Abstract
Ramp lesions play a major role in both anteroposterior and rotational instability following anterior cruciate ligament rupture. The meniscotibial ligament (MTL) is the most important structure to repair and is the primary stabilizer of the posterior horn of the medial meniscus. The posteroinferior insertion of the MTL on the posterior horn of the medial has been described, forming a posterior “belt.” Isolated MTL lesion diagnosis can be challenging, as the absence of a meniscocapsular ligament lesion prevents its correct visualization through transnotch vision. This article details a technique to diagnose and repair the “belt lesion” of the medial meniscus.
Technique Video
This video presents a detailed technique to diagnose and repair the “belt lesion” of the medial meniscus
First described in the 1980s, the literature regarding ramp lesions has grown substantially over the last decade.1,2 Defined as posterior longitudinal tears at the meniscocapsular junction, their major role in both anteroposterior and rotational instability following anterior cruciate ligament (ACL) rupture has been revealed.3, 4, 5 Since preoperative diagnosis is problematic due to the low sensitivity of magnetic resonance imaging, arthroscopic evaluation using transnotch vision during ACL reconstruction remains the gold standard.6, 7, 8, 9, 10 Given their frequency, estimated to be between 9.3% and 29.6% of ACL rupture cases, additional systematic research on ramp lesions by exploring the posteromedial compartment is necessary.6, 7, 8, 9, 10, 11
The anatomy of the posterior horn of the medial meniscus (PHMM) has been studied to better understand these lesions, their injury mechanism, and the structures to be repaired. In 2019, DePhillipo et al.12 described a common insertion of the meniscotibial (MTL) and meniscocapsular (MCL) ligaments on the posterior aspect of the PHMM. This anatomy has been further developed in 2021 by Cavaignac et al., revealing a distinguished posteroinferior insertion of the MTL forming a posterior "belt" of the PHMM (Fig 1).13 Isolated MTL tears can be categorized as type III ramp lesions according to Thaunat et al.14 and may cause meniscal extrusion or rotational instability (Fig 2).15,16 However, their diagnosis is particularly challenging, as the absence of an MCL lesion prevents correct visualization of the MTL through transnotch vision. The present technique describes the arthroscopic exploration and repair of these medial meniscus "belt lesions” (Video 1, Table 1).
Fig 1.
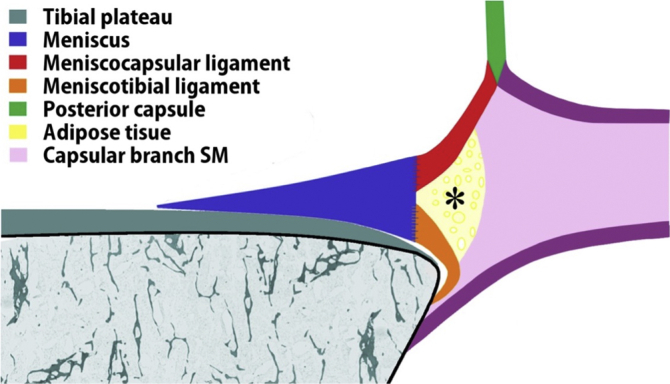
Diagram of a sagittal cut of the posteromedial corner of the knee proposed by Cavaignac et al.13 The proximal insertion of the meniscotibial ligament is on the inferior edge of the base of the medial meniscus. ∗Adipose tissue located between the meniscus in front and the tendinous capsular branch of the semimembranosus (SM).
(Reprinted with permission from The American Journal of Sports Medicine.)
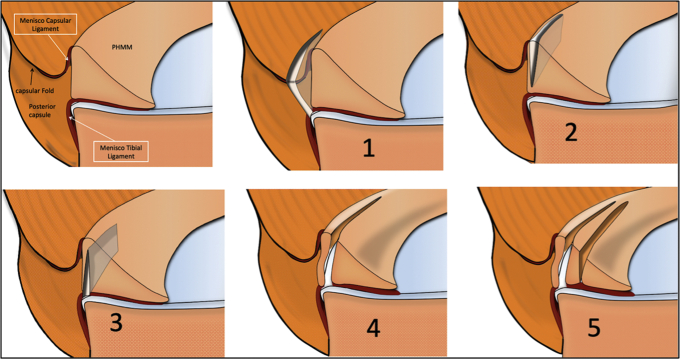
Fig 2.
Ramp lesion subtypes according to Thaunat’s classification.14 Representation of the meniscocapsular area of the posterior horn of the medial meniscus (PHMM) with the 5 subtypes of ramp lesions: 1, capsulosynovial junction complete tear; 2, red zone partial superior tear; 3, red zone partial inferior tear; 4, red zone complete tear; 5, complete double tear. Isolated MTL tears, or “belt lesions,” can be classified as type 3.
(Reprinted with permission from The American Journal of Sports Medicine.) (MTL, meniscotibial ligament.)
Table 1.
Surgical Steps and Pearls and Pitfalls of “Belt Lesion” Repair
| Surgical Step | Pearls | Pitfalls and Tips |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MCL, meniscocapsular ligament; MTL, meniscotibial ligament.
Surgical Technique (With Video Illustration)
Patient Setup
The patient is placed supine on a standard operative table. A lateral post is positioned just proximal to the knee upon the tourniquet to block external hip rotation. A foot roll is positioned so that the knee could be installed at 90° of flexion. The knee is free and can be mobilized in all amplitudes.
Injury Assessment
A high anterolateral portal is performed to spare the infrapatellar fat pad.17 An anteromedial portal is performed as standard. PHMM instability is first assessed by meticulous probing through anterior visualization. A transnotch approach is then performed for posteromedial retro-condylar exploration. Internal rotation of the tibia is performed to tension the posteromedial capsule and investigate for MCL tears. In the event of discordance between unexplained anterior meniscal hypermobility despite the integrity of the MCL, an isolated MTL injury was suspected (Fig 3). Through anterior vision, the PHMM is lifted with a probe. The MTL is revealed, and a rupture can be diagnosed as an interruption of the posterior "belt" (Fig 4).
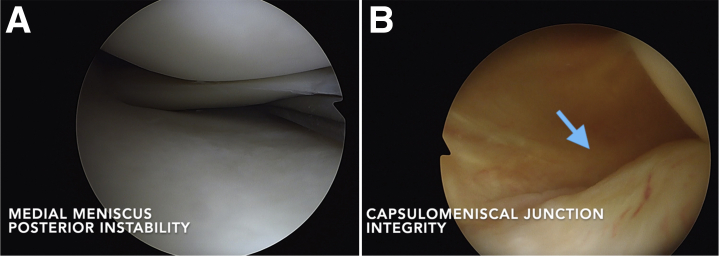
Fig 3.
Anterior probing and transnotch vision. (A) Anterior arthroscopic view of the medial meniscus: PHMM posterior instability is assessed by anterior probing. (B) Transnotch view of the posterior horn of the medial meniscus: The capsulomeniscal junction is found intact through transnotch vision (blue arrow).
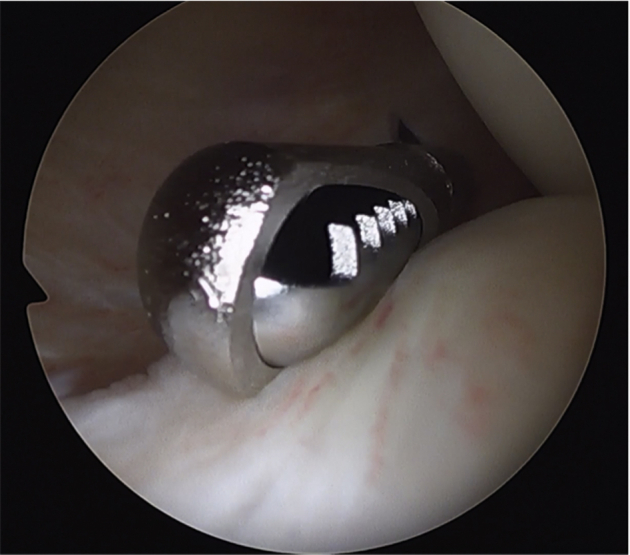
Fig 4.
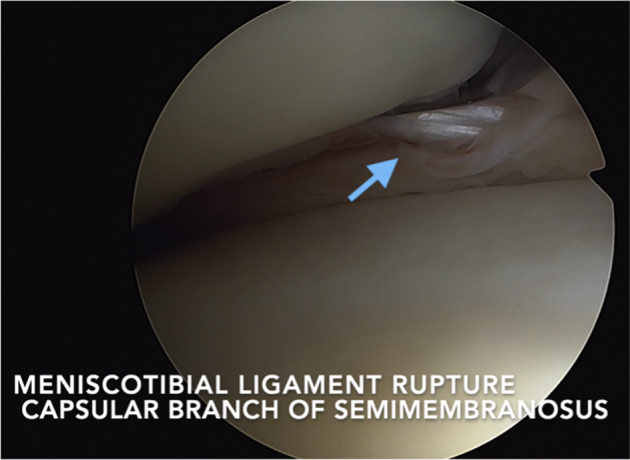
Anterior arthroscopic view of the medial meniscus: MTL integrity checking. A complete rupture of the MTL is diagnosed, and the capsular branch of the semimembranosus is visible through it (blue arrow). (MTL, meniscotibial ligament.)
“Belt Lesion” Repair
A posteromedial portal is performed under transnotch vision. With the tibia positioned in internal rotation, the MCL was debrided using a needle or a shaver (Fig 5). The "belt lesion" is then visible, and the tibial plateau passes through it.
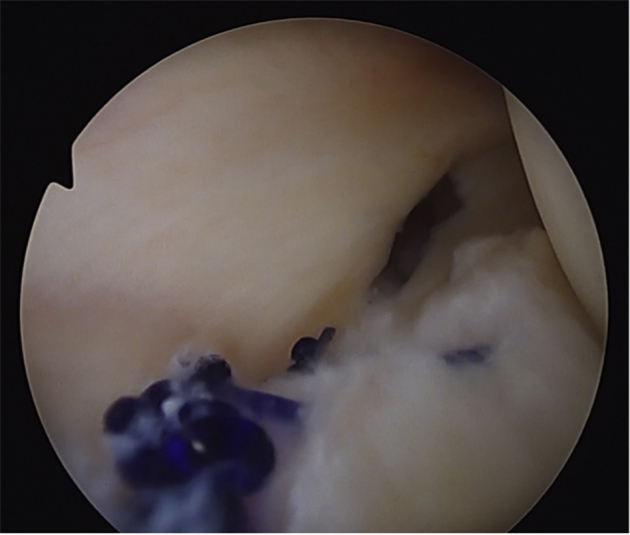
Fig 5.
Transnotch view of the posterior horn of the medial meniscus: MCL debridement.
The MCL was debrided with a shaver by a posteromedial portal to reveal the MTL lesion. (MCL, meniscocapsular ligament; MTL, meniscotibial ligament.)
A Suture Hook (Arthrex, Naples, FL) is introduced by the posteromedial portal and loaded with a no. 0 absorbable monofilament suture (polydioxanone). A left curved hook device is used for the right knee and vice versa. It is first passed through both the MCL and MTL and then through the posterior meniscal wall. The polydioxanone suture is extracted and collected by the posteromedial portal using a grasper. A self-locking sliding knot is tied using a knot-pusher, secured by two inverted half-keys. Separate points are performed in the same way to repair the entire lesion, going from the most medial to the most lateral one (Fig 6). Once the repair is completed, anterior probing is performed through anterior vision. The correction of posterior instability is checked. The meniscus can be lifted again to evaluate the proper reinsertion of the MTL on the lower portion of the PHMM (Fig 7).
Fig 6.
Transnotch view of the posterior horn of the medial meniscus. MTL lesion repair with separate points. Separate points performed through the posteromedial approach allow for precise MTL lesion repair under arthroscopic control. (MTL, meniscotibial ligament.)
Fig 7.
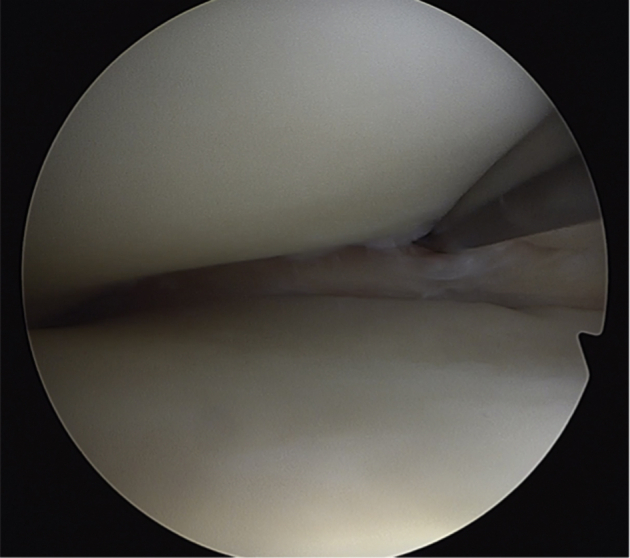
Anterior arthroscopic view of the medial meniscus. MTL repair evaluation. Complete closure of the MTL lesion was evaluated with anterior probing. The stability of the PHMM is checked. (MTL, meniscotibial ligament; PHMM, posterior horn of the medial meniscus.).
Rehabilitation
Weight-bearing is partial in the immediate postoperative period and protected by crutches until the fourth week. Knee flexion is limited to 90° for 6 weeks. Early rehabilitation is focused on the restoration of full extension. Cycling is allowed at 6 weeks, nonpivoting sports at 4 months, pivoting noncontact sports at 6 months and pivoting contact sports at 8 to 9 months.
Discussion
The presented technique involves the arthroscopic exploration and repair of an isolated MTL rupture. Several hypotheses have been described regarding the injury mechanism of ramp lesions. Hughston18 supposed that excessive anterior tibial translation in the context of ACL tears could cause reflex contraction of the semimembranosus, leading through the capsular branch to a traction lesion of the MCL and/or MTL. He also suggested that in this setting, the meniscus could be trapped between the femur and tibia, resulting in PHMM injury. These hypotheses are consistent with recent anatomical and histologic descriptions. In 2021, Cavaignac et al.13 described 2 distinct ligament insertions on the PHMM, one posterosuperior for the MCL and one posteroinferior for the MTL. A capsular branch of the semimembranosus also has been described, directly attached to the MCL, the MTL and the posteromedial joint capsule. This is in line with our observation of an isolated lesion of the MTL and the capsular branch of the semimembranosus visualized through it (Video 1).
Ramp lesions can lead to posteromedial instability.2 Biomechanical studies have reported a significant increase in both anteroposterior3, 4, 5 and rotational laxity3,4,16 when a ramp lesion is associated with an ACL tear. The MTL appears to be the primary stabilizer of PHMM, as similar results have been found in the case of an isolated rupture.3,15,16 Thus, it acts as a true posterior “belt” for the medial meniscus. The diagnosis of this lesion is a challenge in itself, and its biomechanical importance has prompted us to pay particular attention to its investigation and management. To our knowledge, this Technical Note is the first to focus on the diagnosis and repair of an isolated MTL lesion.
Different techniques have been described to repair PHMM, particularly ramp lesions.19 Despite technical improvements, the failure rate remains high.20 With the classic anteromedial portal, debridement of the lesion may be limited, and the all-inside anchor sutures cannot provide a complete closure of the lesion. Since 2013, we have observed a decrease in the secondary meniscectomy rate for any type of medial meniscus repair from 25%20 to 7%,11 with a 5-year mean follow-up. These results follow the routine performance of a transnotch vision combined with anterior probing associated with posteromedial hook repair in the case of ramp lesions. Regarding isolated MTL lesions, we chose to use a posterior meniscocapsular opening to debride the MTL lesion, allowing us to monitor its complete closure through hook sutures via the posteromedial portal.
The main disadvantage of this technique is the need for an additional posteromedial portal with risks of vasculo-nervous injury. However, this approach is safe as long as a few prerequisites are respected. Another disadvantage of this technique is the learning curve for the execution of this approach and for meniscal hook repair. The advantages and disadvantages are summarized in Table 2.
Table 2.
Advantages and Disadvantages of the Present Technique
| Advantages | Disadvantages |
|---|---|
|
|
|
|
|
|
|
|
|
MTL, meniscotibial ligament; PHMM, posterior horn of the medial meniscus; PM, posteromedial.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.G., A.F., and E.C. report grants from Arthrex. B.S.-C. is a paid consultant, receives royalties and research support, and has made presentations for Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video presents a detailed technique to diagnose and repair the “belt lesion” of the medial meniscus
References
- 1.Hamberg P., Gillquist J., Lysholm J. Suture of new and old peripheral meniscus tears. J Bone Joint Surg Am. 1983;65:193–197. doi: 10.2106/00004623-198365020-00007. [DOI] [PubMed] [Google Scholar]
- 2.Sonnery-Cottet B., Serra Cruz R., Vieira T.D., Goes R.A., Saithna A. Ramp lesions: An unrecognized posteromedial instability? Clin Sports Med. 2020;39:69–81. doi: 10.1016/j.csm.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 3.DePhillipo N.N., Moatshe G., Brady A., et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: A biomechanical study. Am J Sports Med. 2018;46:2422–2431. doi: 10.1177/0363546518774315. [DOI] [PubMed] [Google Scholar]
- 4.Stephen J.M., Halewood C., Kittl C., Bollen S.R., Williams A., Amis A.A. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400–408. doi: 10.1177/0363546515617454. [DOI] [PubMed] [Google Scholar]
- 5.Ahn J.H., Bae T.S., Kang K.-S., Kang S.Y., Lee S.H. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39:2187–2193. doi: 10.1177/0363546511416597. [DOI] [PubMed] [Google Scholar]
- 6.Bollen S.R. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: A previously unrecognised association. J Bone Joint Surg Br. 2010;92:222–223. doi: 10.1302/0301-620X.92B2.22974. [DOI] [PubMed] [Google Scholar]
- 7.DePhillipo N.N., Cinque M.E., Chahla J., Geeslin A.G., Engebretsen L., LaPrade R.F. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2233–2237. doi: 10.1177/0363546517704426. [DOI] [PubMed] [Google Scholar]
- 8.Hatayama K., Terauchi M., Saito K., Aoki J., Nonaka S., Higuchi H. Magnetic resonance imaging diagnosis of medial meniscal ramp lesions in patients with anterior cruciate ligament injuries. Arthroscopy. 2018;34:1631–1637. doi: 10.1016/j.arthro.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Liu X., Feng H., Zhang H., Hong L., Wang X.S., Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–837. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 10.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Praz C., Rosenstiel N., et al. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI Study Group Database: A risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46:3189–3197. doi: 10.1177/0363546518800717. [DOI] [PubMed] [Google Scholar]
- 12.DePhillipo N.N., Moatshe G., Chahla J., et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am J Sports Med. 2019;47:372–378. doi: 10.1177/0363546518814258. [DOI] [PubMed] [Google Scholar]
- 13.Cavaignac E., Sylvie R., Teulières M., et al. What is the relationship between the distal semimembranosus tendon and the medial meniscus? A gross and microscopic analysis from the SANTI Study Group. Am J Sports Med. 2021;49:459–466. doi: 10.1177/0363546520980076. [DOI] [PubMed] [Google Scholar]
- 14.Thaunat M, Ingale P, Penet A, et al. Ramp lesion subtypes: Prevalence, imaging, and arthroscopic findings in 2156 anterior cruciate ligament reconstructions [Published online April 21, 2021]. Am J Sports Med. https://doi.org/10.1177/03635465211006103 [DOI] [PubMed]
- 15.Paletta G.A., Crane D.M., Konicek J., et al. Surgical treatment of meniscal extrusion: A biomechanical study on the role of the medial meniscotibial ligaments with early clinical validation. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120936672. 2325967120936672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peltier A., Lording T., Maubisson L., Ballis R., Neyret P., Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:2967–2973. doi: 10.1007/s00167-015-3751-0. [DOI] [PubMed] [Google Scholar]
- 17.Sonnery-Cottet B., Archbold P., Zayni R., et al. High lateral portal for sparing the infrapatellar fat-pad during ACL reconstruction. Orthop Traumatol Surg Res. 2011;97:870–873. doi: 10.1016/j.otsr.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Hughston J.C. Mosby; Saint Louis, MO: 1993. Knee ligaments: Injury and repair. [Google Scholar]
- 19.Acosta J., Ravaei S., Brown S.M., Mulcahey M.K. Examining techniques for treatment of medial meniscal ramp lesions during anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2020;36:2921–2933. doi: 10.1016/j.arthro.2020.05.041. [DOI] [PubMed] [Google Scholar]
- 20.Rochcongar G., Cucurulo T., Ameline T., et al. Meniscal survival rate after anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res. 2015;101(suppl 8):323–326. doi: 10.1016/j.otsr.2015.09.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video presents a detailed technique to diagnose and repair the “belt lesion” of the medial meniscus
This video presents a detailed technique to diagnose and repair the “belt lesion” of the medial meniscus