from the Alsace region in France. Eur J Neurol. 2020;27:1783–1787. doi: 10.1111/ene.14316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu R., Zhao J., Fisher M. The global impact of COVID-19 on acute stroke care. CNS Neurosci Ther. 2020;26:1103–1105. doi: 10.1111/cns.13442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pasarikovski C.R., da Costa L. The impact of the Covid-19 pandemic on stroke volume. Can J Neurol Sci. 2020;47:847–848. doi: 10.1017/cjn.2020.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rinkel L.A., Prick J.C.M., Slot R.E.R., et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol. 2021;268:403–408. doi: 10.1007/s00415-020-10069-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhai P., Ding Y., Li Y. The impact of COVID-19 on ischemic stroke. Diagn Pathol. 2020;15:78. doi: 10.1186/s13000-020-00994-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leira E.C., Hess D.C., Torner J.C., Adams H.P. Rural-urban differences in acute stroke management practices: a modifiable disparity. Arch Neurol. 2008;65:887–891. doi: 10.1001/archneur.65.7.887. [DOI] [PubMed] [Google Scholar]
- 29.Blumenthal S.J., Kagen J. The effects of socioeconomic status on health in rural and urban America. JAMA. 2002;287:109. [PubMed] [Google Scholar]
- 30.Elliot V.L., Morgan D., Kosteniuk J., Chow A.F., Bayly M. Health-related stigma of noncommunicable neurological disease in rural adult populations: a scoping review. Health Soc Care Community. 2019;27:e158–e188. doi: 10.1111/hsc.12694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alajmi J., Jeremijenko A.M., Abraham J.C., et al. COVID-19 infection among healthcare workers in a national healthcare system: the Qatar experience. Int J Infect Dis. 2020;100:386–389. doi: 10.1016/j.ijid.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mani N.S., Budak J.Z., Lan K.F., et al. Prevalence of coronavirus disease 2019 infection and outcomes among symptomatic healthcare workers in Seattle, Washington. Clin Infect Dis. 2020;71:2702–2707. doi: 10.1093/cid/ciaa761. [DOI] [PMC free article] [PubMed] [Google Scholar]