Abstract
Objectives:
To identify predictors of infant sleep arrangement and examine the directionality of the relationships between maternal depressive symptoms, infant sleep problems, and bedsharing.
Design:
Secondary analysis of longitudinal data from the Mothers and Others: Family-Based Obesity Prevention for Infants and Toddlers randomized trial.
Setting:
Central North Carolina, USA.
Participants:
Four-hundred and twenty-eight predominantly low-income, non-Hispanic Black mother-infant pairs.
Measurements:
Data were collected at 28 weeks pregnancy and 1, 3, 6, 9, 12, and 15 months postpartum. Maternal depressive symptoms were measured using the Center for Epidemiological Studies Depression Scale and infant sleep variables were measured using the Brief Infant Sleep Questionnaire.
Results:
The prevalence of reported bedsharing increased from 16.7% at 1 month to 35.6% at 15 months postpartum. Bedsharing was associated with shortened breastfeeding duration and maternal perception of an infant sleep problem. Concurrently, maternal perception of an infant sleep problem, but not presence of maternal depressive symptoms, was associated with an increased likelihood of bedsharing. Longitudinally, neither maternal perception of an infant sleep problem nor presence of maternal depressive symptoms predicted bedsharing. Bedsharing predicted an increased likelihood of maternal perception of an infant sleep problem and presence of maternal depressive symptoms.
Conclusion:
Prevalence of bedsharing increased over time and was predictive of maternal depressive symptoms. Providers should discuss the conflicting infant sleep recommendations with their patients and provide safe-sleep guidelines for mothers who intend to bedshare.
Keywords: bedsharing, maternal depression, perceived infant sleep problems
INTRODUCTION1
The prevalence of bedsharing in the United States has increased over the past thirty years.1 In 1993, only 6.5% of caregivers reported usually bedsharing with their infant, whereas in 2015 the prevalence increased to 24.4%.1,2 According to results from the Pregnancy Risk Assessment Monitoring System (PRAMS), 35.3% of non-Hispanic Black (NHB) mothers and 37.0% of non-Hispanic Asian or Pacific Islander mothers reported their baby “often” or “always” bedshared, while the prevalence among non-Hispanic White mothers was 17.5%.2 Evidence suggests bedsharing is positively associated with maternal depression.3 NHB mothers have an increased likelihood of postpartum depression,4 indicating a potential relationship between maternal depressive symptoms (MDS) and bedsharing among NHB mothers.
Despite the increasing prevalence of bedsharing in the United States, infant sleep location remains a heavily debated topic.5 The American Academy of Pediatrics (AAP) discourages bedsharing, and encourages room-sharing, due to studies that have identified associations between bedsharing and risk of Sudden Infant Death Syndrome (SIDS).6 Even the room-sharing recommendation has received scrutiny due to associations between room-sharing, decreased infant sleep duration, and unsafe sleep practices.7,8 Others argue bedsharing should be recommended because the association with SIDS is insignificant in the absence of additional risk factors, like caregiver smoking or excessive alcohol consumption.9 The Academy of Breastfeeding Medicine (ABM) published guidelines that encourage bedsharing to promote breastfeeding duration and exclusivity, particularly in light of the protective effect of breastfeeding against SIDS.10
Research on the effects of bedsharing for mothers is limited and mixed. Among NHB mothers, the decision to bedshare is most heavily influenced by the home environment (e.g. safety and size of household), breastfeeding status, and desire to bond with their infant.11,12 Among breastfeeding mothers, bedsharing has been associated with longer breastfeeding duration, shorter nighttime disruptions, and longer maternal sleep duration.10 Other studies reported bedsharing mothers are more likely to report their infant’s sleep as problematic due to poor maternal sleep quality and shorter periods of continuous sleep, both of which have been associated with MDS.8,13-16 Bedsharing has also been associated with positive infant outcomes. Bedsharing infants, in comparison to non-bedsharing infants, experience increased nighttime mother-infant interactions, greater self-regulation, and have a more positive affect.17
Previous study designs have made it difficult to determine if the relationships between bedsharing and maternal-infant sleep outcomes vary by mothers who initially decide to bedshare versus mothers who bedshare in response to a problem.11 For example, mothers may identify their infant’s sleep as a problem and then decide to bedshare15 to soothe their infant more efficiently.12,18,19 Or, mothers could begin by bedsharing, increasing their likelihood of being awoken during the night due to proximity to their infant.13 Similarly, it is unclear whether MDS influence the decision to bed share,16 or if the decision to bedshare diminishes maternal sleep quality, subsequently increasing MDS.20 These potential relationships align with the transactional model of infant sleep development which emphasizes the bidirectionality between parenting and infant sleep, whereby parental emotions and behaviors are influenced by infant sleep patterns and vice versa.21
It is important to understand the impact of bedsharing on maternal health and behaviors during the postpartum period, especially among NHB mothers due to their high prevalence of bedsharing. In this paper, we examine longitudinal associations between MDS, maternal report of an infant sleep problem (ISP), and bedsharing in a sample of predominantly low-income, NHB mothers participating in the Mothers and Others: Family-Based Obesity Prevention for Infants and Toddlers randomized trial.22 We fill a gap within current literature by examining sociodemographic characteristics associated with bedsharing among NHB mother-infant pairs. In recognition of the transactional model of infant sleep development,21 we aim to assess the directionality between MDS, maternal report of an ISP, and bedsharing to determine if bedsharing is contributing to the presence of MDS and/or perception of an ISP or if the presence of MDS and/or perception of an ISP are contributing to the decision to bedshare. We hypothesized bedsharing would be concurrently associated with the presence of MDS and maternal perception of an ISP. Longitudinally, we hypothesized bedsharing would predict the presence of MDS and maternal perception of an ISP.
METHODS
Design
Data for this secondary analysis come from 428 NHB mother-infant pairs participating in the Mothers & Others intervention, a two-group randomized controlled trial that tested differences in infant size and growth during the first 15 months of life between an obesity prevention (intervention) group and an injury prevention (control) group. The intervention was comprised of home visits from peer educators and materials to promote responsive feeding and care. The control group also received home visits from peer educators, with information and corresponding materials focused on injury prevention.23
Both groups received sleep information during a home visit at 30-weeks’ gestation. During the control group’s home visit, participants were provided with recommendations to prevent SIDS: “Your baby should not sleep in an adult bed, on a couch, or on a chair alone, with you, or with anyone else.” Conversely, the sleep information provided to the intervention group focused on infant sleep behavior expectations: “Your newborn baby will fall asleep dreaming, she will stay in a light (active) state for a longer period before moving into deep sleep. This process is vital but means she will wake up more easily if a phone rings, the T. V. makes a loud noise, or you try to change her position, like laying her down in a bassinet.” Breastfeeding was recommended to both the control and intervention group due to the inverse association between breastfeeding and SIDS. The intervention group also received additional information on the benefits of breastfeeding including its ability to prevent chronic disease and infection.
A detailed description of the Mothers & Others study has been previously published.22 The Institutional Review Board of Our University approved the study protocol and analysis. The study is registered with the National Clinical Trial Registry (NCT01938118 at clinicaltrials.gov).
Participants
Eligible participants were 18-39 years old with a singleton pregnancy, NHB, English speaking, and able to identify a study partner that would also receive the intervention (e.g., infant’s father, infant’s grandmother, infant’s other relative, or non-relative). Exclusion criteria after birth included premature birth (<36 weeks; n=21), an extended mother or infant hospital stay post-birth (>7 days; n=28), low birthweight (<2500 grams; n=15), multiple birth (n=3), or diagnosis of a congenital anomaly or condition that would significantly affect infant feeding or growth (e.g., Down syndrome, cleft lip or palate; n=2). Additionally, 61 mothers were lost to follow-up, declined to participate, or moved away.23 After birth, 299 mothers remained eligible and were followed through the duration of the study. Comparisons of characteristics between mothers who remained eligible to participate in Mothers & Others after birth versus mothers who became ineligible revealed few differences (Supplementary Table 1). For this current analysis, the analytic sample includes data from 295 mothers (140 in the intervention group and 155 in the control group) with complete data on MDS at baseline (28 weeks’ gestation), as well as MDS and infant sleep at 1, 3, 6, 9, 12, and/or 15-month visits.
Measurement
Dependent and Independent Variables
Bedsharing.
Items from the Brief Infant Sleep Questionnaire (BISQ) assessed infant sleep behaviors at 1, 3, 6, 9, 12, and 15 months postpartum.24 The survey assessed where the infant typically slept by asking mothers to describe their baby’s current sleeping arrangement (“infant crib in a separate room”, “infant crib in parents’ room”, “in parents’ bed”, “infant crib in room with sibling”, or “other”). Infant sleep arrangement was categorized into 3 groups: bedsharing (infant slept in same bed as mother), room-sharing (infant slept in crib or co-sleeper in mother’s room), or separate room (infant and mother slept in different rooms). Room-sharing was the referent group due to the AAP recommendation that suggests infants and caregivers room-share without bedsharing.25
Maternal perception of an ISP.
Using the BISQ, mothers reported their perception of their infant’s sleep at each visit (“a small problem”, “a very serious problem”, or “not a problem at all”). Because of the low number of mothers reporting their infants’ sleep as “a very serious problem” (n=15), maternal perception of infant sleep was coded dichotomously as “yes” when mothers reported that their infant’s sleep was a “small problem” or a “very serious problem” and “no” if mothers stated their infant’s sleep was “not a problem at all.”
MDS.
The presence of MDS was assessed at each visit using the 20-item Center for Epidemiological Studies Depression Scale (CESD-Scale).26,27 Response options for each item ranged from 0 (“Rarely or None of the Time”) to 3 (“Most of Almost all the Time”). Total scores were continuous and ranged from 0 to 58, with higher scores indicating greater depressive symptomology, and a score at or above 16 indicating presence of MDS. These measures showed adequate internal consistency at each visit (Cronbach’s α > 0.85).
Potential Confounding Variables
Infant temperament.
Maternal perception of two dimensions of infant temperament, activity level (AL) and distress to limitations (DTL), was measured postnatally at 3, 6, 9, and 12 months using the Infant Behavior Questionnaire-Revised (IBQ-R).28 The 16-item AL sub-scale assesses maternal perception of infant gross motor activity such as movement of arms and legs, and squirming. The 16-item DTL sub-scale assesses maternal perception of infant fussiness, crying, and distress. Scores for both the DTL and AL sub-scales were continuous and calculated by taking the mean of the sub-scale items. Scores ranged from 1 to 7 with higher scores indicating the perception that an infant is more active or easily distressed. These measures showed adequate internal consistency at each visit (Cronbach’s α > 0.70).
Breastfeeding.
Breastfeeding status was collected at each visit using items from the Infant Feeding Practices Study II questionnaire.29,30 During each visit, mothers completed a questionnaire assessing their current breastfeeding status (still breastfeeding “yes” or “no”), breastfeeding exclusivity (infant only receives human milk “yes” or “no”), and the age of their infant when breastfeeding was discontinued. To calculate the duration of any breastfeeding, mothers’ responses to the question “How old was [infant] when you stopped breastfeeding?” were converted to months. Responses were continuous, ranging from 0-12 months.
Additional covariates.
Enrollment in Medicaid, maternal education level (some high school or less, high school graduate/GED, some college, or college graduate), maternal age, marital status, household composition, and the number of nighttime infant awakenings were potential confounders. Confounding was determined by evaluating the relationships between the outcome and potential confounders and by using a 10% change-in-estimate criterion for inclusion.31
Data collection
Participants were followed with an online survey at 1-month postpartum and a combination of online surveys and home visits at 3, 6, 9, 12, and 15 months postpartum. Data were collected from 2013 to 2018. Written, informed consent was obtained from study participants prior to the baseline assessment.
Data analysis
Descriptive statistics were used to examine variable distributions at each timepoint. To test for effects of attrition, comparisons in key study characteristics between the baseline sample and the samples at each subsequent study visit were assessed using linear regression for continuous variables and logistic regression for categorical variables. Mixed-effects multinomial and logistic regression models were used to assess longitudinal and directional associations between maternal report of an ISP, MDS, and bedsharing, controlling for repeated measures by subject.
To test for associations between concurrent MDS or perception of an ISP and bedsharing, three mixed-effects multinomial models were analyzed. In these models, the likelihood of bedsharing was determined using a 3-level dependent variable (bed sharing, room-sharing [referent group], or separate rooms). In the first model, presence of MDS was the independent variable (Table 3). In the second model, maternal perception of an ISP was the independent variable. The third, adjusted model, contained presence of MDS, maternal perception of an ISP, and study intervention group, as the additional SIDS information provided to the control group and the sleep behavior information provided to the intervention group may have influenced parental decisions regarding sleep location or perception of an ISP. All models were adjusted for visit to control for changes in bedsharing across time. Interaction terms between a) MDS and visit; b) perception of an ISP and visit; and c) MDS and perception of an ISP were not significant and were not included in final models.
Table 3.
Relationship between bedsharing, presence of maternal depressive symptoms, and maternal perception of an infant sleep problema
| Bedsharing |
||
|---|---|---|
| Unadjusted Relative Risk Ratio (95% CI)a |
Adjusted Relative Risk Ratio (95% CI)a |
|
| CONCURRENT MODELS | ||
| Model 1 | ||
| Depressive symptomsb, yes | 1.62 (1.04-2.52) * | |
| Model 2 | ||
| Perception of an infant sleep problem, yes | 1.90 (1.21-2.99) * | |
| Model 3 c | ||
| Depressive symptomsb, yes | -- | 1.52 (0.99-2.33) |
| Perception of an infant sleep problem, yes | -- | 1.79 (1.12-2.86) * |
| LAGGED MODELS (Time t→ Time t+1) d | ||
| Model 4 | ||
| Depressive symptomsb, yes | 1.66 (1.07-2.58) * | |
| Model 5 | ||
| Perception of an infant sleep problem, yes | 1.82 (1.11-2.99) * | |
| Model 6 e | ||
| Depressive symptomsb, yes | -- | 1.31 (0.68-2.51) |
| Perception of an infant sleep problem, yes | -- | 1.92 (0.96-3.84) |
Note. 95% CI: 95% Confidence Interval
Mixed-effects multinomial models tested longitudinal associations. Robust clusters were used to control for repeated measures across subjects. All models were adjusted for visit.
Presence of depressive symptoms indicated by score ≥ 16 on the Center for Epidemiological Studies-Depression Scale, measured at each visit.
Model adjusted for visit and study intervention group. Chi-square goodness of fit for multinomial models=p>0.05.
t is the timepoint (i.e., home visit) preceding time t+1; t+1 is the timepoint succeeding time t.
Model adjusted for visit, breastfeeding outcomes (exclusivity and duration), infant distress to limitations, infant activity level, and study intervention group. Chi-square goodness of fit for multinomial models= p>0.05.
p<0.05
To test for directionality, we generated lagged variables for perception of an ISP, presence of MDS, and bedsharing. While the concurrent independent variables shared the same recall period as the dependent variable, the lagged measures refer to independent variables collected during the home visit that preceded measurement of the dependent variable. For example, at the 6-month home visit, concurrent presence of MDS referred to presence of MDS at the 6-month home visit whereas lagged presence of MDS referred to presence of MDS at the previous, 3-month home visit.
In the first lagged model, lagged MDS or presence of MDS at time t was the independent variable, where t is the timepoint preceding time t+1 (Table 3). In the second lagged model, lagged maternal perception of an ISP was the independent variable. The adjusted lagged model, contained lagged presence of MDS, lagged maternal perception of an ISP, study intervention group, and additional confounding variables (e.g., activity level, distress to limitations, breastfeeding duration, and breastfeeding exclusivity). All models were adjusted for visit to control for changes in bedsharing across time. Logistic models were used to determine the association between bedsharing at time t and odds of MDS (Figure 1) and maternal perception of an ISP (Figure 2 ) at time t+1. The multinomial goodness of fit test was used to evaluate each multinomial logistic regression model32 and all analyses were conducted using Stata 15 (StataCorp, College Station, TX). Statistical significance was set at P<0.05.
Figure 1.
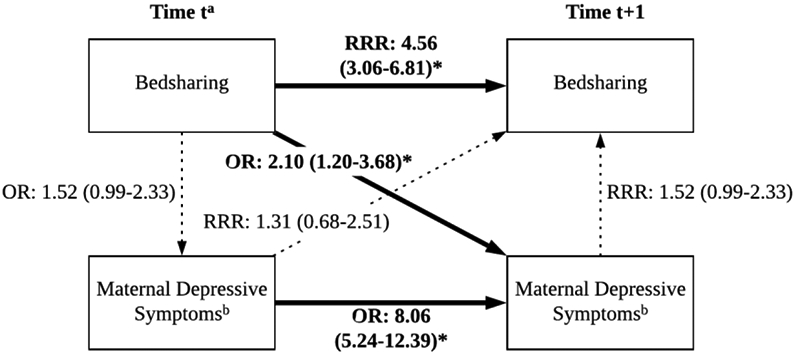
Directionality of the associations between bedsharing and presence of maternal depressive symptoms. Parentheses indicate 95% confidence intervals; non-significant paths indicated by the dotted lines.a,b
Note. OR: Odds Ratio; RRR: Relative Risk Ratio. Adjusted logistic and multinomial mixed-effects models tested bidirectional longitudinal associations. Robust clusters were used to control for repeated measures across subjects. Models adjusted for maternal perception of an infant sleep problem, breastfeeding exclusivity and duration, infant activity level, infant distress to limitations, study intervention group, and visit.
at is the timepoint preceding time t+1
bDefined as a score ≥16 on the Center for Epidemiological Studies-Depression Scale, measured at each visit.
*p<0.05; dotted line: p≥0.05
Figure 2.
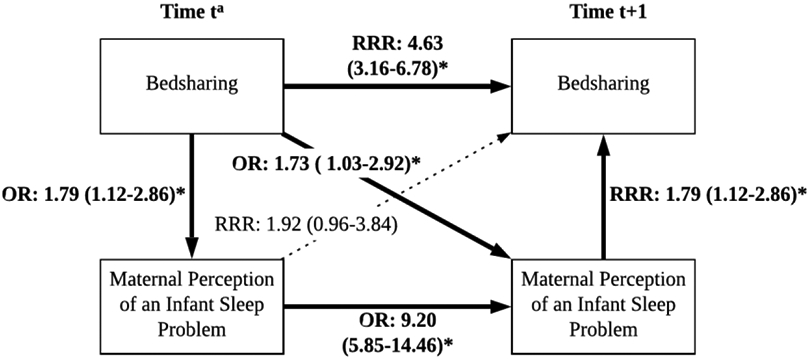
Directionality of the associations between bedsharing and maternal perception of an infant sleep problem. Parentheses indicate 95% confidence intervals; non-significant path indicated by the dotted line.a
Note. OR: Odds Ratio; RRR: Relative Risk. Adjusted logistic and multinomial mixed-effects models tested bidirectional longitudinal associations. Robust clusters were used to control for repeated measures across subjects. Models adjusted for presence of maternal depressive symptoms, number of nighttime infant awakenings, breastfeeding duration, infant activity level, infant distress to limitations, study intervention group, and visit.
at is the timepoint preceding time t+1
*p<0.05; dotted line: p≥0.05
RESULTS
Sample characteristics
Among this sample of NHB mothers, most were enrolled in Medicaid, employed, and not married or in a domestic partnership (Table 1). One third of mothers exhibited depressive symptoms (CESD ≥16 points) at baseline. Between month 1 and month 15, prevalence of maternal depressive symptomology ranged from 15% to 21%. The proportion of infants bedsharing increased over time. At the 1-month assessment, 17% of mothers reported they were currently bedsharing, compared to 36% of mothers at the 15-month assessment. Despite the different sleep information provided to the control versus the intervention group, there were no significant differences in key study characteristics by treatment group at any timepoint (Supplementary Table 2). Comparisons of sociodemographic characteristics revealed few differences between the baseline sample and the sample at each study visit. There were more mothers at month 1 whose highest level of education was graduating high school or attaining a GED. At months 3, 6, and 15 there were more mothers who had graduated college.
Table 1.
Baseline and longitudinal maternal, infant, & household characteristics from Mothers & Others study participants
| Baseline- 28 weeks’ gestation (N=295) |
Month 1 (N=241) |
Month 3 (N=252) |
Month 6 (N=230) |
Month 9 (N=224) |
Month 12 (N=201) |
Month 15 (N=206) |
|
|---|---|---|---|---|---|---|---|
| Maternal and household characteristics | |||||||
| Age (years), mean (SD) | 25.7 (5.2) | 25.8 (5.2) | 25.8 (5.3) | 25.9 (5.2) | 25.9 (5.2) | 25.7 (5.2) | 25.9 (5.2) |
| Education, n (%) | |||||||
| Some high school or less | 40 (13.5) | 36 (14.9) | 35 (13.9) | 30 (13.0) | 14.5 (14.5) | 28 (13.8) | 28 (13.5) |
| High school graduate/GED | 105 (35.6) | 75 (40.0)a | 85 (33.7) | 78 (33.8) | 35.5 (35.5) | 73 (36.0) | 70 (33.8) |
| Some college | 103 (34.9) | 89 (36.8) | 88 (34.9) | 79 (34.2) | 33.3 (33.3) | 66 (32.5) | 70 (33.8) |
| College graduate | 47 (15.9) | 42 (17.4) | 44 (17.5)a | 44 (19.1)a | 16.7 (16.7) | 36 (17.7) | 39 (18.8)a |
| Married/domestic partnership, yes, n (%) | 90 (30.5) | 77 (31.8) | 81 (32.1) | 69 (29.9) | 72 (31.6) | 62 (30.5) | 64 (30.9) |
| Medicaid, yes, n (%) | 210 (71.9) | 172 (71.4) | 178 (71.5) | 162 (70.7) | 161 (71.2) | 138 (68.7) | 141 (68.8) |
| Number of people living in household, mean (SD) | 3.7 (1.7) | 3.8 (1.7) | 3.7 (1.7) | 3.7 (1.7) | 3.7 (1.7) | 3.7 (1.7) | 3.7 (1.6) |
| Infant’s father living in same household, yes, n (%) | 140 (47.5) | 116 (47.9) | 122 (48.4) | 107 (46.3) | 108 (47.4) | 94 (46.3) | 98 (47.3) |
| Infant’s grandmother living in same household, yes, n (%) | 85 (28.8) | 70 (28.9) | 72 (28.6) | 68 (29.4) | 68 (29.8) | 64 (31.5) | 64 (30.9) |
| Employed, yes, n (%) | 240 (81.4) | 195 (80.6) | 205 (81.4) | 195 (80.1) | 183 (80.3) | 166 (81.8) | 171 (82.6) |
| Depressive symptomsf,g, yes, n (%) | 80 (27.1) | 42 (18.2)a | 33 (14.5)a | 36 (17.7)a | 37 (18.5)a | 37 (20.8)a | 28 (15.8)a |
| Treatment group, interventionh, yes, n (%) | 140 (47.5) | 119 (49.2) | 123 (48.4) | 116 (50.2) | 114 (50.0) | 102 (50.3) | 106 (51.2) |
| Infant characteristics | |||||||
| Infant’s sleep locationg, n (%) | |||||||
| Parent’s bed | -- | 40 (16.7) | 58 (23.0)c | 64 (28.1)c | 64 (28.2)c | 64 (32.0)c | 72 (35.6)c |
| Parent’s room | -- | 187 (78.2) | 176 (69.8)c | 134 (58.8)c | 121 (53.3)c | 89 (44.5)c | 77 (38.1)c |
| Separate room away from parent | -- | 12 (5.0) | 18 (7.1) | 30 (13.2)c | 42 (18.5)c | 47 (23.5)c | 53 (26.2)c |
| Infant awakenings per nightg, mean (SD) | -- | 2.6 (1.0) | 1.8 (1.1)d | 1.6 (1.2)d | 1.5 (1.4)d | 1.1 (1.1)d | 1.0 (1.1)d |
| Maternal perception of an infant sleep problemg, yes, n (%) | -- | 32 (13.4) | 23 (9.1) | 28 (12.3) | 36 (15.9) | 29 (14.5) | 33 (16.0) |
| Infant dietg | |||||||
| Breastfeeding duration (months), mean (SD) | -- | 3.0 (3.3) | 3.1 (3.3) | 3.2 (3.3) | 3.0 (3.2) | 3.1 (3.2) | 3.3 (3.4)d |
| Still breastfeeding, yes, n (%) | -- | 196 (81.2) | 103 (43.3)c | 69 (31.2)c | 43 (20.5)c | 32 (17.0)c | 25 (12.5)c |
| Exclusively breastfeeding, yes, n(%) | -- | 48 (20.0) | 29 (18.8) | 5 (3.7)c | 0 (0.0)c | 0 (0.0)c | 0 (0.0)c |
| Infant temperamentg,i | |||||||
| Distress to limitations, mean score (SD) | -- | -- | 3.4 (0.7) | 3.4 (0.9) | 3.8 (0.9)e | 3.9 (0.9)e | -- |
| Activity level, mean score (SD) | -- | -- | 3.9 (1.0) | 4.4 (1.0)e | 4.6 (1.0)e | 4.4 (1.1)e | -- |
| Infant sex, male, n (%) | -- | 121 (50.6) | 123 (49.2) | 116 (50.2) | 113 (50.0) | 103 (51.0) | 105 (51.0) |
Note. N: Sample Size; SD: Standard Deviation; GED: General Education Development Test
Significantly different (P <0.05) from baseline visit in longitudinal logistic model testing for an effect of visit, controlling for repeated measures across subjects.
Significantly different (P <0.05) from baseline visit in longitudinal regression model testing for an effect of visit, controlling for repeated measures across subjects.
Significantly different (P <0.05) from month 1 visit in longitudinal logistic model testing for an effect of visit, controlling for repeated measures across subjects.
Significantly different (P <0.05) from month 1 visit in longitudinal regression model testing for an effect of visit, controlling for repeated measures across subjects.
Significantly different (P <0.05) from month 3 visit in longitudinal regression model testing for an effect of visit, controlling for repeated measures across subjects.
Presence of depressive symptoms indicated by score ≥16 on the Center for Epidemiological Studies-Depression Scale.
Denotes a time-varying characteristic (i.e., a characteristic that was measured at multiple time points); all other characteristics are time invariant.
Study intervention group received home visits from peer educators and materials used to promote responsive feeding and care.
Derived from the Infant Behavior Questionnaire-Revised (IBQ-R).
Predictors of infant sleep location
A number of maternal and infant characteristics were associated with bedsharing (Table 2; Supplementary Table 3). Compared to mothers who reported room-sharing, mothers were more likely to report bedsharing with their infant if they lived in the same house as the infant’s grandmother. Mothers were less likely to report bedsharing if they had a longer breastfeeding duration or if they lived in the same house as the infant’s father.
Table 2.
Maternal, infant, and household predictors of infant sleep arrangement
| Bedsharinga Relative Risk Ratio (95% CI) |
Separate Roomsb Relative Risk Ratio (95% CI) |
|
|---|---|---|
| Predictors | ||
| Depressive symptomsc, yes | 1.62 (1.04- 2.52) * | 1.06 (0.63-1.76) |
| Perception of an infant sleep problem, yes | 1.90 (1.21-2.99) * | 1.61 (0.91-2.85) |
| Maternal report of infant night-time awakenings | 1.08 (0.92-1.26) | 0.81 (0.65-1.01) |
| Maternal age (years) | 0.97 (0.94-1.02) | 1.04 (0.99-1.10) |
| Education | ||
| Some high school or less | Ref | Ref |
| High school or GED | 0.66 (0.35-1.24) | 1.55 (0.63-3.77) |
| Some college | 0.79 (0.43-1.46) | 2.66 (1.08-6.56) * |
| College graduate | 0.53 (0.26-1.10) | 4.48 (1.69-11.88) * |
| Marital status, married/partnered | 0.91 (0.56-1.45) | 1.97 (1.13-3.43) * |
| Pre-pregnancy BMI (kg/m2)d | 1.01 (0.98-1.04) | 0.97 (0.94-1.00) |
| Medicaid, yes | 1.02 (0.64-1.63) | 0.38 (0.22-0.65) * |
| Number of people living in household | 1.03 (0.92-1.16) | 0.79 (0.64-0.98) * |
| Infant’s father living in same household, yes | 0.62 (0.40-0.96) * | 1.78 (1.05-3.00) * |
| Infant’s grandmother living in same household, yes | 1.87 (1.19-2.95) * | 0.88 (0.51-1.54) |
| Breastfeeding duration | 0.90 (0.84-0.98) * | 1.04 (0.96-1.13) |
| Still breastfeeding, yes | 1.14 (0.70-1.84) | 0.81 (0.47-1.38) |
| Exclusive breastfeeding, yes | 0.56 (0.26-1.21) | 0.89 (0.24-3.33) |
| Infant activity levele | 0.87 (0.72-1.05) | 0.93 (0.72-1.20) |
| Infant distress to limitationse | 1.14 (0.91-1.43) | 0.89 (0.83-1.25) |
| Treatment group, interventionf | 1.22 (0.80-1.88) | 0.81 (0.47-1.38) |
Note. 95% CI: 95% Confidence Interval; Ref: Reference Group; GED: General Education Development Test; BMI: Body Mass Index
Represents likelihood of bed-sharing versus room-sharing adjusted for visit. Robust clusters were used to control for repeated measures across subjects.
Represents likelihood of infant sleeping in a separate room apart from their mother versus room-sharing adjusted for visit. Robust clusters are used to control for repeated measures across subjects.
Presence of depressive symptoms indicated by score ≥ 16 on the Center for Epidemiological Studies-Depression Scale.
Calculated from self-reported pre-pregnancy height and weight. Calculated by diving weight in kilograms (kg) by height in meters squared (m2).
Derived from the Infant Behavior Questionnaire-Revised (IBQ-R) at months 3, 6, 9, and 12.
Mothers in the obesity prevention intervention arm compared to the injury-prevention control arm.
p<0.05
Compared to mothers who reported room-sharing, mothers were more likely to report sleeping in a room separate from their infant if they were married or in a domestic partnership, had an education level of some college or higher, or if the infant’s father lived in the same household. Mothers were less likely to report their infant sleeping in a separate room if they were a Medicaid recipient, or if they had a larger number of people living in their household.
Presence of MDS and bedsharing
In concurrent mixed-effects multinomial models, presence of MDS was significantly associated with bedsharing (Table 3). Mothers who exhibited depressive symptomology had a higher likelihood of bedsharing, compared to room-sharing. These results were attenuated in the adjusted model controlling for study intervention group and maternal perception of an ISP. In the unadjusted lagged model, MDS at time 1 significantly predicted likelihood of bedsharing at time 2, these results were no longer significant in the adjusted model (Table 3; Figure 1).
Maternal report of ISP and bedsharing
In concurrent mixed-effects multinomial models, maternal perception of an ISP was significantly associated with bedsharing (Table 3). Mothers who stated their infant’s sleep was a problem had a higher likelihood of bedsharing, compared to room-sharing. These results remained significant in the adjusted model controlling for study intervention group and presence of MDS. In the unadjusted lagged model, maternal perception of an ISP at time 1 significantly predicted likelihood of bedsharing at time 2, these results were no longer significant in the adjusted model (Table 3; Figure 2).
Directionality of the associations between the presence of MDS, perception of an ISP, and bedsharing
Mothers who reported bedsharing at time t had significantly higher odds of MDS at time t+1 compared to mothers who reported room-sharing or sleeping in a separate room from their infant (Figure 1). These results persisted in adjusted models. Similarly, mothers who reported bedsharing at time t had significantly higher odds of reporting their infant’s sleep as a problem at time t+1 compared to those who were room-sharing or sleeping in separate rooms (Figure 2), these results also persisted in adjusted models.
DISCUSSION
In this study, we identified several sociodemographic characteristics associated with infant sleep location. Compared to room-sharing, infants were more likely to sleep in a room separate from their mother if their mother was married or in a domestic partnership, had an education level of at least some college, or if the infant’s father was living in the same household as the infant. The likelihood of the mother and infant sleeping in separate rooms was decreased among Medicaid recipients and larger households. Compared to room-sharing, the likelihood of bedsharing was increased if the mother had MDS, perceived an ISP, or the infant’s grandmother was living in the same household as the infant. The likelihood of bedsharing was decreased if the infant’s father was living in the same household as the infant, or the mother reported increased breastfeeding duration. We also documented that bedsharing predicted the presence of MDS and maternal perception of an ISP.
From 1 to 15 months postpartum, the prevalence of bedsharing increased, with over a third of mothers at the 15-month visit reporting they routinely bedshared. These levels are consistent with PRAMS data that noted 35.3% of NHB mothers, ranging from 2 to 6 months postpartum, reported “often or always” bedsharing.2 Similar to previous work,33 we found NHB mothers who lived in a different household from their infant’s father were more likely to bedshare, while NHB mothers who were married or cohabitating with their infant’s father were more likely to sleep in a room separate from their infant. Both bed and room-sharing have been previously associated with increased risk of marital discordance,34 indicating married mothers may choose to sleep in a room separate from their infant in order to limit martial conflict.
While the recent ABM guidelines referenced multiple sources that noted the positive relationship between bedsharing and breastfeeding,10 in our sample a longer breastfeeding duration was surprisingly associated with lower likelihood of bedsharing. This finding may be because most of the studies around bedsharing and breastfeeding duration have been conducted among non-Hispanic white mothers, who generally have lengthier breastfeeding durations compared to NHB mothers as a result of systemic, historical, and cultural barriers that make breastfeeding more challenging for NHB women.35 The majority of mothers in our sample were also unmarried, enrolled in Medicaid, and employed, all of which are factors associated with a shortened breastfeeding duration and may have influenced the relationship between bedsharing and breastfeeding duration seen in our analysis.36-38
Maternal perception of an ISP was concurrently associated with an increased likelihood of bedsharing. This finding is supported by evidence that has shown maternal perception of an ISP is correlated with increased nighttime awakenings and infants with increased nighttime awakenings, are more likely to bedshare.15 Despite the significant concurrent relationship, maternal perception of an ISP was not predictive of bedsharing. Qualitative evidence has shown the decision to bedshare is most commonly driven by breastfeeding status, convenience, tradition, and household composition.12,19 While maternal perception of an ISP was related to bedsharing in this study, it appears a mother’s decision to bedshare was not a reaction to their infant’s sleep problem.
The concurrent relationship between MDS and bedsharing was attenuated after adjustment for maternal perception of ISP. This finding may reflect the importance of the relationship between MDS and perception of an ISP on the decision to bedshare. In this cohort, MDS were concurrently and longitudinally associated with maternal perception of an ISP and vice versa (data not shown). While the reciprocal pathway between maternal mental health and infant sleep has been established,21 what remains unclear is how this pathway applies to bedsharing mothers. Previous studies have found MDS are higher among bedsharing mothers,33 mothers who report an ISP,39 and mothers who self-reported poor sleep quality.20 Our current analysis provides a potential mechanism linking perception of an ISP to bedsharing and MDS: Bedsharing mothers who perceive their infants to have a sleep problem may have an increased likelihood of poor sleep quality,8 subsequently increasing their risk of depressive symptoms, which in turn could affect their perception of their infant’s sleep. In support of this mechanism, we found that bedsharing predicted MDS and maternal perception of an ISP. We are not aware of other studies examining directionality between bedsharing, MDS, and maternal perception of an ISP; however, among co-sleeping (bedsharing or room-sharing) mothers and toddlers, maternal sleep duration mediated the relationship between perception of toddler sleep problems and maternal mental health symptoms.40
This study is one of the first to analyze the directionality among MDS, perception of an ISP, and bedsharing among a sample of predominantly low-income, NHB mother-infant pairs. The longitudinal data enabled us to assess predictors of and changes in infant sleep arrangement throughout infancy. This study fills an important gap in the literature, as the majority of studies on infant sleep arrangement and maternal mental health have not addressed this topic among NHB women,16,20 or have not differentiated between bedsharing and room-sharing within their analyses.40 Given that NHB mothers are more likely to bedshare2 and experience postpartum depression,4 assessing how bedsharing may impact NHB mothers is especially important. Despite its strengths, this analysis contained several limitations. All measures were collected via maternal self-report, which may have led to shared method variance. Research also suggests subjective sleep measures are more likely to reflect poor maternal sleep outcomes.8,13 Additionally, mothers may have been less likely to self-report behaviors that contradicted the AAP infant sleep recommendations (e.g.. bedsharing). The small sample size of mothers who reported their infant’s sleep as “a very serious problem” prevented us from comparing them to mothers who reported their infant’s sleep as “a small problem.” We do not have a record of the physical size of the home or the number of bedrooms. It is possible that the choice to bedshare is related to the availability of space and that low availability of space and lack of autonomy to choose one’s preferred sleeping arrangement are factors underlying these relationships. Finally, we did not measure maternal sleep duration which could influence both MDS and maternal perception of an ISP, independent of bedsharing. Studies should aim to collect objective maternal-infant sleep measures. It would also be useful to collect prenatal data on preferred infant sleep location, this would enable researchers to further examine the relationships between infant sleep location and health outcomes, potentially providing a stronger understanding of the direction of these relationships.
CONCLUSION
Infant sleep location is debated due to the contrasting recommendations around SIDS reduction versus increased breastfeeding duration. This paper documents a high prevalence of bedsharing among low-income, NHB mothers. Mothers who perceived their infant’s sleep to be a problem had an increased likelihood of bedsharing. We also documented that bedsharing is predictive of MDS and maternal perception of an ISP. While bedsharing has been associated with positive infant health outcomes, maternal mental health and sleep may be adversely impacted. We suggest health professionals acknowledge that the choice to bedshare is driven by a complex interaction of individual, cultural, and social factors. They should aim to provide safe-sleep guidelines for mothers who intend to bedshare and discuss the conflicting infant sleep recommendations with their patients. We hope these findings will highlight the importance of enacting research and recommendations that recognize the dyadic nature of maternal and infant sleep.
Supplementary Material
ACKNOWLEDGEMENTS
This study was supported by a grant from the National Institute of Child Health and Human Development (NICHD), R01HD073237 [to M.E. Bentley]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Abbreviations:Non-Hispanic Black (NHB); American Academy of Pediatrics (AAP); Sudden Infant Death Syndrome (SIDS); Academy of Breastfeeding Medicine (ABM); maternal depressive symptoms (MDS); infant sleep problem (ISP); Brief Infant Sleep Questionnaire (BISQ); Center for Epidemiological Depression (CESD)
DISCLOSURE STATEMENT
The authors report no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Colson ER, Willinger M, Rybin D, et al. Trends and factors associated with infant bed sharing, 1993-2010: the National Infant Sleep Position Study. JAMA Pediatr. 2013;167(11):1032–1037. doi: 10.1001/jamapediatrics.2013.2560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bombard JM, Kortsmit K, Warner L, et al. Vital Signs: Trends and Disparities in Infant Safe Sleep Practices - United States, 2009-2015. MMWR Morb Mortal Wkly Rep. 2018;67(1):39–46. doi: 10.15585/mmwr.mm6701e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luijk MPCM, Mileva-Seitz VR, Jansen PW, et al. Ethnic differences in prevalence and determinants of mother-child bed-sharing in early childhood. Sleep Med. 2013;14(11):1092–1099. doi: 10.1016/j.sleep.2013.04.019 [DOI] [PubMed] [Google Scholar]
- 4.Liu CH, Giallo R, Doan SN, Seidman LJ, Tronick E. Racial and ethnic differences in prenatal life stress and postpartum depression symptoms. Arch Psychiatr Nurs. 2016;30(1):7–12. doi: 10.1016/j.apnu.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 5.Doering JJ, Salm Ward TC, Strook S, Campbell JK. A comparison of infant sleep safety guidelines in nine industrialized countries. J Community Health. 2019;44(1):81–87. doi: 10.1007/s10900-018-0556-3 [DOI] [PubMed] [Google Scholar]
- 6.Moon RY, TASK FORCE ON SUDDEN INFANT DEATH SYNDROME. SIDS and Other Sleep-Related Infant Deaths: Evidence Base for 2016 Updated Recommendations for a Safe Infant Sleeping Environment. Pediatrics. 2016;138(5). doi: 10.1542/peds.2016-2940 [DOI] [PubMed] [Google Scholar]
- 7.Paul IM, Hohman EE, Loken E, et al. Mother-Infant Room-Sharing and Sleep Outcomes in the INSIGHT Study. Pediatrics. 2017;140(1). doi: 10.1542/peds.2017-0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volkovich E, Bar-Kalifa E, Meiri G, Tikotzky L. Mother-infant sleep patterns and parental functioning of room-sharing and solitary-sleeping families: a longitudinal study from 3 to 18 months. Sleep. 2018;41(2). doi: 10.1093/sleep/zsx207 [DOI] [PubMed] [Google Scholar]
- 9.Marinelli KA, Ball HL, McKenna JJ, Blair PS. An Integrated Analysis of Maternal-Infant Sleep, Breastfeeding, and Sudden Infant Death Syndrome Research Supporting a Balanced Discourse. J Hum Lact. 2019;35(3):510–520. doi: 10.1177/0890334419851797 [DOI] [PubMed] [Google Scholar]
- 10.Blair PS, Ball HL, McKenna JJ, et al. Bedsharing and breastfeeding: the academy of breastfeeding medicine protocol #6, revision 2019. Breastfeed Med. 2020;15(1):5–16. doi: 10.1089/bfm.2019.29144.psb [DOI] [PubMed] [Google Scholar]
- 11.Ward TCS. Reasons for mother-infant bed-sharing: a systematic narrative synthesis of the literature and implications for future research. Matern Child Health J. 2015;19(3):675–690. doi: 10.1007/s10995-014-1557-1 [DOI] [PubMed] [Google Scholar]
- 12.Joyner BL, Oden RP, Ajao TI, Moon RY. Where Should My Baby Sleep: A Qualitative Study of African American Infant Sleep Location Decisions . J Natl Med Assoc. 2010;102(10):881–889. [DOI] [PubMed] [Google Scholar]
- 13.Volkovich E, Ben-Zion H, Karny D, Meiri G, Tikotzky L. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep Med. 2015;16(11):1305–1312. doi: 10.1016/j.sleep.2015.08.016 [DOI] [PubMed] [Google Scholar]
- 14.Mindell JA, Leichman ES, Walters RM. Sleep location and parent-perceived sleep outcomes in older infants. Sleep Med. 2017;39:1–7. doi: 10.1016/j.sleep.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 15.Bruni O, Baumgartner E, Sette S, et al. Longitudinal study of sleep behavior in normal infants during the first year of life. J Clin Sleep Med. 2014;10(10):1119–1127. doi: 10.5664/jcsm.4114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teti DM, Crosby B. Maternal depressive symptoms, dysfunctional cognitions, and infant night waking: the role of maternal nighttime behavior. Child Dev. 2012;83(3):939–953. doi: 10.1111/j.1467-8624.2012.01760.X [DOI] [PubMed] [Google Scholar]
- 17.Lerner RE, Camerota M, Tully KP, Propper C. Associations between mother-infant bed-sharing practices and infant affect and behavior during the still-face paradigm. Infant Behav Dev. 2020;60:101464. doi: 10.1016/j.infbeh.2020.101464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culver ED. Exploring bed-sharing mothers’ motives and decision-making for getting through the night intact: a grounded theory. J Midwifery Womens Health. 2009;54(5):423–423. doi: 10.1016/j.jmwh.2009.06.010 [DOI] [Google Scholar]
- 19.Ball HL. Reasons to bed-share: Why parents sleep with their infants. J Reprod Infant Psychol. 2002;20(4):207–221. doi: 10.1080/0264683021000033147 [DOI] [Google Scholar]
- 20.Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32(7):847–855. doi: 10.1093/sleep/32.7.847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. doi: 10.1016/j.smrv.2009.05.003 [DOI] [PubMed] [Google Scholar]
- 22.Wasser HM, Thompson AL, Suchindran CM, et al. Family-based obesity prevention for infants: Design of the “Mothers & Others” randomized trial. Contemp Clin Trials. 2017;60:24–33. doi: 10.1016/j.cct.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wasser HM, Thompson AL, Suchindran CM, et al. Home-based intervention for non- Hispanic black families finds no significant difference in infant size or growth: results from the Mothers & Others randomized controlled trial. BMC Pediatr. 2020;20(1):385. doi: 10.1186/s12887-020-02273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–7. doi: 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- 25.Hirai AH, Kortsmit K, Kaplan L, et al. Prevalence and factors associated with safe infant sleep practices. Pediatrics. 2019;144(5). doi: 10.1542/peds.2019-1286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 27.Sit DKY, Wisner KL. Identification of postpartum depression. Clin Obstet Gynecol. 2009;52(3):456–468. doi: 10.1097/GRF.0b013e3181b5a57c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behavior and Development. 2003;26(1):64–86. doi: 10.1016/S0163-6383(02)00169-8 [DOI] [Google Scholar]
- 29.Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant Feeding Practices Study II: study methods. Pediatrics. 2008;122 Suppl 2:S28–35. doi: 10.1542/peds.2008-1315c [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Questionnaires: Breastfeeding and Infant Feeding Practices. Breastfeeding and infant feeding practices. https://www.cdc.gov/breastfeeding/data/ifps/questionnaires.htm. Published 2019. Accessed December 1, 2020. [Google Scholar]
- 31.Bliss R, Weinberg J, Webster T, Vieira V. Determining the probability distribution and evaluating sensitivity and false positive rate of a confounder detection method applied to logistic regression. J Biom Biostat. 2012;3(4):142. doi: 10.4172/2155-6180.1000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fagerland MW, Hosmer DW, Bofin AM. Multinomial goodness-of-fit tests for logistic regression models. Stat Med. 2008;27(21):4238–4253. doi: 10.1002/sim.3202 [DOI] [PubMed] [Google Scholar]
- 33.Salm Ward TC, Robb SW, Kanu FA. Prevalence and Characteristics of Bed-Sharing Among Black and White Infants in Georgia. Matern Child Health J. 2016;20(2):347–362. doi: 10.1007/s10995-015-1834-7 [DOI] [PubMed] [Google Scholar]
- 34.Teti DM, Shimizu M, Crosby B, Kim B-R. Sleep arrangements, parent-infant sleep during the first year, and family functioning. Dev Psychol. 2016;52(8):1169–1181. doi: 10.1037/dev0000148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asiodu IV, Bugg K, Palmquist AEL. Achieving breastfeeding equity and justice in black communities: past, present, and future. Breastfeed Med. 2021;16(6):447–451. doi: 10.1089/bfm.2020.0314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mercier RJ, Burcher TA, Horowitz R, Wolf A. Differences in breastfeeding among medicaid and commercially insured patients: A retrospective cohort study. Breastfeed Med. 2018;13(4):286–291. doi: 10.1089/bfm.2017.0228 [DOI] [PubMed] [Google Scholar]
- 37.Cooklin AR, Donath SM, Amir LH. Maternal employment and breastfeeding: results from the longitudinal study of Australian children. Acta Paediatr. 2008;97(5):620–623. doi: 10.1111/j.1651-2227.2008.00740.x [DOI] [PubMed] [Google Scholar]
- 38.Brand E, Kothari C, Stark MA. Factors related to breastfeeding discontinuation between hospital discharge and 2 weeks postpartum. J Perinat Educ. 2011;20(1):36–44. doi: 10.1891/1058-1243.20.1.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Halal CS, Bassani DG, Santos IS, et al. Maternal perinatal depression and infant sleep problems at 1 year of age: Subjective and actigraphy data from a population-based birth cohort study. J Sleep Res. April 2020:e13047. doi: 10.1111/jsr.13047 [DOI] [PubMed] [Google Scholar]
- 40.Covington LB, Armstrong B, Black MM. Perceived Toddler Sleep Problems, Co-sleeping, and Maternal Sleep and Mental Health. J Dev Behav Pediatr. 2018;39(3):238–245. doi: 10.1097/DBP.0000000000000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


